Abstract
Background: Clinic-to-clinic telemedicine can increase visit frequency in pediatric patients with type 1 diabetes (T1D) living far from a diabetes specialty clinic, but the impact on adoption of diabetes technology is unclear.
Materials and Methods: Pediatric patients with T1D in Colorado and surrounding states who received diabetes care using clinic-to-clinic telemedicine were enrolled. Medical records and surveys were reviewed to ascertain technology use, and data were compared to patients from the main clinic population.
Results: Patients (N = 128, baseline mean age 12.4 ± 4.2 years, median T1D duration 3.3 years [IQR 1.4–7.7], mean A1c 8.9% ± 1.8%, 60% male, 75% non-Hispanic white, 77% private insurance) who utilized telemedicine were included. Technology use among telemedicine patients was not associated with gender, T1D duration, insurance, distance from the main clinic or rural designation but was associated with ethnicity and A1c. Compared to the main clinic cohort (N = 3636), continuous glucose monitor (CGM) use and pump/CGM combination use was lower among patients participating in clinic-to-clinic telemedicine (CGM: 29.7% vs. 56.0%, P < 0.001; CGM/pump combination: 27.3% vs. 40.3%, P = 0.004). Technology use was associated with lower A1c regardless of cohort.
Conclusions: Compared to patients attending in-person clinic, pediatric T1D patients who use clinic-to-clinic telemedicine due to their distance from the main clinic, have lower CGM and combination CGM/pump use. For both telemedicine and main clinic patients, CGM and CGM/pump combination was associated with lower A1c. Additional research is needed to explore reasons for this discrepancy and find methods to improve CGM use in this population.
Keywords: Type 1 diabetes, Pediatric, Telemedicine, Technology, Insulin pump, Continuous glucose monitor
Introduction
Since the Diabetes Control and Complications Trial showed that lower hemoglobin A1c (A1c) levels correlate with reductions in long-term complications related to type 1 diabetes (T1D),1 extensive research has been dedicated to determining the optimal target A1c and the best methods to optimize glycemic outcomes. The American Diabetes Association (ADA) and the International Society for Pediatric and Adolescent Diabetes (ISPAD) have developed clinical guidelines to achieve these long-term goals for diabetes management.2,3 Visits with a pediatric endocrinologist every 3 months3 and a goal A1c of <7%2 (changed recently from <7.5%) are among the recommendations for T1D pediatric patients. Only 19.3% and 7.1% of pediatric patients (younger than 18 years of age) with T1D achieved those targets, respectively, in the 2015–2016 T1D Exchange Clinic Registry cohort, which consists of patients seen at major specialized diabetes clinics and does not reflect the status of all pediatric patients with T1D,4 which is concerning that actual numbers may be lower.
These targets are even more of a challenge for those in rural areas as research has shown that patients who live further from a diabetes clinic attend fewer clinic visits.5 Also, this is further exacerbated for pediatric patients as there are fewer pediatric endocrinologists than adult diabetes care providers for the number of patients in a region, and most are in large academic facilities within cities.6 Thus, the use of telemedicine technologies allows local providers to maintain a role in the ongoing management of their patient's diabetes care, while also increasing the frequency of patient contact with an endocrinologist.5 Increased contact allows for more frequent insulin adjustments, which is especially important in pediatric patients whose insulin needs change frequently,7,8 and may result in overall glycemic improvement, although this may continue to be limited due to a paucity of pediatric endocrinology providers and clinic appointments.
The use of diabetes technologies (insulin pumps, continuous glucose monitors [CGM], and hybrid closed-loop [HCL] systems) has been associated with improvements in A1c, glycemic variability, hypoglycemia, and hyperglycemia in people with T1D.9–13 The improvement in A1c has been particularly apparent in those using CGM.14,15 Glycemic data, trend arrows, and alerts from CGM help pediatric patients and their caregivers make more informed care management decisions.
This is especially relevant for adolescents and young adults who frequently have suboptimal A1c levels and are in need of targeted interventions.16 Advancements in diabetes technology and the development of HCL systems offer additional opportunities to improve glycemia.9,10 A combination approach using diabetes technology and telemedicine-enabled clinical visits to supplement in-person care provides a unique opportunity to improve pediatric diabetes care and outcomes and to reach patients with access barriers, including those who live further from the specialty clinic.
Despite a great deal of research related to the use of telemedicine in increasing the number of clinic visits for patients living a great distance from the main clinic,5,17,18 much is still to be learned about how the use of clinic-to-clinic telemedicine affects uptake and use of diabetes technology. The goal of this analysis was to determine the use of diabetes devices in patients using telemedicine due to living far from the main diabetes specialty clinic to potentially alleviate the disparity in access to care related to living in a rural or distant location and lack of proximity to specialty care.
Materials and Methods
Study design
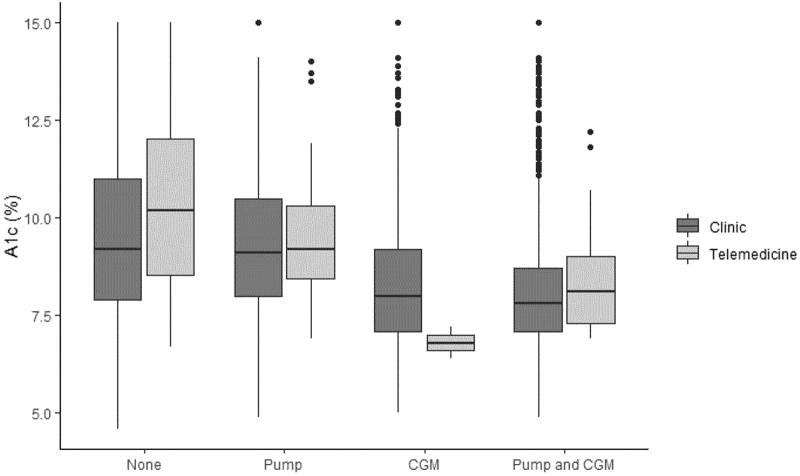
The Barbara Davis Center for Diabetes (BDC) provides services for pediatric T1D patients from all over Colorado, most of Wyoming and parts of Nebraska, and Kansas. Many patients are unable to travel to the main BDC clinic on a regular basis, making it difficult to receive routine diabetes care. In 2012, the BDC initiated a clinic-to-clinic telemedicine program to improve access to subspecialty diabetes care for these patients and their families (Fig. 1). The model involves the patient being seen at a local site, typically a local primary care or hospital-affiliated clinic, where a medical assistant, nurse, or diabetes educator obtains vitals, download devices, and rooms the patient in a telemedicine-enabled room. The diabetes provider who is responsible for both in person and telemedicine care is located at the BDC, conducts a routine clinic visit, including discussion of interval history and review of systems, and reviews recent laboratories, glucose values, and insulin doses to provide recommendations on insulin adjustments, laboratory orders, or other medical needs. The family then receives education and reviews recommendations with the local diabetes educator.
FIG. 1.
Four-point star indicates location of telemedicine site; solid five-point star indicates location of main clinic. BDC, Barbara Davis Center for Diabetes. Color images are available online.
The diabetes educators are employed by the local site and not by the BDC. While dieticians and social workers from the BDC are not available to meet with these families at the time of the visit, they are available by phone to discuss any specific concerns the families may have. In addition, some sites include dieticians as educators and are able to provide this service at the time of the visit.
This model augments the in-person care for these families; but still requires at least one face-to-face visit each year with a BDC provider to assure continuity of care and allows patients to have equal access directly to educators, dieticians, and social workers at the main clinic. The expense to the patient using this model is variable, dependent on a number of factors, including the type of insurance and the individual deductibles, among other factors, and thus was not tracked for this study and the subject of future research.
Patients with T1D and families were eligible to participate in a study (Telemedicine Study) assessing the impact of clinic-to-clinic telemedicine in a pediatric population.5 The study was approved by both the Wyoming and University of Colorado Institutional Review Boards. All patients evaluated in this report had a diagnosis of T1D. Baseline data were collected from the time of enrollment in the Telemedicine Study, which began in 2012. Patients with T1D duration of <6 months were excluded, as these patients are less likely to be using diabetes technology, more likely to have had recent visits at the main clinic, and more likely to have had more recent and more frequent visits to initiate diabetes education. To evaluate glycemic outcomes and demographic characteristics within the Telemedicine Study cohort, the participants were stratified into two groups based on the most recent health care visit: (1) using technology (insulin pump only, CGM only, or both insulin pump, and CGM) and (2) not using technology.
In addition, post hoc analysis was done to compare the participants of the study with the main clinic patients to determine if there are differences in technology use between participants utilizing clinic-to-clinic telemedicine and those who received their diabetes care in person at the main clinic. Comparisons between the Telemedicine Study participants and the main clinic cohort were made using data obtained from the most recent clinic visit as of December 2019. The Telemedicine Study participants were excluded from the main clinic cohort to prevent duplication of data.
Data for this analysis were collected before the onset of the COVID-19 pandemic and therefore only represent the telemedicine services that were provided before the emergent transition to in-home telemedicine. The patients enrolled in this study were using telemedicine because they lived in a rural or distant location from the main clinic (BDC) and could benefit from the use of technology to reduce their need to travel great distances to receive care.
All study data were entered into a secure database, Research Electronic Data Capture (REDCap) system.19
Study measures
Demographics
Descriptive characteristics were obtained at baseline of the Telemedicine Study or at the most recent clinic visit (main clinic cohort) through electronic medical records and survey data. Characteristics included duration of T1D, age, gender, race/ethnicity, insurance status, history of insulin pump or CGM use, and A1c values. Only patients with a clinic visit (either telemedicine or in-person) in the previous 12 months were included in the analysis. Distance from the BDC clinic was also determined using ZIP codes. Rural designation was based on the CMS.gov rural ZIP code list.
Diabetes measures
(1) A1c to assess measure of glycemia, (2) technology use was defined as the use of an insulin pump and/or a CGM at the most recent clinical visit. Combination insulin pump and CGM use indicated that the user wore both a CGM and pump; however, the use of an HCL system was not determined. These data were obtained through surveys for the telemedicine study cohort and electronic medical records for both groups.
Telemedicine survey
Telemedicine Study participants completed a survey following each visit. Among other questions analyzed elsewhere,5 the surveys included history and current use of diabetes technology, current insurance status, and current location (ZIP code).
Statistical analysis
The distributions of all variables were examined before analysis. Descriptive statistics reported include mean ± standard deviation, median (25th, 75th percentile), or frequencies (%). Continuous variables were compared using t-tests or Kruskal–Wallis Rank Sum tests for variables with two levels, and the Wilcoxon test for variables with more than two levels. Chi-squared or Fisher's exact tests were used for categorical variables. All analyses were performed using R (R Core Team, Vienna).
Results
A total of 128 patients with T1D for more than 6 months who enrolled in the Telemedicine Study were included in the analysis (Table 1). At enrollment, mean age was 12.4 ± 4.2 years, 60.2% male, median diabetes duration was 3.3 years [IQR 1.4–7.7], and mean A1c was 8.9% ± 1.8%. A total of 3636 patients were included in the main clinic cohort (demographics in Table 1).
Table 1.
Demographics
| Telemedicine study cohort |
Main clinic cohort |
P | |
|---|---|---|---|
| N = 128 | N = 3636 | ||
| Age at initial telemedicine visit, years | 12.4 (4.2) | N/A | N/A |
| Age at most recent clinic visit, years | 17.4 (4.5) | 14.7 (4.5) | <0.001 |
| Male gender | 77 (60.2) | 1912 (52.6) | 0.111 |
| T1D duration at initial telemedicine visit | 3.3 [1.4–7.7] | N/A | N/A |
| T1D duration, years | 8.9 [6.0–14.0] | 5.6 [2.9–9.3] | <0.001 |
| A1c at initial telemedicine visit, % | 8.9 (1.8) | N/A | N/A |
| A1c at most recent clinic visit | 9.1 (1.8) | 8.8 (2.1) | 0.131 |
| Duration of study participation, years | 2.3 [1.3–4.0] | N/A | N/A |
| No. of telemedicine visits completed | 4 [2–7] (range 1–15) | N/A | N/A |
| Race/ethnicity | |||
| Hispanic | 9 (7.0) | 562 (15.5) | 0.015 |
| Non-Hispanic black | 1 (0.8) | 138 (3.8) | |
| Non-Hispanic white | 96 (75.0) | 2362 (65.0) | |
| Other | 4 (3.1) | 171 (4.7) | |
| Unknown | 18 (14.1) | 402 (11.1) | |
| Insurance type | |||
| Private | 77 (71.3) | 2373 (65.3) | 0.198 |
| Medicaid | 31 (28.7) | 1263 (34.7) | |
| CGM use before telemedicine | 26 (21.5) | N/A | N/A |
| Pump use before telemedicine | 75 (58.6) | N/A | N/A |
| Driving distance to main clinic, km | 386.2 (170.2) | 105.2 (120.5) | <0.001 |
| Rural designation for primary residence | 69 (53.9) | 502 (13.8) | <0.001 |
Bold indicates p < 0.05.
N (%), mean (SD), or median [IQR].
CGM, continuous glucose monitor; T1D, type 1 diabetes.
Telemedicine study cohort
No technology use versus technology use
Telemedicine Study participants were stratified based on technology use at the most recent health care visit (Table 2). Participants in the technology use cohort (n = 86) included those who used an insulin pump and/or a CGM. The participants who used technology had significantly lower A1c levels at the most recent clinic visit compared to those who were not (9.0% ± 1.8% vs. 10.4% ± 2.5%, P = 0.002). Approximately, 80% of pump users in the technology-use group had been on a pump before starting telemedicine, where only 30% had been on CGM before starting telemedicine, likely related to the advancements in CGM technology and the increase in CGM uptake in more recent years. Age at initiation of telemedicine-enabled care, gender, baseline A1c, insurance type, distance to the main clinic, and rural designation were not significantly different between the two groups.
Table 2.
Comparison of Telemedicine Study Participants Not Using Technology Versus Using Technology (Insulin Pump Only, Continuous Glucose Monitor Only, or Combination)
| Not using technology (N = 42) | Using technology (N = 86) | P | |
|---|---|---|---|
| Age at initial telemedicine visit, years | 13.2 (3.9) | 12.1 (4.3) | 0.152 |
| Male gender | 29 (69.0) | 48 (55.8) | 0.214 |
| T1D duration at initial telemedicine visit, years | 3.5 [1.8–8.4] | 3.2 [1.4–7.7] | 0.726 |
| T1D duration, years | 9.7 [6.8–14.5] | 8.8 [6.0–13.9] | 0.443 |
| A1c at initial telemedicine visit, % | 9.2 (2.3) | 8.8 (1.5) | 0.239 |
| A1c at most recent telemedicine visit, % | 10.4 (2.5) | 9.0 (1.8) | 0.002 |
| Insurance type | 0.311 | ||
| Private | 16 (61.5) | 61 (74.4) | |
| Medicaid | 10 (38.5) | 21 (25.6) | |
| Driving distance to main clinic, km | 360.3 (150.1) | 398.9 (178.6) | 0.229 |
| Rural designation of primary residence | 23 (54.8) | 46 (53.5) | 1.000 |
| Race/ethnicity | 0.002 | ||
| Hispanic | 6 (14.3) | 3 (3.5) | |
| Non-Hispanic black | 1 (2.4) | 0 (0.0) | |
| Non-Hispanic white | 25 (59.5) | 71 (82.6) | |
| Other | 4 (9.5) | 0 (0.0) | |
| Unknown | 6 (14.3) | 12 (14.0) | |
| Patients with CGM use before telemedicine | 1 (2.5) | 25 (30.9) | 0.001 |
| Patients with pump use before telemedicine | 6 (14.3) | 69 (80.2) | <0.001 |
Bold indicates p < 0.05.
N (%), mean (SD), or median [IQR].
Technology use by age group
Additional analysis was completed to break down the technology use types and A1c levels by age group (Table 3). Groups included those <6 years old, between 6 and <12 years, between 12 and <18 years, and older than 18 years. There were significant differences between the most recent A1c levels across the groups, with the lowest A1c being in the <6 year olds (A1c 7.4% [7.1–7.8], P = 0.017). In addition, there was a significant difference in the technology distribution between age groups with more CGM or combination technology use in the younger age groups, and more pump only use as the age increases (P < 0.001). There were no significant differences in number of telemedicine visits or gender.
Table 3.
Telemedicine Cohort by Age Group
| <6 years (N = 4) | 6 to <12 years (N = 18) | 12 to <18 years (N = 61) | 18+ (N = 45) | p | |
|---|---|---|---|---|---|
| Age at most recent visit, years | 6.0 (1.6) | 11.1 (1.5) | 16.6 (1.6) | 22.1 (1.7) | <0.001 |
| Male gender | 3 (75.0) | 8 (44.4) | 36 (59.0) | 15 (33.3) | 0.384 |
| A1c at most recent visit, % | 7.4 [7.1–7.8] | 8.25 [7.3–9.4] | 8.4 [7.7–9.8] | 9.3 [8.5–11.2] | 0.017 |
| Technology use | <0.001 | ||||
| Pump only | 0 (0.0) | 4 (22.2) | 23 (37.7) | 21 (46.7) | |
| CGM only | 2 (50.0) | 0 (0.0) | 1 (1.6) | 0 (0.0) | |
| Combination | 1 (25.0) | 11 (61.1) | 19 (31.1) | 4 (8.9) | |
| No. of telemedicine visits | 2.00 [1.50–3.50] | 3.50 [2.00–6.50] | 4.00 [2.00–7.00] | 3.00 [1.50–5.00] | 0.210 |
Bold indicates p < 0.05.
N (%), mean (SD), or median [IQR].
Telemedicine versus general clinic
Data from 128 telemedicine and 3636 main clinic patients were included in this analysis (Table 4). Data were collected from the most recent clinic visit that occurred during the previous 12 months. There was a significantly higher percentage of patients with CGM use and combination pump and CGM use in the main clinic compared to the Telemedicine Study cohort (56.0% vs. 29.7%, P < 0.001, and 40.3% vs. 27.3%, P = 0.004, respectively). There was a higher proportion of patients in the Telemedicine Study cohort than in the main clinic cohort that used an insulin pump (64.8% vs. 56.2%, P = 0.065), however, it did not reach statistical significance. The Telemedicine Study cohort lived significantly further away than the main clinic cohort (386.2 km vs. 105.2 km, P < 0.001) and there was a significantly higher percentage of rural patients in the Telemedicine Study cohort (53.9% vs. 13.8%, P < 0.001) as is expected. Insurance type was not significantly different between the two groups (P = 0.271).
Table 4.
Comparison of Most Recent Clinic Visit for Telemedicine Study Cohort Versus Main Clinic Cohort
| Main clinic (n = 3814) | Telemedicine study (n = 128) | p | |
|---|---|---|---|
| No technology use | 1020 (28.1) | 42 (32.8) | 0.282 |
| Technology users | 2616 (71.9%) | 86 (67.2%) | |
| All pump users | 2044 (56.2) | 83 (64.8) | 0.065 |
| Pump only | 579 (15.9) | 48 (37.5) | <0.001 |
| All CGM users | 2037 (56.0) | 38 (29.7) | <0.001 |
| CGM only | 572 (15.7) | 3 (2.3) | <0.001 |
| Pump and CGM users | 1465 (40.3) | 35 (27.3) | 0.004 |
| Insurance type | 0.954 | ||
| Private | 2373 (65.3) | 77 (71.3) | |
| Medicaid | 1242 (34.2) | 31 (28.7) | |
| Other | 20 (0.5) | 0 (0.0) | |
| Driving distance to main clinic, km | 105.2 (120.5) | 386.2 (170.2) | <0.001 |
| Rural designation of primary residency | 502 (13.8) | 69 (53.9) | <0.001 |
Bold indicates p < 0.05.
N (%), mean (SD), or median [IQR].
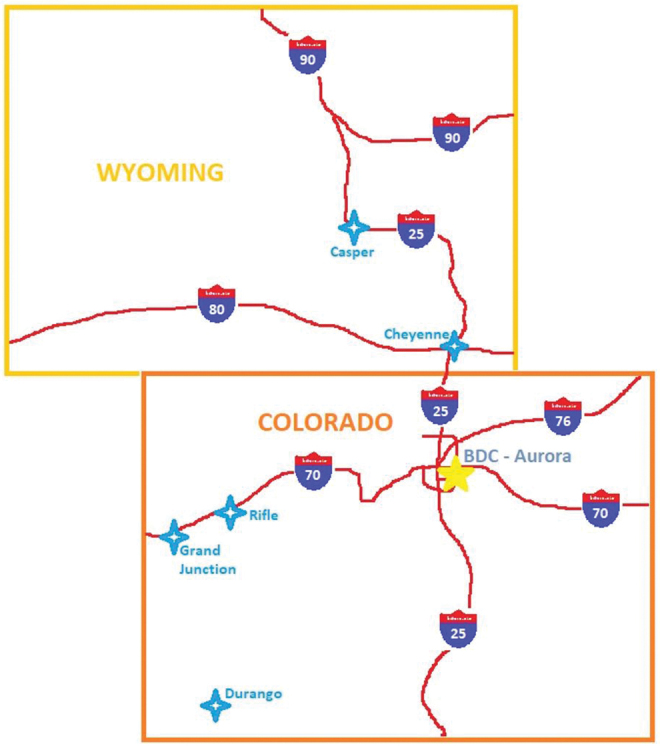
Whether in the Telemedicine Study cohort or the main clinic, A1c was significantly lower with technology use (Fig. 2). In the Telemedicine Study cohort, those without technology use (n = 42) had median [IQR] A1c of 10.2% [8.5–12.0], while pump only (n = 48, 9.2% [8.5–10.3]), CGM alone (n = 3, 6.8% [6.6–7.0]), and pump/CGM combination (n = 35, 8.1% [7.3–9.0]) were significantly different (P = 0.001). In the main clinic cohort, similar A1c differences were found (no technology use: n = 1020, 9.2% [7.9–11.0]; pump alone: n = 579, 9.1% [8.0–10.5], CGM: n = 572, 8.0% [7.1–9.2], and pump/CGM combination: n = 1465, 7.8% [7.1–8.7], P < 0.001).
FIG. 2.
P = 0.001 within telemedicine cohort and P < 0.001 within main clinic cohort across device category.
Conclusions
Pediatric patients who attended diabetes clinic via clinic-to-clinic telemedicine before the COVID-19 pandemic were less likely to use a CGM or combination CGM/insulin pump as part of their diabetes care regimen compared to pediatric patients attending face-to-face clinic visits at the main diabetes center despite receiving clinical care from diabetes providers who care for patients in both settings. For all patients regardless of method of diabetes care visits, any technology use was associated with significantly lower A1c values, further supporting the importance of diabetes technology in the management of T1D.
In fact, CGM use only independently correlated with lower A1c values in both the telemedicine and the main clinic cohort, indicating the significant role CGM can play in diabetes management with or without insulin pump use, although the telemedicine cohort had a small number of participants using CGM alone (Table 4 and Fig. 2). It must be noted that those in the telemedicine cohort who were on CGM alone were aged 3.6, 17.3, and 3.6 years with a duration of T1D of 0.6–0.7 years, indicating a potential influence of the honeymoon period on lowering the A1c and therefore may not be specific to the CGM in this group.
It is likely that pumps alone are more challenging to use than a CGM and therefore are not as successful in reducing HbA1c levels independently and further research is needed to determine the differences in CGM and pump use and the relationship with glycemic outcomes. It will be important to explore reasons for the discrepancy in device use among patients using clinic-to-clinic telemedicine, as well as factors that lead to the higher use of insulin pumps compared to CGM in the telemedicine cohort, to ensure equal access to the best diabetes care and to develop methods to improve the uptake of diabetes technology in these patients.
The use of insulin pumps, CGMs, and HCL systems improves glycemic outcomes.9,10,12,13,20 There are inherent barriers to device uptake and use20–22 regardless of where families live or the method of receiving health care. The improvement in glycemia is most notable in those using CGM, which is consistent with findings from other multicenter studies.14,15 In this study, we found that CGM use was lower in pediatric patients who used telemedicine for routine clinical care due to living a great distance from the main clinic.
There was no difference in technology use for patients who had private or public insurance, and the physical distance of the patients from the diabetes center did not correlate with device use, although there was a significant difference in distance and rural designation between the Telemedicine Study cohort and the main clinic cohort, as would be expected. The lack of an association with physical distance from the main clinic and device use suggests that the commute to the academic medical center may not be a significant barrier for some families or that the perceived benefit of the visit outweighs the burden of the commute. In fact, many of these patients and their families are accustomed to driving long distances for other aspects of their normal lives, such as shopping, work, and recreation. Variables such as family size, income, and access to transportation should be further explored.
Continuity of care improves quality health care and outcomes.23,24 An integrated telemedicine model has the capacity to increase continuity of care and coordination of care between specialty and primary care providers; and potentially better provider-patient/family relationships, and research is needed to determine the most effective way to leverage this opportunity to increase acceptance and use of diabetes technology. Previous data indicate that 15% of patients prescribed an insulin pump did not actually start using it for at least one year.25
Before the COVID-19 pandemic, there was little published experience with remote insulin pump training, although one small study had success with adults who had some baseline knowledge of pumps.26 The pandemic resulted in a rapid and necessary transition to home-based telemedicine for medical care, including insulin pump initiation, and more is being understood about the use of telemedicine for diabetes education and training.27,28
Telemedicine can also allow for convenient follow-up after device initiation to ensure patients' education around these complex devices is complete and thorough and new knowledge or updates can be easily disseminated. As mentioned previously, the current clinic-to-clinic telemedicine model at the BDC involved scheduling patients through a local site where the number of visits may be limited, resulting in wait lists and delays in receiving diabetes care. The adaptation that has occurred during the COVID-19 pandemic may lead to the development of additional telemedicine models that could improve access to care, reduce wait times, and increase acceptance and use of diabetes technology.
This analysis has strengths and limitations. The BDC is a large specialty clinic caring for pediatric and adult patients with T1D; therefore, the sample size for this analysis is large. The center has nearly 10 years of experience with clinic-to-clinic telemedicine, and with the number of sites and patients involved continuing to grow, this indicates the success of this model for pediatric diabetes care. A major limitation to the study is that patients included in the telemedicine cohort were limited to pediatric patients attending telemedicine clinic at the designated centers who signed consent to participate in the research study. Additional patients participated in clinic-to-clinic telemedicine, but were not enrolled in the study due to inability to be reached for consent or declining to participate. This study was not designed as a longitudinal comparison between telemedicine participants and the main clinic, so it is not possible to know which cohort had higher uptake of technology over time.
While attempts are made to ensure equal access to diabetes educators for patients receiving care through telemedicine, the relationship between the patient and the local educator will vary from site to site, potentially effecting the patient's exposure to diabetes technologies and thereby impacting the uptake. It will therefore be important for future telemedicine models to consider the training and knowledge of local educators and to assess patient contact with other staff to identify ways to overcome this potential barrier to technology use. While it is likely that the overall expense to the patient participating in telemedicine was decreased, the individual cost for telemedicine compared to traveling to the main clinic for an in-person visit can vary significantly, and therefore was not evaluated in this study; however, this will be an important component of telemedicine research going forward.
The COVID-19 pandemic occurred after data were collected and analyzed. This study does not reflect the urgent transition to in-home telemedicine that took place when the COVID-19 pandemic forced the temporary discontinuation of in-person clinic visits.
Clinic-to-clinic telemedicine increases the frequency of patient contact with pediatric endocrinologists5; however, these families are less likely than their counterparts who attend routine in-person visit at the main clinic to utilize CGM and CGM/pump combinations. Regardless of the distance to the main clinic, pediatric patients who use technology, whether an insulin pump, a CGM, or both, have lower A1c levels, indicating the importance of device use in this population. Overall, a majority of children with T1D continue to struggle to meet glycemic targets16 and increasing diabetes technology use, especially CGM, may be one method to improve diabetes health. CGM uptake will be increasingly important as HCL systems continue to improve and more systems become commercially available. As we continue to seek opportunities to use telemedicine technology to reduce the barriers to care for those with lower incomes and who reside in rural or distant locations, it is important to continue to study various models of telemedicine in diabetes care with a focus on increasing access to diabetes technologies that may improve glycemic control for these patients.
Authors' Contributions
E.C.C. and R.P.W. developed the concept for the article. L.P. analyzed the data. T.R.L. and G.T.A. collected study data for analysis. E.C.C., R.P.W., R.S., J.F.T., and G.T.A. wrote the article. All authors were responsible for reviewing and revising this article and assume responsibility and accountability for the results.
Author Disclosure Statement
R.P.W. has received research funding from Dexcom, Eli Lilly & Co and Tandem Diabetes Care and received honorarium from Tandem Diabetes Care. The other authors have no conflicts of interest.
Funding Information
National Institutes of Health (NIH) K12DK094712, National Institutes of Health/National Center for Research Resources (NCRR) UL1TR002535.
References
- 1. The Diabetes Control and Complications Trial (DCCT): Design and methodologic considerations for the feasibility phase. The DCCT Research Group. Diabetes 1986;35:530–545. [PubMed] [Google Scholar]
- 2. American Diabetes Association: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43(S1):S1–S212. [DOI] [PubMed] [Google Scholar]
- 3. Pihoker C, Forsander G, Fantahun B, et al. : ISPAD Clinical Practice Consensus Guidelines 2018: the delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes 2018;19(S27):84–104. [DOI] [PubMed] [Google Scholar]
- 4. Hermann JM, Miller KM, Hofer SE, et al. : The Transatlantic HbA1c gap: differences in glycaemic control across the lifespan between people included in the US T1D Exchange Registry and those included in the German/Austrian DPV registry. Diabet Med 2020;37:848–855. [DOI] [PubMed] [Google Scholar]
- 5. Wood CL, Clements SA, McFann K, et al. : Use of telemedicine to improve adherence to American Diabetes Association standards in pediatric type 1 diabetes. Diabetes Technol Ther 2015;18:7–14. [DOI] [PubMed] [Google Scholar]
- 6. Lu H, Holt JB, Cheng YJ, et al. : Population-based geographic access to endocrinologists in the United States, 2012. BMC Health Serv Res 2015;15:541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dovc K, Boughton C, Tauschmann M, et al. : Young children have higher variability of insulin requirements: Observations during hybrid closed-loop insulin delivery. Diabetes Care 2019;42:1344–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Malik FS, Taplin CE: Insulin therapy in children and adolescents with type 1 diabetes. Pediatr Drugs 2014;16:141–150. [DOI] [PubMed] [Google Scholar]
- 9. Garg SK, Weinzimer SA, Tamborlane WV, et al. : Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 Diabetes. Diabetes Technol Ther 2017;19:155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brown SA, Kovatchev BP, Raghinaru D, et al. : Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med 2019;381:1707–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Forlenza GP, Buckingham BA, Christiansen MP, et al. : Performance of omnipod personalized model predictive control algorithm with moderate intensity exercise in adults with type 1 diabetes. Diabetes Technol Ther 2019;21:265–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Klonoff DC, Ahn D, Drincic A: Continuous glucose monitoring: a review of the technology and clinical use. Diabetes Res Clin Pract 2017;133:178–192. [DOI] [PubMed] [Google Scholar]
- 13. Lang EG, King BR, Miller MN, et al. : Initiation of insulin pump therapy in children at diagnosis of type 1 diabetes resulted in improved long-term glycemic control. Pediatr Diabetes 2017;18:26–32. [DOI] [PubMed] [Google Scholar]
- 14. Laffel LM, Kanapka LG, Beck RW, et al. : Effect of continuous glucose monitoring on glycemic control in adolescents and young adults with type 1 diabetes: A randomized clinical trial. JAMA 2020;323:2388–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mulinacci G, Alonso GT, Snell-Bergeon JK, Shah VN: Glycemic outcomes with early initiation of continuous glucose monitoring system in recently diagnosed patients with type 1 diabetes. Diabetes Technol Ther 2019;21:6–10. [DOI] [PubMed] [Google Scholar]
- 16. Foster NC, Beck RW, Miller KM, et al. : State of type 1 diabetes management and outcomes from the t1d exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Reid MW, Krishnan S, Berget C, et al. : CoYoT1 clinic: home telemedicine increases young adult engagement in diabetes care. Diabetes Technol Ther 2018;20:370–379. [DOI] [PubMed] [Google Scholar]
- 18. Thomas JF, Novins DK, Hosokawa PW, et al. : The use of telepsychiatry to provide cost-efficient care during pediatric mental health emergencies. Psychiatr Serv Wash DC 2018;69:161–168. [DOI] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Thielke R, et al. : Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tanenbaum ML, Hanes SJ, Miller KM, et al. : Diabetes device use in adults with type 1 diabetes: barriers to uptake and potential intervention targets. Diabetes Care 2017;40:181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Naranjo D, Tanenbaum ML, Iturralde E, Hood KK: Diabetes technology: uptake, outcomes, barriers, and the intersection with distress. J Diabetes Sci Technol 2016;10:852–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Messer LH, Berget C, Vigers T, et al. : Real world hybrid closed-loop discontinuation: predictors and perceptions of youth discontinuing the 670G system in the first 6 months. Pediatr Diabetes 2020;21:319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shin DW, Cho J, Yang HK, et al. : Impact of continuity of care on mortality and health care costs: A Nationwide Cohort Study in Korea. Ann Fam Med 2014;12:534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cabana MD, Jee SH: Does continuity of care improve patient outcomes? J Fam Pract 2004;53:974–980. [PubMed] [Google Scholar]
- 25. Alonso GT, Hink R, De Georgeo MR, et al. : Improving the insulin pump initiation process for pediatric patients with type 1 diabetes through application of lean quality improvement methods. Perm J 2018;22. [Epub ahead of print]; DOI: 10.7812/TPP/17-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Parks L, Kim TY: Using remote communication technology in insulin pump training. J Diabetes Sci Technol 2015;10:398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vigersky RA, Velado K, Zhong A, et al. : The effectiveness of virtual training on the MiniMed 670G system in people with type 1 diabetes during the COVID-19 pandemic. Diabetes Technol Ther 2020. [Epub ahead of print]; DOI: 10.1089/dia.2020.0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pinsker JE, Singh H, McElwee Malloy M, et al. : A virtual training program for the tandem t:slim X2 insulin pump: Implementation and outcomes. Diabetes Technol Ther 2021. [Epub ahead of print]; DOI: 10.1089/dia.2020.0602. [DOI] [PubMed] [Google Scholar]