Abstract
The treatment of rectal cancer is complex and involves specialized multidisciplinary care, although the tenet is still rooted in a high-quality total mesorectal excision. The robotic platform is one of many tools in the arsenal to assist dissection in the low pelvis. This article is a comprehensive review of the oncological outcome comparing robotic vs laparoscopic rectal cancer resection, with a particular focus on total mesorectal excision. There is no statistical difference in total mesorectal grade, circumferential margin, distal margin, and lymph node harvest. Survival data are less mature, but there is also no difference in disease-free or overall survival between the two techniques. Although additional randomized trials are still needed to validate these findings, both techniques are currently acceptable in the minimally invasive treatment of rectal cancer, and surgeon preference is paramount to safe and optimal resection.
Keywords: laparoscopic, minimally invasive surgery, rectal cancer, rectal carcinoma, robotic, TME, total mesorectal excision
INTRODUCTION
The treatment of rectal cancer involves a multidisciplinary approach including some combination of operative resection, radiation therapy, and systemic therapy for locally advanced disease.1 The order in which these modalities are delivered continues to evolve as total neoadjuvant therapy gains momentum in the literature.2 However, surgical resection—and particularly a total mesorectal resection (TME)—continues to be the mainstay therapy for cure.3
Laparoscopic surgery has been adopted during the past few decades for colectomies and has resulted in less pain, faster recovery, and shorter hospital length of stay without jeopardizing oncological outcomes. Lee et al4 summarized the existing high-quality data regarding open vs laparoscopic resection of colon cancer including the North American Clinical Outcomes of Surgical Therapy Trial, the European Colon carcinoma Laparoscopic or Open Resection trial, and the UK Conventional versus Laparoscopic-Assisted Surgery In Colorectal Cancer trial. Laparoscopy naturally expanded to proctectomies, hoping to help overcome the challenges that the fixed anatomy of the confined pelvis presents. A few multicenter randomized surgical trials comparing open vs laparoscopic rectal cancer were recently published and showed no significant differences in terms of disease-free survival and local recurrence between the two techniques.5–7
There are still significant limitations to traditional laparoscopic instrumentation that the robotic platform attempts to improve. Greater degrees of freedom in movement of wristed instruments, additional assistant arms, and three-dimensional visualization are advantages of the robotic system that are particularly attractive for operations in the challenging anatomic space of the pelvis.8,9 Robotic-assisted surgery is already widely used in the fields of urology, gynecology, thoracic surgery, and head and neck surgery for these reasons, and interest in applying this platform to surgery for rectal cancer continues to grow.
An increasing number of studies have been done to compare oncological outcomes of robot-assisted surgery to laparoscopic surgery in the treatment of rectal cancer. The main markers of quality oncological resection include TME grade, circumferential margin status, distal and proximal margin status, and adequate lymph node harvest, as these have been shown to correlate with decreased recurrence and improved survival.10–12 This literature review summarizes the current data on TME grade and other aspects of oncological outcome in robot-assisted operations for rectal cancer vs traditional laparoscopy.
INCLUDED STUDIES
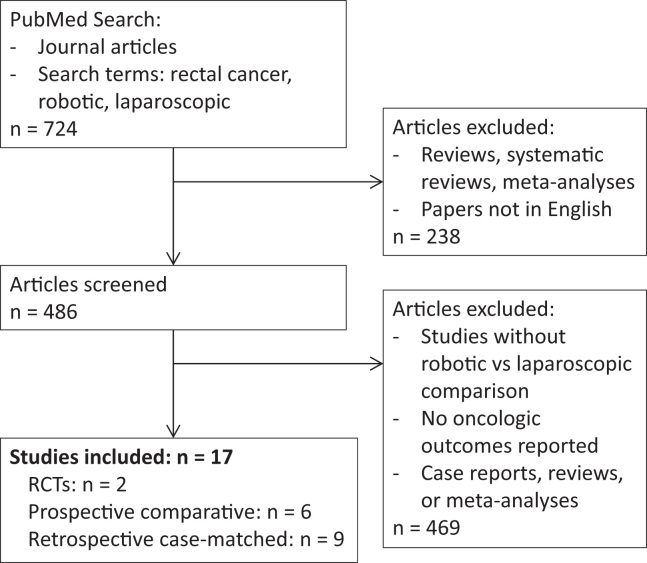
A literature search was conducted on PubMed for journal articles using the search terms “rectal cancer,” “robotic,” and “laparoscopic.” Review articles, meta-analyses, and papers not in English were excluded. From this se search result, we selected studies comparing oncological outcomes (TME grade, margin status, lymph node harvest, survival) in robot-assisted surgery to laparoscopy in rectal cancer resection and TME (Figure 1). Selected studies were published between 2009 and 2019. There were two prospective randomized controlled trials comparing the two technologies: the multicenter Robotic vs Laparoscopic Resection for Rectal Cancer (ROLARR) trial published in 2017 by Jayne et al,13 and the single-center study by Kim et al in 2018.14 The remainder of relevant studies were comparative studies of nonrandomized robotic vs laparoscopic cases or retrospective case-matched series. A study in 2019 by Garfinkle et al15 used a large nationwide database (American College of Surgeons National Surgical Quality Improvement Program) to perform a propensity score analysis of open vs laparoscopic vs robotic surgery for rectal cancer.
Figure 1.
17 studies were selected from an initial search of 724 articles on PubMed. RCTs = randomized controlled trials.
Multiple abdominal-type operations for rectal cancer were described in these trials, including tumor-specific TME, TME, and abdominoperineal resection (APR). Most studies included both patients who received neoadjuvant chemoradiation therapy and those who did not, according to institution or guideline criteria, whereas three studies (Kim et al,16 Huang et al,17 and Lim et al18) focused specifically on rectal cancer resections after neoadjuvant chemoradiation. The included studies in this review are summarized in Table 1.
Table 1.
Characteristics and reported oncological outcomes of included studies
| Year | Authors | Study design | Operations | n (R vs L) | TME complete | CRM negative | Distal margin | Proximal margin | LN harvest | DFS | CSS | OS | Other endpoints |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | Baik et al26 | Prospective, comparative, nonrandomized | LAR | 56 vs 57 | ✓ | ✓ | ✓ | ✓ | ✓ | — | — | — | Postoperative complications, operation time, hemoglobin change, time to flatus passage, time to soft diet, LOS, conversion to open, recurrence |
| 2009 | Patriti et al36 | Prospective, comparative, nonrandomized | PME, TME, APR, CAA | 29 vs 37 | — | ✓ | ✓ | — | ✓ | ✓ | ✓ | Operation time, EBL, conversion to open, hospital stay, 30-day morbidity, long-term morbidity | |
| 2010 | Park et al38 | Case-matched cohort | TME (LAR, CAA, APR) | 41 vs 82 | — | ✓ | ✓ | ✓ | ✓ | — | — | — | Operation time, conversion to open, time to flatus passage, time to regular diet, LOS, postoperative mortality, postoperative morbidity |
| 2011 | Kwak et al39 | Case-matched cohort | TME (LAR, CAA, APR) | 59 vs 59 | — | ✓ | ✓ | — | ✓ | — | — | — | Operation time, conversion to open, postoperative morbidity, operative mortality, recurrence |
| 2013 | D’Annibale et al34 | Prospective, comparative, nonrandomized | TME | 50 vs 50 | — | ✓ | ✓ | — | ✓ | — | — | — | Operation time, conversion to open, postoperative complications, anastomotic leak, oral reintake, LOS, IPSS, IIEF |
| 2015 | Cho et al31 | Case-matched cohort | LAR, CAA | 278 vs 278 | — | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Conversion to open, operation time, EBL, LOS, time to flatus passage, time to liquid diet, time to soft diet, postoperative complications, postoperative mortality, late complications |
| 2015 | Park et al37 | Case-matched cohort | ISR-CAA | 106 vs 106 | — | ✓ | ✓ | ✓ | ✓ | ✓ | — | ✓ | Operation time, EBL, conversion to open, protective stoma, time to diet, LOS, stoma-free at last follow-up, postoperative mortality, postoperative morbidity, LN positivity, local recurrence |
| 2016 | Kim et al16 | Case-matched cohort | NA-CRT: LAR, Hartmann, APR | 33 vs 66 | ✓ | ✓ | ✓ | ✓ | ✓ | — | — | — | EBL, conversion to open, operation time, time to flatus passage, LOS, postoperative morbidity, reoperation |
| 2017 | Huang et al17 | Case-matched cohort | NA-CRT: LAR, ultra-low, ISR-CAA | 40 vs 38 | — | ✓ | ✓ | ✓ | ✓ | — | — | — | Operation time, EBL, postoperative complications, time to flatus passage, time to soft diet, LOS |
| 2017 | Jayne et al13 | Randomized clinical trial | HAR, LAR, APR | 235 vs 224 | ✓ | ✓ | — | — | ✓ | — | — | — | Conversion to open, intraoperative complications, early postoperative complications, late postoperative complications, 30-day mortality |
| 2017 | Kim et al32 | Case-matched cohort | AR, LAR, APR | 224 vs 224 | — | ✓ | ✓ | — | ✓ | — | — | — | Operation time, conversion to open, diverting stoma, postoperative morbidity, postoperative mortality, LOS |
| Case-matched cohort for 5-year follow-up | 196 vs 192 | — | — | — | — | — | ✓ | ✓ | ✓ | ||||
| 2017 | Lim et al18 | Prospective, comparative, nonrandomized | NA-CRT: LAR, ISR, CAA, APR | 74 vs 64 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | — | ✓ | Operation time, conversion to open, recurrence |
| 2017 | Valverde et al27 | Prospective, comparative, nonrandomized | Sphincter-sparing | 65 vs 65 | ✓ | ✓ | ✓ | ✓ | — | — | — | — | Operation time, diverting ostomy, EBL, drainage, conversion to open, reoperation, morbidity, LOS, mortality |
| 2018 | Crolla et al33 | Prospective, comparative, nonrandomized | AR, LAR, APR | 168 vs 184 | — | ✓ | — | — | ✓ | — | — | — | Operation time, LOS, conversion to open, SSI, anastomotic leak, mortality, other |
| 2018 | Kim et al14 | Randomized controlled trial | LAR, APR, Hartmann | 66 vs 73 | ✓ | ✓ | ✓ | ✓ | ✓ | — | — | — | GOALS, return of bowel function, morbidity, postoperative pain scores, QOL |
| 2018 | Panteleimonitis et al40 | Case-matched cohort | HAR, LAR, APR, Hartmann | 63 vs 61 | — | ✓ | — | — | ✓ | — | — | — | Operation time, EBL, conversion to open, LOS, 30-day readmission, 30-day reoperation, 30-day mortality, anastomotic leak |
| 2019 | Garfinkle et al15 | Cohort–propensity score analysis | LAR, APR | 154 vs 213 | — | ✓ | ✓ | — | ✓ | — | — | — | Operation time, conversion, postoperative morbidity and mortality, LOS, hospital readmission |
APR = abdominoperineal resection; AR = anterior resection; CAA = coloanal anastomosis; CRM = circumferential resection margin; CSS = cancer-specific survival; DFS = disease-free survival; EBL = estimated blood loss; GOALS: global operative assessment of laparoscopic skills; HAR = high anterior resection; IIEF = International Index of Erectile Function; IPSS = International Prostate Symptoms Score; ISR = intersphincteric resection; L = laparoscopic; LAR = low anterior resection; LN = lymph node; LOS = hospital length of stay; NA-CRT = neoadjuvant chemoradiation therapy; OS = overall survival; PME = partial mesorectal excision; QOL = quality of life; R = robotic; SSI = surgical site infection; TME = total mesorectal excision.
TME GRADE OUTCOMES
TME has been the gold standard for oncological resection of mid to low rectal cancer since its wide adoption in the mid-1980s.19 High-quality TME has been shown to reduce local recurrence rates and increase disease-free survival.3,20–22 However, surgical quality assessment of correct anatomic dissection via TME grade reporting continues to be inconsistent in clinical practice.23
Nagtegaal et al10 recommended three defined groups to categorize macroscopic mesorectal grading based on the Dutch TME trial: 1) complete, intact mesorectum with only minor irregularities of a smooth mesorectal surface and no defect deeper than 5 mm and no coning toward the distal margin; 2) nearly complete, moderate bulk to the mesorectum, but irregularity of the mesorectal surface and/or moderate coning of the specimen, without visible muscularis propria; and 3) incomplete, little bulk to the mesorectum with defects down onto muscular propria and/or very irregular circumferential resection margin. This seminal article did not observe any difference in prognosis between the complete and near-complete groups, but did note that overall recurrence rates were statistically significantly worse at 2 years in the group with an incomplete mesorectum (35.6% vs 21.5%, p = 0.01). Another study dedicated to investigating surgical TME quality confirmed that the presence of defects in the mesorectum predisposes patients to local and distant recurrences, reiterating the importance of sound surgical dissection in the correct TME plane.24
Various factors besides surgical skill can affect the success of TME completeness. Sapci et al25 showed in a study of nearly 700 patients that operative approach (open vs laparoscopic vs robotic), body mass index, and gender were not associated with a noncomplete mesorectal grade, but distal tumors within 5 cm from the anal verge, nonrestorative procedures (abdominoperineal resection), and positive circumferential margins were associated with a noncomplete mesorectum. This suggests that the confines of the narrow pelvis complicate a complete TME for a low-lying rectal mass, a problem the robotic platform hopes to alleviate.
Given the importance of TME completeness on short- and long-term oncological outcomes, it is surprising that TME grade is sparsely reported in the robotic literature. Table 2 summarizes the studies that included data on TME grade and completeness. Only Baik et al26 in 2009 reported a statistically significant difference in favor of robot over laparoscopy, with 92.9% in their robotic group achieving a complete TME compared to 75.4% in their laparoscopic group (p = 0.033). In contrast, the ROLARR trial reported a similar 76.4% vs 77.6% complete TME in robot vs laparoscopy (p = 0.14).13 Kim et al14 in their smaller randomized controlled trial in 2018 also achieved similar results, with 80.3% in their robotic group vs 78.1% in the laparoscopic group (p = 0.599). A case-matched cohort study in 2016 by Kim et al16 also reported no difference in TME completeness (97.0% in robotic vs 90.9% in laparoscopic, p = 0.41). Similarly, independent, prospective nonrandomized studies by Lim et al18 and Valverde et al27 in 2017 comparing robotic to laparoscopic rectal cancer resections and found no difference in TME grade completeness, (95.9% vs 100%, p = 0.384; and 88% vs 82%, p = 0.28, respectively). This comprehensive review highlights the current low standardized reporting of TME grade in the robotic rectal resection literature. As more oncological data mature, TME grade is expected to be reported more often because it has become a more recognized universal outcome measure.
Table 2.
Total mesorectal excision grade outcomes
| Study | TME complete | p Value | |
|---|---|---|---|
| Robot | Lap | ||
| Baik et al26 | 92.9% | 75.4% | 0.033 |
| Kim et al16 | 97.0% | 90.9% | 0.41 |
| Jayne et al13 | 76.4% | 77.6% | 0.14 |
| Lim et al18 | 95.9% | 100% | 0.384 |
| Valverde et al27 | 88.0% | 82.0% | 0.28 |
| Kim et al14 | 80.3% | 78.1% | 0.599 |
Lap = laparoscopic; TME = total mesorectal excision.
The Commission on Cancer National Accreditation Program for Rectal Cancer recommends standardized synoptic format pathological reporting to include all required data elements outlined in the College of American Pathologists rectal cancer protocols, including tumor depth of invasion, nodal status, completeness of the mesorectal excision, status of the circumferential margin, and the response of the tumor to neoadjuvant therapy.28 The National Accreditation Program for Rectal Cancer guidelines also highlight the importance of photographic documentation of the TME specimen to be presented at a rectal cancer tumor board to assess surgical quality as a multidisciplinary group. Not only does this pathological information form the basis for decisions on adjuvant therapy, but also it serves as an important indicator of surgical quality and can function as a guide for surgical improvement.29
Given the paucity of TME completeness in the current robotic literature, the oncological outcomes remain important and are highlighted here.
OTHER ONCOLOGICAL OUTCOMES
Circumferential Margin
A negative circumferential resection margin (CRM) is strong prognostic indicator of survival. To date, it has been the most studied element of oncological resection and is associated intimately with a complete TME.11 Factors shown to increase the risk of a positive CRM include tumor size > 5.9 cm, a distance of ≤ 2.6 cm from the dentate line, incomplete TME, and high-risk features such as microvascular and perineural invasion.30 Furthermore, Nagtegaal et al10 showed that even in patients with a negative CRM, the overall recurrence rate was greater with incomplete TME (28.6% vs 14.9%, p = 0.03), highlighting that the quality of macroscopic TME has additional value beyond microscopic CRM determination.
In the ROLARR trial, there was no statistical difference in the CRM-negative resection rate between the robotic group and the laparoscopic group (94.9% vs 93.8%, p = 0.56).13 The remaining nonrandomized comparative trials and case-matched series also did not show any statistically significant difference in CRM-negative rates. Most showed a greater than 90% CRM-negative rate in both robotic and laparoscopic resections. In 2015, Cho et al31 compared 278 robotic cases with a case-matched group of 278 laparoscopic cases and demonstrated CRM-negative rates of 95% vs 95.3%, respectively (p = 1.0). In a similar-size and -design study published in 2017, Kim et al32 found comparable results (96% robotic vs 95.1% laparoscopic, p = 0.823). A Dutch study in 2018 comparing 168 robotic rectal cancer patients to 184 laparoscopic patients produced similar findings (95.2% vs 97.8%, p = 0.24).33 Of note, one small Italian study in 2012 by D’Annibale et al34,35 reported a statistically significant difference in CRM status in favor of robotic surgery when using a CRM cutoff of 2 mm, with 100% negative margins in the robotic arm vs 88% in the laparoscopic arm (p = 0.022). The clinical importance of this result when compared to the rest of the studies is unclear. See Table 3 for all reported CRM outcomes. In summary, the use of robotic technology does not appear to improve CRM negativity rates when compared to laparoscopy.
Table 3.
Circumferential margin outcomes
| Study | CRM negative (> 1 mm) | p Value | |
|---|---|---|---|
| Robot | Lap | ||
| Baik et al26 | 92.9% | 91.2% | 0.749 |
| Patriti et al36 | 100% | 100% | Not reported |
| Park et al38 | 92.7% | 96.3% | 0.542 |
| Kwak et al39 | 98.3% | 100.0% | > 0.999 |
| D’Annibale et al*34 | 100% | 88% | 0.022 |
| Cho et al31 | 95.0% | 95.3% | 1.000 |
| Park et al37 | 92% | 91% | 0.976 |
| Kim et al16 | 78.8% | 84.8% | 0.42 |
| Huang et al17 | 100% | 94.7% | 0.14 |
| Jayne et al13 | 94.9% | 93.8% | 0.56 |
| Kim et al32 | 96.0% | 95.1% | 0.8231 |
| Lim et al18 | 95.9% | 100% | 0.384 |
| Valverde et al27 | 94% | 89% | 0.47 |
| Crolla et al33 | 95.2% | 97.8% | Univariable p = 0.24, multivariable p = 1.00 |
| Kim et al14 | 92.4% | 93.2% | 0.999 |
| Panteleimonitis et al40 | 96.8% | 98.4% | 1.000 |
| Garfinkle et al15 | 94.8% | 96.2% | 0.46 |
CRM = circumferential resection margin; Lap = laparoscopic, *CRM > 2 mm corresponds to the study by D'Annibale et al. exclusively.
Distal Margin
Another principle of rectal cancer surgery is achieving an adequate distal resection margin, as this contributes to lower local recurrence rates. The National Comprehensive Cancer Network guidelines recommend a gross resection margin of 4 to 5 cm below the distal edge of the tumor. The robotic platform theoretically helps to overcome the surgical challenges of the narrow anatomic space of the pelvis. The ROLARR trial did not report measured distal margins but did report one patient in their laparoscopic arm with a positive distal margin compared to none in the robotic arm.13 Cho et al,31 in 2015, reported a mean distal margin of 2.0 cm in the robotic group compared to 2.2 cm in their laparoscopic group, with a nonsignificant p value of 0.161. Kim et al,32 in 2017, also reported no difference in mean distal margins of 2.3 cm vs 2.4 cm in their robotic vs laparoscopic groups (p = 0.374). No studies demonstrated a statistically significant difference between the two platforms for distal margin. Some studies also compared proximal margins, all showing no statistically significant differences when reporting greater than 5 cm both robotically and laparoscopically. Distal and proximal margin outcome data are consolidated in Table 4.
Table 4.
Distal and proximal margin outcomes
| Study | Distal margin | p Value | Proximal margin | p Value | ||
|---|---|---|---|---|---|---|
| Robot | Lap | Robot | Lap | |||
| Baik et al,26 mean ± SD | 4.0 ± 1.6 cm | 3.6 ± 1.7 cm | 0.497 | 10.9 ± 4.0 cm | 10.8 ± 4.3 cm | 0.971 |
| Patriti et al,36 mean ± SD | 2.1 ± 0.9 cm | 4.5 ± 7.2 cm | > 0.05 | — | — | — |
| Park et al,38 mean ± SD | 2.1 ± 1.4 cm | 2.3 ± 1.5 cm | 0.438 | 17.2 ± 6.2 cm | 18.5 ± 8.5 cm | 0.417 |
| Kwak et al,39 median (IQR) | 2.2 cm (1.5–3.0 cm) | 2.0 cm (1.2–3.5 cm) | 0.865 | — | — | — |
| D’Annibale et al,34 mean ± SD | 3 ± 1.1 cm | 3 ± 1.6 cm | 0.908 | — | — | — |
| Cho et al,31 mean ± SD | 2.0 ± 1.4 cm | 2.2 ± 1.4 cm | 0.161 | 10.8 ± 6.0 cm | 11.2 ± 6.1 cm | 0.536 |
| Park et al37, mean ± SD | 1.2 ± 0.8 cm | 1.2 ± 0.7 cm | 0.739 | 20.3 ± 7.4 cm | 21.0 ± 10.7 cm | 0.575 |
| Kim et al,16 mean ± SD | 2.2 ± 1.5 cm | 2.2 ± 1.7 cm | 0.95 | 17.4 ± 2.7 cm | 14.2 ± 6.0 cm | 0.15 |
| Huang et al,17 mean ± SD | 1.7 ± 1.4 cm | 1.7 ± 1.1 cm | 0.99 | 9.6 ± 3.4 cm | 11.0 ± 6.3 cm | 0.23 |
| Kim et al,32 mean ± SD | 2.3 ± 2.6 cm | 2.4 ± 2.2 cm | 0.3746 | — | — | — |
| Lim et al,18 mean ± SD | 1.7 ± 1.4 cm | 2.2 ± 1.5 cm | 0.339 | 12.8 ± 4.1 cm | 14.0 ± 5.1 cm | 0.070 |
| Valverde et al,27 distal margin > 1 mm | 98% | 87% | 0.61 | 17 ± 9 cm | 19 ± 10 cm | 0.17 |
| Kim et al,14 median (range) | 1.5 cm (0.04–6.7 cm) | 0.7 cm (0–2.5 cm) | 0.11 | 12.3 cm (4.7–35.8 cm) | 13.2 cm (6.8–29.0 cm) | 0.727 |
| Garfinkle et al,15 distal margin negative | 98.7% | 100% | — | — | — | — |
IQR = interquartile range; Lap = laparoscopic; SD = standard deviation.
Lymph Node Harvest
Only one study reported a statistically significant difference in the number of lymph nodes harvested using robotic vs laparoscopic surgery, highlighted in Table 5. Kim et al,14 in 2018, obtained a median harvest of 18 lymph nodes in their robotic group vs 15 in their laparoscopic group (p = 0.04). In addition, they reported 90.9% of the robotic group vs 74.0% of their laparoscopic group had more than 12 lymph nodes harvested (p = 0.009). This was their only statistically significantly different outcome among all their postoperative pathological outcomes. The largest study by Cho et al,31 in 2015, reported the mean number of lymph nodes harvested by robotic vs laparoscopic surgery to be 15.0 vs 16.2, with a nonsignificant difference (p = 0.069). The randomized ROLARR trial described the mean lymph node harvest as 23.2 vs 24.1, but no statistical comparison was performed.13 Kim et al,32 in 2017, also found no statistically significant difference in the mean number of lymph nodes harvested, with 20.2 in their robotic group and 21.0 in their laparoscopic group (p = 0.4410). Interestingly, several studies reported mean lymph nodes harvested to be less than the ideal 12 lymph nodes recommended by the American Joint Committee on Cancer, the College of American Pathologists, and the National Comprehensive Cancer Network, but still found no statistically significant difference.18,33,36 Because lymph node harvest is often determined by a sufficiently high ligation of the mesenteric vessels, it is not unexpected that the robotic platform does not clearly confer an advantage over laparoscopy in this oncological outcome.
Table 5.
Lymph node harvest outcomes
| Study | Lymph node harvest (mean ± SD) | p Value | |
|---|---|---|---|
| Robot | Lap | ||
| Baik et al,26 mean ± SD | 18.4 ± 9.2 | 18.7 ± 12 | 0.831 |
| Patriti et al,36 mean ± SD | 10.3 ± 4 | 11.2 ± 5 | > 0.05 |
| Park et al,38 mean ± SD | 17.3 ± 7.7 | 14.2 ± 8.9 | 0.060 |
| Kwak et al,39 median (IQR) | 20 (12–27) | 21 (14–28) | 0.702 |
| D’Annibale et al,34 mean ± SD | 16.5 ± 7.1 | 13.8 ± 6.7 | 0.053 |
| Cho et al,31 mean ± SD | 15.0 ± 8.1 | 16.2 ± 8.1 | 0.069 |
| Park et al,37 mean ± SD | 13.2 ± 7.3 | 15.2 ± 10.8 | 0.126 |
| Kim et al,16 mean ± SD | 22.3 ± 11.7 | 21.6 ± 11.0 | 0.82 |
| Huang et al,17 mean (range) | 16.7 (4–46) | 15.6 (6–29) | 0.49 |
| Jayne et al,13 mean ± SD | 23.2 ± 11.97 | 24.1 ± 12.91 | — |
| Kim et al,32 mean ± SD | 20.2 ± 12.1 | 21.0 ± 14.4 | 0.4410 |
| Lim et al,18 mean ± SD | 11.6 ± 6.9 | 14.7 ± 6.5 | 0.971 |
| Crolla et al,33 median (range) | 14 (2–44) | 7 (0–44) | Univariable p < 0.0005 |
| Kim et al,14 median (range) | 18 (7–59) | 15 (4–40) | 0.04 |
| Panteleimonitis et al,40 median (IQR) | 17 (13–23.35) | 16 (12–23.5) | 0.639 |
| Garfinkle et al,15 mean ± SD | 15.6 ± 7.6 | 16.6 ± 7.4 | 0.29 |
IQR = interquartile range; Lap = laparoscopic; SD = standard deviation.
Survival
Few studies reported on long-term overall or disease-free survival, and their results are tabulated in Table 6. Patriti et al,36 in 2009, stated no difference in overall and disease-free survival between the robotic and laparoscopic groups throughout the duration of the study, but did not report a full 5-year follow-up. In the 2015 study by Cho et al,31 92.2% of the robotic group survived whereas 93.1% of the laparoscopic group survived to 5 years (p = 0.422); 81.8% (robotic) vs 79.6% (laparoscopic) were cancer free at 5 years (p = 0.538).31 Park et al, 37 in 2015, compared robotic vs laparoscopic outcomes for intersphincteric resections and reported a 5-year overall survival of 88.5% vs 88.4% (p = 0.899) and a disease-free survival of 80.6% vs 82.8% (p = 0.298). Kim et al, 32 in 2017, compared a case-matched subset of their robotic vs laparoscopic patients who reached the 5-year follow-up and reported 90.5% vs 78.0% overall survival, respectively, without a statistically significant difference (p = 0.3231); and 72.6% vs 68.0% disease-free survival, respectively, without a statistically significant difference (p = 0.6409). However, after multivariate analysis of their matched patients, they reported the robotic approach was a statistically significant prognostic factor for overall survival and cancer-specific survival (p = 0.0040, Hazard Ratio = 0.333; p = 0.0161, Hazard Ratio = 0.367).32 Last, in 2017, Lim et al18 reported no statistically significant difference in overall survival (90% vs 93.3%, p = 0.424) or disease-free survival (76.8% vs 76.0%, p = 0.834) between robot and laparoscopy. In summary, no studies thus far have demonstrated a statistically significant difference in overall survival, disease-free survival, or cancer-specific survival.
Table 6.
Survival outcomes
| Study | DFS (5-year) | CSS | OS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Robot | Lap | p Value | Robot | Lap | p Value | Robot | Lap | p Value | |
| Patriti et al36 | No difference | — | — | — | — | No difference | — | ||
| Cho et al31 | 81.8% | 79.6% | 0.538 | 93.6% | 95.5% | 0.120 | 92.2% | 93.1% | 0.422 |
| Park et al37 | 80.6% | 82.8% | 0.298 | — | — | — | 88.5% | 88.4% | 0.899 |
| Kim et al32 | 72.6% | 68.0% | 0.6409 | 90.5% | 79.5% | 0.4465 | 90.5% | 78.0% | 0.3231 |
| Lim et al18 | 76.8% | 76.0% | 0.834 | — | — | — | 90% | 93.3% | 0.424 |
CSS = cancer-specific survival; DFS = disease-free survival; Lap = laparoscopy; OS = overall survival.
CONCLUSION
The majority of studies comparing robotic vs laparoscopic surgery for rectal cancer showed no statistically significant differences in oncological outcomes of TME completeness, CRM, distal margin, lymph nodes harvested, and survival (overall, disease free, and cancer specific). Data thus far confirm the noninferiority of the robotic approach compared to laparoscopy in terms of oncological outcomes. Although not addressed in this review, nononcological outcomes such as complications, hospital length of stay, patients’ postoperative experience, cost, and surgical ergonomics also weigh in on the potential advantages or disadvantages of the robotic platform. Further prospective, randomized multicenter trials are needed to evaluate and weigh the potential benefits of the robotic platform against the cost of technology in the treatment of rectal cancer to define more fully the indications for its use. The oncological data for robotic rectal cancer resection are still immature because the majority of publications do not include data on TME grade and completeness, which is well correlated with lower local recurrence rates and greater survival rates. Because TME grade, at its core, is an indication of surgical quality, it would seem to be a good indicator of whether the robotic platform truly provides the technical advantages over laparoscopy it claims to provide.
Footnotes
Disclosure Statement: The authors have no conflicts of interest to disclose.
Funding Support: No funding was received in support of this project.
Author Contributions: Jessica Lam, MD, Michael S Tam, MD, and Elisabeth C McLemore, MD, participated in conception and design. Jessica Lam, MD, Michael S Tam, MD, and R. Luke Rettig, MD, participated in data analysis and interpretation. Jessica Lam, MD, Michael S Tam, MD, R. Luke Rettig, MD, and Elisabeth C McLemore, MD, provided administrative, technical, and material support.
REFERENCES
- 1.National Comprehensive Cancer Network. Rectal cancer (Version 6.2020). Accessed November 29, 2020. http://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf
- 2.Cercek A, Roxburgh CSD, Strombom P, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol 2018. Jun;4(6):e180071:1–8. DOI: 10.1001/jamaoncol.2018.0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: A prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 2009. Mar;373(9666):821–8. DOI: 10.1016/S0140-6736(09)60485-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JK, Delaney CP, Lipman JM. Current state of the art in laparoscopic colorectal surgery for cancer: Update on the multi-centric international trials. Ann Surg Innov Res 2012. Jul;6(1):1–8. DOI: 10.1186/1750-1164-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015. Apr;372(14):1324–32. DOI: 10.1056/NEJMoa1414882 [DOI] [PubMed] [Google Scholar]
- 6.Fleshman J, Branda ME, Sargent DJ, et al. Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: Follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 2019. Apr;269(4):589–95. DOI: 10.1097/SLA.0000000000003002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevenson ARL, Solomon MJ, Brown CSB, et al. Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: The Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 2019. Apr;269(4):596–602. DOI: 10.1097/SLA.0000000000003021 [DOI] [PubMed] [Google Scholar]
- 8.Intuitive. da Vinci: Robotic surgical systems. Accessed November 29, 2020. https://www.intuitive.com/en-us/products-and-services/da-vinci
- 9.Hance J, Rockall T, Darzi A. Robotics in colorectal surgery. Dig Surg 2004. 21(5–6): 339–43. DOI: 10.1159/000081350 [DOI] [PubMed] [Google Scholar]
- 10.Nagtegaal ID, van de Velde CJH, van der Worp E, Kapiteijn E, Quirke P, van Krieken JHJM, Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group. Macroscopic evaluation of rectal cancer resection specimen: Clinical significance of the pathologist in quality control. J Clin Oncol 2002. Apr;20(7):1729–34. DOI: 10.1200/JCO.2002.07.010 [DOI] [PubMed] [Google Scholar]
- 11.Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 2008. Jan;26(2):303–12. DOI: 10.1200/JCO.2007.12.7027 [DOI] [PubMed] [Google Scholar]
- 12.Tepper JE, O’Connell MJ, Niedzwiecki D, et al. Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 2001. Jan;19(1):157–63. DOI: 10.1200/JCO.2001.19.1.157 [DOI] [PubMed] [Google Scholar]
- 13.Jayne D, Pigazzi A, Marshall H, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: The ROLARR randomized clinical trial. JAMA 2017. Oct;318(16):1569–80. DOI: 10.1001/jama.2017.7219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim MJ, Park SC, Park JW, et al. Robot-assisted versus laparoscopic surgery for rectal cancer: A phase II open label prospective randomized controlled trial. Ann Surg 2018. Feb;267(2):243–51. DOI: 10.1097/SLA.0000000000002321 [DOI] [PubMed] [Google Scholar]
- 15.Garfinkle R, Abou-Khalil M, Bhatnagar S, et al. A comparison of pathologic outcomes of open, laparoscopic, and robotic resections for rectal cancer using the ACS-NSQIP proctectomy-targeted database: A propensity score analysis. J Gastrointest Surg 2019. Feb;23(2):348–56. DOI: 10.1007/s11605-018-3974-8 [DOI] [PubMed] [Google Scholar]
- 16.Kim YS, Kim MJ, Park SC, et al. Robotic versus laparoscopic surgery for rectal cancer after preoperative chemoradiotherapy: Case-matched study of short-term outcomes. Cancer Res Treat 2016. Jan;48(1):225–31. DOI: 10.4143/crt.2014.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang YM, Huang YJ, Wei PL. Outcomes of robotic versus laparoscopic surgery for mid and low rectal cancer after neoadjuvant chemoradiation therapy and the effect of learning curve. Medicine (Baltimore) 2017. Oct;96(40):e81711–7. DOI: 10.1097/MD.0000000000008171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim DR, Bae SU, Hur H, et al. Long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision of mid-low rectal cancer following neoadjuvant chemoradiation therapy. Surg Endosc 2017. Apr;31(4):1728–37. DOI: 10.1007/s00464-016-5165-6 [DOI] [PubMed] [Google Scholar]
- 19.Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986. Jun;1(8496):1479–82. DOI: 10.1016/S0140-6736(86)91510-2 [DOI] [PubMed] [Google Scholar]
- 20.Arbman G, Nilsson E, Hallböök O, Sjödahl R. Local recurrence following total mesorectal excision for rectal cancer. Br J Surg 1996. Mar;83(3):375–9. DOI: 10.1002/bjs.1800830326 [DOI] [PubMed] [Google Scholar]
- 21.Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: The Basingstoke experience of total mesorectal excision, 1978–1997. Arch Surg 1998. Aug;133(8):894–9. DOI: 10.1001/archsurg.133.8.894 [DOI] [PubMed] [Google Scholar]
- 22.Kapiteijn E, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001. Aug;345(9):638–46. DOI: 10.1056/NEJMoa010580 [DOI] [PubMed] [Google Scholar]
- 23.Kanters AE, Cleary RK, Obi SH, et al. Uptake of total mesorectal excision and total mesorectal excision grading for rectal cancer: A statewide study. Dis Colon Rectum 2020. Jan;63(1):53–9. DOI: 10.1097/DCR.0000000000001526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maurer CA, Renzulli P, Kull C, et al. The impact of the introduction of total mesorectal excision on local recurrence rate and survival in rectal cancer: Long-term results. Ann Surg Oncol 2011. Jul;18(7):1899–906. DOI: 10.1245/s10434-011-1571-0 [DOI] [PubMed] [Google Scholar]
- 25.Sapci I, Velazco JS, Xhaja X, et al. Factors associated with noncomplete mesorectal excision following surgery for rectal adenocarcinoma. Am J Surg 2019. Mar;217(3):465–8. DOI: 10.1016/j.amjsurg.2018.10.051 [DOI] [PubMed] [Google Scholar]
- 26.Baik SH, Kwon HY, Kim JS, et al. Robotic versus laparoscopic low anterior resection of rectal cancer: Short-term outcome of a prospective comparative study. Ann Surg Oncol 2009. Jun;16(6):1480–7. DOI: 10.1245/s10434-009-0435-3 [DOI] [PubMed] [Google Scholar]
- 27.Valverde A, Goasguen N, Oberlin O, et al. Robotic versus laparoscopic rectal resection for sphincter-saving surgery: Pathological and short-term outcomes in a single-center analysis of 130 consecutive patients. Surg Endosc 2017. Oct;31(10):4085–91. DOI: 10.1007/s00464-017-5455-7 [DOI] [PubMed] [Google Scholar]
- 28.Commission on Cancer. National Accreditation Program for Rectal Cancer: A quality program of the American College of Surgeons: Optimal resources for rectal cancer care, 2020 standards. Accessed December 28, 2020. https://www.facs.org/-/media/files/quality-programs/cancer/naprc/optimal_resources_for_rectal_cancer_care_2020_standards.ashx
- 29.Hendren S, McKeown E, Morris AM, et al. Implementation of a hospital-based quality assessment program for rectal cancer. J Oncol Pract 2014. May;10(3):e120–9. DOI: 10.1200/JOP.2014.001387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hiranyakas A, da Silva G, Wexner SD, Ho YH, Allende D, Berho M. Factors influencing circumferential resection margin in rectal cancer. Colorectal Dis 2013. Mar;15(3):298–303. DOI: 10.1111/j.1463-1318.2012.03179.x [DOI] [PubMed] [Google Scholar]
- 31.Cho MS, Baek SJ, Hur H, et al. Short and long-term outcomes of robotic versus laparoscopic total mesorectal excision for rectal cancer: A case-matched retrospective study. Medicine (Baltimore) 2015. Mar;94(11):e5221–10. DOI: 10.1097/MD.0000000000000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim J, Baek SJ, Kang DW, et al. Robotic resection is a good prognostic factor in rectal cancer compared with laparoscopic resection: Long-term survival analysis using propensity score matching. Dis Colon Rectum 2017. Mar;60(3):266–73. DOI: 10.1097/DCR.0000000000000770 [DOI] [PubMed] [Google Scholar]
- 33.Crolla RMPH, Mulder PG, van der Schelling GP. Does robotic rectal cancer surgery improve the results of experienced laparoscopic surgeons? An observational single institution study comparing 168 robotic assisted with 184 laparoscopic rectal resections. Surg Endosc 2018. Nov;32(11):4562–70. DOI: 10.1007/s00464-018-6209-x [DOI] [PubMed] [Google Scholar]
- 34.D’Annibale A, Pernazza G, Monsellato I, et al. Total mesorectal excision: A comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 2013. Jun;27(6):1887–95. DOI: 10.1007/s00464-012-2731-4 [DOI] [PubMed] [Google Scholar]
- 35.Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH, Pathology Review Committee Cooperative Clinical Investigators. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: Not one millimeter but two millimeters is the limit. Am J Surg Pathol 2002. Mar;26(3):350–7. DOI: 10.1097/00000478-200203000-00009 [DOI] [PubMed] [Google Scholar]
- 36.Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Biancafarina A, Casciola L. Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. JSLS 2009. Apr–Jun;13(2):176–83. [PMC free article] [PubMed] [Google Scholar]
- 37.Park JS, Kim NK, Kim SH, et al. Multicentre study of robotic intersphincteric resection for low rectal cancer. Br J Surg 2015. Nov;102(12):1567–73. DOI: 10.1002/bjs.9914 [DOI] [PubMed] [Google Scholar]
- 38.Park JS, Choi GS, Lim KH, Jang YS, Jun SH. Robotic-assisted versus laparoscopic surgery for low rectal cancer: Case-matched analysis of short-term outcomes. Ann Surg Oncol 2010. Dec;17(12):3195–202. DOI: 10.1245/s10434-010-1162-5 [DOI] [PubMed] [Google Scholar]
- 39.Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS. Robotic vs laparoscopic resection of rectal cancer: Short-term outcomes of a case–control study. Dis Colon Rectum 2011. Feb;54(2):151–6. DOI: 10.1007/DCR.0b013e3181fec4fd [DOI] [PubMed] [Google Scholar]
- 40.Panteleimonitis S, Pickering O, Abbas H, et al. Robotic rectal cancer surgery in obese patients may lead to better short-term outcomes when compared to laparoscopy: A comparative propensity scored match study. Int J Colorectal Dis 2018. Aug;33(8):1079–86. DOI: 10.1007/s00384-018-3030-x [DOI] [PMC free article] [PubMed] [Google Scholar]