The COVID-19 pandemic underscores the need to address potential risk of transmission of infectious diseases among dental health care workers (DHCWs) and patients. As with the emergence of other novel pathogens, infection control protocols have changed dramatically1 over the past 2 years. Before the 1980s, dentists rarely wore eye protection, masks, or gloves. Our experience with HIV changed that. Today, our protocols include enhanced personal protective equipment, environmental disinfection, and ventilation upgrades.2
During the height of the COVID-19 pandemic, dental offices were forced to close, depriving patients of essential health care services. As offices began reopening, both DHCWs and patients were hesitant to return. Despite low dental office transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),3 worry still exists. Today, almost 2 years since the pandemic began, our workforce is greatly diminished and hiring is difficult.4, 5, 6, 7
Awareness of ongoing SARS-CoV-2 testing practices at an office may help both DHCWs and patients perceive a higher degree of safety. A year into the pandemic, New Jersey dentists, dental hygienists, and dental assistants were surveyed regarding their perceptions of safety. Of the 495 respondents who returned their surveys from December 21, 2020, through February 3, 2021, 47.9% indicated feeling safer if they were tested weekly for COVID-19, 54.5% indicated feeling safer if their coworkers were tested, and 68.0% indicated feeling safer if patients were tested before start of treatment.8
In addition, 21 patients participating in a COVID-19 pilot study (CA Feldman, DMD, unpublished data, March 1, 2022) were asked about their perceptions of COVID-19 testing in dental offices. Patient preferences strongly favored ongoing COVID-19 testing. When asked whether knowing that all patients are tested makes them feel safer when coming for their dental appointments, 94.7% said yes. When asked whether knowing that their dental and office staff members are regularly tested makes them feel safer, 100% said yes. When asked their preference if they had a choice of going to a dental office where patients and staff members are tested or not tested, 89.5% preferred an office that tested patients and staff members. And when respondents were asked to rate on a 5-point Likert scale how comfortable taking a COVID-19 test before treatment made them feel about going to the dentist (ranging from 1-5, in which 1 was a lot more comfortable and 5 was a lot less comfortable), the mean (standard deviation) score was 1.63 (0.68), suggesting that patients would likely favor a dental office that performed regular SARS-CoV-2 screening.
Measures that increase perception of DHCW and patient safety may enhance access and promote delivery of oral health care services. Vaccination is one such tool. However, nonuniform vaccine acceptance, potential emergence of vaccine-resistant variants, likelihood of waning immunity from vaccination with time, and the difficulty in ascertaining vaccination status suggest that consideration of additional measures is warranted. Furthermore, emerging data suggest a tendency for diminished adherence to the use of enhanced personal protection equipment among vaccinated workers, perhaps an unintended consequence of the sense of safety provided by vaccination.9 Another such strategy is regular SARS-CoV-2 screening of DHCWs and patients.10 , 11 SARS-CoV-2 screening, through triage and testing, has become standard practice in many health care environments but has not been adopted widely in dentistry. Factors such as testing availability, cost, convenience, and administrative burden of Clinical Laboratory Improvement Amendments waiver certification and result reporting, as well as understanding the rationale for testing and its acceptance, may influence the adoption of screening for SARS-CoV-2 infection in a dental practice.
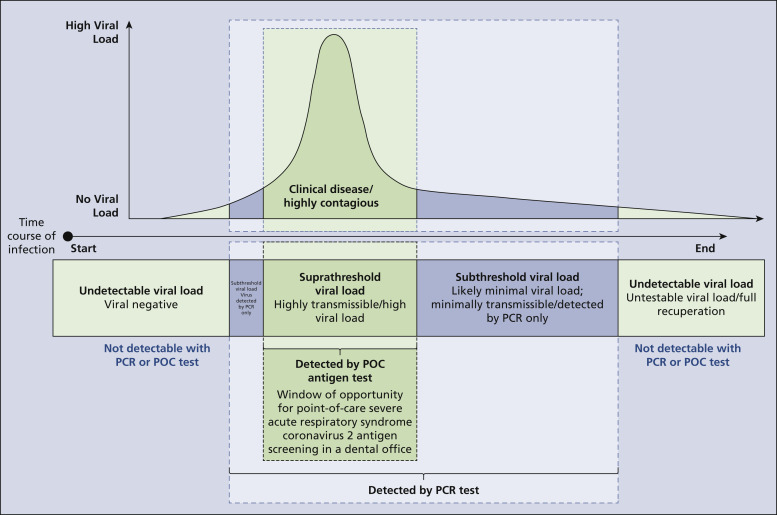
Although triage for COVID-19 symptoms can restrict exposure and infection transmission from symptomatic workers and patients, it does not identify people who are infected but asymptomatic. The figure illustrates how SARS-CoV-2 testing can help identify infected people regardless of the presence of symptoms. It is particularly important to identify infected workers and patients with viral loads that render them infectious and contagious.12
Figure.
A window of opportunity. Point-of-care (POC) antigen testing can detect a high percentage of potentially infectious asymptomatic workers and patients, thereby minimizing transmission risk and increasing workers' and patients' sense of safety. Polymerase chain reaction (PCR) viral testing, perceived to be more accurate than antigen tests, also can be used in a dental office to identify potentially infectious workers and patients; but PCR testing likely also will identify those who are not infectious but have subthreshold viral loads or remnant viral particles.
As point-of-care (POC) sensitivity ranges overlap with SARS-CoV-2 viral loads most likely to enable virus transmission,12 , 13 we posit that POC tests can supplement other mitigation strategies effectively to create the safest possible environment for our patients and coworkers, particularly in regions with high positivity rates or low vaccination rates. Today, POC testing of workers and patients is cost-effective, with kits available for approximately $5 apiece. This can minimize office disruption caused by staffing shortages due to illness and augment DHCW and patient safety.13
SARS-CoV-2 viral clinical diagnostic tests based on high-end real-time polymerase chain reaction (PCR) are designed for high sensitivity and specificity.14 But these tests are expensive and time consuming, and results are not available in a timely manner. From a public health perspective, a low-cost POC-delivery rapid antigen test that can identify most infectious people has great utility in limiting onward spread of infection despite its lower sensitivity. POC rapid antigen tests can identify those carrying higher viral loads and hence are at higher risk of transmitting the infection to others.15 , 16
In contrast, the more protracted turnaround time for the PCR reference standard tests may identify patients with low viral loads who have been out in the community through peak infectivity before being directed to quarantine, especially if asymptomatic. Worse, this may result in quarantining an asymptomatic postinfectious person with waning viral load detectable via PCR at the end of the course of infection. This perspective suggests that we correct our misconception that the rapid antigen tests are less useful because of lower accuracy than is PCR-based testing.17 In fact, the rapid-turnaround POC delivery and lower sensitivity may be the key features that enhance the rapid test’s usefulness.
A high negative predictive value (a high percentage of true-negative test results among all those who test negative) provides assurance that the risk of contracting an infectious disease from a patient or coworker would be minimal, given how unlikely it is that the patient or coworker has the infectious pathogen. A high positive predictive value (a high percentage of true-positive test results among all those who test positive), in contrast, limits needlessly putting workers on sick leave or canceling a patient visit owing to a false-positive test. As a screening test, the POC rapid antigen test has high negative predictive value during a period of low prevalence and a high positive predictive value when the community prevalence is higher.
Conclusions
SARS-CoV-2 carries significant morbidity and mortality. Screening for SARS-CoV-2 is 1 effective mitigation strategy that could be added to a practitioner’s armamentarium. Understanding the strengths and weaknesses of available tests for screening, coupled with an assessment of local disease prevalence, can help drive specific decisions for each practice. As there are limitations to POC testing, practitioners should continue to implement engineering and work practice controls as a means to mitigate SARS-CoV-2 transmission and create a safer dental practice environment. The POC rapid antigen test should be considered, as it provides an easy, cost-effective means to screen for infectivity and helps identify most virus-positive people in real time, thereby decreasing risk of transmission and augmenting workers’ and patients’ sense of safety.
Biographies
Dr. Feldman is the dean and a professor, Rutgers School of Dental Medicine, Newark, NJ; a professor, Rutgers School of Public Health, Rutgers University, Piscataway, NJ; and an adjunct professor, School of Dental Medicine, University of Pennsylvania, Philadelphia, PA.
Dr. Fredericks-Younger is an assistant dean for graduate programs and an assistant professor, Rutgers School of Dental Medicine, Newark, NJ.
Dr. Subramanian is an associate professor, Rutgers School of Dental Medicine, Newark, NJ.
Dr. Gennaro is a professor, Rutgers New Jersey Medical School, Newark, NJ and a professor, Rutgers School of Public Health, Rutgers University, Piscataway, NJ, principal investigator, Public Health Research Institute, Rutgers New Jersey Medical School, Newark, NJ; a member, Cancer Institute of New Jersey, New Brunswick, NJ; and a core member, Global Health Institute, New Brunswick, NJ.
Dr. Coker is an assistant professor, Rutgers School of Dental Medicine, Newark, NJ, and an assistant professor, Rutgers School of Public Health, Rutgers University, Piscataway, NJ.
Dr. Fine is the chair and a professor, Rutgers School of Dental Medicine, Newark, NJ.
Footnotes
Disclosures. None of the authors reported any disclosures.
Research reported in this publication was supported by the National Institute of Dental & Craniofacial Research of the National Institutes of Health under awards U19DE028717, U01DE028727, and X01DE030407. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors wish to thank Veerasathpurush Allareddy, Cyril Meyerowitz, MaryAnn McBurnie, Ellen Funkhouser, Pat Ragusa, Sara Gill, and Julie Chapman-Green for their guidance and assistance.
Commentaries represent the opinions of the authors and not necessarily those of the American Dental Association.
References
- 1.Samaranayake L., Fakhruddin K.S. Pandemics past, present, and future: their impact on oral health care. JADA. 2021;152(12):972–980. doi: 10.1016/j.adaj.2021.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Update to office procedures during COVID-19. American Dental Association. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/coronavirus/update_to_office_procedures_during_covid19.pdf
- 3.Estrich C.G., Mikkelsen M., Morrissey R., et al. Estimating COVID-19 prevalence and infection control practices among US dentists. JADA. 2020;151(11):815–824. doi: 10.1016/j.adaj.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19: economic impact on dental practices week of November 15, 2021 QOW results. American Dental Association, Health Policy Institute. https://surveys.ada.org/reports/RC/public/YWRhc3VydmV5cy02MThkNzE2ODQzYmNkMDAwMGZjMGY0ZWMtVVJfM3BaeGhzWm12TnNMdjB4
- 5.Gurenlian J.R., Morrissey R., Estrich C.G., et al. Employment patterns of dental hygienists in the United States during the COVID-19 pandemic. J Dent Hyg. 2021;95(1):17–24. [PubMed] [Google Scholar]
- 6.Mensik H. Patients were still hesitant to seek medical care out of virus fears this spring, survey finds. Healthcare Dive. https://www.healthcaredive.com/news/patients-were-still-hesitant-to-seek-medical-care-out-of-virus-fears-this-s/605224/
- 7.Versaci M.B. Understaffed and ready to hire, dentists face applicant shortages as they emerge from COVDI-19 pandemic. ADA News. June 9, 2021. https://www.ada.org/publications/ada-news/2021/june/dentists-face-applicant-shortages-as-they-emerge-from-covid-19-pandemic
- 8.Coker M.O., Subramanian G., Davidow A., et al. Impact of DHCWs’ safety perception on vaccine acceptance and adoption of risk mitigation strategies. JDR Clin Trans Res. February 22, 2022 doi: 10.1177/23800844211071111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chandu VC, Baddam VRR, Mupparapu M, Marella Y. Vaccination induced complacency in adherence to COVID-19 precautionary measures among oral health care professionals in India and the United States: a retrospective pretest-posttest design. Hum Vaccin Immunother. Published online October 6, 2021. https://doi.org/10.1080/21645515.2021.1978794 [DOI] [PMC free article] [PubMed]
- 10.Shirazi S., Stanford C.M., Cooper L.F. Testing for COVID-19 in dental offices: mechanism of action, application, and interpretation of laboratory and point-of-care screening tests. JADA. 2021;152(7):514–525.e8. doi: 10.1016/j.adaj.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lieberthal B., McCauley L.K., Feldman C.A., Fine D.H. COVID-19 and dentistry: biological considerations, testing strategies, issues, and regulations. Compend Contin Educ Dent. 2021;42(6):290–297. [PubMed] [Google Scholar]
- 12.Jones T.C., Biele G., Mühlemann B., et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science. 2021;373(6551):eabi5273. doi: 10.1126/science.abi5273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corman V.M., Haage V.C., Bleicker T., et al. Comparison of seven commercial SARS-CoV-2 rapid point-of-care antigen tests: a single-centre laboratory evaluation study. Lancet Microbe. 2021;2(7):e311–e319. doi: 10.1016/S2666-5247(21)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forde J.E., Ciupe S.M. Quantification of the tradeoff between test sensitivity and test frequency in a COVID-19 epidemic: a multi-scale modeling approach. Viruses. 2021;13(3):457. doi: 10.3390/v13030457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mina M.J., Parker R., Larremore D.B. Rethinking Covid-19 test sensitivity: a strategy for containment. N Engl J Med. 2020;383(22) doi: 10.1056/NEJMp2025631. [DOI] [PubMed] [Google Scholar]
- 16.Mina M.J., Peto T.E., García-Fiñana M., Semple M.G., Buchan I.E. Clarifying the evidence on SARS-CoV-2 antigen rapid tests in public health responses to COVID-19. Lancet. 2021;397(10283):1425–1427. doi: 10.1016/S0140-6736(21)00425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petersen I., Crozier A., Buchan I., Mina M.J., Bartlett J.W. Recalibrating SARS-CoV-2 antigen rapid lateral flow test relative sensitivity from validation studies to absolute sensitivity for indicating individuals shedding transmissible virus. Clin Epidemiol. 2021;13:935–940. doi: 10.2147/CLEP.S311977. [DOI] [PMC free article] [PubMed] [Google Scholar]