Abstract
Background
Preclinical data suggest that concurrent treatment of anti-CD38 and antiprogrammed death 1 (PD-1)/programmed death ligand 1 (PD-L1) antibodies substantially reduce primary tumor growth by reversing T-cell exhaustion and thus enhancing anti-PD-1/PD-L1 efficacy.
Methods
This phase I/II study enrolled patients with metastatic castration-resistant prostate cancer (mCRPC) or advanced non-small cell lung cancer (NSCLC). The primary objectives of phase I were to investigate the safety and tolerability of isatuximab (anti-CD38 monoclonal antibody)+cemiplimab (anti-PD-1 monoclonal antibody, Isa+Cemi) in patients with mCRPC (naïve to anti-PD-1/PD-L1 therapy) or NSCLC (progressed on anti-PD-1/PD-L1-containing therapy). Phase II used Simon’s two-stage design with response rate as the primary endpoint. An interim analysis was planned after the first 24 (mCRPC) and 20 (NSCLC) patients receiving Isa+Cemi were enrolled in phase II. Safety, immunogenicity, pharmacokinetics, pharmacodynamics, and antitumor activity were assessed, including CD38, PD-L1, and tumor-infiltrating lymphocytes in the tumor microenvironment (TME), and peripheral immune cell phenotyping.
Results
Isa+Cemi demonstrated a manageable safety profile with no new safety signals. All patients experienced ≥1 treatment-emergent adverse event. Grade≥3 events occurred in 13 (54.2%) patients with mCRPC and 12 (60.0%) patients with NSCLC. Based on PCWG3 criteria, assessment of best overall response with Isa+Cemi in mCRPC revealed no complete responses (CRs), one (4.2%) unconfirmed partial response (PR), and five (20.8%) patients with stable disease (SD). Per RECIST V.1.1, patients with NSCLC receiving Isa+Cemi achieved no CR or PR, and 13 (65%) achieved SD. In post-therapy biopsies obtained from patients with mCRPC or NSCLC, Isa+Cemi treatment resulted in a reduction in median CD38+ tumor-infiltrating immune cells from 40% to 3%, with no consistent modulation of PD-L1 on tumor cells or T regulatory cells in the TME. The combination triggered a significant increase in peripheral activated and cytolytic T cells but, interestingly, decreased natural killer cells.
Conclusions
The present study suggests that CD38 and PD-1 modulation by Isa+Cemi has a manageable safety profile, reduces CD38+ immune cells in the TME, and activates peripheral T cells; however, such CD38 inhibition was not associated with significant antitumor activity. A lack of efficacy was observed in these small cohorts of patients with mCRPC or NSCLC.
Trial registration numbers
Keywords: programmed cell death 1 receptor, clinical trials as topic, drug therapy, combination, prostatic neoplasms, lung neoplasms
Background
CD38 belongs to the ADP-ribosyl cyclase family and is widely expressed on the surfaces of immune cells and non-hematopoietic cells.1 The receptor/ligand activity of CD38 has been demonstrated in several types of immune cells, with function varying during development, activation, and differentiation of lymphocytes.1 CD38 is implicated in non-canonical adenosine synthesis, and its overexpression on tumor cells has been implicated in T-cell exhaustion and resistance to immune checkpoint blockade.2 CD38+ tumor-infiltrating immune cell density has been shown to increase following progression to castration-resistant prostate cancer, with an association observed with worse overall survival.3 Preclinical data in lung cancer suggest that concurrent treatment with anti-CD38 and antiprogrammed death 1 (PD-1)/programmed death ligand 1 (PD-L1) antibodies substantially reduces primary tumor growth by suppressing acquired resistance to immune checkpoint blockade, thus enhancing and prolonging anti-PD-1/PD-L1 efficacy.2
Based on the phase III ICARIA-MM study, isatuximab (Sarclisa) is approved in a number of countries in combination with pomalidomide and dexamethasone for the treatment of adult patients with relapsed/refractory multiple myeloma who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor. Based on the phase III IKEMA study, isatuximab in combination with carfilzomib and dexamethasone is approved in the USA for the treatment of adult patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy, and in the European Union for the treatment of adult patients with multiple myeloma who have received at least one prior therapy.4 5
Cemiplimab (Libtayo) is an anti-PD-1 antibody approved for the treatment of the following: (1) patients with metastatic cutaneous squamous cell carcinoma or locally advanced cutaneous squamous cell carcinoma who are not candidates for curative surgery or curative radiation; (2) patients with locally advanced or metastatic basal cell carcinoma previously treated with a hedgehog pathway inhibitor or for whom a hedgehog pathway inhibitor is not appropriate; and (3) patients with non-small cell lung cancer (NSCLC) and high tumor PD-L1 expression as determined by a Food and Drug Administration-approved test, with no EGFR, ALK, or ROS1 aberrations, and is locally advanced, where patients are not candidates for surgical resection or definitive chemoradiation, or metastatic.6
This study was designed to evaluate the combination of isatuximab plus cemiplimab (Isa+Cemi) in patients with metastatic castration-resistant prostate cancer (mCRPC) or advanced NSCLC.
Methods
Study design and objectives
This was an open-label, multicenter, phase I/II study designed to evaluate the safety, preliminary efficacy, and pharmacokinetics (PK) of Isa+Cemi in patients with mCRPC or NSCLC. The primary objectives of phase I, the safety run-in, were to characterize the safety and tolerability of Isa+Cemi in patients with mCRPC (naïve to anti-PD-1/PD-L1 therapy) or NSCLC (progressed on anti-PD-1/PD-L1-containing therapy) and to confirm the recommended phase II dose (RP2D). The primary objective of phase II, using Simon’s two-stage design, was to assess the response rate of Isa+Cemi in patients with mCRPC or NSCLC.
Treatment
Patients received isatuximab 10 mg/kg intravenously every week for 3 weeks (one cycle, 21 days) followed by once every 3 weeks+cemiplimab 350 mg intravenously every 3 weeks. The end of treatment occurred 30 (±7) days following final administration or on receipt of another anticancer therapy, whichever occurred first.
CT/MRI and bone scans were completed every 9 weeks starting at the end of cycle 3. When treating beyond RECIST V.1.1-defined tumor progression, subsequent assessments were based on iRECIST criteria.
Immunohistochemistry (IHC) and multiplex immunofluorescence assays
Single-plex IHC assays used PD-L1 (Ventana, SPC263, ready-to-use) or CD38 (Leica, SPC32, working concentration 1:400) optimized for detection with the OptiView DAB IHC Detection kit on the Ventana Benchmark Ultra platform.
Patients with paired screening and on-treatment biopsies were selected for the multiplexed immunofluorescent platform (MultiOmyx) analysis, using a pair of Cy3-labeled or Cy5-labeled antibodies per round of staining. Formalin-fixed paraffin-embedded tissues were stained with a customized panel to quantify infiltrating immune cells in the tumor microenvironment (TME) according to the vendor-recommended protocol (Neogenomics).
Flow cytometry immunophenotyping
Lymphocyte phenotyping panels capable of detecting CD45 (clone 2D1), CD3 (clone SK7), CD4 (clone SK3), CD8 (clone SK1), CD16 (clone B73.1), CD56 (clone NCAM16.2), CD19 (clone SJ25C1), NKp46 (clone 9e2), HLA-DR (clone L243), granzyme B (clone GB11), and Ki67 (clone Ki67) were used to characterize key functional immune cells.
Blood samples were collected in Cyto-Chex BCT tubes. Whole blood samples were incubated with fluorescently labeled antibodies specific to the surface markers listed previously followed by red blood cell lysis. Samples were subsequently fixed, permeabilized, and stained with anti-Ki67 and antigranzyme B fluorochrome-conjugated antibodies. Specimens were acquired on the FACSCanto II flow cytometer and results were analyzed using FlowJo V.7 software (FlowJo LLC).
Pharmacokinetic analysis
Blood samples were taken at selected time points for PK evaluation of isatuximab and cemiplimab (days 1, 4, 8, and 15) over the first cycle and then mainly at predose. Isatuximab (plasma) and cemiplimab (serum) concentrations were determined using validated immunoassays with lower limits of quantification of 5 µg/mL (isatuximab) and 0.078 mg/L (cemiplimab). Non-compartmental analyses were conducted for both compounds with Phoenix WinNonlin V.8.1 (Pharsight).
Statistical analysis
The efficacy and safety analyses were conducted using the all-treated population. Data from mCRPC and NSCLC cohorts in phase II were analyzed and reported separately using descriptive statistics. Continuous data were summarized using mean, standard deviation, median, minimum, and maximum. Categorical and ordinal data were summarized using number and percentage. A 90% two-sided CI was computed using the Clopper-Pearson method for overall response rate (see online supplemental information for further details).
jitc-2021-003697supp001.pdf (1.2MB, pdf)
Results
Patients
Patients with mCRPC had a median age of 69.5 years, and 15 (62.5%) had an Eastern Cooperative Oncology Group (ECOG) performance score of 1. Patients with NSCLC had a median age of 65.5 years, 14 (70.0%) were men, and 11 (55.0%) had an ECOG performance score of 1 (table 1). At diagnosis, 54.2% of patients with mCRPC had stage IV disease; all patients had metastatic adenocarcinoma with documented disease progression at study entry. Among patients with NSCLC, 12 (60.0%) had adenocarcinoma, 4 (20.0%) had squamous cell carcinoma and 3 (15.0%) had unspecified NSCLC. At study entry, 15 (75.0%) patients had metastatic disease; 3 (15.0%) had locally advanced disease; and 2 (10.0%) had primary disease. Patients with NSCLC were excluded if they had known EGFR sensitizing mutations, ALK rearrangement, ROS1 rearrangement, or BRAF mutation. Patients had to receive one previous anti-PD-1/PD-L1 (nivolumab, pembrolizumab, atezolizumab, durvalumab, avelumab, or cemiplimab)-containing regimen (defined as monotherapy or an anti-PD-1/PD-L1 agent administered in the same cycle as another systemic therapy) as the most recent prior therapy to treat stage IIIB/IV or inoperable recurrent NSCLC. Patients were enrolled who had documented benefit (defined as CR, PR, or stable disease (SD) at ≥1 radiographic imaging scan) but subsequent progression per RECIST V.1.1 during the PD-1/PD-L1-containing regimen within 4 months prior to initiation of study treatment.
Table 1.
Summary of demographics and other baseline characteristics—all-treated population
| mCRPC (n=24) |
NSCLC (n=20) |
|
| Age (years) | ||
| Median (range) | 69.5 (61–88) | 65.5 (53–77) |
| Gender, n (%) | ||
| Male | 24 (100) | 14 (70.0) |
| Female | 0 | 6 (30.0) |
| Race, n (%) | ||
| White | 18 (75.0) | 10 (50.0) |
| Black or African–American | 0 | 1 (5.0) |
| Asian | 6 (25.0) | 5 (25.0) |
| Not reported or unknown | 0 | 4 (20.0) |
| ECOG performance status, n (%) | ||
| 0 | 9 (37.5) | 9 (45.0) |
| 1 | 15 (62.5) | 11 (55.0) |
ECOG, Eastern Cooperative Oncology Group; mCRPC, metastatic castration-resistant prostate cancer; NSCLC, non-small cell lung cancer.
All patients with mCRPC had received ≥1 prior androgen receptor-targeted agent. Most patients (n=17) had received ≤2 previous taxane-based chemotherapy regimens; 16 received curative or palliative radiation therapy; and 18 underwent prior surgery. All patients with NSCLC had received one previous anti-PD-1/PD-L1-containing regimen as the most recent therapy; 14 had received prior chemotherapy; 12 had received one regimen and two received ≥2 regimens; 10 patients had received prior radiation therapy; and 8 underwent prior surgery.
Safety
For patients with mCRPC, the median number of cycles started was 4.5 (range 1–13) and the median duration of exposure to study treatment was 13.5 (range 3–39) weeks. Overall, 21/24 (87.5%) treated patients started ≥2 treatment cycles; 6 patients (25.0%) had ≥1 cycle delayed. The average median cumulative dose of isatuximab was 72.32 mg/kg and the median duration of exposure was 13.5 (range 1–39) weeks.
For patients with NSCLC, the median number of cycles started was 5.0 (range 1–19), and the median duration of exposure to study treatment was 17.0 (range 3–58) weeks. Overall, 17/20 (85.0%) treated patients started ≥2 treatment cycles; 8 patients (40.0%) had ≥1 cycle delayed. The average median cumulative dose of isatuximab was 70.03 mg/kg, and the median duration of exposure was 17.0 (range 1–58) weeks.
Isa+Cemi demonstrated a manageable safety profile with no new safety signals. No dose-limiting toxicities were observed, and the RP2D was the standard regimen for each drug. All patients experienced ≥1 treatment-emergent adverse event (TEAE). Grade≥3 TEAEs occurred in 13 (54.2%) patients with mCRPC and 12 (60.0%) patients with NSCLC (table 2). No grade 5 TEAEs were related to study treatment. The most frequently reported TEAEs of any grade for both cohorts were infusion-related reactions (mCRPC, 50.0%; NSCLC, 45.0%) (online supplemental table 1). Grade≥3 TEAEs reported in >1 patient included infusion-related reactions (mCRPC, 8.3%; NSCLC, 10.0%) and pneumonia (NSCLC, 10.0%; not immune-related). All 24 patients with mCRPC discontinued treatment (progressive disease (PD), n=15; adverse events (AEs), n=4; other, n=4; withdrawal by subject due to AE, n=1). Among patients with NSCLC, 18 (90%) discontinued treatment (PD, n=13; AEs, n=3; other, n=2).
Table 2.
Overview of TEAEs—all-treated population
| n (%) | mCRPC (n=24) |
NSCLC (n=20) |
| Patients with any TEAE (any grade) | 24 (100) | 20 (100) |
| Patients with any TEAE of grade ≥3 | 13 (54.2) | 12 (60.0) |
| Patients with any TEAE of grade 5 | 2 (8.3) | 2 (10.0) |
| Patients with any serious TEAE | 11 (45.8) | 13 (65.0) |
| Patients with any treatment-related TEAE* (any grade) | 19 (79.2) | 14 (70.0) |
| Patients with any treatment-related TEAE of grade ≥3 | 4 (16.7) | 4 (20.0) |
| Patients with any serious treatment-related TEAE | 3 (12.5) | 3 (15.0) |
| Patients with any TEAE leading to definitive study drug discontinuation | 4 (16.7) | 3 (15.0) |
| Patients with any TEAE leading to premature discontinuation of isatuximab | 0 | 0 |
| Patients with any TEAE leading to premature discontinuation of cemiplimab | 0 | 0 |
| Patients with any AESI† | 10 (41.7) | 10 (50.0) |
| Patients with any AESI of grade ≥3 | 3 (12.5) | 3 (15.0) |
*Treatment-related TEAEs are TEAEs related to at least one drug of the combination.
†AESIs include grade ≥2 IARs, grade ≥3 immune-related TEAEs, immune-related AEs of any grade in a patient previously treated with a PI3K inhibitor (only applicable for patients who receive cemiplimab), pregnancy, symptomatic overdose with IMP/NIMP.
AE, adverse event; AESI, adverse event of special interest; IAR, infusion-associated reaction; IMP, investigational medicinal product; mCRPC, metastatic castration-resistant prostate cancer; NIMP, non-investigational medicinal product; NSCLC, non-small cell lung cancer; TEAE, treatment-emergent adverse event.
Immunogenicity was assessed in 39 patients; 1 patient exhibited a cemiplimab-induced antidrug antibody, resulting in an incidence and prevalence of 2.6%. There was no isatuximab-induced antidrug antibody response.
Efficacy
Based on PCWG3 criteria,7 assessment of best overall response with Isa+Cemi in patients with mCRPC revealed no complete responses (CRs), 1 (4.2%) unconfirmed partial response (PR), and 5 (20.8%) patients with SD (table 3). Per RECIST V.1.1,8 patients with NSCLC receiving Isa+Cemi achieved no CR or PR, and 13 (65.0%) achieved SD (table 3). Median progression-free survival was 2.30 months (95% CI 1.91 to 4.27) and 4.01 months (95% CI 1.94 to 4.07) for patients with mCRPC and NSCLC, respectively (online supplemental figure 1).
Table 3.
Summary of response rates—all-treated population
| mCRPC (n=24) |
NSCLC (n=20) |
|
| Best overall response, n (%) | ||
| CR* | 0 | 0 |
| PR* | 1 (4.2) | 0 |
| Stable disease | 5 (20.8) | 13 (65.0) |
| Non-CR/non-PD† | 9 (37.5) | 0 |
| PD | 5 (20.8) | 5 (25.0) |
| Not evaluable‡ | 4 (16.7) | 2 (10.0) |
| Unconfirmed CR | 0 | 0 |
| Unconfirmed PR | 1 (4.2) | 0 |
| PSA response, n (%) | ||
| Responders* | 1 (4.2) | – |
| Unconfirmed response | 1 (4.2) | – |
| Overall response, n (%) | ||
| Responders (CR, PR, or PSA responders)* | 1 (4.2) | 0 |
| 90% CI§ | 0.2 to 18.3 | 0.0 to 13.9 |
*Confirmation of response is required.
†Including patients with no target and non-target lesions identified at baseline and no new lesions reported in postbaseline tumor assessments, or patients with only non-target lesions identified at baseline with non-CR/non-PD reported for non-target lesion and no new lesions reported in postbaseline tumor assessments.
‡Including patients with no postbaseline evaluation prior to the initiation of a new anticancer therapy or the data cut-off date.
§Estimated using Clopper-Pearson method.
CR, complete response; mCRPC, metastatic castration-resistant prostate cancer; NSCLC, non-small cell lung cancer; PD, progressive disease; PR, partial response; PSA, prostate-specific antigen.;
Biomarkers
Baseline levels of CD38+ immune cells, CD38+ tumor cells, PD-L1 tumor-positive score, and tumor-infiltrating immune cells are shown in online supplemental figure 2. Isa+Cemi resulted in ~40% median reduction in the proportion of CD38+ tumor-infiltrating immune cells in the TME in post-therapy biopsies from patients with NSCLC or mCRPC (figure 1A; median 40% (range 0.5%–70%) and 3% (range 0%–50%) at baseline and cycle 2 day 1, respectively; n=13). No consistent modulation of PD-L1 expression on tumor cells (figure 1B) or Tregs in the TME (figure 1C) was observed in post-therapy biopsies. The combination triggered a significant increase in peripheral activated and cytolytic T cells, as well as a robust reduction of natural killer (NK) cells (online supplemental figure 3).
Figure 1.
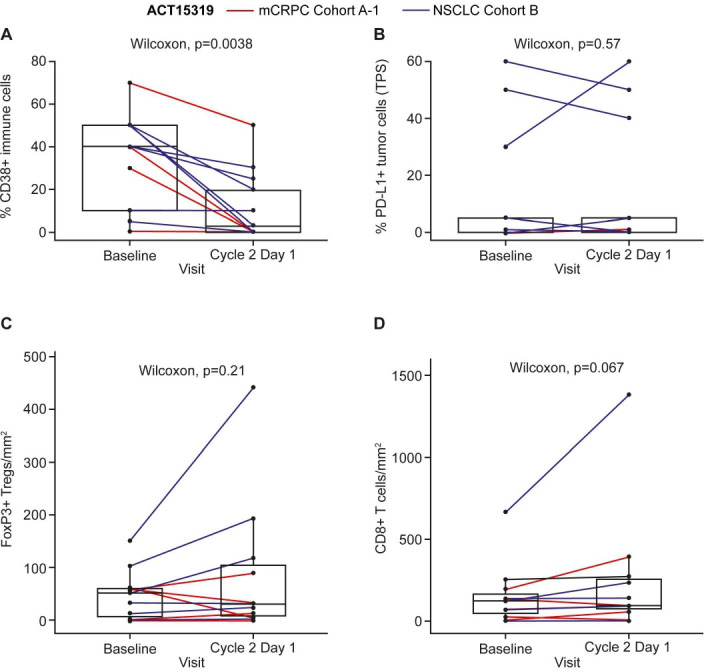
mCRPC, metastatic castration-resistant prostate cancer; NSCLC, non-small cell lung cancer; PD-L1, programmed death ligand 1; TPS, tumor-positive score.
Pharmacokinetic analysis
Results from 33 patients (n=17, NSCLC; n=16, mCRPC) showed consistent isatuximab PK parameters after the first administration across tumor types (online supplemental table 2). The mean isatuximab maximum observed concentration (Cmax) and area under the concentration versus time curve over the first 1 week dosing interval (AUC0–1 week) was 285 µg/mL and 26 600 µg·h/mL, respectively, with low variability (coefficient of variance (CV) for Cmax and AUC0–1 week: 21% and 24%, respectively). At the end of the weekly repeated isatuximab administration, the concentration observed just before the next treatment administration (Ctrough) of cycle 2 showed a twofold higher exposure compared with the first administration and remained within the same magnitude during administration every 3 weeks (Q3W).
Similar findings were observed for cemiplimab (online supplemental table 3), with comparable PK parameters in patients with NSCLC or mCRPC. The mean cemiplimab Cmax and AUC0–3 weeks was 106 mg/L and 934 mg·day/L with low variability (CV for Cmax and AUC0–3 weeks: 24% and 27%, respectively). After Q3W repeated cemiplimab administration, Ctrough of cycle 5 showed a threefold higher exposure compared with the first administration.
Discussion
Despite advances in treatment, mCRPC remains incurable. Studies have demonstrated promising results in select small subgroups of this patient population with immune checkpoint inhibitors, including anti-PD-1 therapy, contributing to responses with a median duration of greater than 15 months, suggesting benefit for some patients.9–11 PD-1 inhibitors have also demonstrated encouraging results for patients with NSCLC and are licensed for use both alone and in combination with chemotherapy.12 An approach for increasing response to treatment is to identify combinations that synergize with immune checkpoint inhibitor therapy, potentially leading to enhanced therapeutic effects and durability.13
The rationale for combining anti-CD38 and anti-PD-1 therapies is supported by studies in multiple myeloma, where data have shown that multiple myeloma cells increase expression of PD-1 by NK cells.14 As a result, the PD-1/PD-L1 axis leads to suppressed antibody-dependent cellular toxicity mediated by isatuximab. Moreover, isatuximab reduces the frequency and function of immune-suppressive Tregs.15 Thus, combining anti-PD-1/PD-L1 antibodies with CD38 blockade might lead to a favorable anti-TME and improved therapeutic benefit.16 Additionally, a recent report demonstrates a mechanism of immune resistance to anti-PD-1/PD-L1 therapy caused by tumor CD38 expression in solid tumor animal models, providing a rationale for the combination of isatuximab and cemiplimab in the clinical setting for the prevention of immune checkpoint blockade resistance and the potential positive impact on antitumor activity.2
This phase I/II study was designed to evaluate the safety, preliminary efficacy, and PK of the combination of isatuximab and cemiplimab in patients with advanced mCRPC or NSCLC. No new safety signals were observed following treatment with Isa+Cemi than what has been published for each drug alone, with both drugs tolerated in combination and no dose-limiting toxicities at the recommended schedules. In the current study, tolerability of Isa+Cemi was similar to that of daratumumab plus atezolizumab based on safety results from a recent study.17 Notably, immune-related TEAEs were reported in one patient each with mCRPC and NSCLC, which is in keeping with previous reports of immune-related TEAEs with similar treatment combinations.18
Interestingly, in the current study, combination therapy with Isa+Cemi led to a near-40% reduction of CD38+ tumor-infiltrating immune cells in the TME, indicating on-target effects of isatuximab. In addition, following treatment with Isa+Cemi, no consistent modulation of PD-L1 on tumor cells or Tregs in the TME was observed in patient biopsies. However, the low levels of CD38-positive cells and PD-L1-positive cells at baseline may have contributed to difficulties analyzing modulatory responses following treatment. Notably, the combination significantly increased peripheral activated and cytolytic T cells, suggesting that peripheral immune activation was induced by this combination therapy. We also observed peripheral NK cell reduction, which is consistent with previous findings suggesting that isatuximab-mediated NK-cell depletion occurs via exhaustion and CD38/SLAMF7-mediated phagocytosis.19
Preclinical data demonstrate the synergistic activity of combined anti-CD38 and anti-PD-1 antibodies in murine multiple myeloma cells,20 supporting the investigation of this combination in clinical trials. However, in these small cohorts of patients with mCRPC and NSCLC in the current study, no significant antitumor activity was observed.
Wu et al recently reported results from TCGA database analysis suggesting CD38 expression is positively correlated with survival and infiltrating T cells in patients with NSCLC.21 In addition, using tumor tissue from 45 patients after surgical resection without any prior radiotherapy or chemotherapy, they further confirmed an increased level of CD38+ CD8 T cells in tumor compared with normal tissue, suggesting its potential involvement in the antitumor immune response.
However, in the present study, we did not observe a significant association of CD38 expression with clinical response. The correlation analysis between CD38 and infiltrated lymphocytes is also not significant. This could be due to (1) difference in prior treatment history: the patients with NSCLC enrolled in present study have progressed from previous anti-PD-1/PD-L1-containing therapy, which could change the baseline CD38 or CD8 expression profile; or (2) limited available biopsies obtained (n=15).
Isatuximab PK parameters in the current study were comparable with those observed in an ongoing study of isatuximab given alone or in combination with cemiplimab in relapsed/refractory multiple myeloma where the same assay method is used (data on file), suggesting no effect of cemiplimab on isatuximab PK. In addition, PK analyses suggest no effect of isatuximab on cemiplimab PK.22
The limitation of the current study was the small number of patients enrolled with each tumor type. The strengths of the current study include the demonstration of a manageable safety profile with Isa+Cemi treatment and the biomarker analyses conducted. Additional studies are warranted to further investigate underlying biomarkers that may inform treatment selection and predict benefit from combination therapy with anti-CD38 and anti-PD-1/PD-L1 agents.
Overall, these results suggest that CD38 and PD-1 modulation by Isa+Cemi has a manageable safety profile, reduces CD38+ immune cells in the TME, and activates peripheral T cells; however, such CD38 inhibition was not associated with significant antitumor activity. A lack of efficacy was observed in these small cohorts of patients with mCRPC and NSCLC.
Acknowledgments
The authors thank the participating patients and their families, and the study centers and investigators for their contributions to the study. Medical writing support was provided by Erin Burns-Tidmore, PhD, of Elevate Medical Affairs, contracted by Sanofi Genzyme for publication support services.
Footnotes
Twitter: @DrIacovelli
PAZ and C-CL contributed equally.
Contributors: PAZ, C-CL, BCC, TMB, MT, AI, RI, W-CS, CM, MS, GD, AG, MG, SP, Y-CS, MP, and JdB were investigators of the study and contributed to data acquisition. GA, RM, RW, HL, YD, MC, LLo, and LLe designed the study and contributed to data analysis and interpretation. All authors revised this work for important intellectual content and assume responsibility for the integrity of the data and the decision to submit for publication; had full access to the study data; and edited and reviewed manuscript drafts and approved the final draft for submission.
Funding: This study was sponsored by Sanofi.
Competing interests: PAZ: Pfizer, Novartis, Sanofi, BMS, MSD, Roche, Amgen, AstraZeneca, Astellas, Janssen, Ipsen, and Bayer. C-CL: Abbvie, BeiGene, Blueprint Medicines, Boehringer Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Eli Lilly, Novartis, PharmaEngine, and Roche. BCC, MT, W-CS, GD, MS, AG, SP, Y-CS, MP: nothing to disclose. TMB: AstraZeneca, Lilly, Bristol Myers Squibb, Foundation Medicine, Pfizer, Loxo, Bayer, Guardant Health, Exelixis, Blueprint Medicines, and Sanofi. AI: Epizyme, Lilly, Merck Sharp & Dohme, Novartis, Pharmamar, Roche, AstraZeneca, Bayer, Bristol Myers Squibb, Chugai, Pfizer. RI: Ipsen, Pfizer, Janssen, Sanofi, Merck, Astellas, and MSD. CM: Amgen, Astellas, AstraZeneca, Bayer, BeiGene, BMS, Celgene, Debiopharm, Genentech, Ipsen, Janssen, Lilly, MedImmune, MSD, Novartis, Pfizer, Roche, Sanofi, and Orion. MG: Bristol Myers Squibb, Merck, Eli Lilly, Esanex, Foundation Medicine, AstraZeneca, and Guardant 360. RM, GA, HL, YD, MC, RW, and LLo are employed by Sanofi and may hold stock and/or stock options in the company. LLe is employed by Excelya on behalf of Sanofi and may hold stock and/or stock options in the company. JdB: AstraZeneca, GlaxoSmithKline, Pfizer, Taiho, Daiichi Sankyo, Bayer, Orion Pharma, Roche/Genentech, Merck Serono, Sierra Oncology, MSD, Terumo, Menarini/Silicon Biosystems, Astellas, BioexcelTherapeutics, Cellcentric, Merck Sharp & Dohme, Qiagen, Sanofi Aventis, and Vertex Pharmaceuticals.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Qualified researchers can request access to patient-level data and related study documents including the clinical study report, study protocol with any amendments, blank case report forms, statistical analysis plan, and dataset specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial subjectss. Further details on Sanofi’s data-sharing criteria, eligible studies, and process for requesting access are at https://www.clinicalstudydatarequest.com.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by EC (reference: 18/LO/0229IRAS project ID: 239401). The subjects gave informed consent to participate in the study before taking part. The study was conducted in accordance with consensus ethics principles derived from international ethics guidelines, including the Declaration of Helsinki and the ICH guidelines for Good Clinical Practice, and all applicable laws, rules, and regulations. Informed consent was obtained prior to conducting any study-related procedures.
References
- 1.Quarona V, Zaccarello G, Chillemi A, et al. CD38 and CD157: a long journey from activation markers to multifunctional molecules. Cytometry B Clin Cytom 2013;84:207–17. 10.1002/cyto.b.21092 [DOI] [PubMed] [Google Scholar]
- 2.Chen L, Diao L, Yang Y, et al. Cd38-Mediated immunosuppression as a mechanism of tumor cell escape from PD-1/PD-L1 blockade. Cancer Discov 2018;8:1156–75. 10.1158/2159-8290.CD-17-1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo C, Crespo M, Gurel B, et al. Cd38 in advanced prostate cancers. Eur Urol 2021;79:736–46. 10.1016/j.eururo.2021.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aventis S. Sarclisa (isatuximab-irfc). prescribing information. Bridgewater, NJ: sanofi-aventis U.S LLC, 2021. [Google Scholar]
- 5.European Medicines Agency . European public assessment report: Sarclisa (isatuximab), 2021. Available: https://www.ema.europa.eu/en/medicines/human/summaries-opinion/sarclisa-0 [Accessed 21 Jun 2021].
- 6.Regeneron . Libtayo (cemiplimab). [Prescribing information], 2020. Available: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761097s005lbl.pdf [Accessed 5 Apr 2020].
- 7.Scher HI, Morris MJ, Stadler WM, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials Working group 3. J Clin Oncol 2016;34:1402–18. 10.1200/JCO.2015.64.2702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 9.Graff JN, Alumkal JJ, Drake CG, et al. Early evidence of anti-PD-1 activity in enzalutamide-resistant prostate cancer. Oncotarget 2016;7:52810–7. 10.18632/oncotarget.10547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tucker MD, Zhu J, Marin D, et al. Pembrolizumab in men with heavily treated metastatic castrate-resistant prostate cancer. Cancer Med 2019;8:4644–55. 10.1002/cam4.2375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antonarakis ES, Piulats JM, Gross-Goupil M, et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: Multicohort, open-label phase II KEYNOTE-199 study. J Clin Oncol 2020;38:395–405. 10.1200/JCO.19.01638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qu J, Mei Q, Liu L, et al. The progress and challenge of anti-PD-1/PD-L1 immunotherapy in treating non-small cell lung cancer. Ther Adv Med Oncol 2021;13:1758835921992968. 10.1177/1758835921992968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han HJ, Li YR, Roach M, et al. Dramatic response to combination pembrolizumab and radiation in metastatic castration resistant prostate cancer. Ther Adv Med Oncol 2020;12:1758835920936084. 10.1177/1758835920936084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu C, Song Z, Wang A, et al. Isatuximab acts through Fc-dependent, independent, and direct pathways to kill multiple myeloma cells. Front Immunol 2020;11:11. 10.3389/fimmu.2020.01771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feng X, Zhang L, Acharya C, et al. Targeting CD38 suppresses induction and function of T regulatory cells to mitigate immunosuppression in multiple myeloma. Clin Cancer Res 2017;23:4290–300. 10.1158/1078-0432.CCR-16-3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Yang R, Chen L, et al. Cd38 as an immunomodulator in cancer. Future Oncol 2020;16:2853–61. 10.2217/fon-2020-0401 [DOI] [PubMed] [Google Scholar]
- 17.ClinicalTrials.gov . A study of daratumumab in combination with atezolizumab compared with atezolizumab alone in participants with previously treated advanced or metastatic non-small cell lung cancer (DARZALEX), 2019. Available: https://clinicaltrials.gov/ct2/show/NCT03023423 [Accessed 19 May 2021].
- 18.Cohen YC, Oriol A, Wu KL, et al. Daratumumab with Cetrelimab, an anti-PD-1 monoclonal antibody, in relapsed/refractory multiple myeloma. Clin Lymphoma Myeloma Leuk 2021;21:46–54. 10.1016/j.clml.2020.08.008 [DOI] [PubMed] [Google Scholar]
- 19.Moreno L, Perez C, Zabaleta A, et al. The mechanism of action of the Anti-CD38 monoclonal antibody Isatuximab in multiple myeloma. Clin Cancer Res 2019;25:3176–87. 10.1158/1078-0432.CCR-18-1597 [DOI] [PubMed] [Google Scholar]
- 20.Verkleij CPM, Jhatakia A, Broekmans MEC, et al. Preclinical rationale for targeting the PD-1/PD-L1 axis in combination with a CD38 antibody in multiple myeloma and other CD38-Positive malignancies. Cancers 2020;12. 10.3390/cancers12123713. [Epub ahead of print: 10 Dec 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu P, Zhao L, Chen Y, et al. CD38 identifies pre-activated CD8+ T cells which can be reinvigorated by anti-PD-1 blockade in human lung cancer. Cancer Immunol Immunother 2021;70:3603–16. 10.1007/s00262-021-02949-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paccaly AJ, Migden MR, Papadopoulos KP, et al. Fixed dose of Cemiplimab in patients with advanced malignancies based on population pharmacokinetic analysis. Adv Ther 2021;38:2365–78. 10.1007/s12325-021-01638-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2021-003697supp001.pdf (1.2MB, pdf)
Data Availability Statement
Data are available upon reasonable request. Qualified researchers can request access to patient-level data and related study documents including the clinical study report, study protocol with any amendments, blank case report forms, statistical analysis plan, and dataset specifications. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial subjectss. Further details on Sanofi’s data-sharing criteria, eligible studies, and process for requesting access are at https://www.clinicalstudydatarequest.com.


