Abstract
Prescription rates of second-generation antipsychotics (SGAs) are rapidly increasing for non-indicated (i.e., off-label) usage. SGAs used for approved indications are associated with significant metabolic adverse effects, including weight gain. The objective of this systematic review and meta-analysis is to evaluate the metabolic adverse effects of SGA use for off-label management of psychiatric illnesses in the adult population. We performed a systematic database search to identify randomized controlled trials (RCTs) that reported on weight and other metabolic outcomes with off-label use of SGAs among adults. Thirty-eight RCTs met inclusion criteria for this review; 35 of these studies, with a total of 4930 patients, were included in the quantitative meta-analysis. Patients treated with olanzapine, risperidone, and quetiapine were more likely to report weight gain as a side effect and experience clinically significant (≥7%) weight gain compared to those treated with a placebo. Among studies that reported weight as a continuous outcome, olanzapine was associated with significantly greater weight gain across all disorders (mean difference (MD) = 3.24 kg, 95% CI: 2.57–3.90 p = 0.001, N = 12 studies). Similar trends were noted with quetiapine and risperidone. A meta-regression analysis revealed a positive dose-response association between olanzapine dose and weight gain (regression coefficient: 0.36, p = 0.001). This review demonstrates that off-label use of SGAs, and particularly olanzapine, is associated with significant weight gain among adult patients. Our findings are concerning given the widespread off-label use of SGAs. Further studies are required to better understand the effects of off-label SGA use on other metabolic parameters. The study was registered with the PROSPERO international database of prospectively registered systematic reviews (PROSPERO #143186).
Subject terms: Psychosis, Schizophrenia
Introduction
Second-generation antipsychotics (SGAs) are approved for the treatment of schizophrenia, bipolar disorder, irritability in autism spectrum disorders, major depressive disorder, and Tourette’s Syndrome. Unfortunately, these medications are indisputably associated with significant metabolic adverse effects [1, 2]. Although clozapine and olanzapine confer the greatest risk [3, 4], no single antipsychotic (AP) drug can be considered metabolically neutral, and this is particularly true in previously AP-unexposed populations [5]. Guidelines for metabolic monitoring in patients receiving APs have been developed for clinicians to follow [6, 7]; however, uptake has been less than optimal.
Prescription trends around the world indicate that APs are being used at increasingly high rates [8, 9]. Concerningly, the most rapid increases in prescription patterns have been attributed to use in non-regulatory body-approved (i.e., off-label) indications where clinical evidence of efficacy and safety is less certain [8, 10]. Off-label use includes populations with attention deficit and hyperactivity disorder (ADHD), anxiety disorders, dementia, eating disorders (EDs), insomnia, obsessive-compulsive disorder (OCD), personality disorders, post-traumatic stress disorder (PTSD), and substance use disorders (SUDs), among others [10]. Despite the well-established association between AP use and significant metabolic adverse effects [1, 3, 4, 11], existing studies of SGAs during off-label use have largely focused on efficacy and comparative effectiveness and do not systematically evaluate metabolic adverse effects. This may lead clinicians to assume that off-label use carries less metabolic risk compared to the higher dose, longer-term exposure often used in approved indications [12]. However, a lack of metabolic data corroborating this assumption means that accurate risk-benefit analysis cannot be carried out. This systematic review and meta-analysis aimed to fill this gap by evaluating the metabolic adverse effects associated with the off-label use of SGAs in the adult population.
Methods
A protocol for this systematic review was designed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology and reporting standard. The study was submitted to the PROSPERO international database of prospectively registered systematic reviews on July 19, 2019 (PROSPERO #143186).
Inclusion and exclusion criteria
Studies were screened and selected according to the following inclusion criteria:
randomized placebo-controlled trial,
adults (age 18–65) with at least one of the following off-label indications: ADHD, OCD, anxiety disorders, insomnia, personality disorders, PTSD, SUD, pathological gambling disorder, and other impulse control disorders.
SGAs: amisulpride, aripiprazole, asenapine, blonanserin, brexpiprazole, cariprazine, clozapine, iloperidone, lurasidone, melperone, olanzapine, paliperidone, perospirone, quetiapine, remoxipride, risperidone, sertindole, sulpiride, and ziprasidone.
Measurement of metabolic outcomes, including weight, Body Mass Index (BMI), waist circumference (WC), fasting plasma glucose (FG), glycated hemoglobin (HbA1c), total, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol, triglyceride (TG), and blood pressure (BP).
We excluded studies conducted in patients that were either under 18 or over 65 years of age, had dementia or an eating disorder, or included pregnant women, due to the differing body composition, physiology, and metabolism in these populations. Studies of individuals with approved indications for SGAs, including schizophrenia, schizoaffective disorder, bipolar disorder, treatment-resistant major depressive disorder, and irritability in autism spectrum disorders were also excluded.
Search strategy
We conducted a systematic search of the literature in accordance with PRISMA recommendations [13]. We identified relevant RCTs that met the predefined inclusion criteria by searching the following sources from inception to March 2021: MEDLINE, EMBASE, PsychINFO, Cochrane CENTRAL, CINAHL, ClinicalTrials.gov, and The ICTRP Search Portal. The reference lists of included studies and reviews were hand-searched for additional studies. An attempt to retrieve unpublished data was made by contacting corresponding authors and experts in the field by email on at least two occasions. Details of the search strategy are found in Supplementary Table 1.
Study selection
Five authors independently screened the title and abstract of all identified studies (SB, VT, RA, ES, NS). The full texts of selected studies were then reviewed at the full-text level by six authors (SB, VT, RA, WM, ES, NS). Two screeners were assigned per article. Any disagreements were resolved by re-checking source papers and discussion between all authors.
Data extraction
Standardized data extraction forms were developed with pre-specified variables of interest for use by authors. All data were extracted by one of six authors (SB, VT, RA, WM, ES, NS) and then independently checked by two authors (ES, NS). These same authors reviewed and resolved any inconsistencies, with input from the authorship group as required. Corresponding authors were contacted if data could not be extracted in a usable form from the published paper.
Bias assessment
The Cochrane Risk of Bias (RoB) tool was used for the assessment of bias in the context of our outcomes of interest (metabolic adverse events). RoB assessment was conducted by four independent reviewers (RA, WM, ES, NS), with two individuals assigned per study. Conflicts were resolved through discussion and agreement reached by all authors. Studies were considered high risk of bias if three or more of the domains were labelled as ‘high risk’.
Outcome measures
Our primary outcome of interest was the difference in weight change following treatment with SGA versus placebo. Our secondary outcomes included weight gain reported dichotomously (either as an adverse effect or as a ≥7% increase from baseline) and other metabolic adverse effects including change in BMI, WC, FG, HbA1c, total-, HDL-, and LDL- cholesterol, TGs and BP.
Synthesis of results
Quantitative data from all studies were pooled in a random-effects meta-analysis using Review Manager 5.3. Mean differences were calculated for continuous data and odds ratios for dichotomous data. We combined data from studies that reported end-point weight and changes in weight between time points. We analyzed the effect of SGA use on each metabolic outcome and completed analyses stratified by SGA and diagnosis subgroups. Heterogeneity was assessed using the I2 statistic. Publication bias for comparisons with 10 or more included studies was assessed using funnel plots. A meta-regression was performed using STATA 16 (Statistics/Data Analysis http://www.stata.com).
Additional analyses
Two sensitivity analyses to explore heterogeneity were performed for the primary outcome, excluding studies: (1) with a high risk of bias, and (2) those reporting only endpoint data. A subgroup analysis comparing weight change between patients not previously exposed to APs (i.e., AP-naïve) and those who had prior AP exposure or in whom previous AP exposure was unclear was also conducted.
Meta-regressions were performed to determine the association between average and cumulative dose with weight gain for comparisons with at least ten studies. The cumulative dose was calculated by multiplying the dose by study duration.
Results
Study selection
Our initial search identified 25,704 results. Following title and abstract screening, 753 studies were assessed for full-text eligibility. A total of 38 studies met inclusion criteria and were included in the review; 35 studies were included in the quantitative meta-analysis while the remaining three studies were described qualitatively. Fig. 1 summarizes the study selection and exclusion process. Characteristics of the included trials are found in Supplementary Table 2.
Fig. 1. PRISMA flow chart of included studies.
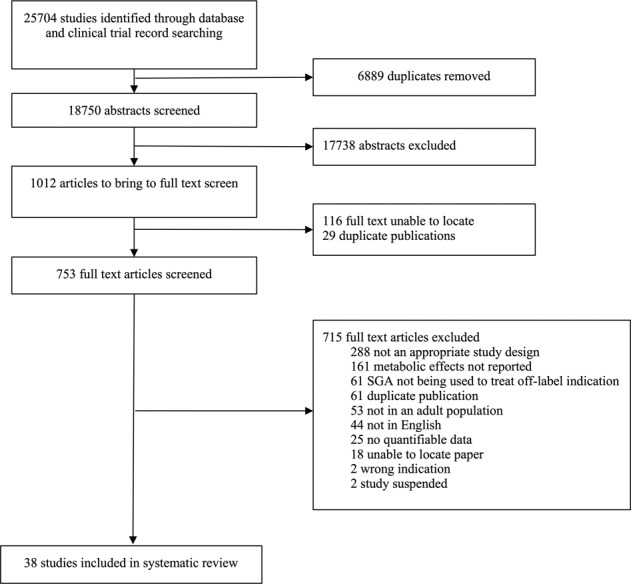
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of included studies.
Study characteristics
The 38 RCTs included in this review were published between 2001 and 2021 across a variety of geographic locations. Of these studies, 15 trials examined olanzapine, 14 examined quetiapine, 6 examined risperidone, and one each examined aripiprazole, paliperidone, and ziprasidone. Details of these studies can be found in Supplementary Table 2. A summary of the risk of bias assessment can be found in Supplementary Figs. 1 and 2.
Meta-analysis of weight gain by off-label indication of SGAs
MD refers to the calculated mean difference and CI represents the confidence interval. N indicates the number of studies, while n indicates sample size (i.e., number of participants).
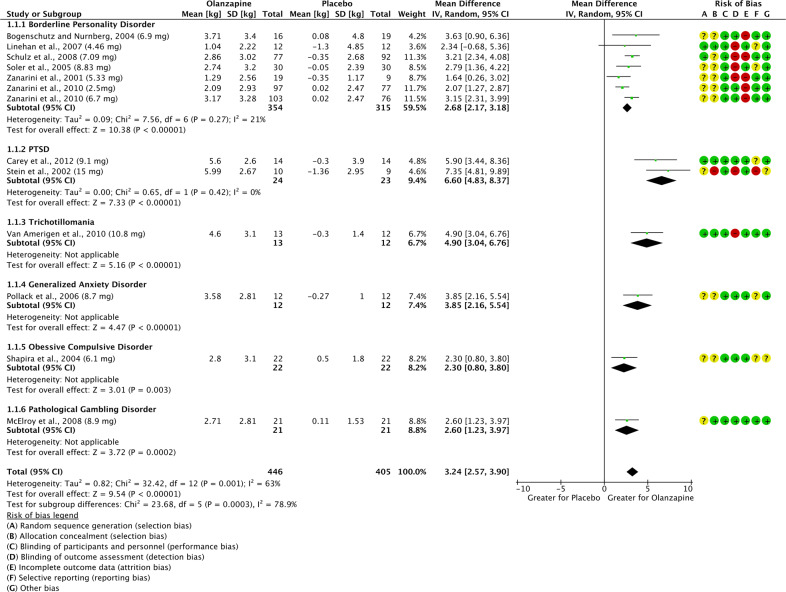
Change in Weight: Olanzapine vs. Placebo (Fig. 2)
Fig. 2. Change in weight on olanzapine vs. placebo.
Forest plot and risk of bias assessment for weight comparison on olanzapine vs. placebo.
Twelve studies (pooled n = 851) examined weight gain associated with the off-label use of olanzapine in patients with borderline personality disorder (BPD; N = 6) [14–19], PTSD (N = 2) [20, 21], trichotillomania (N = 1) [22], general anxiety disorder (GAD; N = 1) [23], OCD (N = 1) [24], and pathological gambling (N = 1) [25]. One study had two olanzapine groups with different doses; these groups were reported independently in the comparison according to dose [19]. The average study duration was 12 weeks; the dose of olanzapine ranged from 2.5 mg/day to 20.0 mg/day, with a mean dose of 7.72 mg/day. Across all diagnoses, olanzapine was associated with significantly greater weight gain (MD = 3.24 kg, 95% CI: 2.57–3.90, p < 0.00001, I2 = 63%). The difference remained significant when grouped by individual diagnoses, with PTSD conferring the largest mean difference (MD = 6.60 kg, 95%CI: 4.83–8.37, p < 0.00001, I2 = 0%, N = 2, n = 47). Results of the subgroup analysis are displayed in Fig. 2.
Sensitivity analyses
-
(i)
No studies reported only endpoint data.
-
(ii)
One study (in a population with PTSD) was identified as having a high risk of bias [21]. When removed, weight gain was still significantly greater with olanzapine (n = 829, MD = 2.98 kg, 95% CI: 2.43–3.54, p < 0.00001, I2 = 47%).
Subgroup analysis (previous AP exposure)
Two studies [18, 22] indicated prior AP exposure as an exclusion criterion. Subgroup analysis did not reveal a significant difference in weight gain between AP-naïve patients compared to those with previous or unspecified AP exposure (p = 0.98, I2 = 0%; Supplementary Fig. 3).
-
2.
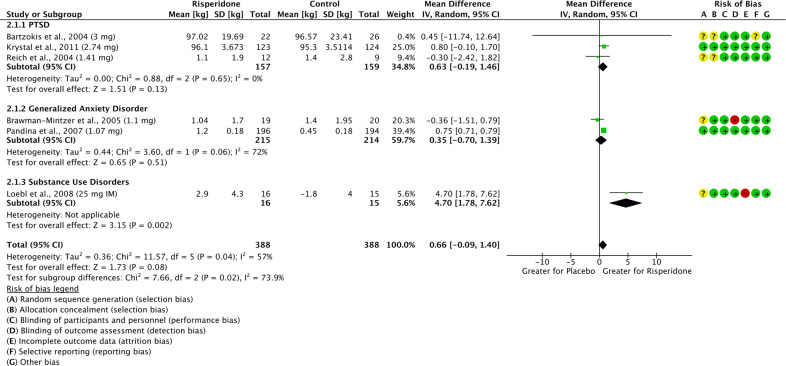
Change in Weight: Risperidone vs. Placebo (Fig. 3)
Fig. 3. Change in weight on risperidone vs. placebo.
Forest plot and risk of bias assessment for weight comparison on risperidone vs. placebo.
Six studies (pooled n = 776) examined weight gain associated with the off-label use of risperidone in patients with PTSD (N = 3) [26–28], GAD (N = 2) [29, 30], and SUD (N = 1) [31]. Three studies included multiple risperidone groups with different doses and were reported independently in the comparison [32–34]. The average study duration was 10 weeks; the average dose of risperidone ranged from 0.5–8 mg/day, with a mean dose of 1.86 mg/day; one study used 25 mg intramuscular risperidone every two weeks (equivalent to 2–3 mg/day [35]). Risperidone did not differ significantly from placebo (MD = 0.66 kg, 95% CI: −0.09 to 1.40, p = 0.08, I2 = 57%). However, subgroup analysis revealed that the effect of risperidone on weight depends on diagnosis (p = 0.02, I2 = 73.9%), with a significant difference in weight gain between risperidone and placebo only being reported for SUD (MD = 4.70 kg, 95% CI: 1.78–7.62, p = 0.002, N = 1, n = 31) (Fig. 3).
Sensitivity analyses
-
(i)
One study [26] reported endpoint data only. The findings remained unchanged after removing this study (n = 728, MD = 0.66 kg, 95% CI: −0.12 to 1.45, p = 0.10, I2 = 65%).
-
(ii)
No studies were identified as having a high risk of bias.
Subgroup analysis (previous AP exposure)
Three studies [26, 27, 30] indicated prior AP exposure as an exclusion criterion. Subgroup analysis did not reveal a significant difference in weight gain between AP-naïve patients compared to patients with unclear or prior AP exposure (p = 0.65, I2 = 0%; Supplementary Fig. 4).
-
3.
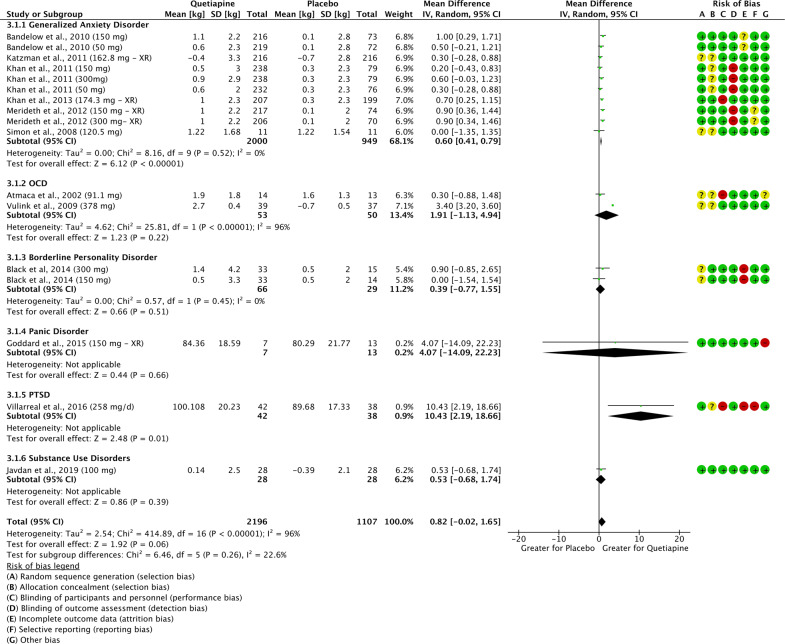
Change in Weight: Quetiapine vs. Placebo (Fig. 4)
Fig. 4. Change in weight on quetiapine vs. placebo.
Forest plot and risk of bias assessment for weight comparison on quetiapine vs. placebo.
Twelve studies (pooled n = 3303) examined weight gain associated with the off-label use of quetiapine in patients with GAD (N = 6) [32–34, 36–38], OCD (N = 2) [39, 40], BPD (N = 1) [41], panic disorder (N = 1) [42], PTSD (N = 1) [43], and SUD (N = 1) [44]. The average study duration was 12 weeks; the average dose of quetiapine ranged from 25 mg/day to 800 mg/day, with a mean dose of 178.5 mg/day. Across all diagnoses, there was no significant difference in weight gain between participants treated with quetiapine compared to placebo (MD = 0.82 kg, 95% CI: −0.02 to 1.65, p = 0.06, I2 = 96%). Subgroup analysis indicated that the effect of quetiapine does not differ between diagnoses (p = 0.26, I2 = 22.6%). Results of this subgroup analysis are displayed in Fig. 4.
Sensitivity analyses
-
(i)
Two studies [42, 43] reported endpoint data only. The findings remained unchanged after removing these studies (n = 3203, MD = 0.72 kg, 95% CI: −0.11 to 1.56, p = 0.098, I2 = 97%).
-
(ii)
One study (in a population with PTSD) was identified as having a high risk of bias [43]. Removing this study had no effect on the outcome (MD = 0.74 kg, 95% CI: −0.11 to 1.57, p = 0.09, I2 = 96%).
Subgroup analysis (previous AP exposure)
Two studies [39, 41] indicated that all patients were AP-naïve. When these were compared with studies including patients with unclear or prior AP exposure, no significant difference was found (p = 0.45, I2 = 0%; Supplementary Fig. 5).
-
4.
Change in Weight: Other SGAs vs. Placebo
Change in weight with other SGAs was only reported in two studies examining paliperidone (OCD; mean dose = 4.94 mg/day) [45] and ziprasidone (GAD; mean dose = 50.24 mg/day) [46]. In these studies, weight gain did not differ between individuals treated with either SGA compared to placebo (Paliperidone: n = 34, MD = 10.41 kg, 95% CI: −2.67 to 23.49, p = 0.12; Ziprasidone: n = 62, MD = 0.37 kg, 95% CI: −1.45 to 2.19, p = 0.69).
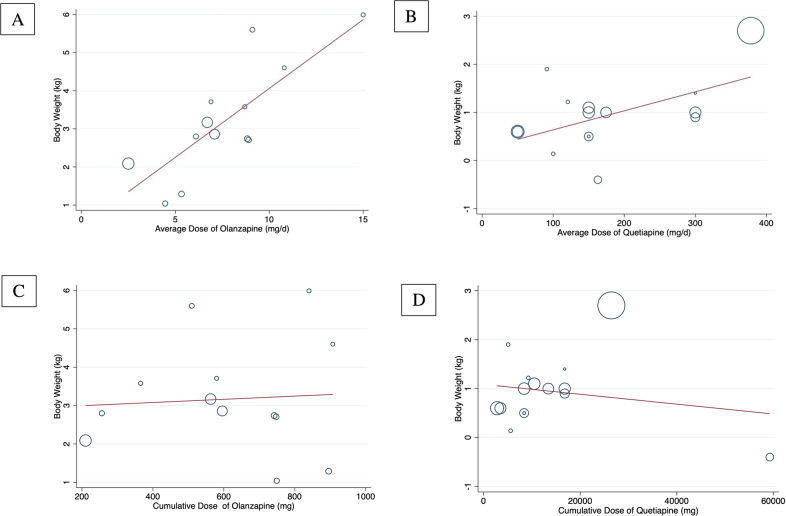
Meta-regression
The association between average AP dose and cumulative AP dose with weight gain were estimated using a random-effects meta-regression model for olanzapine and quetiapine (Fig. 5). There were insufficient studies to perform a meta-regression for risperidone. We found a significant positive association between average olanzapine dose and weight gain (meta-regression coefficient for dose = 0.36 mg, 95% CI: 0.18–0.55, p = 0.001, I2 = 54.6%) (Fig. 5A). There was no significant association between cumulative olanzapine exposure (in mg/day) and weight (Fig. 5C). There was also a small, but significant positive association between average quetiapine dose and weight gain (meta-regression coefficient for dose = 0.004 mg, 95% CI: 0.0002–0.008, p = 0.034, I2 = 91.4%), but not cumulative quetiapine exposure (in mg/day) and weight gain (Fig. 5B and D).
Fig. 5. Average dose and cumulative average dose response on weight gain with olanzapine and quetiapine.
Meta-regression scatterplots for the association between body weight and (A) average olanzapine dose (mg/day)*, (B) average quetiapine dose (mg/day)*, (C) cumulative average olanzapine dose (mg/day), (D) cumulative average quetiapine dose (mg/day). * Refers to significant associations (p < 0.05).
Meta-analysis of dichotomous weight outcomes by SGA type
Olanzapine vs. Placebo
Weight gain as an adverse effect
Ten studies (pooled n = 1182) across a wide range of diagnoses reported weight gain as an adverse effect. The mean dose of olanzapine was 7.50 mg/day (range: 2.5–20 mg/day) across 6–24 weeks of treatment. Individuals who gained weight were 6.58 times more likely to have been given olanzapine compared to placebo (95% CI: 4.06–10.67, p < 00001, I2 = 44%).
≥7% increase in weight
Three studies (pooled n = 911), one in GAD [23] and two in BPD [16, 19] reported the number of participants who experienced ≥7% increase in weight during the study. The mean dose of olanzapine was 6.25 mg/day (range: 2.5–20 mg) across 6–12 weeks of treatment. Individuals who gained ≥7% of their baseline weight were 9.33 times more likely to have been treated with olanzapine compared to placebo (95% CI: 5.63–15.46, p < 0.00001, I2 = 23%).
-
2.
Risperidone vs. Placebo
The primary outcome of mean weight gain was not statistically significant for risperidone; however, a difference was observed in dichotomous reports of weight gain.
Weight gain as an adverse effect
Only two studies (pooled n = 637), one in GAD [30] and one in PTSD [28] reported weight gain as an adverse effect. The mean dose of risperidone was 1.91 mg/day (range: 1–4 mg/day) across 4–24 weeks of treatment. Individuals who gained weight were 2.48 times more likely to have been treated with risperidone compared to placebo (95% CI: 1.31–4.70, p = 0.005, I2 = 84%).
≥7% increase in weight
No data is available to report on this outcome for risperidone.
-
3.
Quetiapine vs. Placebo
The primary outcome of mean weight gain was not statistically significant for quetiapine; however, a difference was observed in dichotomous reports of weight gain.
Weight gain as an adverse effect
Three studies (pooled n = 142), one in panic disorder [42] and two in OCD [39, 47], reported weight gain as an adverse effect. The mean dose of quetiapine was 234.3 mg/day (range: 150–450 mg/day) across 8–10 weeks of treatment. Individuals who gained weight were 4.09 times more likely to have been treated with quetiapine compared to placebo (95% CI: 1.75–9.57, p = 0.001, I2 = 41%).
≥7% increase in weight
Six studies (pooled n = 4104), five in GAD [32, 33, 36, 37, 48] and one in SUD [49] reported the number of individuals who experienced ≥7% increase in weight during the study. The mean dose of quetiapine was 181.3 mg/day (range: 50–300 mg/day) across 8–52 weeks of treatment. Individuals who gained ≥7% of their baseline weight were 2.24 times more likely to have been treated with quetiapine compared to placebo (95% CI: 1.48–3.39, p = 0.0001, I2 = 0%).
-
4.
Other SGAs vs. Placebo
One study each reported weight gain dichotomously as an adverse effect following treatment with either aripiprazole (OCD; mean dose = 10 mg/day) [50], paliperidone (OCD; mean dose = 4.94 mg/day) [45], or ziprasidone (GAD; mean dose = 50.24 mg/day) [46]. For aripiprazole and paliperidone, participants did not experience weight gain. For ziprasidone, although participants in both groups experienced weight gain, there was no significant effect of exposure (OR = 0.75, 95% CI: 0.12–4.88, p = 0.76).
Meta-analysis of other metabolic adverse effects by off-label indication of SGAs
A limited number of studies reported other metabolic adverse effects in addition to weight gain. There was not enough data in the risperidone studies to pool in a meta-analysis.
-
Olanzapine vs. Placebo
One study [19] (n = 451) across three olanzapine dose groups (doses ranging from 2.5–10 mg) found that TG levels significantly increased by 0.26 mg/dl (95% CI 0.13–0.40, p < 0.001) in patients with BPD. There was no statistically significant difference for total cholesterol, HDL-C, and LDL-C, and insufficient data for HbA1c, WC, BMI, FG, and BP.
Quetiapine vs. Placebo
Three studies [32, 33, 36] (n = 1793) for quetiapine found that TG levels significantly increased by 15.33 mg/dl (95% CI 6.71–23.95, p < 0.001, I2 = 34%), total cholesterol increased by 3.36 mg/dl (95% CI 0.38–6.35, p = 0.03, I2 = 0%), and HDL decreased by 1.59 mg/dl (95% CI −2.52 to −0.65, p < 0.001, I2 = 0%). There was no statistically significant difference for FG, LDL-C, or BMI, and insufficient data for HbA1c, WC and BP.
Publication bias
Funnel plots could only be created for the olanzapine and quetiapine comparisons of body weight, as these were the only comparisons that included at least ten studies. No substantial publication bias was identified (Supplementary Figs. 6 and 7).
Discussion
This systematic review and meta-analysis identified RCTs with data evaluating metabolic side effects of SGAs during off-label use. We established that olanzapine induces significant weight gain in patients when used for off-label purposes. Quetiapine and risperidone also caused greater weight gain compared to placebo although the differences were not statistically significant. Patients treated with all three medications were also more likely to report weight gain as a side effect and to experience clinically significant weight gain. The effects of aripiprazole, paliperidone, and ziprasidone on weight could not be determined in a meta-analysis given that these agents were only reported in a single study each.
In order to explore potential mediators of metabolic adverse effects, we attempted to conduct subgroup analyses according to patient diagnosis. However, the limited number of studies in each diagnostic category (fewer than or equal to two studies per SGA) precluded any meaningful conclusions from being made. Nevertheless, among comparisons that found a significant difference according to diagnosis, PTSD (olanzapine comparison) and SUD (risperidone comparison) were identified as having one of the strongest weight gain effects. Interestingly, the PTSD studies employed the highest mean dose; therefore, this finding could reflect the significant dose-effect identified in our olanzapine meta-regression analysis. On the other hand, there may be intrinsic (e.g., biological) and other illness-related factors (e.g., poor diet, sedentary behaviour, and high smoking rates) specific to PTSD that increase the predisposition to metabolic disease, which is then further exacerbated by antipsychotic use. For example, PTSD has been associated with increased rates of obesity and metabolic syndrome, which is postulated to be related to dysfunction of the hypothalamic-pituitary-adrenal axis resulting from chronic stress [51]. Differences in patient demographics and baseline risk factors between studies prevented us from comparing weight gain across diagnostic groups while controlling for these key variables. Additional studies are needed to explore this intriguing question further and determine whether specific clinical populations are more likely to gain weight during off-label therapy with SGAs. Conversely, while different propensities for weight gain between diagnostic populations will be important to examine, it can be argued that, at least in populations that are similar in age and physiological aspects of metabolism, the observed metabolic disturbances may depend more on the metabolic liability of the AP than on patient diagnosis, as has been observed during on-label use [52].
Furthermore, while previous AP exposure represents an important mediator of the degree of AP-induced weight gain during on-label use [53, 54], the majority of included studies failed to provide information on previous AP exposure. This prevented us from conducting a meaningful subgroup analysis according to patient treatment status (AP-naïve vs. previous AP exposure). Although it may be argued that the likelihood of previous AP exposure in these populations is lower than that in schizophrenia or other approved indications, the increasing prevalence of APs for off-label use makes it difficult to assume that these patients were AP-naïve at the time of the study [8, 10]. Therefore, the lack of reporting on this point represents an important gap in the literature.
Our results are largely consistent with the substantial evidence of clinically significant weight gain reported during approved use of SGAs [4, 11]. In the current work, patients treated with olanzapine gained 3.24 kg compared to placebo. For quetiapine and risperidone, the respective mean differences in weight change of 0.82 and 0.66 kg were not statistically significant; however, dichotomous weight outcomes suggested that the risk of adverse weight gain on these agents is in fact higher than for placebo. While a direct comparison between on- and off-label use was not possible, our results note a similar degree of weight gain with olanzapine and quetiapine as that reported during AP use in adults with approved indications [55]. Furthermore, our finding that olanzapine caused greater weight gain than the other SGAs was expected given that olanzapine carries one of the highest metabolic liabilities, quetiapine and risperidone carry intermediate risk [56, 57], and aripiprazole, paliperidone, and ziprasidone have the lowest risk [55]. These findings are corroborated by our analysis of weight gain as a dichotomous side effect in which olanzapine, quetiapine, and risperidone were also associated with increased risk of weight gain. Although patient demographics such as age and sex are often similar in studies of on- and off-label antipsychotic use, as mentioned previously, these populations may differ in other important factors such as previous antipsychotic exposure and intrinsic biological risk. Therefore, it would be interesting for a future systematic review to examine this further by comparing the prevalence and severity of metabolic adverse effects of SGA use in on- versus off-label indications.
In the studies that reported on other metabolic parameters, olanzapine was associated with increases in TG levels, while quetiapine was associated with increases in TG and total cholesterol, and decreases in HDL-C. Although the effect of olanzapine on TG levels was quite modest and may not be clinically significant, our findings are consistent with existing data which demonstrate a strong lipidemic signal for olanzapine and quetiapine during approved use [58]. Unfortunately, the limited number of studies reporting on adverse metabolic outcomes other than weight change precluded us from drawing meaningful conclusions. It is important to note, however, that dyslipidemia and dysglycemia have been shown to occur even in the absence of weight gain among patients treated with APs for approved uses [57, 59]. Therefore, it is possible that both weight-dependent and weight-independent metabolic perturbations can occur with off-label use, but the latter have yet to be explored. As such, further research is required before clinical recommendations based on these metabolic risk factors can be made.
A key strength of this study is that we were able to perform meta-regression analyses to examine the effects of dose and cumulative drug exposure on weight gain for two commonly used AP agents, olanzapine and quetiapine. Interestingly, our study identified a positive dose-response association of olanzapine on weight gain. Conversely, the cumulative dose was not significantly associated with weight change. The latter observation may be explained by data suggesting that the most rapid weight gain trajectory occurs early on during olanzapine treatment [53], and may counter assumptions by clinicians regarding the safety of ‘shorter-term’ duration of off-label AP use. While the general relationship between AP dose and metabolic disturbances remains relatively unexplored, our findings are in line with a meta-analysis in which the odds ratio of weight gain increased by five for each 10 mg chlorpromazine equivalent dose increase in olanzapine [60]. The results of our study also indicate that even low AP doses carry the risk of weight gain. To this point, the dose relationship observed in this study occurred across a lower dose spectrum, with ten out of the twelve included studies reporting mean olanzapine doses ≤10 mg. This is an important consideration for clinical practice as it cannot be presumed that metabolic side effects are avoided by prescribing lower doses.
Our meta-regression analysis also showed a small, but significant positive association between daily quetiapine dose and weight gain during off-label use. While a relationship between dose and metabolic effects for approved uses has not been consistently reported [54, 57, 61, 62], significant weight gain has been found with quetiapine across both a lower and higher dosing spectrum [62]. Interestingly, a large nationwide cohort study that included patients with psychiatric disorders other than schizophrenia or bipolar disorder found that low doses of quetiapine (≤200 mg/day) did not lead to an increased risk of type 2 diabetes, unlike what is observed with its use in approved clinical populations [63]. This apparent contradiction may be related to our previous discussion point that metabolic disturbances can occur independently of weight gain. Therefore, further research is required to better characterize the dose-response association of SGAs with metabolic adverse effects other than weight gain, including fasting blood glucose levels and the risk of developing type 2 diabetes.
There are some limitations to this study to acknowledge. First, this review focused on adults aged 18–65, excluding studies in the pediatric and elderly populations. A meta-analysis evaluating the metabolic effects of SGAs in younger populations is particularly warranted given: (1) the rapid rise in off-label prescription in youth and adolescents [8, 64] and, (2) the observation that SGA-induced weight gain is more pronounced in children and adolescents, as well as AP-naïve patients [53, 54]. Furthermore, none of the included studies examined metabolic parameters as a primary study outcome. This may represent a source of bias as these studies may have not been adequately powered to detect any differences in metabolic outcomes. In terms of metabolic reporting, an additional 161 RCTs of off-label SGA use identified in our systematic search were excluded from the review as they did not report on any metabolic outcomes. As this lack of reporting greatly hampers adequate meta-analytic approaches, we encourage investigators of upcoming RCTs to report on metabolic parameters to improve our understanding of the metabolic adverse effects of off-label SGA use. Lastly, intervention and control groups were not compared across sex, ethnicity, age, and baseline weight, which may represent significant confounders of metabolic function [65–67].
Conclusions
This systematic review and meta-analysis demonstrates that off-label use of SGAs, and particularly olanzapine, can cause significant weight gain across different diagnostic groups. Other metabolic adverse events were also documented; however, this body of evidence is currently limited. Taken together, and in keeping with recent clinical practice recommendations, our findings call for caution in off-label AP use, particularly if alternate behavioral or pharmacological therapies are possible. If off-label AP use is felt to be necessary, we urge patient education about the potential for weight gain and other metabolic complications (which may occur even at lower doses), alongside careful periodic clinical re-evaluation of efficacy and continuing treatment need. Additionally, clinicians prescribing these agents off-label should adhere to the same standards of metabolic monitoring as is recommended for approved use.
Supplementary information
Author contributions
All authors contributed to drafting and revising the manuscript and approved its final version. S.M.A., D.S., and M.K.H. were involved in the concept and design of the study. N.S. and E.S. were involved in the systematic search, screening of articles, extraction of data, risk of bias assessment, and statistical analysis. S.B. was involved in the systematic search, screening of articles, extraction of data, and statistical analysis. V.T. was involved in the systematic search, screening of articles, and extraction of data. R.A. and W.M. were involved in the screening of articles, data extraction, and risk of bias assessment. G.R revised the work critically and provided suggestions for improvement.
Funding
N.S. is supported by the CIHR Canada Graduate Scholarship Master’s Program (CGS-M) and the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship. E.S. is supported by the CIHR Canada Graduate Scholarship Master’s Program (CGS-M) and the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship. S.B. Nothing to declare. V.T. Nothing to declare. R.A. is supported by the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship and the Cleghorn Award. W.B.M. Nothing to declare. G.R. has received research support from the Canadian Institutes of Health Research (CIHR), University of Toronto, Research Hospital Fund–Canada Foundation for Innovation (RHF-CFI), and HLS Therapeutics Inc. He has received advisory board support from HLS Therapeutics and consultant fees from Mitsubishi Tanabe Pharma Corporation. S.M.A. is supported in part by an Academic Scholars Award from the Department of Psychiatry, University of Toronto, and has grant support from the Canadian Institutes of Health Research, PSI Foundation, Ontario, and the CAMH Discovery Fund. D.S. is supported in part by an NHMRC Emerging Leadership Fellowship GNT1194635. M.K.H. is supported in part by an Academic Scholars Award from the Department of Psychiatry, University of Toronto, and has grant support from the Banting and Best Diabetes Center (BBDC), the Canadian Institutes of Health Research (PJT-153262) (CIHR), PSI Foundation, Ontario, holds the Kelly and Michael Meighen Chair in Psychosis Prevention, and the Cardy Schizophrenia Research Chair.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Nicolette Stogios, Emily Smith.
These authors jointly supervised this work: Sri Mahavir Agarwal, Margaret K. Hahn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41386-021-01163-7.
References
- 1.Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015;14:119–36. doi: 10.1002/wps.20204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajkumar AP, Horsdal HT, Wimberley T, Cohen D, Mors O, Borglum AD, et al. Endogenous and antipsychotic-related risks for diabetes mellitus in young people with schizophrenia: a danish population-based cohort study. Am J Psychiatry. 2017;174:686–94. doi: 10.1176/appi.ajp.2016.16040442. [DOI] [PubMed] [Google Scholar]
- 3.Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150:1115–21. doi: 10.1016/j.ahj.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Musil R, Obermeier M, Russ P, Hamerle M. Weight gain and antipsychotics: a drug safety review. Expert Opin Drug Saf. 2015;14:73–96. doi: 10.1517/14740338.2015.974549. [DOI] [PubMed] [Google Scholar]
- 5.Galling B, Roldán A, Nielsen RE, Nielsen J, Gerhard T, Carbon M, et al. Type 2 diabetes mellitus in youth exposed to antipsychotics: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73:247–59. doi: 10.1001/jamapsychiatry.2015.2923. [DOI] [PubMed] [Google Scholar]
- 6.Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192:E875–E91. doi: 10.1503/cmaj.191707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canadian Academy of Child and Adolescent Psychiatry, Canadian Academy of Geriatric Psychiatry, Canadian Psychiatric Association. Thirteen Things Physicians and Patients Should Question. Choosing Wisely Canada. https://choosingwiselycanada.org/psychiatry/. Published 2020. Accessed August 23, 2021.
- 8.Pringsheim T, Gardner DM. Dispensed prescriptions for quetiapine and other second-generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open. 2014;2:E225–32. doi: 10.9778/cmajo.20140009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalverdijk LJ, Bachmann CJ, Aagaard L, Burcu M, Glaeske G, Hoffmann F, et al. A multi-national comparison of antipsychotic drug use in children and adolescents, 2005-2012. Child Adolesc Psychiatry Ment Health. 2017;11:55. doi: 10.1186/s13034-017-0192-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20:177–84. doi: 10.1002/pds.2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8:114–26. doi: 10.1038/nrendo.2011.156. [DOI] [PubMed] [Google Scholar]
- 12.Zullino D, Bilancioni R, Conus P, Schwartz B, Khazaal Y, Baumann P. Off-label utilization of antipsychotics. South Afr Psychiatry Rev. 2006;9:38–43. [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bogenschutz MP, George Nurnberg H. Olanzapine versus placebo in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65:104–9. doi: 10.4088/jcp.v65n0118. [DOI] [PubMed] [Google Scholar]
- 15.Linehan MM, McDavid JD, Brown MZ, Sayrs JH, Gallop RJ. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69:999–1005. doi: 10.4088/jcp.v69n0617. [DOI] [PubMed] [Google Scholar]
- 16.Schulz SC, Zanarini MC, Bateman A, Bohus M, Detke HC, Trzaskoma Q, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193:485–92. doi: 10.1192/bjp.bp.107.037903. [DOI] [PubMed] [Google Scholar]
- 17.Soler J, Pascual JC, Campins J, Barrachina J, Puigdemont D, Alvarez E, et al. Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for borderline personality disorder. Am J Psychiatry. 2005;162:1221–4. doi: 10.1176/appi.ajp.162.6.1221. [DOI] [PubMed] [Google Scholar]
- 18.Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2001;62:849–54. doi: 10.4088/jcp.v62n1103. [DOI] [PubMed] [Google Scholar]
- 19.Zanarini MC, Schulz SC, Detke HC, Tanaka Y, Zhao F, Lin D, et al. A dose comparison of olanzapine for the treatment of borderline personality disorder: a 12-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2011;72:1353–62. doi: 10.4088/JCP.08m04138yel. [DOI] [PubMed] [Google Scholar]
- 20.Carey P, Suliman S, Ganesan K, Seedat S, Stein DJ. Olanzapine monotherapy in posttraumatic stress disorder: efficacy in a randomized, double-blind, placebo-controlled study. Hum Psychopharmacol. 2012;27:386–91. doi: 10.1002/hup.2238. [DOI] [PubMed] [Google Scholar]
- 21.Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry. 2002;159:1777–9. doi: 10.1176/appi.ajp.159.10.1777. [DOI] [PubMed] [Google Scholar]
- 22.Van Ameringen M, Mancini C, Patterson B, Bennett M, Oakman J. A randomized, double-blind, placebo-controlled trial of olanzapine in the treatment of trichotillomania. J Clin Psychiatry. 2010;71:1336–43. doi: 10.4088/JCP.09m05114gre. [DOI] [PubMed] [Google Scholar]
- 23.Pollack MH, Simon NM, Zalta AK, Worthington JJ, Hoge EA, Mick E, et al. Olanzapine augmentation of fluoxetine for refractory generalized anxiety disorder: a placebo controlled study. Biol Psychiatry. 2006;59:211–5. doi: 10.1016/j.biopsych.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Shapira NA, Ward HE, Mandoki M, Murphy TK, Yang MC, Blier P, et al. A double-blind, placebo-controlled trial of olanzapine addition in fluoxetine-refractory obsessive-compulsive disorder. Biol Psychiatry. 2004;55:553–5. doi: 10.1016/j.biopsych.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 25.McElroy SL, Nelson EB, Welge JA, Kaehler L, Keck PE., Jr Olanzapine in the treatment of pathological gambling: a negative randomized placebo-controlled trial. J Clin Psychiatry. 2008;69:433–40. doi: 10.4088/jcp.v69n0314. [DOI] [PubMed] [Google Scholar]
- 26.Bartzokis G, Lu PH, Turner J, Mintz J, Saunders CS. Adjunctive risperidone in the treatment of chronic combat-related posttraumatic stress disorder. Biol Psychiatry. 2005;57:474–9. doi: 10.1016/j.biopsych.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 27.Reich DB, Winternitz S, Hennen J, Watts T, Stanculescu C. A preliminary study of risperidone in the treatment of posttraumatic stress disorder related to childhood abuse in women. J Clin Psychiatry. 2004;65:1601–6. doi: 10.4088/jcp.v65n1204. [DOI] [PubMed] [Google Scholar]
- 28.Krystal JH, Rosenheck RA, Cramer JA, Vessicchio JC, Jones KM, Vertrees JE, et al. Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: a randomized trial. Jama. 2011;306:493–502. doi: 10.1001/jama.2011.1080. [DOI] [PubMed] [Google Scholar]
- 29.Brawman-Mintzer O, Knapp RG, Nietert PJ. Adjunctive risperidone in generalized anxiety disorder: a double-blind, placebo-controlled study. J Clin Psychiatry. 2005;66:1321–5. doi: 10.4088/jcp.v66n1016. [DOI] [PubMed] [Google Scholar]
- 30.Pandina GJ, Canuso CM, Turkoz I, Kujawa M, Mahmoud RA. Adjunctive risperidone in the treatment of generalized anxiety disorder: a double-blind, prospective, placebo-controlled, randomized trial. Psychopharmacol Bull. 2007;40:41–57. [PubMed] [Google Scholar]
- 31.Loebl T, Angarita GA, Pachas GN, Huang KL, Lee SH, Nino J, et al. A randomized, double-blind, placebo-controlled trial of long-acting risperidone in cocaine-dependent men. J Clin Psychiatry. 2008;69:480–6. doi: 10.4088/jcp.v69n0321. [DOI] [PubMed] [Google Scholar]
- 32.Bandelow B, Chouinard G, Bobes J, Ahokas A, Eggens I, Liu S, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13:305–20. doi: 10.1017/S1461145709990423. [DOI] [PubMed] [Google Scholar]
- 33.Khan A, Joyce M, Atkinson S, Eggens I, Baldytcheva I, Eriksson H. A randomized, double-blind study of once-daily extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2011;31:418–28. doi: 10.1097/JCP.0b013e318224864d. [DOI] [PubMed] [Google Scholar]
- 34.Merideth C, Cutler AJ, She F, Eriksson H. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the acute treatment of generalized anxiety disorder: a randomized, placebo controlled and active-controlled study. Int Clin Psychopharmacol. 2012;27:40–54. doi: 10.1097/YIC.0b013e32834d9f49. [DOI] [PubMed] [Google Scholar]
- 35.Bai YM, Ting Chen T, Chen JY, Chang WH, Wu B, Hung CH, et al. Equivalent switching dose from oral risperidone to risperidone long-acting injection: a 48-week randomized, prospective, single-blind pharmacokinetic study. J Clin Psychiatry. 2007;68:1218–25. doi: 10.4088/jcp.v68n0808. [DOI] [PubMed] [Google Scholar]
- 36.Khan A, Atkinson S, Mezhebovsky I, She F, Leathers T, Pathak S. Extended-release quetiapine fumarate (quetiapine XR) as adjunctive therapy in patients with generalized anxiety disorder and a history of inadequate treatment response: a randomized, double-blind study. Ann Clin Psychiatry. 2013;25:E7–22. [PubMed] [Google Scholar]
- 37.Katzman MA, Brawman-Mintzer O, Reyes EB, Olausson B, Liu S, Eriksson H. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26:11–24. doi: 10.1097/YIC.0b013e32833e34d9. [DOI] [PubMed] [Google Scholar]
- 38.Simon NM, Connor KM, LeBeau RT, Hoge EA, Worthington JJ, 3rd, Zhang W, et al. Quetiapine augmentation of paroxetine CR for the treatment of refractory generalized anxiety disorder: preliminary findings. Psychopharmacol. 2008;197:675–81. doi: 10.1007/s00213-008-1087-x. [DOI] [PubMed] [Google Scholar]
- 39.Vulink NC, Denys D, Fluitman SB, Meinardi JC, Westenberg HG. Quetiapine augments the effect of citalopram in non-refractory obsessive-compulsive disorder: a randomized, double-blind, placebo-controlled study of 76 patients. J Clin Psychiatry. 2009;70:1001–8. doi: 10.4088/JCP.08m04269. [DOI] [PubMed] [Google Scholar]
- 40.Atmaca M, Kuloglu M, Tezcan E, Gecici O. Quetiapine augmentation in patients with treatment resistant obsessive-compulsive disorder: a single-blind, placebo-controlled study. Int Clin Psychopharmacol. 2002;17:115–9. doi: 10.1097/00004850-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Black DW, Zanarini MC, Romine A, Shaw M, Allen J, Schulz SC. Comparison of low and moderate dosages of extended-release quetiapine in borderline personality disorder: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2014;171:1174–82. doi: 10.1176/appi.ajp.2014.13101348. [DOI] [PubMed] [Google Scholar]
- 42.Goddard AW, Mahmud W, Medlock C, Shin YW, Shekhar A. A controlled trial of quetiapine XR coadministration treatment of SSRI-resistant panic disorder. Ann Gen Psychiatry. 2015;14:26. doi: 10.1186/s12991-015-0064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Villarreal G, Hamner MB, Cañive JM, Robert S, Calais LA, Durklaski V, et al. Efficacy of Quetiapine Monotherapy in Posttraumatic Stress Disorder: A Randomized, Placebo-Controlled Trial. Am J Psychiatry. 2016;173:1205–12. doi: 10.1176/appi.ajp.2016.15070967. [DOI] [PubMed] [Google Scholar]
- 44.Javdan NS, Ghoreishi FS, Sehat M, Ghaderi A, Banafshe HR. Mental health and cognitive function responses to quetiapine in patients with methamphetamine abuse under methadone maintenance treatment. J Affect Disord. 2019;251:235–41. doi: 10.1016/j.jad.2019.03.078. [DOI] [PubMed] [Google Scholar]
- 45.Storch EA, Goddard AW, Grant JE, De Nadai AS, Goodman WK, Mutch PJ, et al. Double-blind, placebo-controlled, pilot trial of paliperidone augmentation in serotonin reuptake inhibitor-resistant obsessive-compulsive disorder. J Clin Psychiatry. 2013;74:e527–32. doi: 10.4088/JCP.12m08278. [DOI] [PubMed] [Google Scholar]
- 46.Lohoff FW, Etemad B, Mandos LA, Gallop R, Rickels K. Ziprasidone treatment of refractory generalized anxiety disorder: a placebo-controlled, double-blind study. J Clin Psychopharmacol. 2010;30:185–9. doi: 10.1097/JCP.0b013e3181d21951. [DOI] [PubMed] [Google Scholar]
- 47.Denys D, de Geus F, van Megen HJ, Westenberg HG. A double-blind, randomized, placebo-controlled trial of quetiapine addition in patients with obsessive-compulsive disorder refractory to serotonin reuptake inhibitors. J Clin Psychiatry. 2004;65:1040–8. doi: 10.4088/jcp.v65n0803. [DOI] [PubMed] [Google Scholar]
- 48.Heyer DB, Meredith RM. Environmental toxicology: Sensitive periods of development and neurodevelopmental disorders. Neurotoxicology. 2017;58:23–41. doi: 10.1016/j.neuro.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 49.Mariani JJ, Pavlicova M, Jean Choi C, Basaraba C, Carpenter KM, Mahony AL, et al. Quetiapine treatment for cannabis use disorder. Drug Alcohol Depend. 2020;218:108366. [DOI] [PubMed]
- 50.Sayyah M, Sayyah M, Boostani H, Ghaffari SM, Hoseini A. Effects of aripiprazole augmentation in treatment-resistant obsessive-compulsive disorder (a double blind clinical trial) Depress Anxiety. 2012;29:850–4. doi: 10.1002/da.21996. [DOI] [PubMed] [Google Scholar]
- 51.Farr OM, Sloan DM, Keane TM, Mantzoros CS. Stress- and PTSD-associated obesity and metabolic dysfunction: a growing problem requiring further research and novel treatments. Metab: Clin Exp. 2014;63:1463–68. doi: 10.1016/j.metabol.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barton BB, Segger F, Fischer K, Obermeier M, Musil R. Update on weight-gain caused by antipsychotics: a systematic review and meta-analysis. Expert Opin Drug Saf. 2020;19:295–314. doi: 10.1080/14740338.2020.1713091. [DOI] [PubMed] [Google Scholar]
- 53.Zipursky RB, Gu H, Green AI, Perkins DO, Tohen MF, McEvoy JP, et al. Course and predictors of weight gain in people with first-episode psychosis treated with olanzapine or haloperidol. Br J Psychiatry. 2005;187:537–43. doi: 10.1192/bjp.187.6.537. [DOI] [PubMed] [Google Scholar]
- 54.Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA. 2009;302:1765–73. doi: 10.1001/jama.2009.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7:64–77. doi: 10.1016/S2215-0366(19)30416-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Lobos CA, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225–33. doi: 10.1016/j.schres.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19:1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 58.Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res. 2004;70:1–17. doi: 10.1016/j.schres.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 59.Kang SH, Lee JI. Metabolic disturbances independent of body mass in patients with schizophrenia taking atypical antipsychotics. Psychiatry Investig. 2015;12:242. doi: 10.4306/pi.2015.12.2.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spertus J, Horvitz-Lennon M, Abing H, Normand SL. Risk of weight gain for specific antipsychotic drugs: a meta-analysis. NPJ Schizophr. 2018;4:12. doi: 10.1038/s41537-018-0053-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Simon V, van Winkel R, De Hert M. Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry. 2009;70:1041–50. doi: 10.4088/jcp.08r04392. [DOI] [PubMed] [Google Scholar]
- 62.Brecher M, Leong RW, Stening G, Osterling-Koskinen L, Jones AM. Quetiapine and long-term weight change: a comprehensive data review of patients with schizophrenia. J Clin Psychiatry. 2007;68:597–603. doi: 10.4088/jcp.v68n0416. [DOI] [PubMed] [Google Scholar]
- 63.Højlund M, Lund LC, Andersen K, Correll CU, Hallas J. Association of low-dose quetiapine and diabetes. JAMA Netw Open. 2021;4:e213209. doi: 10.1001/jamanetworkopen.2021.3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Leslie DL, Rosenheck R. Off-label use of antipsychotic medications in Medicaid. Am J Manag Care. 2012;18:e109–17. [PubMed] [Google Scholar]
- 65.Castellani LN, Costa-Dookhan KA, McIntyre WB, Wright DC, Flowers SA, Hahn MK, et al. Preclinical and clinical sex differences in antipsychotic-induced metabolic disturbances: a narrative review of adiposity and glucose metabolism. J Psychiatr Brain Sci. 2019;4:e190013. [DOI] [PMC free article] [PubMed]
- 66.Liu J, Hanley AJG, Young TK, Harris SB, Zinman B. Characteristics and prevalence of the metabolic syndrome among three ethnic groups in Canada. Int J Obes. 2006;30:669–76. doi: 10.1038/sj.ijo.0803179. [DOI] [PubMed] [Google Scholar]
- 67.Hildrum B, Mykletun A, Hole T, Midthjell K, Dahl AA. Age-specific prevalence of the metabolic syndrome defined by the international diabetes federation and the national cholesterol education program: the Norwegian HUNT 2 study. BMC Public Health. 2007;7:220. doi: 10.1186/1471-2458-7-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.