Abstract
Background
The COVID-19 pandemic has presented new challenges surrounding end-of-life planning and has been associated with increased online discussion about life support.
Research Question
How has online communication about advance care planning (ACP) and specific life-sustaining interventions (LSIs) changed during the pandemic?
Study Design and Methods
Conversations on Twitter containing references to LSIs (eg, “ECMO”) or ACP (eg, “DNR/DNI”) were collected between January 2019 and May 2021. User account metadata were used to predict user demographic information and to classify users as organizations, individuals, clinicians, or influencers. The number of impressions was compared across these user categories and the content of tweets analyzed by using natural language processing models to identify topics of discussion and associated emotional sentiment.
Results
There were 202,585 unique tweets about LSIs and 67,162 unique tweets about ACP. Users who were younger, male, or influencers were more likely to discuss LSIs online. Tweets about LSIs were associated with more positive emotional sentiment scores than tweets about ACP (LSIs, 0.3; ACP, –0.2; P < .001). Among tweets about ACP, most contained personal experiences related to the death of loved ones (27%) or discussed discrimination through do-not-resuscitate orders directed at the elderly and disabled (19%). Personal experiences had the greatest retweet-to-tweet-ratio (4.7), indicating high levels of user engagement. Tweets about discrimination contained the most negative net sentiment score (–0.5).
Interpretation
The observed increase in tweets regarding LSIs and ACP suggests that Twitter was consistently used to discuss treatment modalities and preferences related to intensive care during the pandemic. Future interventions to increase online engagement with ACP may consider leveraging influencers and personal stories. Finally, we identified do-not-resuscitate-related discrimination as a commonly held public fear, which should be further explored as a barrier to ACP completion and can be proactively addressed by clinicians during bedside goals-of-care discussions.
Key Words: COVID-19, decision-making, end of life, mechanical ventilation, medical informatics
Abbreviations: ACP, advance care planning; DNI, do-not-intubate; DNR, do-not-resuscitate; ECMO, extracorporeal membrane oxygenation; LSI, life-sustaining intervention; NHDM, National Healthcare Decisions Month
Graphical Abstract
Take-home Points.
Study Question: How have online discussions about ACP developed amid a setting of increased media coverage focused on life support during the COVID-19 pandemic?
Results: There were 202,585 tweets about life support and 67,162 unique tweets about ACP. Most ACP tweets shared personal experiences or discussed “DNR/DNI”-related discrimination against vulnerable groups. Personal experiences contained the most engagement, whereas tweets about discrimination contained the most negative sentiment.
Interpretation: During the pandemic, routine discussions about life support were more frequent and more positively perceived than discussions about ACP.
Advance care planning (ACP) discussions clarify a person’s values and preferences about medical treatments in the event they are unable to communicate or if their clinical status rapidly deteriorates. Media coverage of life-sustaining interventions (LSIs) has greatly increased during the COVID-19 pandemic, which presents an important opportunity to integrate ACP into discussions about LSIs and further engage patients and health care professionals in this practice.1, 2, 3, 4
It is important to distinguish between routine discussions about LSIs, which focus on specific medical interventions, and ACP discussions, which focus on aligning patient’s values and goals with the specific medical interventions they receive.3 , 5, 6, 7 Participation in ACP is important because lack of planning often leads to goal-discordant care in which patients receive LSIs that they may not have wanted had they established their preferences in advance. However, only about one-in-three US adults have completed an advance directive, owing to multiple barriers for both patients and physicians, including, but not limited to: (1) lack of understanding about ACP; (2) insufficient time during physician appointments to discuss ACP; (3) a belief that ACP does not apply to young or healthy patients; (4) reliance on family or physician-led decision-making over autonomous decision-making; and (5) discomfort with talking about death and dying.8, 9, 10, 11, 12, 13, 14
Online discussions about ACP may have a significant impact on people’s perceptions and behaviors related to ACP. Although the online completion of advance directives has increased nearly fivefold during the COVID-19 pandemic, no prior studies have examined online discussions about ACP during the pandemic in relation to discussions about LSIs.15 To characterize how online communication about ACP and LSIs may have changed during the pandemic, we studied Twitter discussions that referenced LSIs, including CPR, ventilators, and extracorporeal membrane oxygenation (ECMO), and those that included more deliberate conversations related to ACP. Twitter provides a real-time source of data from > 300 million active users worldwide contributing > 500 million tweets daily and has been extensively used to identify ongoing health care issues.16, 17, 18, 19, 20, 21, 22, 23, 24 Analysis of social media content may inform on public viewpoints during critical situations and accordingly could be used to tailor the messaging of public health recommendations.
Study Design and Methods
Search Strategy and Definitions
We collected English-language tweets related to LSIs and ACP between January 2019 and May 2021. Twitter provides an application programming interface that enables collection of historical tweet content and metadata such as retweets and geolocation. With Twitter’s application programming interface, we searched for tweets containing variations of the words “DNR” (do-not-resuscitate), “DNI” (do-not-intubate), “advance directives,” “ECMO,” “CPR,” “high flow oxygen,” “dialysis,” and “ventilation.” Variations for the search term “advance directives” included “living will,” “medical directive,” and “medical power of attorney.” Tweets containing “DNR” or “DNI” were grouped together as “DNR/DNI” because most tweets referenced both terms concurrently. Tweets returned from the search terms “DNR/DNI” and “advance directives” were categorized as tweets about ACP. Although LSIs refer to a broad set of interventions intended to prolong life following organ failure, we chose to selectively examine discussions about cardiopulmonary interventions related to the treatment of COVID-19. Thus, only tweets referencing “ECMO,” “CPR,” and “ventilation” were included in the LSI category. Twitter data reflect information users choose to share publicly, and thus institutional review board approval was not required.
User Classification
Twitter users were classified as clinicians, individuals, influencers, or organizations. A user was marked as an organization and further classified as a news, health, or government organization if either its display name or profile biography contained relevant key words (eg, “department,” “organization,” “news,” “government,” “hospital”). Key words representing organizations were chosen based on review of Twitter profiles from users in the data set and key words used in previous related studies.17 Users were labeled as influencers if they did not meet the criteria for an organization but had at least 100,000 followers or a verified Twitter account.17 Verified status on Twitter distinguishes authentic high-profile users from impersonators.25 Of the remaining users, clinicians were identified and further classified as ICU physicians, non-ICU physicians, or nurses if profile biographies contained relevant key words (eg, “MD,” “DO,” “RN,” “physician,” “surgeon,” “nurse,” “intensivist,” “critical care”). Clinicians with > 100,000 followers or verified status were classified as influencers. All remaining users were classified as individuals. The performance of our classification algorithm was compared with a manually verified random sample of 400 unique users. The estimated overall accuracy of the algorithm was 93% (e-Fig 1). Finally, we applied a multimodal deep neural architecture model to predict the age and gender of nonorganization accounts using profile pictures and user biographies.26
Text and Statistical Analysis
Text parsing was used to remove components from tweets without semantic value (eg, special characters, punctuations, URLs).27 Each message was divided into individual words and lemmatized to the base dictionary form (eg, “better” reduced to “good”). Words appearing in < 5 tweets, auxiliary verbs, and conjunctions were excluded.
Latent Dirichlet allocation, an unsupervised machine learning approach, was then performed to analyze the content of tweets.28 The latent Dirichlet allocation algorithm uses the frequency and co-occurrence of linguistic units to generate a probabilistic model for assigning individual tweets to distinct topics.29 To validate findings from the latent Dirichlet allocation analysis and create representative names for each topic, the identified topic areas were manually reviewed by using a commonly used iterative six-step thematic analysis.30
To evaluate the sentiment of tweets, we used VADER (Valence Aware Dictionary and sEntiment Reasoner), an established lexicon-based model for computing sentiment.31 This tool provides a compound score for each tweet that accounts for the intensity of expressed emotion, ranging from 1 (extreme positive) to –1 (extreme negative).
All analyses were performed by using MATLAB R2021a (MathWorks, Inc.). To assess differences between types of users and the identified topics, χ2 tests were used. To identify cells contributing to the significance of the χ2 test results, adjusted residuals were calculated for each cell, and a Bonferroni-adjusted P < .001 was used to indicate statistical significance.32 Mann-Whitney U tests were used to assess differences in nonnormally distributed user characteristics between groups.
Results
Search Results
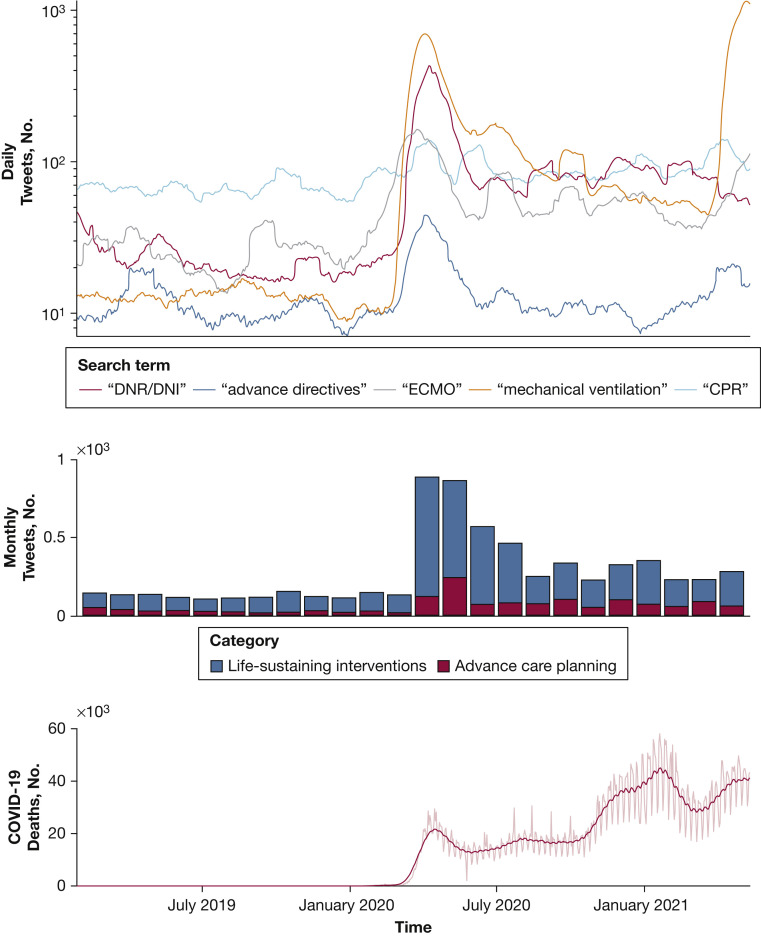
Between January 2020 and May 2021, there were 202,585 unique tweets about LSIs by 125,693 users and 67,162 unique tweets about ACP by 41,920 users. Conversations about both LSIs and ACP peaked during the first global spike in COVID-19 deaths from March to May 2020 (e-Fig 2, Fig 1 ). During this period, tweets about LSIs reached a maximum of 979 tweets per day on April 6, 2020. References to mechanical ventilation comprised a majority of LSI tweets (72%), followed by references to “ECMO” (14.5%) and CPR (13.5%). Tweets referencing CPR showed the smallest increase during the first peak in COVID-19 deaths, shifting from a maximum of 93 tweets per day before March 2020 to a maximum of 138 tweets per day after.
Figure 1.
Number of tweets and COVID-19 deaths over time. Daily global COVID-19 deaths (light red) and 31-day moving average of daily COVID-19 deaths (red) were obtained from World Health Organization Coronavirus (COVID-19) Dashboard Data Explorer (Geneva: World Health Organization, 2020). DNR/DNI = do-not-resituate/do-not-intubate; ECMO = extracorporeal membrane oxygenation.
Despite a considerable increase from baseline during this period, tweets about ACP were less frequently shared than tweets about LSIs. ACP tweets reached a maximum of 472 tweets on April 8, 2020. Following May 2020, the number of daily tweets for all search terms gradually decreased yet remained higher than the baseline prior to COVID-19.
When comparing the geolocation of created tweets across groups, LSIs were more frequently mentioned than ACP in parts of Africa and the Indian subcontinent (e-Fig 3). This discrepancy suggests that the terms “advance directives” and “DNR/DNI” may have been introduced to users in these English-speaking developing countries but are less utilized by these populations.
Results of User Classification
Twitter users posting about LSIs and ACP were classified as organizations, influencers, individuals, or clinicians (Table 1 ). Across all types of users, more total users participated in conversations about LSIs than ACP (Fig 2 ). Organizations (N = 26,182) were further classified into health (34%), news (33%), and government (13%) organizations. Clinicians (N = 36,158) were further classified as non-ICU physicians (20%), nurses (10%), and ICU physicians (4%). Among all users, ICU physicians had the greatest percentage of tweets referencing LSIs (85.7%), whereas nurses had the least (69.2%) (e-Fig 4).
Table 1.
User Demographic Characteristics
| Characteristics | ACP | LSIs | P Value |
|---|---|---|---|
| Predicted sex (n = 35,464; 105,967)a | < .001 | ||
| Male | 19,678 (55.5) | 71,952 (67.9) | |
| Female | 15,786 (44.5) | 34,012 (32.1) | |
| Predicted age, y (n = 35,464; 105,967)a | < .001 | ||
| ≤ 18 | 4,871 (13.7) | 19,275 (18.2) | |
| 19-29 | 3,618 (10.2) | 12,451 (11.7) | |
| 30-39 | 7,952 (22.4) | 25,373 (23.9) | |
| ≥ 40 | 19,023 (53.6) | 48,868 (46.1) | |
| User type (n = 41,920; 125,693) | < .001 | ||
| Organizations | 6,456 (15.4) | 19,726 (15.7) | |
| Influencers | 383 (0.9) | 1,836 (1.5) | |
| Individuals | 25,099 (59.9) | 77,955 (62) | |
| Clinicians | 9,982 (23.8) | 26,176 (20.8) |
Data are presented as No. (%). P values were obtained from the χ2 test for independence. ACP = advance care planning; LSIs = life-sustaining interventions.
Sex and age were predicted for only nonorganization users.
Figure 2.
Comparison of contributors and impressions for users tweeting about ACP and LSIs. Box plots show the median value (horizontal bar), interquartile range (box), and 95% CI (vertical lines). Asterisks indicate a significant difference between content categories obtained from the Mann-Whitney U test with P < .001. ACP = advance care planning; LSIs = life-sustaining interventions.
Although users in both groups were mostly male, more male individuals tweeted about LSIs than about ACP (LSIs, 68%; ACP, 56%; P < .0001). Most users were > 40 years of age in both groups; however, users tweeting about LSIs tended to be younger than those tweeting about ACP.
The impact of each tweet was calculated by using impressions, which quantify the number of followers that may be exposed to a user’s tweets and is a commonly used metric for potential exposure.17 , 33 Impressions for each user were computed by multiplying the number of created tweets by the number of their followers. Users tweeting about LSIs had more total followers, unique tweets, and impressions, likely as this group had more overall users (e-Table 1). Furthermore, influencers created more median impressions related to LSIs than about ACP (LSIs, 33,917; ACP, 24,048; P < .001) (e-Table 1, Fig 2). Organizations, individuals, and clinicians had more impressions about ACP content than about LSIs; however, these impressions were an order of magnitude lower than the impressions of influencers.
Results of Sentiment and Topic Analysis
Tweets referencing LSIs had a greater median sentiment than those referencing ACP (LSIs, 0.3; ACP, –0.2; P < .001), as shown in Figure 3 . A topic analysis was performed to further understand the content domains of conversations within the ACP group. Table 2 presents the key words, representative tweets, and mean sentiment for identified topics.
Figure 3.
Violin plots showing the discrepancy in expressed sentiment in tweets about ACP and LSIs. The shaded areas represent the probability distribution of the emotional sentiment for each category of tweets. Box plots were overlaid to demonstrate the median value (horizontal bar), interquartile range (box), and 95% CI (vertical lines). ACP = advance care planning; LSIs = life-sustaining interventions.
Table 2.
Summary of Content Found in Tweets About ACP
| Topic | Topic Key Words | Representative Tweet | Sentiment |
|---|---|---|---|
| Calls to establish ACP | wish, decision, life, talk, think, power, attorney, choice, important, need | “PLEASE FOR THE LOVE OF GOD establish an advance directive for if you’re incapacitated. Choose someone who will respect your wishes to be power of attorney!! Do NOT leave it up to chance…”a | 0.46 (0.03 to 0.73) |
| National Healthcare Decisions Month | learn, resource, national, #nhdd, talk, #acp, webinar, april, importance | “Today is National Healthcare Decisions Day, a day designed to educate the public and healthcare providers about the importance of advance care planning… #NHDD2021”b | 0.60 (0.36 to 0.77) |
| Research | support, discussion, research, service, study, improve, work | “Just published in #jqps: New study on communication tool for engaging patients in #advancecareplanning during the #covid19 pandemic…”b | 0.13 (–0.48 to 0.51) |
| Personal experiences | hospital, patient, die, sign, death, treatment, form, require, family | “My mother had a DNR and when she had end of life hospice care I prayed for God to take her for days because of her suffering before I held her hand as she took her last breath….”c | –0.27 (–0.66 to 0.38) |
| Legal advice | decision, right, consent, legal, choice, against, decide, power, attorney | “The law does not require the patient’s or next of kin’s permission to put a DNR on someone. A doctor or medical professional can put one on a person without even informing them, this is as the UK law stands right now.”d | 0.08 (–0.49 to 0.48) |
| Discrimination | home, death, disabled, old, notice, send, government, vulnerable, many | “… We have likely prevented few if any deaths and the govt has created far more with DNR orders on the old and disabled and by sending sick old people out of hospitals to care homes.”d | –0.51 (–0.79 to 0.08) |
| COVID-19 precautions | mask, wear, please, sick, risk, worker, resource, waste, virus | “… If you don’t wear a mask be sure to carry a copy of your DNR with you at all times. You don’t deserve a hospital bed if you won’t wear a mask.”a | –0.05 (–0.51 to 0.44) |
Sentiment is presented as median (interquartile range). ACP = advance care planning; DNR = do-not-resuscitate.
Individual user; predicted age, 19 to 29 years; predicted sex, female.
Organization account.
Nurse user; predicted age, 30 to 39 years; predicted sex, female.
Individual user; predicted age: ≥ 40 years, predicted sex, male.
Identified topics include personal experiences (27%), “DNR/DNI”-related discrimination during COVID-19 (19%), COVID-19 precautions (16%), legal advice (15%), research studies (13%), public appeals to create advance directives (6%), and National Healthcare Decisions Month (NHDM), a communications campaign held April to promote the importance of ACP (4%). Tweets about discrimination focused primarily on responses to government plans to initiate unilateral DNR orders, in which physicians may enact a DNR without patient consent, for the elderly and disabled during COVID-19. Tweets containing legal advice included debates about decision-making in theoretical end-of-life scenarios as well as definitions of terms related to advanced directives, such as medical power of attorney.
Most topics did not show a strong net positive or negative sentiment (e-Fig 5, Table 2). However, tweets referencing NHDM contained the most positive median (interquartile range) emotional sentiment, 0.6 (0.36 to 0.77). In contrast, tweets about “DNR/DNI”-related discrimination contained the most negative median (interquartile range) sentiment, –0.51 (–0.79 to 0.08).
Tweets with calls to action, personal experiences, and references to DNR-related discrimination reached daily maximums coinciding with the first global spike in COVID-19 deaths (Fig 4 ). Conversations about these topics rapidly subsided over the following months, except for residual conversations about personal experiences and discrimination. The topic of NHDM reached three peaks of similar magnitude during the months of April in 2019, 2020, and 2021, corresponding to the national awareness month occurring each April. Notably, NHDM was the only topic not to reach a new maximum at the beginning of the pandemic.
Figure 4.
Topics of advance care planning tweets over time. Topics without appreciable temporal correlations were omitted for better visualization. NHDM = National Healthcare Decisions Month; WHO = World Health Organization.
There was a significant association between types of users and identified topics within ACP tweets (χ2 = 4,810; P < .0001) and retweets (χ2 = 37,508; P < .0001) (Table 3 ). Organizations were more likely to share messages about NHDM, research, and calls to establish ACP but less likely to share personal experiences, legal advice, or content related to discrimination. In contrast, individuals were more likely to tweet about personal experiences, legal advice, discrimination, and COVID-19 precautions but less likely to mention NHDM, research, or calls to establish ACP. Similarly, clinicians were more likely to reference personal experiences and less likely to reference NHDM or calls for action. However, clinicians were more likely to retweet posts about all topics besides personal experiences, suggesting a willingness to share precreated content about ACP over original messaging. Influencers were more likely to tweet about research and less likely to tweet about discrimination.
Table 3.
Content Domains of ACP Tweets and Retweets According to Type of User
| Topic | Organizations |
Influencers |
Individuals |
Clinicians |
All Users |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tweets | Retweets | Tweets | Retweets | Tweets | Retweets | Tweets | Retweets | Tweets | Retweets | RT:T | |
| Calls for action | 1,430 (11.9)a | 1,471 (3.9)a | 42 (7.5) | 245 (1.3)b | 1,978 (4.9)b | 1,263 (1.3)b | 788 (5.5)b | 849 (4)a | 4,238 (6.3) | 3,828 (2.2) | 0.9 |
| NHDM | 1,591 (13.3)a | 2,065 (5.5)a | 19 (3.4) | 77 (0.4)b | 844 (2.1)b | 846 (0.8)b | 397 (2.8)b | 789 (3.7)a | 2,851 (4.2) | 3,777 (2.1) | 1.3 |
| Personal experiences | 2,295 (19.1)b | 5,025 (13.4)b | 134 (24.1) | 7,988 (41.4)b | 11,807 (29.2)a | 68,875 (69.1)a | 4,121 (28.9)a | 4,934 (23.2)b | 18,357 (27.3) | 86,822 (48.8) | 4.7 |
| Legal advice | 1,271 (10.6)b | 1,649 (4.4) | 66 (11.8) | 356 (1.8)b | 6,251 (15.5)a | 4,672 (4.7) | 2,184 (15.3) | 1,625 (7.6)a | 9,772 (14.5) | 8,302 (4.7) | 0.8 |
| Discrimination | 1,400 (11.7)b | 9,811 (26.1)a | 64 (11.5)b | 2,046 (10.6)b | 8,366 (20.7)a | 14,189 (14.2)b | 2,731 (19.2) | 6,726 (31.6)a | 12,561 (18.7) | 32,772 (18.4) | 2.6 |
| COVID-19 precautions | 1,135 (9.5)b | 2,412 (6.4)b | 59 (10.6) | 5,830 (30.2)a | 7,178 (17.8)a | 5,027 (5)b | 2,264 (15.9) | 2,115 (9.9)a | 10,636 (15.8) | 15,384 (8.7) | 1.4 |
| Research | 2,867 (23.9)a | 15,102 (40.2)a | 173 (31.1)a | 2,744 (14.2)b | 3,953 (9.8)b | 4,839 (4.9)b | 1,754 (12.3) | 4,253 (20)a | 8,747 (13) | 26,938 (15.1) | 3.1 |
| Total | 11,989 | 37,535 | 557 | 19,286 | 40,377 | 99,711 | 14,239 | 21,291 | 67,162 | 177,823 | 2.6 |
Data are presented as No. (%) unless otherwise indicated. Statistically significant cells representing values greater than expecteda or less than expectedb when comparing across different user types at Bonferroni-adjusted P < .001. ACP = advance care planning; NHDM = National Healthcare Decisions Month; RT:T = retweet:tweet ratio.
Tweets sharing personal experiences had the highest retweet-to-tweet ratio (4.7) across all users, suggesting that these tweets had the most support. Content related to legal advice (0.8) or public appeals to establish ACP (0.9) had the lowest retweet-to-tweet ratios.
Discussion
This study tracked discussions about ACP and LSIs on Twitter and used machine learning techniques to characterize participating users and public perceptions surrounding these topics during the COVID-19 pandemic. Our findings suggest that although the COVID-19 pandemic has increased public discussion about previously uncommonly discussed LSIs, conversations about ACP received far less viewership and were associated with more negative emotional sentiment. We also found that systemic discrimination through advance directives is a commonly cited perspective in online discussions.
The excessive demand for mechanical ventilation and ECMO services, in addition to complexities involving allocation of equipment, personnel, and resources, likely drove the observed surge in Twitter conversations related to LSIs.34 Younger age and male sex users were more likely to contribute to these discussions. This finding may represent that younger users perceive ACP discussions as less relevant given their lower overall risk than older users.35 All user types were less likely to tweet about ACP, which was also associated with more negative emotional sentiment. This is consistent with the perception that ACP is associated with death or dying, and that many users feel it is less appropriate to share negative emotions online. Although clinicians tweeting about ACP left more impressions on a per-user basis, fewer clinicians talked about ACP than about LSIs. This result suggests clinicians have the potential to promote ACP online but more often choose to participate in conversations about LSIs. These findings could be explained by previous research that suggests that, although clinicians are educated about ACP, they are often afraid of talking about death and may forget to initiate ACP conversations with patients in the rush of clinical practice.36, 37, 38, 39
Approximately 19% of ACP tweets recognized DNR/DNI orders as a form of discrimination during the pandemic and were associated with the most negative sentiment. These findings suggest that public reservations about DNR/DNI may be rooted in fear of biased treatment of groups such as the elderly or people with disabilities. Such reservations are not unexpected, as one in five patients aged > 50 years experiences discrimination in health care settings, often because of new or worsening disability.40 In addition, older patients tend to receive shorter, less intensive care and have higher rates of DNR/DNI orders, independent of clinical status.41, 42, 43 Unfortunately, public discourse during COVID-19 has reintroduced the potential for discriminatory behaviors, such as counting physical and mental disability as part of resource allocation criteria, blanket DNR orders for people in care homes, and Twitter hashtags attacking “baby boomers.”44, 45, 46 Clinicians may more effectively approach ACP conversations at the bedside by proactively acknowledging concerns related to systemic DNR/DNI-related discrimination, knowing that it is brought up in nearly one of five Twitter conversations about ACP.
One potential opportunity to increase ACP-related content may be to leverage awareness campaigns such as NHDM to promote messages that reach online audiences more effectively. NHDM has been hosted by the Institute of Healthcare Improvement each April since 2008 to educate both the public and providers about the importance of ACP.47, 48, 49 Tweets containing appeals to complete advance directives peaked during every April of the study period, highlighting existing social media awareness that might be further leveraged to change the narrative toward more positive messaging around ACP. However, the frequency of NHDM-related tweets did not increase from 2019 to 2021 despite elevated mortality during the pandemic, reflecting the challenge of connecting this campaign to real-time events. Encouraging collaboration between institutions participating in NHDM may allow for more coordinated situational responses to future crises that may result in more goal-concordant care.
Notably, tweets containing personal experiences with ACP had considerably more public support than tweets simply promoting NHDM. Although these personal stories were primarily shared by individuals or clinicians, organizations participating in NHDM might produce more meaningful and effective campaigns by collaborating with these users or modifying their shared content to focus more on patient stories. There is considerable research to suggest that storytelling can improve learning, which is vital to increase awareness and improve public sentiment relating to ACP.50 Similarly, organizations may consider collaborating with influencers to share content, because these users had the greatest impact on a per-user basis. In addition, users who select to follow ACP-focused organizations are more likely to already be familiar with these resources. For example, tweets sharing research articles related to ACP had extensive public exposure, but organizations created and shared these posts more than any other user. This suggests that among followers of organizations, most users are not engaging with the tweets, and only a small percentage share the original messaging. To increase user engagement and reduce unidirectional messaging, NHDM organizers may even consider directing tweets about ACP to specific users using the “@” symbol.
There are several limitations to the current analysis. First, we may have under-identified the number of tweets about LSIs or ACP. Tweets relevant to either topic may have been missed because they were not covered by our search terms, which did not account for misspellings or non-English-language tweets. Our findings may also not be generalizable to the entire public, as Twitter users are a self-selected group that may not adequately represent certain demographic characteristics, including elderly people. For international tweets from non-English-speaking countries, English-speaking users could represent a biased sample of highly educated or affluent users rather than the general public. In addition, the use of key words to classify organizations and clinicians may have resulted in misclassification of users that did not provide adequate description in their Twitter biography. The aforementioned limitations would have resulted in nondifferential misclassification of the user types and bias our findings toward the null. Finally, there may have been tweets in the LSIs group that were focused on setting preferences about life support (eg, “I don’t want ECMO if I get COVID-19”). As we could not discriminate these tweets, our result only applies to the official use of ACP terminology. Further attempts to understand the content of discussions related to LSIs is warranted.
Interpretation
During the pandemic, discussions about LSIs gained more impressions and were perceived with more positive emotional sentiment than discussions about ACP, suggesting that routine discussions about life support therapies were more popular than value-based discussions surrounding life support preferences. Our findings suggest that younger individuals, men, and users with influencer status were more likely to focus on LSIs than ACP and thus are potential targets for future interventions aimed at increasing engagement in ACP. Furthermore, personal experiences with death were commonly shared by individuals and clinicians tweeting about ACP and had the most user engagement. Incorporating these empowering personal stories into media campaigns and influencer content may increase public exposure and re-sharing of ACP content. Finally, we identified DNR-related discrimination of vulnerable groups as a commonly held fear during the pandemic. Proactively addressing patient concerns about discrimination may be helpful for clinicians when discussing ACP at the bedside.
Further studies are warranted to better characterize the online prevalence of specific end-of-life priorities, the socioeconomic and cultural influences governing these priorities, and the evolving role of social media in promoting ACP. Given the remarkable ability of social media to disseminate information, our findings provide some guidance for the medical community to better leverage this resource to engage with the public during emergencies.
Acknowledgments
Author contributions: V. R. P. is the guarantor of the manuscript content, including the data and analysis. V. R. P. had full access to all study data and takes responsibility for the integrity of the data and accuracy of the data analysis. V. R. P., S. G., and C. J. B. contributed to the study design. All authors contributed to data interpretation and drafting of the manuscript.
Financial/nonfinancial disclosures: None declared.
Other contributions: The authors thank Dr David Ring, MD, PhD, for helpful discussion and critical review of the original manuscript.
Additional information: The e-Figures and e-Table are available online under "Supplementary Data."
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Supplementary Data
References
- 1.Block B.L., Smith A.K., Sudore R.L. During COVID-19, outpatient advance care planning is imperative: we need all hands on deck. J Am Geriatrics Soc. 2020;68(7):1395–1397. doi: 10.1111/jgs.16532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpern S.D. Shaping end-of-life care: behavioral economics and advance directives. Semin Respir Crit Care Med. 2012;33(4):393–400. doi: 10.1055/s-0032-1322403. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A., Bahl B., Rabadi S., Mebane A., Levey R., Vasudevan V. Value of advance care directives for patients with serious illness in the era of COVID pandemic: a review of challenges and solutions. Am J Hosp Palliat Care. 2021;38(2):191–198. doi: 10.1177/1049909120963698. [DOI] [PubMed] [Google Scholar]
- 4.Curtis J.R., Kross E.K., Stapleton R.D. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19) JAMA. 2020;323(18):1771–1772. doi: 10.1001/jama.2020.4894. [DOI] [PubMed] [Google Scholar]
- 5.Farrell T.W., Ferrante L.E., Brown T., et al. AGS position statement: resource allocation strategies and age-related considerations in the COVID-19 era and beyond. J Am Geriatrics Soc. 2020;68(6):1136–1142. doi: 10.1111/jgs.16537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detering K.M., Hancock A.D., Reade M.C., Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silveira M.J., Kim S.Y.H., Langa K.M. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benson WF, Aldrich N. Advance care planning: ensuring your wishes are known and honored if you are unable to speak for yourself, Critical Issue Brief, Centers for Disease Control and Prevention. 2012. Accessed April 18, 2022. www.cdc.gov/aging
- 9.Denvir M.A., Highet G., Robertson S., et al. Future care planning for patients approaching end-of-life with advanced heart disease: an interview study with patients, carers and healthcare professionals exploring the content, rationale and design of a randomised clinical trial. BMJ Open. 2014;4(7) doi: 10.1136/bmjopen-2014-005021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schichtel M., Wee B., MacArtney J.I., Collins S. Clinician barriers and facilitators to heart failure advance care plans: a systematic literature review and qualitative evidence synthesis [published online ahead of print July 22, 2019]. BMJ Support Palliat Care. https://doi.org/10.1136/bmjspcare-2018-001747 [DOI] [PubMed]
- 11.Dingfield L.E., Kayser J.B. Integrating advance care planning into practice. Chest. 2017;151(6):1387–1393. doi: 10.1016/j.chest.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 12.Yadav K.N., Gabler N.B., Cooney E., et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Affairs. 2017;36(7):1244–1251. doi: 10.1377/hlthaff.2017.0175. [DOI] [PubMed] [Google Scholar]
- 13.Cheung J.T.K., Au D., Ip A.H.F., et al. Barriers to advance care planning: a qualitative study of seriously ill Chinese patients and their families. BMC Palliative Care. 2020;19(1):80. doi: 10.1186/s12904-020-00587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernard C., Tan A., Slaven M., Elston D., Heyland D.K., Howard M. Exploring patient-reported barriers to advance care planning in family practice. BMC Family Practice. 2020;21(1):94. doi: 10.1186/s12875-020-01167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Auriemma C.L., Halpern S.D., Asch J.M., Van Der Tuyn M., Asch D.A. Completion of advance directives and documented care preferences during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Network Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.15762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.About Twitter Our company purpose, principles, leadership. https://about.twitter.com/en/who-we-are/our-company.html
- 17.Thackeray R., Burton S.H., Giraud-Carrier C., Rollins S., Draper C.R. Using Twitter for breast cancer prevention: an analysis of breast cancer awareness month. BMC Cancer. 2013;13(1):508. doi: 10.1186/1471-2407-13-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinnenberg L., DiSilvestro C.L., Mancheno C., et al. Twitter as a potential data source for cardiovascular disease research. JAMA Cardiol. 2016;1(9):1032. doi: 10.1001/jamacardio.2016.3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu J.M., Pelullo A.P., Hassan S., Siderowf L., Merchant R.M., Werner R.M. Gender differences in Twitter use and influence among health policy and health services researchers. JAMA Intern Med. 2019;179(12):1726. doi: 10.1001/jamainternmed.2019.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goff D.A., Kullar R., Laxminarayan R., Mendelson M., Nathwani D., Osterholm M. Twitter to engage, educate, and advocate for global antibiotic stewardship and antimicrobial resistance. Lancet Infect Dis. 2019;19(3):229–231. doi: 10.1016/S1473-3099(19)30058-1. [DOI] [PubMed] [Google Scholar]
- 21.Hanson C.L., Burton S.H., Giraud-Carrier C., West J.H., Barnes M.D., Hansen B. Tweaking and tweeting: exploring twitter for nonmedical use of a psychostimulant drug (Adderall) among college students. J Medical Internet Res. 2013;15(4) doi: 10.2196/jmir.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padmanabhan D.L., Ayyaswami V., Prabhu A.V., Sinclair C., Gugliucci M.R. The #PalliativeCare conversation on Twitter: an analysis of trends, content, and caregiver perspectives. J Pain Sympt Manag. 2021;61(3):495–503.e1. doi: 10.1016/j.jpainsymman.2020.08.023. [DOI] [PubMed] [Google Scholar]
- 23.Yousefinaghani S., Dara R., Mubareka S., Papadopoulos A., Sharif S. An analysis of COVID-19 vaccine sentiments and opinions on Twitter. Int J Infect Dis. 2021;108:256–262. doi: 10.1016/j.ijid.2021.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sedrak M.S., Cohen R.B., Merchant R.M., Schapira M.M. Cancer communication in the social media age. JAMA Oncol. 2016;2(6):822–823. doi: 10.1001/jamaoncol.2015.5475. [DOI] [PubMed] [Google Scholar]
- 25.Twitter verification requirements—how to get the blue check. [cited 2021 Jul 21] https://help.twitter.com/en/managing-your-account/about-twitter-verified-accounts
- 26.Demographic Inference and Representative Population Estimates from Multilingual Social Media Data. The World Wide Web Conference. [cited 2021 Sep 5] https://dl.acm.org/doi/10.1145/3308558.3313684
- 27.Stone B., Dennis S., Kwantes P.J. Comparing methods for single paragraph similarity analysis. Topics Cognitive Sci. 2011;3(1):92–122. doi: 10.1111/j.1756-8765.2010.01108.x. [DOI] [PubMed] [Google Scholar]
- 28.Blei D.M., Ng A.Y., Jordan M.I. Latent Dirichlet allocation. J Machine Learning Res. 2003;3(Jan):993–1022. [Google Scholar]
- 29.Griffiths T.L., Steyvers M. Finding scientific topics. PNAS. 2004;101(suppl 1):5228–5235. doi: 10.1073/pnas.0307752101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Braun V., Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 31.Hutto C., Gilbert E. VADER: a parsimonious rule-based model for sentiment analysis of social media text. Proceedings of the International AAAI Conference on Web and Social Media. 2014;8(1):216–225. [Google Scholar]
- 32.Beasley T.M., Schumacker R.E. Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. J Experimental Educ. 1995;64(1):79–93. [Google Scholar]
- 33.Lindenwann W.K. Setting minimum standards for measuring public relations effectiveness. Public Relations Rev. 1997;23(4):391–402. [Google Scholar]
- 34.Ramanathan K., Antognini D., Combes A., et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020;8(5):518–526. doi: 10.1016/S2213-2600(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waterloo S.F., Baumgartner S.E., Peter J., Valkenburg P.M. Norms of online expressions of emotion: comparing Facebook, Twitter, Instagram, and WhatsApp. New Media Society. 2018;20(5):1813–1831. doi: 10.1177/1461444817707349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vleminck A.D., Pardon K., Beernaert K., et al. Barriers to advance care planning in cancer, heart failure and dementia patients: a focus group study on general practitioners’ views and experiences. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0084905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barnes S., Gott M., Payne S., et al. Communication in heart failure: perspectives from older people and primary care professionals. Health Social Care Community. 2006;14(6):482–490. doi: 10.1111/j.1365-2524.2006.00636.x. [DOI] [PubMed] [Google Scholar]
- 38.Seymour J., Almack K., Kennedy S. Implementing advance care planning: a qualitative study of community nurses’ views and experiences. BMC Palliative Care. 2010;9(1):4. doi: 10.1186/1472-684X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nortjé N., Stepan K. Advance care planning conversations in the oncology setting: tips from the experts. J Canc Educ. 2021;36(2):325–329. doi: 10.1007/s13187-019-01631-1. [DOI] [PubMed] [Google Scholar]
- 40.Rogers S.E., Thrasher A.D., Miao Y., Boscardin W.J., Smith A.K. Discrimination in healthcare settings is associated with disability in older adults: health and retirement study, 2008–2012. J Gen Intern Med. 2015;30(10):1413–1420. doi: 10.1007/s11606-015-3233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cook I., Kirkup A.L., Langham L.J., Malik M.A., Marlow G., Sammy I. End of life care and do not resuscitate orders: how much does age influence decision making? A systematic review and meta-analysis. Gerontol Geriatr Med. 2017;3 doi: 10.1177/2333721417713422. 2333721417713422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moore N.A., Wiggins N., Adams J. Age as a factor in do not attempt cardiopulmonary resuscitation decisions: a multicentre blinded simulation-based study. Palliat Med. 2015;29(4):380–385. doi: 10.1177/0269216314566838. [DOI] [PubMed] [Google Scholar]
- 43.Wiel E., Di Pompéo C., Segal N., et al. Age discrimination in out-of-hospital cardiac arrest care: a case-control study. Eur J Cardiovasc Nursing. 2018;17(6):505–512. doi: 10.1177/1474515117746329. [DOI] [PubMed] [Google Scholar]
- 44.Fraser S., Lagacé M., Bongué B., et al. Ageism and COVID-19: what does our society’s response say about us? Age Ageing. 2020;49(5):692–695. doi: 10.1093/ageing/afaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen B., McNamara D.M. Disability discrimination, medical rationing and COVID-19. ABR. 2020;12(4):511–518. doi: 10.1007/s41649-020-00147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meisner B.A. Are you OK, boomer? Intensification of ageism and intergenerational tensions on social media amid COVID-19. Leisure Sci. 2021;43(1-2):56–61. [Google Scholar]
- 47.National Healthcare Decisions Day—April 16. The Conversation Project. [cited 2021 Jul 31] https://theconversationproject.org/nhdd/
- 48.National Healthcare Decisions Day NHPCO. 2020 [cited 2021 Jul 31] https://www.nhpco.org/national-healthcare-decisions-day/
- 49.National Healthcare Decisions Day. [cited 2021 Jul 31] https://fivewishes.org/nhdd Available from:
- 50.Lordly D. Once upon a time…. storytelling to enhance teaching and learning. Can J Dietetic Practice Res. 2007;68(1):30–35. doi: 10.3148/68.1.2007.30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.