Abstract
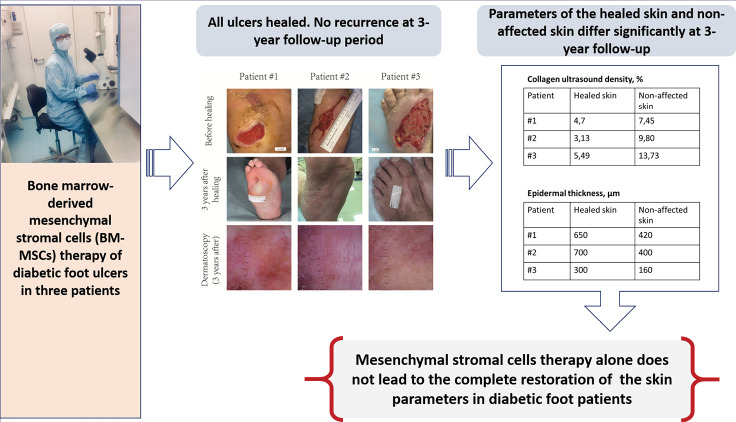
Introduction: Mesenchymal stromal cells (MSCs) administration is an effective option for the treatment of diabetic foot ulcers (DFUs). However, to date, studies assessing long-term outcomes and evaluating skin parameters after cell-based therapy are lacking. We presented the clinical outcomes of 3 patients, treated for DFUs with the bone marrow MSCs 3 years earlier.
Methods: Ultrasound examination was used to compare collagen density and epidermal thickness in areas of healed ulcers in comparison with non-affected skin used as a control. Ultrasound and dermatoscopy were used to exclude neoplasm formation, to assess scar contracture and wound recurrence.
Results: In all patients, no ulcer recurrence was detected, which was lower than the expected 60% rate of re-ulceration in diabetic patients in a 3-year period (OD [odds ratio] = 0.095, P = 0.12). No neoplasm formation, no contracture of hypertrophic scar, and adjacent tissue were registered. Collagen ultrasound density was decreased by 57% (P = 0.053) and epidermal thickness was increased by 72% (P = 0.01) in the area of healed ulcers in all patients.
Conclusion: MSCs therapy alone did not result in the complete restoration of the skin parameters within a 3-year period. MSCs may represent important adjuvant to the therapy, however, other novel approaches are required to achieve better results.
Keywords: Cell therapy, Diabetic foot ulcer, Mesenchymal stem cells, Mesenchymal stromal cells, Regenerative medicine, Wound healing
Introduction
Foot complications are identified as the most common cause of morbidity among diabetic patients. 1 Clinical trials as well as meta-analyses showed that stem cell-based therapy was a novel effective option for the treatment of diabetic foot ulcers (DFUs). 2-4 However, to date, the evidence regarding long-term outcomes of stem cell-based therapy is lacking.
Previously, we showed that the topical application of bone marrow-derived mesenchymal stromal cells (MSCs) at low doses resulted in a significant increase (up to 5-fold) in the re-epithelialization rate, which led to the complete closure of 4.2, 42.0, 20.4 cm2 hard-to-heal neuropathic DFUs in three diabetic patients. 5 However, the recurrence of DFUs after healing is a significant clinical challenge. It has been estimated that within 3 years after healing, ulcer recurrence occurs in about 60% of patients. 6
In the present study we aimed to obtain 3-year follow-up results of MSCs treatment in these 3 patients with the focus on ulcer recurrence, neoplasm formation, scar formation, scar, and adjacent tissues contraction, collagen density, and epidermal thickness in comparison with the non-affected skin of the control zone.
To the best of our knowledge, this is the first study, presenting long-term outcomes of topical application of MSCs at low doses used for the treatment of neuropathic DFUs.
Methods
Patients
Results of a DFU treatment with MSCs are described elsewhere. 5 Briefly, three type 2 diabetic patientsreceived a single topical application of MSCs (passage ≤ 2) suspension in saline at a dose of 4×104 cells/cm2 of the wound area for neuropathic DFU treatment in 2015 and were followed up consecutively.
Area of DFUs was 4.2 (Patient #1), 42.0 (Patient #2), and 20.4 cm2 (Patient #3). The ulcers of all patients epithelized on the 18th, 154th, and 98th days after the topical application of autologous MSCs, respectively. Patients were scheduled for a long-term clinical follow-up 3 years after the initial procedure.
Corresponding areas of the contralateral foot were used as a control to assess collagen density and epidermal thickness of non-affected skin in 2 patients (Patient #2 and #3). An area of intact skin, adjacent to the healed wound on the ipsilateral foot was used as a control for Patient #1 whose contralateral foot was amputated.
Ultrasonic examination
Ultrasound analysis (DUB® SkinScanner 22 MHz, Taberna Pro Medicum GmbH, Lueneburg, Germany) was performed for assessment of epidermal thickness, collagen density, and detection of neoplastic changes. Collagen density and epidermal thickness assessment were based on automatic echogenicity analysis performed using DUB® SkinScanner v. 5.1 original software as previous studies. 7,8
Dermatoscopy
Dermatoscopy (HEINE DELTA 20, HEINE Optotechnik GmbH & Co, Gilching, Germany) was performed to assess the integrity of the skin, signs of malignant skin lesions, and to compare dermoscopic structures in affected and non-affected areas.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 7 (GraphPad Software Inc., San Diego, USA). Ratio paired t-test was used for the analysis of differences in collagen density and epidermal thickness data, the differences were presented as geometric means of ratios (MR). The z-test was used to compare differences in re-ulceration risks (Odds ratio, OD). The significance level was established as P < 0.05.
Results
All patients had special educational training on the foot care at the Endocrinology Clinic of Sechenov University, used diabetic therapeutic footwear, and maintained acceptable glycemic control (HbA1c 7.5÷8.5%) during a 3-year follow-up period.
At the 3-year follow-up, all patients had no recurrences of ulceration in the area of the healed neuropathic DFU, which was lower (OD = 0.095, P = 0.12) than the expected 60% rate of re-ulceration in diabetic patients in a 3-year period, 6 but the difference was not statistically significant. Clinical, dermatoscopic, and ultrasound examinations revealed no signs of neoplastic changes at the site of treatment and in the control zone.
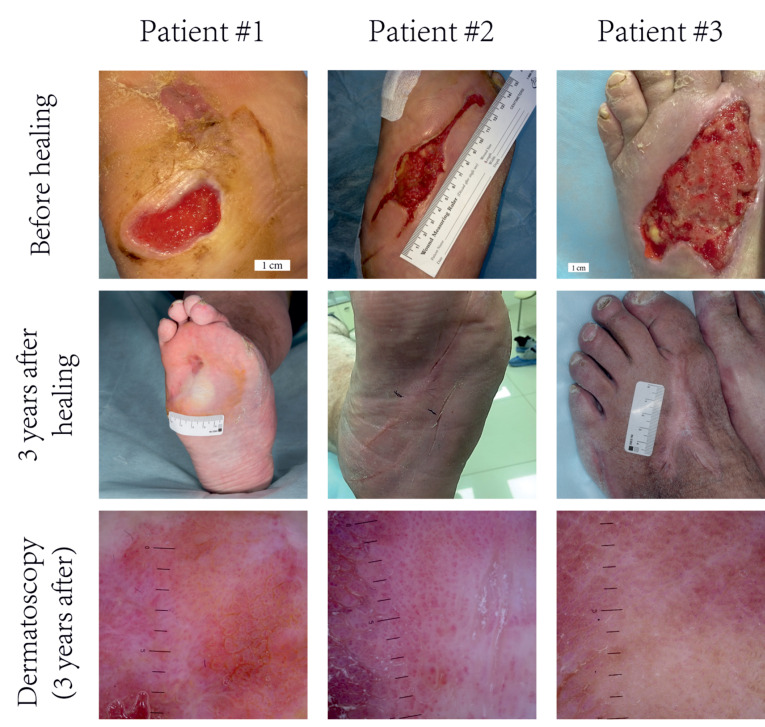
In all patients,ultrasounddata displayed changes in the zone of the healed ulcers that corresponded to the processes of hypertrophic scar formation as well as signs of a developed vasculature in this tissue. However, the hypertrophic scar did not require any surgical intervention in any of the patients. There was no evidence of keloid character in the scar tissue. No signs of scar or adjacent tissue contracture were noted in any of the patients at the site of treatment with MSCs (Fig. 1). In the zone of the healed ulcers and in the non-affected zone, a dermatoscopic examination revealed no signs of erosions. All patients had concomitant chronic pigmented purpura associated with diabetes mellitus at the site of treatment and in the control zone, but skin rash was mild and did not require specific therapy. Plantar scars in 2 patients showed grouped, dotted, centered, and hairpin vessels on a pink-whitish background; the scar on the dorsal surface of the foot in the third case revealed dotted and centered vessels and some areas of structureless and reticular pigmentation.
Fig. 1.
Process of DFU healing—before therapy and 3 years after healing. Ulcer recurrence, scar or adjacent tissue contracture, and neoplastic lesions were absent in all patients.
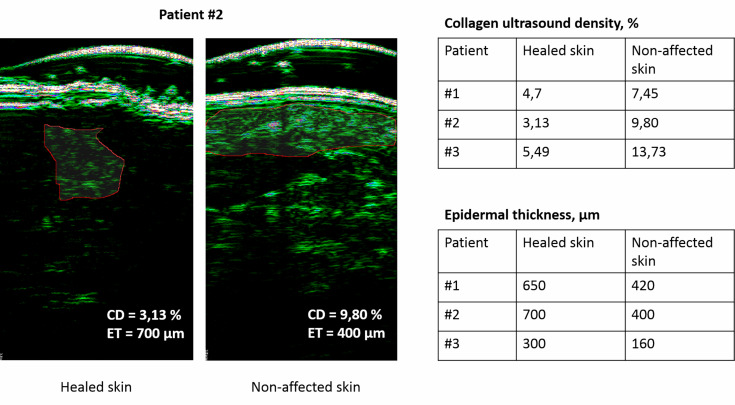
Statistically significantly increased epidermal thickness (MR = 1.72, 95% CI = [1.35-2.19], P = 0.01) in the area of healed ulcers was observed in all 3 patients in comparison with non-affected skin of the control zones. Collagen density was drastically decreased in all 3 patients in comparison with non-affected skin of the control zones, however, the differences were not statistically significant (MR = 0.43, 95% CI = [0.18[1.02], P = 0.053) (Fig. 2).
Fig. 2.
Increased epidermal thickness and decreased collagen density in the region of healed wounds of Patient #2 in comparison with the non-affected skin of the control zone. Red line indicates zones of interest. Raw data of collagen density and epidermal thickness are presented.
Discussion
The potential of mesenchymal stem cells is being actively studied in various in vitro and in vivo works to investigate the possibilities for the treatment of a wide range of pathologies, including bone, 9 cartilage, 10 and skin damage. The clinical efficacy of MSCs in the short term has been already demonstrated, however, the question of utmost importance is the efficacy and safety of MSC-based therapy in the long term. To the best of our knowledge, this is one of the longest follow-up period trials that showed the outcomes of the topical administration of MSCs in patients with DFUs and a single long-term trial of the topical administration of MSCs at low doses. In the present study, we showed that MSC-based therapy is a safe option in the long term. In line with our findings, Lu et al showed the absence of serious adverse events (including malignant tumors) related to bone marrow MSCs and bone marrow mononuclear cells injections used for the treatment of critical limb ischemia (CLI) and foot ulcers in patients with diabetes during the 3-year follow-up period. 11
DFUs, even when healed successfully, have a high rate of recurrence in the long term. In our study, we showed the absence of ulcer recurrence in 3 patients who received topical MSCs transplantation in combination with basic prophylactic measures (therapeutic footwear, foot care) and patient education. The role of diabetic therapeutic footwear and patient education should not be underestimated because these measures make a significant impact on the prevention of re-ulceration. 6
Priesand et al described the case of the malignant transformation of the site of a prior DFU becoming verrucous carcinoma. 12 We examined the site of prior DFUs as well as formed hypertrophic scars by means of dermatoscopy and ultrasound and did not note any visible signs of neoplasms. However, drawing conclusions regarding the absence of malignization requires additional tests, for example, a biopsy. Patients in the present study did not have any indications that warranted a biopsy and thus it was not performed.
Scar tissue contracture is one of the common complications after wound healing that often requires additional surgical intervention, particularly when located in the nearby joints. 13 We examined hypertrophic scars and concluded that there was an absence of scar and adjacent tissue contracture.
A normal collagen density and adequate epidermal thickness are important parameters of healthy well-functioning skin. In the present 3-year follow-up study we demonstrated the absence of adverse events, however, we documented 57% decrease in the collagen density and 72% increase in the epidermal thickness in the area of healed ulcers in comparison with non-affected skin of the control zones. In our study, we used low doses of MSCs. We suppose that the use of higher doses of MSCs would not result in better healing outcomes in the long term. Collagen density was decreased by 2.3 times, however, the differences did not reach statistical significance. Lack of statistical significance can be explained by the fact that collagen density in the area of healed ulcer in Patient #1 was close to the control not because it reached normal anatomical parameters, but rather because this patient had no contralateral limb and the control zone was on the same limb as healed ulcer and had decreased collagen density itself.
Previously, an improvement in functional and physiological parameters was shown when assessing the clinical outcomes of bone marrow mononuclear cell-based therapy in the long term, 14 however, the authors did not study the changes in the structure of foot tissue.
In our study, MSCs therapy was an effective approach for initial DFU healing, however, it did not result in the full restoration of normal anatomical parameters of the skin in the long term. Notably, our findings are in accordance with the results of previous studies which showed that the administration of autologous MSCs to patients with liver failure led to positive outcomes in the short term, however, significant improvements were not observed in the long term. 15
Although there are limitations due to the small number of patients, the present study provides valuable preliminary results regarding the long term outcomes of MSCs therapy used in the treatment of diabetic wounds.
Conclusion
This 3-year follow-up case series study, even though in the limited number of patients, shows that topical administration of MSCs at low doses for the treatment of neuropathic DFUs may represent a safe and promising option. However, MSCs-based therapy and basic prophylactic measures alone did not result in complete restoration of the normal anatomical parameters of the skin, even though it was extremely efficient for initial wound closure at early stages. MSCs-based therapy may represent feasible adjuvant to the therapy, however, other novel approaches are required to achieve better healing outcomes. Further clinical trials are required to confirm the findings of this study.
Funding sources
This work was supported by Sechenov University 5-100 program.
Ethical statement
This work was approved by the Local Ethical Committee of Sechenov University (approval no. 04-15, April 15, 2015).
Competing interests
None.
Authors’ contribution
NM, AM, IG, PB, AL designed the study. IK, OK, AL, MK analyzed and interpreted the data. NM, IK, OK, MK drafted the manuscript, AM, AL, IG, PB provided essential corrections and critically revised the manuscript for important intellectual content. All authors agreed to be responsible for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have approved the final manuscript.
Research Highlights
What is the current knowledge?
√ MSCs are promising candidates for the treatment of non-healing DFUs.
√ Previous studies show that MSCs are capable of improving wound healing.
√ Information regarding long-term outcomes of MSCs therapy is lacking.
What is new here?
√ MSCs therapy does not lead to the complete restoration of the skin parameters in the long term.
√ In a 3-year follow-up, decreased collagen density and increased epidermal thickness were observed in the area of the healed DFUs.
√ MSCs may represent an adjuvant to the therapy, however, other novel approaches are required to achieve better skin restoration.
References
- 1.Lim JZM, Ng NSL, Thomas C. Prevention and treatment of diabetic foot ulcers. J R Soc Med. 2017;110:104–9. doi: 10.1177/0141076816688346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopes L, Setia O, Aurshina A, Liu S, Hu H, Isaji T. et al. Stem cell therapy for diabetic foot ulcers: a review of preclinical and clinical research. Stem Cell Res Ther. 2018;9:188. doi: 10.1186/s13287-018-0938-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu D, Chen B, Liang Z, Deng W, Jiang Y, Li S. et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: a double-blind, randomized, controlled trial. Diabetes Res Clin Pract. 2011;92:26–36. doi: 10.1016/j.diabres.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Guo J, Dardik A, Fang K, Huang R, Gu Y. Meta-analysis on the treatment of diabetic foot ulcers with autologous stem cells. Stem Cell Res Ther. 2017;8:228. doi: 10.1186/s13287-017-0683-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maksimova N, Krasheninnikov M, Zhang Y, Ponomarev E, Pomytkin I, Melnichenko G. et al. Early passage autologous mesenchymal stromal cells accelerate diabetic wound re-epithelialization: A clinical case study. Cytotherapy. 2017;19:1548–50. doi: 10.1016/j.jcyt.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong DG, Boulton AJ, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367–75. doi: 10.1056/NEJMra1615439. [DOI] [PubMed] [Google Scholar]
- 7.Choi SJ, Lee SN, Kim K, Joo DH, Shin S, Lee J. et al. Biological effects of rutin on skin aging. Int J Mol Med. 2016;38:357–63. doi: 10.3892/ijmm.2016.2604. [DOI] [PubMed] [Google Scholar]
- 8.Bolke L, Schlippe G, Gerß J, Voss W. A collagen supplement improves skin hydration, elasticity, roughness, and density: Results of a randomized, placebo-controlled, blind study. Nutrients. 2019;11:2494. doi: 10.3390/nu11102494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khoramgah MS, Ranjbari J, Abbaszadeh HA, Mirakabad FST, Hatami S, Hosseinzadeh S. et al. Freeze-dried multiscale porous nanofibrous three dimensional scaffolds for bone regenerations. Bioimpacts. 2020;10:73–85. doi: 10.34172/bi.2020.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hesari R, Keshvarinia M, Kabiri M, Rad I, Parivar K, Hoseinpoor H. et al. Comparative impact of platelet rich plasma and transforming growth factor-β on chondrogenic differentiation of human adipose derived stem cells. Bioimpacts. 2020;10:37–43. doi: 10.15171/bi.2020.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu D, Jiang Y, Deng W, Zhang Y, Liang Z, Wu Q. et al. Long-Term Outcomes of BMMSC Compared with BMMNC for Treatment of Critical Limb Ischemia and Foot Ulcer in Patients with Diabetes. Cell Transplant. 2019;28:645–52. doi: 10.1177/0963689719835177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Priesand SJ, Holmes CM. Malignant Transformation of a Site of Prior Diabetic Foot Ulceration to Verrucous Carcinoma: A Case Report. Wounds. 2017;29:E125–E131. [PubMed] [Google Scholar]
- 13.Choi YS, Khan G, Nam SM, Park ES. Successful Treatment of Post-Traumatic Elbow Scar Contracture Using Combined Approach of Surgical Release & Early Fractional Laser Resurfacing. Medical Lasers. 2018;7:32–7. doi: 10.25289/ml.2018.7.1.32. [DOI] [Google Scholar]
- 14.Matoba S, Tatsumi T, Murohara T, Imaizumi T, Katsuda Y, Ito M. et al. Long-term clinical outcome after intramuscular implantation of bone marrow mononuclear cells (Therapeutic Angiogenesis by Cell Transplantation [TACT] trial) in patients with chronic limb ischemia. Am Heart J. 2008;156:1010–8. doi: 10.1016/j.ahj.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 15.Peng L, Xie DY, Lin BL, Liu J, Zhu HP, Xie C. et al. Autologous bone marrow mesenchymal stem cell transplantation in liver failure patients caused by hepatitis B: short‐term and long‐term outcomes. Hepatology. 2011;54:820–8. doi: 10.1002/hep.24434. [DOI] [PubMed] [Google Scholar]