Abstract
Purpose:
The Coronavirus Disease 2019 (COVID-19) pandemic has caused significant morbidity and mortality worldwide. Patients with rheumatoid arthritis (RA) face unique challenges during the pandemic, including concerns regarding infection risk, drug shortages, limited access to care, social isolation, and mental health. This review will examine the multifaceted impacts of the COVID-19 pandemic on patients living with RA.
Recent Findings:
In patients with RA, risk factors for severe COVID-19 outcomes include older age and comorbidities, similar to those in the general population. Glucocorticoids, but not other classes of disease-modifying antirheumatic drugs (DMARDs), appear to be associated with higher risk of severe COVID-19 outcomes. RA patients have been affected by changes in access to care, telemedicine, drug shortages, anxiety, and social isolation, which may be contribute to disease flares.
Summary:
Glucocorticoids, but not other DMARDs, are associated with higher risk of severe COVID-19 outcomes in RA patients. Further studies are needed to explore the impact of specific DMARDs on COVID-19 outcomes, understand the broader implications of the COVID-19 pandemic on RA disease activity, and optimize the use of telemedicine in RA management.
Keywords: COVID-19, coronavirus, rheumatoid arthritis
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic, caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), is an unprecedented global health crisis (1). Since the onset of the pandemic, patients with rheumatoid arthritis (RA) have expressed concerns regarding potential higher risks of poor COVID-19 outcomes due to immunosuppressive treatments, an underlying inflammatory state, associated comorbidities such as interstitial lung disease (ILD) and glucocorticoid-induced diabetes mellitus, and racial/ethnic and socioeconomic disparities (2*). Reports from early in the pandemic suggested that rheumatic disease patients may be at higher risk of respiratory failure and death from COVID-19 (Table 1) (3*, 4*, 5**). However, accumulating evidence suggests patients with rheumatic disease may not be at higher risk of severe COVID-19 outcomes after accounting for age, comorbidities, and glucocorticoid use (6*, 7, 8*, 9*). In addition, the risk for infection and certain outcomes may vary according to rheumatic disease type, disease activity, and specific disease modifying anti-rheumatic drugs (DMARDs).
Table 1.
Key studies examining COVID-19 outcomes in rheumatic disease patients.
| Reference | Location | Study Population | COVID-19 Ascertainment | Primary Finding | Limitations |
|---|---|---|---|---|---|
| Williamson et al. (OpenSAFELY) (5) | United Kingdom | General population (>17 million adults) | Positive molecular testing | RA/SLE/Psoriasis associated with higher risk of COVID-19 related death (HR 1.19, 95% CI: 1.11 to 1.27). | Multiple testing; adjusting for causal intermediates*; unmeasured confounding†; inclusion of non-laboratory confirmed COVID-19 cases; missing data; lumping of RA, SLE, and psoriasis; lack of information about DMARDs and disease activity. |
| Ye et al. (3) | Wuhan, China | COVID-19 patients with rheumatic disease versus without rheumatic disease | Positive molecular testing (n=20) or positive IgM and IgG (n=1) | Respiratory failure more common in rheumatic disease patients than comparators (38% vs. 10%, p<0.01). | Small sample size (n=21 rheumatic disease patients); unmeasured confounding; collider bias.‡ |
| D’Silva & Serling-Boyd et al. (4); Serling-Boyd & D’Silva et al. (6) | Boston, MA | COVID-19 patients with rheumatic disease versus without rheumatic disease | Positive molecular testing | Higher odds of mechanical ventilation in rheumatic disease patients versus comparators in first two months of pandemic (OR 3.11, 95% CI: 1.07 to 9.05). Improved risk of mechanical ventilation six months into the pandemic. | Collider bias may bias results towards null; adjusting for causal intermediates. |
| D’Silva & Jorge et al. (9) | United States | COVID-19 patients with rheumatic disease versus without rheumatic disease | Positive molecular testing or diagnostic code | Higher risks of hospitalization and acute renal failure mediated by comorbidities. Higher risk of venous thromboembolism (RR 1.60, 95% CI: 1.14 to 2.25), regardless of comorbidities. | Unmeasured confounding; inaccuracies in ICD-10 coding; lack of geographic information; collider bias. |
| Pablos et al. (30) | Spain | COVID-19 patients with rheumatic disease versus without rheumatic disease | Positive molecular testing | Higher odds of severe COVID-19 with glucocorticoids (OR 2.20, 95% CI: 1.36 to 3.54). | Limited to hospitalized patients; small sample sizes in subgroups; collider bias. |
| Gianfrancesco et al. (31) | International Physician-Reported Registry | Hospitalized versus non-hospitalized rheumatic disease patients with COVID-19 | Physician-reported diagnosis | Prednisone doses ≥10 mg daily associated with higher odds of hospitalization (OR 2.05, 95% CI: 1.06 to 3.96). TNF inhibitors associated with lower odds of hospitalization (OR 0.40, 95% CI: 0.19 to 0.81). | Selection bias (more severe cases more likely to be captured); unmeasured confounding; large number of unresolved cases (35%) at time of publication. |
COVID-19, Coronavirus Disease 2019; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; HR, hazard ratio; DMARD, disease-modifying antirheumatic drug; OR, odds ratio; CI, confidence interval; RR, relative risk; TNF, tumor necrosis factor; ICD-10, International Classification of Diseases, 10th Revision.
Causal intermediates are covariates that are causally influenced by the exposure and also causally affect the outcome of interest. For example, if the exposure is rheumatic disease and the outcome is COVID-19 related death, a comorbidity such as diabetes may be a causal intermediate as rheumatic disease treatments such as glucocorticoids can cause diabetes, which in turn can cause more severe COVID-19.
Unmeasured confounding refers to covariates that may not be measured and/or adjusted for in analyses. For example, glucocorticoid use may be an unmeasured confounder in the OpenSAFELY study.
Collider bias occurs when analyses are restricted by a collider variable, which is a variable that is a common effect of the exposure and outcome. In studies where the exposure is COVID-19 infection and the outcomes are COVID-19-related outcomes such as hospitalization, mechanical ventilation, or death, conditioning on the common effect of COVID-19 may bias results towards the null.
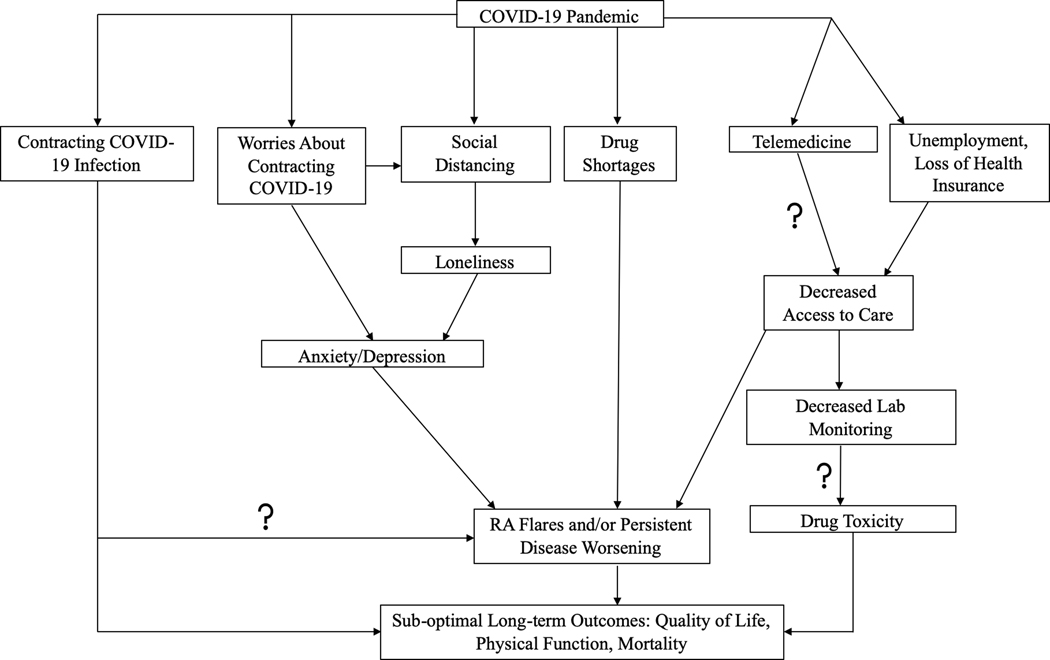
In addition to concerns regarding COVID-19 outcomes, patients with RA have faced unique challenges during the pandemic (Figure 1). For example, early in the pandemic, hydroxychloroquine was promoted as a potential COVID-19 prophylactic and treatment, leading to drug shortages for patients with rheumatic diseases, including RA (10). Many patients also faced difficulties with accessing care because of transitions to telemedicine and loss of health insurance resulting from unemployment (2*). In addition, the pandemic has led to increased rates of fear, anxiety, depression, and social isolation in the general population, all of which can be magnified in patients living with chronic diseases like RA and may contribute to RA flares (2*, 11).
Figure 1.
Impacts of the COVID-19 pandemic on patients living with rheumatoid arthritis. COVID-19, Coronavirus Disease 2019; RA, rheumatoid arthritis. Question mark indicates further research needed.
In this review, we will examine the multifaceted impacts of the COVID-19 pandemic on patients with RA. We will first examine outcomes of COVID-19 in patients with rheumatic diseases including RA. We will then examine secondary impacts of the pandemic, including drug shortages, access to care, and mental health.
COVID-19 Outcomes in RA Patients
Prior to the COVID-19 pandemic, evidence showed that RA patients had higher risk of infection than the general population, due to a number of factors, including immunosuppression, a chronic inflammatory state, and comorbidities (12). For instance, Doran et al. compared the frequency of infections in a population-based incidence cohort of RA patients to general population comparators and found that RA patients had higher risk of infections than comparators without RA (adjusted hazard ratio [HR] 1.70, 95% CI: 1.42 to 2.03) (13). The most common infections included those affecting the respiratory tract, skin, and musculoskeletal system (13). In a study using the Consortium of Rheumatology Researchers of North America (CORRONA) registry, higher RA disease activity was associated with higher rates of infection (14). Additionally, prednisone doses >7.5 mg daily were associated with six-fold higher rates of infections requiring hospitalization, and TNF inhibitors and methotrexate were associated with higher risk of outpatient infections (14). However, these studies mainly examined risk of bacterial infections. There is limited data suggesting that glucocorticoids, JAK inhibitors, and TNF inhibitors may be associated with higher risk of viral respiratory infections (12, 15).
These prior observations led to concerns that RA patients would have higher risk of COVID-19 and poor COVID-19 outcomes compared to the general population. However, there remains significant uncertainty given observational studies and clinical trials suggesting that some immunosuppressive agents commonly used to treat RA may actually improve COVID-19 outcomes (16, 17**, 18**). The largest study to date evaluating the risk of severe COVID-19 in patients with RA, called OpenSAFELY, was completed early in the first three months of the pandemic (5**). In this population-based observational study, investigators examined risk factors for COVID-19 related death in a population of 17.2 million adults in the United Kingdom (5**). In addition to risk factors such as older age, male sex, obesity, non-white race, and diabetes, a diagnosis of RA, lupus, or psoriasis was associated with greater risk of COVID-19 related death (adjusted HR 1.19, 95% CI: 1.11 to 1.27) (5**). While there were a number of strengths to this study, including its large size and use of a hard outcome like mortality, there were also several methodologic limitations, including multiple testing, unmeasured confounding, adjustment for causal intermediates, inclusion of non-laboratory confirmed COVID-19 cases, and missing data regarding smoking, obesity, and ethnicity. Information on use of immunosuppressive agents and rheumatic disease activity were not available. Perhaps most importantly, this study combined RA, lupus, and psoriasis into a single category, although these diseases are quite distinct from one another, limiting conclusions that can be drawn regarding the risk for RA patients (19).
In contrast to the OpenSAFELY study, early case series reported generally mild COVID-19 clinical courses in patients with rheumatic diseases, and observational studies from single-center and multi-center cohorts reported similar incidence of COVID-19 among rheumatic disease patients and the general population (20, 21, 22, 23, 24*, 25). However, early comparative cohort studies from Wuhan, China, and Boston, MA, reported higher risk of respiratory failure requiring mechanical ventilation in COVID-19 patients with rheumatic diseases versus comparators (3*, 4*). In the Wuhan study, 21 rheumatic disease patients with COVID-19 (8 of whom had RA) were identified among 2,326 COVID-19 patients, and respiratory failure was more common in rheumatic disease patients than comparators (38% versus 10%, p<0.01) (3*). However, due to the small sample size, this study could not adjust for confounders.
In the Boston study, patients with COVID-19 by positive molecular test and rheumatic disease were systematically identified using diagnostic codes followed by chart review (4*). Fifty-two rheumatic disease patients (of whom 19 [37%] had RA) were identified and matched by age, sex, and date of COVID-19 diagnosis to 104 comparators without rheumatic disease two months into the pandemic (4*). Patients with rheumatic disease had higher odds of requiring mechanical ventilation than comparators (multivariable odds ratio [OR] 3.11, 95% CI: 1.07 to 9.05) after adjusting for age, body mass index, smoking, and number of comorbidities (4*). In an extension of this study that included 143 patients with rheumatic disease (44 [31%] with RA) six months into the pandemic, the risk of mechanical ventilation in rheumatic disease patients versus comparators was attenuated (adjusted HR 1.51, 95% CI: 0.93 to 2.44), and there was a trend towards improvement in mechanical ventilation risk over time (6*). The improvement in COVID-19 outcomes in rheumatic disease patients as the pandemic progresses has been replicated in other studies and may reflect detection of milder cases and improvements in therapies and supportive care for COVID-19 (26*).
In a large multi-center electronic health record network in the United States, COVID-19 outcomes were examined in patients living with systemic autoimmune rheumatic diseases (SARDs) versus exposure-score matched comparators (9*). COVID-19 was determined by diagnostic codes or positive molecular testing. In total, 2,379 SARD patients were identified, of whom 1,181 (50%) had RA (9*). In the primary model, in which SARD patients were matched to comparators on age, sex, race/ethnicity, and body mass index, SARD patients had significantly higher risks of hospitalization (relative risk [RR] 1.14, 95% CI: 1.03 to 1.26), renal failure requiring renal replacement therapy (RR 1.81, 95% CI: 1.07 to 3.07), and venous thromboembolism (VTE, RR 1.74, 95% CI: 1.23 to 2.45) versus comparators (9*). In an extended model that also matched for comorbidities, all risks were largely attenuated, except for the risk of VTE (9*). This and the studies from Boston suggest that comorbidities are an important mediator and/or confounder of the risk of poor COVID-19 outcomes in patients with rheumatic diseases, similar to risk factors in the general population (9*). Patients with RA are at baseline at higher risk of VTE than the general population and require close monitoring for VTE during COVID-19 (27). In addition, given the association between RA and lung disease (such as ILD, bronchiectasis, and bronchiolitis), a significant risk factor in the general population for poor COVID-19 outcomes, it is important to closely monitor RA patients with lung disease for COVID-19 complications (28, 29*).
Several studies have examined the impact of DMARDs on COVID-19 outcomes. A comparative cohort study from Spain of patients with COVID-19 infection included 228 rheumatic disease patients and 228 comparators without rheumatic disease (30*). In this study, the investigators found no higher odds of severe COVID-19 associated with hydroxychloroquine, conventional synthetic DMARDs, or biologic/targeted synthetic DMARDs (30*). However, there were higher odds of severe COVID-19 associated with glucocorticoid use (OR 2.20, 95% CI: 1.36 to 3.54) (30*). A French cohort study demonstrated similar findings (8*).
The Global Rheumatology Alliance (GRA) physician-reported registry has also examined the relationship between DMARDs and severe COVID-19. In an early study, the GRA reported risk factors for hospitalization in 600 rheumatic disease patients with COVID-19 (230 [38%] with RA) (31**). Prednisone doses 10 mg daily were associated with higher odds of hospitalization (adjusted OR 2.05, 95% CI: 1.06 to 3.96), while conventional synthetic and biologic/targeted synthetic DMARDs were not (31**). Interestingly, TNF inhibitors were associated with a reduced odds of hospitalization (adjusted OR 0.40, 95% CI: 0.19 to 0.81), suggesting a possible protective effect that is also supported by evidence of exuberant TNF responses in post-mortem lymph node specimens from patients with fatal COVID-19 (31**, 32*). Additional studies are needed to further investigate these associations. The GRA study is limited by selection bias (as physicians may report more severe cases), unmeasured confounding, and lack of an active comparator for medication analyses.
In summary, the available evidence at this time suggests that many risk factors associated with poor COVID-19 outcomes in rheumatic disease patients are similar to those observed in the general population, including older age, comorbidities, and obesity. There may be a slightly higher risk of severe COVID-19 outcomes in rheumatic disease patients, as observed in some studies such as OpenSAFELY, and these associations may be driven by certain disease-specific factors such as glucocorticoid use (5**, 31**). The relationship between glucocorticoid use and severe COVID-19 outcomes may be related to confounding by indication, as patients with more severe rheumatic disease may be more likely to take glucocorticoids, and increased disease activity has been associated with higher risk of other infections prior to COVID-19 (14). The timing of glucocorticoid exposure may also impact the risk of severe COVID-19. Early glucocorticoid exposure may be associated with harm, while late glucocorticoid exposure may reduce COVID-19 mortality by treating hyperinflammation, as observed in the RECOVERY trial of dexamethasone versus placebo in COVID-19 (17**).
The American College of Rheumatology (ACR) has released guidance regarding the management of rheumatic diseases during the ongoing COVID-19 pandemic, with frequent updates to capture the rapidly evolving literature (33). For patients with a known SARS-CoV-2 exposure or confirmed COVID-19, the ACR recommends holding most DMARDs and resuming within 7–14 days of symptom resolution (33). Hydroxychloroquine may be continued during COVID-19 infection, and patients and providers can engage in shared decision-making to determine whether to continue or hold IL-6 receptor inhibitors given some reports of their efficacy for the treatment of COVID-19 (33, 34*). Regardless of exposure or infection status, glucocorticoids should be kept at the lowest possible dose to maintain control of the rheumatic disease (33). These guidelines are consistent with the results of the observational studies reviewed herein.
Secondary Impacts of the COVID-19 Pandemic on RA Patients
In addition to potentially higher risks of infection and poor outcomes, patients with RA have faced many other challenges during the COVID-19 pandemic, including changes in access to care due to the switch to telemedicine and unemployment, drug shortages, social isolation, and anxiety and depression. During the first 2 weeks of the pandemic in the US, a cross-sectional survey of 530 patients with rheumatic disease, 61% of whom had RA, was conducted (2*). Almost 200 patients (42%) reported changes in care, such as cancelled/postponed appointments and switch to telemedicine visits (2*). Seventy-four patients (14%) reported self-imposed changes to medications or doses, and 58 (11%) had physician-directed medication changes (2*). In qualitative analyses, many patients noted anxiety, loneliness, and worsening arthritis symptoms (2*).
Indeed, the pandemic has had significant implications on mental health and rheumatic disease symptoms. In open-ended interviews with 112 patients in New York City, patients reported increased fatigue, anxiety, stress, and worsening musculoskeletal symptoms and cognitive function (35*). In addition to worries about developing COVID-19, patients expressed worries about medication changes, family, work, and finances (35*). Many patients with rheumatic diseases believe they are at higher risk of poor COVID-19 outcomes and therefore follow strict social distancing measures (36*). While necessary to prevent the spread of COVID-19, strict social distancing can foster loneliness, which can exacerbate anxiety, depression, and rheumatic disease flares.
The GRA also conducted a Patient Experience Survey to capture the impact of the COVID-19 pandemic on rheumatic disease patients (37). These data have demonstrated the consequences of hydroxychloroquine drug shortages (38*). Among 9,393 patient respondents from around the world, 3,872 (41%) were taking an antimalarial treatment (38*). Of these, 230 (6%) were unable to continue antimalarial treatment due to drug shortages (38*). Patients experiencing drug shortages reported higher levels of rheumatic disease activity and poorer mental and physical health (38*).
Meanwhile, the switch to telemedicine has caused significant shifts in rheumatic disease care, and the impact of telemedicine on the diagnosis and management of RA remains unclear. Using validated instruments to measure disease activity and functional status is crucial to achieving treat-to-target objectives in RA management (39). An ACR working group recommended adaptations to disease activity and functional status measures for use in telemedicine, including replacing provider-assessed joint counts with patient-reported joint counts (39). Further studies are needed to optimize the implementation of patient-reported outcomes, treat-to-target strategies, and laboratory monitoring for high risk medications in the telemedicine setting (40).
In addition to patient-reported surveys, survey studies of rheumatology providers have also revealed changes in care due to the pandemic. A survey of 1,286 providers was conducted in countries belonging to the European League Against Rheumatism (EULAR) (41*). Over 80% of respondents reported cancelling new and follow-up in-person visits, many of which were replaced with virtual evaluation (41*). Seventy-four percent of respondents reported that they were less likely to start a biologic/targeted synthetic DMARD during the pandemic (41*). Lastly, 58% of respondents noted a longer interval between symptom onset and rheumatologic evaluation, which may significantly impact the ability to achieve early diagnosis and treat-to-target management (41*).
Conclusion
The COVID-19 pandemic has had profound implications for patients living with RA. In general, observational studies have not consistently found that patients with RA are at higher risk of poor outcomes from COVID-19 compared to the general population. However, rheumatic disease patients with comorbidities and those on glucocorticoids do seem to be at higher risk of severe COVID-19. Additional population-based studies are needed to examine whether having RA or using specific DMARDs are associated with greater COVID-19 risk and/or more severe COVID-19 outcomes. In addition to concerns regarding infection risk, patients with RA have faced challenges including changes in access to care, drug shortages, anxiety, and social isolation, all of which may be associated with worse RA control. Further studies are needed to optimize the use of telemedicine in RA care.
Key Points:
Whether patients with rheumatoid arthritis (RA) or those who use certain disease-modifying antirheumatic drugs (DMARDs) are at higher risk for severe COVID-19 remains poorly understood, but patients with RA who are on glucocorticoids appear to have higher risk of severe COVID-19.
The COVID-19 pandemic has created unique challenges for RA patients, including changes in access to care, drug shortages, social isolation, and anxiety, all of which may be associated with RA flares.
Further studies are needed to determine the optimal use of telemedicine to achieve early diagnosis and treat-to-target management in RA care.
Acknowledgments
Funding/Support: KMD is supported by the National Institutes of Health Ruth L. Kirschstein Institutional National Research Service Award [T32-AR-007258] and Rheumatology Research Foundation Scientist Development Award. ZSW is supported by NIH/NIAMS [K23AR073334 and L30 AR070520].
Footnotes
Conflicts of Interest: KMD has no disclosures. ZSW reports research support from Bristol-Myers Squibb and Principia and consulting fees from Viela Bio and Medpace.
References
- 1.Coronavirus disease 2019 dashboard: World Health Organization; [12–28-20]. Available from: https://covid19.who.int/.
- 2. Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR, et al. Experiences of patients with rheumatic diseases in the US during early days of the COVID-19 pandemic. ACR Open Rheumatol. 2020;2(6):335–43.32311836 * This is the first survey study of rheumatic disease patients during the COVID-19 pandemic. This article demonstrated changes in access to care, medication changes, and feelings of anxiety and loneliness among rheumatic disease patients during the first 2 weeks of the pandemic.
- 3. Ye C, Cai S, Shen G, Guan H, Zhou L, Hu Y, et al. Clinical features of rheumatic patients infected with COVID-19 in Wuhan, China. Ann Rheum Dis. 2020;79:1007–13.32444415 * This is an early study from the first few months of the COVID-19 pandemic in Wuhan, China. This study showed COVID-19 patients with rheumatic disease had higher odds of respiratory failure versus patients without rheumatic disease.
- 4. D’Silva KM, Serling-Boyd N, Wallwork R, Hsu TYT, Fu X, Gravallese EM, et al. Clinical characteristics and outcomes of patients with Coronavirus Disease 2019 (COVID-19) and rheumatic disease: A comparative cohort study from a United States “hot spot”. Ann Rheum Dis. 2020;79:1156–62.32457048 * This is an early study from the first two months of the COVID-19 pandemic in Boston, Massachusetts, USA. This study showed COVID-19 patients with rheumatic disease had higher odds of mechanical ventilation versus comparators without rheumatic disease matched on age, sex, and date of COVID-19 diagnosis.
- 5. Williamson E, Walker AJ, Bhaskaran KJ, Bacon S, Bates C, Morton CE, et al. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. Nature. 2020;584:430–36.32640463 ** This is the largest general population-based study to date examining risk factors for COVID-19 mortality. This study showed that patients with rheumatoid arthritis, systemic lupus erythematosus, or psoriasis had slightly higher risk of COVID-19 mortality than those without these diseases.
- 6. Serling-Boyd N, D’Silva KM, Hsu TY, Wallwork R, Fu X, Gravallese EM, et al. Coronavirus disease 2019. outcomes among patients with rheumatic diseases 6 months into the pandemic. Ann Rheum Dis. 2020; Advance online publication. * This study examined COVID-19 outcomes in rheumatic disease patients versus comparators six months into the COVID-19 pandemic and found no significantly higher risk of hospitalization, mechanical ventilation, or death after adjusting for confounders, and there was a trend towards improvement in risk of mechanical ventilation over time.
- 7.Akiyama S, Hamdeh S, Micic D, Sakuraba A. Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: a systematic review and meta-analysis. Ann Rheum Dis. 2020; Advance online publication. [DOI] [PubMed] [Google Scholar]
- 8. Severity of COVID-19 and survival in patients with rheumatic and inflammatory diseases: data from the French RMD COVID-19 cohort of 694 patients. Ann Rheum Dis. 2020; Advance online publication. * This study from a French cohort of patients with rheumatic diseases and COVID-19 showed that patients with rheumatic diseases on glucocorticoids, but not other DMARDs, were at higher risk of severe COVID-19.
- 9. D’Silva KM, Jorge A, Cohen A, McCormick N, Zhang Y, Wallace ZS, et al. COVID-19 Outcomes in Patients with Systemic Autoimmune Rheumatic Diseases (SARDs) Compared to the General Population: A US Multi-Center Comparative Cohort Study. Arthritis Rheum. 2020; Advance online publication. * This was the first study of COVID-19 outcomes in rheumatic disease patients from a large multi-center electronic health record network. Risks of severe COVID-19 outcomes in rheumatic disease patients were attenuated after adjusting for comorbidities, except for the risk of venous thromboembolism.
- 10.Sattui SE, Liew JW, Graef ER, Coler-Reilly A, Berenbaum F, Duarte-García A, et al. Swinging the pendulum: lessons learned from public discourse concerning hydroxychloroquine and COVID-19. Expert Review of Clinical Immunology. 2020;16(7):659–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, Caporali R. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmunity Reviews. 2020;19(5):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doran MF, Crowson CS, Pond GR, O’Fallon WM, Gabriel SE. Frequency of infection in patients with rheumatoid arthritis compared with controls: A population-based study. Arthritis Rheum. 2002;46(9):2287–93. [DOI] [PubMed] [Google Scholar]
- 14.Au K, Reed G, Curtis JR, Kremer JM, Greenberg JD, Strand V, et al. High disease activity is associated with an increased risk of infection in patients with rheumatoid arthritis. Ann Rheum Dis. 2011;70(5):785–91. [DOI] [PubMed] [Google Scholar]
- 15.Kilian A, Chock YP, Huang IJ, Graef ER, Upton LA, Khilnani A, et al. Acute respiratory viral adverse events during use of antirheumatic disease therapies: A scoping review. Semin Arthritis Rheum. 2020;50(5):1191–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McInnes IB. COVID-19 and rheumatology: first steps towards a different future? Ann Rheum Dis. 2020;79(5):551–2. [DOI] [PubMed] [Google Scholar]
- 17. Horby PW, Landray MJ. Dexamethasone in Hospitalized Patients with COVID-19: Preliminary Report. N Engl J Med. 2020; Advance online publication. ** This landmark randomized clinical trial (RECOVERY) demonstrated that dexamethasone reduced mortality among patients with severe COVID-19 requiring oxygen supplementation or mechanical ventilation.
- 18. Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N Engl J Med. 2020; Advance online publication. ** This landmark double-blind placebo-controlled randomized clinical trial showed that baricitinib plus remdesivir was superior to remdesivir alone in reducing recovery time among hospitalized COVID-19 patients.
- 19.Hyrich KL, Machado PM. Rheumatic disease and COVID-19: epidemiology and outcomes. Nat Rev Rheumatol. 2020; Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haberman R, Axelrad J, Chen A, Castillo R, Yan D, Izmirly P, et al. Covid-19 in immune-mediated inflammatory diseases - Case series from New York. N Engl J Med. 2020;383:85–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monti S, Balduzzi S, Delvino P, Bellis E, Quadrelli VS, Montecucco C. Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis. 2020;79(5):667–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Favalli EG, Ingegnoli F, Cimaz R, Caporali R. What is the true incidence of COVID-19 in patients with rheumatic diseases? Ann Rheum Dis. 2020; Advance online publication. [DOI] [PubMed] [Google Scholar]
- 23.Emmi G, Battiol A, Mattioli I, Silvestri E, Di Scala G, Urban ML, et al. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmun Rev. 2020;19:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Michelena X, Borrell H, Lopez-Corbeto M, Lopez-Lasanta M, Moreno E, Pascual-Pastor M, et al. Incidence of COVID-19 in a cohort of adult and pediatric patients with rheumatic diseases treated with targeted biologic and synthetic disease-modifying anti-rheumatic drugs. Semin Arthritis Rheum. 2020;50:564–70.32425260 * This early study investigated the incidence of COVID-19 among rheumatic disease patients in Barcelona, Spain, using telephone surveys and electronic health record review. The study found a similar incidence rate of COVID-19 in rheumatic disease patients and the general population.
- 25.Conticini E, Bargagli E, Bardelli M, Rana GD, Baldi C, Cameli P, et al. COVID-19 pneumonia in a large cohort of patients treated with biological and targeted synthetic antirheumatic drugs. Ann Rheum Dis. 2020; Advance online publication. [DOI] [PubMed] [Google Scholar]
- 26. Jorge A, D’Silva KM, Cohen A, Wallace ZS, McCormick N, Zhang Y, et al. Temporal trends in severe COVID-19 outcomes in patients with rheumatic disease: a cohort study. Lancet Rheumatol. 2020; Advance online publication. * This study examined temporal trends in COVID-19 outcomes in rheumatic disease patients using a large multi-center electronic health record network. The study found improvements in severe COVID-19 outcomes in rheumatic disease patients over time during the pandemic.
- 27.Kim SC, Schneeweiss S, Liu J, Solomon DH. The risk of venous thromboembolism in patients with rheumatoid arthritis. Arthritis Care Res 2013;65(10):1600–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spagnolo P, Lee JS, Sverzellati N, Rossi G, Cottin V. The lung in rheumatoid arthritis: Focus on interstitial lung disease. Arthritis Rheumatol. 2018;70(10):1544–54. [DOI] [PubMed] [Google Scholar]
- 29. Drake TM, Docherty AB, Harrison EM, Quint JK, Adamali H, Agnew S, et al. Outcome of Hospitalization for COVID-19 in Patients with Interstitial Lung Disease. An International Multicenter Study. Am J Respir Crit Care Med. 2020;202(12):1656–65.33007173 * This study found that patients with interstitial lung disease, including both idiopathic pulmonary fibrosis and other fibrosing lung diseases, are at increased risk of death from COVID-19 compared to age, sex, and comorbidity matched comparators without ILD.
- 30. Pablos JL, Galindo M, Carmona L, Lledó A, Retuerto M, Blanco R, et al. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis. 2020; Advance online publication. * This comparative cohort study from Spain showed that older age, male sex, comorbidities, and glucocorticoid use (but not other DMARDs) were associated with severe COVID-19 in rheumatic disease patients versus comparators without rheumatic disease.
- 31. Gianfrancesco MA, Hyrich KL, Al-Adely S, Carmona L, Danila MI, Gossec L, et al. Characteristics associated with hospitalization for COVID-19 in people with rheumatic disease: Data from the COVID-19 Global Rheumatology Alliance Physician-Reported Registry. Ann Rheum Dis. 2020;79:859–66.32471903 ** This early study from the Global Rheumatology Alliance Physician-Reported COVID-19 registry showed that rheumatic disease patients on glucocorticoids, but not other DMARDs, had higher odds of hospitalization. TNF inhibitor use was associated with lower odds of hospitalization.
- 32. Kaneko N, Kuo H-H, Boucau J, Farmer JR, Allard-Chamard H, Mahajan VS, et al. Loss of Bcl-6-Expressing T Follicular Helper Cells and Germinal Centers in COVID-19. Cell. 2020;183:1–15.33007260 * This study of lymph nodes from patients with fatal COVID-19 showed excessive TNF levels and aberrant germinal center formation, suggesting inhibition of TNF may promote a more robust and effective immunologic response to COVID-19. Further studies are needed to explore this hypothesis.
- 33.Mikuls TR, Johnson SR, Fraenkel L, Arasaratnam RJ, Baden LR, Bermas BL, et al. American College of Rheumatology Guidance for the Management of Rheumatic Disease in Adult Patients During the COVID-19 Pandemic: Version 2. Arthritis & Rheumatology. 2020;72(9):e1–e12. [DOI] [PubMed] [Google Scholar]
- 34. Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, et al. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N Engl J Med. 2020;0:1–12. * This randomized clinical trial showed that tocilizumab was associated with reduced likelihood of progression to the composite outcome of mechanical ventilation or death versus placebo in patients hospitalized with COVID-19. Given that this finding differs from prior negative clinical trials, further studies are needed to determine which COVID-19 patients may benefit from tocilizumab.
- 35. Mancuso CA, Duculan R, Jannat-Khah D, Barbhaiya M, Bass AR, Mehta B. Rheumatic Disease-Related Symptoms During the Height of the COVID-19 Pandemic. HSS Journal ® 2020; Advance online publication. * This study used open-ended interviews with rheumatic disease patients to determine the impact of the COVID-19 pandemic. Patients reported fatigue, anxiety, stress, and worsening musculoskeletal symptoms and cognitive function due to the pandemic.
- 36. Hooijberg F, Boekel L, Vogelzang EH, Leeuw M, Boers M, Van Vollenhoven R, et al. Patients with rheumatic diseases adhere to COVID-19 isolation measures more strictly than the general population. Lancet Rheumatol. 2020;2(10):e583–e5.33106791 * This study from the Netherlands showed that patients with rheumatic diseases adhered to more strict social distancing than what was recommended by the public health department.
- 37.Sirotich E, Dillingham S, Grainger R, Hausmann JS, Robinson P, Yazdany J, et al. Capturing Patient-Reported Outcomes During the COVID-19 Pandemic: Development of the COVID-19 Global Rheumatology Alliance Patient Experience Survey. Arthritis Care Res. 2020;72(7):871–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sirotich E, Kennedy K, Surangiwala S, Semalulu T, Large M, Liew J, et al. Antimalarial drug shortages during the COVID-19 pandemic: Results from the Global Rheumatology Alliance Patient Experience Survey. American College of Rheumatology Convergence; Virtual 2020. * This study from the Global Rheumatology Alliance Patient Experience Survey showed that many patients on hydroxychloroquine experienced drug shortages during the pandemic, and patients experiencing drug shortages reported worse rheumatic disease symptoms.
- 39.England BR, Barber CEH, Bergman M, et al. Adaptation of American College of Rheumatology Rheumatoid Arthritis Disease Activity and Functional Status Measures for Telehealth Visits. Arthritis Care Res. 2020; Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taylor PC. Adopting PROs in virtual and outpatient management of RA. Nature Reviews Rheumatology. 2020;16(9):477–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dejaco C, Alunno A, Bijlsma JW, Boonen A, Combe B, Finckh A, et al. Influence of COVID-19 pandemic on decisions for the management of people with inflammatory rheumatic and musculoskeletal diseases: a survey among EULAR countries. Ann Rheum Dis. 2020; Advance online publication. * This survey study of rheumatology providers reported that providers were less likely to start biologic or targeted synthetic DMARDs during the pandemic compared to prior to the pandemic.