Abstract
Purpose: The aim of this study was to document the types of treatment that Quebec physiotherapists use for knee osteoarthritis (OA), to assess whether treatment choices are consistent with current practice guidelines, and to explore the factors associated with using certain treatments. Method: Physiotherapists in Quebec answered a cross-sectional survey that was sent through licensing bodies and social media contacts. The respondents were asked which treatments they would use for a typical case of knee OA. We used descriptive statistics to determine the proportions of physiotherapists who chose each treatment and explored the associations between the use of treatments and demographic factors. Results: A total of 195 Quebec physiotherapists participated in this study, 74.9% of whom were women. The most common treatment choices were mobility exercises (96.4%), followed by education (93.8%), strengthening exercises (85.1%), thermotherapy and cryotherapy (72.3%), manual therapy (53.3%), and electrotherapy (42.1%). Selecting either manual or electrotherapy was significantly associated with working in private practice. Conclusions: The great majority of physiotherapists included mobility and strengthening exercises, both of which are the recommended approaches for treating knee OA. Physiotherapists in private practice were more likely to select manual therapy and electrotherapy.
Key Words: electric stimulation therapy; exercise therapy; musculoskeletal manipulations; osteoarthritis, knee; practice guideline
Mots-clés : : arthrose, directives cliniques, genou, manipulations musculosquelettiques, thérapie par l’exercice, thérapie par électrostimulation
Abstract
Objectif : exposer les types de traitements qu’utilisent les physiothérapeutes du Québec pour l’arthrose du genou, afin d’évaluer si leurs choix respectent les directives cliniques actuelles, et explorer les facteurs associés à l’utilisation de certains traitements. Méthodologie : les physiothérapeutes du Québec ont participé à un sondage transversal qui leur a été transmis par leurs organismes de réglementation et les médias sociaux. Les répondants ont été invités à indiquer quel type de traitement ils utiliseraient dans un cas typique d’arthrose du genou. Les chercheurs ont utilisé des statistiques descriptives pour déterminer les proportions de physiothérapeutes choisissant chaque traitement et ont exploré les associations entre des traitements sélectionnés et des facteurs démographiques. Résultats : au total, 195 physiothérapeutes du Québec, dont 74,9 % de femmes, ont participé à la présente étude. Les traitements les plus choisis étaient les exercices de mobilité (96,4 %), l’éducation (93,8 %), les exercices de renforcement (85,1 %), la thermothérapie et la cryothérapie (72,3 %), la thérapie manuelle (53,3 %) et l’électrothérapie (42,1 %). Le choix de la thérapie manuelle ou de l’électrothérapie était significativement associé au travail en pratique privée. Conclusion : la grande majorité des physiothérapeutes ont sélectionné les exercices de mobilité et de renforcement, qui représentent les approches recommandées pour le traitement de l’arthrose du genou. Les physiothérapeutes en pratique privée étaient plus susceptibles de sélectionner la thérapie manuelle et l’électrothérapie.
Osteoarthritis (OA) is a very common disease among adults, with one Canadian in eight (13%) reportedly affected in 2011,1 and knee OA is among the most common types.1 Non-pharmacologic treatments for knee OA include a wide array of physiotherapy (PT) interventions. In the context of this study, we reviewed the literature to determine current best practice guidelines for knee OA, selecting high-quality articles that addressed non-pharmacologic treatments for knee OA. Research has shown that therapeutic exercises are recommended as the main non-pharmacologic treatment for knee OA.2–9
More specifically, three treatments are widely recommended to improve knee OA outcomes: exercise therapy,2–7,9,10 weight loss,2,4,6,8 and walking aids.2,4,8 There is controversy about the evidence for recommending patient education without exercise and manual therapy on its own.2,4,8,9,11–14 With respect to electrotherapy (transcutaneous electrical nerve stimulation), the data vary from recommended,11 to conditional,2,4,12 to uncertain,8,13 and no benefit.9 Data on the effectiveness of ultrasound show some benefit,9 uncertain,8 and no benefit.13 Despite some recent opinions that the evidence is insufficient,9,13 for the most part the use of heat or cold,4,11–13 knee braces, and insoles and shoes are recommended (the literature has not reported a specific type of shoe; patients may consult a podiatrist for footwear advice).2,4,8,11,12
Although there is evidence that certain non-surgical and non-pharmacologic approaches are effective, the extent to which these are used in clinical practice in Canada is not known. In Ireland and in the United Kingdom, most physiotherapists used exercise therapy for knee OA, but almost two-thirds of them also used electrotherapy and manual therapy.15–17 A Canadian qualitative study found that therapeutic exercise was a mainstay of treatment, and it identified a set of barriers to and facilitators of managing patients with knee OA.18 However, to our knowledge, no larger scale surveys in Canada have investigated the choice of treatment for patients with knee OA.
This study was carried out in Quebec, the second-most populous province in Canada. Since 2015, the law in Quebec permits physiotherapists to refer patients directly to medical specialists. In this context, we sought to determine whether physiotherapists were able to correctly identify suspected cases of new-onset inflammatory arthritis versus OA and whether they managed these cases appropriately. For this article, we considered only cases of knee OA. The specific goal of our study was to document what types of modalities Quebec physiotherapists used for a case scenario representing a patient with knee OA and to assess whether this choice was consistent with current clinical practice guidelines as explained earlier (exercise therapy, weight loss, walking aids). We also sought to identify the factors associated with selecting various treatments for knee OA.
Methods
We performed a cross-sectional survey of physiotherapists who worked in the musculoskeletal field in the province of Quebec. We recruited licensed physiotherapists by sending out emails through l’Ordre professionnel de la physiothérapie du Québec (Quebec Professional Order of Physiotherapy). Two other physiotherapist associations – Canadian Physiotherapy Association and Fédération des Cliniques de Physiothérapie du Québec (Quebec Federation of Physiotherapy Clinics) also publicized the survey through their social media. We excluded physiotherapists who were not licensed to work in Quebec. We housed the survey on a protected SurveyMonkey online platform (SurveyMonkey Inc., San Mateo, CA), and it was active from April to October 2018. We obtained ethical approval for this project from the Ethics Committee of the Université de Montréal, and participants consented to participate after reading an informed consent form.
Members of our team (physiotherapists and rheumatologists) designed the survey questionnaire in both English and French, and physiotherapists pretested it in both languages before it was sent out. It collected demographic (age, gender) and workplace information (type of clientele, private clinic vs. public institution, solo vs. group practice) and presented four case scenarios in which physiotherapists had to identify the most likely medical diagnosis (new-onset rheumatoid arthritis, knee OA, new-onset ankylosing spondylitis, or low back pain). Each scenario asked the respondents which treatments they would use and how important referring to other specialists would be. The main study goal was to determine whether physiotherapists were able to correctly identify cases of new-onset inflammatory arthritis versus OA and whether they managed these cases appropriately. For this article, we only considered the knee OA case.
The knee OA scenario represented an uncomplicated case of mild chronic knee pain in a 55-year-old man, as follows:
Mr. Y. is a 55-year-old man who has had an increase in pain in both his knees (left > right) over the past 5 years. He also has pain in both hands and feet. Pain increases with activity and can reach up to 8 out of 10 on the visual analogue pain scale. Upon physical examination, he presents with deformities in both hands and pain of 2 out of 10 on palpation in the proximal interphalangeal joints and distal interphalangeal joints. There are nodules on the distal interphalangeals bilaterally. He also presents with various deformities in both knees (left > right) with no effusion, but there is crepitus and pain upon movement. He has mild pain (2 out of 10) in his feet at the metatarsophalangeal joints and has hallux valgus deformities bilaterally. He has decreased range of motion in flexion in both knees (R: 105 out of 111, L: 92 out of 101) and decreased muscle strength in extension in both knees (4 out of 5 from the muscle manual testing). Over the past year, his walking distance without an aid has gone down to 100 m. With a cane, he can walk up to 300 m. He has increased difficulty going up and down stairs without support. Applying ice helps reduce the pain slightly.
Data analysis consisted of performing univariate analyses to compile a description of our sample, and we also used χ2 analyses to compare the results from our sample with statistics for the physiotherapist workforce in Quebec collected by the Canadian Institute for Health Information.19 Next, we examined the frequency of use of the various modalities. We then used inferential statistics (bivariate comparisons and logistic regression) to determine the associations among demographic factors, workplace characteristics, correct identification of the diagnosis as knee OA, and use of certain modalities, notably exercises, electrotherapy, use of heat or cold, and manual therapy. To carry out these analyses, we used IBM SPSS Statistics, Version 25 (IBM Corporation, Armonk, NY).
To address any potential sources of bias, we asked the participants to, before answering the questions attached to the vignettes, “Answer the questions according to what you really do in your current clinical practice.”
Results
A total of 299 Quebec physiotherapists responded to the survey; 21 responded to the English version and 278 to the French version. We excluded data from 1 physiotherapist who did not treat patients with musculoskeletal problems. Of the final 298 respondents, 195 completed the questions on the knee OA case and were therefore included in our analyses.
According to 2011 national statistics, 1,850 physiotherapists were working in the musculoskeletal field in Quebec.19 Thus, our sample of 195 represents an 11% response rate. Table 1 presents the demographic and workplace characteristics of the study participants. Our sample was similar to that of the provincial physiotherapist population with respect to age, gender, and sector of practice; however, our sample had more physiotherapists working in rural areas than urban (14% vs. 8%, p = 0.007) and more physiotherapists with higher than a bachelor’s-level education than with a BSc (40% vs. 21%, p < 0.001).
Table 1.
Demographic and Workplace Characteristics of Study Respondents (N = 195)
| Characteristic and category | No. (%) of respondents |
|---|---|
| Age group, y | |
| 18–34 | 76 (39.0) |
| 35–45 | 51 (26.2) |
| 46–55 | 45 (23.1) |
| 56–65 | 22 (11.3) |
| > 65 | 1 (0.5) |
| Gender | |
| Male | 48 (24.6) |
| Female | 146 (74.9) |
| Other | 1 (0.5) |
| Highest level of education | |
| Bachelor’s | 117 (60.0) |
| Professional master’s | 53 (27.2) |
| Research master’s | 22 (11.3) |
| Professional doctorate | 1 (0.5) |
| Research doctorate | 2 (1.0) |
| University of graduation for PT entry to practice degree | |
| Université de Montréal | 90 (46.2) |
| McGill University | 45 (23.1) |
| Université Laval | 41 (21.0) |
| Université de Sherbrooke | 2 (1.0) |
| Other Canadian university | 10 (5.1) |
| University outside Canada | 7 (3.6) |
| Experience, y | |
| 0–5 | 46 (23.6) |
| 6–10 | 27 (13.8) |
| 11–15 | 35 (17.9) |
| 16–20 | 16 (8.2) |
| 21–25 | 20 (10.3) |
| > 25 | 51 (26.2) |
| Post-graduate courses taken* | |
| Manual therapy | 155 (79.5) |
| McKenzie | 58 (29.7) |
| Sport PT | 56 (28.7) |
| Approach to chronic pain | 50 (25.6) |
| Osteopathy | 28 (14.4) |
| Rheumatology | 10 (5.1) |
| Electrotherapy | 3 (1.5) |
| Other | 63 (32.3) |
| None | 16 (8.2) |
| Caseload,† % | |
| 1–25 | 16 (8.2) |
| 26–50 | 13 (6.7) |
| 51–75 | 22 (11.3) |
| 76–100 | 144 (73.8) |
| Age group of patients, y | |
| Paediatric (0–17) | 13 (6.7) |
| Adult (18–65) | 154 (79.0) |
| Elderly (> 65) | 28 (14.4) |
| Sector of practice | |
| Private | 95 (48.7) |
| Public | 71 (36.4) |
| Private and public | 29 (14.9) |
| Type of practice | |
| Solo | 43 (22.1) |
| Group (PT professionals only) | 26 (13.3) |
| Group (PT professionals and other health professionals without a physician) | 63 (32.3) |
| Group (PT professionals and other health professionals including a physician) | 63 (32.3) |
| Geographical distribution | |
| Urban | 168 (86.2) |
| Rural | 27 (13.8) |
Note: Percentages may total more than 100 because of rounding.
Courses taken after the entry-to-practice degree to specialize in certain areas of PT; respondents could take more than one.
Percentage of patients seen by therapists who present with musculoskeletal pathologies.
PT = physiotherapy.
Of the 195 respondents who completed the questions on the knee OA scenario, 83% (161) correctly diagnosed the knee OA case. We present the treatment choices for this scenario in Figure 1. Almost all the respondents selected mobility exercises (96%) and patient education (94%), and a large majority chose strengthening exercises (85%). Seventy-two percent would use heat or cold, 53% would use manual therapy, and 42% would use electrotherapy.
Figure 1 .
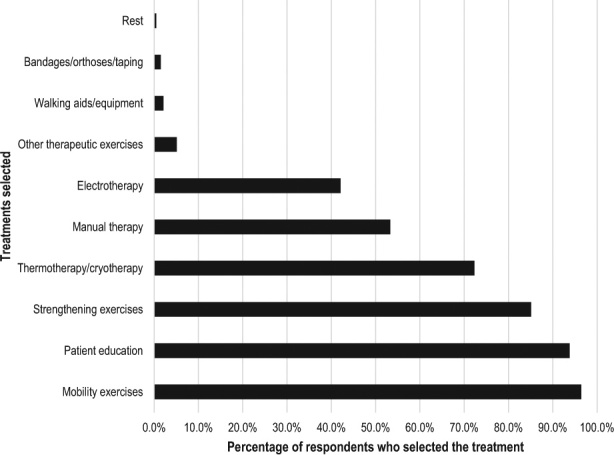
Treatments selected by the respondents for the case of knee osteoarthritis.
Almost all the respondents selected mobility exercises and patient education, so we did not analyze the factors associated with using these modalities. However, we analyzed the factors associated with using strengthening exercises, electrotherapy, heat or cold therapy, and manual therapy. We present the bivariate analysis of factors associated with using these four modalities in Table 2.
Table 2.
Factors Associated with Selecting Different Treatments for a Case of Knee OA (Bivariate Analysis: χ2 or Fisher’s Exact Test)
| Factor and category | Electrotherapy |
Thermotherapy or cryotherapy |
Manual therapy |
Strengthening exercises |
||||
|---|---|---|---|---|---|---|---|---|
| % selecting | p-value | % selecting | p-value | % selecting | p-value | % selecting | p-value | |
| > 50% MSK caseload | ||||||||
| No | 31.0 | 0.19 | 72.4 | 0.99 | 20.7 | < 0.001 | 86.2 | 1.00 |
| Yes | 44.0 | 72.3 | 59.0 | 84.9 | ||||
| Gender | ||||||||
| Female | 41.1 | 0.56 | 72.6 | 0.97 | 50.7 | 0.15 | 85.6 | 0.70 |
| Male | 45.8 | 72.9 | 62.5 | 83.3 | ||||
| Level of education beyond bachelor’s degree | ||||||||
| No | 39.7 | 0.41 | 70.7 | 0.54 | 48.3 | 0.09 | 81.9 | 0.012 |
| Yes | 45.6 | 74.7 | 60.8 | 89.9 | ||||
| Experience, y | ||||||||
| < 5 | 39.1 | 0.64 | 73.9 | 0.73 | 60.9 | 0.19 | 89.1 | 0.34 |
| 6–20 | 46.2 | 69.2 | 56.4 | 87.2 | ||||
| ≥ 21 | 39.4 | 74.6 | 45.1 | 80.3 | ||||
| Sector of practice | ||||||||
| Private | 49.5 | 0.041 | 70.5 | 0.59 | 76.8 | < 0.001 | 84.2 | 0.73 |
| Public | 35.0 | 74.0 | 31.0 | 86.0 | ||||
| Urban–rural | ||||||||
| Urban | 41.7 | 0.79 | 72.0 | 0.83 | 52.4 | 0.51 | 83.3 | 0.09 |
| Rural | 44.4 | 74.1 | 59.3 | 96.3 | ||||
| Type of practice | ||||||||
| Solo | 46.5 | 0.72 | 65.1 | 0.35 | 62.8 | 0.027 | 86.0 | 0.84 |
| Group with no medical doctor | 39.1 | 71.3 | 58.6 | 83.9 | ||||
| Group with medical doctor | 41.3 | 77.8 | 39.7 | 87.3 | ||||
| Manual therapy or osteopathy courses taken | ||||||||
| Yes | 44.1 | 0.21 | 72.7 | 0.81 | 61.5 | <0.001 | 84.5 | 0.58 |
| No | 32.4 | 70.6 | 14.7 | 88.2 | ||||
| Chronic pain, sports PT, or electrotherapy courses taken | ||||||||
| Yes | 45.5 | 0.38 | 63.6 | 0.014 | 62.5 | 0.020 | 85.2 | 0.97 |
| No | 39.3 | 79.4 | 45.8 | 85.0 | ||||
| Any post-graduate courses taken | ||||||||
| Yes | 41.3 | 0.50 | 72.1 | 1.00 | 57 | 0.001 | 85.5 | 0.71 |
| No | 50.0 | 75.0 | 12.5 | 81.3 | ||||
| Correctly diagnosed OA | ||||||||
| Yes | 43.5 | 0.38 | 73.9 | 0.28 | 56.5 | 0.05 | 87.6 | 0.036 |
| No | 35.3 | 64.7 | 38.2 | 73.5 | ||||
OA = osteoarthritis; MSK = musculoskeletal; PT = physiotherapy.
Selecting strengthening exercises was significantly associated with correctly diagnosing knee OA (p = 0.036), and using electrotherapy was associated with working in the private sector (p = 0.041). Using heat or cold was, interestingly, associated with not having taken any of the following courses: chronic pain, sports PT, and electrotherapy (p = 0.014). However, selecting manual therapy as a treatment was associated with several factors: having a larger caseload in the musculoskeletal area (p < 0.001); working in the private sector (p < 0.001) and as a solo practitioner (p = 0.027); and having taken courses on manual therapy or osteopathy (p < 0.001), having taken courses on chronic pain, sports PT or electrotherapy (p = 0.020), and having taken any courses versus no courses in the musculoskeletal area (p = 0.001).
We then constructed a logistic model to determine which factors were independently associated with selecting manual therapy (see Table 3). Having less experience, working in the private sector, and having taken either manual therapy or osteopathy post-graduate courses were independently associated with choosing manual therapy. However, correctly diagnosing the case of knee OA was not associated with selecting manual therapy.
Table 3.
Factors Associated with Selecting Manual Therapy as a Treatment for Knee OA (Multiple Logistic Regression)
| Factor | OR (95% CI) | p-value |
|---|---|---|
| Caseload > 50% MSK | 1.88 (0.60, 5.87) | 0.28 |
| Male gender | 1.08 (0.47, 2.48) | 0.86 |
| Education: higher than bachelor’s degree | 0.80 (0.31, 2.07) | 0.65 |
| Experience, y | ||
| 21+ (Ref.) | 1.00 | |
| < 5 | 4.02 (1.11, 14.55) | 0.03 |
| 6–20 | 2.54 (1.11, 5.80) | 0.03 |
| Working in the public sector | 0.20 (0.09, 0.44) | < 0.01 |
| Courses: manual therapy and/or osteopathy | 7.38 (2.29, 23.75) | < 0.01 |
| Sector of practice | ||
| Works in a group with a physician (Ref.) | 1.00 | |
| Works in solo practice | 1.30 (0.46, 3.63) | 0.62 |
| Works in a group without a physician | 1.12 (0.49, 2.58) | 0.79 |
| Correctly diagnosing the case of knee OA | 2.40 (0.96, 6.01) | 0.06 |
OA = osteoarthritis; OR = odds ratio; MSK = musculoskeletal; Ref. = reference.
We also reanalyzed the data for the subsample of those who had correctly diagnosed the case of knee OA (161). The results of the logistic regression were similar except that we did not find an association between experience and use of manual therapy.
Discussion
The vast majority of physiotherapists in Quebec would use mobility or strengthening exercises or patient education to treat knee OA. This is in line with current clinical practice guidelines, which strongly recommend therapeutic exercises. In fact, physiotherapists who correctly diagnosed the scenario as knee OA were more likely to select strengthening exercises.
Current literature considers patient education, particularly in conjunction with exercise, to be a beneficial intervention.2,4,6,8,11,13 In general, patients who are educated about their condition are more satisfied, may adhere more to treatment, and have better outcomes.6
We found that more than 40% of physiotherapists would use electrotherapy, even though the evidence for its efficacy in knee OA is uncertain;7–9,20 in addition, more than 70% of respondents would use heat (which is for the most part recommended)4,11–13 or cold despite the low degree of evidence for the latter (although it has been shown that cold packs decrease knee swelling).21 A little more than half of the physiotherapists would use manual therapy despite the lack of evidence to recommend this mode of treatment on its own.2,4
It must be pointed out that clinical practice guidelines have changed over the years,8 and some may judge the existing data to be insufficient to guide their practice. Other reasons why physiotherapists may use modalities that are not part of OA recommendations may be that they typically use these modalities to relieve pain (e.g., electrotherapy, ice) and as an adjunct either at the beginning or at the end of a session to reduce discomfort that a patient may have had during PT.22 Our questionnaire did not ask whether the physiotherapists would use heat or cold in a therapy session versus suggesting the patient use heat or cold at home.
An interesting finding is that physiotherapists working in the private sector tended to use electrotherapy and manual therapy more often than those in the public sector. Manual therapy is a very common treatment used by therapists working in private practice with a musculoskeletal clientele.6 Another reason for this finding may be the gradual reduction of outpatient PT service delivery in the Quebec public sector, as well as across Canada. This means that the majority of patients receiving PT in the public sector are receiving in-patient therapy after surgery or have been recently discharged from hospital.23 Physical therapists in the public sector manage very few patients receiving non-surgical treatment of their knee OA24 and certainly not on regular repeated occasions, whereas they would receive a series of electrotherapy or manual therapy treatments in the private sector.
It is not surprising that the physiotherapists who had taken continuing education courses in manual therapy and osteopathy were the ones who selected manual therapy as an option for treating knee OA, as were those with less clinical experience. This may be explained by the fact that, in Quebec, PT schools only began to teach manual therapy as a part of the core curriculum (and not solely as a post-graduate course) during the mid-1990s. Also, physiotherapists who had taken post-graduate courses in chronic pain, sports PT, or electrotherapy chose heat or ice treatment less often than did physiotherapists who had not taken any of those courses. Physiotherapists who opt to take such courses may be representative of professionals who use more evidence-based approaches.
Our sample of Quebec physiotherapists overwhelmingly selected exercise to treat knee OA, and this finding is similar to the results of studies carried out in the United Kingdom and Ireland.15–17 In our study, fewer respondents selected both manual therapy and electrotherapy than other studies, possibly reflecting the increasing shift over the past decade toward evidence-based practice. Thermotherapy use was similar in Ireland and Quebec (in the 70% range).15
Given that clinical recommendations are constantly evolving, adhering to guidelines can be subject to several barriers, such as the practitioner’s understanding and willingness to accept a guideline, as well as feasibility, accessibility, and acceptability to patients.25 Abandoning current practices is also very challenging for some health professionals,25 especially because guidelines do not always take into account patients’ individual contexts.26
Our study had several limitations. The main one, and one that is common to all surveys, is selection bias, which may limit the generalizability of our results to the wider population of physiotherapists. Second, we estimate the response rate at 11%, which is not high but is comparable to a previous Canadian Internet survey in PT.27 Third, although our sample was representative of the demographics of the Quebec physiotherapist population, two variables were exceptions: (1) more respondents than expected lived in rural areas (although the numbers were still relatively small, with the distribution heavily weighted toward urban areas) and (2) more respondents than expected had higher education. Persons with post-graduate degrees may be more likely to participate in research projects such as ours. It is also possible that those with an advanced degree have more knowledge about evidence-based practice, which could explain the high level of conformity with current recommendations. Fourth, our survey used a checklist, which, although it made the questionnaire easy and quick to complete, might have introduced a power-of-suggestion bias; in other words, physiotherapists may have selected responses that may or may not have reflected their responses if they had been surveyed in another manner. Finally, although the survey identified the generalized type of exercise as mobility or strengthening, it did not specify the exact exercise or its frequency, duration, or intensity; recent research has supported the notion that exercise programmes for knee OA should be reported as type of exercise and its frequency, duration, or intensity so that clinicians can better implement effective exercise strategies.28
Conclusion
The majority of the physiotherapists included mobility or strengthening exercises in their treatment choices; both are interventions for which the most evidence exists. A great majority of respondents also selected education. This could mean that most physiotherapists in Quebec who treat a musculoskeletal clientele are aware of the current clinical practice guidelines for managing knee OA. Professionals working in the private (vs. public) sector use manual therapy and electrotherapy more often, both treatments for which the evidence is insufficient. It may be useful to undertake regular in-service education to update physiotherapists working in private practice on the current evidence-based recommendations.
Key Messages
What is already known on this topic
Clinical practice guidelines for non-pharmacologic treatment for knee osteoarthritis (OA) exist. The most recommended treatment modalities include therapeutic exercises, weight loss, and walking aids. Physiotherapists use a multitude of approaches to treat patients with knee OA.
What this study adds
The great majority of Quebec physiotherapists use mobility and strengthening exercises in treating patients with knee OA, a practice that concurs with current practice guidelines. Physiotherapists who work in the private (vs. public) sector use manual therapy and electrotherapy, both treatments with insufficient evidence.
References
- 1. Hochman J. Osteoarthritis. Toronto: Arthritis Society; 2017. [cited 2018 June 8]. Available from: https://www.arthritis.ca/about-arthritis/arthritis-types-(a-z)/types/osteoarthritis. [Google Scholar]
- 2. Bennell KL, Hunter DJ, Hinman RS. Management of osteoarthritis of the knee. BMJ. 2012;345(2):e4934. 10.1136/bmj.e4934. Medline:22846469 [DOI] [PubMed] [Google Scholar]
- 3. Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;(4):CD004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4):465–74. 10.1002/acr.21596. Medline:22563589 [DOI] [PubMed] [Google Scholar]
- 5. Iversen MD. Managing hip and knee osteoarthritis with exercise: what is the best prescription? Ther Adv Musculoskelet Dis. 2010;2(5):279–90. 10.1177/1759720x10378374. Medline:22870454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Page CJ, Hinman RS, Bennell KL. Physiotherapy management of knee osteoarthritis. Int J Rheum Dis. 2011;14(2):145–51. 10.1111/j.1756-185x.2011.01612.x. Medline:21518313 [DOI] [PubMed] [Google Scholar]
- 7. Rodriguez-Merchan EC. Conservative treatment of acute knee osteoarthritis: a review of the Cochrane Library. J Acute Dis. 2016;5(3):190–3. 10.1016/j.joad.2016.03.003. [DOI] [Google Scholar]
- 8. McAlindon TE, Bannuru RR, Sullivan M, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–88. 10.1016/j.joca.2014.01.003. Medline:24462672 [DOI] [PubMed] [Google Scholar]
- 9. Skelly A, Chou R, Dettori J, et al. Noninvasive nonpharmacological treatment for chronic pain: a systematic review. Comparative Effectiveness Review No. 209. Rockville (MD): Agency for Healthcare Research and Quality; 2018. [PubMed] [Google Scholar]
- 10. Abbott J, Robertson M, Chapple C, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–34. 10.1016/j.joca.2012.12.014. Medline:23313532 [DOI] [PubMed] [Google Scholar]
- 11. Brosseau L, Rahman P, Toupin-April K, et al. A systematic critical appraisal for non-pharmacological management of osteoarthritis using the appraisal of guidelines research and evaluation II instrument. PLoS One. 2014;9(1):e82986. 10.1371/journal.pone.0082986. Medline:24427268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Poitras S, Avouac J, Rossignol M, et al. A critical appraisal of guidelines for the management of knee osteoarthritis using Appraisal of Guidelines Research and Evaluation criteria. Arthritis Res Ther. 2007;9(6):R126. 10.1186/ar2339. Medline:18062805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: the Chronic Osteoarthritis Management Initiative of the US Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43(6):701–12. 10.1016/j.semarthrit.2013.11.012. Medline:24387819 [DOI] [PubMed] [Google Scholar]
- 14. Kroon FP, van der Burg LR, Buchbinder R, et al. Self-management education programmes for osteoarthritis. Cochrane Database Syst Rev. 2014(1):CD008963. 10.1002/14651858.cd008963.pub2. Medline:24425500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. French H. Physiotherapy management of osteoarthritis of the hip: a survey of current practice in acute hospitals and private practice in the Republic of Ireland. Physiotherapy. 2007;93(4):253–60. 10.1016/j.physio.2006.12.008 [DOI] [Google Scholar]
- 16. Holden MA, Nicholls EE, Hay EM, et al. Physical therapists’ use of therapeutic exercise for patients with clinical knee osteoarthritis in the United Kingdom: in line with current recommendations? Phys Ther. 2008;88(10):1109–21. 10.2522/ptj.20080077. Medline:18703675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walsh NE, Hurley MV. Evidence based guidelines and current practice for physiotherapy management of knee osteoarthritis. Musculoskelet Care. 2009;7(1):45–56. 10.1002/msc.144. Medline:18972322 [DOI] [PubMed] [Google Scholar]
- 18. MacKay C, Hawker G, Jaglal S. A qualitative study exploring the barriers and facilitators to optimal physical therapy management of early knee osteoarthritis symptoms. Osteoarthritis Cartilage. 2017;25(Supplement 1):S396. 10.1016/j.joca.2017.02.681. [DOI] [Google Scholar]
- 19. Canadian Institute of Health Information (CIHI) . Physiotherapists, 2016: data tables. Ottawa: CIHI; 2016. [Google Scholar]
- 20. Cetin N, Aytar A, Atalay A, et al. Comparing hot pack, short-wave diathermy, ultrasound, and TENS on isokinetic strength, pain, and functional status of women with osteoarthritic knees: a single-blind, randomized, controlled trial. Am J Phys Med Rehabil. 2008;87(6):443–51. 10.1097/phm.0b013e318174e467. Medline:18496246 [DOI] [PubMed] [Google Scholar]
- 21. Brosseau L, Yonge K, Welch V, et al. Thermotherapy for treatment of osteoarthritis. Cochrane Database Syst Rev. 2003;(4):CD004522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Iversen MD. Rehabilitation interventions for pain and disability in osteoarthritis: a review of interventions including exercise, manual techniques, and assistive devices. Orthop Nurs. 2012;31(2):103–8. 10.1097/nor.0b013e31824fce07. Medline:22446803 [DOI] [PubMed] [Google Scholar]
- 23. Deslauriers S, Raymond M-H, Laliberté M, et al. Access to publicly funded outpatient physiotherapy services in Quebec: waiting lists and management strategies. Disabil Rehabil. 2017;39(26):2648–56. 10.1080/09638288.2016.1238967. Medline:27758150 [DOI] [PubMed] [Google Scholar]
- 24. Delaurier A, Bernatsky S, Raymond M-H, et al. Wait times for physical and occupational therapy in the public system for people with arthritis in Quebec. Physiother Can. 2013;65(3):238–43. 10.3138/ptc.2011-62. Medline:24403693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O’Connell NE, Ward SP. Low back pain: what have clinical guidelines ever done for us? J Orthop Sports Phys Ther. 2018;48(2):54–7. 10.2519/jospt.2018.0602. Medline:29385945 [DOI] [PubMed] [Google Scholar]
- 26. Mercuri M, Sherbino J, Sedran RJ, et al. When guidelines don’t guide: the effect of patient context on management decisions based on clinical practice guidelines. Acad Med. 2015;90(2):191–6. 10.1097/acm.0000000000000542. Medline:25354075 [DOI] [PubMed] [Google Scholar]
- 27. Laliberté M, Mazer B, Orozco T, et al. Low back pain: investigation of biases in outpatient Canadian physical therapy. Phys Ther. 2017;97(10):985–97. 10.1093/ptj/pzx055. Medline:29029551 [DOI] [PubMed] [Google Scholar]
- 28. O’Neil J, McEwen D, Del Bel MJ, et al. Assessment of the content reporting for therapeutic exercise interventions among existing randomized controlled trials on knee osteoarthritis. Clin Rehabil. 2018;32(7):980–4. 10.1177/0269215518763714. Medline:29529871 [DOI] [PubMed] [Google Scholar]


