Abstract
Objective:
Compare the acute effects of walking the golf course versus using a golf cart during a round of golf on biological markers of joint disease, joint pain, and cardiovascular parameters in individuals with knee osteoarthritis (OA).
Methods:
Participants with knee OA (n=10) above the age of 50 were recruited for this crossover designed study in which they completed two 18-hole rounds of golf; 1) walking the course 2) using a golf cart (GC). Five control participants (n=5) performed the walking condition only. Step count, heart rate, rating of perceived exertion (RPE) and pain using the numeric pain rating scale (NPRS) were measured during the round. Serum was collected at baseline, 9th hole (halfway), and 18th hole (completion) and tested for biomarkers associated with tissue turnover (cartilage oligomeric matrix protein, COMP), inflammation (TNF-α, IL-1β, IL-6), and degradative enzyme production (MMP-3, MMP-13).
Results:
In knee OA participants, walking the course was associated with significantly higher step count and duration of moderate/vigorous physical activity (72.2% vs. 32.6% of the round) but did lead to a significant increase in knee joint pain (p<0.05). Both conditions caused COMP and MMP-13 concentration increases from baseline to completion (P<0.05) but inflammatory markers (TNF-α, IL-6 and IL-1β, p<0.05) only increased when walking the course. Biomarker concentrations did not increase in control participants.
Conclusion:
Walking the course optimizes the duration of moderate/vigorous activity during a round of golf, but the GC is a beneficial option in those with exacerbated joint pain and inflammation that would otherwise limit participation.
INTRODUCTION
Knee Osteoarthritis (OA) is a leading cause of disability in the United States (US) occurring in 13% of people above the age of 60.1 In these patients aerobic exercise recommendations advocate for a minimum of 30 minutes of daily walking exercise at moderate intensity (40–60% of heart rate maximum), five times/week.2 These recommendations are based on cardiac health and the impact of this type of exercise on an individual’s cartilage disease remain largely unknown. Trials of walking exercise cause significant short-term improvements in knee pain, functional status and quality of life in patients with knee OA. However, sustained compliance with regular walking exercise programs has been reported to be as low as 50%, resulting in a loss of therapeutic benefits soon after program completion.3,4 Evidence suggests that patients stop exercising due to exercise-induced symptom exacerbation, beliefs that exercise could be damaging to their knees, and reduced capacity to perform exercises at intensities and durations recommended to maintain cardiac health.4,5
Golf is a moderate level physical activity involving significant amounts of walking that consumes 3 to 6 metabolic equivalents of task (METs) per round.6 The estimated distance walked per 18-hole round (without any transportation aids) is 7km with greater than 10,000 steps taken.6 In the last 30 years, the notion that golf in the US involves significant amounts of walking has challenged with the advent of the motorized golf cart (GC). Due to pervasive use of GCs, the majority of recently developed golf courses are longer, designed specifically for cart usage, limiting the realistic ability of players to walk the course.7 Prior studies have suggested that walking the course optimizes the cardiovascular benefits of the sport compared to GC use. However, in patients with symptomatic knee OA, the motorized GC could represent an attractive option for transportation around the course by limiting abnormal joint loading, further cartilage injury and potential exacerbation of joint pain. However, no prior study has evaluated the impact of these different loading regimens during a round of golf (walking versus GC use) on an individual’s knee osteoarthritis.
This study utilized a stimulus-response framework for evaluating the effect of exercise on an individual’s knee OA. This is a methodology in which a known mechanical stimulus is applied, and the system is assessed based on the response of specific disease-related markers such as serum biomarkers of cartilage metabolism or imaging studies.8 The impact of joint loading on biomarkers associated with articular cartilage has predominantly focused on the response of cartilage oligomeric matrix protein (COMP)9,10 a structural glycoprotein that binds and stabilizes type-II collagen fibers and is a key regulator of water content within articular cartilage. Increases in COMP have been suggested to be related to stress on the articular cartilage and the movement of water from within the joint. When serum concentrations have been measured in response to lower-extremity loading, there are dose-dependent increases which suggest a potential clinical benefit of this marker in assessing a biological response to loading.9,11 Other serum biomarkers associated with cartilage metabolism have also been investigated on a limited basis in response to a physiologic loading stimulus. For example, matrix metalloproteinases (MMPs) that are known catalyzers of extracellular matrix breakdown of articular cartilage have been shown to increase in the serum in response to joint loading.12 The serum concentration of inflammatory mediators such as IL-6, IL-1β and TNF-α have also been shown to be responsive to joint loading protocols and have relationships to changes in biomechanical variables at the knee.13,14 Both walking and GC use represent different levels of long duration walking, and comparing the concentration of these biomarkers in response to these loading regimens may provide an indicator of the particular exercise’s impact on an individual’s cartilage and inflammation.
The primary objective of this study was to compare two different loading paradigms (walking vs GC use) on the metabolism of cartilage, systemic inflammation and joint pain in individuals with knee OA. The primary hypothesis was that participants with knee OA would have a significant increase in serum COMP concentration (primary biomarker) and joint pain immediately after a round of golf compared to baseline in response to walking the course compared to GC use. Secondary outcomes included the duration of the round performing moderate/vigorous physical activity (MVPA), rating of perceived exertion (RPE) and step count. Over 9 million people above the age of 50 play golf in the United States, a significant proportion of whom likely have knee OA. The findings of the present study may be of particular importance to their continued participation, or provide information for novice individuals with knee OA considering engaging in golf as part of a physician prescribed exercise program as is occurring in countries such as the United Kingdom.6 Control participants without knee OA were also included to evaluate the comparative serum biomarker and pain response while walking the course compared to knee OA participants. Stimulus response frameworks have been shown to aid in differentiating individuals with knee OA and controls, and therefore the inclusion of the control group allowed us to attribute serum biomarker responses to the presence of OA rather than a normal loading effect. Hence this group only performed the walking condition.
METHODS
Participants
The study received ethical approval from our Institutional Review Board. This study conforms to all STROBE guidelines and reports the required information accordingly (see Supplementary Checklist). Informed written consent was provided by participants with symptomatic unilateral medial knee OA (n=10) and control participants without a history of symptomatic knee OA (n=5). OA participants were included if they met American College of Rheumatology (ACR) clinical criteria for knee OA. This includes knee pain plus 3 of the following 6 criteria: age>50 years, morning stiffness <30minutes, crepitus on active movement, tenderness of the bony margins of the joint, bony enlargement of the joint noted on exam and lack of palpable warmth of the synovium. Radiographic grading of knee OA was confirmed according to the Kellgren and Lawrence rating scale 15 by a radiologist who was blinded to the participant demographic information. A K-L grade in the symptomatic knee of 1–3 warranted study inclusion. Control participants had no history of knee OA and did not fulfill ACR criteria for diagnosis. Across both groups (knee OA and controls), participants had to be regular golfers defined as playing an 18-hole round at least 1–2 times/month. Participants were excluded if they had prior total knee arthroplasty, or other lower extremity joint pain (hips or ankles) or low back pain. Conditions precluding walking the golf course such as severe cardiovascular disease, uncontrolled hypertension or stroke led to study exclusion. Participants who typically require pain medications during a round of golf were also excluded.
Study design (Figure 1)
Figure 1:

Study outline – Participants performed 2 rounds of golf: 1) Walking the course or 2) GC between holes with outcome measures taken at the timepoint specified. The order in which participants performed the rounds was randomized.
A two-phase crossover sequential design was used with all OA participants performing two rounds of golf on separate days at least 1 week apart. This was long enough to allow for a washout period between rounds in biomarker concentrations.16 All rounds of golf were played over a 4-month period at a specific 18-hole golf course (Glenview Park District Golf Course, Glenview, IL, USA) with an average walking distance of approximately 7KM, and that allowed players to either walk or use a GC for transportation. Participants with knee OA played the two 18-hole rounds 1 week apart, on days with comparable weather conditions (i.e. temperature between 62–70°F for all rounds in the study). An individual’s rounds (walking vs GC) were played within a temperature of 5°F of each other at the start of the round. To prevent against potential diurnal variability in the biomarkers tested and joint pain, participants performed the rounds at the same time of day in consecutive weeks. Participants were asked if they had any constitutional symptoms (such as fevers or chills) on the day of the round and were allowed to postpone the round if needed, however we had no participants with this issue. In the ‘walking the course’ condition, the participants walked the entire course and used a manual pushcart for their golf clubs. In the GC condition, participants used a motorized GC as transport between holes along standard paths on the course. The order of particular playing conditions (walking the course versus motorized GC usage) was randomized for each of the participants with knee OA. At the time of recruitment, a two-choice random number generator was used to decide which order of round the participants would perform first i.e. a ‘0’ being walking the course, and ‘1’ GC use. Control participants performed the walking condition only. A member of the study team accompanied the participants for safety as requested by our institutional review board (IRB) and to ensure that all subjective outcome measures were performed at the specific time points required during the round. However, the subjective outcome measures were collated and evaluated by separate investigators who were blinded to the specific golfing condition the participants had performed.
Outcome measures
Step count, heart rate measurement, rating of perceived exertion
Participants wore an activity monitor on their left wrist (Garmin Vivoactive HR®). This device has been shown to have good validity for all constant and varying velocities for monitoring step counts and heart rate.17 Following the completion of the round of golf, the players monitors were read on a laptop device with the Garmin® software pre-installed. The proportion of the round a participant’s heart rate was greater than 50% of their calculated heart rate maximum was also measured and defined as moderate/vigorous physical activity (MVPA).18 Participants also rated their perceived exertion (RPE) using the Borg scale CR1018 every third hole during the round.
Numeric Pain Rating Scale (NPRS)
During each golf session pain intensity in each knee will be recorded using an 11-point (0–10) NPRS. The NPRS has previously been validated for the assessment of pain in knee OA19 and was anchored on the left with the phrase ‘no pain’ and on the right with the phrase ‘extreme pain’. NPRS was collected at baseline prior to the start of the round, halfway during the round at the end of the 9th hole and the completion of the 18th hole (round completion). All pain scores were evaluated by an investigator who was blinded to which round that had been performed.
Serum Biomarker Analysis:
Participants did not exercise strenuously 24 hours prior to the day of testing and were seated in a chair 30mins immediately before the start of each round. Prior to the first hole (baseline), 9th hole and at completion of the round, a 5mL blood sample was drawn into a vacutainer tube. Blood was allowed to clot for 30 minutes on ice, centrifuged, decanted and transferred to our laboratory for storage at −80°C until assayed. All serum biomarker assays were performed in duplicate according to manufacturer’s instructions. Serum levels of COMP were determined using the Human COMP Quantikine ELISA kit (R&D systems, Minneapolis, MN). Serum inflammatory cytokine concentrations were determined using a custom Milliplex Human Cytokine\Chemokine Luminex assay (Millipore Corp. St. Louis, MO). Inflammatory markers tested in duplicate were tumor necrosis factor-α (TNF-α), IL-1β, and IL-6. Serum MMP-3, and MMP-13 concentrations were determined using the Luminex Performance Human MMP magnetic panels (R&D systems, Minneapolis, MN). Serum samples were mixed with small (5.6 micron), fluorescent polystyrene microspheres bound with a monoclonal antibody specific for each biomarker analyzed. Following incubation of the beads with serum, the samples were washed to remove unbound proteins, and the specific proteins bound to the antibody beads were labeled with a biotinylated polyclonal secondary antibody. After incubation, the beads were washed again to remove unbound secondary antibody, and the proteins bound to the beads were labeled with streptavidin-phycoerythrin for detection. Beads were then read using a Luminex 200 System (Luminex, Austin, TX) to determine fluorescent intensity for each bead. The median fluorescence intensity of counted beads for each sample were used to determine concentration for the sample.
Statistical analyses
All data were analyzed using SPSS (Version 26, SPSS, Inc. Chicago, IL). The data was firstly examined for normality of distribution and homogeneity of variance. The Mann-Whitney U test was used to examine differences in baseline continuous variables. To determine whether serum biomarker concentrations varied between the walking and GC conditions or with time, a 2x3 (condition x golfing-type duration) analysis of variance (ANOVA) with repeated measures was performed for the biomarker of interest. A paired T-test was performed to compare baseline serum biomarker concentrations with each individual time point for that condition, i.e. 9th hole concentration versus baseline and 18th hole concentration versus baseline. Paired T-tests were also used to compare the maximum heart rate attained, RPE and step count for each golfing condition at each time point. The NPRS scores for each testing condition were compared using the Friedman test with post hoc Wilcoxon Signed-Rank test, secondary to not meeting the assumption of normal distribution. Kendall’s Tau (τ) test was performed to investigate correlations between serum biomarker concentrations. Strength of correlations between biomarker concentrations were defined as weak, τ<0.3, moderate τ=0.3–0.6 and strong τ≥ 0.6.
RESULTS
Participant characteristics: (Table 1)
Table 1 –
Participant Characteristics. T-test were used to compare across groups. The Mann-Whitney U test was used for parameters with a non-normal distribution
| VARIABLE | KNEE OA PARTICIPANTS (N=10) | CONTROL (N=5) | p-value |
|---|---|---|---|
| Mean Age (years, SD) | 67.5 (±5.3) | 62.2 (±3.0) | 0.231 |
| SEX | 7 male (70.0%), 3 female (30.0%) |
3 male (60%) 2 female (40%) |
N/A |
| BMI (Kg/m2, SD) | 27.0 (0.5) | 25.2 (0.2) | 0.423 |
| K-L Grade | GRADE 2 n=2 (20%) GRADE 3 n=5 (50.0%) GRADE 4 n=3 (30.0%) |
N/A | N/A |
| Average times/month play a round of golf | 7.9 (±3.2) | 7.2 (±3.1) | 0.276 |
| Golf Handicap | 17.2 ±3.7† | 17.7 (±3.2) | 0.343 |
| Typical transportation around the course | Walking – 5 (50%) Golf Cart – 5 (50%) |
Walking – 4 (80%) Golf Cart – 1 (20%) |
N/A |
2 subjects did not have a golf handicap
BMI=Body mass index
K-L grade = Kellgren Lawrence grade
Participants with knee OA had a mean age of 67.5 (+/−5.3). Of the ten participants with knee OA 70% were male and 30% female. In terms of golf participation, they played an average 7.9 rounds (+/−3.2) rounds of golf per month with 50% playing without the use of a GC during a typical round. Participants in the symptomatic OA group and control groups had similar characteristics without any differential findings related to demographics (p>0.05 for all demographic characteristics).
Cardiovascular and Round-Related Parameters (Table 2)
Table 2 –
Cardiovascular and Round Related Parameters for OA participants (n=10). Paired T-test were performed to compare these parameters between rounds.
| VARIABLE | WALKING (n=10) | GOLF CART (n=10) | p-value |
|---|---|---|---|
| Step Count (Mean±SD) | 12,227 (±1034) | 7023 (±1022) * | 0.02 |
| Percentage of Round with MVPA (±SD) | 72.2% (±15.7) | 32.6% (±7.8) * | 0.003 |
| Duration of Round (±SD) | 4hrs 32mins (±31.2) | 3hrs 52mins (±22.7) | 0.212 |
p<0.05)
Participants with knee OA did not have a significant increase in subjective rating of perceived exertion with both rounds (walking vs. cart) throughout the round (p>0.05). However as shown by table 2, more objective metrics, showed that when walking the course, participants with knee OA had a significant increase in maximum heart rate attained during the round (p<0.05) and step count (mean step count 12,227 (+/−1034) while walking the course versus 7023 (+/− 1022) while using GC, p=0.001). There was no significant difference in the duration of the round when walking the course which was on average 4 hours and 32mins (+/−31.2) compared to 3hours 52 mins (+/−22.7) when using the GC. Of these rounds, on average individuals with knee OA performed MVPA for 72.2% of the round when walking the course compared to 32.6% when using the GC.
Knee Joint Pain (Figure 2)
Figure 2:
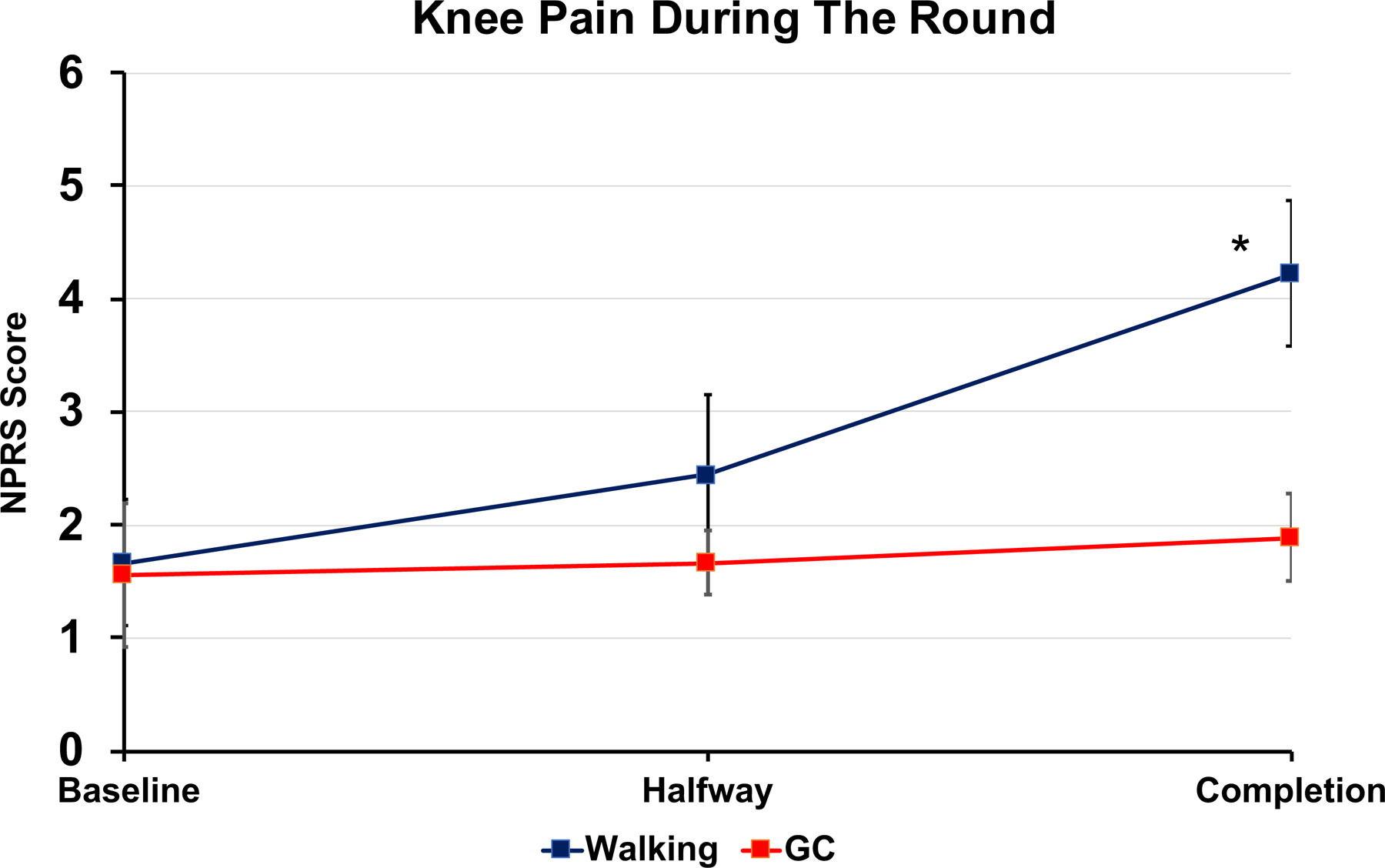
Effected Knee Joint Pain during the round. T-tests were performed to compare baseline pain with each individual time point for that golfing condition. n=10. *p<0.05
There was no significant difference in knee joint pain at baseline i.e., the start of each round (walking versus GC use) Using the Friedman test, NPRS scores in individuals with knee OA, knee pain in the symptomatic knee significantly increased at completion of the round walking the course (mean increase on NPRS 2.56 ± 2.40 X2r = 12.05, p=0.002) compared to baseline. However, when using the GC there was no significant increase in symptomatic knee joint pain compared to baseline (mean increase 0.33±1.41 X2r= 3.15, p=0.207). All control subjects did not have knee pain at baseline and also had no pain at completion of the round.
Serum Biomarker Analyses (Table 3)
Table 3. Serum Biomarker Concentrations for OA participants.
Biomarker concentrations at baseline, halfway (9th hole) and at completion (18th hole) for the ten (n=10) OA participants. Paired T-tests were performed to compare baseline serum biomarker concentrations with each individual time point for that condition. Individual serum concentrations comparisons across conditions were not performed as part of this analysis.
| CONDITION | Baseline | Halfway (9th hole) | Completion (18th hole) |
||
|---|---|---|---|---|---|
| Inflammatory Cytokines | TNF | WALKING | 4.38±3.77 |
5.54±4.65
*
(p=0.029) |
5.71±4.67
*
(p=0.004) |
| GC | 5.90 ± 5.98 | 6.98±7.17 (p=0.091) |
6.40±6.40 (p=0.457) |
||
| IL-1 | WALKING | 3.943 ± 4.56 |
5.63 ± 3.01
*
(p=0.045) |
5.85 ± 2.24
*
(p=0.021) |
|
| GC | 5.47 ± 1.93 | 6.36 ± 1.90 (p=0.314) |
7.63 ± 2.21 (p=0.053) |
||
| IL-6 | WALKING | 1.04±0.45 | 1.50±0.62 (p=0.082) |
1.81±0.58
*
(p=0.04) |
|
| GC | 1.31±0.55 | 1.61±0.36 (p=0.363) |
2.00±0.99 (p=0.129) |
||
| Cartilage Degradative Enzymes | MMP-3 | WALKING | 5024.48±2108.83 |
7729.64±1775.23
*
(p=0.001) |
7843.24±1885.33
*
(p=0.001) |
| GC | 5942.20±1846.27 |
8489.57±1912.70
*
(p=0.005) |
8979.50±1686.57
*
(p=0.001) |
||
| MMP-13 | WALKING | 178.54±48.62 |
246.07±67.23
*
(p=0.013) |
246.85±59.49
*
(p=0.026) |
|
| GC | 245.27±42.08 | 268.33±38.38 (p=0.27) |
290.41±45.38
(p=0.040) |
||
| Extracellular matrix turnover | COMP | WALKING | 813.60±191.92 |
1286.82±266.92
*
(p=0.0001) |
1321.06±310.38
*
(p=0.002) |
| GC | 983.55±346.68 | 1022.55±263.97 (p=0.428) |
1133.06±208.17
*
(p=0.023) |
||
p<0.05)
1). Inflammatory Cytokines
There was a significant increase in serum concentrations of TNF-α and IL-1β at halfway and completion when walking the course but not with the GC. Similarly, the serum IL-6 concentration significantly increased at round completion walking the course but did not when using the GC. A time effect was found for change in serum TNF-α (F2,34= 19.52, p=0.002), IL-1β (F2,34= 19.52, p=0.002) and IL-6 concentrations (F2,34= 8.18, p=0.001) during the rounds. There was no time x golfing condition interaction (TNF-α F2,34=5.12, p=0.012, IL-1β F2,34=1.70, p=0.323, IL-6 F2,34=0.08, p=0.76) for change in concentration of any of these inflammatory cytokines.
2). Cartilage Degradative Enzymes
In both golfing conditions, there were significant increases in the serum concentration of MMP-3 at halfway and completion of the round. Similarly, for change in MMP-13 concentration, repeated measure analysis revealed a time effect (F2,34=10.01 p<0.001) but not a time x golfing condition interaction (F2,34=1.52, p=0.232). There was a significant increase in serum concentration of MMP-13 at the halfway point when walking the course and in both golfing conditions at round completion compared to baseline. Of note however, repeated measure analysis revealed a time effect for MMP-3 concentration change during the rounds F2,32=35.52, p<0.001, but no time x golfing condition interaction (F2,32=0.199, p=0.820).
3). Extracellular matrix Turnover
Compared to baseline there was a significant increase in serum COMP concentration walking the course at both time points (58% at halfway, p=0.0001 and 62% at completion p=0.002 increases respectively). In contrast, when using the GC, the COMP concentrations were elevated by 4% (p=0.428) at completion of the 9th hole and 15% at completion of the 18th hole (p=0.023) when compared to baseline. The repeated measures analysis for serum COMP concentration found a significant playing time effect (baseline vs. halfway vs. completion F2,32= 22.6, P < 0.001). There was also a significant time x golf condition interaction F2,32=8.6, p=0.001). There were no significant changes in COMP concentration in control participants without knee OA during or at completion of the round.
Serum Biomarker Correlations
Considering all samples in individuals with knee OA across both golfing conditions, significant weak correlations for COMP were found with TNF-α (τ=0.20, p=0.024), IL-6 (τ=0.21, p=0.021), and MMP-13 (τ=0.24, p=0.01). Inflammatory cytokines did have moderate to strong significant correlations with each other, with IL-6 correlating to TNF-α (τ=0.40, p<0.001) and IL1-β (τ=0.61, p<0.001) respectively. MMP-13 had moderate to strong correlations with inflammatory cytokines including TNF-α (τ=0.44, p<0.001), IL-6 (τ=0.70, p<0.001) and IL-1β (τ=0.63, p<0.001) concentrations.
DISCUSSION
Physical activity has been shown to have significant positive effects on function and quality of life in patients with knee OA, and yet many do not engage in these programs due to concern regarding progression of joint damage and exacerbation of symptoms. Playing golf recreationally could represent an ideal sport as it allows for differential walking strategies that may be of benefit to individuals with the disease. Our study, for the first time, utilized a stimulus response framework to assess the impact of these loading strategies on individual biological joint disease, joint pain as well as cardiovascular parameters. In keeping with our primary hypothesis, our study found that in individuals with knee OA, there was a significant increase in serum COMP concentration and knee joint pain when walking the course compared to using the GC. Repeated measures analysis showed that the COMP differences were larger, the further into the round we tested participants. Changes in COMP have been shown to be representative of the total knee joint loading experienced. After cyclical physiologic loading of the knee joint there is enhanced diffusion of COMP fragments from the articular cartilage into the systemic circulation.20 In individuals with knee OA, the magnitude of the acute increase in serum COMP concentration from baseline, after as little as 30 minutes of walking has a significant relationship to a decrease in cartilage thickness at 5-years post-testing.21 Prior studies in non-OA individuals during a long-duration activity such as running marathon found that serum COMP concentration can significantly increase from 24–60%14,22, which is comparable to our study in individuals with knee OA when they walked the course. However an intermittent loading pattern such as that during GC usage in our study was associated with a maximum increase of only 15%. These findings are also similar to a prior study which found that in individuals with knee OA continuous walking for 45 minutes on a treadmill was associated with a significant increase in serum COMP and knee joint pain, but the same duration of walking in an interval format was not.16 Of note, there is as yet no threshold cut off for COMP change that suggests destruction to the joint, but the findings we present are likely an indicator of stress placed on the remaining articular cartilage in an individual’s knees.
The changes in serum COMP concentration in the present study did have a significant positive correlation to MMP-13, a collagenase involved in the breakdown of the extracellular matrix of cartilage.14 An increase in serum MMP-13 concentration was found with both golfing conditions at completion of the round suggesting that GC usage does not limit changes in this marker release. The present study also demonstrated a significant increase in inflammatory and cytokine responses while walking the course (TNF-α, IL-1B and IL-6). TNF-α is a pleiotropic cytokine that is released from tissue macrophages and IL-6 is an acute phase reactant, produced by a wide variety of cell types including monocyte/macrophages and fibroblasts. Prior research has demonstrated significant inflammatory and cytokine responses immediately after exercise that can remain elevated for several days.23–25 Although inflammatory marker changes are likely representative of a systemic response to exercise, they do have a relationship to joint pain. Studies have shown that the likelihood of individuals with knee OA engaging in a sport is dependent on the pain experience they have during it.26 If pain and inflammation are exacerbated while walking the course it may limit the participation of individuals in a sport like golf. Overall, the biomarker and pain findings in this study suggest that intermittent long-duration exercise during a round of golf (such as with a GC) causes less pain, change in cartilage stress markers (assessed using COMP concentration as a surrogate) and systemic inflammation compared to walking the course.
However, the pain and biomarker findings above must be balanced against the cardiovascular effects of the respective regimens tested in this study. Regularly walking the course has been shown to have a multitude of health benefits including improved glycemic control, cardiovascular health and lower extremity muscle strength.6 A recent longitudinal study of 300,000 Swedish golfers (a country in which GC use is rare) showed that the average life expectancy of those playing golf regularly was 5% longer than those who do not.27 The present study found that in individuals with knee OA, golf overall had beneficial effects on cardiovascular parameters in both regimens, although these benefits were significantly larger when walking the course. These effects included longer duration of MVPA and higher maximum heart rate attained. This is in keeping with Broman et al18, who found that elderly golfers (>65 years of age) reach high exercise intensity more than half of the total playing time when walking a normal 18 hole golf course. The topography of the course (more hills), as well as holding one’s golf clubs (versus pulling the clubs), and the weight of the golf bag will likely further increase the level of MVPA attained. These were not specifically investigated in our study, in which these factors were standardized. However also similar to our study, Zunzer et al28 found that individuals that used a golf cart, had significantly lower mean heart rate than those who walked the course irrespective of how they pulled or carried their clubs. More specifically it has been shown that on average a golfer walking the course expends approximately 5.3METs compared to 3.5METs when using a golf cart.6 This difference in energy expenditure has been shown to have some relationship to their age and sex which we were unable to ascertain in this study due to the small sample size. A major strength of our study is that it is one of the first that included a crossover sequential design, such that the same participants performed both rounds (walking vs. GC use). Prior comparative studies have been randomized so that participants were placed in a single arm of the study and there was no crossover. Overall, despite the significant cardiovascular benefit of walking the course, participants in the present study still spent >30% of both rounds performing MVPA irrespective of the mode of transportation used and easily surpassed daily aerobic physical activity guidelines. This is of importance for individuals with knee OA who may consider utilizing the GC due to exacerbation of their knee OA symptoms.
Limitations:
The findings of this pilot study are limited by the small sample size of participants with knee OA. In addition, the inclusion criteria necessitated participants playing golf regularly and walking the course therefore the participants were likely more functionally capable than many individuals with knee OA. In addition, OA is generally more common in females with higher BMI and more sedentary, and the future studies should consider utilizing golf as a means to improve physical activity in this population. Biochemical analyses were performed on the serum and not the knee synovial fluid of our participants which theoretically may limit biomarker specificity to the joint of interest. COMP is known to diffuse from the synovial fluid (SF) into the lymphatics and then the bloodstream with significant correlations between its concentration in the SF and the serum being shown in prior studies.29 This marker is present in a number of tissues in the body, but the concentration of this protein in non-articular tissues is several magnitudes lower than articular cartilage and meniscus.30 The inflammatory markers TNF-α, IL-6 and IL-1β that were examined in this study, are not specifically burden of OA disease markers, but maybe released from other tissues in the body and could vary by the time of day they are measured. We aimed to address this limitation in biomarker concentrations by the sequential crossover design of the study with all rounds performed at the same time of day and by excluding participants who had on-going joint pain in their ankles, hips and lumbar spine.
Finally, the present pilot study was designed to investigate transient increases in biomarker concentrations in response to joint loading during golf. However, the rate of decrease in concentration of these biomarkers back to baseline following walking, could be informative of the longer-term effect of this level of joint loading, and would be beneficial to investigate in future studies.
CONCLUSION
In individuals with knee OA, a round of golf maybe a particularly beneficial activity by allowing them to attain national aerobic physical activity guidelines irrespective of the mode of transportation used around the course. Clinicians should encourage individuals with knee OA to walk the course due to increased amounts of moderate intensity exercise performed, potentially modifying cardiovascular risk factors. However, in those individuals in whom joint pain and inflammation are exacerbated, the GC is a viable option that may allow them to still remain active. Future studies should follow patients longitudinally to ascertain longer term effects of these regimens on osteoarthritic cartilage adaptations and overall function in both sedentary individuals and regular golfing cohorts.
Supplementary Material
What is Known?
Golf is a moderate intensity physical activity, advocated as a prescribed exercise intervention, limited by the pervasive use of the golf cart. In knee osteoarthritis the golf cart may represent an approach to optimizing exercise participation, limiting joint stress, inflammation and pain.
What is New?
The stimulus-response framework utilized found that joint stress, pain and inflammation are exacerbated walking the course, but intensity of physical activity is higher. With the golf cart, individuals with knee osteoarthritis spend a significant period of time performing moderate intensity activity. Golf irrespective of mode of transportation should be advocated as an exercise intervention for these individuals.
Acknowledgments
The project described was supported by the Richard F. Materson New Investigator Award from the Foundation for PM&R, the Young Investigator Award from the American Medical Society of Sports Medicine (AMSSM) and the National Center for Advancing Translational Sciences 2KL2TR001424-05A1.
REFERENCES
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism 2008;58(1):26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lundebjerg N Exercise prescription for older adults with osteoarthritis pain: Consensus practice recommendations. Journal of the American Geriatrics Society 2001;49(6):808–823. [DOI] [PubMed] [Google Scholar]
- 3.Ettinger WH Jr., Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997;277(1):25–31. [PubMed] [Google Scholar]
- 4.Rejeski WJ, Brawley LR, Ettinger W, Morgan T, Thompson C. Compliance to exercise therapy in older participants with knee osteoarthritis: implications for treating disability. Med Sci Sports Exerc 1997;29(8):977–985. [DOI] [PubMed] [Google Scholar]
- 5.Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? A qualitative study of primary care patients with osteoarthritis of the knee. Fam Pract 2006;23(5):558–567. [DOI] [PubMed] [Google Scholar]
- 6.Murray AD, Daines L, Archibald D, et al. The relationships between golf and health: A scoping review. British Journal of Sports Medicine 2017;51(1):12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGwin G Jr, Zoghby JT, Griffin R, Rue LW 3rd. Incidence of golf cart-related injury in the United States. The Journal of trauma 2008;64(6):1562–1566. [DOI] [PubMed] [Google Scholar]
- 8.Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Annals of Biomedical Engineering 2004;32(3):447–457. [DOI] [PubMed] [Google Scholar]
- 9.Tseng S, Reddi AH, Di Cesare PE. Cartilage oligomeric matrix protein (COMP): A biomarker of arthritis. Biomarker Insights 2009;2009(4):33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saxne T, Heinegård D. Cartilage oligomeric matrix protein: A novel marker of cartilage turnover detectable in synovial fluid and blood. Rheumatology 1992;31(9):583–591. [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Shahi U, Kumar D, Shahi NT. Serum Cartilage Oligomeric Matrix Protein: Tool for early diagnosis and grading of severity of primary knee osteoarthritis. Int J Osteol Orthop 2014;1:1–7. [Google Scholar]
- 12.Urso ML, Pierce JR, Alemany JA, Harman EA, Nindl BC. Effects of exercise training on the matrix metalloprotease response to acute exercise. European Journal of Applied Physiology 2009;106(5):655–663. [DOI] [PubMed] [Google Scholar]
- 13.Edd SN, Favre J, Blazek K, Omoumi P, Asay JL, Andriacchi TP. Altered gait mechanics and elevated serum pro-inflammatory cytokines in asymptomatic patients with MRI evidence of knee cartilage loss. Osteoarthritis and Cartilage 2017;25(6):899–906. [DOI] [PubMed] [Google Scholar]
- 14.Neidhart M, Müller-Ladner U, Frey W, et al. Increased serum levels of non-collagenous matrix proteins (cartilage oligomeric matrix protein and melanoma inhibitory activity) in marathon runners. Osteoarthritis and Cartilage 2000;8(3):222–229. [DOI] [PubMed] [Google Scholar]
- 15.Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases 1957;16(4):494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayabalan P, Gustafson J, Sowa GA, Piva SR, Farrokhi S. A Stimulus-Response Framework to Investigate the Influence of Continuous Versus Interval Walking Exercise on Select Serum Biomarkers in Knee Osteoarthritis. American Journal of Physical Medicine and Rehabilitation 2019;98(4):287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wahl Y, Düking P, Droszez A, Wahl P, Mester J. Criterion-validity of commercially available physical activity tracker to estimate step count, covered distance and energy expenditure during sports conditions. Frontiers in Physiology 2017;8(SEP). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broman G, Johnsson L, Kaijser L. Golf: A high intensity interval activity for elderly men. Aging Clinical and Experimental Research 2004;16(5):375–381. [DOI] [PubMed] [Google Scholar]
- 19.Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- 20.Mündermann A, Dyrby CO, Andriacchi TP, King KB. Serum concentration of cartilage oligomeric matrix protein (COMP) is sensitive to physiological cyclic loading in healthy adults. Osteoarthritis and Cartilage 2005;13(1):34–38. [DOI] [PubMed] [Google Scholar]
- 21.Erhart-Hledik JC, Favre J, Asay JL, et al. A relationship between mechanically-induced changes in serum cartilage oligomeric matrix protein (COMP) and changes in cartilage thickness after 5 years. Osteoarthritis and Cartilage 2012;20(11):1309–1315. [DOI] [PubMed] [Google Scholar]
- 22.Kim HJ, Lee YH, Kim CK. Changes in serum cartilage oligomeric matrix protein (COMP), plasma CPK and plasma hs-CRP in relation to running distance in a marathon (42.195 km) and an ultra-marathon (200 km) race. European Journal of Applied Physiology 2009;105(5):765–770. [DOI] [PubMed] [Google Scholar]
- 23.Harkey MS, Luc BA, Golightly YM, et al. Osteoarthritis-related biomarkers following anterior cruciate ligament injury and reconstruction: A systematic review. Osteoarthritis and Cartilage 2015;23(1):1–12. [DOI] [PubMed] [Google Scholar]
- 24.Atkinson AJ Jr., Colburn WA, DeGruttola VG, et al. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clinical Pharmacology and Therapeutics 2001;69(3):89–95. [DOI] [PubMed] [Google Scholar]
- 25.Scott JPR, Sale C, Greeves JP, Casey A, Dutton J, Fraser WD. Effect of exercise intensity on the cytokine response to an acute bout of running. Medicine and Science in Sports and Exercise 2011;43(12):2297–2306. [DOI] [PubMed] [Google Scholar]
- 26.Beckwée D, Vaes P, Cnudde M, Swinnen E, Bautmans I. Osteoarthritis of the knee: Why does exercise work? A qualitative study of the literature. Ageing Research Reviews 2013;12(1):226–236. [DOI] [PubMed] [Google Scholar]
- 27.Farahmand B, Broman G, De Faire U, Vågerö D, Ahlbom A. Golf: A game of life and death - Reduced mortality in Swedish golf players. Scandinavian Journal of Medicine and Science in Sports 2009;19(3):419–424. [DOI] [PubMed] [Google Scholar]
- 28.Zunzer SC, von Duvillard SP, Tschakert G, Mangus B, Hofmann P. Energy expenditure and sex differences of golf playing. Journal of Sports Sciences 2013;31(10):1045–1053. [DOI] [PubMed] [Google Scholar]
- 29.Gheita TA, El-Awar AH, El-Ansary MM, Raslan HM, El-Defrawy AO. Cartilage oligomeric matrix protein (COMP) levels in serum and synovial fluid in osteoarthritis (OA) patients: Correlation with clinical, radiological and laboratory parameters. Osteoarthr Cartil 2015;23(2). [Google Scholar]
- 30.Neidhart M, Hauser N, Paulsson M, Dicesare PE, Michel BA, Häuselmann HJ. Small fragments of cartilage oligomeric matrix protein in synovial fluid and serum as markers for cartilage degradation. British Journal of Rheumatology 1997;36(11):1151–1160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


