Abstract
Background
The knowledge of risk perceptions in primary care could help health authorities to manage epidemics.
Methods
A European multi-center cross-sectional study was conducted in France, Belgium and Spain to describe the perceptions, the level of anxiety and the feeling of preparedness of primary healthcare physicians towards the COVID-19 infection at the beginning of the pandemic. The factors associated with the feeling of preparedness were studied using multivariate logistic regressions.
Results
A total of 511 physicians participated to the study (response rate: 35.2%). Among them, only 16.3% (n=82) were highly anxious about the pandemic, 50.6% (n=254) had the feeling to have a high level of information, 80.5% (n=409) found the measures taken by the health authorities suitable to limit the spread of COVID-19, and 45.2% (n=229) felt prepared to face the epidemic. Factors associated with feeling prepared were: being a Spanish practitioner (adjusted OR=4.34; 95%CI [2.47; 7.80]), being a man (aOR=2.57, 95%CI [1.69; 3.96]), finding the measures taken by authorities appropriate (aOR=1.72, 95%CI [1.01; 3.00]) and being highly informed (aOR=4.82, 95%CI [2.62; 9.19]).
Conclusions
Regarding the dramatic evolution of the pandemic in Europe in the weeks following the study, it appears that information available at this time and transmitted to the physicians could have given a wrong assessment of the spread and the severity of the disease. It seems essential to better integrate the primary care physicians into the information, training and protection channels. A comparison between countries could help to select the most effective measures in terms of information and communication.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-021-01588-5.
Keywords: Primary Health Care, COVID-19, Pandemic, Anxiety, Health information, Management, Sentinel Surveillance
Background
At the end of 2019, a new coronavirus (SARS-CoV-2), causing respiratory infections (COVID-19), emerged in China and further spread worldwide [1]. The number of reported cases increased steadily in Europe at the beginning of March 2020 [2], generating fears and anxiety among the general population and health care workers [3–5].
Previous health crisis due to coronaviruses (SARS in 2002/2003, MERS-CoV in 2012), or other infectious diseases (H1N1 pandemic influenza in 2009, Ebola in 2014) have shown the importance of collecting feedback of healthcare professionals [6–8]. Indeed, knowledge of primary healthcare professionals’ perceptions and behavior represents an essential tool for health authorities to implement control measures and communication campaigns [9]. Knowing perceptions and behavior at the beginning of the pandemic is particularly relevant as it enables health authorities to adapt and specifically target their actions.
Here we describe the perceptions, anxiety and feeling of preparedness of primary healthcare physicians towards the COVID-19 infection at the beginning of the pandemic in Europe, in three European countries: Belgium, France, and Spain.
Methods
Design and study population
A cross-sectional study was carried out in February-March 2020 among all the primary care physicians involved in European sentinel surveillance networks: “Sciensano” (Belgium), “Réseau Sentinelles” (France), and “Red Centinela Sanitaria” (Castile and León, Spain). The participants included were general practitioners (GPs) and pediatricians (only in Spain). Physicians were invited to participate in the study on a voluntary basis. The representativeness of Belgian, French and Spanish sentinel physicians has been previously studied [10–12].
Data collection and study period
The questionnaire was built according to the literature [13, 14], and was validated by a panel of experts: members of the French national public health agency (i.e. Santé publique France), epidemiologists and biostatisticians, a general practitioner and a sociologist. The survey included 24 questions and addressed topics on (i) anxiety due to the ongoing pandemic (from the physician and the patient perspectives), (ii) practices’ changes (probability of seeing infected patients, repercussions on the consultations’ organization, anticipated preparation measures), (iii) information received from health authorities (regarding the COVID-19 epidemic in China, the risk for the local population, the case definition, the management of suspected cases), and (iv) feeling of preparedness. The detailed questionnaire is available in a supplementary file (see Additional file 1). To characterize healthcare professionals, demographic characteristics were collected: age, gender and the practice area. Physician practice area was defined according to the physician’s views of his or her practice as “urban”, “suburban” or “rural” (recoded as “urban” vs. “rural”). Some other variables were recoded in order to facilitate the analyses and the presentation of the results. The level of anxiety and the probability of seeing infected patients were measured by a scale from 0 (no anxiety) to 10 (major anxiety), and classified into low (≤2), moderate (3 to 6) and high (≥7). Variables with the following modalities: “Not at all”, “Not really”, “Yes, moderately” and “Yes, absolutely” were made as binary variables, with “Not at all” for “No” and the three other options for “Yes”. The level of information about the pandemic was evaluated through a score based on the perceived knowledge about four topics: the epidemic situation in China, the risk for the local population, the case definition and the management of suspected cases. Physicians were considered as poorly (n<2 topics), moderately (n=2-3) or highly (n=4) informed. Electronic surveys were built on LymeSurvey. An email with a link to the survey was sent to the physicians of the three sentinel networks, and a reminder was sent after one week. Electronic surveys were available from 14 to 27 February 2020 in France, from 19 to 28 February 2020 in Belgium and from 20 February to 2 March 2020 in Spain.
Statistical analyses
Pearson’s chi-squared test and Fisher’s exact test were used for estimating the p-value of qualitative variables, and Kruskal-Wallis rank sum test for quantitative ones. The factors associated with the feeling of preparedness were studied using univariate and multivariate logistic regressions. The multivariate analysis was performed using a backward elimination procedure until all variables reached statistical significance (p≤0.05). Statistical analyses were performed using the R software version 3.5.0 [15].
Ethics approval
This study was conducted in agreement with country-specific regulations on privacy and data collection and treatment. In addition, approvals by Ethical Review Boards or Committees were obtained when needed according to the country-specific regulations.
Results
Perception and preparedness of primary care physicians at the beginning of the COVID-19 pandemic
The electronic survey was filled by 35.2% (511/1450) of the investigated healthcare practitioners. Participating physicians were distributed as followed: 12.1% (n=62) from Belgium, 67.1% (n=343) from France and 20.8% (n=106) from Spain. Men represented 57.4% (n=292), median age was 56 years (IQR [42; 62]), and 70.7% (n=359) were working in urban areas (Table 1).
Table 1.
Characteristics of primary care physicians by country
| Total N (%) N=511 |
Belgium N (%) N=62 |
France N (%) N=343 |
Spain N (%) N=106 |
p-value | |
|---|---|---|---|---|---|
| Participation | |||||
| Targeted physicians | 1450 | 98 | 1224 | 128 | |
| Respondents | 511 (35.2%) | 62 (63.3%) | 343 (28.0%) | 106 (82.8%) | |
| Type of physicians (m.d.=0) | |||||
| General Practitioners | 491 (96.1%) | 62 (100%) | 343 (100%) | 86 (81.1%) | |
| Pediatricians | 20 (3.9%) | 0 | 0 | 20 (18.9%) | |
| Sex (m.d.=2) | |||||
| Female | 217 (42.6%) | 26 (41.9%) | 131 (38.2%) | 60 (57.7%) | <10−2 |
| Male | 292 (57.4%) | 36 (58.1%) | 212 (61.8%) | 44 (42.3%) | |
| Age (years) (m.d.=9) | |||||
| 25-39 | 106 (21.1%) | 3 (4.8%) | 100 (29.9%) | 3 (2.9%) | <10−5 |
| 40-54 | 114 (22.7%) | 9 (14.5%) | 84 (25.1%) | 21 (20%) | |
| ≥ 55 | 282 (56.2%) | 50 (80.6%) | 151 (45.1%) | 81 (77.1%) | |
| Median (IQR) | 56 (42; 62) | 61 (56; 65) | 52 (37; 60) | 60 (55; 62) | <10−5 |
| Practice area (m.d.=3) | |||||
| Rural | 149 (29.3%) | 22 (35.5%) | 79 (23%) | 48 (46.6%) | <10−4 |
| Urban | 359 (70.7%) | 40 (64.5%) | 264 (77%) | 55 (53.4%) | |
| Physicians’ anxiety (m.d.=7) | |||||
| Low anxiety feeling | 176 (34.9%) | 24 (38.7%) | 140 (41.3%) | 12 (11.7%) | <10−5 |
| Moderate anxiety feeling | 246 (48.8%) | 28 (45.2%) | 164 (48.4%) | 54 (52.4%) | |
| High anxiety feeling | 82 (16.3%) | 10 (16.1%) | 35 (10.3%) | 37 (35.9%) | |
| Median (IQR) | 4 (2; 6) | 3 (2; 6) | 3 (2; 5) | 6 (4; 7) | <10−5 |
| Patients’ anxiety (m.d.=4) | |||||
| Low anxiety feeling | 107 (21.1%) | 13 (21%) | 73 (21.3%) | 21 (20.4%) | 0.85 |
| Moderate anxiety feeling | 286 (56.4%) | 38 (61.3%) | 188 (55%) | 60 (58.3%) | |
| High anxiety feeling | 114 (22.5%) | 11 (17.7%) | 81 (23.7%) | 22 (21.4%) | |
| Median (IQR) | 4 (3; 6) | 5 (3; 6) | 5 (3; 6) | 4 (3; 6) | 0.89 |
| Risk of seeing infected patients in the next 2 weeks (m.d.=3) | |||||
| Low risk | 400 (78.7%) | 46 (74.2%) | 295 (86%) | 59 (57.3%) | <10−5 |
| Moderate risk | 97 (19.1%) | 15 (24.2%) | 46 (13.4%) | 36 (35%) | |
| High risk | 11 (2.2%) | 1 (1.6%) | 2 (0.6%) | 8 (7.8%) | |
| Median (IQR) | 1 (0; 2) | 1 (1; 3) | 1 (0; 2) | 2 (1; 5) | <10−5 |
| Finding the measures taken by the health authorities suitable to limit the spread of COVID-19 (m.d.=3) | 409 (80.5%) | 51 (82.3%) | 275 (80.2%) | 83 (80.6%) | 0.93 |
| Changes in professional practices (m.d.=4) | 207 (40.8%) | 30 (48.4%) | 124 (36.3%) | 53 (51.5%) | <10−2 |
| Impact on consultations (m.d.=3) | 72 (14.2%) | 8 (12.9%) | 39 (11.4%) | 25 (24.3%) | <10−2 |
| Types of consequences (m.d.=5) | |||||
| Questions about any links with China during consultations | 44 (61.1%) | 4 (50%) | 19 (48.7%) | 21 (84%) | |
| Increased consultation time due to question about COVID-19 | 22 (30.6%) | 1 (12.5%) | 14 (35.9%) | 7 (28%) | |
| Specific consultations for information on COVID-19 | 6 (8.3%) | 0 | 1 (2.6%) | 5 (20%) | |
| Phone calls on COVID-19 | 6 (8.3%) | 2 (25%) | 3 (7.7%) | 1 (4%) | |
| Consultations of patients who thought they had contracted COVID-19 | 6 (8.3%) | 1 (12.5%) | 4 (10.3%) | 1 (4%) | |
| Anticipation of the epidemic arrival (m.d.=3) | 337 (66.3%) | 40 (64.5%) | 200 (58.3%) | 97 (94.2%) | <10−5 |
| Types of anticipation measures (m.d. =32) | |||||
| Search of guidelines | 205 (60.8%) | 33 (82.5%) | 113 (56.5%) | 59 (60.8%) | |
| Purchase of protection equipment | 122 (36.2%) | 4 (10%) | 63 (31.5%) | 55 (56.7%) | |
| Re-use of the influenza pandemic kits | 106 (35.7%) | N.A. | 80 (40%) | 26 (26.8%) | |
| Office reorganization to avoid patients’ influx | 60 (17.8%) | 9 (22.5%) | 34 (17%) | 17 (17.5%) | |
| Other measures | 13 (3.9%) | 1 (2.5%) | 9 (4.5%) | 3 (3.1%) | |
| Level of information regarding the epidemic (m.d.=9) | |||||
| Low information level | 80 (16.3%) | 6 (9.6%) | 59 (17.5%) | 15 (14.6%) | 0.05 |
| Moderate information level | 168 (33.5%) | 14 (22.6%) | 120 (35.6%) | 34 (33,0%) | |
| High information level | 254 (50.6%) | 42 (67.7%) | 158 (46.9%) | 54 (52.4%) | |
| Feeling prepared to face the epidemic (m.d.=4) | 229 (45.2%) | 28 (45.2%) | 139 (40.6%) | 62 (60.2%) | <10−2 |
m.d.: missing data; IQR: interquartile range; N.A.: not available
No differences in sex, age or location of sentinel professionals were observed for Belgium and Spain between respondents and non-respondents. In France, the GPs who participated in the study were slightly younger compared to the French GPs (mean age of 50 vs. 53 years old respectively, p-value <10−3) and less urban (77% vs. 86% respectively, p-value <10−3). However, there was no difference in sex ratio (62% of men in the study vs. 59% among the French GPs, p-value=0.37).
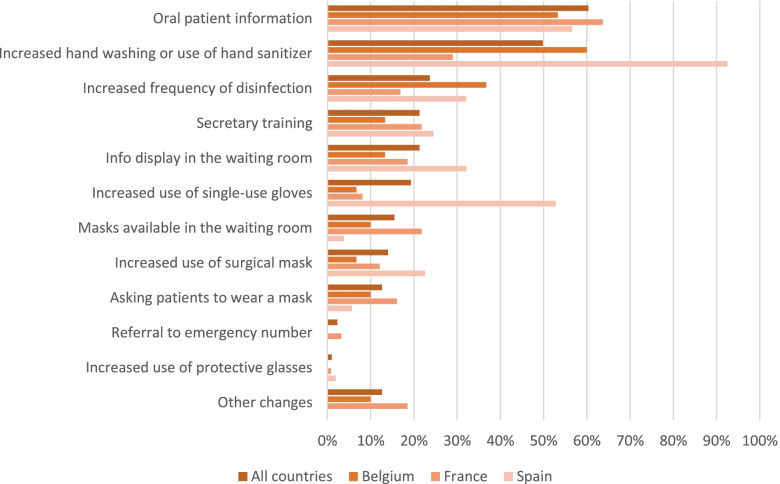
Only 16.3% of physicians (n=82) and 22.5% (n=114) of patients were highly worried about the COVID-19 pandemic. The physicians were 80.5% (n=409) to find the measures taken by the health authorities appropriate to control its spread, and 40.8% (n=207) had made changes in their professional practices (Table 1). The most frequent changes were “increased oral information given to patients about COVID-19” (60.4%, n=125), “increased handwashing or hand sanitizing” (49.8%, n=103), and “increased frequency of disinfection” (23.7%, n=49) (Fig. 1). Physicians reported impacts on their consultations (like an increase in time) for 14.2% of them (n=72), and 66.3% (n=337) had started anticipating the epidemic arrival. The main anticipation measures were the research of action guidelines (60.8%, n=205) and the purchase of protection equipment (36.2%, n=122).
Fig. 1.
Professional changes by country at the beginning of the COVID-19 pandemic
Half of the physicians (50.6%, n=254) felt they received clear information from health authorities overall. For 90.6% (n=454), the main source of information consisted of emails sent by health authorities (Fig. 2).
Fig. 2.
Source of information by country when facing a suspected case of COVID-19
Factors associated with preparedness
Less than half of primary care physicians (45.2%, n=229) felt prepared for the epidemic arrival, ranging from 40.6% (139/342) in France to 60.2% (62/103) in Spain. Factors positively associated with feeling prepared were: being a Spanish practitioner (adjusted OR=4.34; 95%CI [2.47; 7.80]), being a man (aOR=2.57, 95%CI [1.69; 3.96]), finding the measures taken by authorities appropriate (aOR=1.72, 95%CI [1.01; 3.00]) and being highly informed (aOR=4.82, 95%CI [2.62; 9.19]). Factors negatively associated were: being moderately (aOR=0.34; 95%CI [0.21; 0.53]) or highly worried (aOR=0.27; 95%CI [0.14; 0.52]) (Table 2).
Table 2.
Factors associated with the feeling of preparedness among primary care physicians (univariate and multivariate analyses)
| n | Feeling prepared | OR [95% CI] Univariate analysis |
p-value | OR [95% CI] Multivariate analysis |
p-value | ||
|---|---|---|---|---|---|---|---|
| Age | 25-39 | 105 | 43 (41.0%) | Ref. | 0.01 | ||
| 40-54 | 114 | 39 (34.2%) | 0.76 [0.44;1.32] | ||||
| ≥ 55 | 278 | 142 (51.1%) | 1.53 [0.97;2.42] | ||||
| Country | France | 342 | 139 (40.6%) | Ref. | 0.01 | Ref. | <10−5 |
| Belgium | 62 | 28 (45.2%) | 1.2 [0.69;2.07] | 0.94 [0.5;1.75] | |||
| Spain | 103 | 62 (60.2%) | 2.21 [1.41;3.48] | 4.34 [2.47;7.8] | |||
| Sex | Female | 216 | 78 (36.1%) | Ref. | 0.001 | Ref. | <10−4 |
| Male | 291 | 151 (51.9%) | 1.91 [1.33;2.74] | 2.57 [1.69;3.96] | |||
| Type of practice area | Rural | 149 | 69 (46.3%) | Ref. | 0.74 | ||
| Urban | 358 | 160 (44.7%) | 0.94 [0.64;1.38] | ||||
| Physicians’ anxiety | Low | 176 | 104 (59.1%) | Ref. | <10−4 | Ref. | <10−5 |
| Moderate | 245 | 93 (38.0%) | 0.42 [0.28;0.63] | 0.34 [0.21;0.53] | |||
| High | 82 | 31 (37.8%) | 0.42 [0.24;0.72] | 0.27 [0.14;0.52] | |||
| Patients’ anxiety | Low | 107 | 54 (50.5%) | Ref. | 0.46 | ||
| Moderate | 285 | 126 (44.2%) | 0.78 [0.5;1.21] | ||||
| High | 114 | 49 (43.0%) | 0.74 [0.43;1.26] | ||||
| Risk of seeing infected patients in the next 2 weeks | Low | 399 | 186 (46.6%) | Ref. | 0.03 | ||
| Moderate | 97 | 35 (36.1%) | 0.65 [0.41;1.02] | ||||
| High | 11 | 8 (72.7%) | 3.05 [0.87;14.1] | ||||
| Practice changes | No | 300 | 131 (43.7%) | Ref. | 0.39 | ||
| Yes | 206 | 98 (47.6%) | 1.17 [0.82;1.67] | ||||
| Impact on consultations | No | 435 | 191 (43.9%) | Ref. | 0.16 | ||
| Yes | 72 | 38 (52.8%) | 1.43 [0.87;2.36] | ||||
| Feeling response measures appropriate | No | 99 | 32 (32.3%) | Ref. | 0.01 | Ref. | 0.05 |
| Yes | 408 | 197 (48.3%) | 1.95 [1.24;3.14] | 1.72 [1.01;3] | |||
| Level of information | Low | 80 | 21 (26.2%) | Ref. | < 10−5 | Ref. | < 10−5 |
| Moderate | 167 | 46 (27.5%) | 1.07 [0.59;1.98] | 1.02 [0.54;2] | |||
| High | 254 | 161 (63.4%) | 4.86 [2.82;8.67] | 4.82 [2.62;9.19] | |||
| Anticipation | No | 171 | 84 (49.1%) | Ref. | 0.20 | ||
| Yes | 336 | 145 (43.2%) | 0.79 [0.54;1.14] | ||||
Discussion
This study enabled to identify the initial risk perceptions and the feeling of preparedness among primary care physicians from Belgium, France, and Spain when COVID-19 pandemic emerged in Europe and when only isolated cases were observed in those three countries.
At the beginning of the COVID-19 pandemic, between mid-February and the beginning of March 2020, the majority of primary care physicians investigated were little to moderately worried about the disease. As suggested by the results of the study, this could be explained by a low perceived risk of handling infected patients, the feeling to be well-informed and the trust in health authorities’ ability to implement appropriate measures to limit the spread of the disease. Moreover, as the pandemic was still emerging in Europe, it appeared that the general population was not yet really concerned about its evolution and severity. About 20% of the patients followed by the physicians surveyed in the three countries were very worried about the COVID-19 pandemic, whereas this rate was around 30% among the general population over the pandemic course [16]. The global feeling of low to moderate anxiety, both for health professionals and the general population, could appear to be contradictory with the predominant feeling of the physicians of being insufficiently prepared to face the COVID-19 pandemic, as they were not directly involved in the management of this growing epidemic. Regarding the dramatic evolution of the pandemic in Europe in the weeks following the study, it appears that the scientific data available at this time and transmitted to the physicians could have given a wrong assessment of the spread and the severity of the disease [17, 18]. A previous study had highlighted that making available an internal information channel to ensure factual, accurate, and reliable information while preventing information overload represents a key measure in increasing infectious disease preparedness [19]. With the current hindsight on the pandemic, it seems essential to better integrate the primary care physicians into the information, training and protection channels for this kind of health risk, which may be lacking at this level, unlike the hospital level, and this is could be managed by the health authorities [20].
Differences between countries concerning the level of anxiety and the feeling of preparedness were observed, with Spanish physicians feeling more anxious (even more anxious than their patients) but more prepared, while Belgian and French physicians were little worried and moderately prepared. Such variations have been previously studied across countries, with Asian countries feeling more prepared than European or Northern American countries to face emerging diseases [13, 21]. However, no comparison between European countries has been undertaken. The national epidemic context was rather similar over the study period in the three countries involved in the study: 6 COVID-19 cases and 2 related-deaths were reported in France; 134 cases and no deaths in Spain; no cases or deaths in Belgium [2]. The main difference is that the study started in Spain later than in France, and was ended up one week later than in Belgium and France. The anxiety of the Spanish GPs could have been higher, as the European situation was complicated at that time (i.e. Italian situation). This contradictory feeling of anxiety and preparedness among Spanish physicians could be explained also by differences in organization and structure of the primary care services. In Spain, the primary care physicians are included in a complex structure of the public health system (including health administrative services, hospitals and primary care) that were contacted and informed periodically by the health authorities. While these contacts may have helped Spanish primary care professionals feel prepared, they may also have made the physicians anxious about the pandemic. Thus, communication regarding the epidemiological context could have been emphasized in Spain compared to Belgium and France, as well as the preparation of the health services, which could contribute to the higher feeling of preparedness of the Spanish GPs. A comparison could be of interest in adapting one country’s most effective public health measures in terms of information and communication to the other countries [21–23]
This study has some limitations. Physicians included are part of sentinel surveillance networks, which generate inherent biases (these professionals are more interested in research, well-informed and specially concerned with advances in clinical practice), making the results not representative of the primary care physicians in these countries. In France, the réseau Sentinelles representativeness has been previously studied, showing no particular differences regarding age and professional activities [10]. In Belgium, the Sentinel GPs have been selected to cover the whole country and form a representative sample of GPs in the country regarding age, sex and geographical distribution [11]. In Spain, Red Centinela Sanitaria evaluates representativeness yearly using cluster analysis and principal components analysis to ensure a good representation [12]. Even if the representativeness of the physicians participating in these three sentinel networks tries to be reached as much as possible, selection biases inherent to the present study could have occurred, linked in particular to the data collection process. Indeed, inclusion was made on a voluntary basis. However, this had no impact on the representativeness of the Belgian and Spanish physicians in terms of age, sex and location of practice. Regarding the differences observed in France in terms of age and location of practice, this does not seem to have influenced physicians’ feeling of preparedness or anxiety. Indeed, the perceptions of French participating GPs were similar to the ones of Belgian GPs. Finally, this cross-sectional study lacks a follow-up during this COVID-19 pandemic, which could have been particularly interesting to evaluate and adapt the guidelines and information campaigns. Repeating this study through the course of the COVID-19 pandemic, under different conditions of the epidemic and of awareness, could help identify critical aspects to be further improved.
Conclusions
The present study could help health authorities to define preparedness planning for primary care physicians against an emerging epidemic, and identify areas of improvement in terms of information and actions.
Supplementary Information
Additional file 1. Physicians’ questionnaire on early perception of the COVID-19 pandemic.
Acknowledgements
We thank all the physicians participating in this study.
Abbreviations
- GPs
General practitioners
- aOR
Adjusted odds ratio
- CI
Confidence interval
Authors’ contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by GC, TB, VAM, SC, VAT, ODA, LAJE, VCD and MS. The first draft of the manuscript was written by GC, TB and BT and all authors commented on previous versions of the manuscript. All authors read and approved the final version of the manuscript.
Funding
This study was supported by REACTing, a collaborative network of major French research institutions coordinated by Inserm. The funder had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit this article for publication. All researchers’ decisions have been entirely independent from funders.
Availability of data and materials
Data will be available from the corresponding author on reasonable request. Requests will be submitted to the scientific committees of each country. Data provided will have to respect the constraints on privacy and treatment imposed by the national regulatory authorities.
Declarations
Ethics approval and consent to participate
In Belgium and France, there were no specific ethics approval required for the present study. However, the Belgian sentinel network was approved as a whole by the Ethical Committees of the Scientific Society of Flemish GPs and the Catholic University of Louvain (UCL). In France, the sentinel protocol was approved by the French Data Protection Agency (CNIL#471393) and the French ethical research committee. In Spain, the protocol was approved by the Health Sentinel Network Committee, according to the Order SAN/620/2016, that regulates the organization and functioning of the Health Sentinel Network of Castile and León (BOCYL nº 132, 11 July 2016). Consent was obtained from all individual participants included in the study. An email was sent to the physicians of the sentinel networks, with information and a link to accept or decline their participation.
Consent to publication
not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.ECDC. COVID-19 situation update for the EU/EEA and the UK. https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea. Accessed 09 June 2020.
- 3.Nelson LM, Simard JF, Oluyomi A, et al. US Public Concerns About the COVID-19 Pandemic From Results of a Survey Given via Social Media. JAMA Intern Med. 2020;180(7):1020–1022. doi: 10.1001/jamainternmed.2020.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanafelt T, Ripp J, Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA. 2020;10.1001/jama.2020.5893. doi:10.1001/jama.2020.5893. [DOI] [PubMed]
- 5.Asmundson GJG, Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. J Anxiety Disord. 2020 Mar;70:102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed]
- 6.Albarrak AI, Mohammed R, Al Elayan A, et al. Middle East Respiratory Syndrome (MERS): Comparing the knowledge, attitude and practices of different health care workers. J Infect Public Health. 2019;S1876-0341(19):30239–4. doi: 10.1016/j.jiph.2019.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aghaizu A, Elam G, Ncube F, et al. Preventing the next ‘SARS’ - European healthcare workers’ attitudes towards monitoring their health for the surveillance of newly emerging infections: qualitative study. BMC Public Health. 2011;11:541. doi: 10.1186/1471-2458-11-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vinck L, Isken L, Hooiveld M, Trompenaars M, Ijzermans J, Timen A. Impact of the 2009influenza A(H1N1) pandemic on public health workers in the Netherlands. Euro Surveill. 2011;16(7):19793. doi: 10.2807/ese.16.07.19793-en. [DOI] [PubMed] [Google Scholar]
- 9.Jaakkimainen RL, Bondy SJ, Parkovnick M, Barnsley J. How infectious disease outbreaks affect community-based primary care physicians: comparing the SARS and H1N1 epidemics. Can Fam Physician. 2014;60(10):917–925. [PMC free article] [PubMed] [Google Scholar]
- 10.Souty C, Turbelin C, Blanchon T, Hanslik T, Le Strat Y, Boëlle PY. Improving disease incidence estimates in primary care surveillance systems. Popul Health Metr. 2014;12:19. Published 2014 Jul 26. doi:10.1186/s12963-014-0019-8. [DOI] [PMC free article] [PubMed]
- 11.Van den Block L, Onwuteaka-Philipsen B, Meeussen K, Donker G, Giusti F, Miccinesi G, Van Casteren V, Alonso TV, Zurriaga O, Deliens L. Nationwide continuous monitoring of end-of-life care via representative networks of general practitioners in Europe. BMC Fam Pract. 2013;14:73. doi: 10.1186/1471-2296-14-73. [DOI] [PMC free article] [PubMed]
- 12.Vega Alonso AT, Gil Costa M, Ruiz Cosin C, Zapatero Villalonga E. La Red de Médicos Centinelas de Castilla y León: aplicación del análisis de conglomerados para la obtención de una población representativa [A sentinel physicians network in Castile and León: the use of cluster analysis to obtain a representative population]. Gac Sanit. 1990;4(20):184–188. doi:10.1016/s0213-9111(90)71028-x. [DOI] [PubMed]
- 13.Wong TY, Koh GC, Cheong SK, et al. A cross-sectional study of primary-care physicians in Singapore on their concerns and preparedness for an avian influenza outbreak. Ann Acad Med Singapore. 2008;37(6):458–464. [PubMed] [Google Scholar]
- 14.Edeghere O, Fowler T, Wilson F, et al. Knowledge, attitudes, experience and behaviour of frontline health care workers during the early phase of 2009 influenza A(H1N1) pandemic, Birmingham, UK. J Health Serv Res Policy. 2015;20(1):26–30. doi:.10.1177/1355819614554243 [DOI] [PubMed]
- 15.The R Foundation. The R Project for Statistical Computing [Available from: https://www.rproject.org/].
- 16.Pashazadeh Kan F, Raoofi S, Rafiei S, Khani S, Hosseinifard H, Tajik F, Raoofi N, Ahmadi S, Aghalou S, Torabi F, Dehnad A, Rezaei S, Hosseinipalangi Z, Ghashghaee A. A systematic review of the prevalence of anxiety among the general population during the COVID-19 pandemic. J Affect Disord. 2021;293:391–398. doi: 10.1016/j.jad.2021.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shangguan Z, Wang MY, Sun W. What Caused the Outbreak of COVID-19 in China: From the Perspective of Crisis Management. Int J Environ Res Public Health. 2020;17(9). doi:10.3390/ijerph17093279. [DOI] [PMC free article] [PubMed]
- 18.Peeri NC, Shrestha N, Rahman MS, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49(3):717–26. doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belfroid E, Timen A, van Steenbergen JE, Huis A, Hulscher ME. Which recommendations are considered essential for outbreak preparedness by first responders? BMC Infect Dis. 2017;17(1):195. doi: 10.1186/s12879-017-2293-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kidd MR. Five principles for pandemic preparedness: lessons from the Australian COVID-19 primary care response. Brit J General Pract. 2020;70(696):316–7. doi: 10.3399/bjgp20X710765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tse DM, Li Z, Lu Y, Li Y, Liu Y, Wong WCW. Fighting against COVID-19: preparedness and implications on clinical practice in primary care in Shenzhen, China. BMC Fam Pract. 2020;21(1):271. doi: 10.1186/s12875-020-01343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cag Y, Erdem H, Gormez A, Ankarali H, Hargreaves S, Ferreira-Coimbra J, Rubulotta F, Belliato M, Berger-Estilita J, Pelosi P, Blot S, Lefrant JY, Mardani M, Darazam IA, Cag Y, Rello J. Anxiety among front-line health-care workers supporting patients with COVID-19: A global survey. Gen Hosp Psychiatry. 2021;68:90–96. doi: 10.1016/j.genhosppsych.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhagavathula AS, Aldhaleei WA, Rahmani J, Mahabadi MA, Bandari DK. Knowledge and Perceptions of COVID-19 Among Health Care Workers: Cross-Sectional Study. JMIR Public Health Surveill. 2020; 6(2):e19160. doi: 10.2196/19160. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Physicians’ questionnaire on early perception of the COVID-19 pandemic.
Data Availability Statement
Data will be available from the corresponding author on reasonable request. Requests will be submitted to the scientific committees of each country. Data provided will have to respect the constraints on privacy and treatment imposed by the national regulatory authorities.