Abstract
Objectives:
The aim of this study was to compare the accuracy of an image-guided system (Callisto eye; Carl Zeiss, Oberkochen, Germany) with the manual marking technique in the positioning of a toric intraocular lens (IOL).
Methods:
A total of 80 eyes of 80 patients who underwent cataract surgery with a monofocal, single-piece, hydrophobic, biconvex, toric, aspheric IOL (Acrysof IQ SN6AT, Alcon Laboratories, Inc., Fort Worth, TX, USA) implantation were included. Before surgery, all of the patients underwent a complete eye examination that included evaluation of uncorrected (UCVA) and corrected distance visual acuity (CDVA), spherical equivalent (SE), astigmatic refraction (AR), keratometry, biometry, as well as meridian registration with the IOLMaster 700 (Carl Zeiss, Oberkochen, Germany), slit lamp examination, intraocular pressure measurement, and dilated retinal examination. The diopter of the toric IOL was calculated with an online calculator (Alcon, Fort Worth, TX, USA). At 3 months post surgery, the UCVA, CDVA, SE, and residual astigmatism were recorded, and the pupils of all of the patients were fully dilated to determine the toric IOL marker positions.
Results:
Group 1, the Callisto eye system group, comprised 45 eyes, and Group 2, the manual marking technique group, was composed of 35 eyes. The preoperative values of both groups were statistically similar in terms of the SE, corneal cylinder, axial length, logMAR UDVA, and logMAR CDVA. At postoperative 3 months, there were no significant differences between the 2 groups in the logMAR UDVA, logMAR CDVA, degree of misalignment of toric IOL, or mean deviation from target-induced astigmatism values. The mean deviation degree from the intended axis was 2.04±1.84 in the Callisto eye system group (Group 1) and 3.24±2.64 in the manual marking technique group (Group 2). However, this difference did not have any effect on the logMAR UDVA.
Conclusion:
The image-guided markerless system was found to be as effective as manual marking in the positioning of toric IOLs.
Keywords: Astigmatism, Callisto eye, manual marking, toric intraocular lenses
Introduction
Technological advancements in intraocular lenses (IOLs) and diagnostic equipment have enabled surgeons to improve measurement of refractive values with greater precision. Achieving a postoperative high level of uncorrected visual acuity has become a main goal of cataract surgery. An effective way to correct astigmatism using a toric IOL was first reported by Shimizu et al. (1) in 1994. In order to successfully obtain high-precision compensation for astigmatism, it is important to position a toric IOL at the correct axis, which relies on corneal marking. An additional limitation of a toric IOL is postoperative rotation, which may occur due to the lens material, size, or design (2, 3).
The most important step in the correction of astigmatism with a toric IOL is positioning the lens at the correct axis. Manual marking of the peripheral cornea at the horizontal (0–180°) or vertical (90–270°) axis with the patient in the seated position is a commonly used method (4, 5). The next step is to use a control marker device and rotate the IOL into the correct position. The manual marking technique, however, is subject to human error and may erode the corneal epithelium. An image-guided system marketed as Callisto eye (Carl Zeiss, Oberkochen, Germany) has been developed that permits non-touch corneal marking. The aim of this study was to evaluate the accuracy of this system and compare the results with the manual marking technique.
Methods
This retrospective study was approved by the institutional review board of Istanbul’s Medipol University School of Medicine and adhered to the ethical standards of the Declaration of Helsinki. All of the patients provided signed, informed consent. The data of patients who had undergone phacoemulsification surgery with toric IOL implantation were selected and included in this study. The Callisto eye system was used in Group 1 (45 eyes), and in Group 2 (35 eyes), the manual marking technique was used. Patients with 1.25 diopter (D) or higher astigmatism were included. The exclusion criteria applied were irregular astigmatism, glaucoma, and retinal diseases, such as macular degeneration and diabetic retinopathy.
Before surgery, a complete eye examination that included assessment of the uncorrected visual acuity (UCVA), corrected distance visual acuity (CDVA), spherical equivalent (SE), astigmatic refraction (AR), biometry, and meridian registration with an IOLMaster 700 biometer (Carl Zeiss, Oberkochen, Germany), slit lamp examination, intraocular pressure measurement, and dilated retinal examination was performed on all of the patients. The diopter of the toric IOL was calculated using an online calculator (Alcon Laboratories, Fort Worth, TX, USA). Keratometry values were measured with the IOLMaster 700. At the post-surgical 3-month examination, UCVA, CDVA, SE, and AR were measured while the pupils were fully dilated to determine the position of markers of the toric IOL. A narrow slit beam was positioned on the marker, and the angle of the beam was measured with the Axis Assistant smartphone application (Centro Oftalmico Varas Samaniego, Guayaquil, Ecuador) (6) (Fig. 1).
Figure 1.

(a) Angle of slit as seen on the screen of a smart phone, (b) Angle of slit seen on a smart phone as measured with the Axis Assistant smartphone application (Centro Oftalmico Varas Samaniego, Guayaquil, Ecuador).
A monofocal, single-piece, hydrophobic, biconvex, toric aspheric IOL (Acrysof IQ SN6AT; Alcon Laboratories, Fort Worth, TX, USA) was implanted in all of the patient eyes. The viscoelastic device behind the toric IOL was completely removed to facilitate IOL posterior capsule adhesion. The optic zone diameter of this lens is 6.0 mm with a total diameter of 13.0 mm, and this IOL is manufactured with cylinders from 1.50 D to 6.00 D in 0.75 D increments.
In the Callisto eye group, a reference image was taken with the IOLMaster 700 and the data were transferred to the Callisto eye image-guided system, which was already connected to an Opmi Lumera 700 surgical microscope (Carl Zeiss, Oberkochen, Germany). Live-stream images from the microscope were captured by the Callisto eye system, and registered images were overlayed for a translucent view (Fig. 2). Confirmation was established with the view of the limbal vessel. In the next step, 3 parallel blue lines represent the toric IOL axis and a yellow line to represent the 0–180° axis. The toric IOL was positioned at the target axis. In the manual marking group, the slit lamp position of 0–180° was marked (Fazio; Janach, Como, Italy) and the toric IOL was positioned at the target axis with an intraoperative marker (Mendez; Janach, Como, Italy). Cataract surgery was performed with a high-fluid phacoemulsification machine (Centurion Vision System, Alcon Laboratories, Fort Worth, TX, USA) using a 2.2-mm temporal clear corneal incision made by an experienced surgeon (KB).
Figure 2.
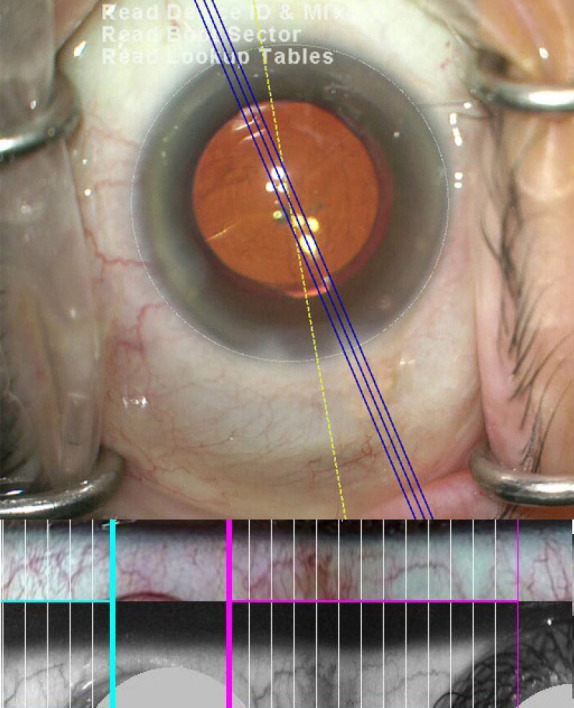
Callisto eye system (Carl Zeiss, Oberkochen, Germany) overlayed angle data of the limbal vessel. The 3 parallel blue lines are the Z align product.
Statistical Analysis
The study data were analyzed using IBM SPSS Statistics for Windows, Version 19.0 software (IBM Corp., Armonk, NY, USA). Normality analyses were performed using the Kolmogorov–Smirnov test. The Student’s t-test was used for parametric analysis, and the Wilcoxon rank-sum test was used if parametric analysis was not possible. A p value of <0.05 was considered statistically significant. The difference between the target-induced astigmatism and postoperative refractive astigmatism was the difference vector. Software developed by Sait Egrilmez, which was based on the Alpins Method for vector analysis, was also used (7, 8).
Results
This study included 80 eyes of 80 patients (46 females, 34 males) (Table 1). The Callisto eye group (Group 1) comprised 45 eyes (26 female, 19 male) with a mean age of 62.2±9.3 years (range: 53-74 years). The manual marking technique group (Group 2) was composed of 35 eyes (20 females, 15 males) with a mean age of 62.3±9.6 years (range: 52-72 years). Of the 80 eyes, 52 had with-the-rule astigmatism (26 in Group 1 or 57.7%, and 19 in Group 2, or 54.3%); 16 eyes had oblique astigmatism; and 12 eyes had against-the-rule astigmatism. All of the procedures were performed with no complications. The preoperative SE, corneal cylinder, UDVA, and CDVA values for both groups were statistically similar. There were no significant differences between groups in the values of UDVA, CDVA, or degree of misalignment of the toric IOL (Table 2).
Table 1.
Patient demographic data
| Callisto eye Mean±SD | Manual marking Mean±SD | p | |
|---|---|---|---|
| Total patients (eyes) | 45(45) | 35(35) | - |
| Female/male | 26/19 | 20/15 | - |
| Age (years) | 62.2±9.3 | 62.3±9.6 | 0.244 |
| Preoperative SE (D) | -0.82±1.16 | 0.91±1.23 | 0.126 |
| Preoperative astigmatism D | 2.26±0.93 | 2.37±0.88 | 0.261 |
| Axial length (mm) | 23.44±1.83 | 23.14±1.74 | 0.180 |
| Preoperative UDVA (logMAR) | 0.64±0.18 | 0.65±0.17 | 0.168 |
| Preoperative CVDA (logMAR) | 0.42±0.14 | 0.45±0.17 | 0.232 |
CDVA: Corrected distance visual acuity; D: Diopter; SE: Spherical equivalent; UDVA: Uncorrected distance visual acuity.
Table 2.
Postoperative values in the Callisto eye and manual marking groups
| Callisto eye (n=45) Mean±SD |
Manual marking (n=35) Mean±SD |
P | |
|---|---|---|---|
| Postoperative UDVA (logMAR) | 0.13±0.12 | 0.14±0.11 | 0.124 |
| Postoperative CDVA (logMAR) | 0.05±0.05 | 0.06±0.07 | 0.106 |
| Mean deviation from TIA (D) | 0.12±0.10 | 0.14±0.12 | 0.110 |
| Postoperative IOL misalignment (degree) | 2.04±1.84 | 3.24±2.64 | 0.080 |
CDVA: Corrected distance visual acuity; TIA: Target-induced astigmatism; UDVA: Uncorrected distance visual acuity.
Discussion
A number of studies have demonstrated that the implantation of a toric IOL has achieved better uncorrected vision and a lower degree of postoperative astigmatism; a larger percentage of patients have been able to live without glasses (9). Accurate implantation of a toric IOL at the target axis is required in order to correct astigmatism precisely. It has been well-documented that a 3° deviation from the target axis results in about a 10% undercorrection of astigmatism (10). There are 2 primary causes of toric IOL misalignment: erroneously positioning of the IOL and late rotation of the IOL in the capsular bag (4, 5). Different techniques to position a toric IOL on the target axis have previously been described (11, 12).
The manual marking method is a two-step procedure. The first step involves marking the horizontal axis using a slit lamp while the patient is seated, in order to compensate for cyclotorsion. These marks are then used after toric IOL implantation as reference marks for the target axis. The effectiveness of this method has been evaluated in many studies (11, 12).
In this study, the Callisto eye image-guided system used in Group 1 captured high-quality, infrared reference images automatically, which were registered with the IOLMaster 700. Second, these images and live-stream images from the Opmi Lumera 700 were transferred to the Callisto eye system where these 2 images were overlayed for a translucent view. Third, the surgeon approved this view and determined both the steep axis and incision site; these points could then also be viewed through the eyepiece of the microscope. In Group 2, a marker with a pendulum was used to mark the horizontal axis. The effectiveness of this type of marker has been reported previously (13, 14).
Markerless toric IOL positioning systems have been compared with the manual marker technique in previous studies. There are currently 3 image-guided markerless systems available. The Verion image-guided system (Alcon Laboratories, Fort Worth, TX, USA) and the TrueVision 3D visualization system (Leica Camera, Wetzler, Germany) are also available in addition to the Callisto eye system. Solomon et al. (15) compared the Callisto eye system with intraoperative aberrometry and found that the Callisto eye yielded less refractive astigmatism. Similarly, Meyer et al. (16) compared the Callisto eye system with the manual technique and found that use of the Callisto eye resulted in less toric IOL misalignment. The results of a study conducted by Titiyal et al. (17) supported these 2 studies. Our findings are consistent with these studies. We also found less toric IOL misalignment in the Callisto eye group than in the manual marking group. However, this finding did not have an effect on UDVA at 3-month follow-up examinations. Our results confirm that the Callisto eye image-guided system is an effective method for the precise positioning of toric IOLs. Elhofi and Helaly (18) compared the effectiveness of the Verion system with that of the manual marking technique and found both techniques to be equally effective. Webers et al. (19) also found that the Verion image-guided system and the manual marking technique were equally successful. In their study, Kim et al. (20) compared a SensoMotoric Instruments device (Teltow, Germany) with the manual technique and found it to be more precise. In a similar study, Montes de Oca et al. (21) compared a 3-dimensional computer-guided system (TrueVision 3D Systems, Inc., Goleta, CA, USA) with manual marking and found the accuracy level of toric IOL positioning to be similar. Woodcock et al. (22) used intraoperative aberrometry to perform toric IOL positioning and found that this technique was more effective than manual marking.
There are some limitations to this study. Our work was retrospective research with a limited number of patients; a prospective study with a larger number of patients would give us more valuable information about toric IOLs. Secondly, we did not compare rotation of non-toric IOLs with toric IOLs. A prospective comparative study on this topic is warranted.
In conclusion, we compared the Callisto eye system technique with manual marking methods used to position the toric IOL on the target axis and found no significant differences in logMAR UDVA, deviation of target axis, or residual astigmatism between groups. Both methods were found to be effective and accurate.
Footnotes
Disclosures
Ethics Committee Approval: Institutional review board of the Istanbul Medipol University Faculty of Medicine 28.4.2020/333.
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Involved in design and conduct of the study (BK, HE); preparation and review of the study (BK, HE); data collection (BK, HE); and statistical analysis (BK, HE).
References
- 1.Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses:correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994;20:523–6. doi: 10.1016/s0886-3350(13)80232-5. [DOI] [PubMed] [Google Scholar]
- 2.Patel CK, Ormonde S, Rosen PH, Bron AJ. Postoperative intraocular lens rotation:a randomized comparison of plate and loop haptic implants. Ophthalmology. 1999;106:2190–6. doi: 10.1016/S0161-6420(99)90504-3. [DOI] [PubMed] [Google Scholar]
- 3.Schwenn O, Kottler U, Krummenauer F, Dick HB, Pfeiffer N. Effect of large positioning holes on capsule fixation of plate-haptic intraocular lenses. J Cataract Refract Surg. 2000;26:1778–85. doi: 10.1016/s0886-3350(00)00496-x. [DOI] [PubMed] [Google Scholar]
- 4.Viestenz A, Seitz B, Langenbucher A. Evaluating the eye's rotational stability during standard photography:effect on determining the axial orientation of toric intraocular lenses. J Cataract Refract Surg. 2005;31:557–61. doi: 10.1016/j.jcrs.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Gökçe SE, Ayar O, Özmen MC, Yazgan S, Akdemir MO, Koç M. The Results of Toric Intraocular Lens Implantation in Cataract Patients with Preexisting Corneal Astigmatism. Journal of Glaucoma-Cataract. 2015;10:125–8. [Google Scholar]
- 6.Varas J. Axis Assistant. [Accessed May 3, 2020]. Available at: http://blog.varas.com/axis/
- 7.Egrilmez S, Dalkilic G, Yagci A. Vector analysis software on analyzing astigmatism [Article in Turkish.] Turk J Ophthalmol. 2003;33:404–16. [Google Scholar]
- 8.Alpins N. Astigmatism analysis by the Alpins method. J Cataract Refract Surg. 2001;27:31–49. doi: 10.1016/s0886-3350(00)00798-7. [DOI] [PubMed] [Google Scholar]
- 9.Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric Intraocular Lenses in the Correction of Astigmatism During Cataract Surgery:A Systematic Review and Meta-analysis. Ophthalmology. 2016;123:275–86. doi: 10.1016/j.ophtha.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Febbraro JL, Koch DD, Khan HN, Saad A, Gatinel D. Detection of static cyclotorsion and compensation for dynamic cyclotorsion in laser in situ keratomileusis. J Cataract Refract Surg. 2010;36:1718–23. doi: 10.1016/j.jcrs.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 11.Graether JM. Simplified system of marking the cornea for a toric intraocular lens. J Cataract Refract Surg. 2009;35:1498–500. doi: 10.1016/j.jcrs.2009.04.033. [DOI] [PubMed] [Google Scholar]
- 12.Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking method for a toric intraocular lens:mapping method. J Refract Surg. 2011;27:375–9. doi: 10.3928/1081597X-20101005-01. [DOI] [PubMed] [Google Scholar]
- 13.Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. J Cataract Refract Surg. 2012;38:2094–9. doi: 10.1016/j.jcrs.2012.07.039. [DOI] [PubMed] [Google Scholar]
- 14.Kose B, Albayrak S. Results of Callisto Eye System in Toric Intraocular Lens Alignment. Beyoglu Eye J. 2020;5:1–4. doi: 10.14744/bej.2020.86547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solomon JD, Ladas J. outcomes:computer-assisted registra- tion versus intraoperative aberrometry. J Cataract Refract Surg. 2017;43:498–504. doi: 10.1016/j.jcrs.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Mayer WJ, Kreutzer T, Dirisamer M, Kern C, Kortuem K, Vounotrypidis E, et al. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J Cataract Refract Surg. 2017;43:1281–6. doi: 10.1016/j.jcrs.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 17.Titiyal JS, Kaur M, Jose CP, Falera R, Kinkar A, Bageshwar LM. Comparative evaluation of toric intraocular lens alignment and visual quality with image-guided surgery and conventional three-step manual marking. Clin Ophthalmol. 2018;12:747–53. doi: 10.2147/OPTH.S164175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elhofi AH, Helaly HA. Comparison Between Digital and Manual Marking for Toric Intraocular Lenses:A Randomized Trial. Medicine (Baltimore) 2015;94:e1618. doi: 10.1097/MD.0000000000001618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webers VSC, Bauer NJC, Visser N, Berendschot TTJM, van den Biggelaar FJHM, Nuijts RMMA. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J Cataract Refract Surg. 2017;43:781–8. doi: 10.1016/j.jcrs.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 20.Kim EC, Hwang KY, Lim SA, Yi R, Joo CK. Accuracy of toric intraocular lens implantation using automated vs manual marking. BMC Ophthalmol. 2019;19:169. doi: 10.1186/s12886-019-1175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montes de Oca I, Kim EJ, Wang L, Weikert MP, Khandelwal SS, Al-Mohtaseb Z, Koch DD. Accuracy of toric intraocular lens axis alignment using a 3-dimensional computer-guided visualization system. J Cataract Refract Surg. 2016;42:550–5. doi: 10.1016/j.jcrs.2015.12.052. [DOI] [PubMed] [Google Scholar]
- 22.Woodcock MG, Lehmann R, Cionni RJ, Breen M, Scott MC. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser:One-month results. J Cataract Refract Surg. 2016;42:817–25. doi: 10.1016/j.jcrs.2016.02.048. [DOI] [PubMed] [Google Scholar]


