Abstract
Objective
We describe the most frequently used musculoskeletal diagnoses in Veterans Health Administration care. We report the number of visits and patients associated with common musculoskeletal International Classification of Diseases (ICD)-10 codes and compare trends across primary and specialty care settings.
Design
Secondary analysis of a longitudinal cohort study.
Subjects
Veterans included in the Musculoskeletal Diagnosis Cohort with a musculoskeletal diagnosis from October 1, 2015, through September 30, 2017.
Methods
We obtained counts and proportions of all musculoskeletal diagnosis codes used and the number of unique patients with each musculoskeletal diagnosis. Diagnosis use was compared between primary and specialty care settings.
Results
Of more than 6,400 possible ICD-10 M-codes describing “Diseases of the Musculoskeletal System and Connective Tissue,” 5,723 codes were used at least once. The most frequently used ICD-10 M-code was “Low Back Pain” (18.3%), followed by “Cervicalgia” (3.6%). Collectively, the 100 most frequently used codes accounted for 80% of M-coded visit diagnoses, and 95% of patients had at least one of these diagnoses. The most common diagnoses (spinal pain, joint pain, osteoarthritis) were used similarly in primary and specialty care settings.
Conclusion
A diverse sample of all available musculoskeletal diagnosis codes were used; however, less than 2% of all possible codes accounted for 80% of the diagnoses used. This trend was consistent across primary and specialty care settings. The most frequently used diagnosis codes describe the types of musculoskeletal conditions, among a large pool of potential diagnoses, that prompt veterans to present to the Veterans Health Administration for musculoskeletal care.
Keywords: International Classification of Diseases, Musculoskeletal Diseases/Diagnosis*, Musculoskeletal Pain/Diagnosis*, Veterans
Introduction
The United States adopted the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) on October 1, 2015, which resulted in an expansion from 14,000 diagnostic codes in the Ninth Revision (ICD-9) to nearly 70,000 in ICD-10 [1]. The rationale for this transition included increased diagnostic specification and enhanced data quality for research and public health uses, clinical decision-making, outcomes measurement, and claims processing and reimbursement [1, 2]. There have been no studies describing the actual use patterns of ICD-10 diagnostic codes or the most frequently used codes in the clinical setting. Describing actual use patterns within a diagnostic subgroup provides data on what conditions are being treated most frequently in a health system and the treatment setting in which patients are diagnosed (e.g., primary care vs specialty care).
Musculoskeletal conditions are one example of a diagnostic subgroup where changes in the number and specificity of codes (i.e., including codes to identify condition laterality and anatomic site involvement) occurred in the transition from ICD-9 to ICD-10. “Diseases of the Musculoskeletal System and Connective Tissue” are now represented by more than 6,400 ICD-10 codes, compared with 892 similar ICD-9 codes [3].
We recognize the transition to ICD-10 as an opportunity in health services research to examine early use of ICD-10 codes within a single health system. As the largest integrated health care system in the United States with a research division devoted to health services research and system-level examination of electronic health record data, the Veterans Health Administration (VHA) provides a unique resource for describing the use of ICD-10 [4]. The burden of musculoskeletal disorders is well established in veterans receiving health care in the VHA [5–9]. VHA data provide the advantage of being relatively independent from third-party payer influence as compared with other health systems.
We examined the use of ICD-10 diagnostic “M-codes,” representing “Diseases of the Musculoskeletal System and Connective Tissue,” in the VHA. The primary aim of this analysis was to describe the most frequently assigned musculoskeletal condition diagnoses across visits and across unique patients in VHA care. We also examined diagnosis code use in primary and specialty care settings. We hypothesized that specialty care settings may show relatively greater use of specific ICD-10 codes to describe musculoskeletal conditions, as compared with primary care, because of the model of referral and triage from primary care with a more generalized diagnosis to specialty care for further evaluation and confirmatory or definitive diagnosis. In an exploratory aim, we compared the use of diagnoses across similar top-level groupings of ICD-10 M-codes to assess use patterns across types of conditions by anatomic region and/or condition etiology.
Methods
Musculoskeletal Diagnosis Cohort
Data were obtained from the Musculoskeletal Diagnosis (MSD) Cohort, a longitudinal cohort of veterans with musculoskeletal diagnoses who received VHA care between January 1, 2000, and September 30, 2017 (n = 7,133,669) [5]. Patients were included in the cohort on the basis of a search of VHA electronic health record data sources for the presence of at least one of a possible 1,685 ICD-9 musculoskeletal diagnoses or 27,221 ICD-10 musculoskeletal diagnoses received during two or more outpatient visits within 18 months or one or more inpatient stay(s). This algorithm was chosen by the MSD authors to reflect relatively greater confidence in inpatient coding, given that inpatient codes are assigned by professional coders after medical record review with an emphasis on completeness in service of reimbursement, relative to outpatient care codes, which are entered by a single provider at the time of encounter [5].
Additional sociodemographic and clinical data were extracted from the VHA Corporate Data Warehouse to allow for longitudinal analyses after entry into the cohort. Corporate Data Warehouse data include the records of VHA inpatient and outpatient visits, including patient demographics, diagnostic and procedure codes, and clinical note documentation.
Analysis of ICD-10 Code Use
For the present analysis, our sample included all patients from the MSD Cohort with at least one M-code musculoskeletal diagnosis during an outpatient visit from October 1, 2015, through September 30, 2017—the first 2 years after ICD-10 implementation. This study period overlapped the final 2 years, during which new, eligible patients were included in the MSD Cohort. For patients who entered the MSD Cohort before October 1, 2015, only one ICD-10 M-code from an outpatient visit was needed to enter our subset. For patients who had not previously entered the MSD Cohort on October 1, 2015, one qualifying MSD Cohort entry diagnosis was needed to enter the MSD Cohort before September 30, 2017, with a second confirmatory diagnosis within 18 months of the first diagnosis. Once entered in the MSD Cohort, an individual needed only one ICD-10 M-code to be included in our subset. An individual with only one ICD-10 M-code during our study period and no additional qualifying MSD Cohort entry diagnoses would not be included in our subset.
Sociodemographic variables for our sample based on MSD Cohort entry date included sex, race/ethnicity, marital status, body mass index, and pain intensity numeric rating scale score. Age as of the beginning of our study period (October 1, 2015) was calculated from patient date of birth. We identified the most frequently used M-code diagnoses across all visits with an M-code and calculated the proportion of all patients in our sample who had a given code used during at least one encounter. Next, using VHA administrative clinic identifier codes (known as stop codes) to identify primary care visits, we compared the musculoskeletal diagnosis codes used in primary care and specialty care settings. Primary care included traditional primary care, women’s health primary care, and home-based primary care. We determined the proportion of each M-code diagnosis assigned in primary care and specialty care visits, as well as the cumulative frequency distribution for each care setting.
In an exploratory analysis, we organized the top-level groupings of M-codes (Mxx) in the ICD-10 hierarchy into nine groupings of conditions based on anatomic region or etiology of condition to explore use patterns. Groupings included “Infectious or Inflammatory Arthropathies” (M00.x—M02.x, M04.x, M05.x—M14.x), “Osteoarthritis” (M15.x—M19.x), “Peripheral Joint Disorders” (M20.x—M25.x), “Dentofacial Disorders” (M26.x—M27.x), “Connective/Soft Tissue Disorders” (M30.x—M36.x, M60.x—M63.x, M65.x—M67.x, M70.x—M79.x), “Spinal Disorders” (M40.x—M43.x, M45.x—M49.x, M50.x—M54.x), “Osteopathies” (M80.x—M85.x, M86.x—M90.x), “Chondropathies” (M91.x—M94.x), and “Other Disorders” (M95.x, M96.x, M97.x, M99.x). Spinal disorders (including spondylopathies, deforming dorsopathies, and other dorsopathies) and peripheral joint disorders were grouped by involvement of similar anatomic regions. All other groupings were organized by similar pathophysiology and/or tissue type involvement (i.e., soft tissue involvement, osseous tissue involvement, etc.).
This study was approved by the Institutional Review Board of the VA Connecticut Healthcare System.
Results
Sample Demographics
Between October 1, 2015, and September 30, 2017, there were 3,497,545 unique patients from the MSD Cohort who met the eligibility criteria for our sample. These patients received 31,100,151 individual musculoskeletal diagnoses across all outpatient visits. Table 1 presents the sociodemographic and clinical characteristics of our sample.
Table 1.
Demographic characteristics of sample of patients from MSD Cohort with M-code diagnoses from October 1, 2015, through September 30, 2017
| Variable | Total |
|---|---|
| N | 3,497,545 |
| Age, mean, y | 59.5 |
| Sex, % | |
| Female | 9.2 |
| Male | 90.8 |
| Race/ethnicity, % | |
| White | 68.8 |
| Black | 19.3 |
| Hispanic | 6.7 |
| Other | 5.2 |
| Marital status, % | |
| Married | 54.4 |
| Divorced/separated | 26.9 |
| Single/never married | 12.9 |
| Widowed | 5.0 |
| Unknown/other | 0.7 |
| NRS pain score, % | |
| No pain (NRS = 0) | 26.7 |
| Mild pain (NRS = 1–3) | 12.9 |
| Moderate pain (NRS = 4–6) | 20.2 |
| Severe pain (NRS = 7–10) | 17.8 |
| Missing | 22.3 |
| Body mass index, mean, kg/m2 | 30.0 |
Diagnosis Frequency by Visit Diagnosis and Unique Patient
Of the more than 6,400 ICD-10 M-code diagnoses available, 5,723 were used at least once. Over the 2-year study period, 61% of codes used (3,463 codes) were used fewer than 100 times and 28% (1,628 codes) were used fewer than 10 times across all approximately 31 million musculoskeletal diagnoses. “Low Back Pain” (M54.5) was the most frequently used diagnostic code (18.3%) across all M-coded visit diagnoses, followed by “Cervicalgia” (M54.2, 3.6%).
The 10 most common diagnoses, by visit and by patient, are presented in Table 2. The most common diagnoses were generally consistent across visits and patients. Low back pain, neck pain, knee pain, shoulder pain, gout, and osteoarthritis were the most common diagnoses, both by visit and by patient. “Generalized Muscle Weakness” (M62.81) was the fifth most common diagnosis by M-coded visit diagnoses (2.8%) but was the twelfth most common diagnosis by patient (5.2%). “Unspecified Osteoarthritis, Unspecified Site” (M19.90) was the ninth most common diagnosis by patient (6.1%) and the twelfth most common diagnosis by visit (1.3%). Frequency of use for each of the 100 most common M-code diagnoses, both individually and as a cumulative sum, are presented in Supplementary Data Table 1.
Table 2.
Ten most common ICD-10 M-Codes, by visit and by patient
| By Visit | By Patient | |
|---|---|---|
| 1 | M54.5—Low Back Pain (18.3%) | M54.5—Low Back Pain (43.1%) |
| 2 | M54.2—Cervicalgia (3.6%) | M25.561—Pain in Right Knee (10.8%) |
| 3 | M25.561—Pain in Right Knee (3.1%) | M54.2—Cervicalgia (10.6%) |
| 4 | M25.562—Pain in Left Knee (2.9%) | M25.562—Pain in Left Knee (10.2%) |
| 5 | M62.81—Muscle Weakness, Generalized (2.8%) | M25.569—Pain in Unspecified Knee (9.7%) |
| 6 | M25.511—Pain in Right Shoulder (2.8%) | M25.511—Pain in Right Shoulder (8.6%) |
| 7 | M25.569—Pain in Unspecified Knee (2.4%) | M25.512—Pain in Left Shoulder (7.5%) |
| 8 | M25.512—Pain in Left Shoulder (2.4%) | M10.9—Gout, Unspecified (6.9%) |
| 9 | M10.9—Gout, Unspecified (2.0%) | M19.90—Unspecified Osteoarthritis, Unspecified Site (6.1%) |
| 10 | M17.9—Osteoarthritis of Knee, Unspecified (1.5%) | M17.9—Osteoarthritis of Knee, Unspecified (5.3%) |
Percentage of total visits (n = 31,100,151) and patients (n = 3,497,545) given in parentheses.
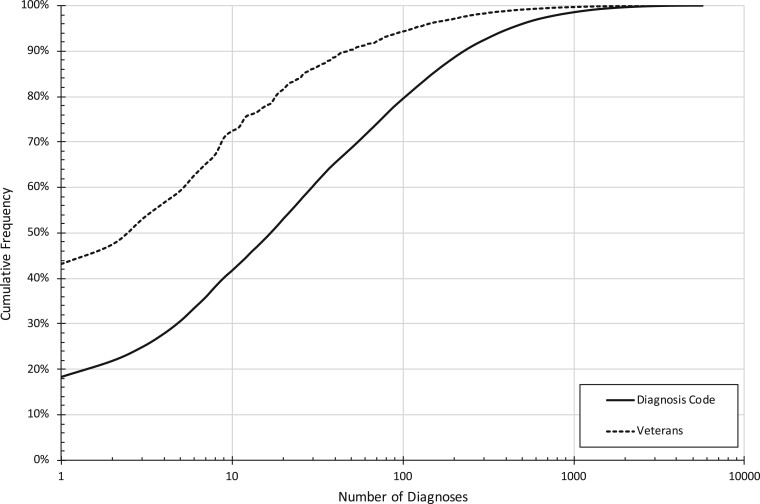
Figure 1 presents the cumulative frequency distribution for individual diagnoses and unique patients. The 10 most commonly used diagnoses account for nearly 42% of all M-code diagnoses, with 72% of patients receiving care for at least one of these diagnoses. Similarly, the 100 most commonly used diagnoses account for nearly 80% of all diagnoses and include 95% of patients.
Figure 1.
Cumulative frequency distribution of ICD-10 “M-Code” diagnoses, based on visit diagnoses (solid line) and unique veterans (dashed line), ordered by total visit diagnosis frequency.
Diagnosis Frequency by Primary and Specialty Care Setting
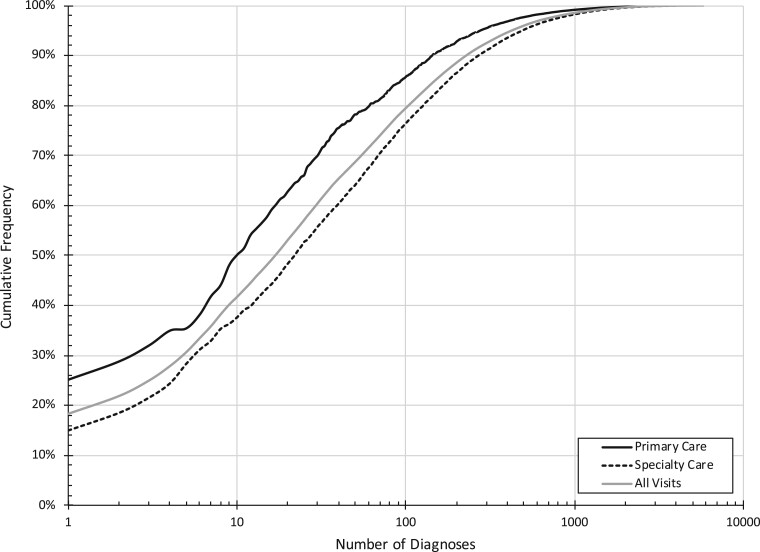
Of the 31,100,151 diagnoses examined, 10,216,589 (32.9%) occurred in primary care settings. Supplementary Data Table 1 shows the distribution of diagnosis use across primary and specialty care for the 100 most common diagnoses. Many of the most commonly used diagnoses followed a similar use pattern across both care settings (Figure 2), with “Low Back Pain” (M54.5) being the most common in both (25.1% of all primary care M-code diagnoses and 15.0% of all specialty care M-code diagnoses). Diagnoses including arthritis, unspecified joint pain, and gout were more common in primary care, including “Pain in Unspecified Knee” (M25.569; 50.2% of total diagnosis use), “Gout, Unspecified” (M10.9; 66.6%), “Unspecified Osteoarthritis, Unspecified Site” (M19.90; 63.4%), “Primary Osteoarthritis, Unspecified Site” (M19.91; 68.5%), “Pain in Unspecified Joint” (M25.50; 57.3%), “Polyarthritis” (M13.0; 58.1%), “Chronic Gout, Unspecified, Without Tophus (Tophi)” (M1A.9XX0; 62.5%), and “Other Specified Arthritis, Multiple Sites” (M13.89; 63.4%). Codes describing podiatric conditions were more frequently used in specialty care settings, including “Other Hammer Toe(s) (Acquired)” of the right (M20.41; 97.5%), left (M20.42; 97.8%), or unspecified foot (M20.40; 95.1%); “Hallux Valgus (Acquired)” of the right (M20.11; 95.7%), left (M20.12; 96.0%), or unspecified foot (M20.10; 91.2%); and “Flat Foot [Pes Planus] (Acquired)” of the left foot (M21.42; 93.8%) or the right foot (M21.41; 93.8%). Codes describing “Segmental and Somatic Dysfunction” of the lumbar spine (M99.03; 98.0%), thoracic spine (M99.02; 97.7%), and cervical spine (M99.01; 97.6%) were also more frequently used in specialty care settings. Codes describing “Complete Rotator Cuff Tear or Rupture” of the right shoulder (M75.121; 90.5%) or left shoulder (M75.122; 90.6%) were more commonly used in specialty care settings. Notably, “Muscle Weakness (Generalized)” (M62.81; 94.6%) and “Osteomyelitis” (M86.9; 92.2%) were also used primarily in specialty care settings. Of the 3,463 diagnoses used fewer than 100 times, 2,527 were used more frequently in a specialty care setting (73.0%), and of the 1,628 diagnoses used fewer than 10 times, 1,158 were used more frequently in a specialty care setting (71.1%).
Figure 2.
Cumulative frequency distribution of ICD-10 “M-Code” diagnoses by care setting for primary care (solid line) and specialty care (dashed line), ordered by total visit diagnosis frequency. Cumulative frequency distribution for all visit diagnoses is shown in grey.
Diagnosis Frequency by Condition Grouping
The most common group of conditions across all diagnoses was Spinal Conditions (35.6% of all diagnoses), followed by Peripheral Joint Disorders (26.0%), Connective/Soft Tissue Disorders (17.8%), and Osteoarthritis (10.4%). For all condition groupings, a negative exponential distribution described the pattern of code use across all codes used, with very few codes having exceptionally frequent use within each grouping. For example, “Low back pain” (M54.5) and “Cervicalgia” (M54.2) accounted for 61.4% of all Spinal Disorders diagnoses, with a rapid drop-off in frequency beyond these two codes. Joint Disorders demonstrated a more gradual decrease across the five most common codes (describing pain in the knee with known or unknown laterality and pain in the shoulder with known laterality), followed by a rapid decrease beyond these codes. All groupings reached a “steady state” of less than 1% of code use in each grouping between the tenth and twenty-third most common M-codes.
Discussion
To our knowledge, this is the first study to describe early ICD-10 use in musculoskeletal-related care. We found that of more than 6,400 ICD-10 M-codes describing “Diseases of the Musculoskeletal System and Connective Tissue,” only 1.6% of codes accounted for more than 80% of the total diagnoses recorded in clinical care. Low back pain was the most frequently used code, and 43% of the unique patients in the sample received this diagnosis. Ten diagnosis codes account for nearly 42% of all M-code diagnoses, with 72% of patients receiving care for at least one of these diagnoses. Similarly, the 100 most commonly used diagnoses account for nearly 80% of all diagnoses and include 95% of patients. Our results highlight a contrast between the potential for diagnostic specification introduced by the ICD-10 and real-world use of only a small subset of available diagnosis codes in most cases. The patterns of code use can provide valuable information about the types of conditions commonly treated in the health system and may facilitate resource allocation toward the most commonly treated conditions. Although the ICD-10 system has increased the number of codes available to describe conditions for which patients are presenting for care, clinicians continue to use mostly general, nonspecific codes in the majority of cases, possibly because the most common musculoskeletal conditions are themselves largely nonspecific.
The sample used in this study was a subset of the larger MSD Cohort of patients with musculoskeletal conditions and was similar in sociodemographic and clinical characteristics to the original cohort [5] and other published demographic data from the National Center for Veterans Analysis and Statistics (NCVAS) [10–12]. The proportion of female veterans in our sample (9.2%) was similar to data for veterans reported by the NCVAS (9.6%) during 2017 [10]. There was a slightly greater difference in the proportion of white, non-Hispanic/Latinx veterans between our sample (68.8%), data from the NCVAS (75.6%) [12], and data from the original MSD Cohort as of 2011 (73.6%) [5]. We hypothesize this variation to be due to continued increase in the diversity of the general veteran population and to NCVAS-reported data representing the entire veteran population and not just those receiving VHA health care [11, 12].
Our findings are consistent with previous studies that show veterans are most likely to report and present with low back pain, neck pain, and joint conditions as compared with other types of musculoskeletal disorders [13–15]. With respect to groupings of diagnoses, the original MSD Cohort study found that the most common cohort entry diagnoses were nontraumatic joint disorders, back disorders, and osteoarthritis [5]. As of 2011, there was an increasing prevalence in joint disorders, back disorders, and neck pain disorders, with a decrease in osteoarthritis, in this cohort. The proportion of spinal disorders (back disorder plus neck pain disorders), joint disorders, and osteoarthritis in our sample is consistent with these trends. Data from the Global Burden of Disease study from 2010 and 2019 similarly showed spinal conditions as the most common musculoskeletal condition; identified osteoarthritis as the most prevalent joint condition; and found spinal conditions, osteoarthritis, and joint conditions to be increasingly more common and more burdensome with respect to disability [16–21].
The ICD-10 system revisions related to musculoskeletal care involved increasing anatomic specification by including additional codes to describe condition laterality and anatomic site involvement [22]. However, among musculoskeletal disorders, conditions without an easily identifiable pathoanatomic cause are common—for example, nonspecific low back pain [23–26]. Increasing diagnostic specification must be balanced with potential overutilization of health care services [27–30], especially given recommendations advising against unnecessary advanced diagnostic and imaging procedures for spinal and extremity musculoskeletal conditions that do not alter clinical decision-making, patient management, or care planning [31–33]. Given the high prevalence of asymptomatic abnormalities detected on advanced diagnostic procedures related to musculoskeletal disorders, there is a risk of overtreatment and “labeling” patients, which could lead to an increase in patient anxiety and treatment seeking [26, 34].
We examined diagnostic code use across both primary care and specialty care settings and found consistent use of the most common diagnoses across clinical settings, with only a few used primarily in one setting relative to the other. The diagnoses that were more commonly used in primary care settings included mainly those related to arthritis and gout. This could be expected, as primary care management of these conditions is common.
Furthermore, diagnoses that were more frequently used in specialty care settings, such as muscle weakness, osteomyelitis, and foot conditions, were those that often require interventions or expertise that reside outside primary care. Muscle weakness may require referral to specialty care intervention, including neurology and neurosurgery, which likely explains its disproportionate use in specialty care. Similarly, patients with osteomyelitis may require referral for advanced imaging with specialty care confirmation of a preliminary diagnosis made in a primary care setting or require management involving surgical intervention/debridement. Diagnoses related to several foot-related conditions were more common in specialty care, which may be expected given that their management most often occurs in podiatry clinics.
Regardless of care setting, treatment of musculoskeletal disorders is largely similar across similar conditions [35–40], including multimodal, team-based treatments that minimize reliance on opioid medications and promote self-management through a variety of nonpharmacological interventions. Among nonpharmacological interventions, several have been found to have small to moderate positive effects on pain-related outcomes, but there is little evidence of superiority for any specific treatment. Given the commonality in care plans across conditions and that evidence to guide clinical management toward highly specified intervention for many general musculoskeletal conditions is limited, more specific or detailed diagnosis codes likely have diminished importance for most patients with musculoskeletal disorders. Additionally, given that more specific musculoskeletal diagnoses often do not necessarily lead to divergent management from broadly categorized guidelines, the added complexity of the ICD-10 diagnosis system may be well designed for use in a pathology-based model but may not have the same level of utility in the classification models common to musculoskeletal management [41–44]. Further studies should evaluate the impact of selection of specific and nonspecific diagnostic codes on management and, most importantly, on patient outcomes.
We recognize several limitations to the interpretation and application of these findings. We used the MSD Cohort as an existing dataset of patients with musculoskeletal conditions. The MSD Cohort is biased toward including chronic cases because of eligibility criteria requiring two ICD diagnosis codes within 18 months for outpatient visits. Individuals with episodic complaints spaced greater than 18 months apart or those with an acute but short-lived musculoskeletal condition are less likely to be included in the cohort.
Although patients could enter the MSD Cohort and our subset simultaneously during our study period (with at least two qualifying outpatient MSD Cohort entry diagnoses), we may have excluded individuals with only a single M-code diagnosis during this period. However, we suspect this scenario to be infrequent, given that our sample reasonably represents the population of the patients receiving VHA health care (including specifically for musculoskeletal disorders) and that most VHA users have at least one health care visit per year.
We examined data from the first 2 years of ICD-10 implementation, which may capture a learning curve associated with the initial use of these new codes. Increased familiarity with the use of ICD-10 in the clinical setting may mean that some of the less frequently recorded diagnoses become more commonly used over time, which may yield different results in the future.
Furthermore, we included only M-code diagnoses representative of “Diseases of the Musculoskeletal System and Connective Tissue” as defined by ICD-10. This subset of diagnoses is not comprehensive of all conditions related to the musculoskeletal system, particularly those of traumatic origin.
We examined only diagnoses that occurred in outpatient visits in patients with a history of musculoskeletal disorders, and the use of the ICD-10 coding system in inpatient care may be different. It is not clear whether these patients’ previous musculoskeletal-related visits may have indirectly influenced provider diagnostic coding of future visits. Given the relative independence between VHA and third-party payer reimbursement, these findings may describe practice only within a fully capitated model. Conversely, we may be describing coding practices that are less influenced by reimbursement and more representative of the diagnosing provider’s clinical reasoning and thought process at the point of care.
The present study does not identify a specific reason for low uptake of many codes. It may be attributable to the actual epidemiological distribution of musculoskeletal disorders in the VHA, as well as a provider’s willingness or capacity to adopt the more complex ICD-10 coding system. Other issues, such as features of the clinical workflow and/or the electronic health record user interface or relative freedom from third-party reimbursement in VHA, may also play a role. We consider our findings from the VHA as a starting point that describes early use of ICD-10 in musculoskeletal care across a national health care system and may support future comparisons of adoption in other health systems.
Conclusion
We found that although a diverse sample of all available ICD-10 M-codes were used during the first 2 years after implementation, less than 2% accounted for the vast majority of diagnoses used. The most common codes used were primarily nonspecific and described more general conditions for which patients most often present, while a wide array of more detailed codes were used less frequently. Future research should go beyond our descriptive analysis to critically evaluate ICD-10 in the context of its proposed benefits, especially the value of diagnostic specificity in relation to providing high-quality musculoskeletal care.
Supplementary Data
Supplementary Data may be found online at http://painmedicine.oxfordjournals.org.
Supplementary Material
Contributor Information
Brian C Coleman, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Joseph L Goulet, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Diana M Higgins, Anesthesiology, Critical Care, and Pain Medicine Service, VA Boston Healthcare System, Boston, Massachusetts; Boston University School of Medicine, Boston, Massachusetts.
Harini Bathulapalli, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Todd Kawecki, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Christopher B Ruser, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Lori A Bastian, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Steve Martino, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
John D Piette, Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, Michigan; University of Michigan School of Public Health, Ann Arbor, Michigan, USA.
Sara N Edmond, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Alicia A Heapy, Pain Research, Informatics, Multimorbidities, and Education (PRIME) Center, VA Connecticut Healthcare System, West Haven, Connecticut; Yale School of Medicine, Yale University, New Haven, Connecticut.
Funding sources: This work was supported by the United States Department of Veterans Affairs, Veterans Health Administration, Office of Academic Affiliations, Office of Research and Development, and by the United States Department of Veterans Affairs Health Services Research and Development Service (HSR&D) Award # IIR-16-262 (Goulet, PI), HSR&D Award # IIR 12-118, and HSR&D Award # CIN 13-407. Research reported in this publication was also supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under Award Number UG3 AT009767. JDP receives support as a VA HSR&D Research Career Scientist.
Conflicts of interest: The authors have no additional conflicts of interest, financial or otherwise, to disclose.
Disclaimer: The contents of this manuscript represent the view of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or United States Government. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This article is a product of the NIH-DoD-VA Pain Management Collaboratory. For more information about the Collaboratory, visit https://painmanagementcollaboratory.org/.
References
- 1.U.S. Centers for Disease Control and Prevention, National Center for Health Statistics. International Classification of Diseases (ICD-10-CM/PCS) transition—background. Available at: https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm (accessed August 27, 2018).
- 2. Bowman S. Why ICD-10 is worth the trouble. J AHIMA 2008;79(3):24–9. [PubMed] [Google Scholar]
- 3.U.S. Centers for Medicare & Medicaid Services. ICD-9-CM diagnosis and procedure codes: abbreviated and full code titles. Available at: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html (accessed April 15, 2019).
- 4. Justice AC, Erdos J, Brandt C, et al. The Veterans Affairs Healthcare System: A unique laboratory for observational and interventional research. Med Care 2006;44(8 suppl 2):S7–12. [DOI] [PubMed] [Google Scholar]
- 5. Goulet JL, Kerns RD, Bair M, et al. The Musculoskeletal Diagnosis Cohort: Examining pain and pain care among veterans. Pain 2016;157(8):1696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dorflinger L, Moore B, Goulet J, et al. A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management. J Gen Intern Med 2014;29(suppl 4):870–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haskell SG, Brandt CA, Krebs EE, et al. Pain among veterans of operations Enduring Freedom and Iraqi Freedom: Do women and men differ? Pain Med 2009;10(7):1167–73. [DOI] [PubMed] [Google Scholar]
- 8. Haskell SG, Mattocks K, Goulet JL, et al. The burden of illness in the first year home: Do male and female VA users differ in health conditions and healthcare utilization. Womens Health Issues 2011;21(1):92–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Higgins DM, Fenton BT, Driscoll MA, et al. Gender differences in demographic and clinical correlates among veterans with musculoskeletal disorders. Womens Health Issues 2017;27(4):463–70. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Minority Veterans report: military service history and VA benefit utilization statistics. Published March 2017. Available at: https://www.va.gov/vetdata/docs/SpecialReports/Minority_Veterans_Report.pdf (accessed March 18, 2021).
- 11.U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. VA utilization profile—FY 2017. Published May 2020. Available at: https://www.va.gov/vetdata/docs/Quickfacts/VA_Utilization_Profile_2017.pdf (accessed March 18, 2021).
- 12.U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Veteran population. Published March 12, 2021. Available at: https://www.va.gov/vetdata/veteran_population.asp (acceessed March 18, 2021).
- 13. Lisi AJ, Brandt CA. Trends in the use and characteristics of chiropractic services in the Department of Veterans Affairs. J Manipulative Physiol Ther 2016;39(5):381–6. [DOI] [PubMed] [Google Scholar]
- 14. Hinojosa R, Hinojosa MS. Activity-limiting musculoskeletal conditions in US veterans compared to non-veterans: Results from the 2013 National Health Interview Survey. PLoS One 2016;11(12):e0167143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beehler GP, Rodrigues AE, Mercurio-Riley D, Dunn AS. Primary care utilization among veterans with chronic musculoskeletal pain: A retrospective chart review. Pain Med 2013;14(7):1021–31. [DOI] [PubMed] [Google Scholar]
- 16. Storheim K, Zwart J-A. Musculoskeletal disorders and the Global Burden of Disease study. Ann Rheum Dis 2014;73(6):949–50. [DOI] [PubMed] [Google Scholar]
- 17. Hoy D, March L, Brooks P, et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73(6):968–74. [DOI] [PubMed] [Google Scholar]
- 18. Hoy D, March L, Woolf A, et al. The global burden of neck pain: Estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73(7):1309–15. [DOI] [PubMed] [Google Scholar]
- 19. Smith E, Hoy DG, Cross M, et al. The global burden of other musculoskeletal disorders: Estimates from the Global Burden of Disease 2010 Study. Ann Rheum Dis 2014;73(8):1462–9. [DOI] [PubMed] [Google Scholar]
- 20. Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain—where to from here? Am J Public Health 2019;109(1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease Study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021;396(10267):2006–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Averill RB, Butler RR. Misperceptions, misinformation, and misrepresentations: The ICD-10-CM/PCS saga. J AHIMA 2013. Available at: https://library.ahima.org/doc?oid=301014#.YKe7Py9h3X8 (accessed March 18, 2021). [Google Scholar]
- 23. Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332(7555):1430–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389(10070):736–47. [DOI] [PubMed] [Google Scholar]
- 25. Hartvigsen J, Hancock MJ, Kongsted A et al. ; Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention. Lancet 2018;391(10137):2356–67. [DOI] [PubMed] [Google Scholar]
- 26. Deyo RA. Diagnostic evaluation of LBP: Reaching a specific diagnosis is often impossible. Arch Intern Med 2002;162(13):1444–7. [DOI] [PubMed] [Google Scholar]
- 27. Lemmers GPG, van Lankveld W, Westert GP, van der Wees PJ, Staal JB. Imaging versus no imaging for low back pain: A systematic review, measuring costs, healthcare utilization and absence from work. Eur Spine J 2019;28(5):937–50. [DOI] [PubMed] [Google Scholar]
- 28. Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet 2017;390(10090):156–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.PerryUndem Research/Communication. Unnecessary tests and procedures in the health care system. The ABIM Foundation. Published May 1, 2014. Available at: http://www.choosingwisely.org/wp-content/uploads/2015/04/Final-Choosing-Wisely-Survey-Report.pdf (accessed April 29, 2019).
- 30. Carroll AE. The high costs of unnecessary care. JAMA 2017;318(18):1748–9. [DOI] [PubMed] [Google Scholar]
- 31. Bussieres AE, Taylor JA, Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults-an evidence-based approach-part 3: Spinal disorders. J Manipulative Physiol Ther 2008;31(1):33–88. [DOI] [PubMed] [Google Scholar]
- 32. Bussieres AE, Peterson C, Taylor JA. Diagnostic imaging guideline for musculoskeletal complaints in adults—an evidence-based approach, Part 2: Upper extremity disorders. J Manipulative Physiol Ther 2008;31(1):2–32. [DOI] [PubMed] [Google Scholar]
- 33. Bussieres AE, Taylor JA, Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults—an evidence-based approach, Part 1: Lower extremity disorders. J Manipulative Physiol Ther 2007;30(9):684–717. [DOI] [PubMed] [Google Scholar]
- 34. Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 2015;36(4):811–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Interagency Pain Research Coordinating Committee. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. Washington, DC: US Department of Health and Human Services, National Institutes of Health; 2016. [Google Scholar]
- 36. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: Systematic review. Br J Sports Med 2020;54(2):79–86. [DOI] [PubMed] [Google Scholar]
- 37. Kligler B, Bair MJ, Banerjea R, et al. Clinical policy recommendations from the VHA state-of-the-art conference on non-pharmacological approaches to chronic musculoskeletal pain. J Gen Intern Med 2018;33(suppl 1):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Becker WC, DeBar LL, Heapy AA, et al. A research agenda for advancing non-pharmacological management of chronic musculoskeletal pain: Findings from a VHA state-of-the-art conference. J Gen Intern Med 2018;33(suppl 1):11–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Caneiro JP, Roos EM, Barton CJ, et al. It is time to move beyond ‘body region silos’ to manage musculoskeletal pain: Five actions to change clinical practice. Br J Sports Med 2020;54(8):438–9. [DOI] [PubMed] [Google Scholar]
- 40. Driscoll MA, Kerns RD. Integrated, team-based chronic pain management: Bridges from theory and research to high quality patient care. Adv Exp Med Biol 2016;904:131–47. [DOI] [PubMed] [Google Scholar]
- 41. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: Identifying and staging patients for conservative treatment. Physical Therapy 1995;75(6):470–85. [DOI] [PubMed] [Google Scholar]
- 42. Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: Evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther 2007;37(6):290–302. [DOI] [PubMed] [Google Scholar]
- 43. Karayannis NV, Jull GA, Hodges PW. Physiotherapy movement based classification approaches to low back pain: Comparison of subgroups through review and developer/expert survey. BMC Musculoskelet Disord 2012;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Alrwaily M, Timko M, Schneider M, et al. Treatment-based classification system for low back pain: Revision and update. Phys Ther 2016;96(7):1057–66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.