Highlights
-
•
Exercise programs and rigid bracing reduce pain in people with vertebral fractures.
-
•
Exercise and bracing may not increase activity or quality of life after vertebral fracture.
-
•
Exercise is not associated with harm after vertebral fracture.
Keywords: Bracing, Exercise, Osteoporotic vertebral fracture, Rehabilitation
Abstract
Background
Osteoporotic vertebral fractures affect a large number of older adults
Objectives
Systematically review evidence of the benefits and harms of non-surgical and non-pharmacological management of people with osteoporotic vertebral fractures compared with standard care (control); and evaluate the benefits and harms of non-surgical and non-pharmacological management of people with osteoporotic vertebral fractures compared with an alternative non-pharmacological, non-invasive intervention.
Design
Systematic review and meta-analysis of randomized controlled trials. Five electronic databases (CINAHL, EMBASE, MEDLINE, PUBMED, and COCHRANE) were searched. Eligible trials included participants with primary osteoporosis and at least one vertebral fracture diagnosed on radiographs, with treatment that was non-surgical and non-pharmacological involving more than one session.
Results
Twenty randomized controlled trials were included with 2083 participants with osteoporotic vertebral fractures. Exercise, bracing, multimodal therapy, electrotherapy, and taping were investigated interventions. Meta-analyses provided low certainty evidence that exercise interventions compared to no exercise were effective in reducing pain in patients with osteoporotic vertebral fractures (mean difference (MD)= 1.01; 95% confidence interval (CI): 0.08, 1.93), and low certainty evidence that rigid bracing intervention compared with no bracing was effective in reducing pain in patients with osteoporotic vertebral fractures (MD= 2.61; 95%CI: 0.95, 4.27). Meta-analyses showed no differences in harms between exercise and no exercise groups. No health-related quality of life or activity improvements were demonstrated for exercise interventions, bracing, electrotherapy, or multimodal interventions.
Conclusions
Exercise and rigid bracing as management for patients with osteoporotic vertebral fractures may have a small benefit for pain without increasing risk of harm.
Trial registration
PROSPERO registration number CRD42012002936
Introduction
Vertebral fractures are a common consequence of osteoporosis. Annually, there are 400,000 osteoporotic vertebral fractures (OPVFs) occurring in the European Union 6 (United Kingdom, Italy, France, Germany, Spain, plus Sweden)1 and this number is expected to increase by 23% by the year 2030.1 Typically, OPVFs result in significant and persistent back pain, spinal deformity, and reduced mobility and quality of life.2, 3, 4 OPVFs also are a marker of poor bone health and predict future fractures, both vertebral and non-vertebral.5, 6 Lindsay et al5 reported that a single vertebral fracture is associated with a five-fold increase in further vertebral fractures. OPVFs are also a burden to the community with the mean cost of care for the 12-month period following an OPVF ranging from €1928 to €14,474 (approximately 13,156 BRL to 98,763 BRL).1
Surgical and pharmacological interventions commonly used for the management of OPVFs have limited efficacy and potential risk of harm. A recent Cochrane review7 reported moderate to high certainty evidence that vertebral augmentation, a percutaneous injection of bone cement under image guidance into a fractured vertebra for patients with OPVFs (acute or subacute), showed no important change for pain, quality of life, or disability when compared to sham treatments. The authors reported uncertainty regarding risk of this procedure, including risk of future fracture. Another systematic review showed very low certainty evidence that opioids and non-steroidal anti-inflammatory medications provide acute pain relief for people with OPVFs when compared to alternative medicine.8 Concerningly, opioids showed no significant effects for pain relief when compared to placebo, and were associated with more adverse events such as gastrointestinal disorders.8
In comparison to vertebral augmentation and analgesia or anti-inflammatory medication, non-surgical and non-pharmacological management is non-invasive and might be expected to result in less harm. Further, these interventions (e.g. exercise therapy, bracing) may address problems associated with OPVFs including pain and limited activity. Previous systematic reviews have shown very low certainty evidence that exercise interventions for people with OPVFs7, 8, 9 may have small benefits for pain, quality of life and physical performance and few adverse events. Rzewuska et al's10 systematic review demonstrated low certainty evidence for the use of spinal orthoses for managing pain and disability in patients with OPVFs in the medium-term and very low certainty evidence for the effectiveness of a rigid orthosis compared to a soft spinal orthosis in reducing pain in the short-term.
Currently, there is insufficient evidence about the benefits and harms of non-surgical and non-pharmacological interventions to guide clinicians, which may lead to variable and suboptimal care for patients with OPVFs. Previous systematic reviews have not been comprehensive in their inclusion of a range of non-surgical and non-pharmacological interventions for OPVFs and little emphasis has been given on synthesising the evidence on harms as well as benefits.7, 8, 9, 10 As literature searches in other reviews have not been updated since 2017 there is a need to consider new randomized controlled trials completed since.
This systematic review aims to evaluate the evidence from randomized controlled trials on the benefits and harms of non-surgical and non-pharmacological management of people with OPVFs compared with standard care (control); and, to compare the benefits and harms of non-surgical and non-pharmacological management of people with OPVFs compared with an alternative non-pharmacological, non-invasive intervention.
Methods
A systematic review and meta analyses were conducted following the PRISMA Statement.11 This systematic review was prospectively registered on the PROSPERO database (CRD42012002936).
Eligibility criteria
The trials were eligible if they were: randomized controlled trials; included participants with a diagnosis of primary osteoporosis and a vertebral fracture demonstrated on radiographs; the experimental group received non-pharmacological or non-surgical management of more than one session (e.g., strengthening, balance, or motor control exercise interventions, bracing, taping, electrotherapy) and the comparison group received standard care or an alternative intervention (e.g., soft brace compared to rigid brace); and if at least one outcome was reported at the conclusion of the intervention.
Search strategy
The electronic databases MEDLINE, EMBASE, CINAHL, PUBMED, and COCHRANE were searched until April 2021. Search strategies for each database were constructed using the concepts of population, intervention, and design. Population was defined as participants with primary osteoporosis and at least one vertebral fracture demonstrated on radiographs. Intervention was defined as a non-surgical or non-pharmacological intervention for OPVFs. The design was limited to randomized controlled trials. Within each concept, synonyms and MeSH terms were combined with the “OR” operator. The concepts were then combined with the “AND” operator (see Supplemental online material). Database searching was supplemented by checking reference lists of included trials and citation tracking.
Study selection
The first 50 titles and abstract were assessed by two reviewers independently to pilot inclusion and exclusion criteria. After confirming high levels of agreement, all titles and abstracts were assessed independently by two reviewers according to the eligibility criteria. Full copies of articles unable to be excluded by this process were obtained and again reviewed. Disagreements were resolved by discussion, and in one case a third reviewer was consulted to achieve consensus.
Data extraction
The following data were extracted: author, year and country of publication, characteristics of participants (sex, age); description of intervention and control; pain measures (visual analogue scale), activity measures, quality of life measures, adverse events and participant adherence to interventions, type of comparison, and studies included in the analysis. Data extraction was performed by one reviewer and checked by a second reviewer.
Risk of bias
The methodological quality of the trials was assessed by two reviewers independently using the Physiotherapy Evidence Database (PEDro). Any differences in assessment were resolved by discussion. The PEDro score has reported inter-rater reliability of moderate range [ICC= 0.68 (95%CI 0.57, 0.76)]12 and the use of a summed score out of 10 has been confirmed using Rasch analysis.13 Trials with a score of 6 or more were considered to be of high quality.14
Data analysis
The primary outcome of benefit was determined by the effect of the intervention on pain reduction, and the secondary outcome of benefit was determined by the effect of the intervention on activity and health-related quality of life. The primary outcome of harm was determined by the number of participants experiencing serious and non-serious adverse events. A serious adverse event was defined as the number of participants experiencing an event that was fatal, life threatening, requiring hospitalisation, and/or fractures, or as reported in the included trial as a serious event. A non-serious event was defined as any other adverse event.
For continuous outcomes (pain, activity, quality of life) the post-intervention means ± standard deviation (SD) were extracted. If a mean change score was reported, the post-intervention mean was calculated by adding the mean change to the baseline mean; and baseline SD was used as an estimate of the post intervention SD. Pain outcomes for individual trials were transformed to a common scale (0 to 10). For dichotomous outcomes (adverse events) the number of participants experiencing an adverse event or serious adverse event was recorded.
Meta-analysis was completed using a random effects model and expressed as mean differences (MD) for pain or standardised mean differences (SMD) for activity and quality of life, and relative risks for adverse events. Data were combined for meta-analysis using a minimum of two trials assessed as clinically homogeneous. Trials were considered clinically homogenous if there was a common intervention and outcome. Trial populations were homogenous based on the eligibility criteria. Data used for analysis were taken from assessments at completion of intervention. All analyses were conducted in Review Manager (RevMan) software (Version 5.3.5).15 The results from the trials not able to be combined into meta-analyses were reported in table and narrative form. Positive SMD values were used to indicate that the outcome was favourable to the intervention group. SMD values of < 0.2 indicated a small effect size, 0.2-0.5 a moderate effect size and > 0.8 a larger effect size.16
The GRADE approach was applied to each meta-analysis to assess certainty of evidence.17 This process involved downgrading from high to moderate to low to very low certainty evidence based on domains. Downgrading the evidence one level if: (1) for study limitations, the PEDro score was <6 for the majority (> 50%) of trials in the meta-analysis, (2) for inconsistency, there was greater than low levels of statistical heterogeneity between trials (I2≥ 25%),18 (3) for indirectness, more than 50% of the participants were outside the target group, (4) for imprecision, there were large confidence intervals, such that the lower band of the confidence interval of the estimate of effect could indicate little or no effect, while the upper band could indicate a large effect, (5) for publication bias, as indicated by funnel plot asymmetry on any meta-analysis with at least 10 trials.18 The certainty of evidence was downgraded more than one level based within one domain if there were very serious concerns (for example, for study limitations if the PEDro score was <6 for >75% of trials), or if there were serious concerns in more than one domain. Single randomized trials were considered inconsistent and imprecise, thereby providing low certainty evidence. This could be further downgraded to very low certainty evidence if there was also high risk of bias.19 The GRADE domains were applied by one researcher and checked by a second researcher.
Results
Study selection
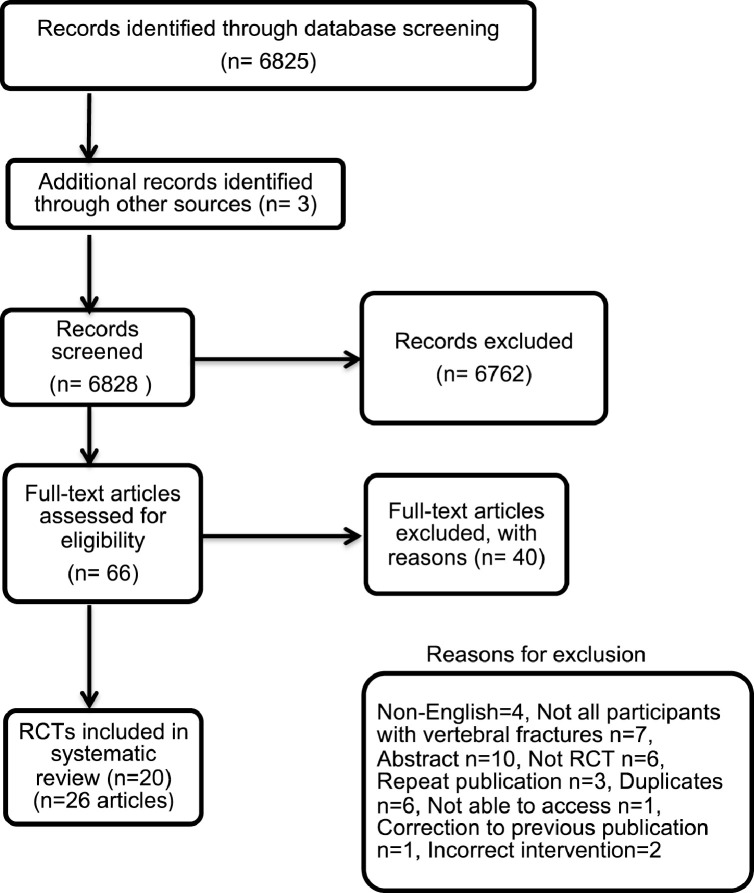
The database search yielded a total of 6,348 articles including duplicates. Forty-five articles were included for full text review and a total of 20 trials (reported in 26 articles) met the inclusion criteria (Fig. 1).
Figure 1.
PRISMA flow diagram.
Study characteristics
A total of 20 randomized controlled trials including 2,083 participants were included. The majority of participants were women (1,873, 89.9%). Participants were predominantly community dwelling, with a mean (SD) age of 72.8 ± 6.2 years. All trials were completed in countries classified as high or upper-middle income status (Table 1).
Table 1.
Trial characteristics.*
| Trial (Economy classification: High, upper-middle, middle, low)51 |
Participants (intervention) Number, N Mean ± SD age Sex, n (%) |
Participants (comparator) Number, N Mean ± SD age Sex, n (%) |
Setting | Intervention components | Dosage | Length of intervention | Comparator |
|---|---|---|---|---|---|---|---|
| Barker et al 201920 (UK) (High) |
N = 216 72.2 ± 8.4 years Female,185 (85.6%) |
N = 196 72.2 ± 8.4 years Female, 173 (88.7%) |
Clinic and home program | Exercise | Strength training intensity set at RPE level 3-4 45min session/week, 3-5/week |
6 sessions over 12 weeks Home program for 12-months |
No exercise |
| Bergland et al 201129 (Norway) (High) |
N = 47 70.8 ± 5.9 years Female, 47 (100%) |
N = 42 72.0 ± 5.8 years Female, 42 (100%) |
Clinic | Exercise | Biweekly 3-month program | No exercise | |
| Berstrom et al 200121 (Sweden) (High) |
N = 20 73.2 ± 8.9 years Female, 20 (100%) |
N = 16 74.1 ± 6.0 years Female, 16 (100%) |
Clinic | Exercise - strengthening Postural advice |
x30 progressive increase resistance | Biweekly 4-month program | Not stated |
| Cergerl et al 201923 (Turkey) (Upper-middle) |
Supervised exercise N = 20 58.9 ± 4.7 years Female, 20 (100%) |
N = 20 59.65 ± 6.45 years Female, 20 (100%) |
Clinic or home program | Exercise | 3 × 8 reps for first 2 weeks. x3 × 10 reps, progress to x3 × 12 reps |
6 weeks | |
| Evstigneeva et al 201622 (Canada) (High) |
N = 40 70.7 ± 8.1 years Female, 40 (100%) |
N = 38 67.6 ± 7.0 years Female, 38 (100%) |
Clinic | Exercise |
40-minute program twice weekly | 12 months | No exercise |
| Giangregorio et al 201827 (Australia Canada) (High) |
N = 71 76 ± 6.4 years Female,71 (100%) |
N = 70 77 ± 7.3 years Female,70 (100%) |
Home program Supported by 6 home visits by physical therapist |
Exercise | 5-8 exercises 2 sets of 8-10 reps** or isometric holds of 3-5 seconds |
12 months | No exercise |
| Gold et al 200426 (USA) (High) |
N = 94 80.2 ± 4.8 years Female, 94 (100%) |
N = 91 82.0 ± 6.2 years Female, 91 (100%) |
Clinic | Exercise Education |
Exercise 3x week for 6 months Coping class x2 week for 6 months |
6 months, cross over with control | No exercise |
| Grahn et al 202032 (Sweden) (High) |
N = 10 71.3 ± 5.3 years Female, 9 (90%) |
N = 10 72.4 ± 6.5 years Female, 10 (100%) |
Fitness Centre and home exercise program | Yoga/mindfulness | Hour class weekly: 30 min yoga/30 min mindfulness training Daily home exercise 30-minutes duration |
10 weeks | No exercise |
| Karaksidou et al 201325 (Greece) (High) |
N = 10 67.6 ± 6.41 years Female, 10 (100%) |
N = 10 69.3 ± 4.4 years Female, 10 (100%) |
Clinic | Exercise | x3 week 1-hour one-to-one sessions with physical therapist |
13-week program | No exercise |
| Malmros et al 199824 (Denmark) (High) |
N = 27 65 years (25:75 percentile 62:70) |
N = 25 68 years (25:75 percentile 64:71) |
Clinic and home exercise program | Exercise | 60-minute twice weekly physical therapy-led sessions | 10-week program | No exercise |
| Papaioannou et al 200228 (Canada) (High) |
N = 37 71.6 ± 7.3 years Female, 37 (100%) |
N = 37 72.2 ± 7.98 years Female, 37 (100%) |
Home program | Exercise | 60-minutes x3 per week | 12 months | No exercise |
| Stranghelle et al (2019)30 (Norway) (High) |
N = 76 74.6 ± 6.1 years Female, 76 (100%) |
N = 73 73.7 ± 5.6 years Female, 73, (100%) |
Clinic | Exercise |
One session, twice weekly, physical therapist led sessions | 12 weeks |
No exercise |
| Kato et al 201937 (Japan) (High) |
N = 141 76 ± 5.2 years |
N = 143 75.5 ± 5.4 years |
Brace - rigid | Wore brace at all times | 12 weeks | Soft brace | |
| Kim et al 201936 (Korea) (High) |
Soft braceN = 20 66.8 ± 11.0 years Female, 14 (70%) Rigid braceN = 20 71.8 ± 8.0 years Female, 14 (70%) |
N = 20 72.2 ± 10.4 Female, 13 (65%) |
Brace - rigid or soft | Worn at all times except when lying down | 8 weeks | No brace | |
| Li et al 201535 Hong Kong (High) |
N = 27 82 ± 8.3 years Female, 27 (100%) |
N = 24 81 ± 6.6 years Female, 24 (100%) |
Brace – rigid or Spinomed | Week 1:24 hours per day Weeks 2-3: 3 hours daily |
3 weeks | Soft lumbar orthosis | |
| Pfeifer et al 201134 (Germany) (High) |
Group A N = 36 72.8 ± 7.1 years Female, 36 (100%) Group B N = 36 72.3 ± 6.7 years Female, 36 (100%) |
N = 36 69.7 ± 8.9 years Female, 36 (100%) |
Brace – Rigid or soft | 2 hours daily | 6 months | No brace | |
| Barker et al 201943 (UK) (High) |
N = 203 72.4 ± 9.3 years Female, 173 (85.6%) |
N = 196 72.2 ± 8.4 years Female, 173 (88.7%) |
Clinic and home program | Multimodal therapy | 6 sessions over 12 weeks Home program for 12-months |
12 months | No therapy |
| Bennell et al 201040 (Australia) (High) |
N = 11 66.2 ± 8.0 years Female, 7 (63.6%) |
N = 9 66.3 ± 11.8 years Female 7 (88.7%) |
Clinic and home program | Multimodal therapy | 45-minute session Standardised treatment, with individualised dosage |
10 weekly sessions |
No intervention |
| Palmer et al 201844 (UK) (High) |
N = 13 73.6 ± 5.9 years Female, 13 (100%) |
N = 12 74.6 ± 7.0 years Female, 8 (67%) |
Taping spine | Daily length of time of application chosen by patient | 4 weeks | Usual care | |
| Rossini et al 200938 (Italy) (High) |
N = N = 20 73.8 ± 7.4 years Female, 20 (100%) |
N = 21 71.7 ± 7.2 years Female, 21 (100%) |
Home program | Electrotherapy | 10 hours per day | 2 months | Sham therapy |
| Zambito et al 200739 (Italy) (High) |
Group 1N = 35 70.8 ± 7.4 years Female, 35 (100%) Group 2 N = 35 70.5 ± 7.6 years Female, 35 (100%) |
N = 35 70.5 ± 8.3 years Female, 35 (100%) |
Clinic |
Group 1Electrotherapy interferential therapy, trunk flexion-extension stretching Group 2 Electrotherapy - horizontal therapy, trunk flexion-extension stretching |
30-40min, 5 days per week | 2 weeks | Sham horizontal therapy |
There were four categories of intervention: exercise,20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 bracing,34, 35, 36, 37 electrotherapy,38, 39 and multimodal therapy including manual therapy, postural advice, exercise, and taping.20,40
Adherence to exercise interventions conducted in clinic settings ranged from “fully compliant” 23, 24, 25 to a mean attendance of 58% of sessions26 (Supplemental online material). Adherence to exercise interventions conducted in home settings (unsupervised) ranged between 62% to 66% of prescribed sessions in trials that reported data27, 28 and undefined in one trial.23 Exercise trials with longer intervention periods ranging from 6 to 12 months exhibited lower adherence rates compared to trials with shorter intervention periods. For example, in one study 66% of participants attended 60% of scheduled exercise classes, with an observed reduction in this rate over the 12-month intervention.27 In comparison, an adherence rate of 100% was reported for two trials with shorter interventions of six and 10 weeks.23, 24 Adherence to electrotherapy interventions was high with 100% of sessions attended39 and 9.2 hours received of the prescribed 10 hours of electrical stimulation per day.38 Reporting of adherence for bracing trials was highly variable, ranging from no data provided34, 35 to 64% of participants wearing a rigid brace and 63% of participants wearing a soft brace for >12 hours at 3-month follow-up.37
Risk of bias in individual studies
Sixteen trials were ranked as higher quality (≥6/10). Most adhered items on the PEDro scale included eligibility criteria, random allocation, and provision of both point measures and measures of variability for at least one key outcome. Eleven trials did not fulfil the criterion of concealed allocation increasing risk of selection bias, and none of the trials blinded the participants or therapists, therefore increasing the risk of performance bias. Six trials reported that more than 15% of participants withdrew from the study, increasing the risk of attrition bias. One individual electrotherapy trial39 included a sham treatment group; however the authors did not explicitly describe blinding of the participants (Supplemental online material).
Synthesis of the results
Effect of exercise interventions versus no exercise for the management of OPVF
Meta-analyses of seven trials22, 23,25, 26,29, 30, 31 with 688 participants provided low certainty evidence that exercise interventions compared with no exercise were effective in reducing the primary outcome of pain in patients with OPVFs (MD = 1.01 units, 95% CI: 0.08,1.93)(Fig. 2A) (Table 2). Due to a high I2 value (90%), a sensitivity analysis compared exercise and no exercise for six trials with a small increase in effect size (MD = 1.25 units, 95% CI: 0.23, 2.27) but I2 remained high. This analysis was performed by omitting one trial29 as the exercise intervention focussed on balance exercise in comparison to strengthening interventions in the other six trials.
Figure 2.
(A) Mean difference (95% CI) of effect of exercise vs. standard care on pain (B) Standardized mean difference (95% CI) of effect of exercise versus standard care on quality of life (C) Standardized mean difference (95% CI) of effect of exercise versus standard care on activity (D) Risk ratio (95% CI) of serious adverse events for exercise versus standard care (E) Risk ratio (95% CI) for non-serious adverse events for exercise versus standard care (F) Mean difference (95% CI) of effect of rigid brace versus no brace on pain.
Table 2.
Summary of findings and certainty of evidence GRADE for Exercise versus no exercise for OPVF.
| Certainty of Evidence |
No. of Participants |
Effect (95% CI) | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication bias | Outcome | Exercise | Control | ||
| 7 | RCT | Not serious | Serious | Not serious | Serious | Undetected | Pain intensity | 349 | 339 | MD = 1.01 (0.08, 1.93) |
Lowab |
| 8 | RCT | Not serious | Serious | Not serious | Serious | Undetected | QOL | 529 | 516 | SMD = 0.26 (-0.11, 0.63) |
Lowab |
| 7 | RCT | Not serious | Serious | Not serious | Serious | Undetected | Activity | 416 | 407 | SMD = 0.11 (-0.36, 0.58) |
Lowab |
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | SAE | 111 | 108 | RR = 0.99 (0.38, 2.59) |
Lowac |
| 2 | RCT | Not serious | Not serious | Not serious | Serious | Undetected | NSAE | 67 | 58 | RR = 0.96 (0.55, 1.87) |
Moderatec |
MD, mean difference; NSAE, non-serious adverse event; QOL, quality of life; RCT, randomized controlled trial; RR, relative risk; SAE, serious adverse event; SMD, standardized mean difference.
Downgraded due to inconsistency there was statistical heterogeneity(I2 values > 25%) with the studies showing differing estimates of the effect size.
Downgraded due to imprecision – there were very large confidence intervals with the higher end indicating appreciable benefit and the lower end indicating either a little effect or worse outcome.
Downgraded due to imprecision – there were very large confidence intervals due to a small number of adverse events.
Meta-analysis of two trials22,27 with 219 participants provided low certainty evidence of no difference between exercise and no exercise groups regarding the primary outcome of risk of serious adverse events (RR = 0.99, 95%CI 0.38, 2.59) (Fig. 2 E). Meta-analysis of two trials21,33 with 125 participants showed moderate certainty evidence of no difference between exercise and no exercise groups regarding risk of non-serious adverse events (RR = 0.96, 95%CI: 0.5, 1.87) (Fig. 2 F). Eleven exercise trials20, 21, 22,24, 25, 26, 27, 28,30,33,40 with 1460 participants, reported adverse events ranging from two events25 to 184 events.27 One trial26 reported serious adverse events of two fractures related to the exercise intervention. Seven trials reported non-serious adverse events related to the interventions such as knee pain, neck pain, adverse skin reactions to tape, breathing difficulties.20,22,25, 26, 27,33,40
Meta-analyses provided low certainty evidence of no differences between exercise and no exercise regarding the secondary outcomes of health-related quality of life and activity (Fig. 2 B and C) (Table 2). Other individual trials could not be included, as they did not assess these outcomes.21-22,27 Two trials involving a total of 553 participants provided low certainty evidence of similar costs and health utilisation for participants in exercise and comparison groups.41, 42
Effect of bracing versus no bracing for the management of OPVFs
Meta-analyses of two trials34,36 with 100 participants provided low certainty evidence that rigid bracing interventions compared with no bracing were effective in reducing the primary outcome of pain in patients with OPVFs (MD = 2.61 units, 95%CI: 0.95, 4.27) (Figure 2 F) (Table 3).
Table 3.
Summary of findings and certainty of evidence GRADE for Bracing versus no brace for OPVF.
| Certainty of Evidence |
No. of Participants |
Effect (95%CI) | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication bias | Outcome | Brace | No brace | ||
| Rigid brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | Pain intensity | 50 | 50 | MD = 2.61 (0.95, 4.27) |
Lowab |
| Soft brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | Pain intensity | 49 | 50 | MD = 2.39 (-0.45, 5.23) |
Lowab |
| Rigid brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | QOL | 50 | 50 | SMD = -0.55 (-1.43, 0.33) |
Lowab |
| Soft brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | QOL | 49 | 50 | SMD = -0.49 (-1.76, 0.78) |
Lowab |
| Rigid brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Not serious | Not serious | Serious | Undetected | Activity | 50 | 50 | SMD = -0.13 (-0.54, 0.28) |
Moderateb |
| Soft brace vs no brace | |||||||||||
| 2 | RCT | Not serious | Serious | Not serious | Serious | Undetected | Activity | 49 | 50 | SMD = 0.68 (-0.84, 2.19) |
Lowab |
MD, mean difference; QOL, quality of life; RCT, randomized controlled trial; SMD, standardized mean difference.
Downgraded due to inconsistency – there was statistical heterogeneity (I2 values > 25%) with the studies showing differing estimates of the effect size.
Downgraded due to imprecision – there were very large confidence intervals with the higher end indicating appreciable benefit and the lower end indicating either a little effect or worse outcome.
Three bracing trials with 452 participants reported adverse events.34,36, 37 Serious adverse events included vertebral fractures (n = 16, no significant difference rigid versus soft braces),37 and death unrelated to intervention.36 Non-serious adverse events included pain and discomfort (n = 5).34
Meta-analyses provided low to moderate certainty evidence of no differences between rigid bracing interventions compared with no intervention regarding the secondary outcomes of quality of life or activity (Table 3). Meta-analysis of trials34, 36 investigating soft bracing compared with no bracing provided low certainty evidence of no differences in reducing pain, improving quality of life, or activity. An individual trial could not be included, as it did not assess these outcomes, or provided sufficient data.37
Effect of rigid bracing versus soft bracing for the management of OPVFs
Meta-analyses of four trials34, 35, 36, 37 with 413 participants provided moderate certainty evidence that rigid bracing in comparison to soft bracing interventions showed no difference in pain (MD = -0.10 units, 95%CI: -0.55, 0.35), and low certainty evidence of no difference in activity level (SMD = 0.19, 95%CI: -0.20, 0.58). Meta-analyses of three trials34,36, 37 with 362 participants provided moderate certainty evidence that rigid bracing in comparison to soft bracing interventions showed no difference in quality of life (SMD = -0.09, 95%CI: -0.30, 0.11) in patients with OPVFs.
Effect of electrotherapy versus control (sham) for the management of OPVFs
Individual trials could not be combined in meta-analyses for electrotherapy due to unavailable data and clinical heterogeneity. One trial38 with 41 participants provided very low certainty evidence of no difference in quality of life measures (SMD = 0.27, 95% CI: -0.35, 0.89) compared to sham electrotherapy.
One trial38 reported nine adverse events, five occurred in the sham group and four in the intervention group.
Effect of multimodal therapy and taping versus standard care for the management of OPVFs
One trial40 of multimodal therapy comprising manual therapy, taping, and education compared to usual care with 20 participants demonstrated low certainty evidence of reduced pain at rest (MD = -2.0 units, 95% CI: -3.8, -0.2) in favour of the intervention group. Changes were also demonstrated for measures of quality of life and activity, in favour of the intervention group. One low quality trial43 of taping of the lumbar spine compared to standard care demonstrated non-significant findings for pain at rest (MD = 0.25, 95% CI: -1.75, 2.25) and quality of life (SMD = 0.67, 95% CI: -0.18, 1.47), and cutaneous reaction to tape in three participants was reported.
Discussion
Meta-analyses22, 23,25, 26,29, 30, 31 provided low certainty evidence that exercise interventions compared to no exercise were effective in reducing pain in people with OPVFs. Meta-analyses34,36 provided low certainty evidence that rigid bracing intervention compared with no bracing was effective in reducing pain in patients with OPVFs. No health-related quality of life or activity improvements were demonstrated for exercise interventions, bracing, electrotherapy, or multimodal interventions. Meta-analyses showed low to moderate certainty evidence of no differences in harms comparing exercise and no exercise groups. Our review includes six trials not included in previous reviews and systematically evaluated the effect of non-surgical and non-pharmacological management of OPVFs on harms as well as benefits.
One explanation for why exercise and bracing reduced pain could be both these interventions reduced loading on the spine. A common component of the programs included back extension strengthening or postural control, which reduces flexion and loading on the spine. Takahashi et al.44 found increased load during trunk flexion in healthy adults. Rohlmann et al.45 demonstrated high forces in spinal segments in activities of daily living that involved moving the center of mass anteriorly for example upper body flexion, lifting, or stair walking in patients with instrumented vertebral body replacements. Interestingly, walking was ranked as having the lowest resultant force (N). Pain in people with OPVFs is typically increased during loading activities such as bending and eased when lying down.46
While the results on outcomes for exercise and bracing appear promising for reducing pain, their clinical significance requires further consideration. For example, effect of exercise versus no exercise on pain, (MD = 1.01 units, 95% CI: 0.08, 1.93), is less than the minimum clinically important difference of 1.8 units.47 The pain outcome for bracing (MD = 2.61 units, 95%CI: 0.95, 4.27) exceeds the minimum clinically important difference; however, the lower band of the confidence interval is less than 1.8 units suggesting there remain some uncertainty about the clinical significance of the effect of rigid bracing on pain reduction for people with OPVFs. While there may be small benefits for pain, there was not a change in activity level or quality of life from exercise, bracing, or multimodal interventions. One possible explanation was that the small reduction in pain may not have been large enough to elicit a change in activity level or quality of life.
Even though the effects on pain may be relatively small and the clinical significance questioned, the effects of exercise and bracing compared to no exercise or brace respectively is consistent with management of other back conditions. A recent meta-analysis focused on exercise compared with no treatment/usual care in participants with persistent non-specific low back pain, demonstrated that exercise therapy on average reduced pain by 1.1 units on 0-10 visual analogue scale (95% CI: 0.74, 1.41),48 which is of similar magnitude to our results. Also, these results may be similar to the effects of commonly prescribed medications. One trial demonstrated significantly lower pain intensity in a group receiving tramadol (100 mg/day) compared to a control group allowed to receive a Chinese medicine for pain relief (0.32 g ‘as needed’), at both immediate- (SMD = -1.23, 95% CI: -2.42, -0.05) and short-term follow-ups (SMD = -1.58, 95% CI: -2.83, -0.33).10
The results of this review provide some support for prescribing exercise programs for people with OPVFs as they may have a small effect on pain and avert a small risk of harm. These results add to the uncertain evidence that exercise programs may also have a role in preventing fragility fractures associated with osteoporosis such as OPVFs.49 It might provide support for exercise as a first-line intervention for management of OPVFs before considering common treatments with questionable efficacy and known harms such as analgesia. However, this review has not considered cost effectiveness. Most programs involved supervision which may increase costs and adherence was as low as 58% completion of prescribed sessions. However, our preliminary data suggest the costs of exercise interventions were similar to standard care.41, 42 A recent paper by Ferreira et al.,50 found that people with low back pain prefer brief low-cost home-based programs. Perhaps a simple low-cost, less resource-intense intervention for people with OPVFs that retains the important components (e.g. load reduction with relative extension and extensor muscle activation) and therefore may achieve the key benefits may be worthwhile. For example, a walking program might achieve the same benefits and also achieve better adherence. None of the exercise trials in this review included a walking program and this may be an area of further research.
This review followed the PRISMA reporting guidelines for systematic reviews and meta-analyses. All the trials included are randomized controlled trials increasing confidence in results, as findings are less subject to bias. The GRADE approach was applied to meta-analyses determining level of certainty in results.
A limitation of our search strategy was that we used a database filter to limit the search to randomized controlled trials rather than a validated filter such as those used in Cochrane reviews. This may have increased the risk of missing potentially relevant trials. However, the small number of additional trials identified through citation tracking suggests our search strategy was sufficiently sensitive. Only trials reported in English were included in our search, which is a limitation of this review. Computation of results for meta-analyses was immediately post intervention only; longer-term results have not been presented in this review. Related to this, each trial included employed variable length interventions, and this also could be considered a limitation. Finally, the fact that all trials were completed in countries classified as high or upper-middle income status means results may not be generalisable to countries of lower socio-economic status.
Conclusion
There is low certainty evidence that exercise interventions and rigid bracing can reduce pain in people with OPFVs without increasing risk of harm. No benefit for health-related quality of life and activity measures were demonstrated for exercise interventions, bracing, or multimodal interventions. Randomized trials testing the effectiveness of simple low-cost exercise interventions for example walking are needed.
Conflict of interest
The authors have no conflict of interest to declare.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.bjpt.2021.100383.
Appendix. Supplementary materials
References
- 1.Borgström F, Karlsson L, Ortsäter G, et al. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos. 2020;15:1–21. doi: 10.1007/s11657-020-0706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silverman S. The clinical consequences of vertebral compression fracture. Bone. 1992;13:S27–S31. doi: 10.1016/8756-3282(92)90193-z. [DOI] [PubMed] [Google Scholar]
- 3.Svensson H, Olofsson EH, Karlsson J, Hansson T, Olsson L-E. A painful, never ending story: older women's experiences of living with an osteoporotic vertebral compression fracture. Osteoporos Int. 2016;27(5):1729–1736. doi: 10.1007/s00198-015-3445-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burger H, Van Daele P, Grashuis K, et al. Vertebral deformities and functional impairment in men and women. J of Bone and Min Res. 1997;12(1):152–157. doi: 10.1359/jbmr.1997.12.1.152. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(3):320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 6.Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297(4):387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 7.Gibbs JC, MacIntyre NJ, Ponzano M, et al. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2019;(7) doi: 10.1002/14651858.CD008618.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dusdal K, Grundmanis J, Luttin K, et al. Effects of therapeutic exercise for persons with osteoporotic vertebral fractures: a systematic review. Osteoporos Int. 2011;22(3):755–769. doi: 10.1007/s00198-010-1497-6. [DOI] [PubMed] [Google Scholar]
- 9.Svensson H, Olsson L-E, Hansson T, Karlsson J, Hansson-Olofsson E. The effects of person-centered or other supportive interventions in older women with osteoporotic vertebral compression fractures—a systematic review of the literature. Osteoporos Int. 2017;28(9):2521–2540. doi: 10.1007/s00198-017-4099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J. 2015;24(4):702–714. doi: 10.1007/s00586-015-3821-5. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 13.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. doi: 10.1016/s0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 14.Wallis JA, Taylor NF. Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery–a systematic review and meta-analysis. Osteoarthr Cartil. 2011;19(12):1381–1395. doi: 10.1016/j.joca.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Review Manager (Revman) [computer program] The Nordic Cochrane Centre; Denmark: 2014. Version Version 5.3. Copenhagen. [Google Scholar]
- 16.Cohen J. Academic press; 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 17.Grade Working Group. https://www.gradeworkinggroup.org/. Published 2020. Accessed.
- 18.Higgins JP. September 2020. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition.www.training.cochrane.org/handbook Published. Accessed. [Google Scholar]
- 19.Gluppe S, Engh ME, Bø K. What is the evidence for abdominal and pelvic floor muscle training to treat diastasis recti abdominis postpartum? A systematic review with meta-analysis. Braz J Phys Ther. 2021 doi: 10.1016/j.bjpt.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barker K, Newman M, Stallard N, et al. Physiotherapy rehabilitation for osteoporotic vertebral fracture—a randomised controlled trial and economic evaluation (PROVE trial) Osteoporos Int. 2020;31(2):277–289. doi: 10.1007/s00198-019-05133-0. [DOI] [PubMed] [Google Scholar]
- 21.Bergström I, Bergström K, Kronhed A-CG, Karlsson S, Brinck J. Back extensor training increases muscle strength in postmenopausal women with osteoporosis, kyphosis and vertebral fractures. Adv Physiother. 2011;13(3):110–117. [Google Scholar]
- 22.Evstigneeva L, Lesnyak O, Bultink I, et al. Effect of twelve-month physical exercise program on patients with osteoporotic vertebral fractures: a randomized, controlled trial. Osteoporos Int. 2016;27(8):2515–2524. doi: 10.1007/s00198-016-3560-4. [DOI] [PubMed] [Google Scholar]
- 23.Çergel Y, Topuz O, Alkan H, Sarsan A, Akkoyunlu NS. The effects of short-term back extensor strength training in postmenopausal osteoporotic women with vertebral fractures: comparison of supervised and home exercise program. Arch Osteoporos. 2019;14(1):82. doi: 10.1007/s11657-019-0632-z. [DOI] [PubMed] [Google Scholar]
- 24.Malmros B, Mortensen L, Jensen MB, Charles P. Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporos Int. 1998;8(3):215–221. doi: 10.1007/s001980050057. [DOI] [PubMed] [Google Scholar]
- 25.Karakasidou P, Skordilis E, Dontas I, Papaioannou N, Lyritis G. Motor control exercise can reduce pain and kyphosis in osteoporotic women with vertebral fractures: A randomised controlled trial. Rev Clin Pharmacol Pharmacokinet Int Ed. 2013;27:95–106. [Google Scholar]
- 26.Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW. Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Am Geriatr Soc. 2004;52(9):1471–1478. doi: 10.1111/j.1532-5415.2004.52409.x. [DOI] [PubMed] [Google Scholar]
- 27.Giangregorio LM, Gibbs JC, Templeton JA, et al. Build better bones with exercise (B3E pilot trial): results of a feasibility study of a multicenter randomized controlled trial of 12 months of home exercise in older women with vertebral fracture. Osteoporos Int. 2018;29(11):2545–2556. doi: 10.1007/s00198-018-4652-0. [DOI] [PubMed] [Google Scholar]
- 28.Papaioannou A, Adachi J, Winegard K, et al. Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int. 2003;14(8):677–682. doi: 10.1007/s00198-003-1423-2. [DOI] [PubMed] [Google Scholar]
- 29.Bergland A, Thorsen H, Kåresen R. Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int. 2011;22(6):1863–1871. doi: 10.1007/s00198-010-1435-7. [DOI] [PubMed] [Google Scholar]
- 30.Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Skelton DA, Bergland A. Effects of a resistance and balance exercise programme on physical fitness, health-related quality of life and fear of falling in older women with osteoporosis and vertebral fracture: a randomized controlled trial. Osteoporos Int. 2020;31(6):1069–1078. doi: 10.1007/s00198-019-05256-4. [DOI] [PubMed] [Google Scholar]
- 31.Gibbs JC, McArthur C, Wark JD, et al. The effects of home exercise in older women with vertebral fractures: a pilot randomized controlled Trial. Phys Ther. 2020;100(4):662–676. doi: 10.1093/ptj/pzz188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grahn Kronhed A-C, Enthoven P, Spångeus A, Willerton C. Mindfulness and modified medical yoga as intervention in older women with osteoporotic vertebral fracture. J Complement Alt Med. 2020;36(7):610–619. doi: 10.1089/acm.2019.0450. [DOI] [PubMed] [Google Scholar]
- 33.Olsen C, Bergland A. The effect of exercise and education on fear of falling in elderly women with osteoporosis and a history of vertebral fracture: results of a randomized controlled trial. Osteoporos Int. 2014;25(8):2017–2025. doi: 10.1007/s00198-014-2724-3. [DOI] [PubMed] [Google Scholar]
- 34.Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011;90(10):805–815. doi: 10.1097/PHM.0b013e31821f6df3. [DOI] [PubMed] [Google Scholar]
- 35.Li M, Law S-w, Cheng J, Kee H-m, Wong MS. A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int. 2015;39(4):270–276. doi: 10.1177/0309364614528204. [DOI] [PubMed] [Google Scholar]
- 36.Kim H-J, Yi J-M, Cho H-G, et al. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. JBJS. 2014;96(23):1959–1966. doi: 10.2106/JBJS.N.00187. [DOI] [PubMed] [Google Scholar]
- 37.Kato T, Inose H, Ichimura S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med. 2019;8(2):198. doi: 10.3390/jcm8020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rossini M, Viapiana O, Gatti D, de Terlizzi F, Adami S. Capacitively coupled electric field for pain relief in patients with vertebral fractures and chronic pain. Clin Orthop Relat Res. 2010;468(3):735–740. doi: 10.1007/s11999-009-1088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zambito A, Bianchini D, Gatti D, Rossini M, Adami S, Viapiana O. Interferential and horizontal therapies in chronic low back pain due to multiple vertebral fractures: a randomized, double blind, clinical study. Osteoporos Int. 2007;18(11):1541–1545. doi: 10.1007/s00198-007-0391-3. [DOI] [PubMed] [Google Scholar]
- 40.Bennell KL, Matthews B, Greig A, et al. Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC musculoskelet Disord. 2010;11(1):36. doi: 10.1186/1471-2474-11-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hassan S, Seung S, Clark R, et al. Describing the resource utilisation and costs associated withvertebral fractures: the Build Better Bones with Exercise (B3E) Pilot Trial. Osteoporos Int. 2020;31(6):1115–1123. doi: 10.1007/s00198-020-05387-z. [DOI] [PubMed] [Google Scholar]
- 42.Barker KL, Newman M, Stallard N, et al. Exercise or manual physiotherapy compared with a single session of physiotherapy for osteoporotic vertebral fracture: three-arm PROVE RCT. Health Technol Assess (Winchester, England) 2019;23(44):1–318. doi: 10.3310/hta23440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Palmer S, Barnett S, Cramp M, Berry A, Thomas A, Clark EM. Effects of postural taping on pain, function and quality of life following osteoporotic vertebral fractures—A feasibility trial. Musculoskeletal Care. 2018;16(3):345–352. doi: 10.1002/msc.1350. [DOI] [PubMed] [Google Scholar]
- 44.Takahashi I, Kikuchi S-i, Sato K, Sato N. Mechanical load of the lumbar spine during forward bending motion of the trunk–a biomechanical study. Spine. 2006;31(1):18–23. doi: 10.1097/01.brs.0000192636.69129.fb. [DOI] [PubMed] [Google Scholar]
- 45.Rohlmann A, Pohl D, Bender A, et al. Activities of everyday life with high spinal loads. PloS One. 2014;9(5):e98510. doi: 10.1371/journal.pone.0098510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong CC, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013;6:205. doi: 10.2147/JMDH.S31659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bellamy N, Carette S, Ford P, et al. Osteoarthritis antirheumatic drug trials. III. Setting the delta for clinical trials–results of a consensus development (Delphi) exercise. J Rheumatol. 1992;19(3):451–457. [PubMed] [Google Scholar]
- 48.Hayden JA, Wilson MN, Stewart S, et al. Exercise treatment effect modifiers in persistent low back pain: an individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med. 2020;54(21):1277–1278. doi: 10.1136/bjsports-2019-101205. [DOI] [PubMed] [Google Scholar]
- 49.Daly RM, Dalla Via J, Duckham RL, Fraser SF, Helge EW. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther. 2019;23(2):170–180. doi: 10.1016/j.bjpt.2018.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ferreira GE, Howard K, Zadro JR, O'Keeffe M, Lin C-WC, Maher CG. People considering exercise to prevent low back pain recurrence prefer exercise programs that differ from programs known to be effective: a discrete choice experiment. J Physiother. 2020;66(4):249–255. doi: 10.1016/j.jphys.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 51.TheWorldBank. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Published 2021. Accessed.
- 52.Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Skelton DA, Bergland A. Physical fitness in older women with osteoporosis and vertebral fracture after a resistance and balance exercise programme: 3-month post-intervention follow-up of a randomised controlled trial. BMC Musculoskel Disord. 2020;21(1):1–11. doi: 10.1186/s12891-020-03495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.