Abstract
Cutaneous leishmaniasis is a neglected and parasitic vector borne diseases that is endemic in tropical and subtropical countries, including Iran. The aim of this study was to explain the present status of CL in Iran. This report is based on data that recorded by cutaneous leishmaniasis surveillance system in 2019, and evaluated in Center for Communicable Diseases Management in Ministry of Health in Iran. Iran has been considered an endemic area for cutaneous leishmaniasis in the world. Dependent to activities for cutaneous leishmaniasis control the number of cases decreased from 23202 in 2008 (Incidence rate 32 per 100000) to 13124 in 2019 (Incidence rate 15.8 per 100000), more cases reported from September to December, in 2019, 46% of cases had one lesion and 21% had 2 lesions, 85% of cases diagnosed when the diameter of lesions had 3 centimeters and bellows.
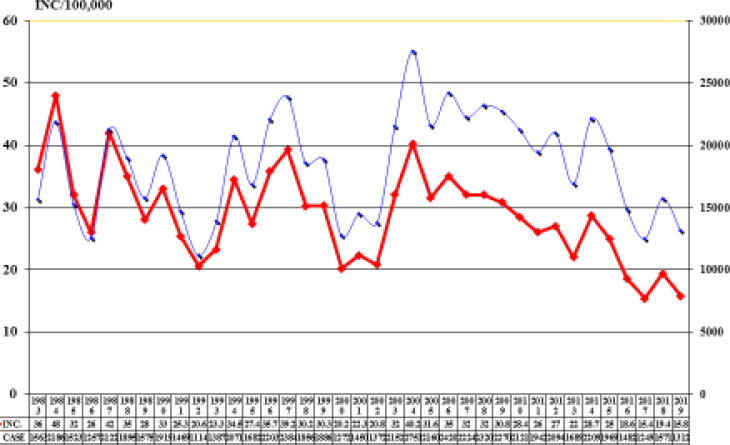
Although the Leishmania control program began in 1977, the incidence of the disease has dropped dramatically since 2008 when the new cutaneous leishmaniasis control program have been implemented. Although in some areas the incidence of the disease increased, but the implementation of the new program has reduced the number of cases, in order to continue reducing the disease, permanent support for the control programs is needed.
Keywords: Human cutaneous leishmaniasis, Surveillance, Iran
Introduction
Leishmaniasis are worldwide parasitic infectious diseases caused by protozoa of Leishmania genus which among them, approximately 20 species are pathogenic for humans (1–2).
Natural transmission to mammalian hosts is usually by the bite of female Phlebotomus or Lutzomya sandflies depending on geography (1). There are three main clinical manifestations with different degrees of severity on the species of parasite involved and elicited host immune responses. These features including cutaneous, mucocutaneous and visceral (1, 3–4). Currently, World Health Organization (WHO) lists leishmaniasis amongst the nine most important tropical and subtropical diseases which has been reported in all continents except Oceania (1, 3). In 2018, 92 countries or territories were considered endemic for, or had previously reported cases of CL. Today more than 1 billion people live in areas endemic for leishmaniasis and are at risk of infection. Cutaneous leishmaniasis (CL) is the most common form of leishmaniasis and causes skin lesions, mainly ulcers, on exposed parts of the body, leaving life-long scars and serious disability or stigma. About 95% of CL cases occur in the Americas, the Mediterranean basin, the Middle East and Central Asia. In 2018 over 85% of new CL cases occurred in 10 countries: Afghanistan, Algeria, Bolivia, Brazil, Colombia, Iran (Islamic Republic of), Iraq, Pakistan, the Syrian Arab Republic and Tunisia. It is estimated that between 600000 to 1 million new cases occur worldwide annually (5–6). Cutaneous leishmaniasis (CL) is a vector borne disease predominantly found in tropical and subtropical countries. It is an important infectious disease in the Eastern Mediterranean countries, including Iran. In the Middle East, cutaneous form is more common than visceral leishmaniasis (VL), and roughly 70–75% of CL incidence is reported from six countries: Afghanistan, Algeria, Brazil, Colombia, Iran (Islamic Republic), and the Syrian Arab Republic (7–11). Some vector borne diseases are endemic in Iran and neighboring countries, but the most I important of them is leishmaniasis (12). Researchers in Iran have conducted several epidemiological studies on leishmaniases since 1941 (5). CL is neglected tropical diseases and cause by various types of intracellular protozoan species of the genus Leishmania. Iran is endemic for old world CL and CL is one of the differential diagnosis for chronic skin diseases (5–6). Two type of CL is endemic in Iran as Zoonotic Cutaneous Leishmaniasis (ZCL) and Antheroponotic Cutaneous Leishmaniasis (ACL). ZCL is causes by Leishmania major and ACL is cause by Leishmania tropica. Main type the disease (more than 85%) is ZCL in Iran (5). Phlebotomus papatasi has been identified as main vector for ZCL in different parts of Iran (8, 13, 14) and also the rodents of Rhombomys opimus, Meriones libycus, Tatera indica, Nesokia indica, and Meriones hurrianae gerbils are repeatedly reported to be infected with L. major in different endemic foci of ZCL and act as reservoirs (8, 13, 15–16). In some different places of 18 endemic provinces transmitting the ZCL especially in rural areas. Phlebotomus sergenti as well as humans and dogs serve as the vectors and reservoirs of ACL (8, 13). Three main district that where transmitting the ACL are Mashhad (in Khorasan Province), Kerman and Bam (in Kerman Province) that almost all of cases in this districts are ACL, except traveled cases. Although in some cities a small number of ACL are transmited as Neyshaboor, Sabzevar, Taybad, Ghom, Shiraz, Isfahan, Yazd, Kashan, Zahedan and Abadan districts. Dependent to national guideline, diagnosis the cases dependent to epidemiological criteria, clinical criteria and laboratory test including confirmation of amastigote forms of Leishmania parasites using direct examination with light microscope with high magnification (1000X), and conduct the standard treatment for confirmed cases, these activities needs for surveillance and CL control (17–19). Based on description of the legal activities of the Ministry of Health and Medical Education In Iran for control the diseases (20) as CL, stablished the diagnostic and treatment centers in endemic districts from 2008, in this centers available facilities for Giemsa stain and medicine for diagnosis suspected cases and standard treatment the cases free of charge dependent to CL national guide line. And also the effective reservoir and vector control and training population about personal protection and intersectoral cooperation has been explained in national guideline (19, 21). Despite the implementation of an effective program for controlling CL in Iran the burden of the diseases are still high in some areas of country (22). Due to strengthen activities for CL control in Iran, WHO supported the implementation of the training courses for health staff in Eastern Mediterranean Region countries (23). Many studies have been conducted on the causes of the spread, increase and outbreak of CL in Iran, which have shown that vegetation cover, climatic factors, disasters and population movement play an important roles in this regard (24–29). In addition, to control the disease while taking special measures in native areas, it is very important to identify high-risk areas to prevent the spread of the disease (30–32).
Materials and Methods
Study area
The CL surveillance system in Iran conducting in all provinces and coverage all population in endemic and non-endemic areas. The population of Iran is 83,992,949 (2019) and the area of Iran is 1,873,959 square kilometers. 18 out of 31 provinces are endemic for CL and around 75% of population in Iran are leaving in CL endemic areas. CL is one of the reporting diseases from 1977 and the surveillance system covered this disease in Iran. There are surveillance system for case finding, recording and reporting and treatment the cases, the strategic plan for CL control, as inter sectoral cooperation, community education, reservoir control, and vector control. CL is endemic in 18 provinces in Iran and some cases diagnosed from non-endemic provinces that had travel to endemic provinces.
Study design
A retrospective, cross-sectional study was carried out using data from the national leishmaniasis surveillance system. The data used in this study include data that collected in Centre for communicable Diseases Control (CDC) in ministry of health and medical education in Iran. The portal online computerized recording system stablished from 2000 for record the information of CL cases in district level, And the information of recorded cases in 2019, evaluate in 2020. The Iranian CDC in Ministry of Health and Medical education is responsible for surveillance and collection of data on communicable diseases from various districts of the country. Leishmaniasis surveillance and control, the Information about CL have been collected over 35 years, from 1983 to 2000 data were recorded and reported in paper format and from 2000 to 2006 based on Epi-info, version 6 software. Online reporting was launched in 2006 for limited districts and after one years the data including microscopical exam as potential tool for the confirmation of all reported cases were gathered online in all districts. The data collected for this survey obtained from surveillance system and include; seasonal trend, individual clinical manifestation, geographical information, laboratory data and treatment methods for all cases of CL. Case definitions were based on the national CL control guideline (19). The zoonosis control department was subset of the center for communicable diseases control and information for CL were accessed and analyzed by this department. Ethical approval for the study was obtained from the national leishmaniasis expert committee.
Statistical analysis
The data were analyzed using Microsoft Excel 2013 at the zoonosis control management in Centre for communicable Diseases Control (CDC).
Results
Iran has been reported an endemic area for CL in the world. In this Report, we describe some CL indicators in Iran. After the earthquake in bam district in 2003 number of cases increase from average 400 cases per year before earthquake to 3125 cases in 2006, in this district in 2006 with support the national committee revised the national plan for surveillance and control the CL in Iran, and stab-lished in Bam district. After 1 year evaluated the results of activities and the national plan conducted in all provinces. The main activities in national plane are: education health personals, intersectoral cooperation, established leishmaniasis diagnosis and treatment center in endemic districts, community education, environment sanitation, vector control and reservoir control. In CL diagnosis and treatment centers, the facilities for diagnosis and medicine for treatment the cases stablished.
Table 1.
Prevalence of CL in different provinces of Iran
| No | Endemic Provinces | Geographical zones | CL Number | CL Incidence rate/100000 |
|---|---|---|---|---|
| 1 | Semnan | Center, East | 719 | 95.9 |
| 2 | Ilam | West, South | 470 | 78.7 |
| 3 | Golestan | North, East | 1188 | 60.9 |
| 4 | Isfahan | North, Center | 3127 | 59.1 |
| 5 | Fars | All | 2002 | 40.0 |
| 6 | Khorasan-Shomali | South | 214 | 24.0 |
| 7 | Khorasan-Razavi | All | 1581 | 23.4 |
| 8 | Yazd | All | 260 | 21.4 |
| 9 | Ghom | Center | 293 | 21.3 |
| 10 | Khoozestan | All | 1013 | 20.7 |
| 11 | Kerman | Center, South | 565 | 17.1 |
| 12 | Systan va Bloochestan | East, South, West | 357 | 12 |
| 13 | Hormozgan | West, South, West | 160 | 8.4 |
| 14 | Kermanshah | West | 117 | 5.9 |
| 15 | Khorasan-Jonoobi | East | 39 | 4.8 |
| 16 | Lorestan | South-west | 69 | 3.8 |
| 17 | Tehran | South | 434 | 3.1 |
| 18 | Booshehr | All | 28 | 2.3 |
Trend and distribution
In 2019, 13124 CL cases were reported in Iran (Incidence rate 15.8 cases per 100000 population). In 2008, 23202 cases reported (Incidence rate 32 cases per 100000 population) and in this year stablished new surveillance system. And dramatically decreased the cases during 12 years. During this year’s we had two pike in 2014 with 22099 cases and in 2018 with 15714 cases (Fig. 1).
Fig. 1.
Trend of cutaneous leishmaniasis Iran 1983–2019
In 2019, 12636 (96%) of cases reported from 18 endemic provinces and 488 (4%) of cases reported from non-endemic provinces that have traveled to endemic provinces. More cases reported from Isfahan Province in center in Iran with 3127 cases and 51.2 incidence rate per 100000. But highest incidence rate was in Semnan Province with 95.9 per 100000 population and 719 cases. CL is endemic in 18 out of 31 provinces and in tab 1 show the number and incidence rate per 100000 of CL in endemic provinces.
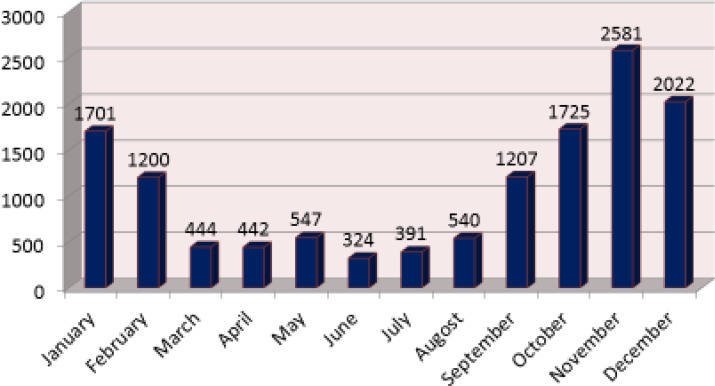
Seasonal aspects
Because more than 85% of cases are Zoonotic in Iran more cases reported from September to December (Fig. 2).
Fig. 2.
Number of C.L cases by month 2019
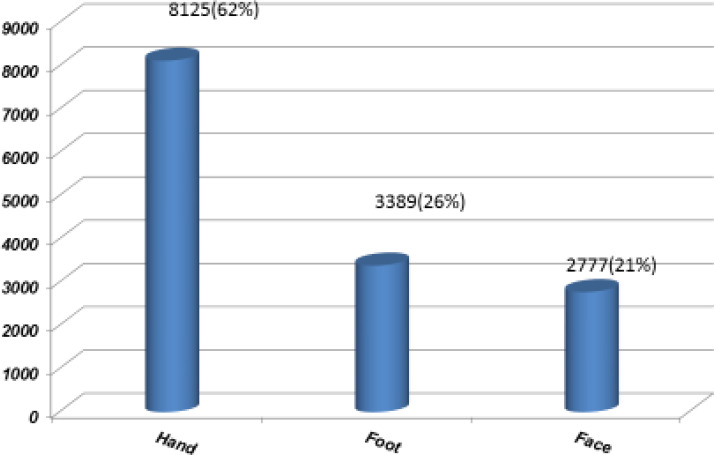
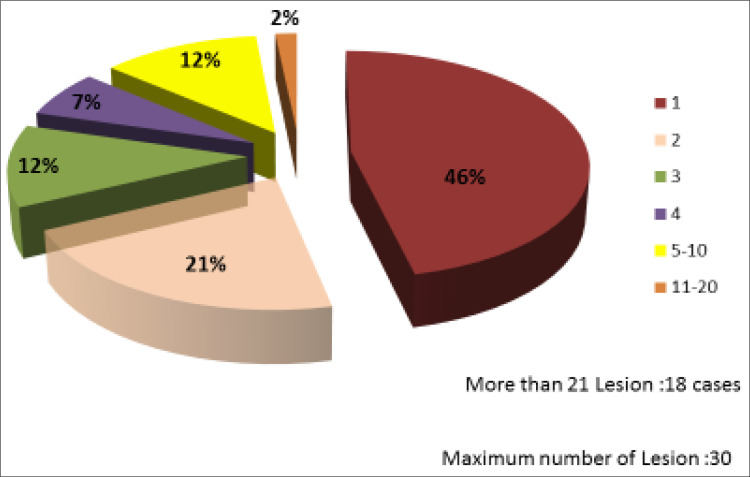
Clinical aspects
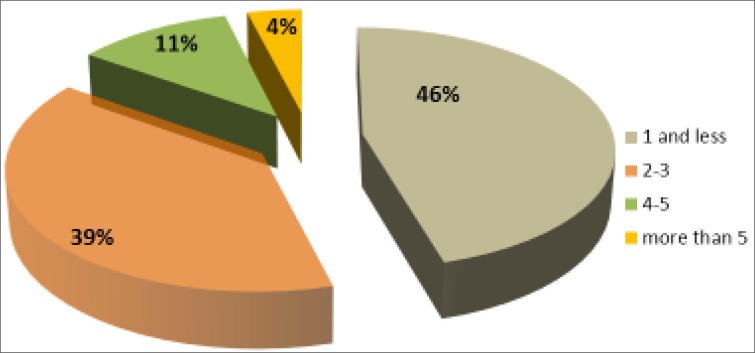
The cutaneous lesions were mostly on the hand (62%) and foot (26%) and face (21%). In 1177 cases (9%) two or more organ were infected (Fig. 3). In 46% of cases had one lesions, and 54% of cases had two or more lesions, 18 cases had more than 21 cases. And maximum number of lesions was 30 lesions (Fig. 4).
Fig. 3.
Location of C. Leishmaniasis lesions Iran 2019
Fig. 4.
Number of C. Leishmaniasis lesions Iran 2019
Diagnosis the cases in early stage is very important because response to treatment is more effective. And the scar gets smaller. The Fig. 5 show the maximum size of the lesions in CL cases and 85% have the 3cm or bellows the diameter.
Fig. 5.
Size of C. Leishmaniasis lesions Iran 2019
Conclusions
Our study has provided available information on CL in 2019 in Iran. The review shows CL is endemic in various parts of 18 provinces in Iran and also explain the main clinical manifestation. Using national CL control guideline was effective to decreasing dramatically number of cases in recent years but Population how are leaving in endemic areas are at risk and also population in other areas is also at risk to take infection if travel to endemic areas. Activities for control the CL in national guideline needs to fallows but it dependent to budget, and unfortunately it is not possible to cover all endemic areas. Also in non-endemic areas with appropriate climate factors and plants conditions and environment sanitation, that increase population of rodent and sand-flies are high risk areas that CL present in this non endemic places. Therefore, Strong support is needed for the implementation of the national CL guideline to prevent and control CL spreading and outbreaks. In the other hand the physician have to more attention to CL in differential diagnosis in skin lesions.
Acknowledgments
The author wish to acknowledge all Health staff in the provincial and district levelthat their activities do the control of CL in Iran. The author declare that they have no competing interests.
References
- 1.Torres-Guerrero E, Quintanilla-Cedillo MR, Ruiz-Esmenjaud J, Arenas R. (2017) Leishmaniasis: a review. F1000Res. 6: 750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oryan A, Akbari M. (2016) Worldwide risk factors in leishmaniasis. Asian Pac J Trop Med. 9(10): 925–932. [DOI] [PubMed] [Google Scholar]
- 3.Salam N, Al-Shaqha WM, Azizi A. (2014) Leishmaniasis in the Middle East: incidence and epidemiology. Plos Negl Trop Dis. 8(10): e3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Postigo JAR. (2010) Leishmaniasis in the world health organization eastern mediterranean region. Int J Antimicrob Agents. 36(S Suppl1): S62–S65. [DOI] [PubMed] [Google Scholar]
- 5.Nadim A, Javadian E, Mohebali M, Momeni A. (2008) Leishmania parasite and leishmaniasis, Markaze Nashre Daneshgahi Publication. [Google Scholar]
- 6.World Health Organization (WHO) (2020) Leishmaniasis. Available at: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis/.
- 7.World Health Organization (WHO) (2020) Leishmaniasis. Available at: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis/.
- 8.Holakouie-Naieni K, Mostafavi E, Boloorani AD, Mohebali M, Pakzad R. (2017) Spatial modeling of cutaneous leishmaniasis in Iran from 1983 to 2013. Acta Trop. 166: 67–73. [DOI] [PubMed] [Google Scholar]
- 9.Heydarpour F, Sari AA, Mohebali M, Shirzadi M, Bokaie S. (2016) Incidence and disability-adjusted life years (Dalys) attributable to leishmaniasis in Iran, 2013. Ethiop J Health Sci. 26(4): 381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization (2014) Manual for case management of cutaneous leishmaniasis in the WHO Eastern Mediterranean Region. WHO Regional Publications, Eastern Mediterranean Series (35). Available at: https://apps.who.int/iris/handle/10665/120002. [Google Scholar]
- 11.World Health Organization (2002) An increasing risk factor for leishmaniasis (Weekly Epidemiological Record. WHO Press. 77(44): 365–370. [Google Scholar]
- 12.Shirzadi MR. (2019) Entomological studies on the mosquito born diseases in Iran: an up-to-date. Insights Biomed. 4(2): 10. [Google Scholar]
- 13.Hanafi-Bojd AA, Yaghoobi-Ershadi MR, Haghdoost AA, Akhavan AA, Rassi Y, Karimi A. (2015) Modeling the distribution of cutaneous leishmaniasis vectors (Psychodidae: Phlebotominae) in Iran: a potential transmission in disease prone areas. J Med Entomol. 52 (4): 557–565. [DOI] [PubMed] [Google Scholar]
- 14.Nezemzadeh-Ezhiyteh H, Mirhendi H, Jafari R, Veysi A, Rassi Y, Oshaghi MA, Arandian MH, Abdoli H, Bahrami S, Zahraei-Ramazani AR, Fadaei R, Ramezanpoor J, Farsi M, Aminian K, Saeidi Z, Yaghoobi-Ershadi MR, Akhavan AA. (2021) An eco-epidemiological study on zoonotic cutaneous leishmaniasis in central Iran. Iran J Public Health. 50(2): 350–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akhoundi M, Mohebali M, Asadi M, Mahmodi MR, Amraei K, Mirzaei A. (2013) Molecular characterization of Leishmania spp. in reservoir hosts in endemic foci of zoonotic cutaneous leishmaniasis in Iran. Folia Parasitol (Praha). 60 (3): 218–24. [DOI] [PubMed] [Google Scholar]
- 16.Gholamrezaei M, Mohebali M, Hanafi-Bojd AA, Sedaghat MM, Shirzadi MR. (2016) Ecological Niche Modeling of main reservoir hosts of zoonotic cutaneous leishmaniasis in Iran. Acta Trop. 160: 44–52. [DOI] [PubMed] [Google Scholar]
- 17.Goto H, Lauletta Lindoso JA. (2010) Report of meeting of the WHO Exper Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010. [Google Scholar]
- 18.World Health Organization (WHO) Control of Leishmaniasis (2010) Report of meeting of the WHO Exper Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010. [Google Scholar]
- 19.Shirzadi MR. (2012) Cutaneous leishmaniasis control guideline in Iran. Tehran: Zoonoses Control Department, Center for Communicable Diseases Control, Ministry of Health and Medical Education. Available at: https://pubmed.ncbi.nlm.nih.gov/26750164/ [Google Scholar]
- 20.Shirzadi MR, Esfahani SB, Mohebali M, Yaghoobi-Ershadi MR, Gharachorlo F, Razavi MR. (2015) Epidemiological status of leishmaniasis in the Islamic Republic of Iran, 1983–2012. East Mediterr Health J. 21(10): 736–742. [DOI] [PubMed] [Google Scholar]
- 21.Piroozi B, Moradi G, Alinia C, Mohamadi P, Gouya MM, Nabavi M, Gharachorloo F, Khademerfan MB, Shirzadi MR. (2019) Incidence, Burden, and Trend of Cutaneous Leishmaniasis over Four Decades in Iran. Iran J Public Health. 48(1): 28–35. [Google Scholar]
- 22.Yaghoobi-Ershadi MR, Akhavan AA, Shirzadi MR, Rassi Y, Khamesipour A, Hanafi-Bojd AA, Vatandoost H. (2019) Conducting international diploma course on leishmaniasis and its control in the islamic republic of Iran. J Arthropod Borne Dis. 13(3): 234–242 [PMC free article] [PubMed] [Google Scholar]
- 23.Mollalo A, Alimohammadi A, Shahrisvand M, Shirzadi MR, Malek MR. (2014) Spatial and statistical analyses of the relations between vegetation cover and incidence of cutaneous leishmaniasis in an endemic province, northeast of Iran. Asian Pac J Trop Dis. 4(3): 176–180. [Google Scholar]
- 24.Shirzadi MR, Mollalo A, Yaghoobi-Ershadi MR. (2015) Dynamic Relations between Incidence of Zoonotic Cutaneous Leishmaniasis and Climatic Factors in Golestan Province. J Arthropod Borne Dis. 9(2): 148–160. [PMC free article] [PubMed] [Google Scholar]
- 25.Nezamzadeh-ezhiyeh H, Mirhendi H, Jafari R, Veysi A, Rassi Y, Oshaghi MA, Arandian MH, Abdoli H, Bahrami S, Zahraei-Ramazani AR, Fadaei R, Ramezanpoor J, Farsi M, Aminian K, Saeidi Z, Yaghoobi-Ershadi MR, Akhavan AA. (2021) An eco-epidemiological study on zoonotic cutaneous leishmaniasis in central Iran. Iran J Public Health. 50(2): 350–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gholamrezaei M, Mohebali M, Hanafi-Bojd AA, Sedaghat MM, Shirzadi MR. (2016) Ecological niche modeling of main reservoir hosts of zoonotic cutaneous leishmaniasis in Iran. Acta Trop. 160: 44–52. [DOI] [PubMed] [Google Scholar]
- 27.Sharifi I, Nakhaei N, Aflatoonian MR, Hakimi Parizi M, Fekri AR, Safizadeh H, Shirzadi MR, Gooya MM, Khamesipour A, Nadim A. (2011) Cutaneous Leishmaniasis in Bam: A Comparative Evaluation of Preand Post-Earthquake Years (1999–2008). Iran J Public Health. 40(2): 49–56. [PMC free article] [PubMed] [Google Scholar]
- 28.Aflatoonian MR, Sharifi I, Aflatoonian B, Shirzadi MR, Gouya MM, Kermanizadeh A. (2016) A Review of impact of bam earthquake on cutaneous leishmaniasis and status: epidemic of old foci, emergence of new foci and changes in features of the disease. J Arthropod Borne Dis. 10(3): 271–280. [PMC free article] [PubMed] [Google Scholar]
- 29.Ramezankhani R, Sajjadi N, Esmaeilzadeh RN, Jozi SA, Shirzadi MR. (2018) Climate and environmental factors affecting the incidence of cutaneous leishmaniasis in Isfahan, Iran. Environ Sci Pollut Res Int. 25(12): 11516–11526. [DOI] [PubMed] [Google Scholar]
- 30.Shirzadi MR, Javanbakht M, Jesri N, Saghafipour A. (2019) spatial distribution of cutaneous leishmaniasis cases referred to health centers of three khorasan provinces in iran using geographical information system. Iran J Public Health. 48(10): 1885–1892. [PMC free article] [PubMed] [Google Scholar]
- 31.Aflatoonian MR, Sharifi I, Babaei Z, Sharifi F, Keyhani A, Salarkia E, Khosravi A, Khamesipour A, Mohebali M, Nadim A, Bamorovat M. (2019) Emerging epidemics of cutaneous leishmaniasis in iran: operational aspects, management and implemented control approaches. J Med Microbiol Infect Dis. 7(3): 52–60. [Google Scholar]
- 32.Doroodgar A, Sadr F, Razavi MR, Doroodgar M, Asmar M. (2015) A new focus of zoonotic cutaneous leishmaniasis in Isfahan Province, Central Iran. Asian Pac J Trop Dis. 5(Suppl 1): S54–S58. [Google Scholar]