Abstract
Purpose
Clean intermittent catheterization (CIC) responsibility among youth with spina bifida is not well-studied. We sought to determine longitudinal trajectories of CIC responsibility to examine the transition of CIC responsibility from caregiver- to self-CIC.
Materials and Methods
We performed a secondary analysis of a prospective cohort study of youth with spina bifida. Participants ages 8-15 years old originally recruited from four hospitals and a statewide spina bifida association were followed every 2 years. Participants who required CIC were included. Group-based trajectory modeling was used to isolate distinct trajectories of CIC responsibility, which was the primary outcome and was graded from caregiver-CIC to shared-CIC to self-CIC. Predictors of trajectory group membership were entered into multivariate logistic regression models and included various demographic, clinical, and psychosocial characteristics, including CIC adherence and CIC mastery.
Results
Of 140 youth in the original cohort study, 89 met eligibility criteria for this study. Mean age was 11 years old at enrollment; 93% had myelomeningocele. Two distinct trajectory groups emerged: 17% had a low-flat trajectory, and 83% had a high-increasing trajectory of CIC responsibility, with shared-CIC by age 8-9 years old and increasing self-CIC responsibility thereafter. Significant predictors of group membership in the high-increasing trajectory group included less severe spinal lesion levels, higher CIC mastery, and lower CIC adherence.
Conclusions
Nearly 1 in 5 youth with spina bifida in our cohort persistently required caregiver-CIC over time, while the remainder achieved shared-CIC responsibility by age 8-9 years old with increasing self-CIC responsibility thereafter.
Introduction
Individuals with spina bifida (SB) have neuropathic bladders from their spinal cord lesions that affect their ability to void and store urine. Fortunately, clean intermittent catheterization (CIC)1 is a regimen that has revolutionized bladder management. CIC can increase urinary continence, which improves quality-of-life,2, 3 and can lower dangerously high bladder storage pressures that are associated with vesicoureteral reflux, infections, and kidney dysfunction.4 However, an effective CIC regimen requires strict user responsibility to ensure that the risks of CIC, including urinary tract infections or trauma,5 are minimized, while the benefits are maximized.
To date, there are no guidelines and only limited evidence on when youth with SB should learn to do CIC responsibly by themselves.6, 7 Parents or adult caregivers are often taught how to perform CIC initially, with a gradual sharing of skills and responsibility with the child as the child develops and matures. As youth with SB transition to adulthood, the goal is eventual total CIC responsibility by the child alone (i.e., self-CIC) to aid in achieving independence in their self-care. However, not every child is well-suited to learn or perform self-CIC responsibly.7 Of additional value would therefore be identifying the demographic, clinical, and psychosocial factors that are associated with transfer of CIC responsibility to the child. These factors can then be measured and targeted early to help children with SB optimize their bladder self-management to the best of their abilities.
Given these knowledge gaps, we sought to determine distinct longitudinal trajectories of CIC responsibility in a well-characterized, longitudinal cohort of youth with SB. We also sought to assess the factors that predict membership in these trajectory groups. Based on a prior study of overall self-responsibility,8 we hypothesized that higher intelligence quotient (IQ) would be at least one predictor of membership in the trajectory group where CIC responsibility is passed more rapidly from parent to child.
Materials and Methods
Study Population and Design
This was a secondary analysis of a longitudinal prospective cohort study that has been described elsewhere.9 In brief, families and youth with SB were recruited from four hospitals and a statewide SB association in the Midwest for a longitudinal study of neuropsychological functioning, social relationships, and psychosocial adjustment among youth with SB. Inclusion criteria were: 1) a diagnosis of SB (myelomeningocele, lipomeningocele, or myelocystocele); 2) age 8-15 years; 3) proficiency in English or Spanish; 4) involvement of at least one primary caregiver; and 5) residence within 300 miles of the laboratory. Participants with any additional major medical or psychiatric condition were not recruited.
The current study was approved by university and hospital Institutional Review Boards and used a multi-method, multi-informant longitudinal research design. The current study used repeated testing data from 4 time points (i.e., Time 1-Time 4), each spaced two years apart, and included only youth who were dependent on CIC based on parent report. Participants missing values at all time points on the primary outcome variable or all predictor variables at Time 1 were excluded.
Measures
The primary outcome was CIC responsibility, which was measured with the catheterization subscale of the Sharing of SB Management Responsibilities Scale (SOSBMR).10 Parents rated who was primarily responsible for each task (e.g., parent, shared, child, or not applicable). The outcome measure was ordered such that the lowest score (i.e., caregiver-CIC) meant the parent was solely responsible, and the highest score (i.e., self-CIC) meant that the child was solely responsible. Shared-CIC encompassed any degree of joint responsibility involving both child and caregiver.
Predictor selection was performed based on clinical knowledge and prior theoretical models.11 All predictors and testing results were obtained at Time 1. Demographic variables included child age, child gender, and child race/ethnicity. Condition-specific clinical variables included lesion level, type of SB, shunt status, and number of shunt revisions. Youth IQ were measured with the Vocabulary and Matrix Reasoning subtests of the Wechsler Abbreviated Scale of Intelligence (WASI).12 Youth adaptive functioning was measured with subtests of the Adaptive Behavior Assessment-Second Edition (ABAS-II).13 Gross motor functioning was measured using an adaptation of the Gross Motor Function Classification System for Cerebral Palsy,14 with higher scores indicating higher level of function. Fine motor functioning and time and punctuality domains were measured with the Scales of Independent Behavior-Revised (SIB-R).15 CIC mastery was measured with the SB Independence Survey (SBIS).16 CIC adherence was measured with the SB Self-Management Profile (SBSMP).17 More details on these measures, including internal consistency and reliability coefficients, are in the Supplement.
Statistical Analysis
Descriptive statistics using frequencies and means were used to describe the sample. To isolate distinct trajectories of CIC responsibility, group-based trajectory modeling with SAS PROC TRAJ18, 19 (SAS Institute, Inc., Cary, NC) was used with the youth’s age as the “time” variable. Group-based trajectory modeling is a useful statistical approach to study the development of shared CIC responsibility, which might unfold differently for different youth over time. It allows (1) the identification of latent subgroups within the sample who have distinct developmental trajectories for shared CIC responsibility and (2) the determination of the shape of the trajectory for each group. The trajectory groups are not determined a priori; they emerge from the data.18 Because data were collected every 2 years, and to have adequate sample sizes at each age level, we operationalized age in two-year increments, as follows: age group 1 = 8-9 years (n=26); age group 2 = 10-11 years (n=40); age group 3 = 12-13 years (n=54); age group 4 = 14-15 years (n=67); and age group 5 = 16-17 years (n=36) which ensured that at least 26 (30%) participants were included in each age group. This method of structuring the data permits a longer-term 10-year longitudinal view (ages 8-17 years) with only 6 years of data on each participant.20 Model selection for SAS PROC TRAJ was performed per standard two-stage technique using Bayesian Information Criteria and examining posterior probabilities of group membership.21 Details are in Supplement.
Next, we conducted multiple imputation (5 imputations) to impute missing data for the Time 1 predictors. The pooled estimates were then used to describe subgroup differences on Time 1 predictors between youth assigned to different CIC responsibility trajectory groups based on chi-squares and between-groups t-tests. Variables found to be statistically significant (p≤0.05) in the univariate analyses were selected as candidates and were entered into a logistic regression model using the imputed data to explore the association between these variables and membership in the CIC responsibility trajectory groups. Backward selection in the logistic regression was used and the significance level was set at 0.05 to achieve the final model. The multiple imputation and all analyses based on the imputed data with pooled estimates were conducted in IBM SPSS Version 26 (IBM Corp, Armonk, NY).
Results
The original longitudinal study has been described previously.9 Of 140 families of children with SB at Time 1, 110 (79%) participated at Time 2, 102 (73%) participated at Time 3, and 93 (66%) at Time 4.
For the current study, the sample only included youth who needed CIC based on parent report (n=100). Eleven youth were excluded because eight had no data on the outcome variable and three had no data on predictor variables resulting in a final cohort of 89 participants for analysis. The sample was 52% female, with a mean age of 11 years at the time of enrollment, 93% had myelomeningocele, and the mean IQ was 87.8 (95% Confidence Interval [CI] 83.8, 91.8; see Table 1).
Table 1.
Youth cohort baseline demographic, clinical, and psychometric characteristics at study enrollment.
| Variable | No. (%) | Mean (95%CI) |
|---|---|---|
| Demographics/ severity | ||
| Age at enrollment, years | 89 (100) | 11.4 (10.8,11.9) |
| Sex | ||
| Male | 37 (41.6) | |
| Female | 52 (58.4) | |
| Type of spina bifida | ||
| Myelomeningocele | 83 (93.3) | |
| Non-myelomeningocele | 6 (6.7) | |
| Lesion level | ||
| Thoracic | 16 (18.0) | |
| Lumbar | 45 (50.6) | |
| Sacral | 25 (28.1) | |
| Missing | 3 (3.3) | |
| Presence of ventricular shunt | 73 (82.0) | |
| Number of shunt revisions | ||
| >=5 | 14 (15.7) | |
| 1-4 | 36 (40.4) | |
| 0 | 34 (38.2) | |
| Missing | 5 (5.6) | |
| Intelligence quotient (WASI IQ) | 88 (98.8) | 87.8 (83.8, 91.8) |
| Gross motor functioning score, Mother’s report * | 89 (100) | 2.1 (1.9, 2.3) |
| Adaptive Function * | ||
| Adaptive Behavior Assessment-Second Edition (ABAS II),Total Subscale score, parent report | 89 (100) | 312.8 (300.3, 325.2) |
| Scales of Independent Behavior-Revised (SIB-R) Fine motor subscale, parent report | 89 (100) | 43.1 (40.9, 45.2) |
| Scales of Independent Behavior-Revised (SIB-R) Time and punctuality subscale, parent report | 89 (100) | 42 (39.8, 44.2) |
| Medical skill mastery: Catheterization * | 89 (100) | 87.1 (83.6, 90.7) |
| The Spina Bifida Independence Survey (SBIS), parent report | ||
| Medical adherence: Catheterization * | 89 (100) | 4.4 (4.3, 4.6) |
| The Spina Bifida Self-Management Profile (SBSMP), parent report |
higher scores indicate higher function, independence, or adherence
Trajectories of Catheterization Responsibility
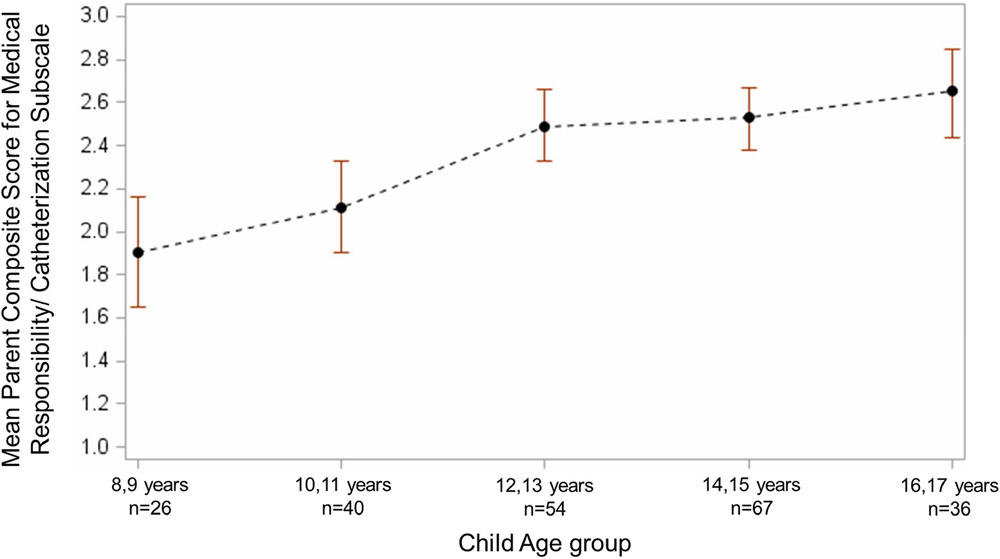
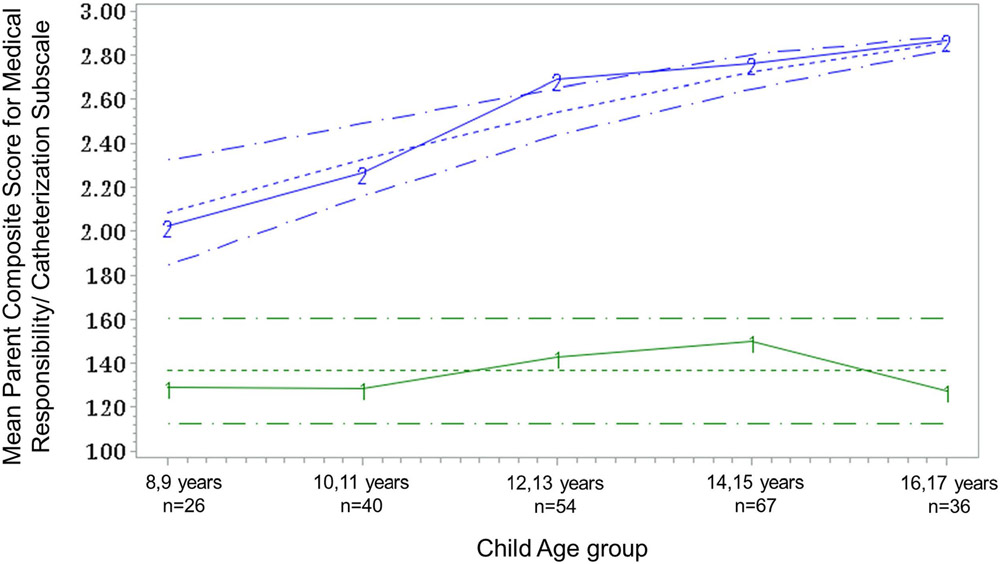
The cohort overall displayed equally shared-CIC responsibility score (i.e., a score of 2) at age 8-9 years old that increased towards child-only CIC responsibility (i.e., score of 3) over time (Figure 1). However, the group-based trajectory analysis revealed two distinct CIC responsibility subgroups within the cohort: group 1 demonstrated a low-flat trajectory (n=15, 17%) and group 2 demonstrated a high-increasing trajectory (n=74, 83%, Figure 2). The high-increasing CIC responsibility trajectory started at a higher score for age group 1, and remained consistently higher for each age group compared with the low flat group (intercept=1.83, SE=0.12; slope=0.26, SE=0.03, p<0.001). The high-increasing group also demonstrated a consistent increase in CIC responsibility scores with increasing age group [mean 1.99 (95%CI 1.72, 2.25) at age 8-9 years to 2.87 (95%CI 2.79, 2.95) at age 16-17 years] compared with the low-flat group, who demonstrated relative stability in CIC responsibility scores with increasing age [mean 1.24 (95%CI 0.36, 2.11) at age 8-9 years to 1.29 (95%CI 0.74,1.83) at age 16-17 years; Table 2].
Figure 1. Mean CIC Self-Responsibility by Age Group.
The cohort overall displayed equally shared CIC responsibility score (i.e., score of 2) by age 8-9 years old that increased towards child-only CIC responsibility (i.e., score of 3) over time.
Figure 2. Two distinct trajectories of CIC self-responsibility found by group-based trajectory modeling.
Trajectory Group 1 (low CIC self-responsibility) constituted 17% (n=15) of the cohort and remained flat and constant over time. Trajectory Group 2 (high-increasing CIC self-responsibility) constituted 83% (n=74) of the cohort and displayed a rapid rise over time.
Table 2.
Mean CIC responsibility score by Trajectory Group (higher score = more child responsibility).
| Trajectory Group 1 (low child responsibility), n=15 |
Trajectory Group 2 (high-increasing child responsibility), n=74 |
|||
|---|---|---|---|---|
| Age Group | n | Mean score (95% CI) | n | Mean score (95% CI) |
| 8, 9 years | 3 | 1.24 (0.36, 2.11) | 23 | 1.99 (1.72, 2.25) |
| 10,11 years | 5 | 1.20 (0.86, 1.54) | 35 | 2.24 (2.04, 2.45) |
| 12, 13 years | 8 | 1.34 (1.00, 1.69) | 46 | 2.69 (2.59, 2.79) |
| 14, 15 years | 12 | 1.48 (1.15, 1.80) | 55 | 2.76 (2.60, 2.83) |
| 16, 17 years | 5 | 1.29 (0.74, 1.83) | 31 | 2.87 (2.79, 2.95) |
Variables Associated with Catheterization Responsibility Trajectory Group
Results of the univariate analyses examining differences between the low-flat and high-increasing CIC responsibility trajectory groups, as a function of the Time 1 predictors, are presented in Table 3. Compared to the low-flat trajectory group, the high-increasing trajectory group had a lower proportion of youth with thoracic-level lesions, and scored higher on IQ, gross motor function, adaptive function scales, fine motor function, and CIC mastery. On the other hand, the high-increasing trajectory group scored lower on CIC adherence. The youth’s sex, type of SB, presence of ventricular shunt, the number of shunt revisions, and SIB-R time and punctuality subscale were not significantly different between the two trajectory groups.
Table 3.
Univariate analyses of candidate variables by Trajectory Group after multiple imputation.
| Variable | Low CIC responsibility Trajectory Group, n |
High increasing CIC responsibility Trajectory Group, n |
X2 + | p | |
|---|---|---|---|---|---|
| Total | 15 | 74 | |||
| Sex | 0.18 | 0.892 | |||
| Male | 6 | 31 | |||
| Female | 9 | 43 | |||
| Type of spina bifida | 0.584 | 0.319 | |||
| Myelomeningocele | 15 | 68 | |||
| Non-myelomeningocele | 0 | 6 | |||
| Lesion level | 11.983 | 0.003 | |||
| Thoracic | 8 | 10 | |||
| Lumbar | 6 | 40 | |||
| Sacral | 1 | 24 | |||
| Presence of ventricular shunt | 13 | 60 | 1.000 | 0.464 | |
| Number of shunt revisions | |||||
| >=5 | 5 | 12 | 3.090 | 0.378 | |
| 1-4 | 4 | 33 | |||
| 0 | 6 | 29 | |||
| Low CIC responsibility Trajectory Group, n=15, Mean (SE) |
High increasing CIC responsibility Trajectory Group n=74, Mean (SE) |
Mean Difference (95% CI) |
T-score | P | |
| Intelligence quotient (WASI IQ) | 77.68 (5.10) | 89.74 (2.11) | 12.06 (1.67, 22.45) | 2.276 | 0.023 |
| Gross motor functioning, Mother’s report* | 1.47 (0.17) | 2.22 (0.13) | 0.75 (0.34, 1.16) | 3.601 | 0.000 |
| Adaptive Behavior Assessment-Second Edition (ABAS II),Total Subscale score, parent report* | 272.47 (14.70) | 320.94 (6.55) | 48.47 (16.94, 80.01) | 3.032 | 0.002 |
| Scales of Independent Behavior-Revised (SIB-R) Fine motor, parent report* | 37.50 (3.44) | 44.18 (1.06) | 6.68 (1.19, 12.17) | 2.383 | 0.017 |
| Scales of Independent Behavior-Revised (SIB-R) Time and punctuality subscale, parent report* | 39.77 (2.75) | 42.45 (1.22) | 2.69 (3.16, 8.53) | 0.901 | 0.368 |
| Medical skill mastery: Catheterization, The Spina Bifida Independence Survey (SBIS), parent report* | 76.00 (6.07) | 89.4 (1.68) | 13.41 (1.05, 25.76) | 2.127 | 0.033 |
| Medical adherence: Catheterization, The Spina Bifida Self-Management Profile (SBSMP), parent report* | 4.77 (0.09) | 4.35 (0.07) | −0.42 (−0.64, −0.20) | −3.744 | 0.000 |
higher scores indicate higher function, independence, or adherence
chi-square or Exact Fisher’s test or LR as appropriate
Results of the logistic regression analysis with CIC responsibility trajectory group membership as the outcome variable are presented in Table 4. Only CIC mastery, CIC adherence, and child lesion level were retained in the final model. Higher CIC mastery was associated with higher odds of being in the high-increasing group, whereas higher CIC adherence was associated with lower odds of being in the high-increasing group. Compared to youth with sacral lesions, youth with thoracic lesions had lower odds to be in the high-increasing group.
Table 4.
Multivariate Logistic regression Analysis Predicting Catheterization Responsibility Trajectory Group Membership (high-increasing vs. low)
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Catheterization Mastery | 1.055 | 1.016-1.095 | 0.003 |
| Catheterization Adherence | 0.059 | 0.005-0.648 | 0.004 |
| Child Lesion level | 0.009 | ||
| Thoracic | 0.039 | 0.003-0.487 | |
| Lumbar | 0.158 | 0.014-1.852 | |
| Sacral | Reference group | - |
Discussion
We found that within 89 families of youth with SB followed longitudinally who performed CIC, two distinct trajectory subgroups emerged for CIC responsibility. Most youth with SB exhibited shared-CIC responsibility by age 8-9 years old, with eventual transfer of CIC responsibility completely to the child by age 16-17 years old. However, a smaller subgroup (17% of cohort) of youth never approached even shared-CIC responsibility. Our findings provide evidence about timing of transfer of CIC responsibility, highlight the heterogeneity of youth with SB, and identify several predictors of trajectory group membership that can be targeted for future interventions.
Prior literature on the timing of transfer of CIC responsibility from the caregiver to the child is limited. Of 64 individuals (mean age 18.4; 91% myelomeningocele) who had documented ages at transition from caregiver- to self-CIC, Atchley and colleagues noted in their single-center retrospective study that 13%, 72%, and 88% had transitioned to self-CIC by age 5, 10, and 14 years old, respectively.6 The authors concluded that 10 years old marked the expected age at which transition of CIC responsibility should occur. Similarly, in their retrospective single-center study, Castillo and colleagues evaluated 200 patients who required CIC (age range 3-19 years old; 92% myelomeningocele), of whom 111 did self-CIC and 89 required caregiver-CIC.7 These authors found that the mean age of reaching self-CIC was 9.45 years old. Our results differ from these findings in several respects. The prior literature dichotomized CIC responsibility into “self-CIC” versus “caregiver-CIC” without an intermediate level “shared-CIC” responsibility. This is important because “shared-CIC” marks where the transfer of CIC skill and technique occurs. “Shared-CIC” is a broad category, but reflects the continuous process of acquiring a skill. If the prior studies had classified patients as doing “self-CIC” when they began to perform it but not completely independently, then their results are compatible with ours. In our study, based on Figure 1, we found that the overall trajectory of CIC responsibility crossed the shared-CIC responsibility threshold around the 8-9 year old age group. However, by using group-based trajectory modeling, we demonstrated that a subgroup of youth with SB (nearly 20%) remained heavily reliant on caregiver-CIC regardless of their biologic age, which would be missed by simply using mean ages of CIC independence. In sum, there should be no set, uniform expected age for acquiring self-CIC responsibility among youth with SB.
Our results do support the prior literature on predictors of who will transition to self-CIC. Atchley and colleagues assessed 287 patients who used CIC and were ≥10 years old in their center.6 They compared 175 patients who did self-CIC against 112 who required caregiver-CIC and noted that, with multivariate analyses, thoracic-level spinal lesions and Medicaid insurance status were associated with lower odds of self-CIC. Castillo and colleagues found that thoracic-level spinal lesions were associated with lower rates of self-CIC compared to caregiver-CIC, though they did not test this in multivariate models.7 Similarly, we found in our multivariate models that thoracic-level lesions were associated with lower odds of being in the high-increasing CIC responsibility trajectory group compared to the low-flat trajectory group. In contrast to our hypothesis, IQ was not associated with trajectory group.
We also demonstrated associations of trajectory group membership with CIC mastery and CIC adherence. Greater CIC mastery was associated with greater odds of membership in the high-increasing compared to the low-flat trajectory group. It is important to note that CIC mastery was based on parent-report. If a parent believes that their child has not mastered performing CIC accurately or reliably, the parent may logically be hesitant to transfer full CIC responsibility to the child alone. Interestingly, and to our surprise, we found that higher CIC adherence was associated with membership in the low-flat trajectory group. Since CIC adherence similarly is parent-reported, this finding may reflect the fact that parents may feel they are more strictly adherent to a prescribed CIC schedule when they perform the CIC than when their child performs it.
Our study has certain limitations. First, our sample size is relatively small, but is part of a larger longitudinal prospective cohort study that has been well-characterized, especially with psychosocial and neuropsychological testing. Regardless, because of the small sample size, the generalizability of our results may be limited, although we did include youth with SB from four different hospitals and a Midwestern statewide SB association. Second, we did not have some clinically relevant data, such as whether surgically created channels (e.g., Mitrofanoff) were used for CIC, or reason for CIC or age at which it was started, or whether individuals could transition independently out of wheelchairs. Channels may affect the physical ability to perform self-CIC, especially in non-ambulatory female patients. However, a prior study found no difference in age of self-CIC between those who used a channel versus urethra for CIC.7 We also did not have data prior to age 8 years old, when the high-increasing trajectory group showed shared-CIC responsibility already. Arguably the age to initiate shared-CIC responsibility can be even younger in appropriately-selected patients. Lastly, there may be inherent bias when the caregiver completes the questionnaires (as opposed to a more impartial clinician), such as with parent-reported CIC responsibility, adherence, or mastery.
Our study has several strengths. The advantages of group-based trajectory modeling are evident in the current study and others. Group-based trajectory modeling allows a longitudinal risk assessment and stratification of the natural heterogeneity of a clinical condition. Longitudinal cohorts may exhibit one overall trajectory, but subgroups that exhibit very different trajectories may be masked. In the current study, the overall cohort demonstrated a favorable rising trajectory of CIC responsibility, but this was driven by 83% of the group, with 17% of this group having a low-flat trajectory, consistent with a higher-risk phenotype for never acquiring self-CIC responsibility. Our study also incorporated other domains lacking in prior literature, such as adaptive behavior function, IQ, time and punctuality, and measures of gross- and fine-motor function.
Conclusions
We found that nearly 1 in 5 youth with SB in our cohort persistently required caregiver-CIC over time, but that the remaining 4 in 5 youth had shared-CIC responsibility by age 8-9 years with increasing self-CIC responsibility thereafter. Lesion level was a primary driver, but CIC mastery and adherence, which are more mutable factors, were also predictors of group membership. Our results reinforce that clinical plans and expectations, such as with transfer of CIC responsibility, should be individualized to each unique youth with SB to optimize their abilities and care.
Supplementary Material
Funding:
This work was supported in part by research grants from the National Institute of Diabetes and Digestive and Kidney Diseases (K23 DK125670) to Dr. Chu, and from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD048629), the March of Dimes Birth Defects Foundation (No. 12-FY13-271), and the National Institute of Nursing Research (R01 NR016235), all to Dr. Holmbeck. Dr. Kayle is a consultant on Dr. Holmbeck’s R01 HD048629 and R01 NR016235.
Footnotes
Conflicts of Interest:
None
References
- 1.Lapides J, Diokno AC, Silber SJ et al. : Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol, 107: 458, 1972 [DOI] [PubMed] [Google Scholar]
- 2.Szymanski KM, Cain MP, Whittam B et al. : Incontinence affects health-related quality of life in children and adolescents with spina bifida. J Pediatr Urol, 14: 279 e1, 2018 [DOI] [PubMed] [Google Scholar]
- 3.Moore C, Kogan BA, Parekh A: Impact of urinary incontinence on self-concept in children with spina bifida. J Urol, 171: 1659, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Dik P, Klijn AJ, van Gool JD et al. : Early start to therapy preserves kidney function in spina bifida patients. Eur Urol, 49: 908, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Kaye IY, Payan M, Vemulakonda VM: Association between clean intermittent catheterization and urinary tract infection in infants and toddlers with spina bifida. J Pediatr Urol, 12: 284 e1, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Atchley TJ, Dangle PP, Hopson BD et al. : Age and factors associated with self-clean intermittent catheterization in patients with spina bifida. J Pediatr Rehabil Med, 11: 283, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castillo J, Ostermaier KK, Fremion E et al. : Urologic self-management through intermittent self-catheterization among individuals with spina bifida: A journey to self-efficacy and autonomy. J Pediatr Rehabil Med, 10: 219, 2017 [DOI] [PubMed] [Google Scholar]
- 8.Kayle M, Chu DI, Stern A et al. : Predictors of Distinct Trajectories of Medical Responsibility in Youth with Spina Bifida. J Pediatr Psychol, 45: 1153, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Driscoll CFB, Ohanian DM, Ridosh MM et al. : Pathways by which Maternal Factors are Associated With Youth Spina Bifida-Related Responsibility. J Pediatr Psychol, 45: 610, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Psihogios AM, Kolbuck V, Holmbeck GN: Condition Self-Management in Pediatric Spina Bifida: A Longitudinal Investigation of Medical Adherence, Responsibility-Sharing, and Independence Skills. J Pediatr Psychol, 40: 790, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holmbeck GN, Kritikos TK, Stern A et al. : The Transition to Adult Health Care in Youth With Spina Bifida: Theory, Measurement, and Interventions. J Nurs Scholarsh, 53: 198, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wechsler D: Manual for the Wechsler Abbreviated Intelligence Scale (WASI): The Psychological Corporation, 1999 [Google Scholar]
- 13.Harrison PL, Oakland T: Adaptive Behavior Assessment System - Second Edition (ABAS-II): The Psychological Corporation, 2003 [Google Scholar]
- 14.Palisano RJ, Rosenbaum P, Bartlett D et al. : Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol, 50: 744, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Bruininks RH, Woodcock RW, Weatherman RF et al. : Scales of Independent Behavior-Revised Comprehensive Manual: Riverside Publishing., 1996 [Google Scholar]
- 16.Wysocki T, Meinhold PM, Taylor A et al. : Psychometric properties and normative data for the parent version of the diabetes independence survey. Diabetes Educ, 22: 587, 1996 [DOI] [PubMed] [Google Scholar]
- 17.Wysocki T, Gavin L: Paternal involvement in the management of pediatric chronic diseases: associations with adherence, quality of life, and health status. J Pediatr Psychol, 31: 501, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Jones BL, Nagin DS, Roeder K: A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories Sociological Methods & Research, 29: 374, 2001 [Google Scholar]
- 19.Jones BL: Traj group-based modeling of longitudinal data, vol. 2021, 2021 [Google Scholar]
- 20.Miller VA, Jawad AF: Decision-Making Involvement and Prediction of Adherence in Youth With Type 1 Diabetes: A Cohort Sequential Study. J Pediatr Psychol, 44: 61, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagin DS: Model Selection. In: Group-Based Modeling of Development. Cambridge, MA: Harvard University Press, pp. 61–77, 2005 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.