Abstract
The unique or specific implant-related complication of dual-mobility total hip arthroplasty (DM-THA) is intraprosthetic dislocation (IPD), and different mechanisms of IPD have been proposed. Early IPD or IPD without polyethylene wear has been reported in modern DM-THA designs. We report the first case of early IPD in Thailand that occurred after attempted closed reduction of DM-THA.
Keywords: Hip Dislocation, Total hip arthroplasty, Dual mobility, Intra-prosthetic dissociation
Introduction
The use of a dual-mobility (DM) bearing in total hip arthroplasty was first developed and introduced by Gilles Bousquet and Andre Rambert in France in 1974 [1]. This bearing design combines small articulation to minimize wear with large articulation to prevent instability. Although Bousquet and Rambert’s DM bearing design was shown to have good long-term survivorship and that it is effective for preventing instability after total hip arthroplasty (THA) [2], intraprosthetic dislocation (IPD) remains a potentially serious complication.
IPD is defined as the separation of the femoral head from the polyethylene (PE) liner. In early DM bearing designs, the major cause of IPD was related to PE wear. The etiologies of PE wear included poor quality of ultra-high-molecular-weight PE and impingement caused by poorly designed femoral necks (such as nonround, larger-stem neck, rough neck surface, and skirted neck) [[2], [3], [4]]. Modern DM bearing designs have been modified to address these shortcomings, and these improvements have lowered the IPD rate [5,6]. However, IPD can occur in another setting from extrinsic causes. Here, we report the first case in Thailand of early IPD after an attempted closed reduction in modern DM-THA.
Case history
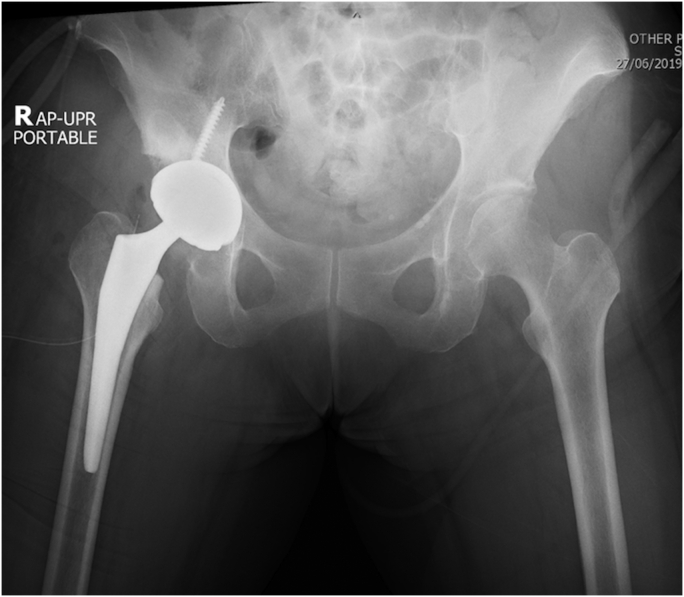
A 61-year-old Thai woman (weight 58 kg; height 160 cm; body mass index 22.6 kg/m2) had progressive left groin pain for 1 year. She was admitted to the hospital with a diagnosis of developmental dysplastic hip and secondary osteoarthritis of the left hip (Fig. 1). She also had a history of bipolar disorder with fluctuated psychotic features. After discussion with the patient and her relatives, we decided to perform THA. During the operation, the patient was placed in the right lateral decubitus position after administration of regional anesthesia. A cementless DM-THA was performed via the posterolateral approach. A prosthesis with the following features was used: 50-mm-diameter Trident acetabular cup with modular dual mobility (MDM X3), size 3 extended-offset Accolade II femoral stem, 22.2-mm-diameter femoral head with +4-mm neck length, and 38-mm-diameter PE liner (Stryker Corporation, Kalamazoo, MI). The operative time was 80 minutes. A postoperative radiograph of both hips is shown in Figure 2. No complications occurred during her hospital admission.
Figure 1.
Preoperative radiograph.
Figure 2.
Postoperative radiograph.
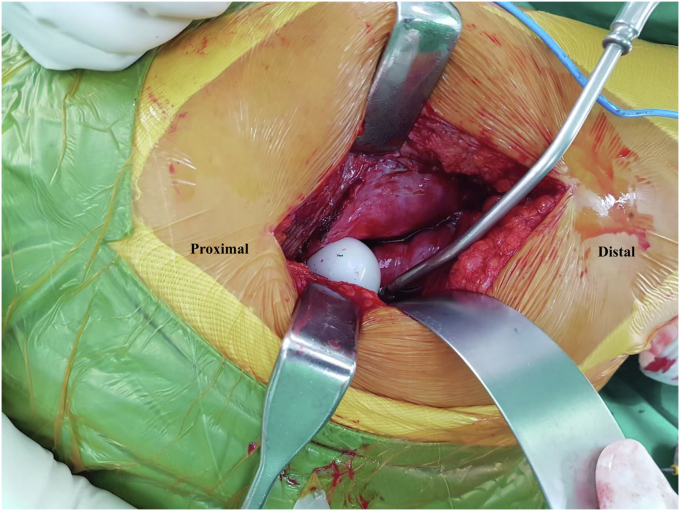
At 3 months after surgery, posterior dislocation of the DM-THA occurred due to a fall. Closed reduction under general anesthesia was successfully performed. Posterior dislocation of DM-THA then occurred a second time at 4 months after index DM-THA. The mechanism of injury was leaning forward (hyperflexion of hip) without falling. The shadow of PE liner was seen around the dislocated femoral head (Fig. 3). During the second closed reduction under general anesthesia, eccentric position of the femoral head was detected by fluoroscopy (Fig. 4). Open reduction and revision of the MDM was then performed the next day. During the operation, the PE liner was found to be dissociated and located under the gluteus maximus muscle (Fig. 5). No malposition of the femoral or acetabular components was observed. An +8-mm-long neck with skirt was inserted instead to improve soft-tissue tension and stability of the hip. A postrevision radiograph is shown in Figure 6. The revision procedure was successful, and no subsequent dislocations have occurred within the 2-year follow-up after revision surgery. The patient’s informed consent was obtained for print and electronic publication of this case report.
Figure 3.
Radiograph of second posterior dislocation of dual mobility-total hip arthroplasty. Arrowhead signs show the shadow of polyethylene liner around the femoral head.
Figure 4.
Postreduction intraoperative fluoroscopy showing eccentric position of femoral head in acetabular cup.
Figure 5.
Intraoperative exploration showed that the polyethylene liner had migrated to beneath the gluteus maximus muscle.
Figure 6.
Postrevision radiographs: (a) anteroposterior and (b) lateral cross-table views.
Discussion
DM-THA has become increasingly popular in recent years. This implant allows improved range of motion and stability by using dual articulation and increased jump distance. Because DM-THA has an additional bearing surface, a unique failure known as IPD can occur. Philippot et al. [2] conducted a long-term study of early-design DM-THA and reported a 5.3% rate of IPD at the 17-year follow-up. In 2000, a modified version of the DM-THA was introduced, including an acetabular cup with an improved coating, smooth and tapered femoral neck, better mechanism for retention of the head in the PE liner, and better quality of highly crosslinked PE [3,7]. Epinette et al. [5] studied the modified or modern DM-THA and found 97.5% survivorship for all-cause revision at 5 years with no incidence of dislocation or IPD. However, other recent studies still reported a rate of IPD ranging from 0.8% to 2.2% in patients receiving the modern DM-THA [8,9]. In addition, the early IPD was still problematic in this contemporary design [10].
A systematic review by De Martino et al. [10] found that most early IPD cases occurred after an attempted closed reduction. The “bottle-opener effect” was proposed as the likely mechanism [11]. This mechanism was explained by the engagement of the outer PE liner on the rim of the acetabular cup or on pelvic bone during an attempted closed reduction. Addona et al. [9] reported a rate of IPD of 71% after closed reduction, and all those cases required revision surgery. They also found that all IPDs occurred after closed reduction under conscious sedation with propofol. General anesthesia or regional anesthesia with complete paralysis may reduce the risk of IPD. Considering the association between femoral head size and early IPD, previous studies reported no cases of IPD occurring in femoral head size smaller than 28 mm [9,10]. Our study first reported the early IPD with a 22.2-mm femoral head. A small number of patients used 22.2-mm femoral head in previous studies [9,10], which might explain this finding.
In our case, even though we performed the closed reduction under general anesthesia, iatrogenic IPD occurred immediately. Closed reduction should be performed gently under fluoroscopy, and forceful levering should be avoided to prevent the bottle opener effect [10]. However, as a specific maneuver for reduction of DM-THA dislocation has not yet been established, the early detection of IPD is essential. We propose the presence of eccentric femoral head in the acetabular cup on postreduction radiograph as a pathognomonic sign for diagnosis of IPD. The shadow of the PE liner in soft tissue on plain radiograph also helps to confirm diagnosis. To the best of our knowledge, our patient was the first early IPD case to use the 22.2-mm-diameter femoral head. Given our belief that IPD in our patient was caused by the bottle opener effect, not by impingement between the femoral head and the PE liner, it appears that this effect can occur in all femoral head sizes.
After detection of early IPD, open reduction and bearing revision should be performed to manage this complication. However, it is very essential that the causes of DM-THA dislocation be identified and remedied. Inadequate restoration of femoral offset and soft-tissue tension were the main causes of DM-THA dislocation in our patient. We proved that these problems could be solved after placing the longer femoral neck. Therefore, correction of the primary etiology was the key to successful management of the DM-THA dislocation and preventing the early IPD.
Summary
We reported the first case of early IPD occurring in femoral head size 22.2 mm. This complication developed immediately after closed reduction of DM-THA dislocation. The presence of eccentric femoral head in the acetabular cup on postreduction radiograph was crucial for diagnosis. Early detection and prompt revision of the bearing were both important to the effective management of this complication. Identification and correction of the primary etiology of DM-THA dislocation are needed to prevent this complication.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Funding disclosure
This was an unfunded study.
Acknowledgments
The authors gratefully acknowledge the patient profiled in this report for granting us permission to report details and images relating to her case.
Informed patient consent
The author(s) confirm that informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2021.10.013.
Appendix A. Supplementary data
References
- 1.Bousquet G., Argenson C., Godeneche J.L., et al. [Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet’s cementless prosthesis. Apropos of 136 cases] Rev Chir Orthop Reparatrice Appar Mot. 1986;72(Suppl 2):70. [PubMed] [Google Scholar]
- 2.Philippot R., Neri T., Boyer B., et al. Bousquet dual mobility socket for patient under fifty years old. More than twenty year follow-up of one hundred and thirty one hips. Int Orthop. 2017;41(3):589. doi: 10.1007/s00264-016-3385-y. [DOI] [PubMed] [Google Scholar]
- 3.Blakeney W.G., Epinette J.-A., Vendittoli P.-A. Dual mobility total hip arthroplasty: should everyone get one? EFORT Open Rev. 2019;4(9):541. doi: 10.1302/2058-5241.4.180045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vielpeau C., Lebel B., Ardouin L., et al. The dual mobility socket concept: experience with 668 cases. Int Orthop. 2011;35(2):225. doi: 10.1007/s00264-010-1156-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epinette J.-A., Harwin S.F., Rowan F.E., et al. Early experience with dual mobility acetabular systems featuring highly cross-linked polyethylene liners for primary hip arthroplasty in patients under fifty five years of age: an international multi-centre preliminary study. Int Orthop. 2017;41(3):543. doi: 10.1007/s00264-016-3367-0. [DOI] [PubMed] [Google Scholar]
- 6.Batailler C., Fary C., Verdier R., et al. The evolution of outcomes and indications for the dual-mobility cup: a systematic review. Int Orthop. 2017;41(3):645. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 7.Epinette J.-A., Béracassat R., Tracol P., et al. Are modern dual mobility cups a valuable option in reducing instability after primary hip arthroplasty, even in younger patients? J Arthroplasty. 2014;29(6):1323. doi: 10.1016/j.arth.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 8.Pai F.-Y., Ma H.-H., Chou T.-F.A., et al. Risk factors and modes of failure in the modern dual mobility implant. A systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):541. doi: 10.1186/s12891-021-04404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Addona J.L., Gu A., De Martino I., Malahias M.A., Sculco T.P., Sculco P.K. High rate of early intraprosthetic dislocations of dual mobility implants: a Single Surgeon Series of primary and revision total hip Replacements. J Arthroplasty. 2019;34(11):2793. doi: 10.1016/j.arth.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 10.De Martino I., D’Apolito R., Waddell B.S., et al. Early intraprosthetic dislocation in dual-mobility implants: a systematic review. Arthroplasty Today. 2017;3(3):197. doi: 10.1016/j.artd.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loubignac F., Boissier F. [Cup dissociation after reduction of a dislocated hip hemiarthroplasty] Rev Chir Orthop Reparatrice Appar Mot. 1997;83(5):469. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.