Abstract
The recent pandemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has increased the global concern over its transmission and prevention. Since there was an incontrovertible perception that environmental conditions might affect the spread of SARS-CoV-2, we analyzed the environmental variables impact on SARS-CoV-2 transmission in Pakistan. Our analytical study revealed that when the temperature remained high for consecutive 10 to 15 days, a significant decrease is witnessed in the forthcoming week in the COVID-19 cases. We found that a persistent high ambient temperature of 36 °C and above is detrimental to SARS-CoV-2 transmission and has paused the community spread of COVID-19 in Pakistan. Importantly, during the fall period of SARS-CoV-2, a high relative humidity of 63–72% was noted that showed a positive role in COVID-19 inhibition. Hence, the community spread of SARS-CoV-2 was paused by the warm humid climate and the ambient temperature was the yardstick in turning down the epidemic in Pakistan.
Keywords: Environmental control, relative humidity, SARS, SARS-cov-2, temperature
Introduction
The Betacoronaviruses, namely Middle East respiratory syndrome (MERS), severe acute respiratory syndrome (SARS), and severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) caused epidemics in Jeddah, Saudi Arabia in 2012, Guangdong, China in 2002, and Wuhan, China in 2019 respectively [1]. While the first two epidemics were confined to a few countries, the COVID-19 has been disseminated globally. The study of SARS had revealed that the coronaviruses could not withstand high temperature and humidity while spread in cold and dry conditions [2] and recent studies reported that low temperature supported SARS-CoV-2 activity and transmissibility [3]. Numerous studies proclaimed that a warmer climate can prevent the COVID-19 transmission [4], but had drawn contradictory conclusions about the roles of temperature and humidity in the control and transmission of COVID-19 [5]. Several reports from China demonstrated that low temperature and low humidity help in the transmission of SARS-CoV-2 [5,6]. The work of Shi et al. suggested that an increase in temperature decreased the incidence of COVID-19 [7]. In New York, USA, Bashir et al. concluded that average temperature and minimum temperature were significantly associated with the COVID-19 pandemic [8]. The work of Tosepu et al. revealed that the average temperature was significantly correlated with the COVID-19 pandemic in Jakarta, Indonesia [9]. In India, an increase in temperature was associated with a decrease in COVID-19 cases [10] but some reports also showed a positive association between daily cases and temperature [11]. Besides, SARS-CoV-2 strains harboring mutations in macrodomain and papain-like protease-2 domain of nonstructural protein P3 were sensitive to temperature (37°C and 40°C) compared to the wild-type strains [12], demonstrating that higher temperature was detrimental to SARS-CoV-2 mutants. In Pakistan, the prevalence and epidemiology have been studied [13] but the roles of environmental variables remained unknown. To date, there are no well-defined reports about the inhibition of community spread of SARS-CoV-2 by climate conditions and we reported that the ambient temperature was the strong barrier in the COVID-19 transmission and community spread. Our study concluded that the warm and humid climate was a key factor in turning down the COVID-19 epidemic in Pakistan.
Method
Our present study examined the climate data of four regions of Pakistan i.e., the capital Islamabad; Karachi, Sindh; Peshawar, Khyber–Pakhtunkhwa; and Lahore, Punjab that had the highest number of COVID-19 cases and death. The epicenter of COVID-19 in Pakistan was roughly along with the latitude 24.8° N to 34.0° N, including the most populated city Karachi (24.8° N), Lahore (31.5° N), Peshawar (34.0° N), and Islamabad (33.6° N). We collected the COVID-19 data of Pakistan from a publicly available database of the COVID-19 worldometer website (https://www.worldometers.info/coronavirus/) and confirmed it from the Pakistan public data bank (https://www.nih.org.pk/) of COVID-19. The temperature data was collected from Accuweather (https://www.accuweather.com/), relative humidity (%) data from the weather and climate (https://weather-and-climate.com/), and validated from the Pakistan Meteorological Department. The infection rate (IR) was determined by the following formula; IR = Total number of COVID-19 positive tests/Total number of tests done x 100.
Statistical analysis
For statistical analysis, the Mann-Whitney test was used to compare temperature and relative humidity values between the cities with and without COVID-19 transmission. The correlation coefficients between temperature/humidity and COVID-19 cases were determined by the Spearman correlation. Significant variations in the number of COVID-19 positive patients between two consecutive months, nonconsecutive months and summer season (June, July, August, September, October) and winter season (March, April, May, November, December) was determined by two-tailed paired t-test. All the analyses were performed by GraphPad Prism version 7 and P < 0.05 was considered significant.
Results and discussion
COVID-19 cases reported from February to August
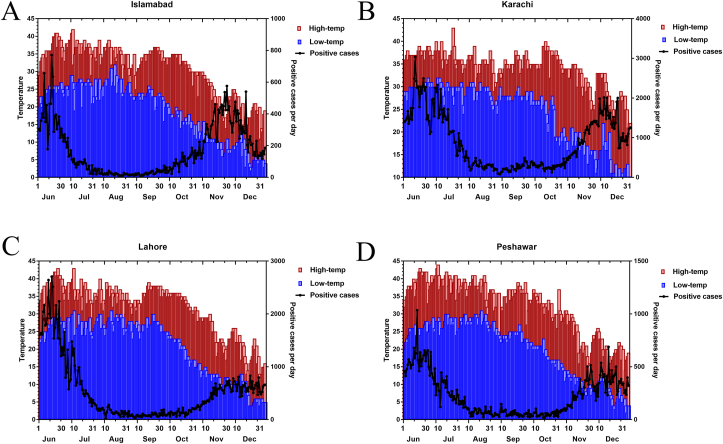
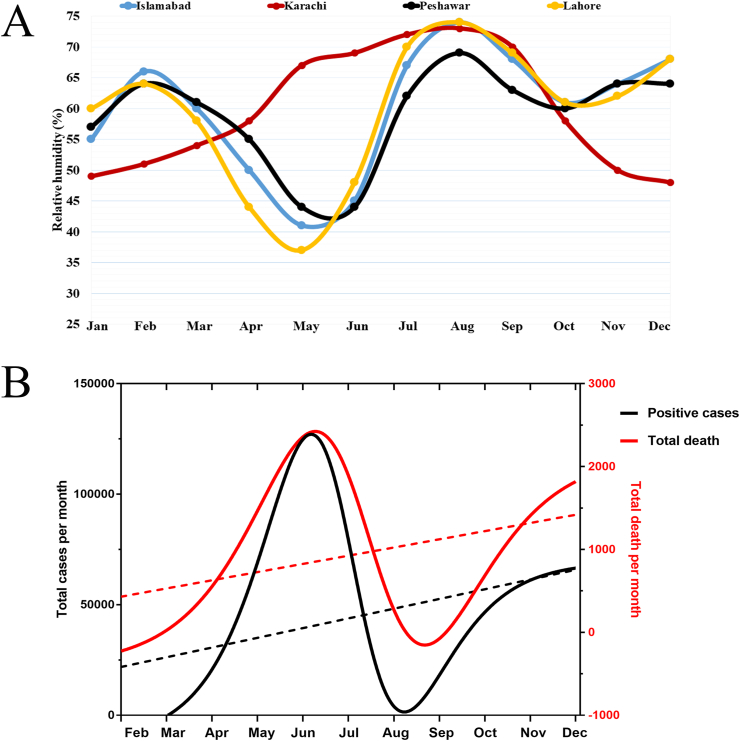
The human coronaviruses caused infections in the cold and dry environment such as the alphacoronavirus HCoV-229E and betacoronavirus HCoV-OC43 were predominantly detected in fall and winter seasons, respectively while imperceptible in the temperate environment [14]. The newly identified SARS-CoV-2 is a betacoronavirus that spread in a low-temperature and dry environment [3] while the effects of warm climate remained uncertain [5]. The first confirmed case of SARS-CoV-2 in Pakistan was reported in the city of Karachi on February 26, 2020. Since then, the epidemic has spread countrywide and Pakistan has become one of the most-affected country worldwide (482,178 positive cases and 10,176 death until December 2020). When the epidemic started in Pakistan, the average high temperature was 21–31 °C with a relative humidity of 51–62%. The epidemic spread in every city of Pakistan in April and May when the average high temperature was 28–35 °C with a relative humidity of 37–64%. These climate conditions were very conducive for COVID-19 transmission and a large-scale community spread occurred and the number of COVID-19 cases grew rapidly. In June, the temperature raised to its peak level, and the average high-temperature ranges 36–38 °C with a relative humidity of 44–68%, and Pakistan reported the maximum number of COVID-19 cases (140, 231 positive cases, and 2816 death). Interestingly, the fall of SARS-CoV-2 was started in June when the temperature consistently remained high (36 °C or above) from June 5 to June 20 in Karachi, Peshawar, Lahore, and Islamabad that resulted in a significant decrease (P < 0.05) in COVID-19 cases from June 15 to June 30 and a steep decrease (P < 0.001) in July as shown in Figs. 1A–D. In July, the average high temperature was 36.6–38.8 °C and the relative humidity was 63-72% (Fig 2A) that dropped the COVID-19 infection rate from 18.94% to 9.52%. In August, the highest average temperature was detected in the city of Peshawar 37.8 °C with the lowest infection rate of 1.8%, followed by Lahore 36.74 °C with 3.4% infection rate, Karachi 36.54 °C with 3.1% infection rate, and Islamabad 36.20 °C with 2.2% infection rate that indicated further decrease in COVID-19 infection. The infection rate and the average temperature were significantly correlated with COVID-19 as shown in Table 1. The beginning, the rise, and the downfall of COVID-19 in Pakistan are shown in Fig 2B and a detailed comparison of COVID-19 among the four regions is provided in Supplementary Table S1.
Fig. 1.
(A-D) The figure depicts the average high and low temperatures of different cities of Pakistan and the occurrence of COVID-19 from 1 June to 31 December 2020. A gradual decrease was witnessed from 14 June in Islamabad (A), from 21 June in Karachi (B), from 19 June in Lahore, and from 20 June in Peshawar (D). The re-emergence of COVID-19 positive cases was detected in November and December in Islamabad, Karachi, Lahore, and Peshawar when the average temperature dropped down below 31 °C.
Fig. 2.
(A) The relative humidity (%) values are shown from January to December that revealed a low relative humidity in May and June in Islamabad, Lahore, and Peshawar while an increase in relative humidity in July and August in all four cities of Pakistan. (B) The total number of positive cases and total death are shown from February to December. The COVID-19 cases were highest in June while dropped down in July, August, and September.
Table 1.
The table showed the significant differences between two consecutive months, nonconsecutive months, and climate variables
| Consecutive months | P-value | Non-consecutive months | P-value |
|---|---|---|---|
| March vs April | 0.055 | March vs May | 0.008 |
| April vs May | 0.026 | April vs June | 0.025 |
| May vs June | 0.003 | May vs July | 0.006 |
| June vs July | 0.004 | June vs August | 0.012 |
| July vs August | 0.002 | July vs September | 0.002 |
| August vs September | <0.001 | August vs October | <0.001 |
| September vs October | <0.001 | August vs November | 0.004 |
| October vs November | 0.002 | September vs November | 0.005 |
| November vs December |
<0.001 |
October vs December |
0.005 |
| Climate variables | Spearman correlation coefficient | P-value | |
| Temperature Average | 0.85 | 0.02 | |
| Temperature minimum | 0.32 | 0.15 | |
| Temperature maximum | 0.71 | 0.08 | |
| Relative humidity | 0.40 | 0.30 | |
| Infection-rate | 0.92 | 0.007 | |
COVID-19 cases reported from September to December
In September, the average high temperature was 35.6–37.0 °C with a relative humidity of 63-70% (Fig 2A) and the COVID-19 infection rate was 1.92%. This indicated consistency in high temperature and humidity and a further decrease was witnessed in COVID-19 cases (Figs. 1A–D). In October, the average temperature was 32.1–36.5°C with a relative humidity of 58–61% and the infection rate slightly increased (2.32%) compared to the previous month. At this point, the COVID-19 in Pakistan was at the bottom (Fig 2B) but in November the COVID-19 community spread re-escalated in all provinces and an increase in infection rate (6.1%) was recorded. We detected a major decrease in the average temperature (23.5–31.1 °C) and a minor drop in relative humidity (48–62%). We hypothesized that if the decrease in temperature is associated with the increase of positive cases, it might show a further increase in COVID-19 cases in December when the weather became cool and dry. Our analysis confirmed a surge in COVID-19 cases in December with an infection rate of 6.8%. These investigations indicated that from August to October the temperature consistently remained high (35–37.8 °C) with high relative humidity (58–72%) that again paused the community spread of COVID-19 in Pakistan. As the environmental condition changed in November and December, three times increase was witnessed in COVID-19 cases which validated that the SARS-CoV-2 spread fast in cool and dry conditions. The statistical analysis proved that there were significant differences between two consecutive and nonconsecutive months (Table 1) and the winter season (March, April, May, November, December) favored the spread of COVID-19 while the summer season (June, July, August, September, October) data analysis indicated that increase in temperature was associated with a decrease in positive cases (P < 0.02, correlation coefficient r = -0.885). From the current findings, we conclude that a persistent high temperature of 36 °C and above with supportive environmental factors such as high relative humidity (63–72%) has paused the community spread of COVID-19 in Pakistan. Previous studies also showed that the SARS-CoV and MERS-CoV had decreased in survival under temperate and humid environment [2,15] and the outbreak of coronaviruses occurred in cool and dry conditions because these viruses take the advantage of air droplet stability and can easily propagate in nasal passages in a cold environment [16,17]. The COVID-19 epidemic has paused in August (infection rate 2.6%) and September (infection rate 1.92%) but re-emerged in November (infection rate 6.1%) and December (infection rate 6.8%) due to a decrease in ambient temperature. From the present study, the ambient temperature and relative humidity are the suppressive factors for COVID-19 transmission but the possibility of the other factors such as solar energy, sun rays, rainfall, precipitation, and air quality could not be neglected.
Transparency declaration
The authors declare no conflicts of interest.
Acknowledgement
The authors would like to thank Prof. Dr. Tahir Irfan Khan (Vice-Chancellor Abbottabad University of Science and Technology) for his valuable discussion during the project. The study was funded by The Office of Research Innovation and Commercialization, Abbottabad University of Science and Technology (Grant no: AUST/ORIC/2021/375).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nmni.2022.100961.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Table S1. The table showed a detailed comparison of COVID-19, temperature, and infection rate in Islamabad, Karachi, Peshawar, and Lahore.
References
- 1.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infec. 2020;26:729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan K.-H., Peiris J.M., Lam S., Poon L., Yuen K., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mecenas P., Bastos R., Vallinoto A., Normando D. medRxiv; 2020. Effects of temperature and humidity on the spread of COVID-19: a systematic review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandal C.C., Panwar M. Can the summer temperatures reduce COVID-19 cases? Public Health. 2020;185:72–79. doi: 10.1016/j.puhe.2020.05.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan S., Jiang S., Li Z.-L. Do humidity and temperature impact the spread of the novel coronavirus? Front Public Health. 2020;8:240. doi: 10.3389/fpubh.2020.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Science of the Total Environment. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Science of the Total Environment. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Science of the Total Environment. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in Jakarta, Indonesia. Science of The Total Environment. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vinoj V., Gopinath N., Landu K., Behera B., Mishra B. 2020. The COVID-19 spread in India and its dependence on temperature and relative humidity. [Google Scholar]
- 11.Kumar S. Effect of meteorological parameters on spread of COVID-19 in India and air quality during lockdown. Science of the Total Environment. 2020;745:141021. doi: 10.1016/j.scitotenv.2020.141021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deng X., Mettelman R.C., O’Brien A., Thompson J.A., O’Brien T.E., Baker S.C. Analysis of coronavirus temperature-sensitive mutants reveals an interplay between the macrodomain and papain-like protease impacting replication and pathogenesis. Journal of Virology. 2019;93(12) doi: 10.1128/JVI.02140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kakakhel M., Wu F., Khan T., Feng H., Hassan Z., Anwar Z., et al. The first two months epidimiological study of COVID-19, related public health preparedness, and response to the ongoing epidemic in Pakistan. New Microbes and New Infections. 2020;37:100734. doi: 10.1016/j.nmni.2020.100734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaunt E.R., Hardie A., Claas E.C., Simmonds P., Templeton K.E. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48(8):2940–2947. doi: 10.1128/JCM.00636-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Otter J., Donskey C., Yezli S., Douthwaite S., Goldenberg S., Weber D. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect. 2016;92(3):235–250. doi: 10.1016/j.jhin.2015.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang W., Marr L.C. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PloS One. 2011;6(6) doi: 10.1371/journal.pone.0021481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kudo E., Song E., Yockey L.J., Rakib T., Wong P.W., Homer R.J., et al. Low ambient humidity impairs barrier function and innate resistance against influenza infection. PNAS. 2019;116(22):10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The table showed a detailed comparison of COVID-19, temperature, and infection rate in Islamabad, Karachi, Peshawar, and Lahore.