Supplemental Digital Content is available in the text.
Abstract
Introduction:
There is growing recognition of the need for effective screening methods and delivering interventions to address health-related social needs (HRSN) in hospital systems, but few studies exist on implementing such a wide-scale undertaking. This article describes the implementation and preliminary findings of a phased roll-out of an institution-wide HRSN screening.
Methods:
We describe the HRSN implementation and data tracking procedures.
Results:
During the first 13 months of the roll-out, 62,315 patient encounters from multiple clinics were eligible for screening, and 52,331 (84.0%) completed the screening. Twelve percent of patients had at least one HRSN need, and 3.5% of those had an urgent need and thus received a social work consult.
Conclusion:
Implementation of the first phase of an institution-wide HRSN screen resulted in high screening and follow-up rates among those with urgent needs, demonstrating feasibility across different clinic settings.
INTRODUCTION
There is growing recognition of the need for effective screening methods for and delivering interventions to address health-related social needs (HRSN).1–3 These social risk factors such as food insecurity, lack of stable housing, and poverty result from biased structural and systemic policies that distribute power and resources unevenly in communities, resulting in social and health inequity.1 Children are especially vulnerable to HRSN, as poverty in childhood correlates to poor health outcomes.4–8 HRSN explain nearly 70% of the variation in poor health quality and short lifespan in a large nationally representative sample of the United States.9 Although HRSN affects all children, HRSN are concentrated in racial and ethnic minority populations and contribute to lingering health disparities between racial groups. Extensive research describes the link between HRSN, health, and health equity1,10,11 and the role healthcare systems should play in addressing social needs.12 Developing a systematic approach to screening for HRSN and providing referrals to appropriate resources are essential in addressing the social drivers of population health in healthcare settings.
Although standardized social needs screens are available for use in healthcare settings, widespread implementation of screening into routine practice is challenging. In addition, there is no standardized protocol for screening in pediatric settings.13 Organizations like the American Academy of Pediatrics provide toolkits with suggestions for screening protocol. Previously developed screening tools include the Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education (WE CARE) tool14; the Centers for Medicare and Medicaid Services social determinants of health tool3; the United States Department of Agriculture Food Security Survey15; and single-item questions about income security, housing stability, and neighborhood safety.16 Most screening does not occur in routine clinical practice but instead it occurs in the context of specific research studies and at single institutions or primary care clinics.17–19 Fewer than 25% of hospitals and 16% of physician practices routinely screen for HRSN.20
This article describes implementing an institution-wide, EMR-based HRSN screening protocol at Nationwide Children’s Hospital (NCH). Our specific aim was to improve screening compliance in primary care settings and clinics from 0% to 70% within 12 months and sustain indefinitely. NCH has implemented several community wellness initiatives, including school-based health programs, workforce development training, and home renovations in the surrounding area.21 NCH leadership recognized the importance of these efforts in their 2017–2022 strategic plan by focusing on population health and wellness as a primary driver of best child health outcomes. This focus provided an opportunity to institute an organization-wide HRSN screen for all patients. The Director of Population Health and Equity Research (senior author) and Senior Vice-President for Strategic Planning championed the design and implementation of the screening approach. This report builds on prior social needs screening in single-site or specific multi-site settings (eg, primary care or urgent care).14 Our implementation method and preliminary results can help other large health systems embark on social needs screening programs. As a quality improvement project and not human subjects research, this project did not require IRB review.
METHODS
Setting
Nationwide Children’s Hospital (NCH) is a large, urban pediatric hospital in Columbus, Ohio. NCH provides care for more than 1.5 million patient visits annually, including 89,000 visits to its primary care network. Medicaid is the insurer for half of all NCH patients and nearly 80% of primary care network patients. The hospital-based system also includes a network of specialty and behavioral health clinics, urgent care clinics, and two emergency departments located on the hospital’s main campus and throughout the city.
Engaging Stakeholders in Planning
A steering committee with a broad group of stakeholders across the institution, including administration, clinic, social work leadership, and parents from the Family Advisory Council, led the HRSN screen’s phased roll-out. The Community Wellness Evaluation lead (first author) and a business planning representative co-chaired this committee. The process began with internal and external assessments of existing HRSN efforts. The internal assessment revealed fragmented and inconsistent screening for HRSN throughout NCH. Screening for any HRSN was done at the discretion of the clinical division, and collection methods were inconsistent, ranging from verbal administration to paper and pen. The external assessment involved literature reviews and interviews with representatives from other children’s hospitals to understand the current state of pediatric HRSN screening.
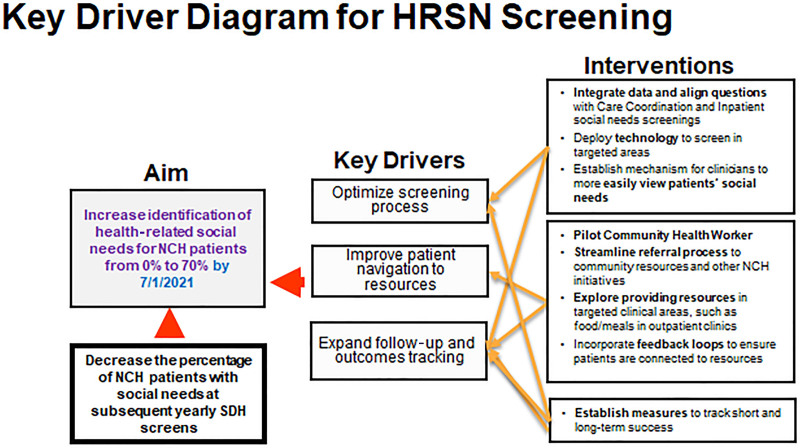
As a result of these assessments, the steering committee identified four key drivers for improving screening compliance: (1) create a universal and standardized method to identify HRSN, (2) administer the screen once a year to all NCH patients, (3) integrate the screen into the EMR, and (4) connect patients and families with community resources to address two tiers of identified needs, general and urgent (Fig. 1). General needs are defined as the risk of homelessness, food insecurity, needing transportation to a medical appointment or pharmacy, and/or having the utility company shut off service for nonpayment. Urgent needs are defined as not having a safe place to sleep tonight, needing community food resources today, not having a plan to get home today, and/or having utilities that are shut off now. Urgent needs received a social work consult, and general needs received a resource sheet for self-referral to community agencies. The steering committee created a key driver diagram and designed interventions to facilitate the HRSN screening and follow-up improvements (Fig. 1). Series of PDSA cycles assisted the project team in reaching our goal of 70% screening in all the settings that we identified.
Fig. 1.
Key driver diagram.
Selection of HRSN Screening Tool
To address the key drivers, standardized screening tool, the committee chose to screen for housing instability, food insecurity, lack of transportation, and inability to pay for utilities, resulting in a total of four items. While there are many HRSN domains, the committee focused on these for the following reasons: (1) Centers for Medicare and Medicaid Services identified them as core social needs and (2) the NCH social work team could readily identify community resources to meet these needs, which is essential given the caution to not screen for needs without appropriate linkages to community resources to address them.22
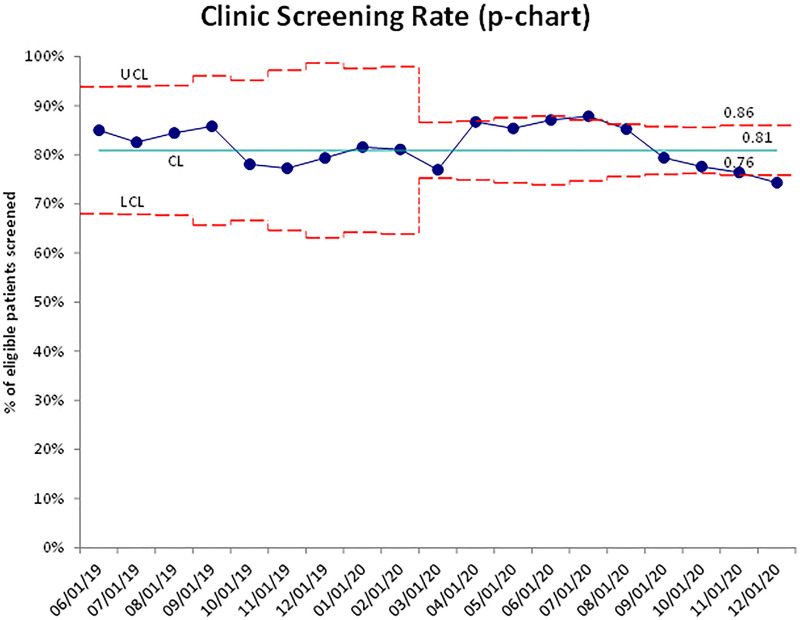
Specific screening items were adapted from evidence-based tools and at a low reading level (between sixth and eighth grade) to ensure comprehension for low literacy populations. In recognition of potential trauma exposures experienced by families,23 the screen aligned with principles of trauma-informed care by including24an introductory statement that explained the purpose of the screen and asked patients to consent to participate. A high percentage of patients and families consented to participate in the screening process (Fig. 2). Patients and families had the opportunity to decline the entire screen, individual screening questions, and/or the social work consult.
Fig. 2.
Control chart of clinic screening rate.
Implementation Process
Clinics were scheduled for a phased roll-out using Plan-Do-Study-Act (PDSA) technique to mitigate any undesired consequences and targeted outreach to clinic leadership to gain better engagement with implementing the screening. All clinics in the initial PDSA cycles had an embedded social worker. This article describes the roll-out to primary care, urgent care, and selected outpatient specialties. The planning phase of these PDSA cycles in new clinics consisted of meeting with physicians, nursing, and social work leadership to provide background about the screen, establish clinic workflow, discuss social work consultation, and address concerns. After this planning meeting, clinic and social work staff were trained by their supervisors. However, physicians did not receive targeted training as they were not operationally part of the screening process.
The first PDSA cycle, the initial HRSN screening roll-out, began in June 2018 in two primary care clinics. We quickly expanded the PDSA by December 31, 2019, to include additional clinical settings—primary care clinics (n = 12), outpatient specialty clinics (n = 12), (Behavioral Health Clinics (n = 2), Healthy Weight and Nutrition Clinics (n = 4), Teen and Pregnant Clinics (n = 2), Birth Control for Teens clinic (n = 1) Genetics Clinic (1 Clinic), Pulmonary Clinic (1 clinic), Cardiology (1 clinic)), and urgent care clinics (n = 7). Outpatient specialty clinics continued to “go live” throughout 2020. All patients were eligible to be screened annually. In most clinics, whoever roomed the patient (eg, nurse, medical assistant) asked the HRSN questions (See Appendix A, Supplemental Digital Content 1, which shows the flow map of the HRSN screening process http://links.lww.com/PQ9/A351). Information Services built flowsheet rows in department navigators in the EMR. The EMR build included cascading logic so that if a family endorsed a social need, a question appeared to assess urgency (See Appendix A, Supplemental Digital Content 1, which shows the flow map of the HRSN screening process, http://links.lww.com/PQ9/A351). If the need was urgent, an alert was displayed to consult social work according to established clinic protocol. Current social work staffing levels were adequate to handle consults for urgent needs. If a social worker was not available, staff could contact the “on-call” social worker. Additionally, social workers could view a dashboard in the EMR for families with urgent needs. The committee requested continued feedback from clinic staff and social workers. The phrasing of questions to identify urgent needs changed three times based on this feedback.
Families with non-urgent needs received a resource sheet. The resource sheet, created in conjunction with the Director of Social Work, included the following sections: emergency Franklin County (where NCH is located) resources (eg, homeless hotline in case families need emergency help in the future), non-emergency resources within Franklin County (eg, enrolling in benefits), resources outside Franklin county, and cultural agencies throughout Franklin County and the state (eg, religious- or ethnic- focused groups). The resource sheet was updated as part of PDSA cycles to have the most up-to-date and relevant information. The resource sheet was also available in Arabic, English, Nepali, Spanish, and Somali.
Social Work Protocol Responding to Needs
When families opted for a consult, social workers documented the encounter using the standard social work note template in the EMR. Social workers documented in the EMR interventions provided to families. Patients remained on the dashboard social work note for that patient appeared or for 7 days.
To provide feedback on the PDSA cycles of HRSN implementation, the project team reviewed weekly data and provided social work supervisors with medical record numbers for patients who did not consult within 7 days of the visit. This intervention ensured that all patients with urgent needs received a social work consult if desired.
Screening Metrics
The evaluation team continually monitored the following metrics during the implementation process:
Percentage of patient encounters with a completed HRSN screen out of total eligible patient encounters reported by the clinic. Completed screens had a response (Yes or No/Decline) to the initial question, “Are you okay with me asking you the questions?” (Appendix A. http://links.lww.com/PQ9/A351. The goal was for each clinic to screen ≥70% of eligible patients.
Percentage of patients with at least one urgent need who received a social work consult within 7 days of the screening. The goal was for ≥ 95% of social work consults to occur within 7 days.
Patient Characteristics
Patient characteristics (including patient sex, race, age, and primary spoken language) were tracked. All patient characteristics were abstracted from the patient’s electronic medical record. Race was categorized as White, Black, Asian, Hispanic, or Other (American Indian, Alaska Native, Multi-racial, Native Hawaiian, or Pacific Islander). The most common languages spoken in the hospital network (English, Arabic, Nepali, Somali, and Spanish) were reported, with the remaining languages reported in aggregate as “Other.” Age was categorized into less than 1, 1–5, 6–10, 11–18, and greater than 18.
Analysis
Descriptive statistics examine patient characteristics, both overall and by clinic type (ie, primary care, urgent care, and other specialty clinics) to evaluate screening rates. We reported both general and urgent needs for screened patients. Social work interventions are identified from discrete fields (eg, completed referral, provided/linked with resources, safety planning, mandated reporting, etc.) included in the social work notes. We only included interventions documented through the discrete field options. Social work consults occurred if a social work note appeared in the EMR within 7 days of the visit when patients disclosed urgent need(s).
We employed statistical process control charting to analyze and display our main outcome measure—HRSN screening rate at the targeted clinics. Specifically, a p-chart is utilized to display the compliance percentages. The upper and lower control limits allowed us to ensure that the screening process is within control and recognize if a “special cause variation” has been induced by our PDSA cycles. Months are displayed on the x axis, and a percentage of patients screened for HRSN are displayed on the y axis.
Additionally, retrospective chart reviews provided further details about social work follow-up because discrete fields may not have captured the breadth of interventions. We reviewed 100 randomly selected patient charts to assess the timing and modality (ie, in-person or telephone) of the consult, along with specific details about the resources provided or referrals given.
RESULTS
Demographic characteristics were reported for the patient, while patients or family members could provide screening responses. Currently, 110,353 patient encounters were eligible for screening, and 85.8% (95,802) were screened (ie, had a documented response [“Yes” or “No”] to the initial question). Patients declined the screen 10.7% of the time. The screening rate did not go below 74% during the first 19 months of implementation; however, screening rates degraded in the last few months of 2020 (Fig. 2). Screening percentages for each clinic ranged from 88.7% (primary care clinics) to 78.8% (outpatient specialty clinics) (Table 1).
Table 1.
Patient and Visit Characteristics of Patients Screened for Social Determinants of Health (N = 110,353)*
| Patient Characteristics | Overall 31 Clinics, % (N) |
Primary Care Clinics 12 Clinics, % (N) |
Urgent Care Clinics 7 Clinics, % (N) |
Outpatient Specialty Clinics† 12 Clinics, % (N) |
|---|---|---|---|---|
| Gender (n = 110,349) | ||||
| Men | 50.5% (55,694) | 50.8% (37,074) | 50.2% (16,446) | 45.3% (1041) |
| Women | 49.5% (54,655) | 49.3% (38,207) | 49.8% (16,326) | 54.7% (1255) |
| Age (y) | ||||
| <1 | 12.9% (14,276) | 14.9% (11,200) | 9.1% (2975) | 4.4% (101) |
| 1–5 | 35.2% (38,873) | 34.2% (25,731) | 39.2% (12,836) | 13.3% (306) |
| 6–10 | 23.8% (26,250) | 23.4% (17,618) | 25.1% (8234) | 17.3% (398) |
| 11–18 | 26.4% (29,178) | 26.6% (20,023) | 24.8% (8141) | 44.2% (1014) |
| >18 | 1.6% (1776) | 1.0% (712) | 1.8% (587) | 20.8% (477) |
| Race (n = 109,394) | ||||
| White | 27.6% (30,189) | 15.4% (11,496) | 53.6% (17,066) | 73.2% (1627) |
| Black | 41.2% (45,048) | 47.5% (35,487)) | 28.5% (9249) | 14.0% (312) |
| Asian | 6.2% (6727) | 7.3% (5456) | 3.8% (1229) | 1.9% (42) |
| Hispanic | 11.7% (12,801) | 15.0% (11,211) | 4.7% (1518) | 3.2% (72) |
| Other | 13.4% (14,629) | 14.8% (11,042) | 10.5% (3416) | 7.7% (171) |
| Language (n = 110,289) | ||||
| English | 72.1% (79,496) | 64.2% (48,291) | 88.6% (29,011) | 95.6% (2194) |
| Arabic | 1.3% (1459) | 1.5% (1151) | 0.9% (299) | 0.4% (9) |
| Nepali | 3.8% (4,234) | 5.0% (3791) | 1.3% (438) | 0.2% (5) |
| Somali | 7.5% (8276) | 9.5% (7176) | 3.3% (1088) | 0.5% (12) |
| Spanish | 10.1% (11,161) | 13.3% (10,020) | 3.3% (1083) | 2.5% (58) |
| Other | 5.1% (5663) | 6.4% (4,836) | 2.5% (809) | 0.8% (18) |
| Screen | ||||
| Completed screen | 86.8% (95,802) | 88.7% (66,776) | 83.0% (27,215) | 78.8% (1811) |
| Declined screen | 13.2% (14,551) | 11.3% (8,508) | 17.0% (5,558) | 21.1% (485) |
*Answered Yes or No/Decline to the introductory question.
**Behavioral Health Clinic (2 clinics), Healthy Weight and Nutrition Clinic (4 clinics), Teen and Pregnant Clinic (2 clinics), Genetics Clinic (1 Clinic), Pulmonary Clinic (1 clinic), Cardiology (1 clinic), and Birth Control for Teens (1 clinic).
The prevalence of screening varied by patient characteristics (Table 2), such that male patients were screened during 70.6% of eligible encounters, compared with 70.4% for female patients (P value = 0.21) (Table 2). Overall screening rates did not fall below 70% for any racial group. Differences in screening rates were observed based on the language spoken, ranging from 63.6% for Arabic speakers to 75.6% for Nepali speakers. The screening rate was lower among patients over 18 (48.5% (1365)). A higher percentage of White patients were not offered the screen, 23.6% (9336), compared with non-White patients. There was little difference in the rate of declining the screen by race: 9.6%–11.9% (Table 2).
Table 2.
Screening Rate by Patient Characteristics
| Answered Screen | Declined Screen | Not Offered Screen | P | |
|---|---|---|---|---|
| % (N) | % (N) | % (N) | ||
| Patient Characteristics | ||||
| Gender (n = 135,824) | 0.21 | |||
| Men | 70.6% (48,307) | 10.8% (7387) | 18.6% (12,689) | |
| Women | 70.4% (47,491) | 10.6% (7164) | 19.0% (12,786) | |
| Age (n = 135,828) | <0.0001 | |||
| <1 | 75.6% (12,975) | 8.8% (1481) | 15.6% (2645) | |
| 1–5 | 72.8% (34,228) | 9.9% (4645) | 17.3% (8134) | |
| 6–10 | 71.5% (22,897) | 10.5% (3353) | 18.1% (5795) | |
| 11–18 | 66.2% (24,517) | 12.6% (4661) | 21.2% (7860) | |
| >18 | 48.5% (1365) | 14.6% (411) | 37.0% (1041) | |
| Race (n = 134,490) | <0.0001 | |||
| White | 64.4% (25,468) | 11.9% (4721) | 23.6% (9336) | |
| Black | 74.2% (39,497) | 10.4% (5551) | 15.4% (8207) | |
| Asian | 71.2% (5930) | 9.6% (797) | 19.3% (1608) | |
| Hispanic | 71.6% (11,213) | 10.1% (1588) | 18.3% (2857) | |
| Other | 72.7% (12,873) | 9.9% (1756) | 17.4% (3088) | |
| Language (n = 135,597) | <0.0001 | |||
| English | 70.3% (68,722) | 11.0% (10,774) | 18.7% (18,315) | |
| Arabic | 63.6% (1174) | 15.4% (285) | 21.0% (388) | |
| Nepali | 75.6% (3889) | 6.7% (345) | 17.7% (912) | |
| Somali | 72.0% (7298) | 9.7% (978) | 18.4% (1862) | |
| Spanish | 71.3% (9779) | 10.1% (1382) | 18.6% (2555) | |
| Other | 70.3% (4879) | 11.3% (784) | 18.4% (1276) |
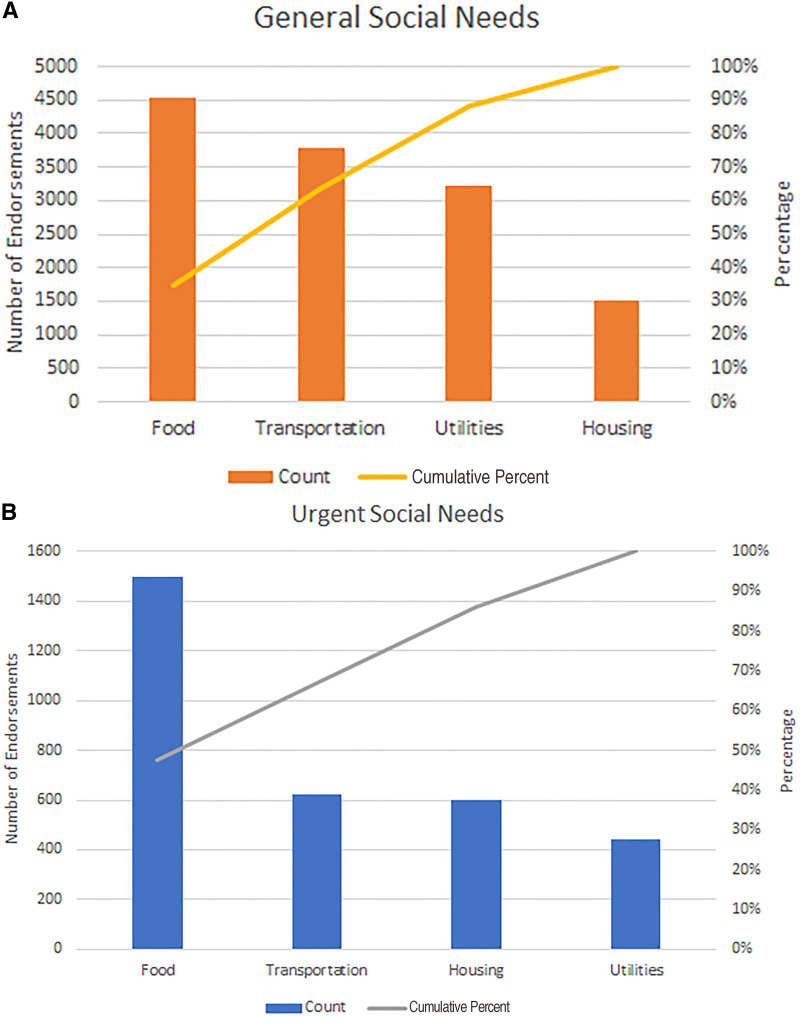
Among patients who completed the screen, 9.7% (n = 9296) endorsed at least one need (See Appendix B, Supplemental Digital Content 2, which shows types of needs reported among those with a completed screen, http://links.lww.com/PQ9/A352). The most frequently endorsed need was food insecurity (4.7%), followed by transportation to medical appointments (4.0%) (Fig. 3A). Urgent needs mirrored this trend, with food insecurity (1.6%) as the most cited need, with transportation (0.6%) and housing (0.6%) as the next most-cited urgent need (Fig. 3B). Thus, the need for food and transportation accounted for 64% of all reported general needs and 67% of urgent needs. Overall, 2.9% of those screened reported an urgent need (See Appendix B, Supplemental Digital Content 2, which shows types of needs reported among those with a completed screen, http://links.lww.com/PQ9/A352).
Fig. 3.
Type of social needs reported by number of endorsements from unique patients and percentage of total needs disclosed. A, Pareto chart of general needs endorsed by type. B, Pareto chart of urgent needs endorsed by type.
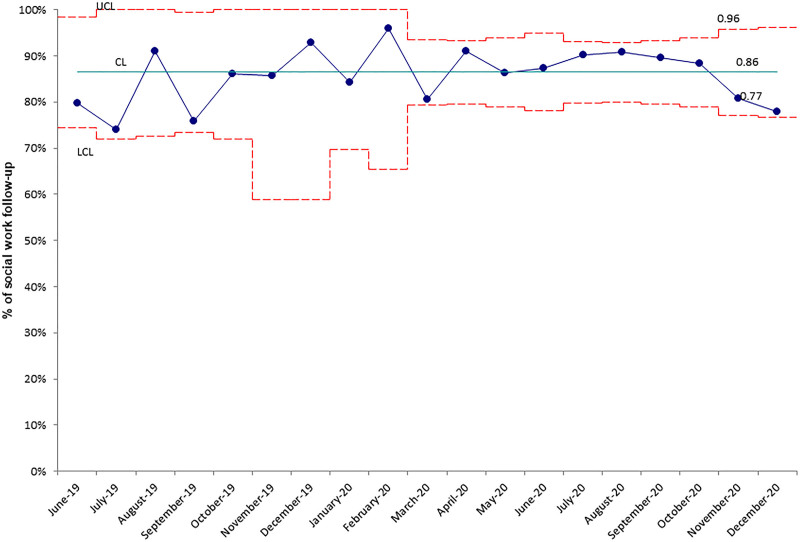
About 86% of social work consults occurred within seven days for patients endorsing an urgent need. This result was below the goal of 95% (Fig. 4). The most frequent social work intervention included providing or linking patients with resources (55.7%), followed by a referral (3.1%). These results represent only referrals and interventions documented in the EMR’s discrete fields, not in the free-text notes.
Fig. 4.
Control chart of clinic social work follow-up rate.
Based on detailed chart reviews of a random sample of patients with urgent needs (n = 100), we learned that 65% of social work consults occurred in the clinic and 35% by phone within a week of their appointment, although there was no answer for 14% of these calls. In addition, social workers mailed resource packets to everyone without a phone or in-person visit. On average, the social work consult lasted 41 minutes (range: 15–240 minutes). The most common resource provided was information on local food banks and pantries.
DISCUSSION
These results indicate early implementation success in achieving or surpassing the 70% screening goal, highlighting the feasibility of standardized, universal HRSN screening in various clinic settings and levels of patient acuity using an EMR platform and social work consult follow-up. We did see a slight degradation in screening rates, which is likely due to the additional volume of patients as clinics continue to “go live” as part of the phased roll-out. Our purpose in utilizing a universal screening approach was to help avoid biases inherent in a targeted screening of patient populations based on perceptions of risk and miss capturing HRSN for patients who may not fit typical risk profiles.25 Overall, 9.7% of patients reported at least one HRSN need, and 2.9% endorsed an urgent need. Social work consults occurred for all families with urgent needs who desired contact, and 85.6% took place within 7 days of screening administration. Initial concerns that social workers would be overwhelmed by identified needs were unfounded. Limiting consults to urgent needs and the early roll-out to clinics with embedded social workers kept the workload change manageable.
Self-disclosure of needs was lower than expected. For example, the food insecurity rate was 4%, which is lower than previous estimates of 14%.26 Verbally administering the screen, as opposed to self-report, may result in lower need disclosures due to social desirability bias or feelings of stigma.27–29 However, the American Academy of Pediatrics recommends screening all patients for HRSNs through a verbal or self-report screen.30 While different modalities may lead to greater need disclosure, the American Academy of Pediatrics recommends both verbal and self-report screening.
Differences in screening rates by patient characteristics were generally small. Still, a more significant difference was observed based on patient age (48.5% for patients over 18 versus 75.6% for patients under 1) and language spoken (63.0% for Arabic speakers versus 70.3% for English speakers). Lower completion rates in non-English speakers suggest opportunities for improving engagement of interpreter services. Lower screening rates for older adolescents/young adults may be caused by staff feeling more comfortable screening parents than unaccompanied older adolescents. This finding warrants further examination to ensure appropriate staff education. Lower rates of screening White families may reflect bias or assumptions of lower needs, which also suggests additional training and accountability in making our universal screening truly universal and representative.
This initiative was not without limitations. First, the screen only included four domains. Including additional domains could provide a more comprehensive profile of HRSN; however, restricting the number of domains aided in obtaining clinic staff buy-in and implementing the screen across multiple clinic settings. Second, providing a resource sheet for families may be insufficient to connect them with resources successfully. While most HRSN screening initiatives distribute lists of available community resources, families may benefit from “warm hand-off” connections to community agencies.18,31 Although our approach offered social work support only for urgent needs, additional navigation support would likely prove valuable. Third, there is not yet a feedback loop between the hospital and community agencies, reducing the ability to track whether referrals resulted in a connection to resources. Future planning will include the incorporation of electronic feedback loops. Finally, it is essential to note that this is not a research study. Processes and tools changed during the implementation and will continue to meet clinical and operational needs best. As such, these results are not intended to be generalizable. Instead, they offer one implementation model that is showing success.
Instituting a health system-wide HRSN screen requires commitment and engagement from multiple partners, ranging from hospital leadership to information technology to interpreter services. This process included balancing complex and sometimes conflicting needs, such as valuing patient choice, integrating the screen into the EMR, not impeding clinic workflow, and appropriately alerting social work. Allowing clinics to determine optimal workflow for the screen proved the most efficient way to manage the complexity of needs. The present study results suggest that this approach was feasible in routine clinical care, achieving high levels of screening and follow-up. Therefore, hospital administration supports continued investment in the HRSN screening initiative. Future plans include completing the screening roll-out, exploring technology options for screen administration, engaging community health workers to provide “warm hand-offs” to resources, and examining screening rates to identify “hot spots” of needs to provide targeted resources at a community level. Notably, while parents described the screening as “acceptable” and “helpful” informative qualitative evaluations (not published), additional research is needed to understand the degree to which families’ social needs are truly and sustainably met.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online January 21, 2022.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Dolce M, Hannah Keedy H, Chavez L, Boch S, Zaim H, Dias B, Chisolm D. Implementing an EMR-based Health-Related Social Needs Screen in a Pediatric Hospital System. Pediatr Qual Saf 2022;7:e512.
REFERENCES
- 1.CoSDoH (CSDH). Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the commission on social determinants of health. World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 2.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21:78–93. [DOI] [PubMed] [Google Scholar]
- 3.Alexander Billioux KV, Susan A, Dawn A. Standardized screening for health-related social needs in clinical settings: The Accountable Health Communities Screening Tool. National Academy of Medicine; 2017. [Google Scholar]
- 4.Feltner C WI, Berkman N, et al. Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: An Evidence Review for the U.S. Preventive Services Task Force Agency for Healthcare Research and Quality. 2018. Available at https://www.ncbi.nlm.nih.gov/books/NBK533720/. Accessed March 16, 2020. [PubMed]
- 5.National Academy of Science EaM. A Roadmap to Reducing Child Poverty. The National Academies; 2019. [PubMed] [Google Scholar]
- 6.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr. 2009;9:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wise PH. Child poverty and the promise of Human Capacity: childhood as a foundation for healthy aging. Acad Pediatr. 2016;16(suppl 3):S37–S45. [DOI] [PubMed] [Google Scholar]
- 9.Hood CM, Gennuso KP, Swain GR, et al. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med. 2016;50:129–135. [DOI] [PubMed] [Google Scholar]
- 10.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGovern L. The relative contribution of multiple determinants to health. Health Affairs Health Policy Brief. 2014:1–9. doi: 10.1377/hpb20140821.404487 [Google Scholar]
- 12.Gottlieb L, Fichtenberg C, Alderwick H, et al. Social determinants of health: what’s a healthcare system to do? J Healthc Manag. 2019;64:243–257. [DOI] [PubMed] [Google Scholar]
- 13.Boch S, Keedy H, Chavez L, et al. An integrative review of social determinants of health screenings used in primary care settings. J Health Care Poor Underserved. 2020;31:603–622. [DOI] [PubMed] [Google Scholar]
- 14.Garg A, Butz AM, Dworkin PH, et al. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120:547–558. [DOI] [PubMed] [Google Scholar]
- 15.Bickel GNM, Price C, Hamilton W, et al. Guide to Measuring Household Food Security, Revised 2000. Department of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 16.Leads H. The opportunity. 2020. Available at https://healthleadsusa.org/the-opportunity/. Accessed March 16, 2020.
- 17.Bottino CJ, Rhodes ET, Kreatsoulas C, et al. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr. 2017;17:497–503. [DOI] [PubMed] [Google Scholar]
- 18.Garg A, Toy S, Tripodis Y, et al. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135:e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hassan A, Scherer EA, Pikcilingis A, et al. Improving social determinants of health: effectiveness of a web-based intervention. Am J Prev Med. 2015;49:822–831. [DOI] [PubMed] [Google Scholar]
- 20.Fraze TK, Brewster AL, Lewis VA, et al. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US Physician Practices and Hospitals. JAMA Netw Open. 2019;2:e1911514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelleher K, Reece J, Sandel M. The healthy neighborhood, healthy families initiative. Pediatrics. 2018;142:e20180261. [DOI] [PubMed] [Google Scholar]
- 22.Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316:813–814. [DOI] [PubMed] [Google Scholar]
- 23.Mendel WE, Sperlich M, Fava NM. “Is there anything else you would like me to know?”: applying a trauma-informed approach to the administration of the adverse childhood experiences questionnaire. J Community Psychol. 2021;49:1079–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.SAMHSA. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 25.Sundar KR. Universal screening for social needs in a primary care clinic: a quality improvement approach using the your current life situation survey. Perm J. 2018;22:18–089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.USDA Economic Research Service. Key Statistics & Graphics. USDA ERS – Key Statistics & Graphics. Available at https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx#:~:text=Household%20food%20insecurity%20affected%2013.6,only%20adults%20were%20food%20insecure.). Accessed March 16, 2020. [Google Scholar]
- 27.Gottlieb L, Hessler D, Long D, et al. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics. 2014;134:e1611–e1618. [DOI] [PubMed] [Google Scholar]
- 28.Gnambs T, Kaspar K. Disclosure of sensitive behaviors across self-administered survey modes: a meta-analysis. Behav Res Methods. 2015;47:1237–1259. [DOI] [PubMed] [Google Scholar]
- 29.Schleifer DD, A, Grisham K. It’s about trust: low-income parents’ perspectives on how pediatricians can screen for social determinants of health. Public Agenda. 2019. [Google Scholar]
- 30.American Academy of Pediatrics. Social determinants of health. Available at https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Screening/Pages/Social-Determinants-of-Health.aspx. Accessed March 16, 2020.
- 31.Smith S, Malinak D, Chang J, et al. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California. Prev Med Rep. 2017;5:134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.