Abstract
Introduction
The high frequency of COVID-19 has had an impact on the psychological health of all countries and socioeconomic groups around the world, with refugees suffering the brunt of the burden. The aim was to assess the relationship between fear of COVID-19 and depression, anxiety, stress, and PTSD among Syrian refugee parents residing in the Greater Toronto Area.
Methods
A convenience sample of 274 Syrian refugee parents residing in Ontario was recruited. Fear of COVID-19 was measured using the Fear of COVID-19 Scale (FCV-19S). Levels of depression, anxiety, stress and PTSD were assessed using the Depression Anxiety Stress Scales (DASS-21), and Primary Care PTSD screen (PC-PTSD). Multiple Linear Regression analyses were performed to assess the relationship between FCV-19S and the DASS-21 subscales and PC-PTSD.
Results
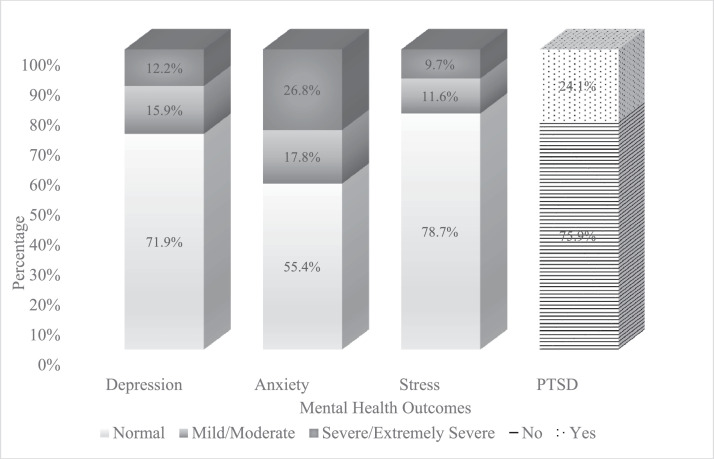
Severe levels of depression, anxiety, and stress were reported by 12.2%, 26.8%, and 9.7% of participants respectively, and 24.1% screened positive for PTSD. FCV-19S was associated with higher levels of stress (β = 0.27, p = 0.006), anxiety (β = 0.40, p <0.001), depression (β = 0.32, p = 0.001) and PTSD (β = 0.04, p = 0.015).
Discussion
Government initiatives should consider tackling fear concerning pandemics among Syrian refugee parents to help enhance their mental well-being.
Keywords: Syrian, Refugee, Canada, Fear of COVID-19, Mental health
1. Introduction
In December of 2019, the coronavirus disease 2019 (COVID-19) was first detected in Wuhan, China (Shereen et al., 2020). In March of the following year, the virus was proclaimed a public health concern and a global pandemic (Cruz et al., 2021; Velavan and Meyer, 2020). As of January 31, 2022, COVID-19 has infected more than 370 million people worldwide, resulting in over 5.6 million deaths (WHO 2021). According to the Government of Canada, more than 3 million COVID-19 cases and over 30,000 death have been reported in Canada (GC. Coronavirus disease (COVID-19) 2021). On December 14, 2020, Canada began administering the first COVID-19 vaccinations, starting with high-risk populations (e.g., front-line workers, and elderly adults). General immunization for all Canadians began in April 2021 and older adults became eligible to receive their second vaccinations in May 2021 (depending on the province or territory) (PHAC 2021).
COVID-19′s high prevalence has had an influence on the physical and phycological health of all nations and socioeconomic groups around the world, regardless of whether they were infected or not, with minorities and refugees bearing the brunt of the burden (Warren et al., 2021; Kirby, 2020). A study by Wang et al. (2021) showed that physical symptoms, resembling COVID-19 infection, were associated with the need for health information, which in turn was associated with adverse mental health outcomes (Wang et al., 2021). The effect of the pandemic on mental health, including high rates of anxiety, depression, post-traumatic stress disorder, psychological distress, and stress in the general population, has been reported in several countries across America, Asia, the Middle East, and Europe (Xiong et al., 2020), with one study reporting that Pakistan and Poland had the highest anxiety, depression, and stress scores (Wang et al., 2021). In particular, it is likely to trigger feelings of fear in individuals, which may elicit or exacerbate mental health issues and overall poor well-being (Fitzpatrick et al., 2020; Shigemura et al., 2020; Ornell et al., 2020).
Fear is normally an adaptive response to a realistic or perceived threat that assures one's survival (Gullone, 2000). It is considered one of the most common psychological reactions to pandemic diseases, which is distinct from other disasters (Ahorsu et al., 2020). Studies in the literature have found that fear of COVID-19 is associated with adverse mental health outcomes. A recent meta-analysis study by Şimşir et al. (2021) included 33 different studies from 18 different countries, conducted among the general population and college and university students, reported that fear of COVID-19 was related to anxiety, traumatic stress, stress, and depression, among other mental health issues (Şimşir et al., 2021). In addition, a study on psychological distress in the general population in China showed that individuals between 18 and 30 years of age or above 60 years of age had the highest COVID-19 Peritraumatic Distress Index (CPDI) scores and that the level of distress was highest among migrant workers (Qiu et al., 2020). Another recent study among immigrant women during the pandemic found that symptoms of depression and anxiety among participants were at a much higher level than prior to the pandemic (Ornelas et al., 2021).
As of October 31, 2020, a total of 44,620 Syrian refugees have been welcomed into Canada since November 2015 (GC. WelcomeRefugees 2021). According to studies, refugees are more prone to negative mental health outcomes than the general population (Filler et al., 2021; Lupieri, 2021). Feelings of insecurity, discrimination, and language barriers could all be contributing factors (Hadfield et al., 2017; Kirmayer et al., 2011; Clarke et al., 2021). For example, a longitudinal study of newly admitted adult Syrian refugees in Canada reported a 15% prevalence of depression at baseline, rising to 18% in the following year (Ahmad et al., 2021).
Another study of 12 Syrian refugee women, who were either pregnant or one-year postpartum when they arrived in Canada, discovered that more than half of the participants exhibited depressive and/or anxiety symptoms (Ahmed et al., 2017). Furthermore, refugee parents are expected to face additional post-migratory stressors due to factors such as difficulty preserving traditional practices within the family (Rosenberg et al., 2021), an unstable family unit and structure (Khamis, 2021; Miller et al., 2018), and a lack of social support and social resources (Khamis, 2021; Åkesson et al., 2019; Cantekin and Gençöz, 2017). The adversities that refugees already face, such as overcrowding, poor hygiene and nutrition, and poor access to health care, shelter, and safety, are magnified by the pandemic condition, putting this population at a higher risk for developing COVID-19 infection and mental illnesses (Júnior et al., 2020).
Given the large number of Syrian refugees in Canada, as well as the high incidence of mental health issues among this population, the psychological impacts of COVID-19 on this cohort must be investigated further. However, little is known about this virus and Syrian refugee parents in Canada from a mental health perspective. Therefore, this study aims to assess the relationship between fear of COVID-19 and mental health outcomes, specifically stress, anxiety, depression, and PTSD, among Syrian refugee parents in Canada.
2. Material and methods
2.1. Participants and data collection
This cross-sectional survey was conducted in the Greater Toronto Area of Canada between the summers of 2019 and 2021. The participants were recruited by convenience sampling. The sample of this study included 274 Syrian refugee parents. Data was collected during the COVID-19 pandemic. In total, 114 refugee parents initially recruited in the summer of 2019 participated in the study in the following summer of 2020. A separate sample of 160 participants were recruited and interviewed in the summer of 2021. At recruitment, the inclusion criteria were as follows: being a Syrian refugee parent with at least one child under the age of 18, having arrived in Canada after 2015, and residing in the Greater Toronto Area.
The questionnaire surveys were completed remotely over the phone in compliance with the COVID-19 pandemic's physical distancing requirements. The participant's oral consent was recorded after trained research assistants read out the consent form to them. Then, the assistants read out loud the questions in Arabic and recorded the respondents' oral responses in Qualtrics on a password-protected electronic tablet.
2.2. Measures
The Depression Anxiety Stress Scales (DASS-21) were used to assess mental health during the COVID-19 pandemic in several Asian (Tee et al., 2020), Middle Eastern (Wang et al., 2021), European (Wang et al., 2020), and North American countries (Wang et al., 2021), in addition to the Primary Care PTSD screen (PC-PTSD). The DASS-21 is a 21-item self-report scale proposed by Lovibond and Lovibond (1995), which is the short version of the original 42-item DASS by the same authors, and was used to measure depression, anxiety, and stress. Each subscale consists of 7 items rated on a 4-point Likert-style response scale assessing the severity of symptoms experienced within the previous week: 0 - “Did not apply to me at all”, 1- “Applied to me to some degree, or some of the time”, 2- “Applied to me a considerable degree, or a good part of the time,” and 3- “Applied to me very much, or most of the time.” As suggested by the authors, the total scores for each subscale are multiplied by 2 to obtain the full scale scores, with scores ranging from 0 to 42 (Lovibond and Lovibond, 1995) and rated on a severity scale: normal (0–9 for depression, 0–7 for anxiety, and 0–14 for stress), mild / moderate (10–20 for depression, 8–14 for anxiety, and 15–25 for stress), severe / extremely severe (21+ for depression, 15+ for anxiety, and 26+ for stress (Lovibond and Lovibond, 1995). The Arabic translated version of the 42-item DASS was reported to have good Cronbach's alpha reliability (0.93 for depression subscale, 0.90 for anxiety subscale, and 0.93 for stress subscale) (Moussa et al., 2017).
The PC-PTSD is a self-report screen for posttraumatic stress disorder (PTSD) in primary care developed by Prins et al. (2003) (Prins et al., 2003). The PC-PTSD screen consists of 4 items that inquired about any experience in the last month that was “frightening, horrible, or upsetting”. The participants’ responses were administered in a Yes/No (no = 0; yes = 1) format with individual scores ranging from 0 to 4. The PC-PTSD is psychometrically reliable in detecting PTSD with an identified optimally efficient cut-off score of 3 for both men and women, Prins et al. (2003).
The Fear of COVID-19 Scale (FCV-19S), used to measure the main independent variable, was originally developed by Ahorsu et al. (2020) and translated into Arabic by Alyami, Henning, Krägeloh and Alyami (2020), showing satisfactory internal consistency (α = 0.88) (Alyami et al., 2021). The scale includes 7 items that assess how uneasy and apprehensive the participants were about COVID-19. The items ranged from general (e.g., “I am most afraid of COVID-19.”) to specific (e.g., “My heart races or palpitates when I think about COVID-19.” A 5-point Likert scale was used to administer participants’ responses, ranging from “1- strongly disagree” to “5- strongly agree”. For all the items on the FVC-19S, a total score varying from 7 to 35 was calculated for each participant.
Sociodemographic factors measured included gender (mother/father), age, number of children, year of arrival to Canada (2016 or earlier/after 2016), self-perceived socioeconomic status (SES) captured by the question “In your current condition, here in Canada, would you say most people would categorize a household like yours as?” (measured in a 5-point Likert scale ranging from “lower income” to “upper incomes”), currently working (yes, no), lived in a refugee camp previously (yes, no) and time of data collection (summer 2020/summer 2021). Other self-reported factors included sense of belonging to Canada (measured in a 4-point Likert response format: very strong, strong, weak, or very weak), current Canadian Language Benchmark Level according to the Canadian language benchmark document (assessed through levels 0–3/ levels 4 and higher, in which level 1 is characterized as “initial basic ability”, level 2 as “developing basic ability,” and higher levels as more advanced linguistic aptitude), sponsorship program (Government-Assisted Refugee (GAR), Privately Sponsored Refugee (PSR), or other) assessed by the question “How are you sponsored?,” and degree of friendship satisfaction based on the question “How satisfied are you with the quality of the friendships you have here?” (measured in a 5-point Likert response format: very satisfied, satisfied, neutral, unsatisfied, or very unsatisfied).
2.3. Analysis
Descriptive statistics were used to summarize the outcome variables, FCV-19S, sociodemographic and other self-reported factors. Continuous variables were expressed as means and standard deviations (SDs), while categorical variables were expressed as frequencies and percentages. Simple linear regression analysis was performed to assess the relationship between FCV-19S and each of the sociodemographic and other self-reported factors with DASS-21 scales and PC-PTSD. Furthermore, four multiple linear regression models were conducted with the dependent variables being DASS-21 scales and PC-PTSD and the independent variables FCV-19S and all of the sociodemographic and other self-reported factors. Unadjusted and adjusted beta coefficient (β) and 95% confidence interval (95% CI) were reported. All regression models were adjusted for the clustering effect of belonging to the same family. All analyses were conducted using the Statistical Package for the Social Science (SPSS, version 26.0). The project was approved by the Research Ethics Board at York University (Certificate # e2019–128).
3. Results
A total of 274 participants were recruited for the present study (114 in the summer of 2020 and 160 in the summer of 2021). The descriptive statistics of the study participants' characteristics are summarized in Table 1. The mean (SD) age of the participants was 37.37 (7.13) years. The majority of the participants were mothers (59.1%) and arrived to Canada in 2016 or earlier (71.2%). Around quarter (23.7%) of total participants reported being employed at the time of data collection. Additionally, more than half of the participants (56.6%) had level 4 or higher of the Canadian language benchmark level. The mean (SD) number of children was 3.51 (1.48). Only 13.1% lived in a refugee camp in the past.
Table 1.
Characteristics of study participants and bivariate relationships.
| NMean (SD) | N (%)^ | Mean (SD) | STRESS | p value | ANXIETY | p value | DEPRESSION | p value | PTSD | p value |
|---|---|---|---|---|---|---|---|---|---|---|
| 2688.31 (10.74) | 2699.98 (11.62) | 2707.36 (10.46) | 2611.19 (1.53) | |||||||
| Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | |||||||
| FEAR OF COVID | 272 (99.3) | 16.20 (7.17) | 0.35 (0.09) | 0.000 | 0.54 (0.10) | 0.000 | 0.42 (0.09) | 0.000 | 0.04 (0.01) | 0.002 |
| Parent | ||||||||||
| Mother | 162 (59.1) | ref | ref | ref | ref | |||||
| Father | 112 (40.9) | −1.06 (1.35) | 0.435 | −1.80 (1.46) | 0.217 | −1.51 (1.31) | 0.248 | −0.12 (0.19) | 0.531 | |
| Age | 37.37 (7.13) | 0.19 (0.10) | 0.046 | 0.12 (0.10) | 0.256 | 0.15 (0.09) | 0.101 | 0.02 (0.01) | 0.205 | |
| Working Status | ||||||||||
| No | 209 (76.3) | ref | ref | ref | ref | |||||
| Yes | 65 (23.7) | −4.25 (1.54) | 0.006 | −5.07 (1.67) | 0.003 | −4.79 (1.49) | 0.001 | −0.48 (0.23) | 0.036 | |
| Canadian language benchmark level | ||||||||||
| Levels 0, 1, 2, and 3 | 108 (39.4) | ref | ref | ref | ref | |||||
| Levels 4 and higher | 155 (56.6) | −4.73 (1.38) | 0.001 | −3.92 (1.49) | 0.009 | −5.45 (1.32) | 0.000 | −0.44 (0.20) | 0.028 | |
| Self-perceived SES# | 2.26 (1.04) | −2.10 (0.63) | 0.001 | −2.74 (0.67) | 0.000 | −2.30 (0.61) | 0.000 | −0.26 (0.09) | 0.005 | |
| Number of children | 3.51 (1.48) | 0.89 (0.46) | 0.053 | 0.87 (0.50) | 0.081 | 0.79 (0.45) | 0.076 | 0.15 (0.07) | 0.022 | |
| Lived in a refugee camp | ||||||||||
| No | 238 (86.9) | ref | ref | ref | ref | |||||
| Yes | 36 (13.1) | 2.52 (1.97) | 0.202 | 2.02 (2.11) | 0.340 | 0.23 (1.92) | 0.904 | 0.29 (0.28) | 0.298 | |
| Year of arrival to Canada | ||||||||||
| 2016 or earlier | 195 (71.2) | ref | ref | ref | ref | |||||
| 2017 or later | 72 (26.3) | −2.40 (1.48) | 0.106 | −2.69 (1.60) | 0.094 | −2.10 (1.45) | 0.150 | −0.05 (0.22) | 0.830 | |
| Satisfaction with friendships* | 2.33 (1.13) | 0.92 (0.59) | 0.122 | 1.81 (0.63) | 0.004 | 1.14 (0.58) | 0.049 | 0.12 (0.08) | 0.173 | |
| Year of data collection | ||||||||||
| 2020 | 114 (41.6) | ref | ref | ref | ref | |||||
| 2021 | 160 (58.4) | 7.78 (2.44) | 0.002 | 8.59 (2.63) | 0.001 | 8.22 (2.36) | 0.001 | 0.89 (0.36) | 0.013 | |
| Sponsorship | ||||||||||
| Government assisted refugee (GAR) | 122 (44.5) | ref | ref | ref | ref | |||||
| Privately sponsored refugee (PSR) | 126 (46.0) | −3.68 (1.41) | 0.010 | −2.52 (1.53) | 0.100 | −2.74 (1.37) | 0.047 | −0.32 (0.20) | 0.117 | |
| Other | 26 (9.5) | 0.49 (2.31) | 0.832 | 2.52 (2.51) | 0.316 | 1.31 (2.25) | 0.561 | 0.57 (0.33) | 0.082 | |
| Sense of belonging to Canada$ | 1.49 (0.63) | 1.82 (1.06) | 0.088 | 2.30 (1.16) | 0.048 | 1.33 (1.04) | 0.199 | 0.24 (0.16) | 0.128 |
Scores range from 1- low income to 5- upper income,.
Scores range from 1- very satisfied to 5- very unsatisfied,.
Score range from 1- very strong to 4- very weak,.
%s may not add up to 100 due to missingness.
For the study sample, good internal consistency, as measured by Cronbach alpha, were reported for the DASS subscales (0.876 for depression subscale, 0.879 for anxiety subscale, and 0.882 for stress subscale), PTSD (0.861), and FCV-19S (0.879). The average (SD) score for fear of COVID-19 among the study participants was 16.20 (7.17). Participants reported an average (SD) score of 7.36 (10.46) for depression, 9.98 (11.62) for anxiety, 8.31 (10.74) for stress and 1.19 (1.53) for PTSD. Fig. 1 presents the levels of depression, anxiety, stress, and PTSD among the study participants. The majority of the study participants reported normal levels of depression, anxiety and stress (71.9%, 55.4%, and 78.7% respectively), and severe and extremely severe levels of depression, anxiety, and stress were reported by 12.2%, 26.8%, and 9.7% of study participants, respectively. With regards to PTSD, 24.1% of participants screened positive for PTSD (defined by a PC-PTSD score of 3 or higher). The findings of the bivariate regression analysis (Table 1) showed a positive association between fear of COVID-19 and stress (β = 0.35, p <0.001), anxiety (β = 0.54, p <0.001), depression (β = 0.42, p <0.001), and PTSD (β = 0.04, p <0.01).
Fig. 1.
Depression, anxiety, stress, and PTSD levels among Syrian refugee parents in Canada.
After adjusting for sociodemographic and all the other self-reported factors (Table 2), fear of COVID-19 was significantly positively associated with all outcomes (stress, anxiety, depression, and PTSD). For example, participants with higher fear of COVID-19 had higher stress (β = 0.27, p = 0.006), anxiety (β = 0.40, p <0.001), depression (β = 0.32, p = 0.001) and PTSD (β = 0.04, p = 0.015) levels. Additionally, the Canadian language benchmark level was negatively associated with all outcomes except PTSD. As the participant's language level increased (≥4), stress (β = −4.31, p = 0.003), anxiety (β = −3.60, p = 0.017) and depression (β = −5.12, p <0.001) levels decreased significantly. Furthermore, results demonstrated a significant positive association between the sense of belonging to Canada and stress (β = 2.30, p = 0.035) and anxiety (β = 2.61, p = 0.022); in another words, the lower the sense of belonging to Canada the higher the stress and anxiety levels. Also, study findings revealed a negative association between self-perceived SES and anxiety (β = −1.83, p = 0.010) and depression (β = −1.43, p = 0.029) levels. Thus, the lower Syrian parents' self-perceived SES was, the higher their anxiety and depression levels were (Table 2).
Table 2.
Adjusted multivariate regression analyses for the stress, anxiety, depression and PTSD outcomes.
| STRESS | p value | ANXIETY | p value | DEPRESSION | p value | PTSD | p value | |
|---|---|---|---|---|---|---|---|---|
| Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | |||||
| FEAR OF COVID | 0.27 (0.10) | 0.006 | 0.40 (0.10) | 0.000 | 0.32 (0.09) | 0.001 | 0.04 (0.01) | 0.015 |
| Parent | ||||||||
| Mother | ref | ref | ref | ref | ||||
| Father | 0.35 (1.64) | 0.829 | 0.40 (1.69) | 0.812 | −0.24 (1.54) | 0.876 | −0.04 (0.24) | 0.871 |
| Age | 0.02 (0.12) | 0.895 | −0.13 (0.12) | 0.288 | −0.01 (0.11) | 0.932 | 0.00 (0.02) | 0.874 |
| Working Status | ||||||||
| No | ref | ref | ref | ref | ||||
| Yes | −2.12 (1.81) | 0.243 | −1.80 (1.87) | 0.335 | −1.91 (1.71) | 0.267 | −0.07 (0.27) | 0.796 |
| Canadian language benchmark level | ||||||||
| Levels 0, 1, 2, and 3 | ref | ref | ref | ref | ||||
| Levels 4 and higher | −4.31 (1.45) | 0.003 | −3.60 (1.49) | 0.017 | −5.12 (1.37) | 0.000 | −0.24 (0.22) | 0.268 |
| Self-perceived SES# | −1.31 (0.69) | 0.057 | −1.83 (0.71) | 0.010 | −1.43 (0.65) | 0.029 | −0.17 (0.10) | 0.094 |
| Number of children | −0.43 (0.54) | 0.427 | −0.07 (0.55) | 0.903 | −0.30 (0.51) | 0.561 | 0.10 (0.08) | 0.240 |
| Lived in a refugee camp | ||||||||
| No | ref | ref | ref | ref | ||||
| Yes | 2.36 (1.97) | 0.233 | 2.25 (2.02) | 0.267 | 0.12 (1.88) | 0.950 | 0.31 (0.29) | 0.289 |
| Year of arrival to Canada | ||||||||
| 2016 or earlier | ref | ref | ref | ref | ||||
| 2017 or later | −2.20 (1.65) | 0.183 | −3.02 (1.71) | 0.079 | −2.10 (1.57) | 0.183 | 0.19 (0.25) | 0.457 |
| Satisfaction with friendships* | 0.46 (0.60) | 0.446 | 1.13 (0.62) | 0.069 | 0.55 (0.57) | 0.334 | 0.03 (0.09) | 0.701 |
| Year of data collection | ||||||||
| 2020 | ref | ref | ref | ref | ||||
| 2021 | 2.88 (2.64) | 0.278 | 4.69 (2.73) | 0.086 | 4.25 (2.52) | 0.093 | 0.54 (0.40) | 0.174 |
| Sponsorship | ||||||||
| Government assisted refugee (GAR) | ref | ref | ref | ref | ||||
| Privately sponsored refugee (PSR) | −2.36 (1.54) | 0.125 | −0.72 (1.59) | 0.653 | −1.05 (1.47) | 0.475 | −0.16 (0.23) | 0.496 |
| Other | 0.75 (2.38) | 0.752 | 2.68 (2.47) | 0.280 | 0.98 (2.27) | 0.668 | 0.71 (0.35) | 0.045 |
| Sense of belonging to Canada$ | 2.30 (1.08) | 0.035 | 2.61 (1.13) | 0.022 | 1.47 (1.03) | 0.155 | 0.29 (0.17) | 0.084 |
| R2 | 0.190 | 0.243 | 0.221 | 0.145 | ||||
Scores range from 1- low income to 5- upper income,.
Scores range from 1- very satisfied to 5- very unsatisfied,.
Scores range from 1- very strong to 4- very weak.
4. Discussion
Refugees may be among the most susceptible to the adverse mental health implications of COVID-19 (Holmes et al., 2020; Júnior et al., 2020). There is currently a scarcity of studies on the impact of the pandemic on refugees' mental health residing in Canada. In the present study, we investigated the association between fear of COVID-19 and the following mental health outcomes: stress, anxiety, depression, and PTSD among Syrian refugee parents in Canada. Our results demonstrate that a multitude of factors influence these mental health outcomes, including fear of COVID-19, language, sense of belonging and self-perceived SES.
When compared to a study examining the impact of the pandemic on physical and mental health in seven middle-income Asian countries, the present study's anxiety results (9.98, SD 11.62) were lower than Thailand's (18.66, SD 5.98), but higher than Pakistan's (8.23, SD 9.69) and Malaysia's (7.80, SD 10.95) (Wang, Tee, et al., 2021). On the other hand, the average stress (8.31, SD 10.74) and depression (7.36, SD 10.46) reported in the present study fell closer to the lower end of the range reported for Vietnam (stress: 3.80, SD 5.81; depression: 2.28, SD 5.43) and Thailand (stress: 21.94, SD 7.74; depression: 19.74, SD 6.99) (Wang et al., 2021). Furthermore, during the COVID-19 pandemic, a study conducted in Australia among Syrian and Iraqi refugees revealed higher rates of PTSD (32.9%) and depression (17.3%), as well as lower rates of anxiety (19.8%), compared to our findings (depression 12.2%, anxiety 26.8%, and stress 9.7%, 24.1% PTSD ) (Liddell et al., 2021). In a study conducted among Syrian refugees in Turkey during the COVID-19 pandemic, (Kira et al., 2021), found higher levels of PTSD (47.7%) and slightly higher levels of depression (13.9%) and anxiety (12.7%) (Kira et al., 2021). Also, another study conducted in Turkey among Syrian refugees by (Kurt et al., 2021), found higher levels of depressive (52.9%) and anxiety symptoms (42.9%) (Kurt et al., 2021) which is higher than previously reported prevalence rates in many hosting countries before the pandemic (Javanbakht et al., 2019, Poole et al., 2018, Tinghög et al., 2017, Acarturk et al., 2021, Acarturk et al., 2018).
COVID-19 fear, according to the American Psychiatric Association (APA), reflects the psychological nature of a phobia that falls within the category of anxiety disorders (APA 2013). For decades, the literature has long emphasized that fear can result in stress, distress and anxiety (Nasar and Jones, 1997; Shin and Liberzon, 2010). Findings from our study indicate that all mental health outcomes were positively associated with fear of COVID-19, such that participants with higher fear of COVID experienced higher levels of stress, anxiety, depression, and post-traumatic stress disorder. These findings are consistent with the literature that have linked fear of COVID-19 to a variety of psychological and mental health concerns, including anxiety (Harper et al., 2021), stress (Rodríguez-Hidalgo et al., 2020), depression (Voitsidis et al., 2021), and post-traumatic stress (Kira et al., 2021). Furthermore, a meta-analysis conducted by Simsir et al. 2021, demonstrated that fear of COVID-19 was strongly associated with anxiety and distress, as well as being moderately related to stress and depression (Şimşir et al., 2021).
Language may be another key stressor, according to the literature, because migrants may not fully comprehend and communicate in a foreign language when they are relocated to another country (Bhandari et al., 2021; Fabio et al., 2019). Our results show that, except for PTSD, the Canadian language benchmark level was negatively associated with all mental health outcomes. As a result, stress, anxiety, and depression levels decreased significantly as the participant's language level improved. Similarly, prior research demonstrated that migration and weak language have a negative influence on the mental health of refugees (Virupaksha et al., 2014; Steel et al., 2002). Júnior et al. 2020, found that due to constraints in accessing in-language public health services and resources, fears of COVID-19 infection may be amplified in Syrian refugees and culturally and linguistically diverse groups in general (Júnior et al., 2020). Also, previous research from the United States, Australia, and Japan has shown how linguistic difficulties prevented migrants from accessing health services and obtaining health-related information (Bhandari et al., 2021; Ilami and Winter, 2021; Ding and Hargraves, 2009).
Belonging is frequently viewed as a good quality of a person's well-being and regarded as part of a healthy state of being (Hagerty et al., 1992). Our findings revealed a significant positive relationship between a person's sense of belonging to Canada and stress and anxiety measures, with the lower one's sense of belonging to Canada, the higher one's stress and anxiety levels. This finding concurs with a Canadian study that investigated the factors that influence positive mental health among refugees and discovered that a sense of belonging to Canada was a significant predictor of mental health (Beiser and Hou, 2017). A recent study conducted by Fuchs et al. 2021, found that the Challenged Sense of Belonging Scale scores were positively associated with better mental health in the three languages of English, Arabic, and Farsi, implying that a less challenged sense of belonging is linked to better mental health (Fuchs et al., 2021).
Finally, study findings revealed a negative association between self-perceived SES and anxiety and depression levels among the study participants. Our findings are in line with a systematic review conducted by Bogic et al. 2015, which discovered a positive association between post-migration SES and depression (Bogic et al., 2015). Besides, research studies found a positive univariate association between these socio-demographic factors and unspecified anxiety disorder (Gerritsen et al., 2006; Marshall et al., 2005; Bogic et al., 2012), but these associations mostly disappeared in multivariate analyses, leaving the relationships either as indeterminate or with no association.
The study has several limitations that must be considered. First, given the cross-sectional nature of the study design, one of the limitations involve the direction of causality between fear of COVID-19 and the associated DASS-21 and PC-PTSD variables. Second, the results are subject to confounding biases such as the participants’ mental health status prior to the onset of COVID-19, perceived risk of being infected by COVID-19, coping abilities, resilience, lockdown stressors, grief of lost ones, and vaccination status at time of interview. Third, as participation in this study was voluntary, there is the possibility for selection bias. Fourth, because self-reports were utilized to measure participants' responses and the 4-item PC-PTSD scale was employed rather than the updated 5-item PTSD screening tool, the study may be subject to information bias (Prins et al., 2003). Lastly, this study did not assess suicidal thoughts during the pandemic. Suicide mortality rate decreased in Canada during the first year of the COVID-19 pandemic (McIntyre et al., 2021).
5. Conclusion
Our research has important policy implications, and the findings could aid in the development of more effective interventions tailored at alleviating mental health issues among Syrian refugee parents in Canada. Government initiatives should consider tackling fear around pandemics among this population to help enhance their mental well-being. Our findings suggest that programs that teach new immigrants languages and bolster their sense of belonging to Canada will highly benefit their mental health of new immigrants. Moreover, learning a country's language will increase the likelihood of new immigrants finding jobs (National Immigration Forum 2017), which in turn enhances their SES, which was found to be significantly positively associated with symptoms of anxiety and depression in our study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by the Social Sciences and Humanities Research Council of Canada [Application number 435–2018–1109].
Contributor Information
Reem Hoteit, Email: rah84@mail.aub.edu.
Christo El Morr, Email: elmorr@yorku.ca.
Hala Tamim, Email: htamim@yorku.ca.
References
- Åkesson P., Chen A.F., Deirmengian G.K., Geary M., Quevedo M.S., Sousa R., Springer B.D., Wang Q. General assembly, prevention, risk mitigation, local factors: proceedings of international consensus on orthopedic infections. J. Arthroplasty. 2019;34:S49–S53. doi: 10.1016/j.arth.2018.09.053. [DOI] [PubMed] [Google Scholar]
- Acarturk C., Cetinkaya M., Senay I., Gulen B., Aker T., and Hinton D., Prevalence andpredictors of posttraumatic stress and depression symptoms among Syrian refugees in arefugee camp, The Journal of nervous and mental disease. 206 (2018) 40-45. 10.1097/NMD.0000000000000693. [DOI] [PubMed]
- Acarturk C., McGrath M., Roberts B., Ilkkursun Z., Cuijpers P., Sijbrandij M., Sondorp E., Ventevogel P., McKee M., and Fuhr D.C., Prevalence and predictors ofcommon mental disorders among Syrian refugees in Istanbul, Turkey: a cross-sectionalstudy, Social psychiatry and psychiatric epidemiology. 56 (2021) 475-484. 10.1007/s00127-020-01941-6. [DOI] [PubMed]
- Ahmad F., Othman N., Hynie M., Bayoumi A.M., Oda A., McKenzie K. Depression-level symptoms among Syrian refugees: findings from a Canadian longitudinal study. J. Ment. Health. 2021;30:246–254. doi: 10.1080/09638237.2020.1765998. [DOI] [PubMed] [Google Scholar]
- Ahmed A., Bowen A., Feng C.X. Maternal depression in Syrian refugee women recently moved to Canada: a preliminary study. BMC Pregn. Childb. 2017;17:1–11. doi: 10.1186/s12884-017-1433-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.-.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alyami M., Henning M., Krägeloh C.U., Alyami H. Psychometric evaluation of the Arabic version of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 2021;19:2219–2232. doi: 10.1007/s11469-020-00316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA American psychiatric association explains DSM-5. BMJ. 2013;346 doi: 10.1136/bmj.f3591. [DOI] [PubMed] [Google Scholar]
- Beiser M., Hou F. Predictors of positive mental health among refugees: Results from Canada’s General Social Survey. Transcult. Psychiatry. 2017;54:675–695. doi: 10.1177/1363461517724985. [DOI] [PubMed] [Google Scholar]
- Bhandari D., Kotera Y., Ozaki A., Abeysinghe S., Kosaka M., Tanimoto T. COVID-19: challenges faced by Nepalese migrants living in Japan. BMC Public Health. 2021;21:1–14. doi: 10.1186/s12889-021-10796-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogic M., Ajdukovic D., Bremner S., Franciskovic T., Galeazzi G.M., Kucukalic A., Lecic-Tosevski D., Morina N., Popovski M., Schützwohl M. Factors associated with mental disorders in long-settled war refugees: refugees from the former Yugoslavia in Germany, Italy and the UK. Br. J. Psychiatry. 2012;200:216–223. doi: 10.1192/bjp.bp.110.084764. [DOI] [PubMed] [Google Scholar]
- Bogic M., Njoku A., Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int. Health Hum. Rights. 2015;15:1–41. doi: 10.1186/s12914-015-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantekin D., Gençöz T. Mental health of Syrian asylum seekers in Turkey: The role of pre-migration and post-migration risk factors. J. Soc. Clin. Psychol. 2017;36:835–859. doi: 10.1521/jscp.2017.36.10.835. [DOI] [Google Scholar]
- Clarke S.K., Kumar G.S., Sutton J., Atem J., Banerji A., Brindamour M., Geltman P., Zaaeed N. Potential impact of COVID-19 on recently resettled refugee populations in the United States and Canada: perspectives of refugee healthcare providers. J. Immig. Minor. Health. 2021;23:184–189. doi: 10.1007/s10903-020-01104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz M.P., Santos E., Cervantes M.V., Juárez M.L. COVID-19, a worldwide public health emergency. Revista Clínica Española (English Edition) 2021;221:55–61. doi: 10.1016/j.rceng.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding H., Hargraves L. Stress-associated poor health among adult immigrants with a language barrier in the United States. J. Immigr. Minor. Health. 2009;11:446. doi: 10.1007/s10903-008-9200-0. [DOI] [PubMed] [Google Scholar]
- Fabio M., Parker L.D., Siddharth M.B. Building on resiliencies of refugee families. Pediatr. Clin. N. Am. 2019;66:655–667. doi: 10.1016/j.pcl.2019.02.011. [DOI] [PubMed] [Google Scholar]
- Filler T., Georgiades K., Khanlou N., Wahoush O. Understanding mental health and identity from Syrian refugee adolescents’ perspectives. Int. J. Ment. Health Addict. 2021;19:764–777. doi: 10.1007/s11469-019-00185-z. [DOI] [Google Scholar]
- Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: The State of America’s mental health. J. Anxiety Disord. 2020;75 doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs L.M., Jacobsen J., Walther L., Hahn E., Ta T.M.T., Bajbouj M., von Scheve C. The Challenged Sense of Belonging Scale (CSBS)—A validation study in English, Arabic, and Farsi/Dari among refugees and asylum seekers in Germany. Measure. Instru. Soc. Sci. 2021;3:1–16. doi: 10.1186/s42409-021-00021-y. [DOI] [Google Scholar]
- GC. Coronavirus disease (COVID-19): Outbreak update. Government of Canada. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html, 2021 (accessed 17 Novemeber, 2021).
- GC. WelcomeRefugees: Key figures. Government of Canada. https://www.canada.ca/en/immigration-refugees-citizenship/services/refugees/welcome-syrian-refugees/key-figures.html, 2021 (accessed 17 November, 2021).
- Gerritsen A.A., Bramsen I., Devillé W., van Willigen L.H., Hovens J.E., Van Der Ploeg H.M. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc. Psychiatry Psychiatr. Epidemiol. 2006;41:18–26. doi: 10.1007/s00127-005-0003-5. [DOI] [PubMed] [Google Scholar]
- Gullone E. The development of normal fear: A century of research. Clin. Psychol. Rev. 2000;20:429–451. doi: 10.1016/S0272-7358(99)00034-3. [DOI] [PubMed] [Google Scholar]
- Hadfield K., Ostrowski A., Ungar M. What can we expect of the mental health and well-being of Syrian refugee children and adolescents in Canada? Can. Psychol./psychologie canadienne. 2017;58:194. https://psycnet.apa.org/doi/10.1037/cap0000102 [Google Scholar]
- Hagerty B.M., Lynch-Sauer J., Patusky K.L., Bouwsema M., Collier P. Sense of belonging: A vital mental health concept. Arch. Psychiatr. Nurs. 1992;6:172–177. doi: 10.1016/0883-9417(92)90028-H. [DOI] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2021;19:1875–1888. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilami A., Winter S. iranian migrants’ lived experiences of access to sexual and reproductive healthcare services in western australia: a conventional content analysis. Sexual. Res. Soc. Policy. 2021;18:533–546. doi: 10.1007/s13178-020-00478-2. [DOI] [Google Scholar]
- Júnior J.G., de Sales J.P., Moreira M.M., Pinheiro W.R., Lima C.K.T., Neto M.L.R. A crisis within the crisis: The mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javanbakht A., Amirsadri A., Suhaiban H.A., Alsaud M.I., Alobaidi Z., Rawi Z., Arfken C.L. Prevalence of possible mental disorders in Syrian refugees resettling in theUnited States screened at primary care. Journal of immigrant and minority health. 2019;21:664–667. doi: 10.1007/s10903-018-0797-3. [DOI] [PubMed] [Google Scholar]
- Khamis V. Psychological distress and neuroticism among Syrian refugee parents in post-resettlement contexts. J. Health Psychol. 2021 doi: 10.1177/1359105320988321. [DOI] [PubMed] [Google Scholar]
- Kira I.A., Shuwiekh H.A., Rice K.G., Ashby J.S., Elwakeel S.A., Sous M.S.F., Alhuwailah A., Baali S.B.A., Azdaou C., Oliemat E.M. Measuring COVID-19 as traumatic stress: Initial psychometrics and validation. J. Loss Trauma. 2021;26:220–237. doi: 10.1080/15325024.2020.1790160. [DOI] [Google Scholar]
- Kira I.A., Alpay E.H., Turkeli A., Shuwiekh H.A., Ashby J.S., Alhuwailah A. Theeffects of COVID-19 traumatic stress on executive functions: The case of Syrian refugeesin Turkey. Journal of Loss and Trauma. 2021:1–21. doi: 10.1080/15325024.2020.1869444. [DOI] [Google Scholar]
- Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. The Lancet Resp. Med. 2020;8:547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer L.J., Narasiah L., Munoz M., Rashid M., Ryder A.G., Guzder J., Hassan G., Rousseau C., Pottie K. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183:E959–E967. doi: 10.1503/cmaj.090292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurt G., Ilkkursun Z., Javanbakht A., Uygun E., Karaoglan-Kahilogullari A., C.Acarturk The psychological impacts of COVID-19 related stressors on Syrian refugeesin Turkey: The role of resource loss, discrimination, and social support. InternationalJournal of Intercultural Relations. 2021;85:130–140. doi: 10.1016/j.ijintrel.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddell B.J., O’Donnell M., Bryant R.A., Murphy S., Byrow Y., Mau V., McMahon T., Benson G., Nickerson A. The association between COVID-19 related stressors andmental health in refugees living in Australia. European journal of. 2021;12:1947564. doi: 10.1080/20008198.2021.1947564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. Psychology Foundation; Sydney, New South Wales: Australia: 1995. Manual For the Depression Anxiety Stress. [Google Scholar]
- Lupieri S. Refugee health during the Covid-19 pandemic: a review of global policy responses. Risk Management and Healthcare Policy. 2021;14:1373. doi: 10.2147/RMHP.S259680. [Online]. Available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall G.N., Schell T.L., Elliott M.N., Berthold S.M., Chun C.-.A. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005;294:571–579. doi: 10.1001/jama.294.5.571. [DOI] [PubMed] [Google Scholar]
- McIntyre R.S., Lui L.M., Rosenblat J.D., Ho R., Gill H., Mansur R.B., Teopiz K., Liao Y., Lu C., and Subramaniapillai M., Suicide reduction in Canada during the COVID-19pandemic: lessons informing national prevention strategies for suicide reduction, Journalof the Royal Society of Medicine. 114 (2021) 473-479. 10.1177/01410768211043186. [DOI] [PMC free article] [PubMed]
- Miller A., Hess J.M., Bybee D., Goodkind J.R. Understanding the mental health consequences of family separation for refugees: Implications for policy and practice. Am. J. Orthopsychiatry. 2018;88:26. doi: 10.1037/ort0000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussa M.T., Lovibond P., Laube R., Megahead H.A. Psychometric properties of an arabic version of the depression anxiety stress scales (DASS) Res. Soc. Work Pract. 2017;27:375–386. doi: 10.1177/1049731516662916. [DOI] [Google Scholar]
- Nasar J.L., Jones K.M. Landscapes of fear and stress. Environ. Behav. 1997;29:291–323. doi: 10.1177/001391659702900301. [DOI] [Google Scholar]
- National Immigration Forum. English language programs help immigrants prepare for jobs. https://immigrationforum.org/article/english-language-programs-help-immigrants-prepare-jobs/, 2017 (accessed November 26, 2021).
- Ornelas I.J., Tornberg-Belanger S., Balkus J.E., Bravo P., Perez Solorio S.A., Perez G.E., Tran A.N. Coping with COVID-19: the impact of the pandemic on latina immigrant women’s mental health and well-being. Health Educ. Behav. 2021;48:733–738. doi: 10.1177/10901981211050638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. Pandemic fear” and COVID-19: mental health burden and strategies. Brazil. J. Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PHAC COVID-19 vaccination in Canada. Public Health Agency of Canada. 2021 https://health-infobase.canada.ca/covid-19/vaccine-administration/ (accessed 17 November, 2021) [Google Scholar]
- Poole D.N., Hedt-Gauthier B., Liao S., Raymond N.A., Bärnighausen T. Majordepressive disorder prevalence and risk factors among Syrian asylum seekers in Greece,BMC. public health. 2018;18:1–9. doi: 10.1186/s12889-018-5822-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Cameron R.P., Hugelshofer D.S., Shaw-Hegwer J., Thrailkill A., Gusman F.D., Sheikh J.I. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim. Care Psychiatry. 2003;9:9–14. https://www.ptsd.va.gov/PTSD/professional/articles/article-pdf/id26676.pdf [Online]. Available. [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Hidalgo A.J., Pantaleón Y., Dios I., Falla D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front. Psychol. 2020;11:3041. doi: 10.3389/fpsyg.2020.591797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg J., Leung J.K., Harris K., Abdullah A., Rohbar A., Brown C., Rosenthal M.S. Recently-arrived Afghan refugee parents’ perspectives about parenting, education and pediatric medical and mental health care services. J. Immigr. Minor. Health. 2021:1–8. doi: 10.1007/s10903-021-01206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020;74:281. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin L.M., Liberzon I. The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology. 2010;35:169–191. doi: 10.1038/npp.2009.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z., Silove D., Phan T., Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: a population-based study. Lancet North Am. Ed. 2002;360:1056–1062. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- Şimşir Z., Koç H., Seki T., Griffiths M.D. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. 2021:1–9. doi: 10.1080/07481187.2021.1889097. [DOI] [PubMed] [Google Scholar]
- Tee M.L., Tee C.A., Anlacan J.P., Aligam K.J.G., Reyes P.W.C., Kuruchittham V., Ho R.C. Psychological impact of COVID-19 pandemic in the Philippines. Journalof affective disorders. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinghög P., Malm A., Arwidson C., Sigvardsdotter E., Lundin A. Saboonchi,Prevalence of mental ill health, traumas and postmigration stress among refugees fromSyria resettled in Sweden after 2011: a population-based survey. BMJ open. 2017;7 doi: 10.1136/bmjopen-2017-018899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop. Med. Int. Health. 2020;25:278. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virupaksha H., Kumar A., Nirmala B.P. Migration and mental health: An interface. J. Natur. Sci. Biol. Med. 2014;5:233. doi: 10.4103/0976-9668.136141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voitsidis P., Nikopoulou V.A., Holeva V., Parlapani E., Sereslis K., Tsipropoulou V., Karamouzi P., Giazkoulidou A., Tsopaneli N., Diakogiannis I. The mediating role of fear of COVID-19 in the relationship between intolerance of uncertainty and depression. Psychol. Psychother. Theo. Res. Pract. 2021;94:884–893. doi: 10.1111/papt.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupała A., Grabowski D., Pan R., Adamus K., Wan X., Hetnał M., Tan Y., Olszewska-Guizzo A., and Xu L., The association between physical and mentalhealth and face mask use during the COVID-19 pandemic: a comparison of two countrieswith different views and practices, Frontiers in psychiatry. 11 (2020) 901. 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed]
- Wang C., Chudzicka-Czupała A., Tee M.L., Núñez M.I.L., Tripp C., Fardin M.A., Habib H.A., Tran B.X., Adamus K., Anlacan J. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans. Asians and Europeans,Scientific reports. 2021;11:1–12. doi: 10.1038/s41598-021-85943-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Fardin M.A., Shirazi M., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., B.Tran, Quek T.T. Mental Health of the General Population during the 2019Coronavirus Disease (COVID-19) Pandemic: A Tale of Two Developing Countries,Psychiatry. International. 2021;2:71–84. doi: 10.3390/psychiatryint2010006. [DOI] [Google Scholar]
- Wang C., Tripp C., Sears S.F., Xu L., Tan Y., Zhou D., Ma W., Xu Z., Chan N.A., Ho andC. The impact of the COVID-19 pandemic on physical and mental health in the twolargest economies in the world: a comparison between the United States and. China,Journal of behavioral medicine. 2021:1–19. doi: 10.1007/s10865-021-00237-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Tee M., Roy A.E., Fardin M.A., Srichokchatchawan W., Habib H.A., X.Tran B., Hussain S., Hoang M.T., Le X.T. The impact of COVID-19 pandemic onphysical and mental health of Asians: A study of seven middle-income countries in. Asia,PloS one. 2021;16 doi: 10.1371/journal.pone.0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren A.M., Zolfaghari K., Fresnedo M., Bennett M., Pogue J., Waddimba A., Zvolensky M., Carlbring P., Powers M.B. Anxiety sensitivity, COVID-19 fear, and mental health: results from a United States population sample. Cogn. Behav. Ther. 2021;50:204–216. doi: 10.1080/16506073.2021.1874505. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2021. WHO Coronavirus (COVID-19) Dashboard.https://covid19.who.int/ (accessed 17 November, 2021) [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., Chen-Li D., Iacobucci M., R.Ho, Majeed A. Impact of COVID-19 pandemic on mental health in the generalpopulation: A systematic review. Journal of affective disorders. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]