Summary:
An 11-year-old male patient presented with a large, highly vascular, destructive mandibular mass. An intraoral biopsy showed pleomorphic spindle cells arranged in intersecting fascicles, with scattered atypia. A diagnosis of low-grade myofibroblastic sarcoma was made. The lesion was treated with preoperative arterial embolization followed by surgical resection and reconstruction with a fibular osteomyocutaneous free flap. To our knowledge, no reports of highly vascular mandibular low-grade myofibroblastic sarcoma are available in the literature.
Low-grade myofibroblastic sarcomas (LGMS) are rare mesenchymal neoplasms.1 LGMS were first described by Mentzel et al in 1998, in a case series of 18 patients.1 It usually presents as painless swelling or an enlarging mass. Classically, it has been described as affecting the oral cavity,1–4 although a recent United States population-based study found that it more commonly affects the extremities.5 It tends to exhibit a pattern of aggressive local invasion and is seen more commonly in adults.3
In this report, we describe the case of a child with a highly vascular LGMS of the mandible. To our knowledge, this is the first description of an LGMS tumor with a robust contribution from the external carotid (EC) system. Here, we review recent literature on the treatment of LGMS and discuss the management of a highly vascular mandibular LGMS.
CASE REPORT
An otherwise healthy 11-year-old boy was referred to the craniomaxillofacial clinic for evaluation of an asymptomatic, slowly growing, right mandibular mass. On examination, there was large expansion of the right preauricular cheek with an underlying firm, nonpulsatile mass.
A CT scan showed a highly vascular, destructive mass centered at the right mandibular ramus extending from the mandibular angle to the ipsilateral condyle. An MRI and MRA of the head were obtained to determine whether this was a vascular malformation. MR imaging showed a 5.2 × 3.9 × 5 cm hypervascular mass with multiple feeding branches originating from an enlarged EC artery. The tumor was fed by branches of the EC laterally, the internal maxillary artery medially, and the superficial temporal artery superiorly (Figs. 1, 2).
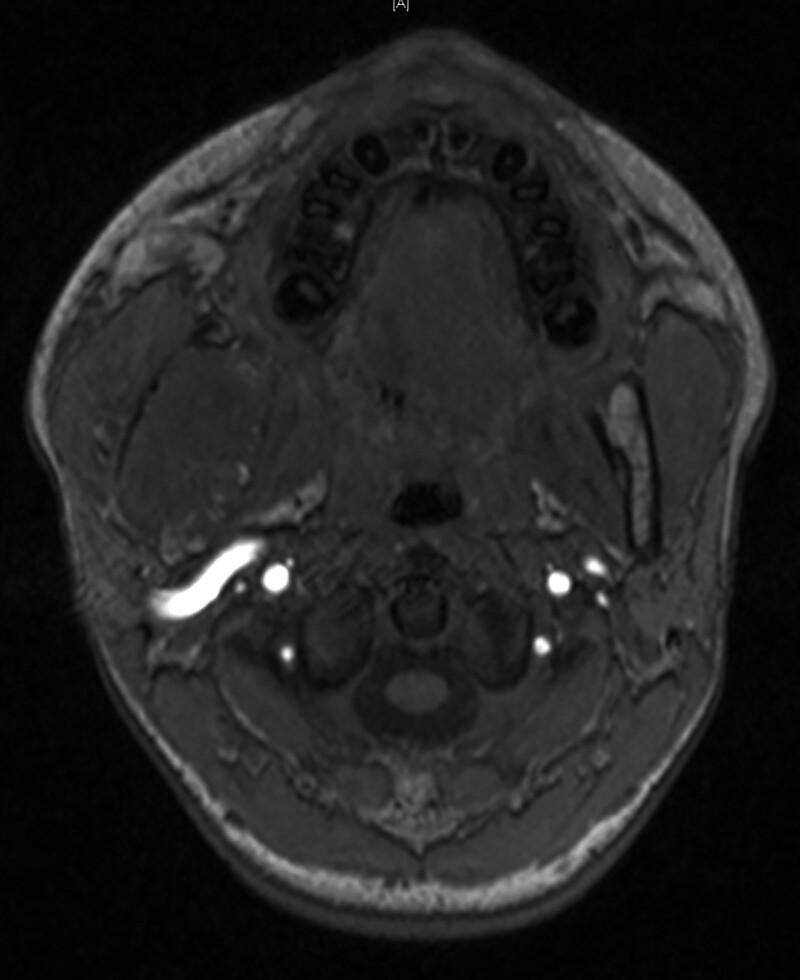
Fig. 1.
MRI axial demonstrating a large expansive, destructive, mass of the right mandible and hypertrophic EC artery.
Fig. 2.
Arteriogram showing a markedly enlarged right EC artery and internal maxillary artery.
An intraoral incisional biopsy showed a neoplasm composed of slightly pleomorphic spindle cells arranged in intersecting fascicles. There were highly atypical cells that contained irregular nuclear membranes and a high nucleus-to-cytoplasm ratio. Immunohistochemical stains showed cells positive for SMA, with strong membranous positivity for CD99 and patchy positive for EMA. Cells were negative for S100, SOX10, TLE1, desmin, pankeratin, CD31, CD34, MUC4, and STAT6. These features were most consistent with a low-grade myofibroblastic sarcoma.
The patient was presented at our institution’s sarcoma tumor board and evaluated by a pediatric oncologist. A recommendation was made for preoperative embolization of vessels followed by surgical resection; no neoadjuvant treatment was recommended. The patient underwent successful embolization of the right middle meningeal artery, superficial temporal artery, and internal maxillary artery by interventional radiology. The next day he underwent tracheotomy, right selective neck dissection, radical excision of right mandibular tumor, reconstruction with a fibular osteomyocutaneous free flap, and maxillomandibular fixation (Fig. 3). The patient tolerated the procedure well, and the postoperative course was uncomplicated.
Fig. 3.
CT scan 3D reconstruction showing postoperative free fibular reconstruction of the mandible.
Surgical pathology reported a final diagnosis of low-grade myofibroblastic sarcoma with negative margins and lymph nodes. The decision was made for observation with serial MRI and chest X-rays, without adjuvant chemotherapy or radiation.
DISCUSSION
LGMS is a rare neoplasm, and it is even more rare for it to present in childhood. There are multiple case reports and case series of LGMS, but none mention highly vascular tumors or tumors requiring preoperative embolization.1–4 As knowledge about this rare malignancy grows, it is important to document unique situations such as this case in which the unusually rich vasculature of the tumor warranted additional planning and intervention.
The main aim of preoperative tumor embolization is to aid in surgical resection by decreasing blood loss. Head and neck tumors that most frequently require embolization include hemangioblastoma, paragangliomas, angiofibromas, and meningiomas.6 Case series have found that tumor embolization reduces intraoperative blood loss, operating time, and recurrence.7–10 It has also been shown to be cost effective and safe, with rare major complications.8
In this case, the day before surgical resection, embolic particles (tris-acryl gelatin microspheres), and coils were used to occlude the EC blood supply to the tumor. Although there are a variety of embolic agents available, particles are more commonly used for embolization of head and neck tumors as they can penetrate more distally into the tumor bed and decrease the risk of cranial nerve injury.11,12 Preoperative embolization should ideally be performed 24–72 hours before surgical resection. This time frame allows for maximal thrombosis of the occluded vessels without formation of collateral arterial channels or recanalization of the occluded arteries.10
Following embolization, our patient underwent surgical resection without chemotherapy or radiation. The role of chemotherapy and radiation in LGMS treatment is unclear. Most of the evidence is limited to case reports with small sample sizes. In a previous report of a LGMS occurring in the mandible of a child, three courses of neoadjuvant chemotherapy were attempted before surgery but the mass continued to grow.4 Therefore, the authors argued that LGMS is poorly responsive to chemotherapy, and surgical resection is the best option.4
Similarly, a review of 96 patients with LGMS from the Surveillance, Epidemiology and End Result database found that surgical excision is the most effective therapy. Chemotherapy and radiation therapy did not independently impact prognosis.13 Another population-based study found no significant difference in survival between patients who had surgery alone and those that underwent surgery and adjuvant radiation.5
Utilizing outcomes data from these prior studies and knowledge of the unique arterial anatomy of this tumor, a multidisciplinary treatment was planned. There was an estimated 70%–80% reduction in arterial flow following embolization of the EC system. No major bleeding was encountered during surgery, and we felt that embolization allowed for a safe, low blood loss surgery. The patient is now 6 months postoperative with no evidence of recurrence.
CONCLUSIONS
LGMS is a rare entity; current consensus for treatment is for surgical resection of the tumor. There is no strong evidence to support the use of adjuvant chemotherapy or radiation therapy. We report the successful treatment of a highly vascular mandibular LGMS in an 11-year-old boy with preoperative arterial embolization followed by surgical resection and reconstruction with a fibular osteomyocutaneous free flap.
Footnotes
Published online 21 January 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Mentzel T, Dry S, Katenkamp D, et al. Low-grade myofibroblastic sarcoma: analysis of 18 cases in the spectrum of myofibroblastic tumors. Am J Surg Pathol. 1998;22:1228–1238. [DOI] [PubMed] [Google Scholar]
- 2.Lokuhetty D, White VA. WHO Classification of Tumours: Soft Tissue and Bone Tumours. Geneva: World Health Organization; [Google Scholar]
- 3.Cai C, Dehner LP, El-Mofty SK. In myofibroblastic sarcomas of the head and neck, mitotic activity and necrosis define grade: a case study and literature review. Virchows Arch. 2013;463:827–836. [DOI] [PubMed] [Google Scholar]
- 4.Keller C, Gibbs CN, Kelly SM, et al. Low-grade myofibrosarcoma of the head and neck: importance of surgical therapy. J Pediatr Hematol Oncol. 2004;26:119–120. [DOI] [PubMed] [Google Scholar]
- 5.Chan JY, Gooi Z, Wong EW, et al. Low-grade myofibroblastic sarcoma: A population-based study. Laryngoscope. 2017;127:116–121. [DOI] [PubMed] [Google Scholar]
- 6.Duffis EJ, Gandhi CD, Prestigiacomo CJ, et al. ; Society for Neurointerventional Surgery. Head, neck, and brain tumor embolization guidelines. J Neurointerv Surg. 2012;4:251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latchaw RE, Gold LH. Polyvinyl foam embolization of vascular and neoplastic lesions of the head, neck, and spine. Radiology. 1979;131:669–679. [DOI] [PubMed] [Google Scholar]
- 8.Dean BL, Flom RA, Wallace RC, et al. Efficacy of endovascular treatment of meningiomas: evaluation with matched samples. AJNR Am J Neuroradiol. 1994;15:1675–1680. [PMC free article] [PubMed] [Google Scholar]
- 9.Macpherson P. The value of pre-operative embolisation of meningioma estimated subjectively and objectively. Neuroradiology. 1991;33:334–337. [DOI] [PubMed] [Google Scholar]
- 10.Moulin G, Chagnaud C, Gras R, et al. Juvenile nasopharyngeal angiofibroma: comparison of blood loss during removal in embolized group versus nonembolized group. Cardiovasc Intervent Radiol. 1995;18:158–161. [DOI] [PubMed] [Google Scholar]
- 11.Gemmete JJ, Ansari SA, McHugh J, et al. Embolization of vascular tumors of the head and neck. Neuroimaging Clin N Am. 2009;19:181–198, Table of Contents. [DOI] [PubMed] [Google Scholar]
- 12.Jindal G, Gemmete J, Gandhi D. Interventional neuroradiology applications in otolaryngology, head and neck surgery. Otolaryngol Clin North Am. 2012;45:1423–1449. [DOI] [PubMed] [Google Scholar]
- 13.Xu Y, Xu G, Wang X, et al. Is there a role for chemotherapy and radiation in the treatment of patients with low-grade myofibroblastic sarcoma? Clin Transl Oncol. 2021;23:344–352. [DOI] [PubMed] [Google Scholar]