Abstract
Background
Sarcopenia is associated with poor outcomes in elderly patients. However, current surgical risk assessment tools for cardiovascular surgery do not include the impact of sarcopenia.
Objectives
This study aimed to assess whether the psoas muscle index, a numerical score used to assess sarcopenia, is associated with outcomes in elderly patients undergoing cardiovascular surgery.
Methods
This nested case-control study evaluated patients aged ≥ 75 years who underwent elective cardiovascular surgery and were admitted to the intensive care unit at Jichi Medical University, Saitama Medical Center between January 1, 2016 and March 31, 2017. The case group (poor outcomes) included patients who either died or were transferred to a rehabilitation facility postoperatively. The control group (good outcomes) included patients who were discharged postoperatively. Clinical factors likely to affect patient outcomes were assessed, and the characteristics of the two outcome groups were compared using logistic regression analysis.
Results
In total, 183 patients were evaluated; among them, 137 and 46 patients were categorized to the good and poor outcome groups, respectively. The psoas muscle index was significantly associated with outcome (odds ratio: 0.25; 95% confidence interval: 0.14 – 0.43; P < 0.001). A psoas muscle index cut-off of 3.24 had a specificity, sensitivity, positive predictive value, and negative predictive value of 0.86, 0.63, 0.58, and 0.87, respectively, for predicting worse outcome at discharge.
Conclusions
The psoas muscle index was strongly associated with discharge to home in patients aged ≥ 75 years who underwent elective cardiovascular surgery. This finding suggests that the psoas muscle index might be useful in identifying the eligibility of older patients for cardiovascular surgery.
Keywords: Thoracic Surgery, Frailty, Sarcopenia, Psoas Muscle, Discharge to Home
1. Background
The risk of mortality and morbidity associated with cardiovascular surgery is generally assessed using prognostic tools such as the European System for Cardiac Operative Risk Evaluation II (EuroSCORE II) and JAPAN scores (1, 2). These scores are calculated based on preoperative data such as age, sex, type of operation, medications, and past medical history. However, they do not include functional status, such as frailty and sarcopenia. Further, it has been reported that the EuroSCORE II cannot predict postoperative quality of life (QOL) (3). In addition, postoperative QOL may be overestimated in elderly patients who underwent cardiovascular surgery with a low preoperative QOL (4). Determining the surgical eligibility of elderly individuals is often challenging because their physiological tolerance to surgical stress varies widely, with some patients becoming bedridden or having poor functional outcomes. Moreover, age itself has been reported to be an important prognostic factor associated with postoperative cognitive dysfunction, including after cardiac surgery (5, 6), which affects patients’ daily activity. Therefore, the prognostic scores calculated using the currently used methods may not be applicable to elderly patients, especially those undergoing cardiovascular surgery (7).
Frailty increases vulnerability to stressors (8) and is associated with intensive care unit (ICU)-acquired weakness, nursing home admission, mortality, and morbidity (9-12). Sarcopenia, a major cause of frailty (13), is defined as aging-related muscle loss and it can adversely affect QOL (14). In patients undergoing cardiovascular surgery, sarcopenia is commonly assessed using the psoas muscle index (PMI), which is calculated by dividing the cross-sectional width of the bilateral psoas muscle at the level of the L3 vertebra by the square of the patient’s height (15). Previous studies have suggested a relationship between mortality and PMI after cardiovascular surgery, as well as several other illnesses (16, 17). However, these studies did not assess postoperative QOL, including the rate of discharge to home as a major outcome. Therefore, the usefulness of the PMI for determining the risk of poor postoperative QOL in patients undergoing heart surgery is still unclear.
2. Objectives
The present study aimed to evaluate the association between PMI and the discharge to home as an index of postoperative QOL after cardiovascular surgery in elderly patients. We hypothesized that a low PMI is associated with a lower rate of discharge to home in elderly patients undergoing cardiovascular surgery.
3. Methods
3.1. Study Design and Patient Population
This was a nested case-control study of patients aged ≥ 75 years who underwent elective cardiovascular surgery and were admitted to the ICU at Saitama Medical Center, Jichi Medical University between January 1, 2016 and March 31, 2017. Patients who underwent cardiovascular operations, including valve replacement, valvuloplasty, coronary artery bypass graft (CABG), and thoracic aortic surgery were included. The exclusion criteria were emergency cardiovascular surgery, transcatheter aortic valve replacement, abdominal aortic replacement, peripheral arterial surgery, and aortic stent-grafting. Patients without PMI data calculated using computed tomography (CT) scans were also excluded.
The study protocol was approved by the appropriate institutional review board. The need for written consent was waived owing to the retrospective nature of the study.
3.2. Nested Case-Control Design
We used a nested case-control design to evaluate the association of factors with the rate of discharge to home, considered one of the most accurate measures to evaluate intensive care outcomes in the elderly (18). The case group was defined as the poor outcome group and included patients who either died or were transferred to a rehabilitation facility postoperatively. The control group was defined as the good outcome group and included patients who were discharged home postoperatively.
3.3. Data Collection
Patient data including sex, body weight, height, body mass index (BMI), medical history, updated Charlson comorbidity index (CCI) (19), primary disease, type of operation, EuroSCORE II, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, and PMI were collected from hospital records. We used the updated CCI because Japanese data were used to validate the score, and it was shown to have a more linearly increasing relationship with mortality than the original CCI (19). PMI scores were calculated by the primary investigator via the manual trace method using CT scan images (Figure 1). At our institution, cardiovascular surgeons routinely obtain a thoracoabdominal CT scan of each patient within 3 months prior to surgery, and we were able to use data from these scans to calculate the PMI.
Figure 1. A computed tomography scan image of the L3 vertebra used to measure the psoas muscle area via the manual trace method. The white line highlights the psoas muscle margin. The manual trace method is used to calculate the area inside the white line.
3.4. Statistical Analysis
Categorical variables were reported as either numbers or percentages, while continuous variables were reported as medians with interquartile ranges or mean values with standard deviation. The collected data were assessed to determine distribution patterns. Normality was compared using the Shapiro-Wilk test. Subsequently, an F-test was used to demonstrate equal variance. Normally distributed data were assessed using Student’s t-test, while non-normally distributed data were assessed using the Mann-Whitney U-test. Differences in categorical variables were compared using Fisher’s exact tests.
Associations between discharge to home and PMI, APACHE II score, updated CCI, EuroSCORE II, and operating time were assessed. These factors were selected to consider their clinical impact on outcomes after cardiac surgery. Logistic regression analyses were used to determine the odds ratios and 95% confidence intervals (CIs). Receiver operating characteristic (ROC) curves were plotted, and the area under the ROC curves for each factor was compared. All statistical analyses were performed using R software (The R Foundation for Statistical Computing, Vienna, Austria, version 3.5.2). All P-values were two-sided, and P ≤ 0.05 was considered significant.
4. Results
Of the 194 patients initially evaluated, 10 patients who did not undergo preoperative CT scans of the pelvic region and 1 patient who underwent lumbar fixation that prevented the calculation of the PMI were excluded. Finally, 183 patients were enrolled in this study. Among them, 137 and 46 patients were included in the good outcome and poor outcome groups, respectively (Figure 2). The patient characteristics are shown in Table 1. There were no significant between-group differences in the sex, age, and updated CCI. The median BMI was also not significantly different. Meanwhile, the mean height and weight, median APACHE II score, median PMI, and median EuroSCORE II scores were significantly different between the two groups.
Figure 2. Patient selection flowchart. In total, 183 patients are divided into the good outcome group (n = 137) and the poor outcome group (n = 46).
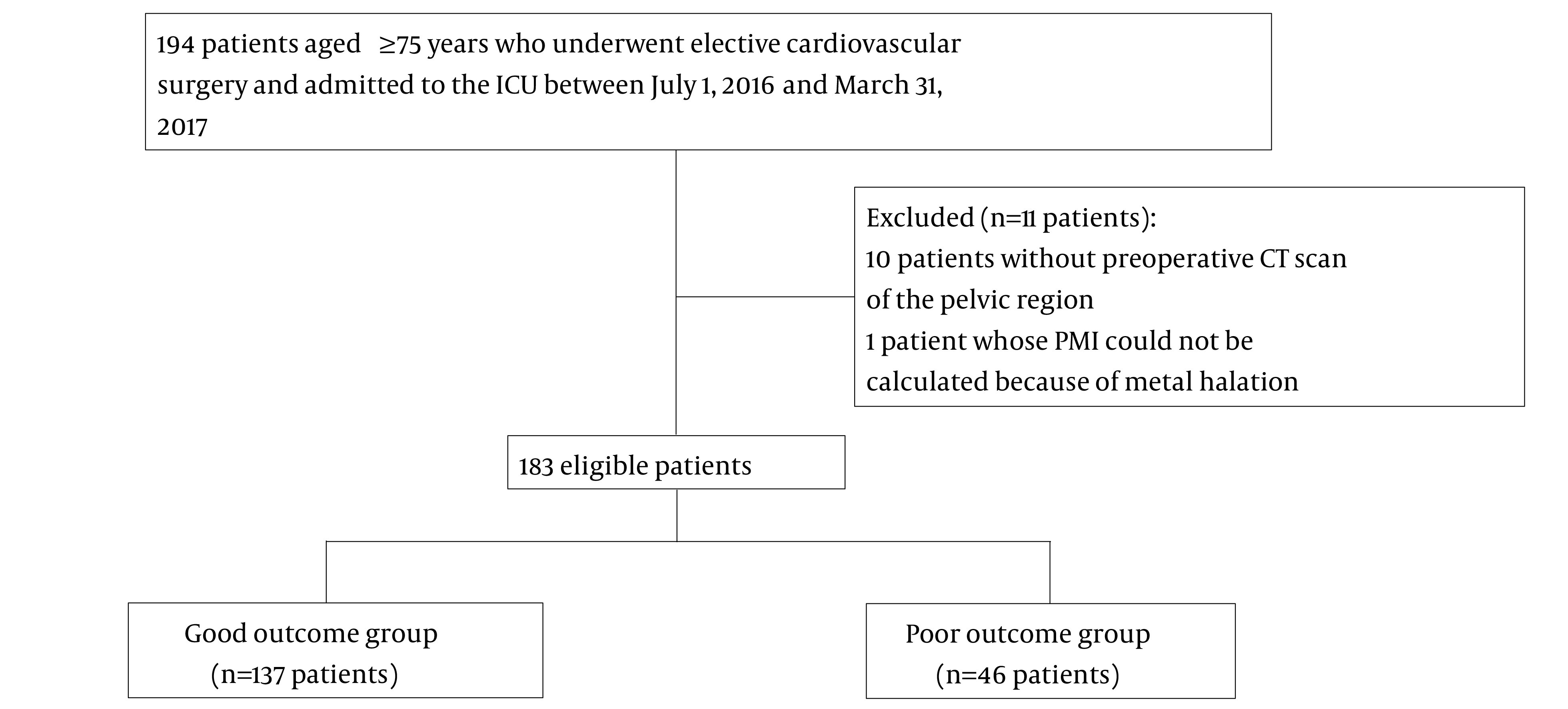
Table 1. Patient Characteristics and Operative Data a.
| Good Outcome Group (n = 137) | Poor Outcome Group (n = 46) | P Value | |
|---|---|---|---|
| Sex, male (%) | 75 (55) | 18 (39) | 0.09 |
| Age (y) | 78 (76 – 80) | 78 (77 – 82.8) | 0.07 |
| Height (cm) | 156.1 (149.5 – 164) | 150.4 (145.9 – 160.3) | 0.03 |
| Weight (kg) | 56.0 (10.7) | 51.9 (11.0) | 0.03 |
| Body mass index | 22.6 (21.0 – 24.4) | 22.1 (19.7 – 24.4) | 0.25 |
| Updated CCI | 3 (2 – 3) | 3 (2 – 3) | 0.22 |
| Dementia (%) | 28 (20) | 20 (43) | < 0.01 |
| Hemodialysis (%) | 8 (6) | 3 (7) | 1 |
| Cancer (%) | 11 (8) | 2 (4) | 0.52 |
| Diabetes (%) | 36 (26) | 14 (30) | 0.57 |
| Hypertension (%) | 94 (69) | 26 (57) | 0.15 |
| Stroke (%) | 18 (13) | 7 (15) | 0.80 |
| EuroSCORE II | 3.49 (2.05 – 5.39) | 6.23 (3.2 – 10.59) | < 0.01 |
| Operation time | 284 (233 – 366) | 327 (262.5 – 428.5) | 0.01 |
| APACHE II | 16 (14 – 18) | 18 (16 – 21) | < 0.01 |
| PMI | 4.2 (0.96) | 3.3 (0.97) | < 0.01 |
| Type of operation | |||
| Valve replacement (%) | 98 (72) | 27 (59) | 0.14 |
| CABG (%) | 36 (21) | 13 (28) | 0.85 |
| Aortic surgery (%) | 26 (19) | 10 (22) | 0.67 |
| Other (%) | 4 (2) | 1 (2) | 1 |
Abbreviations: PMI, psoas muscle index; APACHE II, Acute Physiology and Chronic Health Evaluation II score; CCI, Charlson comorbidity index; EuroSCORE II, European System for Cardiac Operative Risk Evaluation II
aValues are presented as the median (interquartile range), mean (standard deviation), or number (%).
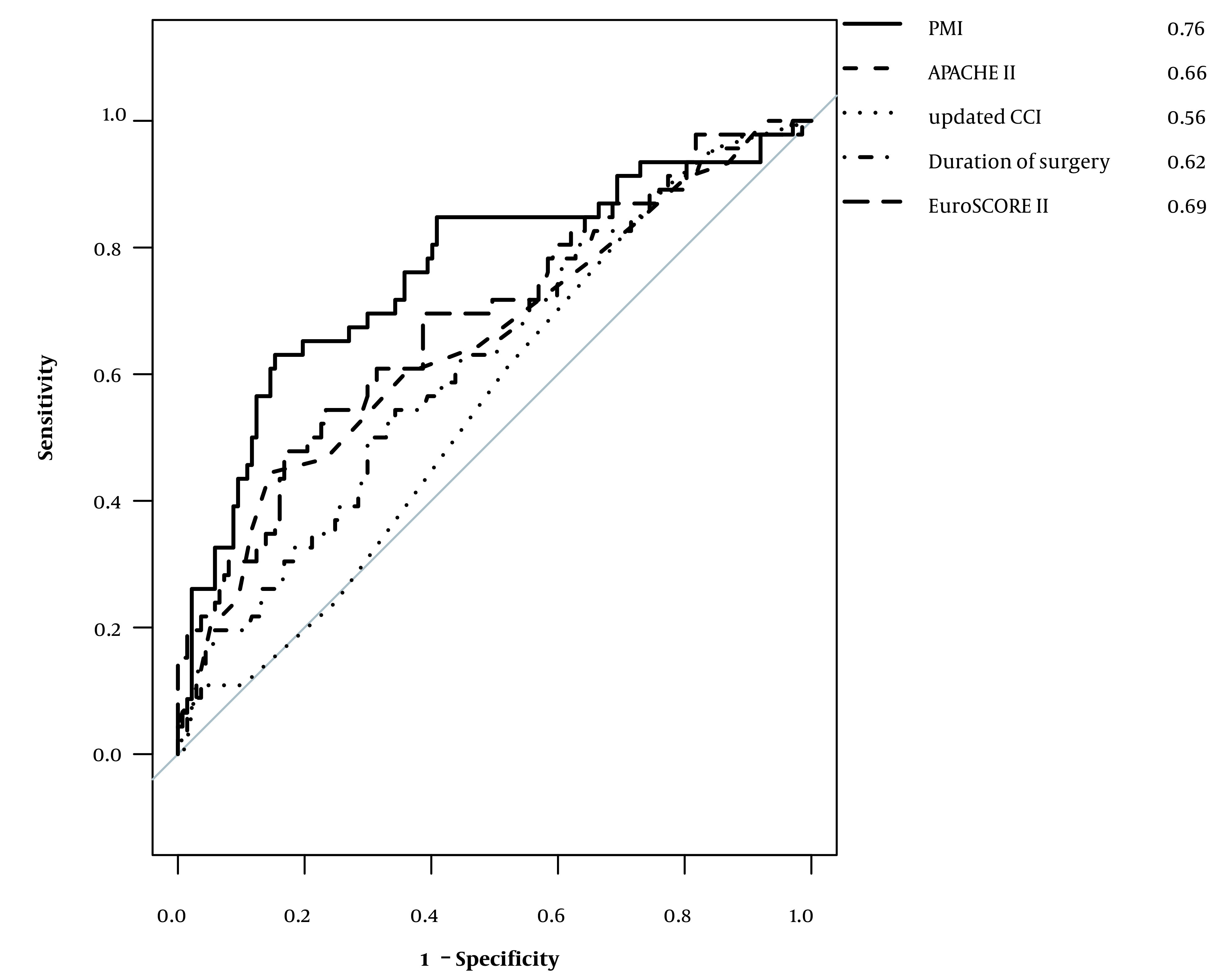
The results of the logistic regression analysis are shown in Table 2. PMI was significantly associated with the outcome at discharge, with an odds ratio of 0.25 (95% CI: 0.14 – 0.43; P < 0.01), which means that a common odds ratio for every one-unit increase in PMI for a poor outcome is 0.25. The ROC curves determined for each factor are shown in Figure 3. Comparison of the area under the curve (AUC) of the ROC for each of the assessed factors showed that PMI had the greatest AUC (AUC: 0.76; 95% CI: 0.67 - 0.85). A PMI cut-off of 3.24 had a specificity, sensitivity, positive predictive value, and negative predictive value of 0.86, 0.63, 0.58, and 0.87, respectively.
Table 2. Results of Conditional Logistic Regression Analyses of Factors Influencing Outcomes.
| Factor | Odds Ratio | 95% CI | P Value |
|---|---|---|---|
| APACHE II | 1.17 | 0.02 – 4.38 | 0.36 |
| EuroSCORE II | 1.13 | 1.02 – 1.26 | 0.014 |
| Operation time | 1 | 0.99 – 1.01 | 0.10 |
| PMI | 0.25 | 0.14 – 0.43 | < 0.01 |
| Updated CCI | 1.3 | 0.99 – 1.71 | 0.06 |
Abbreviations: APACHE II: Acute Physiology and Chronic Health Evaluation II score, EuroSCORE, EURO score II: European System for Cardiac Operative Risk Evaluation II; PMI, psoas muscle index; CCI, Charlson comorbidity index.
Figure 3. Receiver operating characteristic (ROC) curves for each factor. The psoas muscle index (PMI) has the greatest area under the ROC curve, suggesting that PMI is associated with favorable outcomes.
5. Discussion
This study shows that PMI is strongly associated with discharge to home in patients aged ≥ 75 years who underwent cardiovascular surgery. An increase in PMI was associated with a decrease in the odds of a poor outcome (defined as in-hospital death or discharge to a long-term care facility) adjusted by EuroSCORE II, APACHE II, operation time, and the updated CCI for patients aged ≥ 75 years who underwent cardiovascular surgery.
The EuroSCORE II and JAPAN scores were developed to predict postoperative outcomes and determine the appropriateness of cardiovascular surgery. However, these scoring systems do not reflect the influence of frailty, and only predict mortality and complication rates. These scores do not always predict other important outcomes for elderly patients, such as QOL after discharge and the rate of discharge to home. This study showed that PMI was more strongly associated with discharge to home than other clinical scoring systems associated with mortality following cardiovascular surgery.
Several studies have assessed the relationship between PMI and patient prognosis. Associations between poor prognosis and sarcopenia in patients with malignancies (20, 21) and those with traumatic injuries (22) have been reported. An association between mortality and PMI has been reported in patients who underwent cardiovascular surgery. Heberton et al. revealed the usefulness of PMI in predicting mortality in patients undergoing left ventricular assist device implantation (16). Saji et al. also reported an association between PMI and mortality in patients who underwent transcatheter aortic valve replacement (17). Okamura et al. reported that PMI was associated with long-term outcomes in patients who underwent cardiovascular surgery (23). Sarcopenia and frailty can prolong hospital stay and increase the need for transfer to rehabilitation facilities, both of which negatively affect patients’ QOL (24-26).
However, previous studies had important limitations. Some studies have assessed the impact of PMI by dividing the study cohort into two groups. They defined a sarcopenia group as patients below the fiftieth percentile of PMI values and the non-sarcopenia group as those above the fiftieth percentile, which includes the same number of patients (16, 21, 22). There was no justification for dividing patents by PMI to define them as sarcopenic or non-sarcopenic. In the present study, PMI was assessed as a continuous variable. Previous studies also included relatively young patients (approximately 65 years old). Sarcopenia and frailty are serious problems typically affecting the elderly who need intensive care (25), and studies of patients aged older than 75 years should be performed.
Further, previous studies used mortality as the primary outcome. Although mortality is an important outcome, we believe that the QOL of elderly patients is as important as mortality because a postoperative low QOL will result in high medical costs and a large care burden for families. Discharge to a care facility has been reported to be an accurate measure of intensive care and QOL outcomes in elderly patients (19, 27). Therefore, we evaluated the impact of PMI on QOL after cardiovascular surgery with discharge to home as the outcome measure. Our findings indicate that preoperative assessment of PMI may be useful in determining the indications for elective cardiac surgery in patients aged ≥75 years. Importantly, the findings indicate that a new prediction score that includes PMI or another frailty score is needed to assess surgical risk in the elderly.
This study has some limitations. First, it was not possible to adjust for confounding factors because of the retrospective nature of the study. Especially, preoperative QOL scores such as the clinical frailty scale could not be determined (8, 28). However, there is no consensus on the standard measurement of frailty (29). Sarcopenia is a major cause of frailty (13) and could be a surrogate marker of frailty. In this study, sarcopenia was evaluated using PMI, which is an objective indicator. One study used both PMI and intramuscular adipose tissue content to assess sarcopenia (26). A combination of these radiological parameters might assess sarcopenia more meaningfully, although there are few studies on intramuscular adipose tissue content. Second, this study included patients aged ≥ 75 years; therefore, the study had selection bias, and this may limit the generalizability of the findings. Third, the small size of the cohort also limited the number of factors that could be included in the conditional logistic regression analyses. Fourth, this was a single-center study, and the postoperative rehabilitation method was not adequately assessed. Some institutes utilize the active cyclic breathing technique for post-CABG patients (30). Such differences in rehabilitation programs may affect the patients’ postoperative outcomes, and thus the external validity of this study may be compromised. Finally, the long-term survival of the patients is unknown, including changes in living situations (for instance, moving between home and a rehabilitation facility). Discharge to a nursing home or rehabilitation facility following surgery does not always indicate a poor QOL. Some patients may eventually go home after rehabilitation. Therefore, a more complete follow-up evaluation is needed to determine QOL outcomes.
5.1. Conclusions
Compared to other established prognostic scores, PMI is more strongly associated with discharge to home in patients aged ≥ 75 years who undergo elective cardiovascular surgery. PMI may be helpful in determining the suitability of cardiovascular surgery in elderly patients.
Acknowledgments
This work was supported by the Advanced Graduate Program for Future Medicine and Health Care, Tohoku University.
Footnotes
Authors' Contribution: Y.I conceived and designed the evaluation and drafted the manuscript. J.S participated in designing the evaluation, performed parts of the statistical analysis and helped to draft the manuscript. J.S and M.S re-evaluated the clinical data, revised the manuscript and performed the statistical analysis and revised the manuscript. A.L interpreted them and revised the manuscript. All authors read and approved the final manuscript.
Conflict of Interests: There is no conflict of interest.
Data Reproducibility: The data presented in this study will be available on request from the corresponding author by this journal representative at any time during submission or after publication
Funding/Support: We did not receive any financial or human resource support for this research.
Contributor Information
Yudai Iwasaki, Email: yudai.i0213@gmail.com.
Junji Shiotsuka, Email: jshio3417@gmail.com.
Alan Kawarai Lefor, Email: alefor@jichi.ac.jp.
Masamitsu Sanui, Email: msanui@mac.com.
References
- 1.Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44. doi: 10.1093/ejcts/ezs043. discussion 744-5. [DOI] [PubMed] [Google Scholar]
- 2.Motomura N, Miyata H, Tsukihara H, Takamoto S, Japan Cardiovascular Surgery Database O. Risk model of thoracic aortic surgery in 4707 cases from a nationwide single-race population through a web-based data entry system: the first report of 30-day and 30-day operative outcome risk models for thoracic aortic surgery. Circulation. 2008;118(14 Suppl):S153–9. doi: 10.1161/CIRCULATIONAHA.107.756684. [DOI] [PubMed] [Google Scholar]
- 3.Peric V, Borzanovic M, Jovanovic A, Stolic R, Sovtic S, Trajkovic G. The relationship between EuroSCORE preoperative risk prediction and quality of life changes after coronary artery by-pass surgery. Interact Cardiovasc Thorac Surg. 2005;4(6):622–6. doi: 10.1510/icvts.2005.109546. [DOI] [PubMed] [Google Scholar]
- 4.Noyez L. Is quality of life post cardiac surgery overestimated? Health Qual Life Outcomes. 2014;12:62. doi: 10.1186/1477-7525-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soenarto RF, Mansjoer A, Amir N, Aprianti M, Perdana A. Cardiopulmonary bypass alone does not cause postoperative cognitive dysfunction following open heart surgery. Anesth Pain Med. 2018;8(6):e83610. doi: 10.5812/aapm.83610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehsani R, Djalali Motlagh S, Zaman B, Sehat Kashani S, Ghodraty MR. Effect of general versus spinal anesthesia on postoperative delirium and early cognitive dysfunction in elderly patients. Anesth Pain Med. 2020;10(4):e101815. doi: 10.5812/aapm.101815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vetta F, Locorotondo G, Vetta G, Mignano M, Bracchitta S. Prognostic impact of frailty in elderly cardiac surgery patients. Monaldi Arch Chest Dis. 2017;87(2):855. doi: 10.4081/monaldi.2017.855. [DOI] [PubMed] [Google Scholar]
- 8.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Latronico N, Herridge M, Hopkins RO, Angus D, Hart N, Hermans G, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med. 2017;43(9):1270–81. doi: 10.1007/s00134-017-4757-5. [DOI] [PubMed] [Google Scholar]
- 10.Topinkova E. Aging, disability and frailty. Ann Nutr Metab. 2008;52 Suppl 1:6–11. doi: 10.1159/000115340. [DOI] [PubMed] [Google Scholar]
- 11.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, et al. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–23. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- 13.Morley JE. Frailty and sarcopenia in elderly. Wien Klin Wochenschr. 2016;128(Suppl 7):439–45. doi: 10.1007/s00508-016-1087-5. [DOI] [PubMed] [Google Scholar]
- 14.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamaguchi Y, Kaido T, Okumura S, Fujimoto Y, Ogawa K, Mori A, et al. Impact of quality as well as quantity of skeletal muscle on outcomes after liver transplantation. Liver Transpl. 2014;20(11):1413–9. doi: 10.1002/lt.23970. [DOI] [PubMed] [Google Scholar]
- 16.Heberton GA, Nassif M, Bierhals A, Novak E, LaRue SJ, Lima B, et al. Usefulness of psoas muscle area determined by computed tomography to predict mortality or prolonged length of hospital stay in patients undergoing left ventricular assist device implantation. Am J Cardiol. 2016;118(9):1363–7. doi: 10.1016/j.amjcard.2016.07.061. [DOI] [PubMed] [Google Scholar]
- 17.Saji M, Lim DS, Ragosta M, LaPar DJ, Downs E, Ghanta RK, et al. Usefulness of psoas muscle area to predict mortality in patients undergoing transcatheter aortic valve replacement. Am J Cardiol. 2016;118(2):251–7. doi: 10.1016/j.amjcard.2016.04.043. [DOI] [PubMed] [Google Scholar]
- 18.Rady MY, Johnson DJ. Hospital discharge to care facility: A patient-centered outcome for the evaluation of intensive care for octogenarians. Chest. 2004;126(5):1583–91. doi: 10.1378/chest.126.5.1583. [DOI] [PubMed] [Google Scholar]
- 19.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 20.Yuri Y, Nishikawa H, Enomoto H, Ishii A, Iwata Y, Miyamoto Y, et al. Implication of psoas muscle index on survival for hepatocellular carcinoma undergoing radiofrequency ablation therapy. J Cancer. 2017;8(9):1507–16. doi: 10.7150/jca.19175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasahara R, Kawahara T, Ohtake S, Saitoh Y, Tsutsumi S, Teranishi JI, et al. A low psoas muscle index before treatment can predict a poorer prognosis in advanced bladder cancer patients who receive gemcitabine and nedaplatin therapy. Biomed Res Int. 2017;2017:7981549. doi: 10.1155/2017/7981549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fairchild B, Webb TP, Xiang Q, Tarima S, Brasel KJ. Sarcopenia and frailty in elderly trauma patients. World J Surg. 2015;39(2):373–9. doi: 10.1007/s00268-014-2785-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okamura H, Kimura N, Tanno K, Mieno M, Matsumoto H, Yamaguchi A, et al. The impact of preoperative sarcopenia, defined based on psoas muscle area, on long-term outcomes of heart valve surgery. J Thorac Cardiovasc Surg. 2019;157(3):1071–1079 e3. doi: 10.1016/j.jtcvs.2018.06.098. [DOI] [PubMed] [Google Scholar]
- 24.Garnacho-Montero J, Amaya-Villar R, Garcia-Garmendia JL, Madrazo-Osuna J, Ortiz-Leyba C. Effect of critical illness polyneuropathy on the withdrawal from mechanical ventilation and the length of stay in septic patients. Crit Care Med. 2005;33(2):349–54. doi: 10.1097/01.ccm.0000153521.41848.7e. [DOI] [PubMed] [Google Scholar]
- 25.Flaatten H, De Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (>/= 80 years). Intensive Care Med. 2017;43(12):1820–8. doi: 10.1007/s00134-017-4940-8. [DOI] [PubMed] [Google Scholar]
- 26.Kiriya Y, Toshiaki N, Shibasaki I, Ogata K, Ogawa H, Takei Y, et al. Sarcopenia assessed by the quantity and quality of skeletal muscle is a prognostic factor for patients undergoing cardiac surgery. Surg Today. 2020;50(8):895–904. doi: 10.1007/s00595-020-01977-w. [DOI] [PubMed] [Google Scholar]
- 27.van Leeuwen KM, van Loon MS, van Nes FA, Bosmans JE, de Vet HCW, Ket JCF, et al. What does quality of life mean to older adults? A thematic synthesis. PLoS One. 2019;14(3):e0213263. doi: 10.1371/journal.pone.0213263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rockwood K, Theou O. Using the Clinical Frailty Scale in allocating scarce health care resources. Can Geriatr J. 2020;23(3):210–5. doi: 10.5770/cgj.23.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: A review. Eur J Intern Med. 2016;31:3–10. doi: 10.1016/j.ejim.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Salehi Derakhtanjani A, Ansari Jaberi A, Haydari S, Negahban Bonabi T. Comparison the effect of active cyclic breathing technique and routine chest physiotherapy on pain and respiratory parameters after coronary artery graft surgery: A randomized clinical trial. Anesth Pain Med. 2019;9(5):e94654. doi: 10.5812/aapm.94654. [DOI] [PMC free article] [PubMed] [Google Scholar]



