Abstract
Individual differences in interpretation biases—the tendency to interpret ambiguous stimuli as threatening—partially explain the presence of comorbid depressive symptoms among anxious youth. Increasing efforts have examined physiological processes that influence the association between interpretation biases and depressive symptoms in this population, and potential gender differences in this relationship. This study examined the moderating role of respiratory sinus arrhythmia (RSA) suppression (i.e., decrease from baseline)—an index of parasympathetic nervous system reactivity—in the association between interpretation biases and depressive symptoms in clinically anxious youth. One-hundred-and-five clinically anxious children (Mage = 10.09 years, SD = 1.22; 56.7% female; 61.9% racial/ethnic minority) completed measures of self-reported and behaviorally indexed interpretation biases, reported anxiety/depression symptom severity, and participated in a speech task. RSA suppression during the task moderated the association between interpretation biases and depressive symptom severity in the total sample. Separate exploratory moderation analyses were conducted among girls and boys. Among girls, RSA suppression moderated the association between behaviorally indexed interpretation biases and depressive symptoms, and marginally moderated (p = .067) the association between self-reported interpretation biases and depressive symptoms. Among boys, RSA suppression was not a significant moderator. These findings may help identify clinically anxious youth most at-risk for comorbid depressive symptoms.
Keywords: anxiety, child, cognition, depression, emotion
1 ∣. INTRODUCTION
Among youth with anxiety disorders, the presence of a comorbid depressive disorder is exceedingly common (Costello, Egger, Copeland, Erkanli, & Angold, 2011; Merikangas et al., 2010). As many as 56% of anxiety-disordered youth meet criteria for a depressive disorder (Masi et al., 2004), and the two disorders have an 8.2 median odds ratio of co-occurrence (Angold, Costello, & Erkanli, 1999; Costello et al., 2011). These findings are quite troubling, as comorbid depression or even subthreshold depressive symptoms among clinically anxious youth is associated with greater impairment and family dysfunction, lower global functioning, less favorable treatment outcomes, and increased risk for suicidality (O’Neil & Kendall, 2012; Rapee et al., 2013; Rivas-Vazquez, Saffa-Biller, Ruiz, Blais, & Rivas-Vazquez, 2004). Moreover, research suggests that anxiety-depression comorbidity may be more prevalent (Lewinsohn, Rohde, & Seeley, 1995) and more severe (Wadsworth, Hudziak, Heath, & Achenbach, 2001) in girls than boys.
A number of risk factors contribute to comorbid anxiety and depression symptoms in clinically anxious youth, including cognitive biases (e.g., interpretation biases; Muris, Luermans, Merckelbach, & Mayer, 2000) and emotion dysregulation (Suveg, Hoffman, Zeman, & Thomassin, 2009). Yet, synergistic effects between these risks, as well as potential gender differences underlying these effects, are understudied (Cummings, Caporino, & Kendall, 2014). This investigation aimed to fill this gap in the literature by examining emotion regulation, indexed by respiratory sinus arrhythmia (RSA), as a moderator of the association between interpretation biases and comorbid depression symptoms in clinically anxious youth. Exploratory analyses also examined gender differences in these effects.
Interpretation biases reflect a tendency to interpret ambiguous or neutral stimuli in a negative or threatening manner, which increases the risk for anxiety, depression, and their co-occurrence (Alfano, Zakem, Costa, Taylor, & Weems, 2009; Weems, Costa, Watts, Taylor, & Cannon, 2007). For instance, children with anxiety disorders, compared with their nonanxious peers, are more likely to interpret ambiguous scenarios or stimuli in a threatening manner (Barrett, Dadds, & Rapee, 1996; Taghavi, Moradi, Neshat-Doost, Yule, & Dalgleish, 2000). Self-reported trait anxiety correlates with the proportion of homonyms (e.g., “dye” vs. “die”) that children interpret in a threatening manner (Hadwin, Frost, French, & Richards, 1997). Longitudinal studies have also found that interpretation biases in youth remained stable across 3 years (Creswell & O’Connor, 2011) and significantly predicted anxiety severity at a 12-month follow-up after adjusting for baseline anxiety (Dodd, Hudson, Morris, & Wise, 2012).
Interpretation biases are also associated with childhood depression symptoms. For example, Muris et al. (2000) found that children who rated ambiguous stories as threatening endorsed higher depression scores. A study of 8-year-olds (N = 600) found that negative interpretations of ambiguous words and scenarios correlated with depression severity after controlling for anxiety symptoms (Eley et al., 2008), a finding that has been replicated in 6–17-year-old youth (Alfano et al., 2009). A separate study found that 10–14-year-old daughters of depressed mothers (i.e., youth genetically at-risk for depression) interpreted ambiguous words and stories more negatively than did girls of healthy mothers (Dearing & Gotlib, 2009), suggesting that interpretation biases may precede depression. Notably, interpretation biases may also play a role in the co-occurrence of anxiety and depression. In a sample of undergraduate students, maladaptive interpretations of social events were associated with social anxiety, and greater endorsement of these interpretations were associated with comorbid social anxiety and depressive symptoms (Wilson & Rapee, 2005).
There are, however, significant lacunae regarding the role of interpretation biases in comorbid depression among clinically anxious youth. For instance, despite robust associations among interpretation biases and both childhood anxiety (Taghavi et al., 2000) and depression symptoms (Dearing & Gotlib, 2009), not all youth with interpretation biases go on to develop anxiety disorders or comorbid depression. Such heterogeneity in clinical outcomes underscores the need to advance the understanding of individual difference factors, particularly in the affective domain, that may influence interpretation biases–depression associations among clinically anxious youth (Chorpita, 2002; Zahn-Waxler, Shirtcliff, & Marceau, 2008). This line of inquiry has the potential to inform specialized, person-centered approaches to treatment.
One individual difference factor with relevance to the interpretation biases–depression association in clinically anxious youth is RSA (Beauchaine, 2015), defined as the rhythmic fluctuations in heart rate associated with the respiratory cycle. RSA reflects input from the vagus nerve to the heart, and it serves as a measure of the degree of activation of the parasympathetic nervous system (PNS)—the branch of the autonomic nervous system that is involved in processes of self-regulation and restoration (Porges, 2007). According to Porges’ polyvagal theory, this input from the vagus nerve to the heart functions as a “brake” that slows down the heart, resulting in bidirectional connectivity between the heart and central nervous system to regulate arousal (Porges, 2007). High RSA at baseline indicates greater PNS control and signals greater emotion regulatory capacity during resting states (Porges, 2007). Children with higher baseline RSA demonstrate better emotion regulation skills, social skills, and problem-solving skills (Blandon, Calkins, Keane, & O’Brien, 2009; Staton, El-Sheikh, & Buckhalt, 2009). While baseline RSA indexes emotional functioning in the absence of threat, RSA suppression (i.e., the decrease in RSA from baseline) reflects the ability to modulate one's arousal in order to flexibly respond to an immediate threat (Porges, 2007). RSA has been recognized as a biomarker for emotion regulation with clinical relevance to child anxiety and depressive symptoms (Zeman, Cassano, Perry-Parrish, & Stegall, 2006).
Low RSA suppression in response to stressors is generally associated with poorer emotion regulation skills and increased internalizing symptoms in children (Hinnant & El-Sheikh, 2009; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). In contrast, greater RSA suppression is typically associated with better emotion regulation and social skills, and fewer externalizing symptoms in children (Calkins & Keane, 2004; Lunkenheimer, Kemp, Lucas-Thompson, Cole, & Albrecht, 2017). Greater RSA suppression has also been identified as a protective factor against various socioemotional problems. For example, the association between parental problem drinking and child externalizing and internalizing symptom severity was weaker among children with greater RSA suppression (El-Sheikh, 2001). Similarly, among adolescents exposed to high levels of marital conflict, RSA suppression was related to fewer internalizing and externalizing symptoms over time, whereas RSA augmentation (i.e., RSA increase in response to a stressor) increased adolescents’ risk for these outcomes (Philbrook, Erath, Hinnant, & El-Sheikh, 2018).
It is important to note, however, that the protective effects of RSA suppression may be conditional on several factors, such as whether the effects of baseline RSA are accounted for, the context in which RSA is measured, as well as the ethnic composition of the studied samples. Specifically, a recent meta-analysis examining RSA suppression and adaptive functioning in children (N = 4,996) found that although greater RSA suppression was generally associated with fewer internalizing and externalizing symptoms, these effects were stronger in samples containing a high percentage of White children, as well as in studies that controlled for baseline levels of RSA (Graziano & Derefinko, 2013). A separate study found that RSA suppression was differentially associated with internalizing and externalizing symptoms as a function of the type of emotional challenge during which RSA was measured. Specifically, greater RSA suppression during a fearful/sad film clip was associated with greater internalizing symptoms, while blunted (i.e., smaller) RSA suppression during a happy film clip was associated with greater externalizing symptoms (Fortunato, Gatzke-Kopp, & Ram, 2013). Obradović, Bush, and Boyce (2011) found that marital conflict was associated with greater externalizing symptoms among children with greater RSA suppression to a cognitive challenge task, as well as among children with lower RSA suppression to an interpersonal challenge task. With regards to speech tasks specifically, Han, Zhang, Davis, and Suveg (2019) found that children exposed to emotionally supportive parenting exhibited fewer anxiety symptoms in the context of greater RSA suppression, suggesting that RSA suppression in response to a speech task may be protective. Likewise, despite its well-established utility as a physiological index of emotion regulation, RSA can be influenced by changes in motor and attentional demands unrelated to emotional functioning (Bush, Alkon, Obradović, Stamperdahl, & Thomas Boyce, 2011). For example, prior studies have shown that RSA in youth may be influenced by attentional engagement (Beauchaine, 2001) and physical position (e.g., sitting, standing, walking; Houtveen, Groot, & de Geus, 2005). Collectively, these findings underscore the need for a nuanced approach to the interpretation of RSA findings, as well as for more research to parse apart the effects of interpretation biases and RSA suppression on child anxiety and depression psychopathology.
In this vein, research has found that the comorbidity of depressive and anxiety symptoms is more common in girls than in boys (Lewinsohn et al., 1995), and cases of comorbidity between depression and two or more anxiety disorders are found virtually exclusively among adolescent girls (Lewinsohn, Zinbarg, Seeley, Lewinsohn, & Sack, 1997). Girls are also more prone to endorse negative cognitive styles that increase vulnerability to depression (e.g., attributing negative events to internal, stable, and global causes; Hankin & Abramson, 2002; Nolen-Hoeksema, 2001). Girls also suppress negative emotions more than boys (e.g., hiding disappointment; Zahn-Waxler, Crick, Shirtcliff, & Woods, 2006), which is theorized to contribute to girls’ increased susceptibility to internalizing disorders (Zahn-Waxler et al., 2008).
In addition to gender differences in anxiety–depression comorbidity and patterns of cognitive vulnerability, a growing body of evidence suggests that the moderating effect of RSA suppression on the association between risk and psychopathology may also vary as a function of gender. These data, however, are mixed. For instance, El-Sheikh, Harger, and Whitson (2001) found that greater RSA suppression during an adult argument buffered the impact of marital conflict on behavioral problems among boys, but not girls. In contrast, a recent study found that greater RSA suppression during various affective challenges was related to greater externalizing problems among girls who were high in exuberance (a temperamental trait; Morales, Beekman, Blandon, Stifter, & Buss, 2014). A separate investigation found that interparental conflict was related to greater internalizing problems only among girls with low RSA suppression (El-Sheikh & Whitson, 2006). Unfortunately, gender differences in RSA suppression as a moderator of the association between interpretation biases and depression symptoms are yet to be explored, in general, and among clinically anxious youth specifically.
The present investigation examined RSA suppression as a moderator of the association between interpretation biases and depression symptoms in a sample of anxiety-disordered youth. First, consistent with extant literature, we hypothesized that interpretation biases would be related to both anxiety and depression symptoms at the bivariate level. Second, we hypothesized that RSA suppression would moderate the association between interpretation biases and depression symptoms, such that greater interpretation biases would be associated with more severe depression symptoms among children with lower (vs. greater) RSA suppression. Given gender differences in anxiety–depression co-occurrence, emotion regulation, and RSA (Hankin, 2009; Morales et al., 2014; Zahn-Waxler et al., 2008), exploratory moderation analyses were also conducted separately among boys and girls. However, absent a clear pattern of findings in the literature (Graziano & Derefinko, 2013), it was deemed premature to make specific hypotheses regarding gender differences.
2 ∣. METHOD
2.1 ∣. Participants
The present study consisted of a secondary analysis of data collected from child–mother dyads who participated in an investigation examining the effects of maternal interpretation biases on child anxiety.1 Eligibility criteria included: (a) child between 8–12 years of age; (b) child having primary diagnosis of an anxiety disorder, as determined by either the child or mother clinical interview; (c) mother reporting clinical anxiety, by either clinical interview or scoring in the clinical range for anxiety in the Depression, Anxiety, and Stress Scales (Lovibond & Lovibond, 1995), and (d) child residing with mother at the time of enrollment. The latter two inclusion criteria were requirements of the larger-scale investigation that examined the effects of maternal interpretation biases on child anxiety. Exclusionary criteria included: (a) physical disability impairing ability to use a computer; (b) borderline or extremely low intellectual functioning (IQ < 80 based on the Wechsler Intelligence Scale for Children-IV [WISC-IV] Block Design and Vocabulary subtests; see Section 2.2); (c) below average reading comprehension (standardized composite score <75 based on the Wechsler Individual Achievement Test-III [WIAT-III] Reading Comprehension and Fluency subtests; see Section 2.2); (d) child concurrent primary diagnosis of any nonanxiety disorder; (e) child currently receiving behavioral or pharmacological treatment for anxiety; (f) child being a danger to self or others; (g) non-English speaking child or parent; (h) maternal involvement in cognitive-behavioral therapy and/or maternal changes in pharmacological treatment in the 12 weeks preceding study enrollment. Given the goals of the original trial, mothers involved in cognitive-behavioral therapy and/or recent changes in pharmacological treatment were excluded because both of these treatment modalities are designed to improve distorted thinking and anxiety symptoms.
A total of 152 mother–child dyads were initially enrolled and completed the first session. Based on the results from eligibility assessments conducted during the first session, eight families were excluded due to low child cognitive functioning, six families were excluded due to the child not having an anxiety disorder according to clinical interview, 13 families were excluded due to the mother not having clinical levels of anxiety, and 11 families were excluded due to neither the child having an anxiety disorder nor the mother having clinical levels of anxiety. The remaining dyads (n = 114) were invited to complete the second session. Nine additional dyads were excluded due to incomplete data or dropout, leaving a final sample of 105 dyads who completed both sessions and whose data were included in the present study.
The final sample consisted of 105 children ages 8–12 years (Mage = 10.07 years, SD = 1.22; 57% female). Thirty-eight percent of children self-identified ethnically/racially as non-Hispanic White, 28.6% as Hispanic, 17.1% as multiracial, 14.3% as African American, and 1.9% as Asian American. Twenty-three percent of families reported an annual household income of under $40,000, 38.1% between $40,000 and $100,000, 36.2% over $100,000, and 2.9% did not report their income. Three percent of mothers reported less than a high school education, 23.8% had a high school degree or a GED, 53.3% had a college degree, 19.0% had a graduate degree, and 1.0% did not report education. At the time of enrollment, 67% of mothers were married, and 50% of mothers were working full-time. Children met Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) criteria for at least one anxiety disorder, according to semistructured interviews completed separately with the child and mother. Primary diagnoses and comorbid diagnoses are reported in Table 1. Based on results of clinical interviews conducted with the mother and child (separately), 7.6% of children met criteria for current MDD (n = 8), and an additional 3.8% met criteria for past MDD (n = 4).
TABLE 1.
Primary and secondary diagnoses of children (N = 105)
| Primary diagnosis | Percentage | Secondary diagnosis | Percentage |
|---|---|---|---|
| Generalized anxiety disorder | 46.7% | No secondary diagnosis | 30.5% |
| Social anxiety disorder | 27.6% | Specific phobia | 14.3% |
| Specific phobia disorder | 16.2% | Attention-deficit/hyperactivity disorder | 12.4% |
| Separation anxiety disorder | 7.6% | Generalized anxiety disorder | 8.6% |
| Other anxiety disorder | 1.9% | Oppositional defiant disorder | 7.6% |
| Major depressive disorder, current | 7.6% | ||
| Social anxiety disorder | 5.7% | ||
| Separation anxiety disorder | 5.7% | ||
| Major depressive disorder, past | 3.8% | ||
| Obsessive compulsive disorder | 1.0% | ||
| Panic disorder | 1.0% | ||
| Tourette's | 1.0% | ||
| Other anxiety disorder | 1.0% |
2.2 ∣. Procedure
Participants were recruited through local advertisements, child-oriented events, and informational flyers placed in the community in the metropolitan area of Houston, TX. To ensure that enough participants with clinical levels of anxiety were recruited, recruitment materials specifically encouraged participation of families whose children were suffering from anxiety. Mothers who contacted the research staff were given information about the study and subsequently screened according to inclusion and exclusion criteria. Eligible mothers were invited to the first study session. Upon arriving to the laboratory, trained research staff completed the consent process with mother–child dyads. Mothers who provided consent, and whose children provided written assent, continued to participate in the study.
Cognitive and academic functioning were assessed through administration of two subtests of the WISC-IV (Block Design and Vocabulary subtests; Wechsler, 2003) and two subtests of the WIAT-III (Reading Comprehension and Oral Reading Fluency subtests; Wechsler, 2009). After eligibility was confirmed, clinical interviews were conducted with mothers and children (separately) by graduate clinicians under the supervision of a doctoral-level board-certified clinical psychologist. Interviews were conducted in a private room to ensure confidentiality. Mothers completed questionnaires while their child was being interviewed (and vice versa).
Within 2 weeks of the first session, mothers and children who met eligibility criteria were invited to return for a second assessment session. During this visit, the child completed a computerized assessment of interpretation biases (see Section 2.3). Mothers were randomized to either (a) the “positive training” condition, in which they underwent a computer-based interpretation bias training that provided feedback to correct the mother's negative interpretation biases; or (b) a “neutral training” condition through which mothers received no feedback on their interpretation biases. Subsequently, an experimenter conducted a baseline RSA assessment with the child, during which the child was asked to sit still for five minutes with their eyes open, consistent with past work (El-Sheikh, Erath, & Bagley, 2013; Viana et al., 2017, 2019). After completing the baseline RSA assessment, children were instructed to prepare for an anxiety-provoking speech task (i.e., a speech about the child's family in front of a recording video camera) by spending five minutes discussing with their mother how they would approach the task (e.g., what to say, how to present the information). The experimenter provided the family with the opportunity to ask questions before leaving the room for 5 min. Mothers and children were videotaped during the speech preparation task for observational assessment of maternal behaviors (see Section 2). Subsequently, the mother was asked to leave the room, and the child was instructed to deliver a speech about their family in front of a recording video camera. Prior to beginning the speech, the child was told that it would later be rated for quality. The child delivered a speech for up to five minutes, during which their psychophysiological response (RSA) was also recorded.
Upon completion of the study, mother–child dyads were fully debriefed. Dyads were provided information about the results of their diagnostic assessments, recommendations for evidence-based treatments, and contact information for local mental health providers. Each dyad was compensated $50 per session. Children also received a toy at the end of each session. All study procedures were approved by the Institutional Review Board of the University of Houston.
2.3 ∣. Measures
MINI International Neuropsychiatric Interview for Children and Adolescents (MINI-KID; Sheehan et al., 2010).
The MINI-KID was used to ascertain whether children had a primary anxiety disorder, in order to determine eligibility for the study. The MINI-KID is a structured diagnostic interview that assesses the presence of DSM-5 psychiatric disorders in children and adolescents aged 6-to-17 years old. The MINI-KID is organized around diagnostic modules, each of which assesses one of the 24 most common DSM-5 diagnoses. The administrator asks two to four brief screening questions, and only proceeds with additional symptom questions within each module if the screen questions are endorsed. The MINI-KID has demonstrated high reliability and validity for children and adolescents (Sheehan et al., 2010).
In the present study, the MINI-KID parent and child versions were used. The parent version was used with the mother, who reported on her child's symptoms, and the child version was used with the child, who reported on their own symptoms. Mother and child interviews were conducted separately, in adjacent rooms. MINI-KID interviews were conducted by either a board-certified and licensed clinical child and adolescent psychologist, or an advanced graduate student under supervision. Graduate student assessors were trained to use the MINI-KID by observing videotaped samples of interviews conducted by the principal investigator; assessors were required to meet perfect interrater reliability with the PI on three interviews before conducting two independent interviews while being shadowed by the PI (i.e., live supervision). All MINI-KID interviews were videotaped and all diagnoses made were reviewed during supervision sessions with assessors. Fifteen percent of videotaped interviews were reviewed for interrater reliability; as in past work using fully structured interview formats (Duncan et al., 2018; Zvolensky et al., 2019), no instances of diagnostic disagreement were found.
The child's final primary diagnosis was based on the clinical interview with the mother; if the mother did not report a primary diagnosis, but the child did, then the child's final primary diagnosis was the self-reported diagnosis. Diagnostic agreement regarding the presence of a primary anxiety disorder across both mother and child interviews was observed for 48.6% of children; the remaining children received a primary anxiety disorder diagnosis based solely on the clinical interview with the mother (40.0%) or the child (11.4%).
Children's Negative Cognitive Error Questionnaire (CNCEQ; Leitenberg, Yost, & Carroll-Wilson, 1986).
The CNCEQ is a self-report questionnaire designed to assess interpretation biases. Children are instructed to imagine 24 hypothetical scenarios (e.g., “You invite one of your friends to stay overnight at your house. Another one of your friends finds out about it.”) followed by a negative interpretation of the event (e.g., “You think ‘he/she will be real mad at me for not asking them and never want to be friends again’”). For each item, the child indicates the degree to which they would endorse the negative interpretation on a 5-point Likert scale (1 = Not at all like I would think, 5 = Almost exactly like I would think). The CNCEQ has good test–retest reliability and internal consistency in children (Leitenberg et al., 1986). The CNCEQ total score (α = 0.93) was used as a self-report measure of interpretation biases (a predictor variable).
Word Sentence Association Paradigm (WSAP; Beard & Amir, 2009).
Although the CNCEQ is widely used, this “offline” method of assessing children's interpretation biases is susceptible to demand effects and response biases (Hirsch, Meeten, Krahé, & Reeder, 2016). To circumvent this possibility, children also completed a modified version of the WSAP, a behaviorally indexed measure that assesses children's interpretation biases in “real time” as they encounter ambiguity (Gonsalves, Whittles, Weisberg, & Beard, 2019). The task was programmed using DirectRT version 2012 (Jarvis, 2012) and displayed on a 17-inch wide-screen laptop computer screen. To enhance external validity, computerized scenarios were representative of day-to-day situations faced by children. The modified task consisted of 20 trials. For each trial, a fixation cross appeared in the center of the computer screen for 500 milliseconds. Next, an ambiguous sentence (e.g., “Your friend yawns during a conversation with you”) appeared along with two words that represent either a threatening (e.g., “boring”) or benign (e.g., “tired”) interpretation of the sentence. Children were instructed to choose which of the two words best fit with the sentence by pressing the corresponding computer key as quickly and accurately as possible. The stimuli remained on the computer screen until the child responded, upon which the next trial began immediately. Children performed the computerized task individually in a quiet and well-lit room. They sat on a height-adjustable chair, with their heads approximately 60 cm from the center of the screen. The proportion of threatening (vs. benign) interpretations made by participants was used as a performance-based index of interpretation biases (a predictor variable).
Revised Child Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000).
The RCADS assesses the severity of symptoms of major depressive disorder, separation anxiety disorder, social phobia, obsessive-compulsive disorder, panic disorder, and generalized anxiety disorder in children. The self-report form for children contains 47 items that are answered on a 4-point Likert scale (0 = Never, 3 = Always). The RCADS yields a total depression score, total anxiety score, and six anxiety subscale scores corresponding to the anxiety disorder subtypes listed above. The RCADS has demonstrated high internal consistency in both clinical and community samples of children and convergent validity with established measures of anxiety and depression (Chorpita, Moffitt, & Gray, 2005). For the present study, the child-reported total depression subscale score, converted to T-scores (“RCADS-D”; α = 0.84), was used as an index of child depressive disorder symptom severity (the outcome variable).
Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al., 1997).
The SCARED is an instrument designed to assess the severity of panic/somatic symptoms, generalized anxiety, separation anxiety, social phobia, and school phobia. The self-report form for children contains 41 items that are answered on a 3-point Likert scale (0 = Not true, 1 = Somewhat true, 2 = Very true). The SCARED yields a total anxiety score and five subscale scores corresponding to the anxiety subtypes listed above. The SCARED has high internal consistency and test-retest reliability in both clinical and community samples of children, and has good convergent validity with other measures of anxiety (Birmaher et al., 1997, 1999). In addition, the SCARED has strong discriminant validity and there is evidence that it taps depression less than do other anxiety measures (Birmaher et al., 1997, 1999; Silverman & Ollendick, 2005). For the present study, the total anxiety score (α = 0.93) was used as a covariate in all moderation analyses to control for anxiety severity.
2.4 ∣. RSA assessment
Electrocardiogram (ECG) data were collected (a) during a 5-min resting period (upon arrival to the second study session) while children sat still, and (b) during the speech task (final portion of this 1-hr session) according to guidelines established by the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (Camm et al., 1996). Three standard AG-AgCl disposable electrodes in a three-point configuration and a wired ECG transmitter and receiver from BIOPAC were used. ECG data were collected through a BIOPAC MP150 system and recorded online with AcqKnowledge 4.2 with a sampling rate of 1,000 samples/s. To derive RSA indices, respiratory effort was controlled by measuring changes in thoracic circumference using a respiration transducer.
ECG data were processed offline and artifacts and ectopic beats were identified and corrected using Mindware Heart Variability 3.2.1 software (Mindware Technologies). RSA was calculated using the well-validated peak-to-valley method (Lewis, Furman, McCool, & Porges, 2012) by calculating the difference between the maximum heart rate interbeat interval and the minimum interbeat interval during each respiration cycle. Mean baseline RSA was the average of the RSA values for each 30-s epoch across the 5-min baseline. Mean speech RSA was the average of the RSA values for each 30-s epoch during the speech (average speech duration = 2.3 min). RSA suppression was calculated by subtracting mean RSA values during the speech from the mean RSA values during the baseline period (Shanahan, Calkins, Keane, Kelleher, & Suffness, 2014). Thus, larger positive RSA suppression scores reflect a greater decrease in RSA from baseline to speech task.
2.5 ∣. Observational assessment of maternal behaviors
Maternal behaviors during the 5-min speech preparation task were coded by trained observers to account for the potential effects of maternal behaviors on children's RSA suppression. Following procedures outlined in Ginsburg and Grover’s (2014) Coding Manual for Parent–Child Interactions, 11 maternal behaviors were coded by two independent observers on a 5-point Likert scale (0 = Never, A = Most of the time) for each 1-min epoch across the 5-min period and for the 5-min period overall: overcontrol (κ = 0.88), granting of autonomy (κ = 0.89), hostility/negative affect (κ = 0.95), warmth/positive affect (κ = 0.82), unresponsive/uninvolved behavior (κ = 0.96), anxious behavior (κ = 0.91), self-blame/self-criticism (κ = 1.00), criticism/blaming of the child (κ = 1.00), doubts concerning child competency (κ = 1.00), problem-solving (κ = 0.91), and efficacy (κ = 1.00). The overall rating for each of the 11 maternal behaviors was used. Undergraduate and graduate research assistants received 15–20 hr of training by the second author in order to code maternal behaviors. Coders were required to achieve adequate interrater reliability (κ > 0.80) with a master coder (second author) prior to coding independently. Per manual instructions, rater discrepancies greater than one unit were resolved through discussion (Ginsburg & Grover, 2014).
2.6 ∣. Data analyses
First, the distributions of variables of interest (CNCEQ, WSAP, RSA suppression, RCADS-D, SCARED) were examined for skewness, kurtosis, and potential outliers. Bivariate correlational analyses were used to examine associations between variables of interest and identify any relevant covariates. Next, ANOVAs were conducted to examine whether there were main or interactive effects of child gender and race on study variables. Next, two separate multiple regression analyses were conducted to examine RSA suppression as a potential moderator of the associations between child interpretation biases (predictor variables; CNCEQ and WSAP, respectively) and child depressive symptom severity (outcome variable; RCADS-D). The PROCESS macro on SPSS (Hayes, 2018) was used to conduct regression analyses with bias-corrected confidence intervals and 95% bootstrapping of 10,000 resamples, as well as conduct tests of simple slopes at ±1 SD the mean level of the moderator. Given associations of interpretation biases to broader internalizing symptoms (Hinnant & El-Sheikh, 2009; Wilson & Rapee, 2005), anxiety symptom severity (SCARED) was entered as a covariate in all models. As recommended (Graziano & Derefinko, 2013), baseline RSA was also entered as a covariate in all models. Interactions were also examined graphically, as recommended by Cohen and Cohen (1983), and statistically, as recommended by Holmbeck (2002), by examining the 95% bootstrapped confidence intervals for the effect of interpretation biases on depressive disorder symptom severity at each level of the moderator. Finally, exploratory moderator analyses were conducted separately among boys and girls. These exploratory analyses were identical to the moderation analyses described earlier for the total sample.
3 ∣. RESULTS
3.1 ∣. Preliminary analyses
Data were first examined for outliners, linearity, and normality. A case was considered an outlier if it deviated more than 3.29 SD from the sample mean (Tabachnick & Fidell, 2013). One outlier was identified for a high RCADS-D score; this score was corrected to one unit larger than the most extreme score in the distribution (Tabachnick & Fidell, 2013). All study variables demonstrated acceptable levels of skewness and kurtosis (i.e., within range of ±2.0). Means, standard deviations, and ranges of study variables are presented in Table 2. Mean levels of anxiety (SCARED) were consistent with those reported in past studies using these measures in clinical samples of children and adolescents with anxiety disorders (Albano et al., 2018); mean levels of depression (RCADS-D; M = 48.23, SD = 12.51) were lower than those reported in past studies (e.g., M = 54.68 in Southam-Gerow, Chorpita, Miller, & Gleacher, 2008). A total of nine children (9% of the sample) exceeded the clinical threshold for depression on the RCADS-D (i.e., T-score > 65; Chorpita et al., 2000).
TABLE 2.
Descriptive statistics and bivariate correlations among study variables (N = 105)
| Variable | M (SD) | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age (years) | 10.07 (1.22) | 8–12 | — | |||||||||||
| 2. Gender | 57% female | 1, 2 | 0.13 | — | ||||||||||
| 3. Interpretation biases (self-reported; CNCEQ) | 48.45 (18.05) | 24–102 | 0.16 | 0.16 | — | |||||||||
| 4. Interpretation biases (behaviorally-indexed; WSAP) | 0.27 (0.15) | 0–0.70 | 0.02 | 0.15 | 0.51** | — | ||||||||
| 5. Baseline RSA | 6.56 (1.21) | 1.52–9.36 | 0.01 | −0.02 | −0.05 | −0.04 | — | |||||||
| 6. RSA suppression | 1.33 (1.00) | −1.79 to 3.62 | 0.09 | −0.04 | −0.04 | −0.05 | 0.45** | — | ||||||
| 7. Depression (RCADS-D) | 48.23 (12.51) | 31.03–84.41 | −0.08 | 0.12 | 0.60** | 0.37** | −0.02 | 0.02 | — | |||||
| 8. Anxiety (SCARED) | 25.37 (14.14) | 3–70 | −0.04 | 0.15 | 0.65** | 0.39** | 0.04 | 0.08 | 0.62** | — | ||||
| 9. Speech length (min) | 2.26 (1.21) | 0–5 | 0.13 | 0.08 | 0.05 | 0.09 | −0.07 | −0.07 | 0.09 | −0.003 | — | |||
| 10. Speech word count | 249.54 (177.09) | 0–849 | 0.09 | 0.07 | 0.06 | 0.05 | −0.02 | −0.06 | 0.02 | 0.09 | 0.84** | — | ||
| 11. Parent training condition | 51% Neutral | 1, 2 | −0.05 | 0.03 | 0.14 | −0.01 | −0.13 | −0.17 | 0.09 | 0.07 | 0.01 | 0.001 | — | |
| 12. Maternal autonomy granting | 2.26 (0.96) | 0–4 | 0.02 | 0.03 | 0.21* | 0.06 | 0.16 | 0.10 | 0.10 | 0.01 | −0.15 | −0.20* | −0.12 | — |
| 13. Maternal negative affect | 0.59 (0.74) | 0–3 | −0.04 | −0.01 | −0.08 | 0.07 | −0.10 | −0.20* | −0.12 | −0.15 | −0.03 | 0.06 | 0.05 | −0.32** |
Note: Gender 1 = male, 2 = female; CNCEQ = Children's Negative Cognitive Error Questionnaire; WSAP = Word Sentence Association Paradigm, proportion of threatening (vs. benign) interpretations; Baseline RSA = Average respiratory sinus arrhythmia at baseline; RSA suppression = Baseline RSA minus average RSA during speech task; RCADS-D = Revised Children's Anxiety and Depression Scale, depression score; SCARED = Screen for Child Anxiety Related Emotional Disorders, total score; Speech length = Length of child's speech in minutes (Note: RSA data were collected for at least 30 s regardless of speech length); Speech word count = Number of words spoken by child during speech task. Parent training condition 1 = “neutral training” condition, 2 = “positive training” condition. Maternal autonomy granting, Maternal negative affect = Maternal behaviors coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions.
p < .05;
p < .01.
Bivariate correlations between variables are presented in Table 2. There were no associations between age and any of the main study variables. No gender or race differences were found on mean scores for any of the study variables (all ANOVA ps > .09), indicating comparable mean levels of interpretation biases, baseline RSA, RSA suppression, anxiety, and depression between girls and boys and between children of different races. As such, demographic variables were not included as covariates. With regards to maternal behaviors during the mother–child speech preparation task, maternal autonomy granting correlated positively with child self-reported interpretation biases, and maternal negative affect correlated negatively with child RSA suppression. As such, these two maternal behaviors were included as covariates. None of the other maternal behaviors were significantly associated with the key study variables, and thus were not included as covariates.2 Children's speech length (in minutes), speech amount (number of words spoken), or parental condition (interpretation bias modification training or control) did not correlate significantly with any of the variables of interest and were therefore not included as covariates.
Self-reported interpretation biases (CNCEQ) and behaviorally indexed interpretation biases (WSAP) were positively correlated. Greater self-reported interpretation biases were associated with more severe depression and anxiety scores, as were greater behaviorally indexed interpretation biases. Lower baseline RSA was associated with smaller RSA suppression. Neither baseline RSA nor RSA suppression correlated with any other key study variables.
3.2 ∣. Moderation analyses
3.2.1 ∣. Interactions between RSA suppression and self-reported interpretation biases
Statistics for the regression analyses examining the interactions between self-reported interpretation biases and RSA suppression predicting child depression severity are presented in Table 3. The full model was significant and accounted for 48% of the variance in depressive symptoms (F [7, 97] = 12.95, p < .0001). The interaction of self-reported interpretation biases and RSA suppression accounted for 3% of the variance (B = −0.13, SE = 0.06, t = −2.18; F [1, 97] = 4.75, p = .032, 95% CI [−0.26, −0.01]). Visual inspection of the interaction plot indicated that the highest levels of depression were found in children with high levels of interpretation biases and low RSA suppression (Figure 1). Statistical examination of the simple slopes revealed that the association between self-reported interpretation biases and depressive symptoms was significant among children with low (B = 0.35, SE = 0.09, t = 3.92, p = .0002, 95% CI [0.17, 0.53]) and average levels of RSA suppression (B = 0.22, SE = 0.07, t = 3.05, p = .003, 95% CI [0.08, 0.36]), but not among children with high levels of RSA suppression (B = 0.08, SE = 0.10, t = 0.84, p = .405, 95% CI [−0.11, 0.28]). The Johnson-Neyman technique revealed that for RSA suppression below 1.78 ms (68.6% of children), the association between interpretation biases and depression symptom severity was significantly positive.
TABLE 3.
Summary of regression analyses testing the interaction of self-reported interpretation biases and RSA suppression predicting child depressive disorder symptom severity (N = 105)
| Depressive disorder symptom severity |
||||
|---|---|---|---|---|
| Variable | B | SE | t | 95% CI |
| RSA suppression | 6.04* | 2.95 | 2.05 | [0.19, 11.88] |
| Interpretation biases (CNCEQ) | 0.39*** | 0.10 | 3.83 | [0.19, 0.60] |
| Interpretation biases (CNCEQ) × RSA suppression | −0.13* | 0.06 | −2.18 | [−0.26, −0.01] |
| Baseline RSA | 0.20 | 0.88 | 0.23 | [−1.54, 1.94] |
| Anxiety | 0.34*** | 0.09 | 3.79 | [0.16, 0.52] |
| Maternal autonomy granting | −0.30 | 1.09 | −0.27 | [−2.47, 1.88] |
| Maternal negative affect | −0.36 | 1.34 | −0.27 | [−3.02, 2.30] |
| R 2 | .48*** | |||
| F | 12.95*** | |||
| ΔR2 due to interaction | .03* | |||
Note: Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; RSA suppression = Respiratory sinus arrhythmia (RSA) during baseline minus RSA during speech task; CNCEQ = Children's Negative Cognitive Error Questionnaire; Anxiety = Screen for Child Anxiety Related Emotional Disorders (SCARED), total score. Maternal autonomy granting, Maternal negative affect = Maternal behaviors coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions.
p < .05;
p < .001.
FIGURE 1.
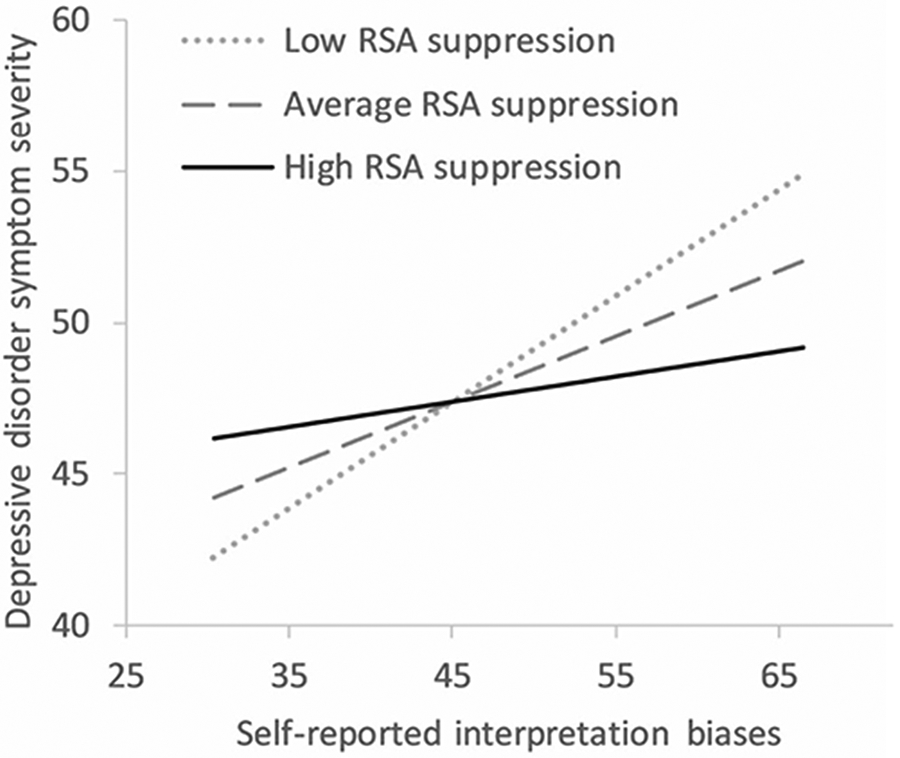
Predicted levels of child depressive disorder symptom severity as a result of the interactive effect of self-reported interpretation biases and RSA suppression (controlling for anxiety, baseline RSA, maternal autonomy granting, and maternal negative affect; N = 105). Note. Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; Self-reported child interpretation biases = Child Negative Cognitive Errors Questionnaire (CNCEQ); RSA suppression = Mean RSA at baseline – mean RSA during challenge speech task. Baseline RSA, anxiety severity (Screen for Child Anxiety Related Emotional Disorders), maternal autonomy granting, and maternal negative affect coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions were included as covariates
3.2.2 ∣. Interactions between RSA suppression and behaviorally indexed interpretation biases
Statistics for the regression analyses examining the interactions between behaviorally indexed interpretation biases and RSA suppression predicting child depression severity are presented in Table 4. The full model was significant and accounted for 45% of the variance in depressive symptoms (F [7, 97] = 11.26, p < .0001). The interaction of behaviorally indexed interpretation biases and RSA suppression accounted for 3% of the variance (B = −18.87, SE = 7.96, t = −2.37; F [1, 97] = 5.61, p = .020, 95% CI [−34.67, −3.06]). Visual inspection of the interaction plot indicated that the highest levels of depression were found in children with high levels of interpretation biases and low RSA suppression (Figure 2). Statistical examination of the simple slopes revealed that interpretation biases and depressive symptom severity were positively related among children with low RSA suppression (B = 31.89, SE = 11.06, t = 2.88, p = .005, 95% CI [9.93, 53.85]), were marginally positive among children with average levels of RSA suppression (B = 12.94, SE = 6.87, t = 1.88, p = .063, 95% CI [−0.70, 26.58]), and were not significantly related among children with high levels of RSA suppression (B = −6.01, SE = 10.00, t = −0.60, p = .549, 95% CI [−25.85, 13.83]). The Johnson-Neyman technique revealed that for RSA suppression below 1.29 ms (51.43% of children), the association between interpretation biases and depression symptom severity was significantly positive.3
TABLE 4.
Summary of regression analyses testing the interaction of behaviorally indexed interpretation biases and RSA suppression predicting child depressive disorder symptom severity (N = 105)
| Depressive disorder symptom severity |
||||
|---|---|---|---|---|
| Variable | B | SE | t | 95% CI |
| RSA suppression | 4.53* | 2.25 | 2.01 | [0.06, 8.99] |
| Interpretation biases (WSAP) | 38.00** | 13.19 | 2.88 | [11.82, 64.17] |
| Interpretation biases (WSAP) × RSA suppression | −18.87* | 7.96 | −2.37 | [−34.67, −3.06] |
| Baseline RSA | −0.38 | 0.89 | −0.43 | [−2.14, 1.38] |
| Anxiety | 0.49*** | 0.07 | 6.57 | [0.34, 0.64] |
| Maternal autonomy granting | 0.96 | 1.06 | 0.91 | [−1.14, 3.06] |
| Maternal negative affect | −0.24 | 1.39 | −0.17 | [−3.01, 2.52] |
| R 2 | .45*** | |||
| F | 11.26*** | |||
| ΔR2 due to interaction | .03* | |||
Note: Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; RSA suppression = Respiratory sinus arrhythmia (RSA) during baseline minus RSA during speech task; WSAP = Word Sentence Association Paradigm, proportion of threatening (versus, benign) interpretations; Anxiety = Screen for Child Anxiety Related Emotional Disorders (SCARED), total score. Maternal autonomy granting, Maternal negative affect = Maternal behaviors coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions.
p < .05;
p < .01;
p < .001.
FIGURE 2.
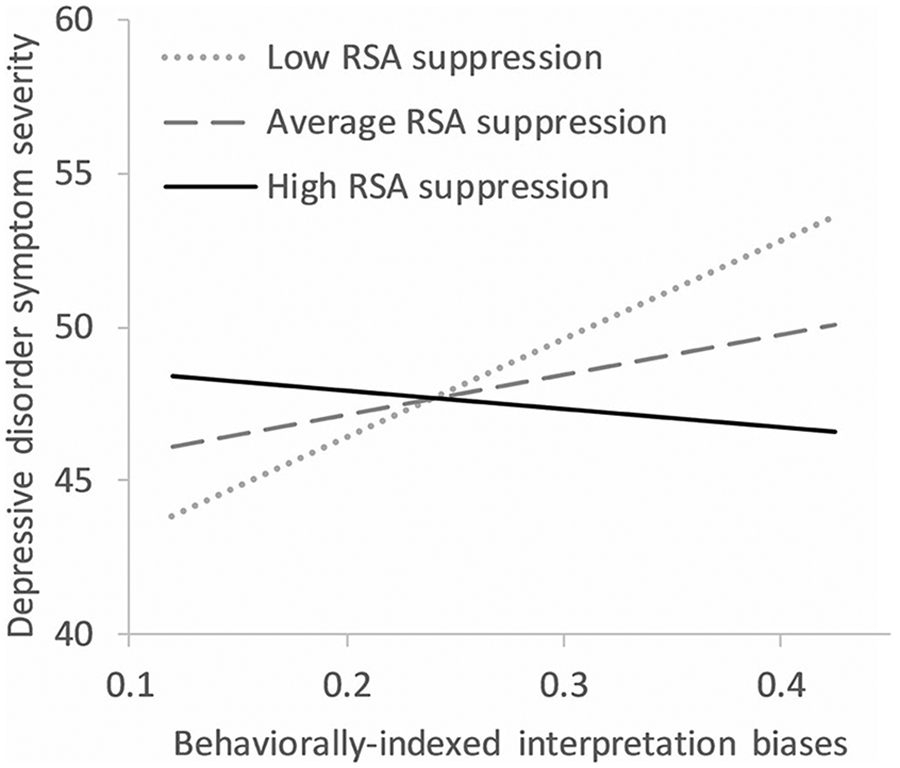
Predicted levels of child depressive disorder symptom severity as a result of the interactive effect of behaviorally indexed interpretation biases and RSA suppression (controlling for anxiety, baseline RSA, maternal autonomy granting, and maternal negative affect; N = 105). Note. Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; Behaviorally indexed interpretation biases = Word Sentence Association Paradigm (WSAP), proportion of threatening (vs. benign) interpretations; RSA Suppression = Mean RSA at baseline – mean RSA during challenge speech task. Baseline RSA, anxiety severity (Screen for Child Anxiety Related Emotional Disorders), maternal autonomy granting, and maternal negative affect coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions were included as covariates
3.2.3 ∣. Exploratory tests of gender differences in interactions between RSA suppression and self-reported interpretation biases
A summary of exploratory regression analyses testing the interaction of RSA suppression and self-reported interpretation biases predicting depressive symptom severity, stratified by gender, is presented in Table 5. Among girls, the full model was significant and accounted for 51% of the variance in depressive symptoms (F [7, 52] = 7.69, p < .0001). The interaction between self-reported interpretation biases and RSA suppression was marginally significant (B = −0.15, SE = 0.08, t = −1.87, 95% CI [−0.32, 0.01]; ΔR2 due to interaction = 0.03, F [1, 52] = 3.50, p = .067, Figure 3a). The highest levels of depression were found in girls with high levels of interpretation biases and low RSA suppression (Figure 3a). Specifically, the association between self-reported interpretation biases and depressive symptoms was significant among girls with low (B = 0.43, SE = 0.14, t = 3.19, p = .002, 95% CI [0.16, 0.70]) and average levels of RSA suppression (B = 0.27, SE = 0.10, t = 2.61, p = .012, 95% CI [0.06, 0.48]), but not among girls with high levels of RSA suppression (B = 0.11, SE = 0.13, t = 0.83, p = .413, 95% CI [−0.16, 0.38]). The Johnson-Neyman technique revealed that for RSA suppression below 1.65 ms (60.0% of girls), the association between interpretation biases and depression symptom severity was significantly positive.
TABLE 5.
Summary of exploratory regression analyses testing the interaction of self-reported interpretation biases and RSA suppression predicting child depressive disorder symptom severity, ran separately by gender
| Depressive disorder symptom severity |
||||||||
|---|---|---|---|---|---|---|---|---|
| Girls (n = 60) |
Boys (n = 45) |
|||||||
| Variable | B | SE | t | 95% CI | B | SE | t | 95% CI |
| RSA suppression | 7.98+ | 4.28 | 1.86 | [−0.61, 16.57] | 0.93 | 4.83 | 0.19 | [−8.85, 10.71] |
| Interpretation biases (CNCEQ) | 0.47** | 0.15 | 3.15 | [0.17, 0.77] | 0.28+ | 0.15 | 1.89 | [−0.02, 0.58] |
| Interpretation biases (CNCEQ) × RSA suppression | −0.15+ | 0.08 | −1.87 | [−0.32, 0.01] | −0.03 | 0.12 | −0.24 | [−0.27, 0.21] |
| Baseline RSA | −1.39 | 1.33 | −1.04 | [−4.07, 1.29] | 1.80 | 1.11 | 1.62 | [−0.45, 4.06] |
| Anxiety | 0.26+ | 0.13 | 1.99 | [−0.003, 0.52] | 0.40** | 0.12 | 3.20 | [0.15, 0.65] |
| Maternal autonomy granting | −1.30 | 1.63 | −0.81 | [−4.56, 1.96] | −0.03 | 1.41 | −0.02 | [−2.89, 2.83] |
| Maternal negative affect | −2.94 | 2.12 | −1.39 | [−7.19, 1.31] | 2.10 | 1.62 | 1.30 | [−1.18, 5.37] |
| R 2 | .51*** | .55*** | ||||||
| F | 7.69*** | 6.45*** | ||||||
| ΔR2 due to interaction | 0.4+ | .001 | ||||||
Note: Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; RSA suppression = Respiratory sinus arrhythmia (RSA) during baseline minus RSA during speech task; CNCEQ = Children's Negative Cognitive Error Questionnaire; Anxiety = Screen for Child Anxiety Related Emotional Disorders (SCARED), total score. Maternal autonomy granting, Maternal negative affect = Maternal behaviors coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions.
p < .07;
p < .01;
p < .001.
FIGURE 3.
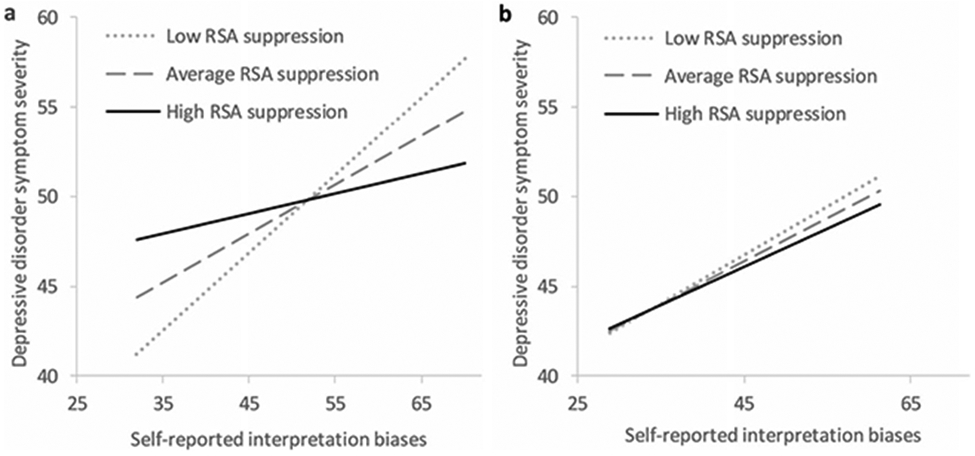
Predicted levels of child depressive disorder symptom severity as a result of the interactive effect of self-reported interpretation biases and RSA suppression (controlling for anxiety, baseline RSA, maternal autonomy granting, and maternal negative affect), (a) among girls (n = 60), and (b) among boys (n = 45). Note. Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; Self-reported child interpretation biases = Child Negative Cognitive Errors Questionnaire (CNCEQ); RSA suppression = Mean RSA at baseline – mean RSA during challenge speech task. Baseline RSA, anxiety severity (Screen for Child Anxiety Related Emotional Disorders), maternal autonomy granting, and maternal negative affect coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions were included as covariates
Among boys, the full model was also significant and accounted for 55% of the variance in depressive symptoms (F [7, 37] = 6.45, p = .0001; Table 5). The interaction between self-reported interpretation biases and RSA suppression was not significant (ΔR2 due to interaction = 0.001, F [1, 37] = 0.06, p = .811; Figure 3b). The main effect of RSA suppression was not significant (p = .811); however, the main effect of self-reported interpretation biases on boys’ depressive symptoms was marginally significant (p = .067).
3.2.4 ∣. Exploratory tests of gender differences in interactions between RSA suppression and behaviorally indexed interpretation biases
A summary of exploratory regression analyses testing the interaction of RSA suppression and behaviorally indexed interpretation biases predicting depressive symptom severity, stratified by gender, is presented in Table 6. Among girls, the full model was significant and accounted for 52% of the variance in depressive symptoms (F [7, 52] = 7.91, p < .0001). The interaction between behaviorally indexed interpretation biases and RSA suppression was significant (B = −26.79, SE = 10.35, t = −2.59, 95% CI [−47.55, −6.03]; ΔR2 due to interaction = .06, F [1, 52] = 6.71, p = .012; Figure 4a). The highest levels of depression were found in girls with high levels of interpretation biases and low RSA suppression (Figure 4a). Specifically, the association between behaviorally indexed interpretation biases and depressive symptoms was significant among girls with low (B = 50.82, SE = 15.23, t = 3.34, p = .002, 95% CI [20.25, 81.39]) and average levels of RSA suppression (B = 22.82, SE = 9.19, t = 2.48, p = .016, 95% CI [4.38, 41.26]), but not among girls with high levels of RSA suppression (B = −5.18, SE = 13.06, t = −0.40, p = .693, 95% CI [−31.39, 21.03]). The Johnson-Neyman technique revealed that for RSA suppression below 1.46 ms (58.3% of girls), the association between interpretation biases and depression symptom severity was significantly positive.
TABLE 6.
Summary of exploratory regression analyses testing the interaction of behaviorally-indexed interpretation biases and RSA suppression predicting child depressive disorder symptom severity, ran separately by gender
| Variable | Girls (n = 60) Depressive disorder symptom severity |
|||||||
|---|---|---|---|---|---|---|---|---|
| Girls (n = 60) |
Boys (n = 45) |
|||||||
| B | SE | t | 95% CI | B | SE | t | 95% CI | |
| RSA suppression | 7.98* | 3.30 | 2.42 | [1.35, 14.60] | −0.78 | 3.53 | −0.22 | [−7.94, 6.37] |
| Interpretation biases (WSAP) | 57.41** | 17.34 | 3.31 | [22.60, 92.21] | 2.44 | 23.58 | 0.10 | [−45.34, 50.22] |
| Interpretation biases (WSAP) × RSA suppression | −26.79* | 10.35 | −2.59 | [−47.55, −6.03] | 0.53 | 15.46 | 0.03 | [−30.79, 31.85] |
| Baseline RSA | −2.51+ | 1.32 | −1.89 | [−5.16, 0.15] | 1.12 | 1.23 | 0.91 | [−1.37, 3.62] |
| Anxiety | 0.43*** | 0.10 | 4.40 | [0.24, 0.63] | 0.57*** | 0.12 | 4.89 | [0.33, 0.80] |
| Maternal autonomy granting | 0.13 | 1.49 | 0.09 | [−2.85, 3.11] | 0.94 | 1.47 | 0.64 | [−2.03, 3.92] |
| Maternal negative affect | −2.16 | 2.13 | −1.01 | [−6.42, 2.11] | 2.32 | 1.85 | 1.25 | [−1.43, 6.07] |
| R2 | .52*** | .46** | ||||||
| F | 7.91*** | 4.51** | ||||||
| ΔR2 due to interaction | .06* | <.001 | ||||||
Note: Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; RSA suppression = Respiratory sinus arrhythmia (RSA) during baseline minus RSA during speech task; WSAP = Word Sentence Association Paradigm, proportion of threatening (versus, benign) interpretations; Anxiety = Screen for Child Anxiety Related Emotional Disorders (SCARED), total score. Maternal autonomy granting, Maternal negative affect = Maternal behaviors coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions.
p < .07;
p < .05;
p < .01;
p < .001.
FIGURE 4.
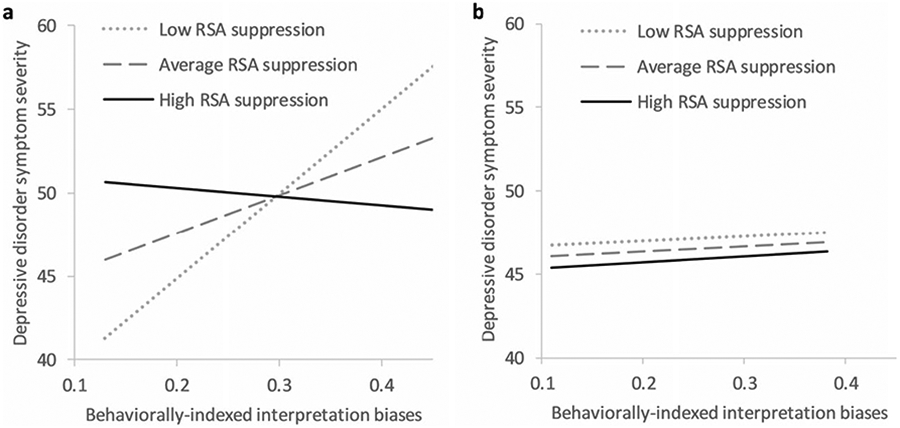
Predicted levels of child depressive disorder symptom severity as a result of the interactive effect of behaviorally-indexed interpretation biases and RSA suppression (controlling for anxiety, baseline RSA, maternal autonomy granting, and maternal negative affect), (a) among girls (n = 60), and (b) among boys (n = 45). Note. Depressive disorder symptom severity = Revised Child Anxiety and Depression Scale (RCADS), depression score; Behaviorally-indexed interpretation biases = Word Sentence Association Paradigm (WSAP), proportion of threatening (vs. benign) interpretations; RSA suppression = Mean RSA at baseline – mean RSA during challenge speech task. Baseline RSA, anxiety severity (Screen for Child Anxiety Related Emotional Disorders), maternal autonomy granting, and maternal negative affect coded during the parent–child speech preparation task using Ginsburg and Grover’s (2014) Coding Manual for Parent-Child Interactions were included as covariates
Among boys, the full model was also significant and accounted for 46% of the variance in depressive symptoms (F [7, 37] = 4.51, p = .001; Table 6). The interaction between behaviorally indexed interpretation biases and RSA suppression was not significant (ΔR2 due to interaction < .001, F [1, 37] = 0.001, p = .973; Figure 4b). The main effects of RSA suppression and behaviorally indexed interpretation biases were not significant (ps = .826 and .918 respectively).4
4 ∣. DISCUSSION
The present investigation examined RSA suppression as a moderator of the covariance between interpretation biases and depressive symptoms in a diverse group of clinically anxious children. Consistent with our first hypothesis, interpretation biases were associated with more severe anxiety and depressive symptoms. This finding is in line with past work identifying interpretation biases as a potent risk factor for anxiety (Taghavi et al., 2000), depression (Muris et al., 2000), and their co-occurrence (Alfano et al., 2009). In line with cognitive models of anxiety and depression (Beck & Clark, 1988; Kendall & Chansky, 1991), a cognitive bias toward threatening or negative interpretations of ambiguous information influences children's emotional (i.e., fear, sadness) and behavioral (i.e., avoidance, withdrawal) responses that may trigger and/or maintain internalizing symptoms. Notably, the current study replicates findings by utilizing a multimethod approach to the assessment of interpretation biases (i.e., self-reports and behavioral assessments) in a diverse sample of clinically anxious children.
Our second hypothesis—that RSA suppression would moderate the association between interpretation biases and depressive symptoms—was supported in the total sample, and partially supported in the subsample of girls. Specifically, in the subsample of girls, the moderation model examining behaviorally indexed interpretation biases as the predictor was statistically significant, yet the moderation model examining self-reported interpretation biases as the predictor was only marginally significant. In both models, girls with low (vs. high) RSA suppression in response to the stressor exhibited a stronger, positive association between interpretation biases and depressive symptoms. It is possible that when girls with a cognitive predisposition for internalizing problems (i.e., high levels of interpretation biases) face a stressor, restricted patterns of physiological regulation further compromise their ability to engage in adaptive forms of coping (Joormann & Vanderlind, 2014). Such repeated failures may lead to feelings of incompetence and worthlessness, which, over time, can contribute to the development of depression (Lumley & Harkness, 2007). On the other hand, girls with more adaptive patterns of physiological responding may be better equipped to handle stressors in a manner that promotes feelings of competency, even if they have cognitive predispositions that put them at risk for internalizing problems. In line with this reasoning, a recent longitudinal study found that adolescent girls with attentional control deficits (i.e., a cognitive inability to shift attention) self-reported increased stress reactivity (which included self-reported physiological arousal), which in turn, led to increased depressive symptoms over time—a pathway which was not found among boys (Rudolph, Monti, & Flynn, 2018).
Among boys, RSA suppression did not significantly moderate the association between interpretation biases and depressive symptoms. Given the gender-stratified analyses were underpowered, the intended conclusion is not that RSA suppression does not play a role among boys in terms of the modeled associations, but rather that RSA suppression might play a stronger role in girls. In fact, that a moderation effect was found among girls despite an underpowered analysis suggests that RSA suppression is likely particularly important among girls.
The findings further underscore the complexities involved in the assessment and interpretation of RSA suppression. For instance, the simple slopes analyses (Figures 1 and 2) suggest that in the context of low interpretation biases, greater RSA suppression is associated with more severe depressive symptoms. Thus, it appears that the most adaptive response is not to suppress RSA in all contexts, but rather, to be able to suppress RSA only when needed (i.e., in the context of high interpretation biases). Relatedly, recent findings suggest that dynamic methods of assessing RSA, as it unfolds continuously on a moment-to-moment basis, may better capture its association to socioemotional health than static methods such as those used in the present investigation (Burt & Obradović, 2013). Dynamic analyses of RSA functioning and its variations (e.g., patterns of suppression and recovery; Miller, Nuselovici, & Hastings, 2016) may thus result in a different pattern of findings.
Although not the focus of the present investigation, it is worth noting that age did not correlate with depressive symptoms. This is somewhat surprising, given past findings of a positive association between child age and depressive symptoms (Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015). However, the sample was comprised of relatively young children with a somewhat narrow age range (8–12 years), which may partially explain the lack of significance. Likewise, mean depression symptoms in the present sample were lower than in other clinical samples (Southam-Gerow et al., 2008), thus limiting the variability of depression scores and potentially dampening the correlations.
There are several clinical implications from these findings. Anxiety-disordered children with comorbid depressive symptoms have less favorable responses to treatment (Berman, Weems, Silverman, & Kurtines, 2000). As such, improving our understanding of the cognitive-affective mechanisms linking anxiety and depression among children can help identify optimal treatment targets (Garber & Weersing, 2010). First, the current findings support transdiagnostic interventions—such as the Unified Protocol (Barlow, Allen, & Choate, 2004)—that target shared risk factors, such as cognitive biases and emotion dysregulation (Ehrenreich, Goldstein, Wright, & Barlow, 2009). While treatment outcomes for youth with anxiety disorders are affected by myriad factors, including anxiety severity, parental psychopathology, and demographic variables (Wergeland et al., 2016), comorbid depressive symptoms are one of many treatment targets that may benefit youth (O’Neil & Kendall, 2012; Rapee et al., 2013). Additionally, the present findings highlight RSA as a potential intervention target for anxiety-disordered children—and perhaps girls especially—who have co-occurring depressive symptoms. Research suggests that RSA is likely a malleable construct (El-Sheikh & Erath, 2011). Recent clinical trials have found that in adult patients, RSA biofeedback training resulted in decreased state-anxiety and emotional stress (Mikosch et al., 2010). Behavioral interventions for children have also shown effects on RSA. For instance, Graziano, Bagner, Sheinkopf, Vohr, and Lester (2012) found that parent–child interaction therapy for prematurely-born and externalizing children resulted in improved baseline RSA and RSA suppression during a 5-min mother–child clean-up task. Moreover, increased maternal use of behaviors taught during treatment (e.g., praise, reflection, and behavioral descriptions) were associated with greater child RSA suppression post-treatment (Graziano et al., 2012). Although such findings indicate that these forms of behavioral intervention can improve RSA responses, their effects have yet to be examined among internalizing youth. As personalized approaches to psychological interventions develop, RSA may be a promising intervention target for girls with co-occurring anxiety and depressive symptoms, who do not respond to conventional psychosocial treatments. Future work on RSA-targeting interventions for youth is a necessary next step.
The findings from the present investigations must be interpreted in the context of limitations. First, the relatively small sample size precludes analyses pertaining to specific subtypes of anxiety disorders. Anxiety disorders are heterogenous in symptomatology, etiology, and prognoses. Recent research has found considerable differences in patterns of the anxiety–depression co-occurrence depending on the specific anxiety disorder (Beesdo et al., 2009). Likewise, effect sizes of the significant moderation results with the total sample were small, explaining only 3% of the variance in depression symptoms. Although the effects were consistent across self-reported and behavioral measures of interpretation biases, additional studies are clearly needed to replicate the current findings in larger samples that can bypass concerns about statistical power to detect such small moderation effects. Second, the cross-sectional nature of the study precludes drawing causal conclusions or examining developmental pathways. Research has found that anxiety most often precedes depression (Cummings et al., 2014), but bidirectional effects have also been reported (Olino, Klein, Lewinsohn, Rohde, & Seeley, 2010). Third, the current sample focused on late childhood. Not only is depression more common in adolescence, but also gender differences in the prevalence of depression become more pronounced during this developmental period (Cummings et al., 2014). Extending the model to a sample of adolescents and young adults could inform whether our findings generalize across developmental periods.
Another limitation is the observed variability in the amount and duration of child speech during the stressful speech task. While the speech task procedures were standardized, some children inevitably spoke longer than others did. However, we found no statistically significant correlations between speech length and speech amount and key study variables, including the RSA estimates. Thus, it seems unlikely that between-person variability in speech length and amount affected the results. Finally, it is possible that other factors not assessed in this study influenced our results. Notably, RSA is not the only physiological indicator that is relevant to youth psychopathology; other indices of stress reactivity such as galvanic skin response, hypothalamic-pituitary-axis (HPA) reactivity, and pre-ejection period may also be relevant (Beauchaine, 2001; El-Sheikh et al., 2009). Future research may benefit from measuring stress reactivity across multiple physiological systems (HPA, PNS, and SNS). Furthermore, given the literature on RSA and externalizing problems (e.g., Lunkenheimer et al., 2015), it is possible that boys had more externalizing problems, which may have influenced the findings. While we tested this possibility by controlling for ODD diagnoses (see Footnote 4), the absence of dimensional data on externalizing problems is a limitation. Finally, although we accounted for the effects of maternal autonomy granting and maternal negative affect in the moderation analyses, it is possible that other maternal behaviors not captured by our coding scheme may have influenced children's RSA suppression values.
The present investigation found that RSA suppression moderated the association between interpretation biases and co-occurring depressive symptoms among clinically anxious children. These findings suggest that low RSA suppression in response to stressors may specifically make children, and especially girls, more vulnerable to the influence of negative interpretation biases on depressive symptoms. On the other hand, children who demonstrate greater RSA suppression in response to stressors may be able to better regulate their arousal in stressful situations. Future work should examine whether transdiagnostic interventions targeting malleable indices of physiological arousal serve to weaken the association between interpretation biases and depressive symptoms in clinically anxious youth.
Supplementary Material
Funding information
This research was funded by grant R21-MH101309 (PI: Viana) from the National institute of Mental Health (NCT02095340). The views of this article are those of the authors and do not necessarily reflect those of the National Institute of Mental Health or National Institutes of Health.
Footnotes
Three publications from this dataset are currently in print and/or in press examining (a) direct and indirect effects of effortful control on child anxiety severity through child interpretation biases (Raines et al., 2019), (b) RSA as a moderator of the association between interpretation biases and child anxiety severity (Trent et al., 2019), and (c) RSA suppression as a moderator of the association between child anxiety sensitivity and fear downregulation (Viana et al., 2019).
Due to space considerations, only maternal behaviors that significantly correlated with key study variables are included in Table 2. Correlations between all 11 maternal behaviors and study variables are presented in the Table S1.
We conducted two additional exploratory analyses to test baseline RSA (cf. RSA suppression) as a potential moderator of the associations between interpretation biases and depressive symptoms in the total sample. The moderation analyses did not meet threshold for statistical significance (ΔR2 due to interaction of CNCEQ and baseline RSA = 0.003, p = .460; ΔR2 due to interaction of WSAP and baseline RSA = 0.01, p = .188).
Given the possibility that externalizing problems influenced the results for boys, moderation analyses were rerun controlling for the presence of a diagnosis of Oppositional Defiant Disorder (ODD; 0 = absent, 1 = present). The moderation results remained the same (ΔR2 due to interaction of RSA suppression and CNCEQ = 0.001, p = .818; ΔR2 due to interaction of RSA suppression and WSAP = 0.0001, p = .951). We thank an anonymous reviewer for suggesting these additional analyses.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Albano AM, Comer JS, Compton SN, Piacentini J, Kendall PC , Birmaher B … Sherrill JT (2018). Secondary outcomes from the Child/Adolescent Anxiety Multimodal Study: Implications for clinical practice. Evidence-Based Practice in Child and Adolescent Mental Health, 3(1), 30–41. 10.1080/23794925.2017.1399485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Zakem AH, Costa NM, Taylor LK, & Weems CF (2009). Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depression and Anxiety 26(6), 503–512. 10.1002/da.20443 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Angold A, Costello EJ, & Erkanli A (1999). Comorbidity. The Journal of Child Psychology, Psychiatry, and Allied Disciplines, 40(1), 57–87. 10.1111/1469-7610.00424 [DOI] [PubMed] [Google Scholar]
- Avenevoli S, Swendsen J, He JP, Burstein M, & Merikangas KR (2015). Major depression in the national comorbidity survey-adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 54(1), 37–44.e2. 10.1016/j.jaac.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, & Choate ML (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35, 205–230. 10.1016/S0005-7894(04)80036-4 [DOI] [PubMed] [Google Scholar]
- Barrett PM, Dadds MR, & Rapee RM (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342. 10.1037/0022-006X.64.2.333 [DOI] [PubMed] [Google Scholar]
- Beard C, & Amir N (2009). Interpretation in social anxiety: When meaning precedes ambiguity. Cognitive Therapy and Research, 33(4), 406–415. 10.1007/s10608-009-9235-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP (2001). Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomie nervous system functioning in psychopathology. Development and Psychopathology, 13(2), 183–214. 10.1017/S0954579401002012 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2015). Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Current Opinion in Psychology, 3(509), 43–47. 10.1016/j.copsyc.2015.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, & Clark DA (1988). Anxiety and depression: An information processing perspective. Anxiety Research, 1(1), 23–36. 10.1080/10615808808248218 [DOI] [Google Scholar]
- Beesdo K, Lau JYF, Guyer AE, McClure-Tone EB, Monk CS, Nelson EE, … Pine D (2009). Common and distinct amygdala-function perturbations in depressed vs anxious adolescents. Archives of General Psychiatry, 66(3), 275–285. 10.1001/archgenpsychiatry.2008.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman SL, Weems CF, Silverman WK, & Kurtines WM (2000). Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy 31(4), 713–731. 10.1016/S0005-7894(00)80040-4 [DOI] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1230–1236. 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SMK (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry 36(4), 545–553. 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Blandon AY, Calkins SD, Keane SP, & O’Brien M (2009). Individual differences in trajectories of emotion regulation processes: The effects of maternal depressive symptomatology and children’s physiological regulation. Developmental Psychology, 44(4), 1110–1123. 10.1037/0012-1649.44.4.1110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt KB, & Obradović J (2013). The construct of psychophysiological reactivity: Statistical and psychometric issues. Developmental Review, 33(1), 29–57. 10.1016/j.dr.2012.10.002 [DOI] [Google Scholar]
- Bush NR, Alkon A, Obradović J, Stamperdahl J, & Thomas Boyce W (2011). Differentiating challenge reactivity from psychomotor activity in studies of children’s psychophysiology: Considerations for theory and measurement. Journal of Experimental Child Psychology, 110(1), 62–79. 10.1016/j.jecp.2011.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, & Keane SP (2004). Cardiac vagal regulation across the preschool period: Stability, continuity, and implications for childhood adjustment. Developmental Psychobiology 45(3), 101–112. 10.1002/dev.20020 [DOI] [PubMed] [Google Scholar]
- Camm AJMM, Malik M, Bigger JTGB, Breithardt G, Cerutti S, Cohen R, … Lombardi F (1996). Heart rate variability: Standards of measurement, physiological interpretation and clinical use. European Heart Journal, 17(3), 354–381. 10.1093/oxfordjournals.eurheartj.a014868 [DOI] [PubMed] [Google Scholar]
- Chorpita BF (2002). The tripartite model and dimensions of anxiety and depression: An examination of structure in a large school sample. Journal of Abnormal Child Psychology, 30(2), 177–190. 10.1023/A:1014709417132 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, & Gray J (2005). Psychometric properties of the revised child anxiety and depression scale in a clinical sample. Behavior Research and Therapy, 43, 309–322. 10.1080/24750573.2017.1297494 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt CE, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Cohen J, & Cohen P (1983). Applied multiple regression for the behavioral sciences (2nd. ed.). Hillsdale, NJ: Laurence Erlbaum. [Google Scholar]
- Costello EJ, Egger HL, Copeland W, Erkanli A, & Angold A (2011). The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. In Silverman WK & Field AP (Eds.), Anxiety disorders in children and adolescents (2nd ed., pp. 56–75). Cambridge, UK: Cambridge University Press. 10.1017/CBO9780511994920 [DOI] [Google Scholar]
- Creswell C, & O’Connor TG (2011). Interpretation bias and anxiety in childhood: Stability, specificity and longitudinal associations. Behavioural and Cognitive Psychotherapy, 39(2), 191–204. 10.1017/S1352465810000494 [DOI] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, & Kendall PC (2014). Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin, 140(3), 816–845. 10.1037/a0034733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing KF, & Gotlib IH (2009). Interpretation of ambiguous information in girls at risk for depression. Journal of Abnormal Child Psychology, 37(1), 79–91. 10.1007/s10802-008-9259-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd HF, Hudson JL, Morris TM, & Wise CK (2012). Interpretation bias in preschool children at risk for anxiety: A prospective study. Journal of Abnormal Psychology, 121(1), 28–38. 10.1037/a0024589 [DOI] [PubMed] [Google Scholar]
- Duncan L, Georgiades K, Wang L, Van Lieshout RJ, MacMillan HL, Ferro MA, … Boyle MH (2018). Psychometric evaluation of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Psychological Assessment, 30(7), 916–928. 10.1037/pas0000541 [DOI] [PubMed] [Google Scholar]
- Ehrenreich JT, Goldstein CR, Wright LR, & Barlow DH (2009). Development of a unified protocol for the treatment of emotional disorders in youth. Child and Family Behavior Therapy, 31(1), 20–37. 10.1080/07317100802701228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley TC, Gregory AM, Lau JYF, McGuffin P, Napolitano M, Rijsdijk FV, & Clark DM (2008). In the face of uncertainty: A twin study of ambiguous information, anxiety and depression in children. Journal of Abnormal Child Psychology, 36(1), 55–65. 10.1007/s10802-007-9159-7 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M (2001). Parental drinking problems and children’s adjustment: Vagal regulation and emotional reactivity as pathways and moderators of risk. Journal of Abnormal Psychology, 110(4), 499–515. 10.1037/0021-843X.110.4.499 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, & Erath SA (2011). Family conflict, autonomic nervous system functioning, and child adaptation: State of the science and future directions. Developmental Psychopathology, 23(2), 703–721. 10.1017/S0954579411000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Erath SA, & Bagley EJ (2013). Parasympathetic nervous system activity and children’s sleep. Journal of Sleep Research, 22(3), 282–288. 10.1111/jsr.12019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Harger J, & Whitson SM (2001). Exposure to interparental conflict and children’s adjustment and physical health: The moderating role of vagal tone. Child Development, 72(6), 1617–1636. 10.1111/1467-8624.00369 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kouros C, Erath SA, Cummings EM, Keller PS, & Staton L (2009). Marital conflict and children’s externalizing behavior: Interactions between parasympathetic and sympathetic nervous system activity. Monographs of the Society for Research in Child Development, 74(1), 1–79. 10.1111/j.1540-5834.2009.00502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, & Whitson SA (2006). Longitudinal relations between marital conflict and child adjustment: Vagal regulation as a protective factor. Journal of Family Psychology, 20(1), 30–39. 10.1037/0893-3200.20.1.30 [DOI] [PubMed] [Google Scholar]
- Fortunato CK, Gatzke-Kopp LM, & Ram N (2013). Associations between respiratory sinus arrhythmia reactivity and internalizing and externalizing symptoms are emotion specific. Cognitive, Affective and Behavioral Neuroscience, 13(2), 238–251. 10.3758/s13415-012-0136-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, & Weersing VR (2010). Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice, 17(4), 293–306. 10.1111/j.1468-2850.2010.01221.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, & Grover RL (2014). Child anxiety prevention study coping and promoting strength: Coding manual for parent-child interactions (pp. 1–21). Baltimore, MD: Johns Hopkins University School of Medicine. [Google Scholar]
- Gonsalves M, Whittles RL, Weisberg RB, & Beard C (2019). A systematic review of the word sentence association paradigm (WSAP). Journal of Behavior Therapy and Experimental Psychiatry, 64, 133–148. 10.1016/j.jbtep.2019.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano PA, Bagner DM, Sheinkopf SJ, Vohr BR, & Lester BM (2012). Evidence-based intervention for young children born premature: Preliminary evidence for associated changes in physiological regulation. Infant Behavior and Development, 35(3), 417–428. 10.1016/j.infbeh.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano PA, & Derefinko K (2013). Cardiac vagal control and children’s adaptive functioning: A meta-analysis. Biological Psychology, 94(1), 22–37. 10.1016/j.biopsycho.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadwin JA, Frost S, French CC, & Richards A (1997). Cognitive processing and trait anxiety in typically developing children: Evidence for an interpretation bias. Journal of Abnormal Psychology, 106(3), 486–490. 10.1037/0021-843X.106.3.486 [DOI] [PubMed] [Google Scholar]
- Han ZR, Zhang X, Davis M, & Suveg C (2019). The role of children’s neurophysiological functioning in the links between emotion-parenting behaviors and child anxiety symptoms: A biological sensitivity to context framework. Family Process, 1–18. 10.1111/famp.12438 [DOI] [PubMed] [Google Scholar]
- Hankin BL (2009). Development of sex differences in depressive and co-occurring anxious symptoms during adolescence: Descriptive trajectories and potential explanations in a multiwave prospective study. Journal of Clinical Child and Adolescent Psychology, 38(4), 460–472. 10.1080/15374410902976288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, & Abramson LY (2002). Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology, 31(4), 491–504. 10.1207/S15374424JCCP3104_8 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to mediation, moderation, and conditional process analyses: A regression-based approach (2nd. ed.). New York, NY: Guilford Press. [Google Scholar]
- Hinnant JB, & El-Sheikh M (2009). Children’s externalizing and internalizing symptoms over time: The role of individual differences in patterns of RSA responding. Journal of Abnormal Child Psychology, 37(8), 1049–1061. 10.1007/s10802-009-9341-1 [DOI] [PubMed] [Google Scholar]
- Hirsch CR, Meeten F, Krahé C, & Reeder C (2016). Resolving ambiguity in emotional disorders: The nature and role of interpretation biases. Annual Review of Clinical Psychology, 12, 281–305. 10.1146/annurev-clinpsy-021815-093436 [DOI] [PubMed] [Google Scholar]
- Holmbeck GN (2002). Post-hoc probing of significant moderational and mediational effects. Journal of Pediatric Psychology, 27(1), 87–96. [DOI] [PubMed] [Google Scholar]
- Houtveen JH, Groot PFC, & de Geus EJC (2005). Effects of variation in posture and respiration on RSA and pre-ejection period. Psychophysiology, 42, 713–719. 10.1111/j.1469-8986.2005.00363.x [DOI] [PubMed] [Google Scholar]
- Jarvis BG (2012). DirectRT [Computer software] (No. 2012). New York, NY: Empirisoft Corporation. [Google Scholar]
- Joormann J, & Vanderlind WM (2014). Emotion regulation in depression: The role of biased cognition and reduced cognitive control. Clinical Psychological Science, 2(4), 402–421. 10.1177/2167702614536163 [DOI] [Google Scholar]
- Kendall PC, & Chansky TE (1991). Considering cognition in anxiety-disordered children. Journal of Anxiety Disorders, 5, 167–185. 10.1016/0887-6185(91)90027-Q [DOI] [PubMed] [Google Scholar]
- Leitenberg H, Yost LW, & Carroll-Wilson M (1986). Negative cognitive errors in children: Questionnaire development, normative data, and comparisons between children with and without self-reported symptoms of depression, low self-esteem, and evaluation anxiety. Journal of Consulting and Clinical Psychology, 54(4), 528–536. 10.1037/0022-006X.54.4.528 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, & Seeley JR (1995). Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry, 34(4), 510–519. 10.1097/00004583-199504000-00018 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, & Sack WH (1997). Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders, 11(4), 377–394. 10.1016/S0887-6185(97)00017-0 [DOI] [PubMed] [Google Scholar]
- Lewis GF, Furman SA, McCool MF, & Porges SW (2012). Statistical strategies to quantify respiratory sinus arrhythmia: Are commonly used metrics equivalent? Biological Psychology, 89(2), 349–364. 10.1016/j.biopsycho.2011.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Lumley MN, & Harkness KL (2007). Specificity in the relations among childhood adversity, early maladaptive schemas, and symptom profiles in adolescent depression. Cognitive Therapy and Research, 31(5), 639–657. 10.1007/s10608-006-9100-3 [DOI] [Google Scholar]
- Lunkenheimer E, Kemp CJ, Lucas-Thompson RG, Cole PM, & Albrecht EC (2017). Assessing biobehavioural self-regulation and coregulation in early childhood: The Parent-Child Challenge Task. Infant and Child Development, 26(1), 1–26. 10.1002/icd.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunkenheimer E, Tiberio SS, Buss KA, Lucas-Thompson RG, Boker SM, & Timpe ZC (2015). Coregulation of respiratory sinus arrhythmia between parents and preschoolers: Differences by children’s externalizing problems. Developmental Psychobiology, 57(8), 994–1003. 10.1002/dev.21323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi G, Millepiedi S, Mucci M, Poli P, Bertini N, & Milantoni L (2004). Generalized anxiety disorder in referred children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 43(6), 752–760. 10.1097/01.chi.0000121065.29744.d3 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, & Koretz DS (2010). Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics, 125(1), 75–81. 10.1542/peds.2008-2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikosch P, Hadrawa T, Laubreiter K, Brandl J, Pilz J, Stettner H, & Grimm G (2010). Effectiveness of respiratory-sinus-arrhythmia biofeedback on state-anxiety in patients undergoing coronary angiography. Journal of Advanced Nursing, 66(5), 1101–1110. 10.1111/j.1365-2648.2010.05277.x [DOI] [PubMed] [Google Scholar]
- Miller JG, Nuselovici JN, & Hastings PD (2016). Nonrandom acts of kindness: parasympathetic and subjective empathic responses to sadness predict children’s prosociality. Child Development, 87(6), 1679–1690. 10.1111/cdev.12629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales S, Beekman C, Blandon AY, Stifter CA, & Buss KA (2014). Longitudinal associations between temperament and socioemotional outcomes in young children: The moderating role of RSA and gender. Developmental Psychobiology, 57(1), 105–119. 10.1002/dev.21267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Luermans J, Merckelbach H, & Mayer B (2000). “Danger is lurking everywhere”: The relation between anxiety and threat perception abnormalities in normal children. Journal of Behavior Therapy and Experimental Psychiatry, 31(2), 123–136. 10.1016/S0005-7916(00)00016-1 [DOI] [PubMed] [Google Scholar]
- O’Neil KA, & Kendall PC (2012). Role of comorbid depression and co-occurring depressive symptoms in outcomes for anxiety-disordered youth treated with cognitive-behavioral therapy. Child and Family Behavior Therapy, 34(3), 197–209. 10.1080/07317107.2012.707086 [DOI] [Google Scholar]
- Obradović J, Bush NR, & Boyce WT (2011). The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: The role of laboratory stressors. Development and Psychopathology, 23(1), 101–114. 10.1017/S0954579410000672 [DOI] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Lewinsohn PM, Rohde P, & Seeley JR (2010). Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: Descriptions of classes and associations with risk factors. Comprehensive Psychiatry, 51(3), 224–235. 10.1016/j.comppsych.2009.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbrook LE, Erath SA, Hinnant JB, & El-Sheikh M (2018). Marital conflict and trajectories of adolescent adjustment: The role of autonomic nervous system coordination. Developmental Psychology, 54(9), 1687–1696. 10.1037/dev0000501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccinelli M, & Wilkinson G (2001). Gender differences in depression. Current Directions in Psychological Science, 10(5), 173–176. 10.1192/bjp.177.6.486 [DOI] [Google Scholar]
- Porges SW (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. 10.1016/j.surg.2006.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raines EM, Viana AG, Trent ES, Woodward EC, Candelari AE, Zvolensky MJ, & Storch EA (2019). Effortful control, interpretation biases, and child anxiety symptom severity in a sample of children with anxiety disorders. Journal of Anxiety Disorders, 67, 102136. 10.1016/j.janxdis.2019.102136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM, & Schniering CA (2013). Effect of comorbidity on treatment of anxious children and adolescents: Results from a large, combined sample. Journal of the American Academy of Child and Adolescent Psychiatry, 52(1), 47–56. 10.1016/j.jaac.2012.10.002 [DOI] [PubMed] [Google Scholar]
- Rivas-Vazquez RA,Saffa-Biller D, Ruiz I, Blais MA,& Rivas-Vazquez A (2004). Current issues in anxiety and depression: Comorbid, mixed, and subthreshold disorders. Professional Psychology: Research and Practice, 35(1), 74–83. 10.1037/0735-7028.35.1.74 [DOI] [Google Scholar]
- Rudolph KD, Monti JD, & Flynn M(2018). Stress reactivity as a pathway from attentional control deficits in everyday life to depressive symptoms in adolescent girls. Journal of Abnormal Child Psychology, 46(3), 613–624. 10.1007/s10802-017-0318-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Calkins SD, Keane SP, Kelleher R, & Suffness R (2014). Trajectories of internalizing symptoms across childhood: The roles of biological self-regulation and maternal psychopathology. Development and Psychopathology, 26(402), 1353–1368. 10.1037/emo0000122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … Wilkinson B (2010). Reliability and validity of the Mini International Neuropsychiatric Interview for children and adolescents (MINI-KID). Journal of Clinical Psychiatry, 71(3), 313–326. 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Ollendick TH (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 34(3), 380–411. 10.1207/s15374424jccp3403 [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Chorpita BF, Miller LM, SGleacher AA (2008). Are children with anxiety disorders privately referred to a university clinic like those referred from the public mental health system? Administration and Policy in Mental Health and Mental Health Services Research, 35(3), 168–180. 10.1007/s10488-007-0154-7 [DOI] [PubMed] [Google Scholar]
- Staton L, El-Sheikh M, & Buckhalt JA (2009). Respiratory sinus arrhythmia and cognitive functioning in children. Developmental Psychobiology, 51(3), 249–258. 10.1002/dev.20361 [DOI] [PubMed] [Google Scholar]
- Suveg C, Hoffman B, Zeman JL, & Thomassin K (2009). Common and specific emotion-related predictors of anxious and depressive symptoms in youth. Child Psychiatry and Human Development, 40(2), 223–239. 10.1007/s10578-008-0121-x [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2013). Using multivariate statistics (6th. ed.). Boston, MA: Allyn & Bacon. [Google Scholar]
- Taghavi MR, Moradi AR, Neshat-Doost HT, Yule W, & Dalgleish T (2000). Interpretation of ambiguous emotional information in clinically anxious children and adolescents. Cognition and Emotion, 14(6), 809–822. 10.1080/02699930050156645 [DOI] [Google Scholar]
- Trent ES, Viana AG, Raines EM, Woodward EC, Candelari AE, Storch EA, & Zvolensky MJ (2019). Interpretation biases and childhood anxiety: The moderating role of parasympathetic nervous system reactivity. Journal of Abnormal Child Psychology, 48(3), 419–433. 10.1007/s10802-019-00605-7 [DOI] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke-Kopp LM (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50(11), 1357–1364. 10.1111/j.1469-7610.2009.02172.x [DOI] [PubMed] [Google Scholar]
- Viana AG, Palmer CA, Zvolensky MJ, Alfano CA, Dixon LJ, & Raines EM (2017). Children’s behavioral inhibition and anxiety disorder symptom severity: The role of individual differences in respiratory sinus arrhythmia. Behaviour Research and Therapy, 93, 38–46. 10.1016/j.brat.2017.03.012 [DOI] [PubMed] [Google Scholar]
- Viana AG, Trent ES, Raines EM, Woodward EC, Storch EA, & Zvolensky MJ (2019). Childhood anxiety sensitivity, fear downregulation, and anxious behaviors: Vagal suppression as a moderator of risk. Emotion, 10.1037/emo0000713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth ME, Hudziak JJ, Heath AC, & Achenbach TM (2001). Latent class analysis of child behavior checklist anxiety/depression in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 40(1), 106–114. 10.1097/00004583-200101000-00023 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2003). Wechsler intelligence scale for children (4th. ed.). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wechsler D (2009). Wechsler individual achievement test (3rd. ed.). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Weems CF, Costa NM, Watts SE, Taylor LK, & Cannon MF (2007). Cognitive errors, anxiety sensitivity, and anxiety control beliefs: Their unique and specific associations with childhood anxiety symptoms. Behavior Modification, 31(2), 174–201. 10.1177/0145445506297016 [DOI] [PubMed] [Google Scholar]
- Wergeland GJH, Fjermestad KW, Marin CE, Bjelland I, Haugland BSM, Silverman WK, … Heiervang ER (2016). Predictors of treatment outcome in an effectiveness trial of cognitive behavioral therapy for children with anxiety disorders. Behaviour Research and Therapy, 76, 1–12. 10.1016/j.brat.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Wilson JK, & Rapee RM (2005). The interpretation of negative social events in social phobia with versus without comorbid mood disorder. Journal of Anxiety Disorders, 19(3), 245–274. 10.1016/j.janxdis.2004.03.003 [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Crick NR, Shirtcliff EA, & Woods KE (2006). The origins and development of psychopathology in females and males. In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Volume one: Theory and method (2nd ed., pp. 76–138). Hoboken, NJ: Wiley. [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, & Marceau K (2008). Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology, 4(1), 275–303. 10.1146/annurev.clinpsy.3.022806.091358 [DOI] [PubMed] [Google Scholar]
- Zeman JL, Cassano M, Perry-Parrish C, & Stegall S (2006). Emotion regulation in children and adolescents. Journal of Developmental and Behavioral Pediatrics, 27(2), 155–168. 10.1016/0375-9601(85)90852-7 [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Rogers AH, Bakhshaie J, Viana AG, Walker R, Mayorga NA, … Ochoa-Perez M, (2019). Perceived racial discrimination, anxiety sensitivity, and mental health among Latinos in a federally qualified health center. Stigma and Health, 4(4), 473–479. 10.1037/sah0000160 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


