Abstract
Objectives:
This study was an evaluation of the effectiveness of the Callisto eye image-guided, markerless system (Carl Zeiss Meditec AG, Jena, Germany) in toric intraocular lens (IOL) positioning.
Methods:
The results of a novel, markerless, alignment system used for IOL positioning were analyzed in this retrospective study. Preoperatively, reference image registration was performed with the IOLMaster 700 biometer (Carl Zeiss Meditec AG, Jena, Germany) and transferred to the Callisto eye system, which was used in conjunction with an Opmi Lumera 700 microscope (Carl Zeiss Meditec AG, Jena, Germany). Using the Callisto Z Align technology, a toric IOL was aligned precisely with the steep axis. One day after surgery, the pupil was fully dilated and a thin slit was placed on the marker of the toric IOL and the angle was measured using an axis calculator smartphone application. The degree of the measured angle and the preoperatively determined angle were compared.
Results:
Sixty eyes of 46 patients were included. The difference in the absolute angle between the intended and the postoperative (at day 1) axes was a mean of 2.71±1.64°.
Conclusion:
The Callisto eye image-guided, markerless system successfully provided assistance in precisely positioning the toric IOL.
Keywords: Astigmatism, Callisto eye, toric intraocular lens
Introduction
Many studies have demonstrated the effectiveness of astigmatism correction with a toric intraocular lens (IOL) (1-3). Implantation of a toric IOL at the correct axis is of the utmost value to correct astigmatism in cataract surgery. The manual marking technique is a popular method, although it has several disadvantages, such as potential human error by both the surgeon and the patient during marking, as well as fading of the corneal marks.
The markerless Callisto eye system (Carl Zeiss Meditec AG, Jena, Germany) is a tool introduced to address these problems. This study is an examination of results achieved at a single center with this intraoperative IOL positioning system.
Methods
This study was approved by the institutional review board of the Istanbul Yeni Yuzyil University Faculty of Medicine and the ethical standards of the Declaration of Helsinki were observed throughout. In this retrospective study, the medical records of patients who underwent phacoemulsification with implantation of a toric monofocal IOL between January 1, 2018 and December 31, 2018 were reviewed. The inclusion criteria were the presence of corneal astigmatism of 1.25 diopter (D) or more, uncomplicated phaco surgery, use of Callisto eye (Fig. 1) during surgery for toric IOL positioning, available first-month medical records, and a pupil dilatation that enabled observation of marking on the IOL. During this period, 96 toric IOLs were implanted and 60 eyes of 46 patients met the study criteria. There were 20 males and 26 females, aged 32 to 72 years (mean: 56±16.4 years).
Figure 1.

Matching angle overlay of the limbal vessel with the results of the Callisto eye system (Carl Zeiss Meditec AG, Jena, Germany). The 3 blue lines are the Z align results.
Preoperative Assessment
All of the patients provided written, informed consent before the surgery. A detailed slit-lamp examination was performed preoperatively. Best spectacle-corrected visual acuity, non-contact intraocular pressure, cornea astigmatism, and anterior chamber evaluation with a Pentacam HR system (Oculus Optikgeräte, Wetzlar, Germany) were recorded. The diopter of the toric IOL was determined using an online calculator. Preoperatively, high quality reference infrared images were registered with an IOL Master 700 biometer (Carl Zeiss Meditec AG, Jena, Germany) while the patient was in a seated position and transferred to the Callisto eye system, which was connected to an Opmi Lumera 700 microscope (Carl Zeiss Meditec AG, Jena, Germany). During toric IOL positioning, these reference images were matched with live stream images from the Opmi Lumera 700 and horizontal and steep axes were determined with the Z Align function.
Surgical Technique
All of the surgeries were performed by a single experienced phaco surgeon (K.B.) under topical anesthesia using a 2.2 mm temporal clear corneal incision. Following injection of an ophthalmic viscosurgical device (OVD), capsulorhexis, phacoemulsification, and irrigation/aspiration of cortical material were performed. The OVD was injected into the capsular bag and a monofocal hydrophobic toric IOL (AcrySof IQ SN6AT3-T9; Alcon Laboratories, Ft. Worth, TX, USA) was implanted in the capsular bag and positioned at the determined axis using the Callisto eye system. The OVD was then removed from the anterior chamber and behind the IOL. Postoperative topical medications applied were dexamethasone 0.1% 4x, nepafenac 0.1% 4x, and moxifloxacin 0.5% 4x for 1 month.
Postoperative Assessment
At postoperative day 1, in order to analyze the accuracy of the Callisto eye system, the pupil was fully dilated with topical tropicamide and epinephrine. A slit-lamp examination was conducted while the patients were asked to look straight ahead. A thin slit was centered and rotated until it overlapped with the marker on the toric IOL. It was ensured that the operated and non-operated eyes were on the same level. The angle of this thin slit was measured accurately with a smartphone axis calculator application.
Results
Sixty eyes of 46 patients (20 male, 26 female) were included in the study. The mean age of the patients was 56±16.4 years (range: 32-72 years). The mean IOL power was 20.1±7.4D (range: 10.0-28.0D) and the mean corneal astigmatism was 2.4±1.4D (range: 1.50-4.50D). With-the-rule astigmatism (at 90±30°) was observed in 30 patients, against-the-rule astigmatism (at 180±30°) in 24 patients, and oblique astigmatism (at 30-60° and 120-150° degrees) in 6 patients.
The mean postoperative astigmatism was 0.56±0.16D. The mean absolute disparity between the target toric IOL axis and the implanted toric IOL axis was 2.71±1.64° (range: -8-6°). A Bland-Altman plot in Figure 2 illustrates the difference between the target axis and the implanted toric IOL axis. Clockwise rotation (CWR) was recorded as a positive value and counterclockwise rotation (CCWR) was recorded as a negative value. CWR was observed in 29 patients (mean: 2.82±1.36°), CCWR in 26 patients (3.11±1.63°), and no rotation was seen in 5 patients. A difference in the absolute angle of ≤1.0° was recorded in 16 (26.6%) eyes, ≤2° in 28 (46.6%) eyes, ≤3° in 37 eyes, ≤4° in 55 eyes, and ≥5° in 5 eyes (range: 5 to -8°).
Figure 2.
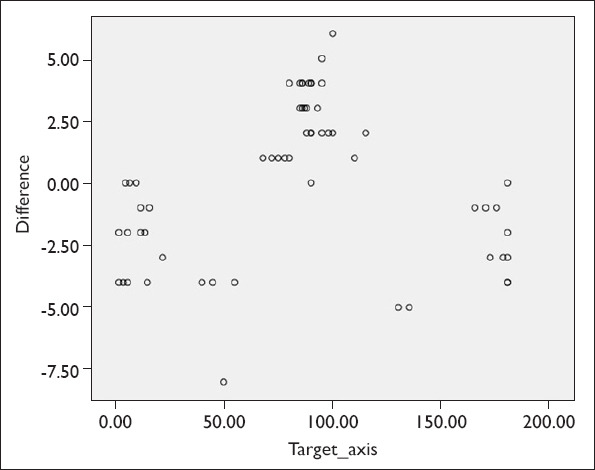
Bland-Altman plot: Target axis versus implanted toric intraocular lens axis.
Discussion
Positioning of the toric IOL on the correct axis is very important since it has been established that a deviation of 3° from the intended axis could cause a 9.05% decrease in astigmatic correction (4). Several techniques have been developed to ensure the best possible positioning, such as manual marking, iris registration, wavefront aberrometry, and image-guided systems (5–7).
This study was an evaluation of the effectiveness of the Callisto eye image-guided system. Preoperative image registration was performed with an IOLMaster 700 biometer while the patient was in a seated position. This device approved the images automatically only if they were of high quality. Therefore, the registration of images was not prone to human error.
In several studies, the effectiveness of automatic computer-based systems both for toric IOL alignment and postoperative toric IOL alignment has been investigated. Solomon et al. (8) assessed the Callisto eye system in comparison with intraoperative aberrometry. They found that Callisto eye yielded less remaining refractive astigmatism. In another study, Carey et al. (9) compared the effectiveness of slit-lamp slit (3.1±1.6°) with a refractive power/corneal analyzer system (2.7±2.0°) for postoperative toric IOL angle measurement and found that the 2 methods were equally effective. Elhofi and Helaly (10) compared the effectiveness of the manual marking technique (4.33±2.72°) with the Verion Image-Guided System (Alcon Laboratories, Ft. Worth, TX, USA) (2.4±1.96°) and found the 2 techniques to be equally effective. In a similar article, Montes de Oca et al. (11) evaluated and compared manual marking (2.88±2.18°) with the computer-guided TrueVision 3D Visualization and Guidance System (Truevision Systems, Goleta, CA, USA) (2.96±2.54°) and found similar accuracy in toric IOL positioning. Webers et al. (12) found that both the Verion Image-Guided System (Alcon Laboratories, Ft. Worth, TX, USA) (1.3±1.6°) and the manual marking technique (2.8±1.8°) were similarly effective. Woodcock et al. (13) compared intraoperative aberrometry with the manual technique and found less refractive astigmatism in the intraoperative aberrometry group. The results of our study were similar. We found that there was a 2.71±1.64° absolute angle difference between the toric IOL axis and the target axis at postoperative day 1. Based on our findings and previous reports (8–13), it can be concluded that computer-based systems are trustworthy.
There are some limitations to our study. First, this was a retrospective study with a limited number of patients. Prospective research with a larger number of patients may provide useful data. Second, because this was designed as an evaluation study, we did not have a control group. In a future study, we plan to compare the manual technique with the Callisto eye system. Third, we evaluated the position of the toric IOL at postoperative day 1. Long-term assessment of the toric IOL may give us valuable information about IOL rotation.
Conclusion
In conclusion, our results demonstrated that the Callisto eye system enabled precise positioning of the toric IOL on the intended axis. This system is easy to use but has a steep learning curve. Further prospective studies of larger patient groups are needed to support this study.
Footnotes
Disclosures
Ethics Committee Approval: The Ethics Committee of Institutional review board of the Istanbul Yeni Yuzyil University Faculty of Medicine provided the ethics committee approval for this study (16.01.2020/058).
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Involved in design and conduct of the study (BK, SA); preparation and review of the study (BK, SA); data collection (BK, SA); and statistical analysis (BK, SA).
References
- 1.Gökçe SE, Ayar O, Özmen MC, Yazgan S, Akdemir MO, Koç M. The Results of Toric Intraocular Lens Implantation in Cataract Patients with Preexistıng Corneal Astigmatism. Journal of Glaucoma-Cataract. 2015;10:125–8. [Google Scholar]
- 2.Kılıç İ, Akova YA, Akman A, Eğrilmez S. The Results of Phacoemulsification and Toric Intraocular Lens Implantation in Patients with High Astigmatism and Cataract. [Article in Turkish] Turk J Ophthalmol. 2012;42:116–9. [Google Scholar]
- 3.Yüce B, Köse B, Yılmaz SG, Eğrilmez S. The Results of Toric Intraocular Lens Implantation in Cases with Cataract and High Astigmatism. Turkiye Klinikleri J Med Sci. 2013;33:1224–30. [Google Scholar]
- 4.Felipe A, Artigas JM, Díez-Ajenjo A, García-Domene C, Alcocer P. Residual astigmatism produced by toric intraocular lens rotation. J Cataract Refract Surg. 2011;37:1895–901. doi: 10.1016/j.jcrs.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. J Cataract Refract Surg. 2012;38:2094–9. doi: 10.1016/j.jcrs.2012.07.039. [DOI] [PubMed] [Google Scholar]
- 6.Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses:historical overview patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39:624–37. doi: 10.1016/j.jcrs.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 7.Garzón N, Poyales F, de Zárate BO, Ruiz-García JL, Quiroga JA. Evaluation of rotation and visual outcomes after implantation of monofocal and multi- focal toric intraocular lenses. J Refract Surg. 2015;31:90–7. doi: 10.3928/1081597X-20150122-03. [DOI] [PubMed] [Google Scholar]
- 8.Solomon JD, Ladas J. outcomes:computer-assisted registration versus intraoperative aberrometry. J Cataract Refract Surg. 2017;43:498–504. doi: 10.1016/j.jcrs.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Carey PJ, Leccisotti A, McGilligan VE, Goodall EA, Moore CB. Assessment of toric intraocular lens alignment by a refractive power/corneal analyzer system and slitlamp observation. J Cataract Refract Surg. 2010;36:222–9. doi: 10.1016/j.jcrs.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 10.Elhofi AH, Helaly HA. Comparison between digital and manual marking of toric intraocular lenses:a randomized trial. Medicine (Baltimore) 2015;94:e1618. doi: 10.1097/MD.0000000000001618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Montes de Oca I, Kim EJ, Wang L, Weikert MP, Khandelwal SS, Al-Mohtaseb Z, et al. Accuracy of toric intraocular lens axis alignment using a 3-dimensional computer-guided visualization system. J Cataract Refract Surg. 2016;42:550–5. doi: 10.1016/j.jcrs.2015.12.052. [DOI] [PubMed] [Google Scholar]
- 12.Webers VSC, Bauer NJC, Visser N, Berendschot TTJM, van den Biggelaar FJHM, Nuijts RMMA. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J Cataract Refract Surg. 2017;43:781–8. doi: 10.1016/j.jcrs.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Woodcock MG, Lehmann R, Cionni RJ, Breen M, Scott MC. Intraoperative aberrometry versus standard preoperative biometry and a toric IOLcalculator for bilateral toric IOL implantation with a femtosecond laser:one month results. J Cataract Refract Surg. 2016;42:817–25. doi: 10.1016/j.jcrs.2016.02.048. [DOI] [PubMed] [Google Scholar]


