Abstract
Valsalva maculopathy (VM) induced by the Valsalva maneuver may cause a sudden, painless, and dramatic loss of vision in healthy individuals due to a premacular location of the hemorrhage and rupture of retinal capillaries. The prognosis is generally good. The hemorrhage usually clears spontaneously without any treatment. Presently described are clinical findings from a case evaluated as VM resulting from a sudden, forceful shout during a quarrel. A 43-year-old female was admitted to the clinic with a 1-day history of sudden, painless loss of vision in the right eye after sudden, strong shout during an argument. There was no history of trauma or any systemic disease. On examination, the visual acuity was finger count at 1 meter in her right eye, and a central subhyaloid and subinternal limiting membrane premacular hemorrhage was noted. Her intraocular pressure values were 14 mmHg in the right eye and 13 mmHg in the left eye. Her blood pressure measurement was 130/80 mmHg. At 1 month, her vision had improved to 20/25 (LogMAR 0.10) and there was resolution of the hemorrhage without treatment. Although VM is considered to be rare, the events and activities with which it is associated are relatively common in daily life. A sudden, forceful shout and Valsalva stress can lead to dangerous, sudden vision loss due to a premacular hemorrhage.
Keywords: Premacular hemorrhage, shouting, Valsalva maculopathy
Introduction
A rapid rise in intraocular venous pressure may result in the spontaneous rupture of perifoveal capillaries, leading to a sudden, painless loss of vision in an otherwise healthy eye, known as Valsalva maculopathy (VM) (1–7). It is a rare, isolated, and self-limited event. The hemorrhage commonly occurs at the macula, and in the vast majority of cases, resolves without sequelae of vision loss. Various clinical presentations have been described, such as occurrence following stressful aerobic exercise, vigorous sexual activity, inflating balloons, prostate and dental surgery, constipation, vomiting, and weight training (1–5). The hemorrhage usually clears spontaneously (3). There are several options for treatment (5). Pulsed neodymium-doped yttrium aluminum garnet lasers and argon lasers have been used to disrupt the posterior hyaloid or internal limiting membrane to improve recovery. Other procedures include pneumatic displacement of the hemorrhage with an intravitreal injection of gas with or without recombinant tissue plasminogen activator and pars plana vitrectomy (5).
Here, an interesting case report of VM due to sudden, forceful shout during an argument is reported. A strong, abrupt shout delivered in circumstances of anger and stress can cause sudden visual loss due to VM and be dangerous in daily life.
Case Report
A 43-year-old female was admitted to the clinic with a 1-day history of sudden, painless loss of vision in the right eye after a very strong shout during a quarrel. There was no history of trauma or any systemic disease. On examination, the visual acuity was finger count at 1 meter in her right eye, and a central subhyaloid and subinternal limiting membrane premacular hemorrhage was noted (Fig. 1). Her intraocular pressure values were 14 mmHg in the right eye and 13 mmHg in the left eye. Blood pressure was also measured and recorded as 130/80 mmHg. Optical coherence tomography angiography analysis supported the diagnosis of VM (Fig. 2). Ocular examination 2 weeks after the initial presentation revealed a decrease in the subhyaloid hemorrhage, but there was no improvement in visual acuity. At the 1-month exam her vision had improved to 20/25 (LogMAR 0.10) and there was resolution of the hemorrhage without treatment. Anisometropia was revealed in a refraction exam. She had a refraction error of -3.50-1.75α180 diopters in the right eye and -0.50α85 diopters in the left eye. Optical coherence tomography was performed and reported as normal (Fig. 3). Informed consent was obtained from the patient for publication of this case report.
Figure 1.
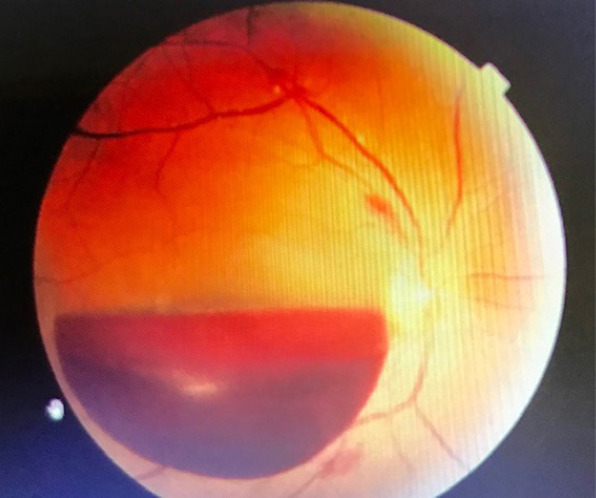
Fundus photo of the right eye illustrating the premacular subhyaloid and subinternal limiting membrane hemorrhage diagnosed as Valsalva maculopathy.
Figure 2.
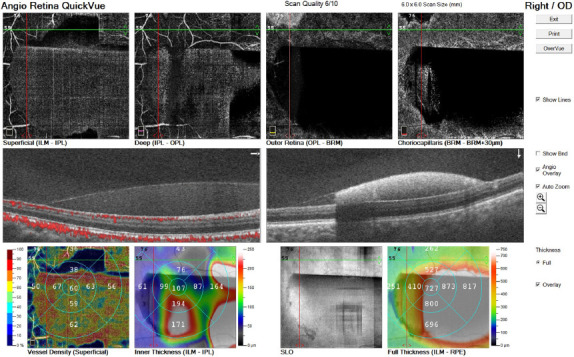
Optical coherence tomography angiography analysis of the patient’s right eye shows subhyaloid and subinternal limiting membrane hemorrhage with Valsalva maculopathy at the time of admission.
Figure 3.
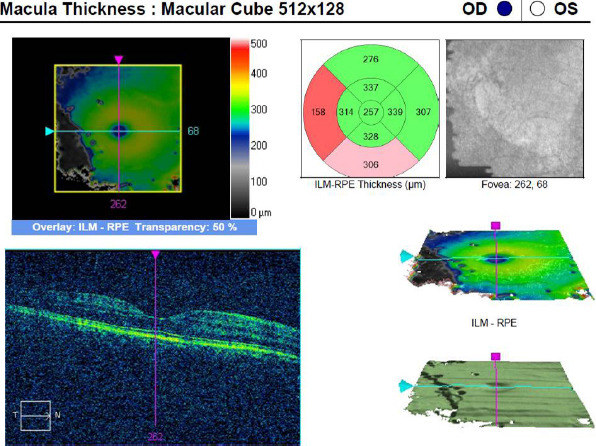
Optical coherence tomography of the patient’s right eye shows the spontaneous resolution of the premacular hemorrhage at the first month exam.
Discussion
The Valsalva maneuver stimulates both sympathetic and parasympathetic branches of the autonomic nervous system (6). A normal physiological response consists of 4 phases: Initial pressure rise, reduced venous return and compensation, pressure release, and return of cardiac output (7). The maneuver is performed with a moderately forceful attempted exhalation against a closed airway, usually performed by pinching the nose closed while expelling air out through the mouth, as if blowing up a balloon. Variations of the maneuver can be used in a medical examination as a test of cardiac function and autonomic nervous control of the heart, or to clear the ears and sinuses (that is, to equalize pressure between them) when ambient pressure changes, as in diving, hyperbaric oxygen therapy, or air travel. Prolonged, strenuous physical exertion with shouting during training exercises has been reported to lead to Valsalva hemorrhagic retinopathy. Several other factors, such as hot weather, altitude, and dehydration, may play an additive role in increasing venous pressure and hypoxia in the retinal vessels, which can then cause retinopathy (8). In this case, a sudden, strained, loud, and forceful shout combined with stress during an argument is believed to have caused a Valsalva maneuver and VM.
Duane coined the term Valsalva hemorrhagic retinopathy in 1972, when he reported 3 cases involving retinal hemorrhage in the macular region, presumably secondary to a sudden increase of intrathoracic pressure (4). A premacular hemorrhage may be idiopathic but is commonly associated with VM, proliferative diabetic maculopathy, macroaneurysm, retinal venous occlusion, and blood dyscrasia. Therefore, a thorough investigation to exclude vascular disorders is required at presentation. Our patient had no systemic disorders, such as diabetes mellitus, hypertension, or other blood dyscrasia. There was no history of physical contact such as pushing or shoving during the argument, which could cause increased chest pressure. The measured blood pressure was 130/80 mmHg at the time of examination and continued to be normal after 1 week of follow up, but we do not know her blood pressure at the time of shouting. A temporary elevation of blood pressure can cause such maculopathies.
Hanazono et al. (8) reported the case of a 19-year-old man with Valsalva retinopathy developing during Japanese cheerleading training (“ouendan”) in a mountainous area. In our case, an isolated, sudden, strong shout caused VM without any accompanying exercise.
The principal treatment options reported for VM are observation, laser hyaloidotomy, laser membranectomy, pneumatic displacement of the hemorrhage using intravitreal injection of gas with or without recombinant tissue plasminogen activator, and pars plana vitrectomy. In this patient, conservative therapy was offered and the premacular hemorrhage had resolved spontaneously at the first month.
Although VM is considered to be rare, the events and activities with which it is associated are relatively common in daily life. Sudden, strong shouts and Valsalva stress may contribute to dangerously sudden visual loss due to premacular hemorrhage. In cases of an unknown cause of premacular hemorrhage in healthy young adults, VM should be considered. Careful and thorough questioning is required and treatment should not be rushed.
Footnotes
Disclosures
Informed consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Involved in design and conduct of the study (BEK); preparation and review of the study (BEK); data collection (BEK, AE, SCO).
References
- 1.Mukherjee C, Kumar A, Mitra A. Valsalva maculopathy:To treat or not to treat. Oman J Ophthalmol. 2018;11:78–81. doi: 10.4103/ojo.OJO_91_2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheikh SA, Untoo RA, Lone IA, Shaheen N. Maculopathy:a rare association of the Valsalva manoeuvre (Valsalva maculopathy) BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.08.2008.0760. bcr08.2008.0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bar-Sela SM, Moisseiev J. Valsalva retinopathy associated with vigorous dancing in a discotheque. Ophthalmic Surg Lasers Imaging. 2007;38:69–71. doi: 10.3928/15428877-20070101-12. [DOI] [PubMed] [Google Scholar]
- 4.Chapman-Davies A, Lazarevic A. Valsalva maculopathy. Clin Exp Optom. 2002;85:42–5. doi: 10.1111/j.1444-0938.2002.tb03071.x. [DOI] [PubMed] [Google Scholar]
- 5.García Fernández M, Navarro JC, Castaño CG. Long-term evolution of Valsalva retinopathy:a case series. J Med Case Rep. 2012;6:346. doi: 10.1186/1752-1947-6-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brody S, Erb C, Veit R, Rau H. Intraocular pressure changes:the influence of psychological stress and the Valsalva maneuver. Biol Psychol. 1999;51:43–57. doi: 10.1016/s0301-0511(99)00012-5. [DOI] [PubMed] [Google Scholar]
- 7.Pstras L, Thomaseth K, Waniewski J, Balzani I, Bellavere F. The Valsalva manoeuvre:physiology and clinical examples. Acta Physiol (Oxf) 2016;217:103–19. doi: 10.1111/apha.12639. [DOI] [PubMed] [Google Scholar]
- 8.Hanazono G, Shinoda K, Obazawa M, Imamura Y, Matsumoto SC, Satofuka S, et al. Valsalva retinopathy developing during Japanese cheerleading training (“ouendan”) Retin Cases Brief Rep. 2013;7:78–81. doi: 10.1097/ICB.0b013e318268a577. [DOI] [PubMed] [Google Scholar]


