Abstract
Background: Treatments of pilon fracture is an important operative challenge due to high prevalence of post-operative complications. In this paper, we aimed to evaluate the complications of the use of low profile plates for pilon fractures. Methods: This clinical trial that was performed in 2017-2021 in Isfahan on 27 patients with pilon fractures. Demographic data of patients such as age, gender, type of pilon fracture and baseline pathology of pilon fractures were collected. Patients were treated using low profile plates under surgical procedures. Within 1 month, 3 months and 6 months after surgeries, patients were visited and assessed regarding superficial wound infections, deep wound infections, and evidence of osteomyelitis, vascular injuries, non-union and mal-union using both physical examinations and imaging studies via X-ray. We also measured the functions of cases using The American Orthopedic Foot and Ankle Score (AOFAS) questionnaire. Results: Most cases had 3 days (33.3%) and 5 days (33.3%) of hospitalization. Superficial wound infection was observed in 7 cases (26%). Deep surgical site infections were observed in 2 cases (7.4%) and we had only 1 case of osteomyelitis (3.7%). No vascular injuries were observed in this study. Evaluation of union among patients showed that 2 cases (7.4%) had non-union and 5 cases (18.5%) had malunion in the anterior-posterior axis, but none of the patients had malunion in the coronal axis. Based on AOFAS questionnaire, the mean score in patients was 88.36±14.20. Conclusion: Treatments of pilon fractures by low profile plates have similar complications compared to other treatment options.
Keywords: Pilon, fracture, complication
Introduction
A pilon fracture is a fracture of the distal tibia in the metaphyseal region of the bone that also affects the articular surface of the ankle and can extend to the diaphysis area of the bone [1]. Pilon fractures are caused by rotational or axial forces, mainly due to falls from heights or accidents caused by motor vehicles [2]. Pilon fractures are rare, accounting for 3 to 10 percent of tibial bone fractures and 1 percent of lower limb fractures, but these fractures involve a large portion of the tibial joint surface in the ankle joint that bears the weight of the body [3,4]. Therefore, this fracture is associated with many complications and treatments do not have a very favorable outcome for the patient.
This fracture is usually accompanied by damage to the surrounding soft tissue. There are limited muscles between the skin and bone surfaces at this level of the lower extremities [5]. Damage energy can be transmitted directly to these soft tissue structures and cause damage to them. Open fractures are common, and even if there is no open lesion, the fracture is usually associated with significant soft tissue damage [1,6]. Furthermore, microscopic damage to the articular cartilage during trauma can cause long-term complications, even with careful reduction [7].
Treatment of pilon fractures is one of the most important challenges for surgeons. There are many features in this type of fracture that are responsible for this challenge, but the most important of them are soft tissue damage and also damage to the distal articular surface of the ankle [8]. According to studies, the amount of joint surface crushing, smoking and age are the most important factors influencing the final outcome of treatment [5,9]. Early surgery following a pilon fracture, due to the thin covering of soft tissue around it, does not heal the wound and increases the risk of infection and potentially carries the risk of amputation. Temporary use of an external stabilizer with or without fibula fixation is a first-line intervention for this type of fracture and is considered a temporary “injury control” strategy [3]. The choice of treatment for pilon fractures varies based on the severity of the soft tissue injury, the fracture pattern, and the surgeon’s experience. There is currently no conclusive evidence of the effectiveness of a particular treatment, such as the use of internal or external stabilizers for this type of fracture, and these methods are usually used alone or in combination to treat patients [10].
There are several treatment options for pilon fractures, each with its own disadvantages and advantages. If there is not enough soft tissue or in cases of open pilon fractures, fibular plates should be used in initiate treatments associated with antro-lateral or antro-medial distal tibial plates.
These treatments include: Closed reduction and casting, combined use of IMN and plate, open reduction, and the use of internal fixation (ORIF), minimally invasive plate osteosynthesis, external stabilization and two-step method of using external stabilization and ORIF [11-13]. In addition to disagreements about the best treatment option, there is controversy about the appropriate time to treat pilon fractures.
Low profile plates are widely used in orthopedic surgeries and are easily bent and have lower thickness compared to other plates. Reconstruction plates or distal radius minimal T-plates are some known low profile plates. Since there is no definitive treatment for pilon fracture and each of the proposed methods to treat this fracture has different benefits and complications, we decided to review the results of treatment of pilon fracture using low profile plates.
Methods and material
Study design
This is a cross-sectional study that was performed in 2017-2021 in Kashani and Al-Zahra hospitals affiliated to Isfahan University of Medical Science. The current study was conducted on patients with pilon fracture using census sampling method. The study protocol was approved by Research committee of Isfahan University of Medical Sciences and the Ethics committee has confirmed it (Ethics code: IR.MUI.MED.REC.1399.429, Iranian Registry of Clinical Trials code: IRCT20200217046523N8).
Inclusion and exclusion criteria
The inclusion criteria were diagnosis of pilon fracture by expert orthopedic, candidate for usage of low profile plates and signing the written informed consent to participate in this study. The exclusion criteria were previous fractures in lower limb, anatomical deformity in ankle, history of neuromuscular diseases such as polio, history of systemic diseases such as diabetes mellitus, presence of simultaneous fractures in the limb, open fracture and massive damage to soft tissue.
Data collection
All patients with pilon fracture that referred to our medical centers entered the study based on inclusion and exclusion criteria. Demographic data of patients such as age, gender, type of pilon fracture and baseline pathology of pilon fractures were collected. Figure 1 indicates the pilon fracture before the treatments by X-ray and Figure 2 shows the pre-operative CT scan of the fracture sites.
Figure 1.

Pilon fracture before treatments by AP x-ray indicating tibia and fibula fractures.
Figure 2.

Pre-operative CT scan of the fracture sites.
Fracture type assessments
Type of pilon fractures was assessed using AO Foundation and Orthopaedic Trauma Association (AO/OTA) classification. Based on this classification, fractures are categorized using alphabets and numbers. The first number indicates the fractured bone. In this regard, 4 is tibia. The second number indicates part of the bone that has fracture. In this regard, 3 is distal of tibia. Based on alphabets, A indicates extra-articular fractures outside 5 cm of the ankle joint and B indicates minor joint damage. Group C represents complete joint damage in which there is no direct continuity between the bone diaphysis and the joint section. This group is used for the majority of high-energy pylon fractures. The final numbers in this classification represent the subgroups of each type and indicate the degree of fragmentation of the joint components.
Surgical procedures
Patients were treated using low profile plates under surgical procedures (Figure 3). Within 1 month, 3 months and 6 months after surgeries (Figure 4), patients were visited and assessed regarding superficial wound infections, deep wound infections, and evidence of osteomyelitis, vascular injuries, non-union and mal-union using both physical examinations and imaging studies via X-ray.
Figure 3.
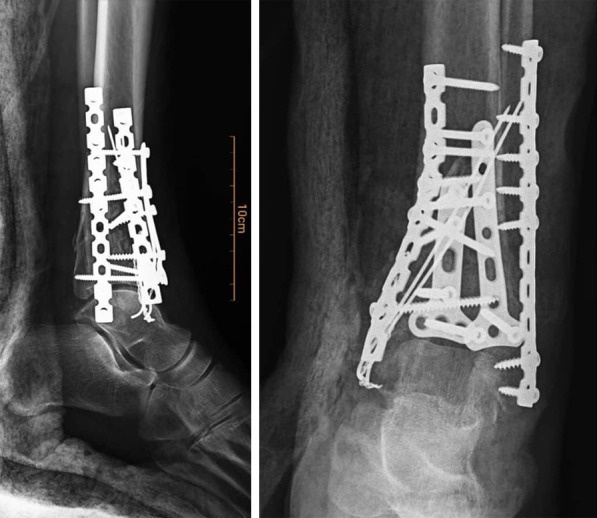
Post-operative imaging of the patients.
Figure 4.

Imaging of the treated limb 3 months after surgical operations.
Follow-up and AOFAS questionnaire
After 6 months, The American Orthopedic Foot and Ankle Score (AOFAS) questionnaire was filled for all patients. AOFAS is a reliable and reproducible measurement tool which is commonly used for the assessment of foot and ankle conditions. This score may be used to assess the ankle, subtalar, talonavicular, and calcaneocuboid joint levels and may be useful for fractures, arthroplasty, arthrodesis, and instability procedures ranging from 0 to 100, with healthy ankles receiving 100 points. This tool covers three main categories: Pain (40 points), function (50 points) and alignment (10 points). The validity and reliability of this questionnaire in Iranian population was approved by Sayyed-Hosseinian and colleagues in 2018 [14].
Statistical analysis
The obtained data were entered into the Statistical Package for Social Sciences (SPSS) (version 24, SPSS Inc., Chicago, IL). Quantitative data were reported as mean ± standard deviation and qualitative data as frequency distribution (percentage). Independent t-test, Chi-square were used to analyze the data. P-value <0.05 was considered as significance threshold.
Results
Study population and fracture types
In this study, data of 27 patients were analyzed. The study population consisted of 22 males (81.5%) and 5 females (18.5%) with a mean age of 48.7±9.55 years. Initial data analysis indicated that 19 patients (70.4%) were smokers and most of the cases had type 2 of pilon fractures (51.9%). These data are indicated in Table 1.
Table 1.
Evaluation of different demographic data of patients
| Variable | Number (%)/mean ± SD | |
|---|---|---|
| Age (year) | 48.7±9.55 | |
| Gender | Male | 22 (81.5%) |
| Female | 5 (18.5%) | |
| Smoking | 19 (70.4%) | |
| Fracture type | 1 | 0 |
| 2 | 14 (51.8%) | |
| 3 | 13 (48.2%) | |
Hospitalization duration and surgical complications
We also found that most cases had 3 days (33.3%) and 5 days (33.3%) of hospitalization. Superficial wound infection was observed in 7 cases (26%). Deep surgical site infections were observed in 2 cases (7.4%) and we had only 1 case of osteomyelitis (3.7%). No vascular injuries were observed in this study.
Evaluation of union among patients showed that 2 cases (7.4%) had non-union and 5 cases (18.5%) had malunion in the anterior-posterior axis, but none of the patients had malunion in the coronal axis (Table 2). We also compared data between patients with type 2 and 3 of fractures but no significant differences could be observed between these patients regarding the surgical complications.
Table 2.
Evaluation of different post-operative factors
| Variable | Number (%) | P-value* | |||
|---|---|---|---|---|---|
|
| |||||
| Type 2 14 | Type 3 13 | Total | |||
| Hospitalization duration (days) | 3 | 5 (35.7%) | 4 (30.7%) | 9 (33.3%) | 0.151 |
| 4 | 4 (28.5%) | 3 (23.1%) | 7 (25.9%) | 0.332 | |
| 5 | 5 (35.7%) | 4 (30.7%) | 9 (33.3%) | 0.079 | |
| 7 | 1 (7.1%) | 1 (7.7%) | 2 (7.5%) | >0.99 | |
| Superficial wound infection | 4 (28.5%) | 3 (23.1%) | 7 (26%) | 0.247 | |
| Deep surgical site infection | 1 (7.1%) | 1 (7.7%) | 2 (7.4%) | >0.99 | |
| Osteomyelitis | 1 (7.1%) | 0 | 1 (3.7%) | 0.063 | |
| vascular injuries | 0 | 0 | 0 | - | |
| Non-union | 1 (7.1%) | 1 (7.7%) | 2 (7.4%) | >0.99 | |
| Malunion in the anterior-posterior axis | 3 (21.4%) | 2 (15.4%) | 5 (18.5%) | 0.663 | |
| Malunion in the coronal axis | 0 | 0 | 0 | - | |
Comparing type 2 and 3.
Lower limb function assessments
Based on AOFAS questionnaire, the mean score in patients was 88.36±14.20. We also measured the mean scores in each domain of the questionnaire. These data are summarized in Table 3.
Table 3.
AOFAS questionnaire mean score in patients
| Variable | Mean ± SD |
|---|---|
| Total AOFAS score | 88.36±14.20 |
| Pain | 35.21±8.69 |
| Function | 44.92±7.24 |
| Alignment | 8.21±1.65 |
Risk assessments for complications
Based on our data, from all patients with non-union and mal-union, 6 cases (85.7%) had histories of smoking which was statistically significant (P<0.001). We also assessed the risks for different complications including non-union, mal-union, superficial and deep wound infection, and osteomyelitis based on smoking condition (compared to non-smokers). Our data showed that smoking was associated with significant increased risks for non-union (OR=1.840), superficial wound infection (OR=1.145) and osteomyelitis (OR=1.112) (P<0.05 for all). These data are shown in Table 4.
Table 4.
Assessments of risks for different complications based on smoking situation
| Condition | P-value | Odds ratio (OR) | CI (95%) | |
|---|---|---|---|---|
|
| ||||
| Upper | Lower | |||
| Non-union | 0.018 | 1.840 | 1.720 | 1.016 |
| Mal-union | 0.162 | Not significant | - | - |
| superficial wound infection | 0.018 | 1.145 | 1.711 | 1.047 |
| deep wound infection | 0.213 | Not significant | - | - |
| osteomyelitis | 0.003 | 1.112 | 1.621 | 1.120 |
Using Pearson’s regression test.
Discussion
In the present study, we assessed the therapeutic results of pilon fractures using low profile plates among 27 patients. Based on our results, most cases had 3 days and 5 days of hospitalization. The prevalence of superficial wound infection was 26% and deep surgical site infections were observed 7.4% of cases and 3.7% of them had osteomyelitis. We observed no vascular injuries among patients. We also assessed the non-union and malunion rates in patients and observed that 7.4% of cases had non-union and 18.5% had malunion in the anterior-posterior axis, but none of the patients had malunion in the coronal axis.
Furthermore, by evaluating the scores of AOFAS questionnaire we found that the mean score was 88.36±14.20 among patients that indicate the effectiveness of low profile plates for treatments of pilon fractures.
There have been various data evaluating possible operative options for pilon fractures and only few have assessed the use of low profile plates. In 2009, Borens and colleagues evaluated data of 17 patients in the United States that have been operated with low profile plates between 1999 and 2001 for a tibial plafond fracture. Based on this study, all cases had fracture union within 14 weeks and no fixation failure was observed. Assessments of treatment results showed that 47% of cases had an excellent result; 41% had a fair result whereas 12% had a poor result. It was also recommended that the use of low profile plates was effective for the treatment of pilon fractures and should be used in conjunction with a staged procedure in the acute trauma setting [15]. Another study was conducted by Tarkin and others that assessed various treatment options for pilon fractures. It was indicated that the use of low profile plates could be associated with acceptable results with lower rates of complications compared to other options [16]. In 2016, Tomás-Hernández and colleagues showed that treating pilon fractures should be performed with the least complications including superficial or deep wound infections [17]. Based on our results, the use of low profile plates for pilon fractures was associated with good therapeutic results and least complications.
An important point of the currents study was that we observed 26% superficial wound infection and 7.4% deep surgical site infections and 3.7% osteomyelitis among our cases. In a study by Sajjadi and colleagues in 2018, they investigated 21 cases undergoing primary ORIF and 20 cases undergoing two-stage approaches for pilon fractures. It was reported that in each group, 9.5% of cases had superficial wound infection, and no deep wound infection and osteomyelitis were observed [18]. It seems that the rates of these complications were higher in our study. In 2021, Janssen and colleagues showed that the rates of infections and osteomyelitis could vary from 5 to 25% in different approaches to pilon fracture and no definite therapeutic technique could be chosen [19].
Furthermore, we found that 7.4% of cases had non-union and 18.5% had malunion in the anterior-posterior axis. Similar results were reported by Danoff and colleagues by assessing 28 open pilon fractures [20]. In another study by Daniels in 2021, they indicated that treatment of pilon fractures by ORIF could be associated with higher rates of non-union and malunion. They declared that more than 20% of cases could suffer from future malunion mostly in anterior-posterior axis and almost 7% of cases had non-union [21]. These data are in line with the findings of our study showing the effectiveness of low profile plates in pilon fractures. We collected the data regarding the complications in previous studies and compared them to our data in Table 5. Based on these findings, we observed similar or higher rates of complications compared to the previously reported papers but the rates of malrotation in the coronal axis were significantly lower in our report.
Table 5.
Summarizing the complications in previous studies and our data
| Complication | Previous study | Our data | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Borens and colleagues [15] | Sajjadi and colleagues [18] | Janssen and colleagues [19] | Danoff and colleagues [20] | Daniels [21] | ||
| Superficial wound infection | N.R | 9.5% | 6% | N.R | 29% | 26% |
| Deep surgical site infection | N.R | 0 | 6% | 14.3% | N.R | 7.4% |
| Osteomyelitis | N.R | 0 | N.R | N.R | 2% | 3.7% |
| vascular injuries | N.R | 0 | N.R | N.R | N.R | 0 |
| Non-union | N.R | 4.8% | N.R | 7.1% | 7% | 7.4% |
| Malunion in the anterior-posterior axis | 12% | 9.5% | 12% | N.R | 20% | 18.5% |
| Malunion in the coronal axis | N.R | 4.8% | N.R | N.R | N.R | 0 |
N.R: not reported.
It should be noted that the important point of the current study was that only few studies have been conducted in this regard and similar studies are restricted in number especially in our region. The results of our study showed that superficial wound infection was the most common complication in patients and therefore, surgeons should pay more attention to the prophylactic strategies in patients. Furthermore, we assessed the complications of low profile plates in patients with pilon fractures and showed relatively lower or similar rates of complications compared to other surgical techniques in previous reports but the complications were almost similar to the studies that assessed low profile plates for pilon fractures. This could be justified as variations in the study populations and characteristics.
Indeed, previous studies have shown similar results and complications for other techniques including ORIF or two-stage operations but we believe that low profile plates have higher effectiveness and similar complications and as a result, we recommend that further attention should be given to the use of low profile plates in treatments of pilon fractures. We should note that the limitations of our study were restricted study population and not comparing the therapeutic outcomes with other techniques. On the other hand, we believe that these findings could have high clinical importance due to the limited conducted studies in this regard.
Conclusion
Treatments of pilon fractures by low profile plates have similar complications compared to other treatment options. These plates are easier to use and we recommend that orthopedic surgeons should pay more attention to the benefits of low profile plates.
Disclosure of conflict of interest
None.
References
- 1.Kottmeier SA, Madison RD, Divaris N. Pilon fracture: preventing complications. J Am Acad Orthop Surg. 2018;26:640–651. doi: 10.5435/JAAOS-D-17-00160. [DOI] [PubMed] [Google Scholar]
- 2.Falzarano G, Pica G, Medici A, Rollo G, Bisaccia M, Cioffi R, Pavone M, Meccariello L. Foot loading and gait analysis evaluation of nonarticular tibial pilon fracture: a comparison of three surgical techniques. J Foot Ankle Surg. 2018;57:894–898. doi: 10.1053/j.jfas.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 3.Fahim M, Rafiee Zadeh A, Shoureshi P, Ghadimi K, Cheshmavar M, Sheikhinia N, Afzali M. Alcohol and multiple sclerosis: an immune system-based review. Int J Physiol Pathophysiol Pharmacol. 2020;12:58–69. [PMC free article] [PubMed] [Google Scholar]
- 4.Chaparro F, Ahumada X, Urbina C, Lagos L, Vargas F, Pellegrini M, Barahona M, Bastias C. Posterior pilon fracture: epidemiology and surgical technique. Injury. 2019;50:2312–2317. doi: 10.1016/j.injury.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Liangjun J, Qiang Z, Hang L, Zhijun P. Injury mechanism, fracture characteristics and clinical treatment of pilon fracture with intact fibula-a retrospective study of 23 pilon fractures. J Clin Orthop Trauma. 2017;8(Suppl 2):S9–S15. doi: 10.1016/j.jcot.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett A, Ramaskandhan J, Siddique M. Total ankle replacement for osteoarthritis following pilon fracture of the tibia. Foot Ankle Int. 2018;39:1008–1018. doi: 10.1177/1071100718793091. [DOI] [PubMed] [Google Scholar]
- 7.Haddad S, Ghadimi K, Abrishamkar R, Asl NSM. Comparing laparoscopy and laparotomy procedures in the radical hysterectomy surgery for endometrial cancer: a basic review. Am J Transl Res. 2021;13:2456–2461. [PMC free article] [PubMed] [Google Scholar]
- 8.Wu D, Peng C, Ren G, Yuan B, Liu H. Novel anterior curved incision combined with MIPO for Pilon fracture treatment. BMC Musculoskelet Disord. 2020;21:176. doi: 10.1186/s12891-020-03207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang SB, Zhang YB, Wang SH, Zhang H, Liu P, Zhang W, Ma JL, Wang J. Clinical efficacy and safety of limited internal fixation combined with external fixation for Pilon fracture: a systematic review and meta-analysis. Chin J Traumatol. 2017;20:94–98. doi: 10.1016/j.cjtee.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogha M, Abtahi H, Asadpour L, Ghazavi H, Pourmohammadi R, Maleki M, Ghadimi K. Therapeutic effect of intratympanic injection of dexamethasone plus hyaluronic acid on patients with Meniere’s disease. Iran J Otorhinolaryngol. 2019;31:217–223. [PMC free article] [PubMed] [Google Scholar]
- 11.Wadehra A, Douthett S, Fallat LM. Single-stage tibiotalocalcaneal arthrodesis with use of an antibiotic-coated intramedullary nail for limb salvage following an open pilon fracture complicated by osteomyelitis: a case report. J Foot Ankle Surg. 2019;58:984–988. doi: 10.1053/j.jfas.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Keiler A, Riechelmann F, Thöni M, Brunner A, Ulmar B. Three-dimensional computed tomography reconstruction improves the reliability of tibial pilon fracture classification and preoperative surgical planning. Arch Orthop Trauma Surg. 2020;140:187–195. doi: 10.1007/s00402-019-03259-8. [DOI] [PubMed] [Google Scholar]
- 13.Scaglione M, Celli F, Casella F, Fabbri L. Tibial pilon fractures treated with hybrid external fixator: analysis of 75 cases. Musculoskeletal Surg. 2019;103:83–89. doi: 10.1007/s12306-018-0550-z. [DOI] [PubMed] [Google Scholar]
- 14.Sayyed-Hosseinian SH, Hassankhani GG, Bagheri F, Alavi N, Shojaie B, Mousavian A. Validation of the Persian version of the American orthopedic foot and ankle society score (AOFAS) questionnaire. Arch Bone Jt Surg. 2018;6:233–239. [PMC free article] [PubMed] [Google Scholar]
- 15.Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg. 2009;129:649–659. doi: 10.1007/s00402-006-0219-1. [DOI] [PubMed] [Google Scholar]
- 16.Tarkin I, Clare M, Marcantonio A, Pape H. An update on the management of high-energy pilon fractures. Injury. 2008;39:142–154. doi: 10.1016/j.injury.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 17.Tomás-Hernández J. High-energy pilon fractures management: state of the art. EFORT Open Rev. 2016;1:354–361. doi: 10.1302/2058-5241.1.000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sajjadi MM, Ebrahimpour A, Okhovatpour MA, Karimi A. The outcomes of pilon fracture treatment: primary open reduction and internal fixation versus two-stage approach. Arch Bone Jt Surg. 2018;6:412–419. [PMC free article] [PubMed] [Google Scholar]
- 19.Janssen SJ, Kloen P. Supercutaneous locking compression plate in the treatment of infected non-union and open fracture of the leg. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-04104-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danoff JR, Saifi C, Goodspeed DC, Reid JS. Outcome of 28 open pilon fractures with injury severity-based fixation. Eur J Orthop Surg Traumatol. 2015;25:569–575. doi: 10.1007/s00590-014-1552-7. [DOI] [PubMed] [Google Scholar]
- 21.Daniels NF, Lim JA, Thahir A, Krkovic M. Open Pilon fracture postoperative outcomes with definitive surgical management options: a systematic review and meta-analysis. Arch Bone Jt Surg. 2021;9:272. doi: 10.22038/abjs.2020.53240.2641. [DOI] [PMC free article] [PubMed] [Google Scholar]


