Abstract
EFSA received a mandate from the EC to assess the effectiveness of some of the control measures against diseases included in the Category A list according to Regulation (EU) 2016/429 on transmissible animal diseases (‘Animal Health Law’). This opinion belongs to a series of opinions where these control measures are assessed, with this opinion covering the assessment of control measures for Lumpy Skin Disease (LSD). In this opinion, EFSA and the AHAW Panel of experts review the effectiveness of: i) clinical and laboratory sampling procedures, ii) monitoring period and iii) the minimum radius of the protection and surveillance zones, and the minimum length of time that measures should be applied in these zones. The general methodology used for this series of opinions has been published elsewhere; nonetheless, the transmission kernels used for the assessment of the minimum radius of the protection and surveillance zones are shown. Several scenarios for which these control measures had to be assessed were designed and agreed prior to the start of the assessment. The monitoring period was assessed as effective, and based on the transmission kernels available, it was concluded that the protection zone of 20 km radius and the surveillance zone of 50 km radius would comprise > 99% of the transmission from an affected establishment if transmission occurred. Recommendations provided for each of the assessed scenarios aim to support the European Commission in the drafting of further pieces of legislation, as well as for plausible ad hoc requests in relation to LSD.
Keywords: disease control measures, Lumpy Skin Disease, LSD, sampling procedures, monitoring period, protection zone, surveillance zone
Summary
This opinion is part of a series of opinions, in which the three‐first Terms of Reference (ToR) of a mandate received from the European Commission have been considered. The background and specific details of this mandate can be found in the opinion. The ToRs in this mandate request an assessment of the effectiveness of:
the clinical and laboratory examination in their capacity to detect disease (or estimate the disease prevalence within an establishment), either in suspect or confirmed animals in a single establishment, or in establishments within restriction zones (ToR 1);
the effectiveness of the duration of the monitoring period (for different scenarios) in the control of suspected and confirmed outbreaks (ToR 2);
the size and duration of the restriction zones, in their capacity for mitigating disease spread (ToR 3).
In order to harmonise the approach to these assessments, the methodology used in this series of opinions, covering all Category A diseases, was agreed on, and published in a separate technical report.
Specific clinical and laboratory procedures for Lumpy Skin Disease (LSD) for each scenario of ToR1 have not been found in the EU legislation. Given that the skin nodules are pathognomonic for LSD and the fact that the sensitivity of polymerase chain reaction (PCR) is higher in tissues (skin and ophthalmic/oral/nasal discharges), laboratory testing to confirm or rule out the disease should target animals with skin nodules. Specific sampling procedures for clinical and laboratory examination have been provided for some scenarios.
To answer ToR 2, and to assess the minimum duration of measures to be implemented in the protection and surveillance zones (ToR 3.2), an extensive literature search (ELS) was carried out. This ELS aimed to assess the average, shortest and longest period between the earliest point of infection of cattle with LSD virus and the time of reporting of a suspicion by the competent authority. The average time to the reporting of a suspicion report was then used to assess the effectiveness of the length of monitoring periods. For most of the scenarios, the existing length of the monitoring period for LSD (28 days) was considered sufficient. Some recommendations were given for some of the relevant scenarios. To assess the effectiveness of the minimum length of time in which the measures should be applied in the protection and surveillance zones, the average and the longest time assessed via the ELS were used, respectively. In this regard, the minimum length of time the protection zone (28 days) and the surveillance zone (45 days) that must be in place according to existing legislation, were considered effective.
To assess the effectiveness of the minimum radius to be implemented in the protection and surveillance zones (ToR 3.1), transmission kernels were used. These kernels had been built using data from previous outbreaks in Israel and Albania. These kernels represent the relative risk of transmission to each individual establishment from the affected establishment. For LSD, it was observed that, assuming transmission from an affected establishment occurs, the probability of transmission beyond the protection zone of 20 km was 0.3% (Israel kernel) or 0.2% (Albania kernel). The probability of infection of an establishment located beyond 50 km is less than 0.1% for both kernels. However, transmission to longer distances cannot be excluded if infected animals moved outside the zones.
1. Introduction
1.1. Background and Terms of Reference as provided by the requestor
Regulation (EU) 2016/429 on transmissible animal diseases (‘Animal Health Law’), hereinafter referred to as Animal Health Law (AHL), requires the Commission to lay down detailed rules on the disease control measures against listed diseases as referred to in point (a), (b) and (c) of its Article 9 (category A, B and C diseases). The Commission is empowered to adopt delegated acts supplementing the rules laid down in Part III of Regulation (EU) 2016/429 on transmissible animal diseases (AHL) on disease control measures for listed diseases as referred to in point (a), (b) and (c) of its Article 9 (category A, B and C diseases). Therefore, the Commission has developed and adopted a Delegated Regulation laying down rules for the prevention and control of certain diseases (‘the Delegated Regulation’). The rules laid down in the Delegated Regulation are in respect of terrestrial animals largely replicating the rules currently in force concerning the disease control measures in the event of animal diseases with serious effects on the livestock as they have proven to be effective in preventing the spread of those diseases within the Union. Consequently, many animal disease control measures laid down in existing Directives will be, to the extent that not already done by the Animal Health Law, replaced by the rules provided in the Delegated Regulation. At the same time, these rules have been aligned with the international standards from the World Organisation for Animal Health (OIE), wherever these existed. However, certain disease control measures proposed in the Delegated Regulation, in particular in its Annexes, were considered as outdated i.e. possibly not based on most recent scientific evidence at the time of development. Their review is considered as necessary. Moreover, for those category A diseases for which rules were not established before or were not detailed enough, certain disease control and risk mitigating measures are, due to the lack of scientific basis, extrapolated from other diseases, for which rules existed in the past. Finally, for some other diseases the evidence and scientific knowledge, was not available to the Commission and to the Member States at the time of developing the Delegated Regulation due to the time constraints. The following diseases are examples of the later: infection with Rift Valley fever (RVF), infection with Mycoplasma mycoides subsp. Mycoides SC (Contagious bovine pleuropneumonia) (CBPP), Contagious caprine pleuropneumonia (CCPP), Sheep pox and goat pox, infection with Peste des petits ruminants virus (PPRV), African horse sickness (AHS), Glanders. In this regard, the existing rules will cease to apply as from the date of application of the Animal Health Law and its complementing legislation including the Delegated Regulation, i.e. from 21 April 2021. Certain of the proposed measures for the prevention and control of category A diseases of terrestrial animals should therefore be assessed in order to ensure that they are effective and updated based on the latest scientific knowledge in this new set of legislation. This is particularly important in the case of those diseases that are less common or have been never reported in the Union.
1.1.1. ToR 1: Sampling of animals and establishments for the detection of category A diseases in terrestrial animals
Based on available scientific information, assess the effectiveness of existing sampling procedures to detect or rule out the presence of each category A disease of terrestrial animals and, in case of absence of effective procedures, develop them, in order to complete the rules provided for in Annex I to the Delegated Regulation. In particular, provide for disease‐specific procedures for the sampling of:
ToR 1.1 Animals for clinical examinations to ensure the detection of the relevant category A disease during the performance of official investigations in establishments that are affected or suspected to be affected by category A diseases and visits in establishments located in restricted zones in accordance with Articles 6(2), 13(3)(c), 14(1) and 26(2) of the Delegated Regulation.
ToR 1.2 Animals for laboratory examinations to ensure the detection of the relevant category A disease during the performance of official investigations in establishments that are affected or suspected to be affected by category A diseases and visits in establishments located in restricted zones in accordance with Articles 6(2), 12(3), 13(3)(c), 14(1), 26(2) of the Delegated Regulation.
ToR 1.3 Establishments to ensure the detection of the relevant category A disease for the performance of visits in establishments located in protection zones larger than 3 km and establishments located in the surveillance zone in accordance with Articles 26(5) and 41 of the Delegated Regulation.
ToR 1.4 Animals for clinical and laboratory examinations to ensure the detection of the relevant category A disease for the movement of animals from restricted zones in accordance with Articles 28(5), 43(5), 56(1)(c) of the Delegated Regulation.
ToR 1.5 Animals for laboratory examinations to ensure the detection of the relevant category A disease before and after being introduced in the affected establishment for repopulation, in accordance with Article 59(2), (3) and (9) of the Delegated Regulation.
1.1.2. ToR 2: Monitoring period
ToR 2.1 Assess the effectiveness of the length of the monitoring periods set out in Annex II of the Delegated Regulation for each category A disease of terrestrial animals. In this regard, it is important to take into consideration that the monitoring period was introduced as a management tool, which represents a time frame of reference assigned to each category A disease for the competent authority to apply certain control measures and to carry out investigations in the event of suspicion and confirmation of category A diseases in terrestrial animals.
This assessment should be carried out with respect to the following situations:
the records analysis carried out by the competent authority in the framework of the epidemiological enquiry referred to in Article 57 of Regulation (EU) 2016/429, in the event of suspicion of a category A disease (Article 8(4) of the Delegated Regulation);
the derogation from killing in the event of an outbreak of a category A disease in establishments keeping animals of listed species in two or more epidemiological units (Article 13(1) of the Delegated Regulation);
the tracing carried out by the competent authority to identify establishments and other locations epidemiologically linked to an establishment affected by a category A disease (Article 17(2) of the Delegated Regulation);
the exemption applied to certain products from the prohibitions laid down in Annex VI taking into account the date they were produced (Article 27(3)(c) of the Delegated Regulation);
the specific conditions for authorising movements of semen from approved germinal product establishments in the protection and surveillance zones (Article 32(c) and 48(c) of the Delegated Regulation);
the repopulation of establishments affected by a category A disease (Article 57(1)(b) and 59(4)(b) of the Delegated Regulation).
ToR 2.2 Propose the length of what should be the monitoring period in those diseases for which the time is assessed as not effective.
1.1.3. ToR 3: Minimum radius of restricted zones and duration of the disease control measures in restricted zones
ToR 3.1 Assess the effectiveness to control the spread of the disease of the minimum radius of the protection and surveillance zones set out in Annex V of the Delegated Regulation for each category A disease of terrestrial animals.
ToR 3.2 Assess the effectiveness to control the spread of the disease of the minimum periods during which the competent authority should apply the restriction measures in the protection and surveillance zones as set out in Annex X and XI for each category A disease of terrestrial animals.
1.1.4. ToR 4: Prohibitions in restricted zones and risk‐mitigating treatments for products of animal origin and other materials
ToR 4.1 Assess the effectiveness to control the spread of disease of prohibitions set out in Annex VI of the Delegated Regulation with respect to the risk associated for each category A disease, to the listed activities and commodities.
ToR 4.2 Review the available scientific information on risk‐mitigating treatments that are effective to control the presence of category A disease agents in products of animal origin and other relevant materials. Based on this:
provide an opinion on the effectiveness of the risk‐mitigating treatments for products of animal origin and other materials produced or processed in the restricted zone set out in Annex VII and VIII, and
if relevant, suggest new treatments or procedures that can be effective to mitigate or to eliminate such risk.
1.2. Interpretation of the Terms of Reference
To address the ToRs of the mandate, EFSA proposed and agreed with the European Commission the following:
The publication of fourteen individual opinions, one per each of the diseases included in the list of category A diseases for terrestrial animals, with each of these opinions providing the answer to ToRs 1, 2 and 3. The current manuscript is one of the 14 opinions covering ToRs 1, 2 and 3 for Lumpy Skin Disease (LSD).
The publication of a unique opinion covering ToR 4 for all diseases listed (i.e. ToR 4 is not covered in this opinion).
To address ToR 1 (effectiveness of sampling procedures), EFSA agreed with the EC on 21 scenarios based on different articles of the Delegated Regulation (EC) 2020/687 (hereinafter referred to as Delegated Regulation), for which the effectiveness of the sampling procedures will be assessed (Annex B). Although these scenarios will be assessed independently, some of these scenarios may be merged if the assessment processes are the same.
To address ToR 2 (effectiveness of the monitoring period), seven scenarios previously agreed with the contractor were defined (Annex C). The assessment of the effectiveness of the monitoring period will be done by assessing its ability to ensure that specific actions can be carried out without posing a risk of disease spread, if the monitoring period is calculated backwards or forwards from a specific date. If the length of the monitoring period estimated by EFSA is longer than the existing monitoring periods, the existing monitoring period will be considered non effective. If the length of the monitoring period estimated by EFSA is shorter than the existing monitoring period, this existing monitoring period will be considered effective from a disease control point of view. No assessment of the plausible unnecessary economic burden that may be placed on the stakeholders as a result of an excessive length of the monitoring periods will be done by EFSA.
The assessment of the minimum duration and the length of the radius of the protection and surveillance zones (ToR 3) will be done independently. The setting of these two zones (protection and surveillance zones) surrounding an affected establishment and the control measures implemented in each one of the zones are based on the general principle that the probability of disease spread is larger the closer the establishment is to an affected establishment. The validity of this statement will not be assessed in this manuscript; nonetheless, the limitations that this assumption may have in the control of certain diseases will, when relevant, be discussed.
-
The following scenarios of the ToR 1 of the Annex B are not relevant for the LSD, and therefore not included in the assessment of the current Opinion:
scenario 6 because the minimum radius of the protection zone for LSD is 20 km,
scenarios 10, 11, 16 and 17 because they are referring to poultry.
The duration of the monitoring period for LSD as described in Annex II of the Delegated Regulation is 45 days.
The minimum length of the radius of the protection zone and surveillance zone for LSD as described in Annex V of the Delegated Regulation are 20 and 50 km, respectively.
The minimum duration of the measures in the protection zone and surveillance zone for LSD as described in Annex X and XI of the Delegated Regulation are 28 and 45 days, respectively.
Vaccination against LSD has not been taken into consideration in the assessment of ToRs 2 and 3 as agreed with the requestor. For ToR 1 some relevant aspects related to vaccination were discussed (a deep review was not requested).
2. Epidemiology and geographical distribution of Lumpy skin disease virus
2.1. Epidemiology
Aetiology
Lumpy Skin Disease (LSD) is a viral disease of cattle and water buffalo caused by Lumpy Skin Disease Virus (LSDV) from the family Poxviridae, genus Capripoxvirus (CaPV) (OIE, 2018). There is only one serotype of LSDV, which is phylogenetically distinct but serologically related to Sheep‐Pox Virus (SPPV) and Goat‐Pox Virus (GTPV). These CaPVs cannot be distinguished serologically and can cross‐react (Tulman et al., 2002; Tuppurainen et al., 2017b).
Epidemiology
Various species of cattle (Bos taurus and Bos indicus) and water buffalo (Bubalus bubalis) are considered to be at risk of LSDV infection (Turan et al., 2017; OIE, 2018) while for animals of Bison ssp., no references were found in the literature. Some wild ruminants such as giraffe (Giraffa spp.) and impala (Aepyceros melampus) have been experimentally infected, and have developed clinical signs leading to death (Young et al., 1970). Antibodies against CaPV have been detected in several wild ruminants in Africa (Hedger and Hamblin, 1983; Barnard, 1997). Generally, high milk‐producing European cattle breeds are more susceptible compared to indigenous African and Asian animals (Tuppurainen et al., 2017a). In European cattle breeds, LSD mortality normally remains below 10% while morbidity can vary from 5% to 45% but in some cases maybe higher (up to 100%) (Tuppurainen et al., 2017b, 2020). LSD does not affect humans (OIE, 2018).
CaPVs are highly resistant and can remain viable in infected tissues for more than 120 days. The virus can also be found in blood, nasal discharge, lacrimal secretion, semen and saliva, which are considered the main sources of direct LSDV transmission (Tuppurainen et al., 2017a). It is not known if transmission can occur via fomites, e.g. by ingestion of feed and water contaminated with infected saliva. Direct skin‐to‐skin contact is considered to play a minor role, if any, in viral transmission (Sprygin et al., 2019). However, this is thought to be a trait of a new recombinant strain (Aleksandr et al., 2020a), which spread first in Russia (Aleksandr et al., 2020b) and is now spreading in Asia (Roche et al., 2020). The transmission across long distances is thought to be the result of the movement of infected animals, but seasonal transmission through arthropod vectors across shorter distances may occur (Sprygin et al., 2019).
While the exact mechanisms of indirect vector transmission remain unclear for most vectors, mechanical transmission seems to be the most plausible way of LSDV transmission as demonstrated for a series of haematophagous vectors such as Aedes aegypti mosquitoes, African ixodid ticks (Amblyomma hebraeum, Rhipicephalus appendiculatus, Rhipicephalus decoloratus), stable flies (Stomoxys calcitrans, S. sitiens and S. indica), horseflies (Haematopota spp.) and horn flies (Haematobia irritans) (Kahana‐Sutin et al., 2017; Sohier et al., 2019; Issimov et al., 2020). Specifically, stable fly transmission has been observed in laboratory settings, and their abundance is associated with increased occurrence of the disease in the field (Kahana‐Sutin et al., 2017; Sprygin et al., 2019). The role and importance for LSDV transmission of each group of vectors may vary between regions, depending on the climate, season, environmental temperature, humidity and vegetation, which favour different insect and tick species (Tuppurainen et al., 2017a,b). Ticks are considered to play a minor role on the transmission of LSDV due to their relative lower abundance and life cycle attached to the host, but have a potential role on the persistence and overwintering of the virus due to vertical transmission (Tuppurainen et al., 2013).
Clinical Signs and Diagnosis
The LSDV incubation period under field conditions ranges from 1 to 5 weeks with viraemia lasting about 12 days (Tuppurainen et al., 2017a).
The disease starts with an initial pyrexia that may exceed 41°C. Based on experimental studies, fever starts from 6 to 9 (OIE, 2018) or 11 days (Moller et al., 2019) after inoculation, and 1–3 days before the appearance of skin nodules (Moller et al., 2019; Sohier et al., 2019) and may persist for up to 1 week (OIE, 2018). The superficial lymph nodes become enlarged. Lachrymation and nasal discharge are usually observed first (Tuppurainen et al., 2017a). The first characteristic skin nodules occur, according to recent experimental studies, from 12 to 26 days post‐feeding by vectors (S. calcitrans, Haematopota spp.), and from 6 to 8 days after intradermal inoculation (Sohier et al., 2019). The appearance of highly characteristic nodular skin lesions of 10–50 mm in diameter varies and may be localised or generalised in severely infected animals (Tuppurainen et al., 2017a). Predilection sites are the skin of the head, neck, perineum, genitalia, udder and limbs (Tuppurainen et al., 2017a; OIE, 2018). The nodules affect the dermis and epidermis and may extend to the underlying subcutis and occasionally to the adjacent striated muscles (EFSA AHAW Panel, 2015). The nodules on the mucous membranes of the eyes, nose and mouth quickly form ulcerated necrotic plaques and cause purulent or mucopurulent nasal discharge and excessive salivation, which contains high concentrations of virus. Sometimes, painful ulcerative lesions develop in the cornea of one or both eyes, leading to blindness in worst cases (Tuppurainen et al., 2017a). Limbs may be oedematous, causing the animal to be reluctant to move (OIE, 2018). In some cases, the skin lesions on the legs and on top of the joints may lead to deep subcutaneous infections complicated by secondary bacterial infections and lameness. Mastitis and pneumonia, caused by the virus itself or from secondary bacterial infections, are common complications (Tuppurainen et al., 2017a). Some general signs and symptoms are also present, such as a decrease in milk production and loss of appetite. Subclinical infections are common in the field.
Tuppurainen et al. (2005) estimated a 67% occurrence of clinical signs in experimentally infected animals within 30 days post‐infection (dpi) (EFSA, 2018). In an intradermal experimental infection, clinical signs occurred in 57% (8 out of 14) (Sohier et al., 2019) of the infected animals within 3 weeks after infection. In some other experimental trials conducted by Sciensano (Belgium) with LSDV in cattle, the sensitivity of detecting clinical signs of LSD in experimentally infected animals was 75% within 3 weeks after infection (EFSA, 2018). In animals experimentally infected by vectors, that have been feeding on infected donor animals, skin nodules appeared over the whole body in 38% (6 out of 16) of the animals within 4 weeks post vector feeding (Sohier et al., 2019). Issimov et al. (2020) experimentally infected six animals by vector feeding and saw one animal with small nodules at the feeding site 10 days post exposure. The other five animals had small swellings to small lesions at the feeding site. Following the first appearance of the skin lesions, the virus can be isolated for up to 35 days and viral nucleic acid can be demonstrated by PCR for up to 3 months (Weiss, 1968; Tuppurainen et al., 2005).
When a homologous live‐attenuated LSD vaccine is used, Differentiating Infected from Vaccinated Animals (DIVA) real‐time PCR and DIVA gel‐based PCR are essential methods for differentiating a vaccine from a field type‐LSDV strain in vaccinated cattle with little nodules developed between 3 and 14 days post vaccination (Menasherow et al., 2016; Agianniotaki et al., 2017). Although rarely used, live virus isolation can also be performed using various cell cultures and electron microscopy can be used for virus detection. Serological testing such as virus neutralisation tests (VNT), antibody ELISAs and Immunoperoxidase Monolayer Assays (IPMA) (Haegeman et al., 2020) is used to detect animals exposed to LSDV or to monitor immunity after vaccination. However, these cannot differentiate infected from vaccinated animals nor between exposures to different CaPVs. IPMA can detect antibodies as early as 14 days after infection/vaccination, which is earlier than the VNT (21 dpi), the OIE recommended serological test (Turan et al., 2017; OIE, 2018), while by ID Screen Capripox Double Antigen (DA), ELISA seroconversion was identified 22 days after dpi (EURL for Capripox viruses,1 personal communication).
Several live attenuated homologous (LSDV Neethling strain based) and heterologous vaccines (based on strains of sheep pox virus (SPPV) or goat pox virus (GTPV)) have been developed to produce immunity against LSDV in susceptible cattle. Vaccines must be administered annually to adult cattle. Mass vaccination using live homologous vaccines is currently the most effective way to control LSD, in combination with other control measures (i.e. vector control, quarantine and biosecurity) (Abdulqa et al., 2016; Turan et al., 2017; EFSA, 2019). However, live vaccines may cause mild adverse reactions in cattle that are not always easily distinguishable from those caused by the virulent LSDV field strain (Tuppurainen et al., 2017a).
2.2. Geographical distribution of Lumpy skin disease
LSDV was first described in Zambia (ex‐Rhodesia) in 1929 and restricted to sub‐Saharan Africa until 1986, when it spread to the Middle East (Abdulqa et al., 2016). The first transcontinental transmission of LSD was reported in Israel in 1989 (Yeruham et al., 1995). In the following years, the disease spread to other countries of the Middle East. In 2012, LSD was introduced again in Israel and spread to other countries of Middle East. In 2013, it started spreading in Turkey where it became endemic (EFSA AHAW Panel, 2015). In August 2015, LSD emerged for the first time to the European Union, in Greece at the border with Turkey, affecting the North Eastern part of Greece by the end of the year (Tasioudi et al., 2016; Antoniou et al., 2017). The disease re‐emerged in the spring of 2016, this time affecting seven countries of South‐Eastern (SE) Europe with numerous outbreaks, in Albania, Bulgaria, Greece, Kosovo2, Montenegro, North Macedonia and Serbia (Tuppurainen et al., 2020). Thanks to the mass vaccination campaigns with homologous LSD vaccines applied in South‐Eastern Europe in affected as well as non‐affected countries (Bosnia and Herzegovina, Croatia,), the disease was contained. LSD outbreaks have not been reported in South‐Eastern Europe since 2017 (EFSA, 2020b).
Nonetheless, LSD remains endemic in Turkey (including western Turkey), where outbreaks continue to be reported during the vector season. LSD was reported in Armenia in 2015 in Georgia and Kazakhstan in 2016. LSD outbreaks were also reported in 2019 and 2020 in Israel, Russia, Saudi Arabia and Syria. LSD was introduced into Asia in July–August 2019, affecting Bangladesh, China and India, and in 2020, LSD was reported in Bhutan, Hong Kong, Myanmar, Nepal, Sri Lanka, Taiwan and Vietnam. LSD remains endemic in several African countries. The American continent and Oceania are still free of LSDV (OIE, 2018). The countries where LSD outbreaks were notified in the last 6 years (2015–2020) to the ADNS and WAHIS notifications systems of European Commission and OIE are presented in Figure 1.
Figure 1.
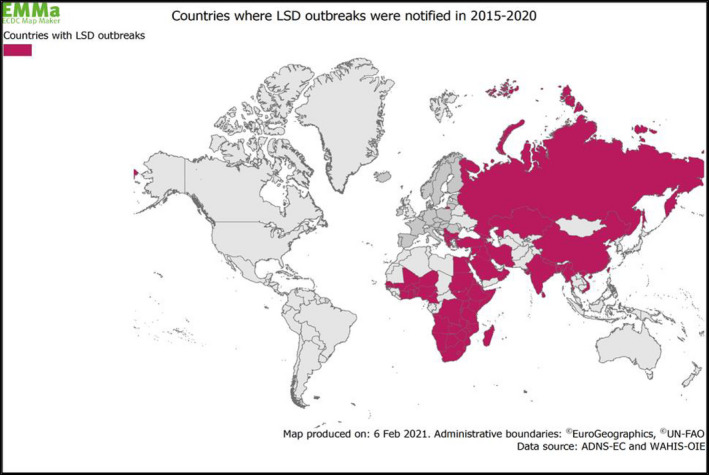
Map of countries (purple) with reported outbreaks of Lumpy Skin Disease in 2015–2020 (Data sources: ADNS‐EC and WAHIS‐OIE)
3. Data and methodologies
3.1. Methodologies
The general methodology applied to all opinions covering the assessment of control measures for the Category A diseases produced under the same mandate has been included in a Technical report published by EFSA (2020a). Specific details of the methodology related to the LSD opinion are presented below.
3.1.1. Methodology used in ToR 1
A qualitative assessment of the clinical and laboratory procedures was performed to answer ToR 1. Estimation of sample size, when needed, was carried out using the RiBESS+ tool.3
To answer the 1st scenario of ToR 1 in the event of LSD suspicion in an establishment, some additional calculations were needed for the true prevalence.
The positive predictive value of the clinical examination at a certain design prevalence (the probability that each selected animal clinically classified as positive is truly LSDV infected) is given by the following equation:
| (1) |
where Seclinical is the sensitivity of the clinical examination, DP is the design prevalence that needs to be detected and Spclinical is the specificity of the clinical examination.
The overall probability to detect LSDV by PCR with a single skin sample would be
| (2) |
where SePCR is the sensitivity of the PCR.
The probability that at least one truly infected animal is detected is given by the equation:
| (3) |
Based on the Seoverall to be achieved, the n (number of samples needed to be collected) can be extrapolated
| (4) |
3.1.2. Methodology used in ToR 2
To answer ToR 2, an extensive literature search (ELS) was outsourced by EFSA (OC/EFSA/ALPHA/2020/02 ‐ LOT 2). The aim of this ELS was to answer the epidemiological question: ‘what is the average, shortest and longest period of time (measured as the number of days from the earliest point of infection with LSDV, to the time of declaration of a suspicion by the competent authority after the clinical investigation by an official veterinarian) for an outbreak of LSD to be reported. To answer this question, an ELS on case reports, papers describing outbreaks or epidemics of LSD and any other relevant grey literature or data was carried out. For the inclusion criteria in the ELS, the earliest point of infection had to have been estimated by carrying out an epidemiological investigation. Papers and other sources of data where the earliest point of infection was determined purely by subtracting a known incubation period from the date of the suspicion of the outbreak were excluded. The ELS was restricted to studies conducted in Europe or describing results obtained in Europe. If none or very few articles were retrieved (less or equal to 5) in the first search, the search was extended to the rest of the world. The general protocol used for the ELS is shown in Annex 5 of the Technical report (EFSA, 2020a).
3.1.3. Methodology used in ToR 3
Methodology for assessing the effectiveness of the minimum radius of the protection and surveillance zones
Studies investigating the transmission of LSDV between establishments using transmission kernels were identified in the published literature. The functional form, parameter estimates and the 95% confidence or credible intervals for the parameters (when provided) of the best fitting kernels were extracted from each study.
For each kernel, the probability of transmission beyond given distances (if transmission were to occur from an infected establishment) was computed using the estimates and the lower and upper 95% confidence limits for the parameters. In addition, the distances at which a threshold probability of transmission beyond that distance is reached were also calculated for each kernel using the estimates, along with its lower and upper 95% confidence limits. More details are provided in Technical report (EFSA, 2020a).
Methodology for assessing the effectiveness of the duration of the protection and surveillance zones
To estimate the duration of measures in the protection and surveillance zones, the outputs obtained from the ELS described in Section 4.2 were used. Further details can be found in the Technical report (EFSA, 2020a).
3.1.4. Uncertainty
A description of the methodology followed to deal with uncertainty is provided in a Technical report published by EFSA (2020a).
4. Assessment
4.1. Assessment of sampling procedures
4.1.1. Assessment of sampling procedures in the event of suspicion or confirmation of Lumpy Skin Disease
4.1.1.1. In the event of a suspicion of Lumpy Skin Disease in kept animals of listed species in an establishment
1.
1st scenario of sampling procedures
ToR 1.1 and ToR 1.2 in accordance with Article 6(2) of the Delegated Regulation (EU) 2020/687
Commission Implemented Regulation 2018/1882 on listed species
The following elements of the scenario were taken into consideration for the assessment:
It concerns an event of suspicion of LSD in an establishment of kept animals of listed species for LSD;
The listed species for LSD as provided in the Commission Implemented Regulation 2018/1882 are Bison ssp., Bos ssp. and Bubalus ssp.;
In the event of a suspicion of LSD, the competent authority shall immediately conduct an investigation to confirm or rule out the presence of LSD;
On the day of the investigation, the official veterinarians must perform clinical examinations and collect samples for laboratory examination.
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures of animals of listed species in a suspected establishment, based on clinical examination (TOR 1.1) and laboratory examination (TOR 1.2) in their ability to detect LSD in kept animals, if the disease is present in that establishment, or to rule it out if not present. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination in the event of a suspicion of LSD were found for the 1st Scenario in EU legislation.
The Food and Agricultural Organization of the United Nations (FAO) has published the ‘Lumpy Skin Disease Field Manual’ where generic information on clinical examination, collection of samples and the epidemiology of LSD is included (Tuppurainen et al., 2017a). This manual does not include specific procedures for the scenarios of the ToRs of this Opinion.
Assessment
In the scenario of a suspicion of LSD in an establishment, the purpose of the clinical examination4 (including both the initial visual inspection of the herd and the individual examination of the animals) is to identify the cases and collect samples for further laboratory analysis.
Development of new procedures
Clinical Examination
The individual clinical examination should focus primarily on those animals showing prominent skin nodules and therefore identified by the owner/farmer/veterinarian as suspects for LSD (targeted sampling). Animals with other general clinical signs such as fever, loss of appetite, depression, lameness and drop of milk production may be considered for clinical examination, especially in endemic, affected or high‐risk areas. In addition, measurement of the body temperature may be used to detect the onset of clinical signs.
The characteristic skin nodules are in most cases visible from a distance, but it should be underlined that in the early stages of the disease, or in mild cases, they may not be detected unless gentle stroking or palpation of the animal's skin is undertaken (EFSA, 2018). Therefore, palpation of the skin should be carried out when skin nodules are not visible especially in endemic, affected or high‐risk areas. Palpation should include at least the predilection sites: head, neck, thorax, perineum, genitalia, udder and limbs.
The sensitivity of the clinical examination to detect animals with clinical signs may range between 50% and 100%5; 75% is considered as the median value (50th percentile of a uniform distribution between 0.5 and 1 (EFSA, 2018)). The specificity cannot always be assumed as 100%.
Laboratory Examination
Titres of LSDV in skin lesions are higher, by five orders of magnitude, compared with their titres in blood (Babiuk et al., 2008). Taking into consideration the fact that not all animals show high titres in blood at such early stages, and that viraemia is intermittent (Babiuk et al., 2008), the sensitivity of the PCR for blood samples is therefore expected to be lower than for skin lesions. The tissue of choice is skin with lesions, preferably skin nodules obtained by skin biopsy, but also scabs and crusts from the ulcerated nodules. Oral, nasal and ophthalmic swabs can be collected from animals with saliva, nasal and lachrymation discharges. An EDTA blood sample can also be collected, where during viraemia, the genome of LSDV can be detected as well by PCR.
PCR specific for capripoxviruses is the laboratory method of choice to confirm or rule out LSD in suspected animals. In animals with clinical signs of LSD, the diagnostic sensitivity of different PCR methods has been reported to be between 90.5% and 100% in blood and 95.5–100% in tissues, while the specificity ranges between 96.7% and 100% in blood and 100% in tissue (Balinsky et al., 2008; Bowden et al., 2008; Stubbs et al., 2012; Haegeman et al., 2013; EFSA, 2018).
In a cattle population where vaccination against LSD, using a homologous live attenuated LSD vaccine, has been implemented, DIVA PCR methods (Menasherow et al., 2016; Agianniotaki et al., 2017) should be used for distinction between a field LSDV strain and a vaccine strain that can cause, in less than 0.1% of the vaccinated population (EFSA, 2017), a post‐vaccination side effect called ‘Neethling response’. This Neethling response is characterised by small nodules remaining for 3–14 days post vaccination. Based on the study of Agianniotaki et al. (2017), the Se of the DIVA PCR for the wild‐type LSDV is 100% (95% CI: 96.67–100%) and the Sp is 100% (95% CI: 97.14–100%). For the vaccine virus, the Se is 98.18% (95% CI: 90.28–99.95%) and the Sp is 100% (95% CI: 97.99–100%). Byadovskaya et al. (2020) reported that the LSDV stain circulating in East Russia since 2018 and in Asia (2019–2020) is detected by most DIVA tests as a vaccine strain and not as a field strain.
Samples for the laboratory analysis must be collected first from animals exhibiting prominent lumps, and then from animals showing less specific clinical signs; samples must be sent to the laboratory without delay.
The confidence to detect or rule out LSD in skin nodules may vary depending on the sensitivity and specificity of the clinical examination, which will not always be 100%, and on the sensitivity of the laboratory tests (given that the specificity is 100%).
In case animals where nodules are detected, and assuming that the specificity of the clinical examination is 100% (only LSDV‐infected animals are considered clinically positive), and with a sensitivity of the PCR in tissues other than blood being higher than 95%, sampling one animal would be enough to detect LSD with 95% confidence.
Nevertheless, if the specificity of the clinical examination is below 100%, the confidence would drop, because an LSD false‐positive animal (animal considered clinically positive for LSD but not infected with LSDV) could be submitted for testing. This is particularly relevant at the low design prevalence (1%).
Assuming (i) a specificity of the clinical inspection of 99.9% (indicating that one in every 1,000 non‐infected animals is considered positive), (ii) a sensitivity of clinical examination of 75% (see below Section 4.1.1.2) and (iii) a design prevalence of 1%, then the positive predictive value (the probability that each selected animal clinically classified as positive is truly LSDV infected) would be 88% (see equation 1 in Section 3.1.1).
The overall probability to detect LSD by PCR with a single skin sample, considering a sensitivity of the PCR in skin lesions of 95%, would be 84% (see equation 2 in Section 3.1.1).
If the probability to detect at least one truly infected animal needs to be greater than 95%, then the number of samples needed is equal or greater than 2 (see Equations 3 and 4 in Section 3.1.1).
In summary, to ensure an overall 95% confidence of detection, skin samples from at least two clinically positive animals are required.
In case blood samples are collected for laboratory diagnosis instead of skin samples and assuming a sensitivity of the PCR in blood of 90%, blood samples from at least two clinically positive animals are required to obtain an overall 95% confidence to detect LSD.
Sampling from several animals, and taking different types of samples from each animal (skin nodules, scabs, ophthalmic/nasal/oral swabs, blood), may increase the confidence to detect or rule out the disease and can prevent technical problems with sampling in the field (e.g. low quality of samples and difficulties to collect samples especially for skin biopsy).
4.1.1.2. For the purposes of the epidemiological enquiry as referred to Article 57 of Regulation (EU)2016/429 in an establishment affected and officially confirmed with LSD
1.
2nd scenario of sampling procedures
ToR 1.2 in accordance with Article 12(3) and the Art. 7 (4) (Preventive killing) of the Delegated Regulation (EU) 2020/687
Article 57 of the Regulation (EU) 2016/429
The following elements of the scenario were taken into consideration for the assessment:
It concerns an affected establishment officially confirmed
Kept animals of listed species found dead or before/when they are killed, are sampled
The Competent authority shall collect samples for laboratory examination
The purposes of the sampling are:
-
a
to support the epidemiological enquiry:
to identify the likely origin of the disease;
to calculate the likely length of time that the disease has been present;
to identify establishments where the animals could have contracted the disease and movements from the affected establishment that could have led to the spread of the disease; and
to obtain information on the likely spread of the listed disease in the surrounding environment, including the presence and distribution of disease vectors
-
b
to confirm/rule out disease in the event of preventive killing.
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures, based on laboratory examination (ToR 1.2), on the ability to detect the disease in the event of preventive killing, and to support the epidemiological investigation (disease detection, prevalence estimation, virus identification, etc.) in kept animals of listed species in an affected establishment, before or when they are killed or found dead. The purposes of the epidemiological enquiry are described in Article 57 of Regulation (EU) 2016/429. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for laboratory examination for the 2nd Scenario were found.
Assessment
When LSD has been officially confirmed in an establishment, further sampling procedures will support the needs of the epidemiological enquiry to obtain information on the origin of the disease, the length of time that the disease is present and the presence and distribution of vectors. In addition, in case preventive killing is decided suppling procedures will confirm or rule out the disease.
Development of new procedures
To support the epidemiological enquiry in an affected establishment, the following sampling procedures maybe implemented.
Estimate the prevalence of animals with clinical signs within the affected establishment
For this purpose, animals that are still alive or those that are found dead or were culled could be examined to identify clinical signs and lesions compatible with LSD. The prevalence of animals with clinical signs and lesions within the establishment can be calculated based on these findings.
Estimate the length of time that the disease is present in the establishment
An approximate estimation of the length of the presence of LSD in the establishment can be based on the age of the skin lesions identified (taking into account the incubation period), by thorough individual clinical examination of the animals that are still alive, or necropsy of those that are found dead. At early stages of the disease, the nodules have a creamy grey to white colour on the cut section, which may initially exude serum, but over the ensuing 2 weeks a cone‐shaped central core or sequestrum of necrotic material/necrotic plug (‘sit‐fast’) may appear within the nodule (OIE, 2018). Therefore, ulcerated skin nodules can be detected at least 15 days after the initial appearance of the nodules.
Supplementary information to support the estimation of the time of infection can be provided by the detection or not of antibodies in animals with clinical signs in an affected establishment. Based on recent experimental studies conducted in the EURL for Capripox viruses1 (Sohier et al., 2019), antibodies can first be detected from 13 to 31 dpi (intradermal and vector feeding) by VNT and from 8 to 29 dpi by IPMA (EURL for Capripox viruses, personal communication) while by ELISA only after 22 dpi (EURL for Capripox viruses, personal communication).
Collect samples for virus isolation and identification and further estimation of the likely origin of the virus
Skin biopsies or nodules for virus isolation should preferably be collected within the first week of the occurrence of clinical signs (Davies, 1991). In contrast to viruses such as Foot and mouth disease virus (FMDV), where sequencing of a part of the genome like VP1 can be enough to determine the origin of the virus (Ularamu et al., 2020), this is not possible for LSDV. Sequencing of three to five different genes (Lamien et al., 2011; Agianniotaki et al., 2017) or Whole genome sequencing (WGS) of the LSDV can help to compare the virus with recently circulating viruses in other countries or regions (Mathijs et al., 2020) and with vaccine viruses (Mathijs et al., 2016). However, even with WGS, it is currently not possible to compare LSD viruses from different establishments and to define the transmission pathway of the virus during the epidemic, as it is possible for FMD (Cottam et al., 2008).
Vector surveillance
Field evidence suggests the involvement of haematophagous arthropod vectors in LSDV mechanical transmission among cattle (EFSA AHAW Panel, 2015). In the EU, the most likely candidate for transmission of LSDV is the ubiquitous biting fly Stomoxys calcitrans, which was shown to transmit the virus under experimental settings (Sohier et al., 2019) and its abundance was highly associated with outbreaks of the disease in Israel (Kahana‐Sutin et al., 2017). Horse flies (Haematopota spp.) were found to experimentally transmit the virus under laboratory conditions (Sohier et al., 2019). Horn flies (Heamatobia irritans) were found in large numbers in outbreaks of grazing beef cattle in Israel (Kahana‐Sutin et al., 2017). They were therefore suggested as vectors based on high abundance. However, transmission of LSDV by these flies was never attempted in the laboratory. Even though there are several experimental studies demonstrating the involvement of certain vectors on the transmission of LSDV, there is a lack of evidence from the field of the recent epidemics occurred in Europe.
To obtain information on the presence, distribution and abundance of the vector species in the affected establishment and the surrounding area, different methods of trapping directly from animals and/or the environment can be used. Virus detection in the collected specimens by PCR methods will provide only an indication of the potential vectors involved with the transmission of the disease and will not imply their effective involvement in LSDV transmission and/or persistence. Further scientific research including well‐designed studies on the field and in experimental trials is necessary to better understand their role in the epidemiology of LSD.
The EFSA Scientific Technical Report Lumpy skin disease: I. Data collection and analysis provides information on life cycle and collection (trapping) methods for vectors potentially involved with LSDV transmission: ticks, midges, mosquitoes, stable flies, horn flies and tabanids (EFSA, 2017).
Confirm or rule out LSD when preventive killing is implemented
In the Delegated Regulation, preventive killing may be applied for the animals of species listed for LSD (Bison ssp., Bos ssp. and Bubalus ssp.) to reduce the likelihood of undetected spread in three cases: (i) in an establishment where LSD is suspected, (ii) in the establishments in temporary restricted zones and (iii) in the establishments of the restricted zones (i.e. the protection and surveillance zones and further restricted zones).
Before preventive killing is undertaken, all animals in the establishment should be subjected to individual clinical examination and if animals with clinical signs are identified, there is no need to continue the individual clinical examination; the establishment should be considered as suspected and the procedures as described in Section 4.1.1.1 should be followed.
In an establishment where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals should be clinically examined to ensure a confidence level of at least 95% to detect or rule out the disease, assuming a low target (design) prevalence of the disease (1% or less).
The sensitivity of the clinical examination to detect animals with clinical signs may range between 50% and 100% (min Test Se = 50% – max Test Se = 100%5) and 75% is considered as the median value (50th percentile of a uniform distribution between 0.5 and 1 (EFSA, 2018).
Detection of infection, when assuming only one or a few animals (1% in larger populations) are infected with 95% confidence, cannot be achieved even if all animals are clinically inspected in the establishments of up to 300 animals. Above that figure, the number of inspected animals should be according to Table 1. The situation is exacerbated if the target (design) prevalence is 0.5%, as shown in Table 1. The sample size in both examples is stratified according to the various groups of animals present in the establishment. The design prevalence had to be adjusted for herd sizes n ≤ 100 and n ≤ 200 accordingly to reflect the assumption of at least one animal presenting clinical signs.
Table 1.
Sample size and confidence level (probability to detect animals with clinical signs) achieved in an establishment as a function of the herd size and the target (design) prevalence of animals with clinical signs (1%) and (0.5%), respectively. Sensitivity of the clinical examination Se = 75%
| Herd size | Example for (design) prevalence of animals with clinical signs 1% | Example for (design) prevalence of animals with clinical signs 0.5% | ||||
|---|---|---|---|---|---|---|
| (Design) Prevalence of animals with clinical signs | Sample size | Confidence level | (Design) Prevalence of animals with clinical signs | Sample Size | Confidence level | |
| 10 | 10%* | 10 | 74% | 10%* | 10 | 74% |
| 20 | 5%* | 20 | 74% | 5%* | 20 | 74% |
| 50 | 2%* | 50 | 75% | 2%* | 50 | 75% |
| 100 | 1% | 100 | 75% | 1%* | 100 | 75% |
| 200 | 1% | 200 | 94% | 0.5% | 200 | 75% |
| 250 | 1% | 250 | 94% | 0.5% | 250 | 75% |
| 300 | 1% | 253 | 95% | 0.5% | 300 | 94% |
| 500 | 1% | 300 | 95% | 0.5% | 500 | 94% |
| 750 | 1% | 312 | 95% | 0.5% | 527 | 95% |
| 1000 | 1% | 345 | 95% | 0.5% | 601 | 95% |
The minimum number of animals with clinical signs in a herd is one. Therefore, the values provided here for the design prevalence is the result of the ratio between 1 and the herd size.
The confidence to detect animals with clinical signs using clinical examination can be improved by increasing the: (i) sensitivity through use of well‐trained veterinarians performing thorough and meticulous individual clinical examination and (ii) number of animals to be tested; preferable all the animals in the establishment.
In case animals with clinical signs are identified, the establishment is considered as suspected and the procedures for the laboratory confirmation that were described in Section 4.1.1.1 should be followed.
In the absence of clinical signs, the confirmation of LSD will be based on the results of laboratory examinations of blood or swabs (oral, nasal ophthalmic) collected from a sample of animals. In Table 2, some examples for different herd sizes and different matrices of samples (blood and swabs) are presented, assuming a low design prevalence of LSD (1%). The design prevalence had to be adjusted for herd sizes where n ≤ 100 to reflect the assumption of at least one animal being infected.
Table 2.
Sample size to achieve a Confidence level of 95% (probability of detecting or ruling out the presence of LSD) in an establishment by using PCR on blood in EDTA, assuming a low design prevalence of 1%. The median sensitivity of PCR methods is used for blood and swabs, respectively
| Herd size | PCR on blood in EDTA (Se = 95.25%) | PCR on oral/nasal/ophthalmic swab (Se = 97.75%) | ||||
|---|---|---|---|---|---|---|
| Design prevalence | Sample size | Confidence | Design prevalence | Sample size | Confidence | |
| 10 | 10%* | 10 | 95% | 10%* | 10 | 98% |
| 20 | 5%* | 20 | 95% | 5%* | 20 | 98% |
| 50 | 2%* | 50 | 95% | 2%* | 49 | 96% |
| 100 | 1% | 100 | 95% | 1% | 98 | 96% |
| 200 | 1% | 163 | 95% | 1% | 159 | 95% |
| 250 | 1% | 204 | 95% | 1% | 199 | 95% |
| 300 | 1% | 199 | 95% | 1% | 194 | 95% |
| 500 | 1% | 236 | 95% | 1% | 230 | 95% |
| 750 | 1% | 245 | 95% | 1% | 239 | 95% |
| 1000 | 1% | 271 | 95% | 1% | 264 | 95% |
The minimum number of animals being infected in a herd is one. Therefore, the values for the design prevalence provided here are the result of the ratio between 1 and the herd size.
The median values for the sensitivity of the PCR were used for each type of sampled matrix, i.e. 95.25% and 97.75% for blood in EDTA and oral/nasal/ophthalmic swab, respectively. The calculations were done using the RiBESS+ tool.
Table 2 shows that when a test with higher sensitivity is used, it is possible to achieve 95% or higher confidence even in smaller herd sizes, e.g. n < 200.
According to a model for the transmission of LSDV between farms (EFSA AHAW Panel, 2016), vaccination has a greater effect in reducing LSDV spread compared to any culling policy, even when low vaccine effectiveness is considered. When vaccination is evenly applied so that 95% of the farms are vaccinated with 75% of the vaccinated animals effectively protected, then total stamping out and partial stamping out result in a similar probability of eradicating the disease. It is important to understand that this conclusion is based on either virus introduction in a region with 95% already vaccinated farms, or in a region where 95% of the farms are vaccinated between 15 and 65 days after introduction of the virus (EFSA AHAW Panel, 2016).
The EFSA AHAW Panel considers that preventive killing in temporary and restricted zones in establishments with no clinical signs and without any evidence of the suspicion of the disease, might not be the choice for LSD control since effective vaccines are available. Quick vaccination of all susceptible animals within these zones, to early reach a high level of immunity, would be the choice to halt the spread of the disease.
4.1.1.3. For granting a specific derogation from killing animals of the categories of article 13.2 of the Delegated Regulation in an LSD affected establishment
1.
3rd scenario of sampling procedures
ToR 1.1 and ToR 1.2 in accordance with Article 13(3)c of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns an LSD affected establishment where infection is officially confirmed
-
In the establishment there are kept animals of listed species of the following specific categories animal categories based on article 13(2):
animals kept in a confined establishment
animals kept for scientific purposes or purposes related to conservation of protected or endangered species
animals officially registered in advance as rare breeds
animals with a duly justified high genetic, cultural or educational value
The competent authority may grant specific derogation from killing all the animals of listed species belonging to any of the above categories in an affected establishment, provided that specific conditions are fulfilled
The animals should be subjected to clinical surveillance, including laboratory examinations.
Sampling procedures should ensure that the animals do not pose a risk of transmission of the category A disease if left alive
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species belonging to the categories described in article 13(2) of an affected establishment, in order to grant a specific derogation from killing these animals, while ensuring that they do not pose a risk for the transmission of the disease. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 3rd scenario.
Assessment
In an establishment affected by LSD, despite infected animals that have been confirmed by either laboratory tests or based on clinical signs, there might be animals which are in the incubation period of the disease (preclinical) and infected animals with a subclinical status. The potential involvement of vectors to the transmission of the disease should also be considered.
Experimental studies show that the onset of clinical signs like fever and skin nodules may range from three to twenty‐six days post infection (Tuppurainen et al., 2005; Babiuk et al., 2008; Moller et al., 2019; Sohier et al., 2019; Issimov et al., 2020; Wolff et al., 2020) during which even a thorough clinical examination will not be able to detect the disease.
In addition, experimental studies using several diagnostic tests showed that they do not yield positive results immediately after infection, but only after a window period ranging from five to 26 dpi (Tuppurainen et al., 2005; Babiuk et al., 2008; Sohier et al., 2019; Issimov et al., 2020) during which the diagnostic tools (clinical examination or laboratory methods) may not be able to detect the disease.
Development of new procedures
Regular clinical examination should be carried out, preferably every day, to early detect the onset of clinical signs, for a period of at least the existing monitoring period of 28 days calculated forwards from the day of confirmation of the latest case.
All the animals intended for derogation of killing should be subjected to thorough individual clinical examination (palpation and temperature measurement included). In addition to what is described in the 1st scenario in Section 4.1.1.1, and since the disease is/has been present in the establishment, the clinical investigation should focus on some early or more generic signs of the disease such as fever, lethargy, lost appetite, nasal/ophthalmic/oral discharge, oedema of the limbs, lameness. Further information such as changes in the individual animal behaviour, in the feed intake and productivity maybe helpful to early detect infected animals.
Sampling all the animals for laboratory examination, as soon as the derogation of killing is decided and irrespectively of the presence of clinical signs, will enable to identify also infected animals without clinical signs, estimate the prevalence of the LSD in the establishment and evaluate the risk. Sampling for laboratory examination can be repeated at any time, but the last sampling should be carried out not earlier than 28 days.
Sampling for laboratory analysis of the animals should be carried out as described in Sections 4.1.1.1 and 4.1.1.2.
Given the potential role of vectors to the transmission of LSD, the animals intended for derogation of killing, should be treated with insecticide or repellent against the relevant vectors. Control of breeding sites and larval population of vectors in the establishment is recommended. Whenever it is applicable keeping the animals in a vector protected establishment will contribute to further reduce the risk of LSD spread.
In addition, vaccination of the healthy animals should be considered by the authorities to further minimise the risk of LSD spread.
4.1.1.4. For the animals of non‐listed species kept in an LSD affected establishment
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of non‐listed species kept in an affected establishment, in their ability to ensure the detection of the virus if the virus is present in these species. For further details, see Annex B.
1.
4th scenario of sampling procedures
ToR 1.1 and ToR 1.2 in accordance with Article 14(1) of the Delegated Regulation (EU) 2020/687
Article 57 of the Regulation (EU) 2016/429
Commission Implemented Regulation 2018/1882 on listed species
The following elements of the scenario should be taken into consideration during for the assessment:
It concerns an affected establishment officially confirmed
In the affected establishment there are kept animals of non‐listed species of epidemiological relevance for the control of the disease
Animals of non‐listed species are those animals that are not listed in Commission Implementing Regulation (EU) 2018/1882 for each of the category A diseases
The animal species acting purely as mechanical carriers of the virus will not be covered
The competent authority is not obliged to carry out the sampling of non‐listed species, but they may establish it in addition to other measures
The purpose of the sampling procedures is to ensure detection of the virus in these species
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 4th scenario.
Assessment
In general, CaPVs are highly host specific and according to our current knowledge, limited data are available on the susceptibility of animal species other than Bos spp. and Bubalus spp. and there is no evidence on their involvement with LSDV transmission.
Giraffe (Giraffa camelopardalis) and impala (Aepyceros melampus) experimentally infected by subcutaneous inoculation of LSDV, demonstrated severe illness with typical symptoms and lesions of the disease and finally died while virus isolation from skin lesions confirmed the presence of LSDV (Young et al., 1970).
In addition, LSDV nucleic acid was detected in skin samples collected from springbok antelopes (Antidorcas marsupialis) in South Africa (Le Goff et al., 2009; Lamien et al., 2011).
Antibodies against SPPV, GTPV and LSDV cannot be differentiated from each other by serological tests and their presence in animal species do not imply that these animals are able to transmit the disease (EFSA AHAW Panel, 2015). Antibodies against CaPV have been detected in in giraffe (Giraffa camelopardalis) and in several antelope species in Africa: blue wildebeest (Connochaetes taurinus), black wildebeest (Connochaetes gnou), springbok (Antidorcas marsupialis), eland (Taurotragus oryx), impala (Aepyceros melampus) and kudu (Tragelaphus strepsiceros), two waterbuck species (Kobus ellipsiprymnus, Kobus defassa), reedbuck (Redunca arundinum), impala (Aepyceros melampus), (Hedger and Hamblin, 1983; Barnard, 1997).
In addition, antibodies were also detected in serum samples collected from African buffalos (Syncerus caffer) (Davies, 1991; Fagbo et al., 2014).
Development of new procedures
Although giraffes, African buffalos, impalas and other antelope species are not natural inhabitants of the European continent and their role on LSD transmission might not be significant, if they are kept in an LSD affected establishment, they should be monitored for clinical signs. In case clinical signs are detected samples should be collected for laboratory analysis. The clinical examination and the sampling for laboratory analysis in case clinical signs are identified, should be carried out as described in Section 4.1.1.1.
The lack of information on the performance of laboratory tests (sensitivity, specificity) in these animal species along with the lack of validation of the diagnostic methods in them will increase the uncertainty on the reliability of the sampling strategy.
4.1.1.5. For wild animals of the listed species within the LSD affected establishment and its surroundings
1.
5th scenario of sampling procedures
ToR 1.1 and ToR 1.2 in accordance with Article 14(1) of the Delegated Regulation (EU) 2020/687
Article 57 of the Regulation (EU) 2016/429
Commission Implemented Regulation 2018/1882 on listed species
The following elements of the scenario were taken into consideration for the assessment:
It concerns an establishment affected by LSD which is officially confirmed
There may exist wild animals of listed species within the establishment and in the surroundings of the establishment
As listed in Commission Implementing Regulation (EU) 2018/1882 for LSD; the wild animals of listed species animals are those of Bison ssp., Bos ssp., Bubalus ssp. species.
The competent authority may establish these sampling procedures in addition to other measures.
The purpose of the sampling procedures in wild animals of listed species is to ensure the detection of the virus, if the virus is present in these wild species
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the wild animals of listed species within the affected establishment and in its surroundings. The purpose of the sampling procedures is to ensure the detection of the virus, if the virus is present in these wild species. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 5th Scenario.
Assessment
In the scenario where wild animals of listed species such as Bison ssp., Bos ssp. and Bubalus ssp. are living in the surrounding area of the affected establishment, maybe infected given the involvement of the haematophagous arthropods in the transmission of the disease.
Development of new procedures
The surveillance of the wildlife around the affected establishment may include the visual inspection of these animals from distance and the inspections of fallen stock and hunted animals to identify clinical signs compatible with LSD.
Samples from animals with clinical signs from dead or hunted animals should be collected for laboratory analysis, following the procedures of Section 4.1.1.1. Wildlife experts would be able to provide additional advice in these circumstances.
The lack of information on the performance of laboratory tests (sensitivity, specificity) in these animal species along with the lack of validation of the diagnostic methods in them will increase the uncertainty on the reliability of the sampling strategy.
4.1.1.6. For non‐affected establishments located in a protection zone with a radius larger than 3 km
1.
7th scenario of sampling procedures
ToR 1.3 in accordance with Article 26(5) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns a protection zone with radius larger than 3 km
Sampling of the non‐affected establishments of kept animals of listed species in the protection zone
In a protection zone with a radius equal to 3 km, official veterinarians must carry inspections in all establishments within the 3 km
In case of a radius larger than 3 km, official veterinarians may not visit all establishments, but a sample of those.
EFSA is requested to assess how many of these establishments should be inspected, in order to ensure the detection of the virus, if the virus is present in animals in these establishments
The purpose of sampling procedure is to ensure the detection of the disease if the disease is present in any of these establishments
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species, for the sampling of establishments located in a protection zone when the radius is larger than 3 km. The purpose of the sampling procedure is to ensure disease detection of the virus if the virus is present in establishments within the protection zone. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for a clinical or laboratory examination were found for the 7th Scenario.
Assessment
For LSD, the minimum radius for the protection zone is 20 and 50 km for the surveillance zone (Annex V of the Delegated Regulation). An assessment of the effectiveness of the length of the radius of the protection and surveillance zone is presented in Section 4.3.1 and is based on kernels estimations.
According to Table 3 (also included in Section 4.3.1), the probability of LSD spreading from an affected establishment beyond 4.5 km is 5%, while beyond 10 km this probability will be below 1.1%. In other words, the probability of transmission within 4.5 km from the affected establishment, if it occurs, is 95%, and 99% within 10 km from the affected establishment. Transmission may occur at longer distances, but with a much lower probability (e.g. transmission beyond 32.6 km occurred in Israel, but with a 0.1% probability).
Table 3.
Distance (km) beyond which the probability of LSDV transmission is equal or lower than a certain threshold. Distances were calculated according to kernels estimated from spread simulations based on epidemics from Israel (2012) and Albania (2016)
| Threshold probability of transmission beyond certain distances (km) | |||||||
|---|---|---|---|---|---|---|---|
| 0.1% | 0.5% | 1% | 5% | 10% | 20% | 50% | |
| Israel 2012 | 32.6 | 14.6 | 10.3 | 4.5 | 3.1 | 2.1 | 1.1 |
| Albania 2016 | 29.3 | 13.2 | 9.3 | 4.1 | 2.8 | 1.9 | 1.0 |
Development of new procedures
All the establishments within the protection zone should be visited and all the animals in an establishment should be clinically examined, provided that it is feasible for the veterinary authorities to perform the visits in a reasonable time to early detect LSD. In case animals with clinical signs are identified, the establishment is considered under suspicion and the procedures for the laboratory confirmation that are described in Section 4.1.1.1 should be followed.
It might not be always feasible for the veterinary authorities to visit all the establishments in the protection zone in a reasonable time to detect the disease as soon as possible. In this case, the authorities should prioritise the visits to all the establishments (with susceptible species) within a certain distance (less than the radius of the protection zone) from the affected one and then gradually extend the visits outwards, to the establishments located beyond this distance up to the borders with the surveillance zone. This distance can be defined using the results of the Kernels as described in Section 4.3.1 and in the Technical Report of the methodology (EFSA, 2020a), according to what the veterinary authorities consider as the acceptable probability of the disease escaping beyond this distance.
Given the high probability (> 95%) of transmission, if occurred, within the 4.5 km radius zone from an affected establishment and consequently the low probability (< 5%) of the disease escaping this zone, implementing surveillance as soon as possible within this 4.5 km zone is recommended to early detect additional infected establishments with high confidence. Beyond this zone, it is recommended to gradually extend the visits to establishments located further to 4.5 km, up to the borders with the surveillance zone.
Visits to establishments epidemiologically linked to an affected establishment should be prioritised and samples should be collected in case a suspicion is raised following the procedures described in Section 4.1.1.1.
All the animals of the listed for LSD species in the visited establishments should be submitted to individual clinical examination (including palpation and temperature measurement).
Since some animals may not show pathognomonic skin nodules (in early stages or mild cases), the clinical investigation should also focus on some early or more generic signs of the disease such as fever, lethargy, lost appetite, oedema of the limbs, lameness, nasal/ophthalmic discharge. In addition, it is necessary to collect further information on the health history of the establishment and the records and documents to be reviewed in order to identify evidence of the presence of the disease such as: morbidity, mortality, clinical observations, changes in productivity and feed intake, purchase or sale of animals, visits of persons likely to be contaminated, transport of animals from holding or areas at risk.
In some cases, the individual clinical examination of all the animals in an establishment in the protection zone is not feasible in reasonable time to enable early detection of the disease. For example, when the number of animals in the establishment is large, or when gathering them all together is difficult (e.g. free grazing animals). In that case, a minimum sample of animals should be clinically examined with at least 95% confidence level to detect or rule out the presence of animals with clinical signs, assuming low target (design) prevalence of the disease following the procedures in Section 4.1.1.2.
In case animals with clinical signs are identified, the establishment is considered as suspected and the procedures for the laboratory confirmation that were described in Section 4.1.1.1 should be followed.
4.1.1.7. For non‐affected establishments located in a surveillance zone
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species, for the sampling of the establishments located within the surveillance zone.
1.
8th scenario of sampling procedures:
ToR 1.3 in accordance with Article 41 of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
Ιt concerns the surveillance zone
Sample of the establishments of kept animals of listed species in the surveillance zone
Official veterinarians carry out visits to a sample of the establishments among others perform clinical examination of kept animals of listed species and if necessary, collection of samples for laboratory examination
The purpose of sampling procedure is to ensure the detection of the disease if the disease is present in any of the establishments
The purpose of the sampling procedure is to ensure disease detection if the virus is present in establishments within the surveillance zone. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 8th scenario.
Assessment
For LSD, the minimum radius for the surveillance zone is 50 km and 20 km for the protection zone (Annex V of the Delegated Regulation. An assessment of the effectiveness of the length of the radius of the protection and surveillance zone is presented in Section 4.3.1 and is based on kernels estimations.
According to the assessment for the length of the radius of the protection and the surveillance zone Section 4.3.1, and as presented in Table 7, the probability of infection beyond a protection zone of 20 km is 0.3% (Israel kernel) and 0.2% (Albania Kernel), while beyond the surveillance zone of 50 km is even less 0.1% for both kernels. In case the surveillance activities in the protection zone do not identify other affected establishments, the probability of LSD having escaped beyond the limits of the protection zone into the surveillance zone is very low.
Table 7.
Probability of transmission of lumpy skin disease virus beyond different distances (km) from an infected establishment point if transmission were to occur
| Distance from the infected establishment (km) | ||||||
|---|---|---|---|---|---|---|
| 10 | 20 | 30 | 50 | 75 | 100 | |
| Israel 2012 | 1.1% | 0.3% | 0.1% | < 0.1% | < 0.1% | < 0.1% |
| Albania 2016 | 0.9% | 0.2% | 0.1% | < 0.1% | < 0.1% | < 0.1% |
Development of new procedures
For the surveillance zone, it is recommended that the efforts will be allocated to enhance passive surveillance by increasing awareness in all establishments, industry and public. In addition, the awareness of the veterinarians at the slaughterhouses should be high during the ante‐mortem animal inspection and post‐mortem inspection of the skin.
Any establishment where more generic signs of the disease such as fever, lethargy, lost appetite, nasal/ophthalmic/oral discharge, oedema of the limbs, lameness and even changes in the individual animal behaviour, in the feed intake and productivity, should be visited, the animals should be clinically examined and samples should be collected following the procedures described in Sections 4.1.1.1 and 4.1.1.2.
Establishments in the surveillance zone epidemiologically linked to an affected establishment or to any other establishment in the protection zone should be also visited, the animals should be clinically examined, and samples should be collected in case a suspicion is raised following the procedures described in Sections 4.1.1.1 and 4.1.1.2.
4.1.2. Assessment of sampling procedures to grant derogations for animal movements
Based on experience obtained from historically endemic countries and from experiments carried out in a controlled environment, LSD can easily be suspected on the basis of the clinical picture in animals, showing skin lesions usually between one to three weeks after infection. However, within the first week following infection the type of lesions could be not easily detectable. In addition, PCR tests start to give positive results in blood only approximately one week after infection (Babiuk et al., 2008), leaving a window of five to 26 days (Sohier et al., 2019) during which animals may be infected, but not yet detected by any diagnostic means (clinical or laboratory). The risk that an undiagnosed infected animal may be present during an LSD outbreak should be considered when designing cattle movement derogations.
Given the role of vectors in the transmission of LSD, the animals intended to be moved should be treated with insecticide or repellent against the relevant vectors, provided that the withdrawal period is respected. Control of breeding sites and larval population of vectors is recommended for the facilities of the establishments. Transport should try to avoid hours of high activity of the vectors with high abundance in the areas where the transmission is taking place.
Biosecurity measures at the establishments of origin and destination and at vehicles during the transport should be in place to reduce any risk of spread of the disease.
In case vaccination is implemented, all the animals to be moved should be vaccinated.
In addition, the specific conditions of the area of the destination, in relation to the epidemiological situation of LSD, the vector abundance and activity, the vaccination coverage (in case vaccination is implemented), the density of the establishments and the commercial activities should be taken into consideration in order to estimate the risk of spread of the disease at destination and the potential impact.
4.1.2.1. From non‐affected establishments located in the protection zone to slaughterhouses located within the protection zone or in the surveillance zone or outside the restricted zone
1.
9th Scenario of sampling procedures
ToR 1.4 in accordance with Article 28(5) of the Delegated Regulation (EU) 2020/687
Article 29 of the Delegated Regulation
The following elements of the scenario were taken into consideration for the assessment:
It concerns the protection zone
Grant derogation for movement of kept animals of listed species from a non‐affected establishment in the protection zone
Animals to be moved to a slaughterhouse located within the protection zone or in the surveillance zone or outside the restricted zone
Clinical examinations and laboratory examination of animals kept in the establishment, including those animals to be moved
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment in a protection zone, in order to grant a derogation from prohibitions in the movement of animals, and allow for the animals to be moved to a slaughterhouse located within the protection zone or in the surveillance zone or outside the restricted zone (Art29). For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 9th scenario.
Development of new procedures
All the animals in the establishment of origin should be clinically examined 24 hours before their movement following the procedures described in Section 4.1.1.1.
In an establishment where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals (including all animals to be moved) should be clinically examined with at least 95% confidence level to detect or rule out the presence of animals with clinical signs, as described in Section 4.1.1.2.
Where clinical signs compatible for LSD are identified, the establishment is considered as suspect, the procedures described in Section 4.1.1.1 are followed and no movements are allowed in this situation.
In addition to clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed.
If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area (protection zone) where the slaughterhouse is located should be high enough (90% farm level coverage or higher according to (EFSA, 2018) to protect the spread of the LSDV. In that case and if the slaughterhouse is located within the protection zone, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment). Clinical examination as described above would be enough. On the contrary if the slaughterhouse is located outside the protection zone, laboratory examination as described above is recommended regardless the vaccination status.
4.1.2.2. From non‐affected establishments located in the protection zone to a plant approved for processing or disposal of animal by‐products in which the animals are immediately killed
1.
12th scenario of sampling procedures
ToR 1.4 in accordance with article 28(5) and article 37 of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns the protection zone
To grant derogation for movement of kept animals of listed species from a non‐affected establishment in the protection zone
The animals to be moved to a plant approved for processing or disposal of animal by‐products in which the kept animals are immediately killed
Clinical examinations and laboratory examinations of animals kept in the establishment, including those animals to be moved
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment in a protection zone, in order to grant derogation from prohibitions in the movement of these animals to a plant approved for processing or disposal of animal by‐products in which the kept animals are immediately killed (Art37). For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 12th Scenario.
Development of new procedures
This scenario is very similar to the 11th scenario of Section 4.1.2.1; therefore, the same procedures will be followed for this scenario as well.
4.1.2.3. From an establishment in a surveillance zone to a slaughterhouse located within or outside the restricted zone and from an establishment outside the surveillance zone to a slaughterhouse situated in the surveillance zone
1.
13th scenario of sampling procedures
ToR 1.4 in accordance with article 43(5) and article 44 of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns kept animals of listed species of the establishments in the surveillance zone
To grant derogation for movement from an establishment in the surveillance zone to be moved to a slaughterhouse within the restricted zone or outside the restricted zone
To grant derogation for movement from an establishment outside the surveillance zone to a slaughterhouse situated in the surveillance zone
Clinical examinations and laboratory examination of animals kept in the establishment, including those animals to be moved
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of listed species in order to grant derogation from prohibitions and allow for these animals to be moved: a) from an establishment in a surveillance zone to a slaughterhouse located within or outside the restricted zone, or b) from an establishment outside the surveillance zone to a slaughterhouse situated in the surveillance zone. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 13th Scenario.
Development of new procedures
All the animals in the establishment of origin should be clinically examined 24 hours before their movement following the procedures described in Section 4.1.1.1.
In an establishment where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals (including all animals to be moved) should be clinically examined with at least 95% confidence level to detect or rule out the presence of animals with clinical signs of as described in Section 4.1.1.2.
In case clinical signs compatible to LSD are identified, the establishment is considered suspect and the procedures for the laboratory confirmation that are described in Section 4.1.1.1 should be followed. The animals intended for movement, even if clinically healthy, should not be dispatched.
In addition to clinical examination, laboratory examination of samples from animals intended to be moved from a non‐affected establishment located in the surveillance zone to a slaughterhouse located outside the restricted zone is necessary to rule out the presence of LSDV, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed.
According to the assessment for the length of the radius of the protection and the surveillance zone in Section 4.3.1, the probability of LSDV having escaped (if transmission occurred) beyond the limits of the protection zone (of 20 km) into the surveillance zone is very low (0.3% Israel Kernel and 0.2% Albania Kernel) while beyond the surveillance zone (of 50 km) is even less (0.1% for both kernels). Therefore, for animals intended to be moved from an establishment located within or outside the surveillance zone to a slaughterhouse situated in the surveillance zone, there is no need for laboratory examination, if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Only clinical examination as described above would be enough.
In case a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the slaughterhouse is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV.
On the contrary, if the slaughterhouse is located outside the restricted zone, samples for laboratory examination of animals intended to be moved are recommended regardless the vaccination status. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed.
4.1.2.4. From an establishment in a surveillance zone to pastures situated within the surveillance zone
1.
14th scenario of sampling procedures
ToR 1.4 in accordance with article 43(5) and article 45(1) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns kept animals of listed species from establishments located in the surveillance zone
To grant derogation for movement from the surveillance zone
To be moved to pastures situated within the surveillance zone
Clinical examinations and laboratory examination of animals kept in the establishment, including those animals to be moved
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of kept ungulates of listed species in order to grant a derogation and allow the animals to be moved from an establishment in the surveillance zone to pastures situated within the surveillance zone. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 14th scenario.
Development of new procedures
All the animals in the establishment of origin should be clinically examined 24 hours before their movement following the procedures described in Section 4.1.1.1.
In an establishment where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals (including all animals to be moved) should be clinically examined with at least 95% confidence level to detect or rule out the presence of animals with clinical signs as described in Section 4.1.1.2.
If animals with clinical signs are identified, the establishment is considered suspect and the procedures for the laboratory confirmation described in Section 4.1.1.1 should be followed. There is a need for increased vigilance on the part of farmers as the grazing animals are usually less supervised and the observation of clinical signs may delay.
In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed.
If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the pastures are located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. In that case, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Clinical examination as described above would be enough.
4.1.2.5. From an establishment in a surveillance zone to an establishment belonging to the same supply chain, located in or outside the surveillance zone
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of kept ungulates of listed species in order to grant derogation and allow to be moved from an establishment in the surveillance zone to an establishment belonging to the same supply chain, located in or outside the surveillance zone, in order to complete the production cycle before slaughter. For further details, see Annex B.
1.
15th scenario of sampling procedures
ToR 1.4 in accordance with article 43(5) and article 45(2) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns the surveillance zone
Grant derogation for movement of kept animals of listed species from the surveillance zone
To be moved to an establishment belonging to the same supply chain, located in or outside the surveillance zone, to complete the production cycle before slaughter
Clinical examinations and laboratory examination of animals kept in the establishment, including those animals to be moved
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 15th Scenario.
Development of new procedures
All the animals in the establishment of origin should be clinically examined 24 hours before their movement following the procedures described in Section 4.1.1.1.
In an establishment, where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals (including all animals to be moved) should be clinically examined with at least a 95% confidence level to detect or rule out the presence of animals with clinical signs, as described in Section 4.1.1.2.
If animals with clinical signs are identified, the establishment is considered suspected and the procedures for the laboratory confirmation that are described in Section 4.1.1.1 should be followed.
In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed.
In case a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the establishment of destination is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. If the establishment of destination is located within the surveillance zone, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Clinical examination as described above would be enough. On the contrary if the establishment of destination is located outside the surveillance zone, laboratory examination as described above would be recommended regardless the vaccination status.
4.1.2.6. From an establishment located in the restricted zone to move within the restricted zone when restriction measures are maintained beyond the period set out in Annex XI of the Delegated Regulation
1.
18th scenario of sampling procedures
ToR 1.4 in accordance with article 56(1) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns the restricted zone when restriction measures are maintained beyond the period set out in Annex XI
To grant derogation for movement of kept animals of listed species from an establishment within the restricted zone
Clinical examinations and laboratory examination of animals kept in the establishment, including those animals to be moved
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment located in the restricted zone of an outbreak in order to allow their move within the restricted zone, when restriction measures are maintained beyond the period set out in Annex XI of the Delegated Regulation. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for clinical or laboratory examination were found for the 18th Scenario.
Development of new procedures
The same sampling procedures should be implemented as those described in Sections 4.1.2.1, 4.1.2.2, 4.1.2.3, 4.1.2.4 and 4.1.2.5.
4.1.3. Assessment of sampling procedures for repopulation purposes
4.1.3.1. For the animals that are kept for the repopulation prior to their introduction
1.
19th scenario of sampling procedures
ToR 1.5 in accordance with article 59(2) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns the repopulation of a previously affected establishment
Animals intended to repopulation shall be sampled prior to their introduction into the establishment of destination
The samples shall be collected from a representative number of animals to be introduced of each consignment from each establishment or from a representative number of animals of each consignment (if animals are all to be introduced at different times or from different establishments of origin)
Laboratory examinations
The purpose sampling procedures is to rule out the presence of the disease
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that are kept for the repopulation prior to their introduction to rule out the presence of the disease. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for laboratory examination were found for the 19th scenario.
Assessment
If animals intended to repopulate previously affected establishments originate from free areas outside the restricted zones of LSD, the risk of re‐introduction of the disease in the establishment of destination is minimised. During the repopulation, the role of vectors to the transmission of the disease should be taken into consideration.
Development of new procedures
All the animals in the establishment of origin should be clinically examined 24 hours before their movement following the procedures described in Section 4.1.1.1.
In an establishment where the number of animals is large, and therefore, the individual clinical examination of all the animals is not feasible, a minimum sample of animals (including all animals to be moved) should be clinically examined with at least a 95% confidence level to detect or rule out the presence of animals with clinical signs, as described in Section 4.1.1.2.
In case clinical signs compatible to LSD are identified, the establishment is considered suspected and the procedures for the laboratory confirmation described in Section 4.1.1.1 should be followed. The animals intended for the repopulation, even if clinically healthy, should not be dispatched.
In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSDV with a confidence at least of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. In case the animals are originated from establishments located in free areas, there is no need for laboratory examination if there are no other reasons based on the authorities’ risk assessment to recommend it (e.g. epidemiological link with an affected establishment or with an affected or high‐risk area). Clinical examination as described above would be enough.
Given the role of vectors in the transmission of LSD, the animals intended for repopulation, should be treated with insecticide or repellent against the relevant vectors and a vector control programme is recommended to be in place in the establishment. The transport of animals is better to avoid season and/or hours of high activity of the vectors with highly abundance in the area, where the transmission is taken place.
In case vaccination is implemented, all the animals that are kept for repopulation should be vaccinated and the level of vaccination coverage, in the area where the establishment of the repopulation is located, should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV.
4.1.3.2. In the event of unusual mortalities or clinical signs being notified during the repopulation
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that have been repopulated in the event of unusual mortalities or clinical signs being notified during the repopulation to rule out the presence of the disease. For further details, see Annex B.
1.
20th scenario of sampling procedures
ToR 1.5 in accordance with article 59(9) of the Delegated Regulation (EU) 2020/687
The following elements of the scenario were taken into consideration for the assessment:
It concerns the repopulated establishment
Unusual mortalities or clinical signs during the repopulation
The official veterinarians shall without delay collect samples for laboratory examination
The purpose of sampling procedures is to rule out the presence of the disease
Summary of sampling procedures
No specific guidelines on sampling procedures for laboratory examination were found for the 20th scenario.
Assessment
During the repopulation of an establishment previously affected by LSD, there is still a risk of re‐introduction of the disease with the new animals being infected either at the establishment of origin or during their transport and a risk of re‐emergence of the disease, if the new animals are infected after their arrival at the establishment of destination. In that case the role of vectors and the possibility of LSDV overwintering should be considered.
Development of new procedures
In the event of animals with clinical signs compatible to LSD, as described in Section 4.1.1.1, are detected during the repopulation, the establishment is considered suspect. The repopulation should be stopped and the procedures for the laboratory confirmation that are described in Section 4.1.1.1 should be followed.
In addition, the establishments from which the suspected animals are originated from, should be considered as suspects. The procedures that are described in Section 4.1.1.1 should be followed as well in the establishments of origin.
Given the role of vectors in the transmission of LSD, the animals used for repopulation, should be treated with insecticide or repellent against the relevant vectors and a vector control programme is recommended to be in place in the establishment. Transport of animals is better to avoid seasons and hours of high activity of the vectors with high abundance in the area, where the transmission can take place.
In case a vaccination programme is implemented, all the animals that are used for repopulation should be vaccinated and the level of vaccination coverage in the area where the establishment of the repopulation is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV.
4.1.3.3. For animals that have been repopulated
The purpose of this section is to assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that have been repopulated, on the last day of the monitoring period calculated forward from the date on which the animals were placed in the repopulated establishment. In case the repopulation takes place over several days, the monitoring period will be calculated forward from the last day in which the last animal is introduced in the establishment. For further details, see Annex B.
Summary of sampling procedures
No specific guidelines on sampling procedures for laboratory examination were found for the 21st scenario.
Assessment
During the repopulation of an establishment previously affected by LSD, there is still a risk of re‐introduction of the disease with the new animals being infected either at the establishment of origin or during their transport, and a risk of re‐emergence of the disease if the new animals are infected after their arrival at the establishment of destination. In that case the role of vectors and the possibility of LSDV overwintering should be considered.
Development of new procedures
The last day of the monitoring period following the latest day of animals’ introduction, all the animals should be subjected to thorough clinical examination (skin palpation and temperature measurement included) as described in Section 4.1.1.1. If clinical signs are identified, then the procedures for the laboratory confirmation described in Section 4.1.1.1 should be followed.
In addition, the establishments from where the suspected or confirmed animals coming from, should be considered as suspects. The procedures that are described in Section 4.1.1.1 should be followed as well in the establishments of origin.
Given the role of vectors in the transmission of LSD, a vector control programme is recommended to be in place in the establishment. The repopulation and the animals transport should try to avoid seasons and hours of high activity of the vectors with high abundance in the area, where the transmission is taken place.
In case a vaccination programme is implemented, all the animals that are used for repopulation should be vaccinated and the level of vaccination coverage in the area where the establishment of the repopulation is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV.
4.2. Assessment of the length of the monitoring period
The concept of the monitoring period was introduced as a management tool for the investigation and control of suspected and confirmed outbreaks of Category A diseases in terrestrial animals. This tool aimed to standardise the methodology by which relevant authorities responded to suspected and confirmed cases of these diseases. In this regard, a disease‐specific monitoring period was set for each of the 14 diseases included in the Category A list. Throughout the EU legislation, the monitoring period is used as an aid in the control of these diseases, although the specific purpose in which the monitoring period is used varies depending on the articles of the legislation.
The length of the monitoring period for each disease is set out in Annex II of the Commission Delegated Regulation supplementing the rules laid down in Part III of Regulation (EU) 2016/429 (Animal Health Law).
The table in Annex C in this opinion describes the seven scenarios for which an assessment of the length of the monitoring period for LSD had been requested.
For the assessment of this ToR, the methodology described in Section 2.3 of the Technical Report (EFSA, 2020a) was followed. In order to assess the length of the monitoring period, the purpose of this monitoring period for each of the scenarios was ascertained.
To answer all scenarios except scenario 5, an extensive literature search (ELS) on the average, shortest and longest period of time between the earliest point of infection of an animal with an LSDV, and the time of reporting of a suspicion by the competent authority, was carried out. The time period between reporting of a suspicion and the notification of the disease was also assessed. Several outcomes were designed for the ELS as shown in the protocol, and the results are presented below.
To answer scenario 5, a literature search was conducted by EFSA on the seroconversion period in cattle, as well as the earliest time of antibody detection in blood, with the outputs being discussed with relevant experts.
4.2.1. Results
Extensive literature search (ELS)
A search was carried out identifying 171 references published after 01/01/2000. Among these references,6 16 were selected to be included in the qualitative review. The full selection process is displayed in Figure 2.
Figure 2.
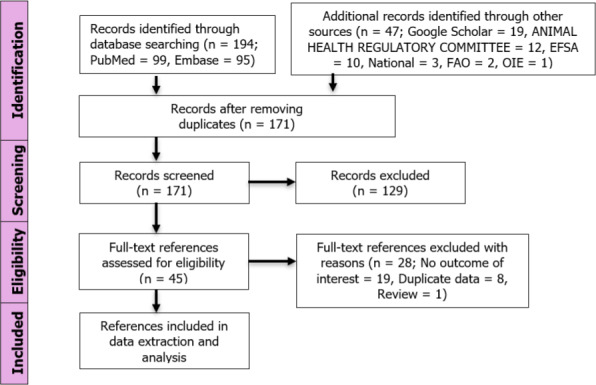
PRISMA diagram, ELS on LSD Monitoring period
Half of the references reported dates instead of periods; these dates were used to calculate the periods of interest. Table 4 provides an overview of the data that were extracted for the main outcome of interest, i.e. the period between the earliest point of infection and the suspicion report.
Table 4.
Summary of the LSD extraction for the ‘period between earliest point of infection and suspicion report’
| Reference | Country | Outbreak year | Period between earliest point of infection and suspicion report (days) |
|---|---|---|---|
| EFSA (2017) | Turkey | 2014 | 201 |
| EFSA AHAW Panel (2016) | Greece | 2015–2016 | 112 |
| Animal Health ‐ Regulatory Committee (2016c) | Greece | 2016 | 32–423 |
| Animal Health ‐ Regulatory Committee (2016b) and Miteva et al. (2017) | Bulgaria | 2016 | 12–274 |
| Animal Health ‐ Regulatory Committee (2016a) | North Macedonia | 2016 | 145 |
| EFSA AHAW Panel (2015a) | Greece | NA | 7–156 |
| EFSA (2018) | Greece and Bulgaria Albania | NA NA | 21–227 15–307 |
| Saegerman et al. (2018) | France | NA | 308 |
Median time between an outbreak and the next closest one in distance, assuming that each outbreak could generate the next closest one in distance.
Mean period (sampled from a gamma distribution with a mean of 10.5 days and shape parameter of 30) based on data from the 2015–2016 outbreaks in Greece.
Min‐max period based on the estimated age of the skin lesions when the animal was detected at the abattoir. The min‐max incubation periods (4–14 days) (OIE, 2002) were added to the age of the lesions.
Min‐max range based on estimated date of infection considering that the index case had been detected early because of the high level of awareness given the proximity with the Greek outbreaks.
Based on clinical findings.
Min–max range assumption used in a transmission model fed with epidemiological data from Israel outbreaks 2012–2013 developed to simulate LSD spread between farms over space after an incursion in Greece.
Median time to detection during the favourable LSD transmission (April to July), based on a spread model used to simulate LSD incursions assuming no vaccination were implemented. Simulated time courses were compared with the number of herds reporting cases during the first 2 weeks of the epidemic in Montenegro in 2016.
Assumption used for a quantitative import risk analysis, based on expert opinion and experimental data.
The longest period was retrieved in the context of an outbreak detected in 2016 at the slaughterhouse in Greece (Animal Health ‐ Regulatory Committee, 2016c). The infection occurred before the animal arrived at the slaughterhouse and it was detected immediately at arrival by the official veterinarian. This case brings evidence for late suspicion, since the age of the skin lesions at detection time was estimated at four weeks, meaning that LSD remained undetected for 32–42 days (37 days average) before it was detected at the abattoir.
The average length of the period based on results from Table 4 was 21 days, with the shortest time to suspicion being 7 days.
Seroconversion in animals
In experimental studies, where animals were infected with LSDV after vector feeding, the earliest day of seroconversion identified by VNT was 14 days (Issimov et al., 2020), and from 17 to 31 days (Sohier et al., 2019; Issimov et al., 2020) after the vectors were placed on the animals. The EURL for Capripox1 identified seroconversion by IPMA from 15 to 29 days after vectors were placed on the animals, while by ID Screen Capripox Double Antigen (DA) ELISA seroconversion was identified 22 days after. In summary, in experiments with vectors, the earliest and the latest day of seroconversion detected by VNT, after the vectors were placed on the animals, have been identified as 14 and 31 days, respectively (see Table 5).
Table 5.
Results from experimental studies with LSDV: antibodies detection with several laboratory methods
| Laboratory method | Type of inoculation | First day of antibody detection* | References |
|---|---|---|---|
| Antibody detection with ID Screen Capripox Double Antigen (DA) ELISA | Vector Feeding | 22 | EURL for Capripox** |
| IVI and IDI | 14–28 | Moller et al. (2019) | |
| IVI | 17–28 | Wolff et al. (2020) | |
| Antibody detection with Virus Neutralization technics (VNT) | Vector Feeding | 14 | Issimov et al. (2020) |
| Vector Feeding | 17–31 | Sohier et al. (2019) | |
| IDI | 13–19 | Sohier et al. (2019); EURL for Capripox** | |
| IVI and IDI | 14 | Moller et al. (2019) | |
| IVI | 17–28 | Wolff et al. (2020) | |
| IVI | 21 | Babiuk et al. (2008) | |
| IVI | 12–18 | Irons et al. (2005) | |
| AI with infected semen | 20–27 | Annandale et al. (2014) | |
| Antibody detection with IPMA | Vector Feeding | 15–29 | EURL for Capripox** |
| IDI | 8–13 | EURL for Capripox** | |
| Antibody detection with indirect immunofluorescence test (iIFT) | IVI and IDI | 7–14 | Moller et al. (2019) |
AI – Artificial insemination with infected semen.
IDI – Intradermal Inoculation.
IVI – Intravenous Inoculation.
Vector Feeding – Inoculation by Vector Feeding.
The first day of antibody detection may vary in the animals of the same experiment, and therefore, a range is provided.
European Union Reference Laboratory for Capripox viruses; link: https://www.eurl-capripox.be/homepage.
Experimental studies, where animals were experimentally infected with LSDV by intradermal or/and intravenous inoculation, show that the earliest day of seroconversion is 7 days post infection/inoculation as identified by indirect immunofluorescence test (iIFT) (Moller et al., 2019), while the latest date of seroconversion is 28 days as identified by ELISA (Moller et al., 2019; Wolff et al., 2020) and also by VNT (Wolff et al., 2020).
In the experimental studies mentioned above, the antibodies remained detectable until the end of the observation period of the trial. The longest period of antibodies detection was 179 dpi with VNT and reported by Irons et al. (2005).
4.2.2. Assessment
Considering the results presented above, an assessment of the effectiveness of the current monitoring period for LSD, depending on the purpose of that period in the different scenarios shown in Annex C, was carried out. For LSD, the length of the monitoring period as defined in Annex II of the Delegated Regulation is 28 days.
1.
1st scenario of monitoring period
ToR 2 in accordance with article 8 and Annex II of the Delegated Regulation (EU) 2020/687
Article 57 of the Regulation (EU) 2016/429
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of the notification of the suspicion of a category A disease in an establishment with kept animals of listed species, for the purposes of the epidemiological enquiry in the event of a suspicion of a LSD outbreak
1.
2nd scenario of monitoring period
ToR 2 in accordance with article 17(2) and Annex II of the Delegated Regulation (EU) 2020/687
Article 57 of the Regulation (EU) 2016/429
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of notification of the suspicion of a category A disease in an establishment with kept animals of listed species, for the purposes of the epidemiological enquiry in the event of confirmation of a LSD outbreak
1.
3rd scenario of monitoring period
ToR 2 in accordance with article 13(b) and Annex II of the Delegated Regulation (EU) 2020/687
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of confirmation of a LSD outbreak in an epidemiological unit in which the disease has not been confirmed, in order to provide derogations from killing the animals in this unit, if this unit has been completely separated, and handled by different personnel during this monitoring period
Scenarios 1, 2 and 3
For the first three scenarios, the main purpose of the use of the monitoring period is to be able to carry a full epidemiological investigation (i.e. in scenarios 1 and 2, at the time of the suspicion and confirmation, respectively), or part of the epidemiological investigation (i.e. scenario 3 where the aim is to identify any possible epidemiological links between the affected establishment and any separated non‐affected epidemiological units).
The length of the monitoring period should then dictate how far back or forward the activities related to tracing (and other activities needed during an epidemiological investigation) should go (checks for production records, animal movement records, etc.). This monitoring period is the time where the infection could have been present unknowingly in an establishment, and due to the regular activities carried out in this establishment, could have spread to other epidemiological units.
In the case of scenario 3, if no epidemiological links between the establishment that has been confirmed positive and the other epidemiological units are found during the investigation (and only if other conditions described in the legislation are met), a derogation from killing the animals in the separated non‐affected epidemiological units could be granted.
The period of time when the disease could have been present, unknowingly, in an establishment, equates then to the time period between the entry of the LSDV into the establishment, and the reporting of the suspicion. Once the suspicion has been officially reported, control measures are implemented, and further spread is in this way prevented.
Based on the ELS carried out and presented above, the average length of the time between infection and the suspicion report was estimated as 21 days based on articles where an epidemiological investigation was carried out. Although the monitoring period defined in the Delegated Regulation is longer than the average calculated using this methodology, it is important to take into account that when the disease is first introduced in an area, detection may be delayed, as it could take up to 37 days on average since the disease has been introduced (see above the latest detection in the slaughterhouse Section 4.2.1). This should be taken into account when carrying out an epidemiological investigation in the index case (first affected establishment) in an area. The length of the monitoring period of 28 days as defined in the Delegated Regulation is considered effective, except for the first affected establishments, where 37 days (average between 32 and 42 days of the longest reported period in ELS) is recommended.
Scenario 4
1.
4th scenario of monitoring period
ToR 2 in accordance with article 27(3)c and Annex II of the Delegated Regulation (EU) 2020/687
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of notification of the suspicion of the LSD outbreak in the protection zone. Products or other materials likely to spread the disease must have been obtained or produced before this time period in order to be exempted from prohibitions of movements
The main purpose of the monitoring period in scenario 4 is to ensure that certain products or materials, likely to spread the disease, that have been produced in a non‐affected establishment located in the protection zone of an affected establishment, can be moved safely and without posing a risk of disease spread. In this scenario, and in contrast with the previous three scenarios, the establishment of concern is neither a suspected nor an affected establishment.
For the assessment of this scenario, we assume that the earliest plausible point of infection of these products or materials in the establishment of concern would be the earliest plausible point of infection of the establishment that originated the protection zone. If these products have been obtained or produced before the earliest point of infection of the affected establishment, then they could be exempted from prohibitions to be moved, as long as other conditions specified in the legislation are met (e.g. the products must have been clearly separated during the production process, storage and transport, from products not eligible for dispatch outside the restricted zone).
As the disease has already been detected in the area, and high awareness is expected, the length of the monitoring period is considered effective in this scenario.
1.
5th scenario of monitoring period
ToR 2 in accordance with article 32 (c), article 48(c) and Annex II of the Delegated Regulation (EU) 2020/687
The purpose of this section is to assess the effectiveness of the length of the Monitoring Period, as the time period calculated forwards from the date of semen collection from animals of listed species kept in approved germinal product establishments in the protection or in the surveillance zone, to prove that the donor animal has tested favourable on a sample taken not earlier than 7 days after the monitoring period
Scenario 5
The aim of the monitoring period is to ensure that semen from animals in a non‐affected establishment (located in a protection or surveillance zone) that has been collected and frozen after the earliest time of infection of the affected establishment that originated the protection zone, is safe to be moved without posing a risk of disease spread.
In this scenario, EFSA is requested to assess the length of time, after the semen was taken, when the animal should be tested in order to allow that semen to be moved. Here, it is assumed that the earliest point of infection of the animal would be on, or after the earliest point of infection of the affected establishment that originated the protection zone, and the latest date the semen could have become contaminated would be the date the semen was collected.
The evidences from the literature presented below demonstrate that LSDV can be found in semen of infected animals, which can be a source of infection and further spread the disease.
An experimental study by Annandale et al. (2014) confirms LSDV transmission to heifers and embryos through semen by artificial insemination (AI). Five out of 11 heifers tested positive for viral DNA in blood by PCR between 10 and 17 dpi, and seroconversion was detected by Virus Neutralisation Test to 8 out of 11 heifers by day 27 post insemination (Annandale et al., 2014). In addition, embryos from two infected heifers tested positive by PCR. The small number of experimental animals and the fact that the LSDV infection via natural mating may differ from that of AI, since the cervix serves as a natural barrier during mating, should be taken into consideration.
The study by Annandale et al. (2018) demonstrated that the common semen processing methods were not effective to eliminate LSDV from cryopreserved bull semen. The use of a modified Percoll® solution with trypsin (Sigma‐Aldrich, Kempton Park, South Africa), to reduce the viral load in semen, had a negative effect to the semen quality (Annandale et al., 2018). Another study by Annandale et al. (2019) shown that the presence of LSDV in frozen‐thawed semen negatively affected embryo yield in in‐vitro embryo production (IVEP) systems.
LSDV has been isolated in the semen of experimentally infected bulls (intravenous injection of a virus suspension) for 22 dpi (Weiss, 1968s), and up to 42 dpi (Irons et al., 2005), while viral DNA was detected in semen by PCR until 159 dpi (Irons et al., 2005).
In the scenario, where the semen might have been contaminated, the latest at the date of collection from an infected donor without clinical signs or with mild clinical signs that remained unnoticed, a serological test would indicate if the donor has ever been exposed to LSDV, and therefore, if the semen has been contaminated.
In the case of an LSD outbreak, based on the existing legislation, the bulls would have to be tested not earlier than the time in days of the monitoring period plus seven days (28 + 7= 35 days) counted after the semen was collected.
Based on the results presented in Section 4.2.1 in relation to the seroconversion, the latest date of seroconversion was identified 31 dpi by VNT (Sohier et al., 2019). Consequently, sampling the animals 35 (28 + 7) days after semen collection as it is foreseen in the Delegated Regulation is considered effective to detect antibodies with several laboratory methods, given that the infection occurred the latest at the day of semen collection.
1.
6th scenario of monitoring period
ToR 2 in accordance with article 57 (1) and Annex II of the Delegated Regulation (EU) 2020/687
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated forward from the date of the final cleaning and disinfection in an affected establishment, after which the repopulation of the establishment may be allowed by the competent authority (assuming relevant control of insects and rodents was carried out).
1.
7th scenario of monitoring period
ToR 2 in accordance with article 59 (4) and Annex II of the Delegated Regulation (EU) 2020/687
Aim: to assess the effectiveness of the length of the Monitoring Period, as the time period calculated forward from the date the first animal was introduced for the purpose of repopulation, during this monitoring period, all animals of the listed species intended for repopulation should be introduced.
Scenarios 6 and 7
In scenarios 6 and 7, the monitoring period is used in the context of repopulation.
In scenario 6, the monitoring period is used to ensure that the repopulation process is not put at risk due to the disease still being present unknowingly in establishments within the surrounding area of the establishment to be repopulated (if an establishment tested positive to LSDV within a distance equal or lower to the radius of the surveillance zone, the repopulation process could not take place).
Repopulation can only take place after a period equal to the monitoring period has elapsed, since the final cleaning, disinfection and disinfestation of the affected establishment.
In this regard, the number of days of the monitoring period for LSD, counted from the day of the final cleaning and disinfection must ensure enough time for any potentially infected surrounding establishment to be reported as a suspicion. Considering the results presented in Section 4.1.2, and taking into account that a good level of awareness is expected due to the disease having been present in the area, the EFSA AHAW Panel considers the existing length of the monitoring period (28 days) effective, as it would allow for the identification of any potentially infected establishment in the surrounding area prior to the repopulation is taking place.
In scenario 7, the monitoring period must be counted forwards from the date in which the first animal is introduced into the establishment to be repopulated, with all the animals intended for repopulation of this establishment being introduced within the length of time of this monitoring period.
The aim of the monitoring period in this scenario is to ensure the early detection of any potentially recently infected animals intended for repopulation once they have been moved into the repopulated establishment. Although the preferred option is that all animals are introduced into the establishment to be repopulated at the same time, this is not always feasible. The first clinical and laboratory sampling of the repopulated animals takes place once all the animals are in situ. By restricting the period of time during which animals may be introduced into the establishment, the period of time during which the disease could be unknowingly spreading within the establishment is reduced.
Assuming that the latest point of infection of the cattle introduced into the repopulated establishment is the day when all the animals have been introduced, and considering that the average length of time to detection is 21 days, it would be likely that some clinical signs would be present in cattle if this visit is carried out 28 days after the last introduction of the cattle. In this scenario, using the average length of time to detection would be justified as a high awareness will exist during the examination of the animals at the first visit. The EFSA AHAW Panel considers the existing length of the monitoring period (28 days) effective as it would allow for early detection of potentially infected cattle at the first visit following re‐stocking.
4.3. Assessment of the minimum radius and time periods of the protection and surveillance zones set in place subsequent to a disease outbreak
4.3.1. Assessment of the minimum radius
The purpose of this section is to assess the effectiveness to control the spread of LSD by implementing a protection and surveillance zones of a minimum radius, as set out in Annex V of the Delegated Regulation, surrounding the establishment where the disease has been confirmed. According to this regulation, the minimum radius for the protection and surveillance zone for LSD should be 20 and 50 km, respectively.
To address this request, transmission kernels (Table 6, Figure 3) have been used to analyse outbreak data from two epidemics of LSD in Israel and Albania (EFSA, 2018). As animal movement restrictions were not in place during these epidemics, the kernels potentially include transmission via movement of infected animals as well as by dispersal of infected vectors. Two functional forms for the kernel were fitted to each epidemic, and in both cases, the fat‐tailed kernel resulted in a better fit than the exponential one. Accordingly, the fat‐tailed kernels were used when assessing the sizes of the protection and surveillance zones. The fitted fat‐tailed kernels for both epidemics are very similar, but the exponential kernels differ (Figure 3).
Table 6.
Transmission kernels for lumpy skin disease virus
| Kernel | Epidemic | Parameters | Reference | |
|---|---|---|---|---|
| d0 | α | |||
| Exponential: | Israel 2012 | 6.67 (5.35, 8.30) | – | EFSA AHAW Panel (2015) |
| Albania 2016 | 2.41 (2.25, 2.58) | – | Gubbins et al. (2020) | |
| Fat‐tailed: | Israel 2012 | 1.05 (0.57, 1.87) | 2.01 (1.76, 2.33) | EFSA AHAW Panel (2015a) |
| Albania 2016 | 0.96 (0.94, 0.99) | 2.02 | Gubbins et al. (2020) | |
Figure 3.
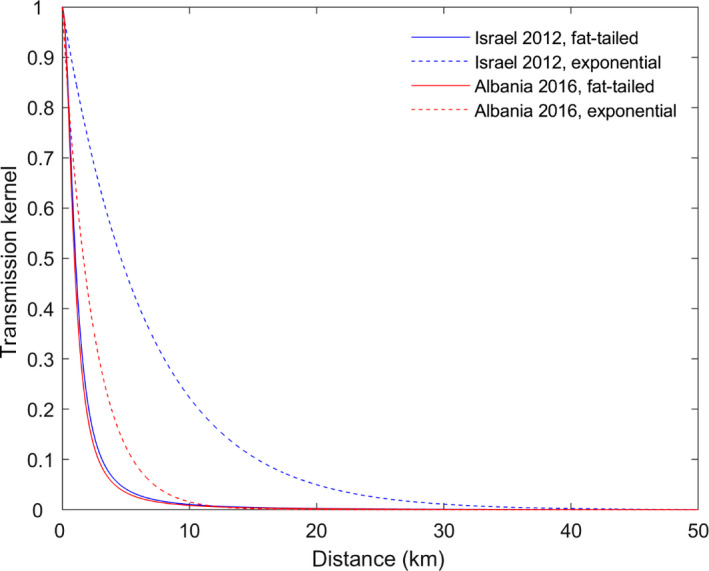
Transmission kernels for lumpy skin disease virus
For the two fat‐tailed kernels in Table 6, the probability of transmission beyond given distances (if transmission were to occur from an infected establishment) was computed using the estimates, lower 95% confidence limits and upper 95% confidence limits, including beyond the proposed radius for the protection and surveillance zones (20 km and 50 km, respectively) (Figure 4). In addition, the distances at which a threshold probability of transmission beyond that distance is reached were also calculated for each kernel using the estimates, lower 95% confidence limits and upper 95% confidence limits (Figure 4). The corresponding values computed using the estimates are summarised in Tables 7 and 8.
Figure 4.
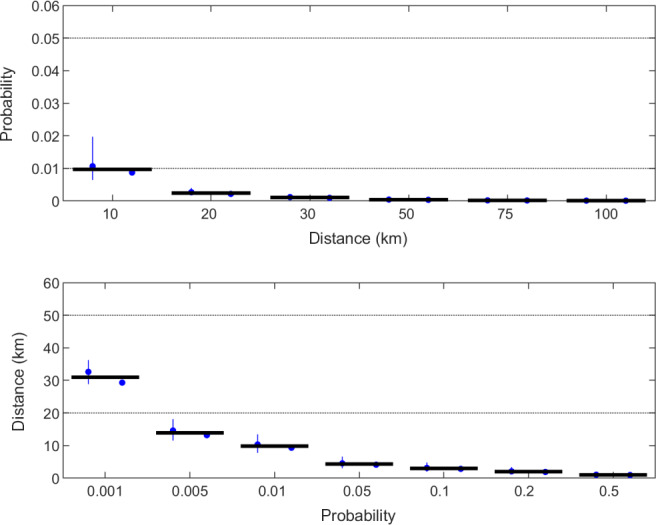
Assessment of the radius of the protection and surveillance zone for LSDV. The top panel shows the probability of transmission beyond a given distance (if transmission were to occur from an infected establishment) computed using the estimates (blue circles) and the lower and upper 95% confidence limits (error bars) for each of the fat‐tailed kernels (and in the same order as) in Table 6. The thick black line indicates the median probability for all kernels. The black dotted lines indicate threshold probabilities of 0.05 and 0.01. The bottom panel shows the distances at which a threshold probability of transmission beyond that distance is reached calculated using the estimates (circles) and lower and upper 95% confidence limits (error bars) for each kernel. The thick black line indicates the median distance for all kernels. The black dotted lines indicate distances of 20 and 50 km (i.e. the proposed radius of the protection and surveillance zones, respectively)
Table 8.
Distances (km) at which the probability of transmission of lumpy skin disease virus beyond that distance reaches a threshold level if transmission were to occur
| Threshold probability of transmission beyond certain distances(km) | |||||||
|---|---|---|---|---|---|---|---|
| 0.1% | 0.5% | 1% | 5% | 10% | 20% | 50% | |
| Israel 2012 | 32.6 | 14.6 | 10.3 | 4.5 | 3.1 | 2.1 | 1.1 |
| Albania 2016 | 29.3 | 13.2 | 9.3 | 4.1 | 2.8 | 1.9 | 1.0 |
Assessment
As expected, we can see from Figures 3, 4, Tables 7 and 8, that the probability of LSD transmission beyond a certain distance from an infected establishment decreases as the distance increases.
Table 7 shows that, if transmission occurs, the probability of transmission from an infected establishment beyond a protection zone of 20 km is 0.3% (Israel) and 0.2% (Albania). Likewise, the probability of transmission beyond a surveillance zone of 50 km is less than 0.1% for both kernels. The minimum radius of both zones, as defined by the Delegated Regulation, provides a probability higher than 99% that LSD will not escape beyond their borders.
In addition, even shorter radiuses such as 10.3 km and 4.5 km can provide confidence of 99% and 95%, respectively, that the transmission will not escape beyond the borders of the zones (Tables 7 and 8).
However, transmission over longer distances cannot be excluded if infected animals are moved outside the zones.
The defined in the legislation minimum radius of 20 km and 50 km of the protection and the surveillance zone are considered effective to restrain with 95% probability the spread of LSD beyond their borders, respectively if transmission were to occur considering the assumptions of the model on animal and vector movement.
A reduction of the minimum radius of the protection and the surveillance zone may be considered. If so, as the kernels used for the assessment of the radius referred to countries outside the EU (Israel and Albania, as vaccination was used in Greece and Bulgaria), a cautious approach of a protection zone of 10 km is recommended (the probability of transmission outside the protection zone being 1.1%) and of a surveillance zone of 30 km (the probability of transmission outside the surveillance zone being 0.1%). If/when further data becomes available, the size of the radius should be reviewed accordingly.
4.3.2. Assessment of the minimum period
The purpose of this section is to assess the effectiveness to control the spread of LSD of the minimum periods during which the competent authority should apply the restriction measures in the protection and surveillance zones as set out in Annex X and XI for the LSD. The length of the minimum period of duration of measures in protection zone is 28 days while for the surveillance zone is 45 days (Annex X of the Delegated Regulation).
To assess the minimum length of time the protection and the surveillance zones should be kept in place, the average (for the protection zones) and the longest (for the surveillance zones) period between the earliest point of infection and the notification of a suspicion will be used (EFSA, 2020a).
Based on the results of the ELS as presented in Table 4 in Section 4.2.1 it follows that the average time between infection and notification of the suspicion is 22 days. Therefore, the minimum period of 28 days indicated in the Delegated Regulation for the restriction measures in the protection zone, is considered effective to detect infected establishments and to prevent the movement of infected animals from the protection zone.
In addition, the maximum period between introduction and suspicion can range from 32 to 56 days with an average of 44 days. Consequently, the minimum period of 45 days indicated in the Delegated Regulation for the restriction measures in the surveillance zone is considered effective to detect infected establishments and to prevent the movement of infected animals from the surveillance zone.
4.3.3. Uncertainty analysis
Although several sources of uncertainty were identified during the scientific assessment (see Annex E), their impact on the outputs of the assessment could not be quantified.
5. Conclusions and Recommendations
| Sampling procedures | Conclusions | Recommendations |
|---|---|---|
| ToR 1 | ||
| In the event of suspicion or confirmation | ||
| 4.1.1.1 (Scenario 1) In the event of a suspicion of LSD in an establishment where animals of the listed species are kept. | The clinical signs of LSD are very specific and the characteristic skin nodules are in most cases visible from a distance. Nevertheless, in the early stages of the disease, or in mild cases, they may not be detected unless gentle stroking or palpation of the animal's skin is undertaken. The sensitivity of the clinical examination to identify animals with clinical signs varies, and the median value is estimated at 75%; while the specificity cannot be always assumed as 100%. In animals with clinical signs of LSD, the diagnostic sensitivity of different PCR methods has been reported to be between 90.5% and 100% in blood and 95.5–100% in tissues, while the specificity ranges between 96.7% and 100% in blood and 100% in tissue. | The individual clinical examination should focus primarily on those animals showing prominent skin nodules. The clinical examination should always include gentle stroking or palpation of the animal's skin. Given the specificity of LSD skin nodules and the fact that the sensitivity of PCR is higher in tissues (skin and ophthalmic/oral/nasal discharges), laboratory testing to confirm or rule out the disease should be targeted to those animals with skin lesions first. Collecting samples from several animals, and different types of samples from each animal (skin nodules, scabs, ophthalmic/nasal/oral swabs, blood) may increase the level of confidence to detect or rule out the disease and can prevent technical problems with sampling in the field (e.g. low quality of samples especially for skin nodules and difficulties with skin biopsy). Assuming a specificity of the clinical examination of 99.9% and a sensitivity of 75%, at least two animals should be collected in an establishment with a prevalence of 1%, to ensure 95% confidence in detecting animals with clinical signs. In cattle population where vaccination against LSD has been implemented, DIVA PCR methods is necessary for the distinction between field and vaccine virus strains. |
| 4.1.1.2. (Scenario 2) For the purposes of the epidemiological enquiry as referred to Article 57 of Regulation (EU)2016/429 in an LSD officially confirmed establishment. |
Epidemiological enquiry
The epidemiological enquiry in an affected establishment may be supported by sampling procedures for the following purposes:
|
Epidemiological enquiry Clinical examination of all the animals to estimate the prevalence of clinical signs in the affected establishment. Virus isolation and Partial or Whole genome sequencing to compare the virus with recently circulating viruses in other countries or regions and with vaccine strains. Estimate the age of the lesions and search for the presence of antibodies in animals with clinical signs to estimate the time of introduction in the establishment. Collect samples of vectors from animals and the environment of the affected establishment to obtain information on the presence, distribution and abundance of the vector species. Virus detection in the collected specimens by PCR methods will provide only an indication of the potential vectors involved with the transmission of the disease and will not imply their involvement in LSDV transmission and/or persistence. Further scientific research including well‐designed studies on the field and experimental trials, is necessary to better understand their role in the epidemiology of LSD. Preventive Killing In case of preventive killing, all the animals (or if not feasible a minimum sample of animals) should be clinically examined with a confidence level to detect or rule out the disease at least 95%, assuming low target (design) prevalence of the disease. In case of preventive killing random sampling of blood and swabs for laboratory analysis by PCR. The sample size should be able to detect the disease with a confidence level of 95%. The AHAW Panel considers that preventive killing in temporary and restricted zones in establishments with no clinical signs and without any evidence of the suspicion of the disease might not be the choice for LSD control since effective vaccines are available. Quick vaccination of all susceptible animals within these zones, to early reach a high level of immunity, would be the choice to halt the spread of the disease. |
| 4.1.1.3. (Scenario 3) For granting a specific derogation from killing animals of the categories of article 13.2 of the Delegated Regulation in an LSD affected establishment. | In an establishment affected by LSD, despite the infected animals confirmed by either laboratory tests or based on clinical signs, there might be animals which are in the incubation period of the disease (preclinical) and animals at subclinical status. The involvement of vectors to the transmission of the disease should be considered. In early stages of the infection there is a window period during which the diagnostic tools (clinical examination or laboratory methods) may not be able to detect the disease. | All the animals intended for derogation of killing should be subjected to thorough individual clinical examination. Regular clinical examination should be carried out, preferably every day, for a period of at least the monitoring period (28 days) calculated forwards from the latest day a case was confirmed. Sampling all the animals for laboratory examination, irrespectively the presence of clinical signs will be able to identify also infected animals without clinical signs. Sampling for laboratory examination can be repeated at any time but the last sampling should be carried out not earlier than 28 days (monitoring period) forwards the day of confirmation of the latest case. Sampling for laboratory analysis of the animals should be carried out as described in Sections 4.1.1.1 and 4.1.1.2. See also 1st scenario in Section 4.1.1.1 and 2nd scenario in Section 4.1.1.2 on sampling procedures. The animals intended for derogation of killing should be treated with insecticide or repellent against the relevant vectors. Control of breeding sites and larval population of vectors in the establishment is recommended. Whenever it is applicable keeping the animals in a vector protected establishment will contribute to further reduce the risk of LSD spread. Vaccination of the healthy animals should be considered to further minimise the risk of spread. |
| 4.1.1.4. (Scenario 4) For the animals of non‐listed species kept in an LSD affected establishment. | In general, CaPVs are highly host specific and according to our current knowledge, limited data are available on the susceptibility of animal species other than Bos spp. and Bubalus spp. and there is no evidence on their involvement with LSD transmission. Giraffe and impala experimentally infected by LSDV, demonstrated severe illness with typical symptoms and lesions of LSD and finally died while LSDV isolated from skin lesions. LSDV nucleic acid was detected in skin samples collected from springbok antelopes in South Africa. Antibodies against SPPV, GTPV and LSDV cannot be differentiated from each other by serological tests and their presence in animal species doesn't imply that these animals are able to transmit the disease. Antibodies against CaPV have been detected in several antelope species in Africa in giraffes and African buffalos. Giraffes, African buffalo, impalas and other antelope species are not natural inhabitants in European continent and their role on LSD transmission might not be significant The available diagnostic methods for LSD may not be validated for these animals. | Giraffes, African buffalos, impalas and other antelope species in case they are kept in an affected by LSD establishment, they should be monitored for clinical signs. On the occurrence of clinical signs laboratory examination should be followed. The lack of information on the performance of laboratory tests (sensitivity, specificity) in these animal species along with the lack of validation of the diagnostic methods in them will increase the uncertainty on the reliability of the sampling strategy. See also 1st scenario in Section 4.1.1.1 and 2nd scenario in Section 4.1.1.2 on sampling procedures. |
| 4.1.1.5. (Scenario 5) For wild animals of the listed species within the LSD affected establishment and its surroundings. | Wild animals of listed species living in the surrounding area of the affected establishment are likely to be infected due to involvement of the haematophagous arthropods in the transmission of the disease. The available diagnostic methods for LSD may not be validated for these animals. | Surveillance of wildlife in the surroundings of an affected establishment may include visual inspection of these animals from distance and inspection of fallen stock and hunted animals to identify clinical signs compatible with LSD. On the occurrence of clinical signs laboratory examination should be followed. The lack of information on the performance of laboratory tests (sensitivity, specificity) in these animal species along with the lack of validation of the diagnostic methods in them will increase the uncertainty on the reliability of the sampling strategy. See also 1st scenario in Section 4.1.1.1 for clinical examination and sampling for laboratory examination in case clinical signs are present. See also 2nd scenario in Section 4.1.1.2 for laboratory sampling in case of absence of clinical signs. |
| 4.1.1.6 (Scenario 7) For non‐affected establishments located in a protection zone with a radius larger than 3 km. | It might not always be feasible to visit all the establishments in the protection zone in a reasonable time to detect the disease as soon as possible. Based on kernels estimations (see also Section 4.3.1) the probability of LSD transmission from an infected establishment beyond the borders of a protection zone of 20 km is 0.3% (Israel Kernel) and 0.2% (Albania Kernel). The probability of an infection occurring within the 4.5 km radius zone from an infected establishment is higher than 95% while the probability of the disease escaping from this area is 0.05%. When assuming a low design prevalence of animals with clinical signs of 1%, in establishments up to 300 animals all the animals should be subjected to clinical examination. | All the establishments within the protection zone should be visited, provided that it is feasible for the veterinary authorities to early detect the disease in a reasonable time. In case it is not feasible to visit all the establishments in the protection zone, the authorities should prioritise their visits to all the establishments located at a certain distance (e.g. 4.5 km or 10 km) from the affected one and then gradually extend the visits outwards to the establishments located beyond this distance up to the borders with the surveillance zone. Visits to establishments epidemiologically linked to an affected establishment should be prioritised and samples should be collected in case a suspicion is raised following the procedures described in Section 4.1.1.1. All the animals of the listed species in the establishments decided to be visited, should be subjected to individual clinical examination (including palpation of the skin and temperature measurement). In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease. See also 1st scenario in Section 4.1.1.1 in case of LSD suspicion in the establishments. |
| 4.1.1.7. (Scenario 8) For non‐affected establishments located in a surveillance zone. | Based on kernels estimations (see also Section 4.3.1) the probability of the disease escaping the protection zone of 20 km is 0.3% (Israel Kernel) and 0.2% (Albania kernel). Based on kernels estimations (see also Section 4.3.1) the probability of the disease escaping the surveillance zone of 50 km is less than 0.1% in both kernels (Israel and Albania) | Efforts should be allocated to increase awareness in the surveillance zone instead of conducting surveillance to the establishments because the probability of LSD having escaped beyond the limits of the protection zone into the surveillance zone is very low; Any establishment where specific or more generic signs of the disease such as fever, lethargy, lost appetite, nasal/ophthalmic/oral discharge, oedema of the limbs, lameness and even changes in the individual animal behaviour, in the feed intake and productivity, should be visited and the animals should be clinically examined and samples should be collected following the procedures described in Sections 4.1.1.1 and 4.1.1.2. Establishments in the surveillance zone epidemiological linked to an affected establishment or to any other establishment in the protection zone should be visited, the animals should be clinically examined and samples should be collected in case a suspicion is raised following the procedures described in Section 4.1.1.1. and Section 4.1.1.2. |
| To grant derogations for animal movements | ||
| 4.1.2.1. (Scenario 9) From non‐affected establishments located in the protection zone to slaughterhouses located within the protection zone or in the surveillance zone or outside the restricted zone. | In early stages of the infection, there is a window during which the diagnostic tools (clinical examination or laboratory methods) may not be able to detect the infection. | Clinical examination of all the animals in the establishment before movement. See also 1st scenario in Section 4.1.1.1. In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. Animals should be protected against vector feeding activity in origin, destination and during transportation In addition to clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the slaughterhouse is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to protect the spread of the LSDV. In that case, and if the slaughterhouse is located within the protection zone, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment). Clinical examination as described above would be enough. On the contrary if the slaughterhouse is located outside the protection zone, laboratory examination as described above is recommended regardless the vaccination status. |
| 4.1.2.2 (Scenario 12) From non‐affected establishments located in the protection zone to a plant approved for processing or disposal of animal by‐products in which the animals are immediately killed. | As scenario 9 in Section 4.1.2.3 | See recommendation above for Section 4.1.2.1 (scenario 9) |
| 4.1.2.3. (Scenario 13) From an establishment in a surveillance zone to a slaughterhouse located within or outside the restricted zone and from an establishment outside the surveillance zone to a slaughterhouse situated in the surveillance zone. | As scenario 9 in Section 4.1.2.3 According to the assessment for the length of the radius of the protection and the surveillance zone in Section 4.3.1, the probability of LSDV having escaped beyond the limits of the protection zone (of 20 km) into the surveillance zone is very low (0.3% Israel Kernel and 0.2% Albania Kernel) while beyond the surveillance zone (of 50 km) is even less (0.1% for both kernels). | Clinical Examination of all the animals in the establishment before movement as described in the 1st scenario in Section 4.1.1.1. In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. In addition to clinical examination, laboratory examination of samples from animals intended to be moved from a non‐affected establishment located in the surveillance zone to a slaughterhouse located outside the restricted zone is necessary to rule out the presence of LSDV, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. For animals intended to be moved from an establishment located within or outside the surveillance zone to a slaughterhouse situated in the surveillance zone, there is no need for laboratory examination, if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Only clinical examination as described above would be enough. Animals should be protected against vector feeding activity at the site of origin, destination and during transportation. If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the slaughterhouse is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to protect the spread of the LSDV. In that case and if the slaughterhouse is located outside the restricted zone, samples for laboratory examination of animals intended to be moved is recommended regardless the vaccination status. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. |
| 4.1.2.4. (Scenario 14) From an establishment in a surveillance zone to pastures situated within the surveillance zone. | As scenario 9 in Section 4.1.2.3 | Clinical Examination of all the animals in the establishment before movement as described in the 1st scenario in Section 4.1.1.1. In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. Animals should be protected against vector feeding activity at the origin, the destination and during transportation. There is a need for increased vigilance on the part of farmers as the grazing animals are usually less supervised and the observation of clinical signs may delay. In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. See also 1st scenario in Section 4.1.1.1. If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where pastures are located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. In that case, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Clinical examination as described above would be enough. |
| 4.1.2.5. (Scenario 15) From an establishment in a surveillance zone to an establishment belonging to the same supply chain, located in or outside the surveillance zone. | As scenario 9 in Section 4.1.2.3 | Clinical Examination of all the animals in the establishment before movement as described in the 1st scenario in Section 4.1.1.1. In some cases, where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. Animals should be protected against vector feeding activity at the site of origin, destination and during transportation. If animals are kept in stables, control of breeding sites and larval population of vectors is recommended. In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSD, with a confidence level of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. If a vaccination programme is implemented, the establishment of origin should be vaccinated, all the animals to be moved should be vaccinated and the level of vaccination coverage in the area where the establishment of destination is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. In that case, and if the establishment of destination is located within the surveillance zone, there is no need for laboratory examination if there are no other reasons based on the national risk assessment to recommended it (e.g. epidemiological link with affected establishment or with affected or high‐risk area). Clinical examination as described above would be enough. On the contrary if the establishment of destination is located outside the surveillance zone, laboratory examination as described above would be recommended regardless the vaccination status. |
| 4.2.1.6 (Scenario 18) From an establishment located in the restricted zone to move within the restricted zone when restriction measures are maintained beyond the period set out in Annex XI of the Delegated Regulation. | Scenarios 9, 12,13,14 and 15, of Sections 4.1.2.1, 4.1.2.2, 4.1.2.3, 4.1.2.4 and 4.1.2.5, respectively. | The recommendations of the scenarios 9, 12,13,14 and 15 of Sections 4.1.2.1, 4.1.2.2, 4.1.2.3, 4.1.2.4 and 4.1.2.5 should be implemented accordingly. |
| For repopulation purposes | ||
| 4.1.3.1 (Scenario 19) For the animals that are kept for the repopulation prior to their introduction. | Animals intended to repopulate previously affected establishments should originate from free areas outside the restricted zones of LSD to avoid re‐introduction of the disease in the establishment of destination. During the repopulation the role of vectors to the transmission of the disease should be taken into consideration. | Clinical examination of all the animals in the establishment before movement as described in the 1st scenario in Section 4.1.1.1. In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. In addition to the clinical examination, laboratory examination of samples from the animals intended to be moved is necessary to rule out the presence of LSDV with a confidence at least of 95%. The procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. In case the animals are originated from establishments located in free areas, there is no need for laboratory examination if there are no other reasons based on the authorities’ risk assessment to recommend it (e.g. epidemiological link with an affected establishment or with an affected or high‐risk area). Clinical examination as described above would be enough. The transport of animals is better to avoid season and/or hours of high activity of the vectors with highly abundance in the area, where the transmission is taken place. Animals should be protected against vector feeding activity at sites of origin, destination and during transportation and a vector control programme is recommended to be in place in the establishment. In case a vaccination programme is implemented, all the animals that are kept for repopulation should be vaccinated and the level of vaccination coverage, in the area where the establishment of the repopulation is located, should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. |
| 4.1.3.2 (Scenario 20) In the event of unusual mortalities or clinical signs being notified during the repopulation. | During the repopulation of an establishment previously affected by LSD, there is still a risk of re‐introduction of the disease with the new animals being infected either at the establishment of origin or during their transport and a risk of re‐emergence of the disease if the new animals are infected after their arrival at the establishment of destination. In that case, the role of the relevant vectors the possibility of LSDV overwintering should be considered. | The repopulation should be stopped and the procedures for the laboratory confirmation that are described in Section 4.1.1.1 in case of suspicion, should be followed. The establishments from where the suspected animals origin, should be considered as suspects. The procedures that are described in Section 4.1.1.1 should be followed as well to the establishments of origin. Animals should be protected against vector feeding activity in the sites of origin, destination and during transportation. The repopulation is better to take place during the season of the year, where the abundance and the activity of the relevant vectors is low. In case a vaccination programme is implemented, all the animals that are indented for repopulation should be vaccinated and, the level of vaccination coverage, in the area where the establishment of the repopulation is located should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. |
| 4.1.3.3 (Scenario 21) For animals that have been repopulated. | During the repopulation of an establishment previously affected by LSD, there is still a risk of re‐introduction of the disease with the new animals being infected either at the establishment of origin or during their transport and a risk of re‐emergence of the disease, if the new animals are infected after their arrival at the establishment of destination. In that case, the role of the relevant vectors the possibility of LSDV overwintering should be considered. | The last day of the monitoring period following the latest day of animals’ introduction, all the animals should be subjected to thorough clinical examination (skin palpation and temperature measurement included) as described in Section 4.1.1.1. In some cases where the individual clinical examination of all the animals in the establishment is not feasible, the minimum sample of animals should be clinically examined with a confidence level at least 95% assuming low target (design) prevalence of the disease as described in Section 4.1.1.2. To rule out the presence of LSD in the animals intended to be moved, with confidence level of 95% through laboratory examinations, the procedures of Section 4.1.1.2 for sampling in the absence of clinical signs should be followed. In addition, the establishments from where the suspected or confirmed animals coming from, should be considered as suspects. The procedures that are described in Section 4.1.1.1 should be followed as well to the establishments of origin. Animals should be protected against vector feeding activity in origin, destination and during transportation. The repopulation is better to take place during the season of the year where the abundance and the activity of the relevant vectors is low. In case vaccination is implemented, all the animals that are indented for repopulation should be vaccinated and the level of vaccination coverage, in the area where the establishment of the repopulation is located, should be high enough (90% farm level coverage or higher according to EFSA (2018)) to prevent the spread of the LSDV. |
| ToR 2 | ||
| 4.2 Length of the monitoring period | The longest length of the period between infection and suspicion of LSD ranged from 32 to 56 days (44 days average). The average length was 22 days, with the shortest time to suspicion being 7 days. Scenario 5 Experimental studies show that the earliest day of seroconversion is 7 days post infection/inoculation as identified by indirect immunofluorescence test (iIFT), while the latest date of seroconversion is 28 days as identified by ELISA and also by VNT. Consequently, sampling the animals 35 (28 + 7) days after semen collection as it is foreseen in the Delegated Regulation is considered effective to detect antibodies with several laboratory methods, given that the infection was occurred the latest at the day of semen collection. Scenarios 6 and 7 Assuming that the latest point of infection of the cattle introduced into the repopulated establishment is the day when the animals are moved, and considering that the average length of time to detection is 22 days, it would be likely that some clinical signs would be present in cattle if this visit is carried out 28 days after the last introduction of the cattle. In this scenario, using the average length of time to detection would be justified as a high awareness will exist during the examination of the animals at the first visit. The EFSA AHAW Panel considers the existing length of the monitoring period (28 days) effective as it would allow for early detection of potentially infected cattle at the first visit following re‐stocking. | Scenarios 1, 2 and 3 The length of the monitoring period of 28 days as defined in the Delegate Regulation is considered effective, except for the first affected establishments, where 44 days (average between 32 and 56 days of the longest monitoring period) is recommended. Scenario 5 None Scenarios 6 and 7 None |
| ToR 3 | ||
| 4.3.1 Assessment of the minimum radius | The defined minimum radius of 20 km and 50 km of the protection and the surveillance zone, respectively, are considered effective to restrain the spread of LSD beyond their borders if it were to occur with 99% probability. In addition, even shorter radiuses such as 10.3 km and 4.5 km can provide 99% and 95% probability, respectively, that the transmission will not escape beyond their limits. | A reduction of the minimum radius of the protection and the surveillance zone may be considered. If so, as the kernels used for the assessment of the radius referred to countries outside the EU (Israel and Albania, as vaccination was used in Greece and Bulgaria), a cautious approach of a protection zone of 10 km is recommended (the probability of transmission outside the protection zone being 1.1%) and of a surveillance zone of 30 km (the probability of transmission outside the surveillance zone being 0.1%). If/when further data becomes available, the size of the radius should be reviewed accordingly. |
| 4.3.2 Assessment of the minimum period | Based on the results of the ELS as presented in Table 4 in Section 4.2.1 it follows that the average time between introduction and suspicion is 22 days. The maximum period between introduction and suspicion can range from 32 to 56 days with an average of 44 days. Consequently, the minimum period of 45 days indicated in the Delegated Regulation for the restriction measures is considered effective to detect infected establishments and to prevent the movement of infected animals from the surveillance zone. | None |
Abbreviations
- ASF
African swine fever
- AHS
African horse sickness
- CSF
Classical swine fever
- CBPP
Contagious bovine pleuropneumonia
- CCPP
Contagious caprine pleuropneumonia
- dpi
days post‐infection
- ELISA
enzyme‐linked immunosorbent assay
- ELS
extensive literature search
- FMD
Foot and mouth disease
- FMDV
Foot and mouth disease virus
- HPAI
Highly Pathogenic Avian Influenza
- LSD
Lumpy skin disease virus
- NCD
Newcastle disease virus
- OIE
World Organization for Animal Health
- PCR
polymerase chain reaction
- PZ
protection zone
- RP
rinderpest virus
- RT‐PCR
reverse transcription polymerase chain reaction
- RVFV
Rift Valley fever virus
- SPGP
Sheep pox and goat pox
- SZ
surveillance zone
- ToR
Terms of Reference
- VNT
Virus neutralisation test
Annex A – Definitions in EU legislation
1.
| Terms | Definitions |
|---|---|
| Clinical examination | The clinical examination comprises: (i) an initial general evaluation of the animal health status of the establishment which comprises all the animals of listed species kept in the establishment; and (ii) an individual examination of the animals included in the sample referred to in point (a). The sampling of animals for clinical examination is carried out in accordance with point A.1 of Annex I for terrestrial animals; (Delegated Regulation article 3) |
| Confined establishment | Means any permanent, geographically limited establishment, created on a voluntary basis and approved for the purpose of movements, where the animals are: (a) kept or bred for the purposes of exhibitions, education, the conservation of species or research; (b) confined and separated from the surrounding environment; and (c) subject to animal health surveillance and biosecurity measures; (AHL: Regulation 2016/429 article 4(48)) |
| Epidemiological unit | Means a group of animals with the same likelihood of exposure to a disease agent; (AHL: Regulation 2016/429 article 4(39)) |
| Establishment | Means any premises, structure, or, in the case of open‐air farming, any environment or place, where animals or germinal products are kept, on a temporary or permanent basis, except for: (a) households where pet animals are kept; (b) veterinary practices or clinics; (AHL: Regulation 2016/429 article 4(27)) |
| Health status | Means the disease status as regards the listed diseases relevant for a particular listed species with respect to: (a) an animal; (b) animals within: (i) an epidemiological unit; (ii) an establishment; (iii) a zone; (iv) a compartment; (v) a Member State; (vi) a third country or territory; (AHL: Regulation 2016/429 article 4(34)) |
| Infected zone | Means a zone in which restrictions on the movements of kept and wild animals or products and other disease control and biosecurity measures may be applied with the view to preventing the spread of a category A disease in the event of official confirmation of the disease in wild animals. (Delegated Regulation article 2(15)) |
| Kept animals | Means animals which are kept by humans, including, in the case of aquatic animals, aquaculture animals; (AHL: Regulation 2016/429 article 4(5)) |
| Outbreak | Means the officially confirmed occurrence of a listed disease or an emerging disease in one or more animals in an establishment or other place where animals are kept or located; (AHL: Regulation 2016/429 article 4 (40) |
| Protection zone | Means a zone around and including the location of an outbreak, where disease control measures are applied in order to prevent the spread of the disease from that zone; (AHL: Regulation 2016/429 article 4(42)) |
| Listed diseases | Means diseases listed in accordance with Article 5(1); (AHL: Regulation 2016/429 article 4 (18)) List of the diseases (AHL: Regulation 2016/429, Annex II) |
| Listed species | Means an animal species or group of animal species listed in accordance with Article 8(2), or, in the case of emerging diseases, an animal species or group of animal species which meets the criteria for listed species laid down in Article 8(2); (AHL: Regulation 2016/429 article 4(20)) List of species and groups of species (Commission Implemented Regulation 2018/1882) |
| Monitoring periods | It is appropriate to follow a single approach for the measures to apply in the event of a category A disease. However, the epidemiology of diseases should be taken into account to establish the appropriate moment for the competent authority to apply control measures and to carry out investigations if there is suspicion or confirmation of those diseases. Therefore ‘monitoring periods’ should be provided, as reference time frames for each category A disease affecting terrestrial animals based on incubation periods and other relevant elements that may affect the spread of the disease. (Delegated Regulation whereas 10). |
| Restricted zone | Means a zone in which restrictions on the movements of certain animals or products and other disease control measures are applied, with a view to preventing the spread of a particular disease into areas where no restrictions are applied; a restricted zone may, when relevant, include protection and surveillance zones; (AHL: Regulation 2016/429 article 4(41)) |
| Surveillance zone | Means a zone which is established around the protection zone, and where disease control measures are applied in order to prevent the spread of the disease from the protection zone; (AHL: Regulation 2016/429 article 4(43)) |
| Wild animals | Means animals which are not kept animals; (AHL: Regulation 2016/429 article 4(8)) |
| Zone | Means: (a) for terrestrial animals, an area of a Member State, third country or territory with a precise geographical delimitation, containing an animal subpopulation with a distinct health status with respect to a specific disease or specific diseases subject to appropriate surveillance, disease control and biosecurity measures; (AHL: Regulation 2016/429 article 4 (35)) |
Annex B – Scenarios of ToR 1
1.
| ToRs | Legislation | Scenario | Description of the Scenario | Elements of the Scenario |
|---|---|---|---|---|
| ToR 1.1 ToR 1.2 | 6(2) of the Delegated Regulation | 1st Scenario | To assess the effectiveness of disease‐specific sampling procedures of animals of listed species in a suspected establishment, based on clinical examination (TOR 1.1) and laboratory examination (TOR 1.2), in their ability to detect a category A disease in kept animals if the disease is present in that establishment, or to rule it out if not present (Art. 6 (2)). |
|
| ToR 1.2 | Art. 12(3) Art. 7 (4) (Preventive killing) of the Delegated Regulation, and Art. 57 Reg.2016/429 | 2nd Scenario | To assess the effectiveness of disease‐specific sampling procedures, based on laboratory examination (ToR 1.2), in their ability to detect the disease in the event of preventive killing, and in their ability to support with the epidemiological investigation (disease detection, prevalence estimation, virus identification, etc.) in kept animals of listed species in an affected establishment, before or when they are killed or found dead. The purposes of the epidemiological enquiry are described in Article 57 of Regulation (EU)2016/429. |
|
| ToR 1.1 ToR 1.2 | Article 13(3)c of the Delegated Regulation | 3rd Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species belonging to the categories described in article 13(2)) of an affected establishment, in order to grant a specific derogation from killing these animals, while ensuring that they do not pose a risk for the transmission of the disease. |
|
| ToR 1.1 ToR 1.2 | Article 14(1) of the Delegated Regulation Art. 57 Reg.2016/429 | 4th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of non‐listed species kept in an affected establishment, in their ability to ensure the detection of the virus if the virus is present in these species. |
|
| ToR 1.1 ToR 1.2 | Article 14(1) of the Delegated Regulation Art. 57 Reg.2016/429 | 5th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the wild animals of listed species within the affected establishment and in its surroundings. The purpose of the sampling procedures is to ensure the detection of the virus, if the virus is present in these wild species |
|
| ToR 1.1 ToR 1.2 | Article 26(2) of the Delegated Regulation | 6th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species in establishments located in the protection zone. The purpose of the sampling procedures is to ensure the detection of the virus, if the virus is present in these animals. |
|
| ToR 1.3 | Article 26(5) of the Delegated Regulation point A.3 of Annex I | 7th Scenario | To assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species, for the sampling of establishments located in a protection zone when the radius is larger than 3 km. The purpose of the sampling procedure is to ensure disease detection of the virus if the virus is present in establishments within the protection zone |
|
| ToR 1.3 | Article 41 of the Delegated Regulation | 8th Scenario | To assess the effectiveness of disease‐specific sampling procedures, based on clinical (ToR 1.1) and laboratory (ToR 1.2) examinations of the animals of listed species, for the sampling of the establishments located within the surveillance zone. The purpose of the sampling procedure is to ensure disease detection if the virus is present in establishments within the surveillance zone |
|
| Derogations to allow animal movements | ||||
| ToR 1.4 | Article 28(5) of the Delegated Regulation Article 29 of the Delegated Regulation | 9th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment in a protection zone, in order to grant a derogation from prohibitions in the movement of animals, and allow for the animals to be moved to a slaughterhouse located within the protection zone or in the surveillance zone or outside the restricted zone (Art29) |
|
| ToR 1.4 | Article 28(5) and Article 30(1) of the Delegated Regulation | 10th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations, to grant a derogation from prohibitions in the movement of day‐old‐chicks located in the protection zone and hatched from eggs originating in the restricted zone or outside the restricted zone. The sampling procedures should ensure that the movement of these day‐old‐chicks to an establishment located in the same Member State but if possible, outside the restricted zone |
|
| ToR 1.4 | Article 28(5) and Article 30(2) of the Delegated Regulation | 11th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations, to grant a derogation from prohibitions in the movement of ready‐to‐lay poultry located in the protection zone to establishments located in the same MS and if possible within the restricted zone. |
|
| ToR 1.4 | Article 28(5) and Article 37 of the Delegated Regulation | 12th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment in a protection zone, in order to grant derogation from prohibitions in the movement of these animals to a plant approved for processing or disposal of animal by‐products in which the kept animals are immediately killed (Art37) |
|
| ToR 1.4 | Article 43(5) and Article 44 of the Delegated Regulation | 13th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of listed species in order to grant derogation from prohibitions and allow for these animals to be moved: a) from an establishment in a surveillance zone to a slaughterhouse located within or outside the restricted zone, b)from an establishment outside the surveillance zone to a slaughterhouse situated in the surveillance zone |
|
| ToR 1.4 | Article 43(5) and Article 45(1) of the Delegated Regulation | 14th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of kept ungulates of listed species in order to grant a derogation and allow for the animals to be moved from an establishment in the surveillance zone to pastures situated within the surveillance zone |
|
| ToR 1.4 | Article 43(5) and Article 45(2) of the Delegated Regulation | 15th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of kept ungulates of listed species in order to grant derogation and allow to be moved from an establishment in the surveillance zone to an establishment belonging to the same supply chain, located in or outside the surveillance zone, in order to complete the production cycle before slaughter |
|
| ToR 1.4 | Article 43(5) and Article 46(1) of the Delegated Regulation | 16th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations to grant derogation of movements of day‐old‐chicks hatched from establishment located in the surveillance zone, from eggs originating within the surveillance zone and eggs originating outside the restricted zone, to an establishment located in the same Member State where they were hatched |
|
| ToR 1.4 | Article 43(5) and Article 46(2) of the Delegated Regulation | 17th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations, to grant a derogation from prohibitions in the movement of ready‐to‐lay poultry located in the surveillance zone to establishments located in the same MS. |
|
| ToR 1.4 | Article 56(1)c of the Delegated Regulation | 18th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on clinical and/or laboratory examinations of the animals of an establishment located in the restricted zone of an outbreak in order to allow their move within the restricted zone, when restriction measures are maintained beyond the period set out in Annex XI |
|
| Repopulation | ||||
| ToR 1.5 | Article 59(2),(3) of the Delegated Regulation | 19th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that are kept for the repopulation prior to their introduction to rule out the presence of the disease. |
|
| ToR 1.5 | Article 59(9) of the Delegated Regulation | 20th Scenario | To assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that have been repopulated, in the event of unusual mortalities or clinical signs being notified during the repopulation; to rule out the presence of the disease. |
|
| ToR 1.5 | Article 59(5) of the Delegated Regulation | 21st Scenario | To assess the effectiveness of disease‐specific sampling procedures based on laboratory examinations of the animals that have been repopulated, on the last day of the monitoring period calculated forward from the date on which the animals were placed in the repopulated establishment. In case the repopulation takes place in several days, the monitoring period will be calculated forward from the last day in which the last animal is introduced in the establishment. |
|
Annex C – Scenarios of ToR 2
1.
| ToRs | Legislation | Scenario | Description of the Scenario | Elements of the Scenarios |
|---|---|---|---|---|
| ToR 2 | Article 8 of the Delegated Regulation Article 57 of 2016/429 Regulation Annex II of the Delegated Regulation | 1st Scenario | To assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of the notification of the suspicion of a category A disease in an establishment with kept animals of listed species, for the purposes of the epidemiological enquiry in the event of a suspicion. |
|
| ToR 2 | Article 17(2) and Article 57 of 2016/429 Regulation Annex II of the Delegated Regulation | 2nd Scenario | To assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of notification of the suspicion of a category A disease in an establishment with kept animals of listed species, for the purposes of the epidemiological enquiry in the event of confirmation of the disease. |
|
| ToR 2 | Article 13(b) of the Delegated Regulation Annex II of the Delegated Regulation | 3rd Scenario | To assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of confirmation of a category A disease in an establishment with kept animals of listed species, during which the epidemiological units in which the disease has not been confirmed were kept completely separated and handled by different personnel, in order to provide derogations from killing. |
|
| ToR 2 | Article 27(3)c of the Delegated Regulation Annex II of the Delegated Regulation | 4th Scenario | To assess the effectiveness of the length of the Monitoring Period, as the time period calculated backwards from the date of notification of the suspicion of the latest outbreak of a category A disease in the protection zone. Products or other materials likely to spread the disease, must had been obtained or produced, before this time period in order to be exempted from prohibitions of movements. |
|
| ToR 2 | Article 32(c) of the Delegated Regulation Article 48(c) of the Delegated Regulation Annex II of the Delegated Regulation | 5th Scenario | To assess the effectiveness of the length of the Monitoring Period, as the time period calculated forwards from the date of semen collection from animals of listed species kept in approved germinal product establishments in the protection or in the surveillance zone, to prove that the donor animal has tested favourable on a sample taken not earlier than 7 days after the monitoring period. |
|
| ToR 2 | Article 57(1)b of the Delegated Regulation Annex II of the Delegated Regulation | 6th Scenario | To assess the effectiveness of the length of the Monitoring Period, as the appropriate time period calculated forwards from the date after the final cleaning and disinfection and when relevant control of insects and rodents was carried out in an affected establishment, after which the repopulation of the establishment may be allowed by the competent authority. |
|
| ToR 2 | Article 59(4)b of the Delegated Regulation Annex II of the Delegated Regulation | 7th Scenario | To assess the effectiveness of the length of the Monitoring Period, as the appropriate time period calculated forwards the date when the first animal was introduced, during which all the animals of listed species intended for repopulation should be introduced. |
|
Annex D – Minimum radius and minimum period of duration of protection and surveillance zones
1.
| Category A diseases | Minimum radius of Protection zone Annex V | Minimum radius of Surveillance zone Annex V | Minimum period of duration of measures in the protection zone (Article 39(1)) Annex X | Additional period of duration of surveillance measures in the protection zone (Article 39(3)) Annex X | Minimum period of duration of measures in the surveillance zone (as referred to in Articles 55 and 56 of this Regulation) Annex XI |
|---|---|---|---|---|---|
| Foot and mouth disease (FMD) | 3 km | 10 km | 15 days | 15 days | 30 days |
| Infection with rinderpest virus (RP) | 3 km | 10 km | 21 days | 9 days | 30 days |
| Infection with Rift Valley fever virus (RVFV) | 20 km | 50 km | 30 days | 15 days | 45 days |
| Infection with lumpy skin disease virus (LSD) | 20 km | 50 km | 28 days | 17 days | 45 days |
| Infection with Mycoplasma mycoides subsp. mycoides SC (Contagious bovine pleuropneumonia) (CBPP) | Establishment | 3 km | 45 days | Not applicable | 45 days |
| Sheep pox and goat pox (SPGP) | 3 km | 10 km | 21 days | 9 days | 30 days |
| Infection with peste des petits ruminants virus (PPR) | 3 km | 10 km | 21 days | 9 days | 30 days |
| Contagious caprine pleuropneumonia (CCPP) | Establishment | 3 km | 45 days | Not applicable | 45 days |
| African horse sickness (AHS) | 100 km | 150 km | 12 months | Not applicable | 12 months |
| Infection with Burkholderia mallei (Glanders) | Establishment | Establishment | 6 months | Not applicable | Not applicable |
| Classical swine fever (CSF) | 3 km | 10 km | 15 days | 15 days | 30 days |
| African swine fever (ASF) | 3 km | 10 km | 15 days | 15 days | 30 days |
| Highly pathogenic avian influenza (HPAI) | 3 km | 10 km | 21 day | 9 days | 30 days |
| Infection with Newcastle disease virus (NCD) | 3 km | 10 km | 21 days | 9 days | 30 days |
Annex E – Uncertainty
1.
| Source or location of the uncertainty | # | Nature or cause of uncertainty as described by the experts | Potential impact of the uncertainty on the assessment |
|---|---|---|---|
| ToR 1 | 1 | Sensitivity and specificity of clinical examination may be variable particularly in the case of mild infections, early stages of the infection or lack of awareness of clinicians (limited Se) or presence of other processes leading to relatively similar clinical signs (limited Sp). This variability in the performance of clinical examination is difficult to characterise. | If clinical examination had a lower performance the effectiveness of the sampling strategies could be overestimated. |
| 2 | Knowledge on the sensitivity and specificity of diagnostic tests in several wild animal and non‐listed species is limited, and diagnostic methods may have not been validated. | The effectiveness of the sampling strategies for these animal species cannot be assessed reliably. | |
| ToR 2 and ToR 3 | 3 | A large variability on the periods between earliest point of infection and suspicion reported in the literature was found, with most studies obtaining their estimates through models based on assumptions (farms becoming infected from closest positive farms in the vicinity, distributions fitted to data, etc.). Furthermore, the time required for suspicion in areas where the disease has not been detected before (lower awareness) is particularly uncertain. | The effectiveness of the proposed monitoring period could be over or underestimated. |
| 4 | Data analysed in the reports found originated from a limited number of countries whose animal populations and production systems may not be representative of those present in other areas of the EU. | The effectiveness of the proposed monitoring period could be over or underestimated. | |
| ToR 1 and ToR 3: kernel estimation | 5 | Kernels are based on analysis of two epidemics (Israel 2012‐3 and Albania 2016) and may not be representative of transmission in other regions due to differences in farm density, vector species and density, management practices, etc. | The effectiveness of the proposed zone size could be over or underestimated. |
| 6 | LSD kernels were fitted using data from outbreaks in which no movement restrictions were in place and could therefore include the effect of transmission via movement of infected animals. | The effectiveness of the proposed zone size could be underestimated. | |
| 7 | The LSD kernels quantify the risk of transmission from an affected establishment at increasing distances if transmission were to occur. Although the probability that transmission actually occurred it is unknown, it would not be expected to happen in all affected establishments. | The effectiveness of the proposed zone size could be underestimated. |
Suggested citation: EFSA AHAW Panel (EFSA Panel on Animal Health and Welfare) , Nielsen SS, Alvarez J, Bicout DJ, Calistri P, Canali E, Drewe JA, Garin‐Bastuji B, Gonzales Rojas JL, Gortázar Schmidt C, Herskin M, Michel V, Miranda Chueca MÁ, Padalino B, Pasquali P, Sihvonen LH, Spoolder H, Ståhl K, Velarde A, Viltrop A, Winckler C, De Clercq K, Gubbins S, Klement E, Stegeman JA, Antoniou S‐E, Aznar I, Broglia A, Van der Stede Y, Zancanaro G and Roberts HC, 2022. Scientific Opinion on the assessment of the control measures for category A diseases of Animal Health Law: Lumpy Skin Disease. EFSA Journal 2022;20(1):7121, 70 pp. 10.2903/j.efsa.2022.7121
Requestor: European Commission
Question number: EFSA‐Q‐2020‐00194
Panel members: Søren Saxmose Nielsen, Julio Alvarez, Dominique Joseph Bicout, Paolo Calistri, Elisabetta Canali, Julian Ashley Drewe, Bruno Garin‐Bastuji, José Luis Gonzales Rojas, Christian Gortázar Schmidt, Mette Herskin, Virginie Michel, Miguel Ángel Miranda Chueca, Paolo Pasquali, Helen Clare Roberts, Liisa Helena Sihvonen, Hans Spoolder, Karl Ståhl, Antonio Velarde, Arvo Viltrop and Christoph Winckler.
Declarations of interest: The declarations of interest of all scientific experts active in EFSA's work are available at https://ess.efsa.europa.eu/doi/doiweb/doisearch.
Acknowledgements: The Panel wishes to thank the following for the support provided to this scientific output: Elisabeth Dorbek‐Kolin from EFSA.
Adopted: 18 February 2021
This article was originally published on the EFSA website http://www.efsa.europa.eu on 30 March 2022 as part of EFSA’s publication procedures.
Notes
European Union Reference Laboratory for Capripox viruses; link: https://www.eurl-capripox.be/homepage
This designation is without prejudice to positions on status and is in line with UNSCR 1244 and the ICJ Opinion on the Kosovo Declaration of Independence. This footnote applies all the time Kosovo is mentioned in this document.
RiBESS+ tool https://efsa.openanalytics.eu/app/ribess
Definition of the term ‘clinical examination’ is provided in the article 3 of the Delegated Regulation: the clinical examination comprises: i) an initial general evaluation of the animal health status of the establishment which comprises all the animals of listed species kept in the establishment; and ii) an individual examination of the animals included in the sample referred to in point (a). The sampling of animals for clinical examination is carried out in accordance with point A.1 of Annex I for terrestrial animals.
Personal communication with Eyal Klement, November 2020.
Because several European studies used outbreak data from Turkey and Israel, references from these countries were also included in the selection.
References
- Abdulqa HY, Rahman HS, Dyary HO and Othman HH, 2016. Lumpy skin disease. Reproductive Immunology: Open Access, 1. 10.4172/2476-1974.100025 [DOI] [Google Scholar]
- Agianniotaki EI, Chaintoutis SC, Haegeman A, Tasioudi KE, De Leeuw I, Katsoulos P‐D, Sachpatzidis A, De Clercq K, Alexandropoulos T, Polizopoulou ZS, Chondrokouki ED and Dovas CI, 2017. Development and validation of a TaqMan probe‐based real‐time PCR method for the differentiation of wild type lumpy skin disease virus from vaccine virus strains. Journal of Virological Methods, 249, 48–57. 10.1016/j.jviromet.2017.08.011 [DOI] [PubMed] [Google Scholar]
- Aleksandr K, Olga B, David WB, Pavel P, Yana P, Svetlana K, Alexander N, Vladimir R, Dmitriy L and Alexander S, 2020a. Non‐vector‐borne transmission of lumpy skin disease virus. Scientific Reports, 10, 7436. 10.1038/s41598-020-64029-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandr K, Pavel P, Olga B, Svetlana K, Vladimir R, Yana P and Alexander S, 2020b. Emergence of a new lumpy skin disease virus variant in Kurgan Oblast, Russia, in 2018. Archives of Virology, 165, 1343–1356. 10.1007/s00705-020-04607-5 [DOI] [PubMed] [Google Scholar]
- Animal Health ‐ Regulatory Committee , 2016a. Lumpy skin disease ‐ FYROM (CVET). European Commission Standing Committee on Plants, Animals, Food and Feed, Animal Health and Welfare section Presentations 5‐6 July 2016. Available online: https://ec.europa.eu/food/sites/food/files/animals/docs/reg-com_ahw_20160705_lumpy-skin-disease_cvet_fyrom.pdf
- Animal Health ‐ Regulatory Committee , 2016b. Lumpy skin disease ‐ Bulgaria. European Commission Standing Committee on Plants, Animals, Food and Feed, Animal Health and Welfare section Presentations 3‐4 May 2016. Place.
- Animal Health ‐ Regulatory Committee , 2016c. Lumpy skin disease ‐ CVET Mission to Greece. European Commission Standing Committee on Plants, Animals, Food and Feed, Animal Health and Welfare section Presentations 3‐4 May 2016. Available online: https://ec.europa.eu/food/sites/food/files/animals/docs/reg-com_ahw_20160503_pres_lumpy-skin-disease-cvet-mission-greece.pdf
- Annandale CH, Holm DE, Ebersohn K and Venter EH, 2014. Seminal transmission of lumpy skin disease virus in heifers. Transbound Emerg Dis, 61, 443–448. 10.1111/tbed.12045 [DOI] [PubMed] [Google Scholar]
- Annandale CH, Smuts MP, Ebersohn K, du Plessis L, Venter EH and Stout TAE, 2018. Effect of semen processing methods on lumpy skin disease virus status in cryopreserved bull semen. Animal Reproduction Science, 195, 24–29. 10.1016/j.anireprosci.2018.04.080 [DOI] [PubMed] [Google Scholar]
- Annandale CH, Smuts MP, Ebersohn K, du Plessis L, Thompson PN, Venter EH and Stout TAE, 2019. Effect of using frozen‐thawed bovine semen contaminated with lumpy skin disease virus on in vitro embryo production. Transbound Emerg Dis, 66, 1539–1547. 10.1111/tbed.13179 [DOI] [PubMed] [Google Scholar]
- Antoniou S‐E, Tsiamadis E, Tasioudi KE, Moraitis S, Plevraki E, Sachpatzidis A, Perdikaris S, Vitalis T, Arakas N, Lianou D, Chondrokouki E, Malemis I, Alexandropoulos T and Dile C, 2017. Lumpy Skin Disease in Greece: An European approach of the management of the Disease. Special edition on Lumpy Skin Disease Edition. Place FAO (Food and Agriculture Organization of the United Nations), FAO (Food and Agriculture Organization of the United Nations). 19–22. pp.
- Babiuk S, Bowden TR, Parkyn G, Dalman B, Manning L, Neufeld J, Embury‐Hyatt C, Copps J and Boyle DB, 2008. Quantification of lumpy skin disease virus following experimental infection in cattle. Transbound Emerg Dis, 55, 299–307. 10.1111/j.1865-1682.2008.01024.x [DOI] [PubMed] [Google Scholar]
- Balinsky CA, Delhon G, Smoliga G, Prarat M, French RA, Geary SJ, Rock DL and Rodriguez LL, 2008. Rapid preclinical detection of sheeppox virus by a real‐time PCR assay. Journal of Clinical Microbiology, 46, 438–442. 10.1128/jcm.01953-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard B, 1997. Antibodies against some viruses of domestic animals in southern African wild animals. Onderstepoort Journal of Veterinary Research, 95–110. [PubMed] [Google Scholar]
- Bowden TR, Babiuk SL, Parkyn GR, Copps JS and Boyle DB, 2008. Capripoxvirus tissue tropism and shedding: a quantitative study in experimentally infected sheep and goats. Virology, 371, 380–393. 10.1016/j.virol.2007.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byadovskaya O, Pestova Y, Kononov A, Shumilova I, Kononova S, Nesterov A, Babiuk S and Sprygin A, 2020. Performance of the currently available DIVA real‐time PCR assays in classical and recombinant lumpy skin disease viruses. Transboundary and Emerging Diseases. 10.1111/tbed.13942 [DOI] [PubMed] [Google Scholar]
- Cottam EM, Wadsworth J, Shaw AE, Rowlands RJ, Goatley L, Maan S, Maan NS, Mertens PPC, Ebert K, Li Y, Ryan ED, Juleff N, Ferris NP, Wilesmith JW, Haydon DT, King DP, Paton DJ and Knowles NJ, 2008. Transmission pathways of foot‐and‐mouth disease virus in the United Kingdom in 2007. PLoS Pathogens, 4, e1000050. 10.1371/journal.ppat.1000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies F, 1991. Lumpy skin disease. A capripox virus infection of cattle in Africa. [DOI] [PubMed]
- EFSA (European Food Safety and Authority), 2017. Lumpy skin disease: I. Data collection and analysis. EFSA Journal 2017;15(4):e04773, 54 pp. 10.2903/j.efsa.2017.4773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA (European Food Safety and Authority), 2018. Lumpy skin disease: scientific and technical assistance on control and surveillance activities. EFSA Journal 2018;16(10):e05452, 40 pp. 10.2903/j.efsa.2018.5452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA (European Food Safety and Authority), 2019. Lumpy skin disease: III. Data collection and analysis. EFSA Journal 2019;17(3):e05638, 26 pp. 10.2903/j.efsa.2019.5638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA (European Food Safety and Authority), 2020a. Technical report on the methodological approach used for the assessment of the control measures for Category A diseases in the context of the new Animal Health Law. EFSA Supporting Publications 2020;17(12):1988E, 66 pp. 10.2903/sp.efsa.2020.en-1988 [DOI]
- EFSA (European Food Safety and Authority), 2020b. Lumpy skin disease epidemiological report IV: data collection and analysis. EFSA Journal 2020;18(2):e06010, 36 pp. 10.2903/j.efsa.2020.6010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA AHAW Panel (EFSA Panel on Animal Health and Welfare), 2015. Scientific Opinion on lumpy skin disease. EFSA Journal 2015;13(1):3986, 73 pp. 10.2903/j.efsa.2015.3986 [DOI] [Google Scholar]
- EFSA AHAW Panel (EFSA Panel on Animal Health and Welfare), 2016. Urgent advice on lumpy skin disease. EFSA Journal 2016;14(8):e04573, 27 pp. 10.2903/j.efsa.2016.4573 [DOI] [Google Scholar]
- Fagbo S, Coetzer JA and Venter EH, 2014. Seroprevalence of Rift Valley fever and lumpy skin disease in African buffalo (Syncerus caffer) in the Kruger National Park and Hluhluwe‐iMfolozi Park, South Africa. Journal of the South African Veterinary Association, 85, e1–e7. 10.4102/jsava.v85i1.1075 [DOI] [PubMed] [Google Scholar]
- Gubbins S, Stegeman A, Klement E, Pite L, Broglia A and Cortinas Abrahantes J, 2020. Inferences about the transmission of lumpy skin disease virus between herds from outbreaks in Albania in 2016. Preventive Veterinary Medicine, 181, 104602. 10.1016/j.prevetmed.2018.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haegeman A, Zro K, Vandenbussche F, Demeestere L, Van Campe W, Ennaji MM and De Clercq K, 2013. Development and validation of three Capripoxvirus real‐time PCRs for parallel testing. Journal of Virological Methods, 193, 446–451. 10.1016/j.jviromet.2013.07.010 [DOI] [PubMed] [Google Scholar]
- Haegeman A, De Leeuw I, Mostin L, Van Campe W, Aerts L, Vastag M and De Clercq K, 2020. An Immunoperoxidase Monolayer Assay (IPMA) for the detection of lumpy skin disease antibodies. Journal of Virological Methods, 277, 113800. 10.1016/j.jviromet.2019.113800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedger R and Hamblin C, 1983. Neutralising antibodies to lumpy skin disease virus in African wildlife. Comparative Immunology, Microbiology and Infectious Diseases. 10.1016/0147-9571(83)90012-7 [DOI] [PubMed] [Google Scholar]
- Irons PC, Tuppurainen ES and Venter EH, 2005. Excretion of lumpy skin disease virus in bull semen. Theriogenology, 63, 1290–1297. 10.1016/j.theriogenology.2004.06.013 [DOI] [PubMed] [Google Scholar]
- Issimov A, Kutumbetov L, Orynbayev MB, Khairullin B, Myrzakhmetova B, Sultankulova K and White PJ, 2020. Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys Spp (Stomoxys Calsitrans, Stomoxys Sitiens, Stomoxys Indica), Diptera: Muscidae. Animals (Basel), 10. 10.3390/ani10030477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahana‐Sutin E, Klement E, Lensky I and Gottlieb Y, 2017. High relative abundance of the stable fly Stomoxys calcitrans is associated with lumpy skin disease outbreaks in Israeli dairy farms. Medical and Veterinary Entomology, 31, 150–160. 10.1111/mve.12217 [DOI] [PubMed] [Google Scholar]
- Lamien CE, Lelenta M, Goger W, Silber R, Tuppurainen E, Matijevic M, Luckins AG and Diallo A, 2011. Real time PCR method for simultaneous detection, quantitation and differentiation of capripoxviruses. Journal of Virological Methods, 171, 134–140. 10.1016/j.jviromet.2010.10.014 [DOI] [PubMed] [Google Scholar]
- Mathijs E, Vandenbussche F, Haegeman A, King A, Nthangeni B, Potgieter C, Maartens L, Van Borm S and De Clercq K, 2016. Complete genome sequences of the neethling‐like lumpy skin disease virus strains obtained directly from three commercial live attenuated vaccines. Genome Announc, 4. 10.1128/genomeA.01255-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathijs E, Vandenbussche F, Ivanova E, Haegeman A, Aerts L, De Leeuw I, Van Borm S and De Clercq K, 2020. Complete coding sequence of a lumpy skin disease virus from an outbreak in Bulgaria in 2016. Microbiol Resour Announc, 9. 10.1128/MRA.00977-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menasherow S, Erster O, Rubinstein‐Giuni M, Kovtunenko A, Eyngor E, Gelman B, Khinich E and Stram Y, 2016. A high‐resolution melting (HRM) assay for the differentiation between Israeli field and Neethling vaccine lumpy skin disease viruses. Journal of Virological Methods, 232, 12–15. 10.1016/j.jviromet.2016.02.008 [DOI] [PubMed] [Google Scholar]
- Miteva A, Alexandrov T, Zdravkova A, Ivanova PP, Chobanov G and Ivanova E, 2017. Emergence of Lumpy Skin Disease in Bulgaria: Epidemiological Situation, Control and Eradication. Special edition on Lumpy Skin Disease Edition, FAO (Food and Agriculture Organization of the United Nations). [Google Scholar]
- Moller J, Moritz T, Schlottau K, Krstevski K, Hoffmann D, Beer M and Hoffmann B, 2019. Experimental lumpy skin disease virus infection of cattle: comparison of a field strain and a vaccine strain. Archives of Virology, 164, 2931–2941. 10.1007/s00705-019-04411-w [DOI] [PubMed] [Google Scholar]
- OIE (World Organisation for Animal Health), 2002. Lumpy skin disease ‐ disease card. Available online: https://www.oie.int/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/Disease_cards/LUMPY_SKIN_DISEASE_FINAL.pdf
- OIE (World Organisation for Animal Health), 2018. Lumpy Skin Disease. Available online: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.04.12_LSD.pdf
- Roche X, Rozstalnyy A, TagoPacheco D, Pittiglio C, Kamata A, Beltran Alcrudo D, Bisht K, Karki S, Kayamori J, Larfaoui F, Raizman E, VonDobschuetz S, Dhingra MS and Sumption K, 2020. Introduction and spread of lumpy skin disease in South, East and Southeast Asia: qualitative risk assessment and management. FAO, Rome. [Google Scholar]
- Saegerman C, Bertagnoli S, Meyer G, Ganière J‐P, Caufour P, De Clercq K, Jacquiet P, Fournié G, Hautefeuille C, Etore F and Casal J, 2018. Risk of introduction of lumpy skin disease in France by the import of vectors in animal trucks. PLoS ONE, 13, e0198506. 10.1371/journal.pone.0198506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohier C, Haegeman A, Mostin L, De Leeuw I, Campe WV, De Vleeschauwer A, Tuppurainen ESM, van den Berg T, De Regge N and De Clercq K, 2019. Experimental evidence of mechanical lumpy skin disease virus transmission by Stomoxys calcitrans biting flies and Haematopota spp. horseflies. Scientific Reports, 9. 10.1038/s41598-019-56605-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprygin A, Pestova Y, Wallace DB, Tuppurainen E and Kononov AV, 2019. Transmission of lumpy skin disease virus: a short review. Virus Research, 269, 197637. 10.1016/j.virusres.2019.05.015 [DOI] [PubMed] [Google Scholar]
- Stubbs S, Oura CA, Henstock M, Bowden TR, King DP and Tuppurainen ES, 2012. Validation of a high‐throughput real‐time polymerase chain reaction assay for the detection of capripoxviral DNA. Journal of Virological Methods, 179, 419–422. 10.1016/j.jviromet.2011.11.015 [DOI] [PubMed] [Google Scholar]
- Tasioudi KE, Antoniou SE, Iliadou P, Sachpatzidis A, Plevraki E, Agianniotaki EI, Fouki C, Mangana‐Vougiouka O, Chondrokouki E and Dile C, 2016. Emergence of Lumpy Skin Disease in Greece, 2015. Transbound Emerg Dis, 63, 260–265. 10.1111/tbed.12497 [DOI] [PubMed] [Google Scholar]
- Tulman ER, Afonso CL, Lu Z, Zsak L, Sur J‐H, Sandybaev NT, Kerembekova UZ, Zaitsev VL, Kutish GF and Rock DL, 2002. The Genomes of Sheeppox and Goatpox Viruses. Journal of Virology, 76, 6054–6061. 10.1128/jvi.76.12.6054-6061.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuppurainen ESM, Venter EH and Coetzer JAW, 2005. The detection of lumpy skin disease virus in samples of experimentally infected cattle using different diagnostic techniques. Onderstepoort Journal of Veterinary Research, 72, 153–164. [DOI] [PubMed] [Google Scholar]
- Tuppurainen ESM, Lubinga JC, Stoltsz WH, Troskie M, Carpenter ST, Coetzer JA, Venter EH and Oura CA, 2013. Evidence of vertical transmission of lumpy skin disease virus in Rhipicephalus decoloratus ticks. Ticks Tick Borne Dis, 4, 329–333. 10.1016/j.ttbdis.2013.01.006 [DOI] [PubMed] [Google Scholar]
- Tuppurainen ESM, Alexandrov T and Beltrán‐Alcrudo D, 2017a. Lumpy skin disease field manual – A manual for veterinarians. Food and Agriculture Organization of the United Nations (FAO). Animal Production and Health Manual Place. Available online: http://www.fao.org/ag/againfo/home/en/news_archive/2017_New_field_manual_on_lumpy-skin-disease.html [Google Scholar]
- Tuppurainen ESM, Venter EH, Shisler JL, Gari G, Mekonnen GA, Juleff N, Lyons NA, De Clercq K, Upton C, Bowden TR, Babiuk S and Babiuk LA, 2017b. Review: capripoxvirus diseases: current status and opportunities for control. Transboundary and Emerging Diseases, 64, 729–745. 10.1111/tbed.12444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuppurainen ESM, Antoniou SE, Tsiamadis E, Topkaridou M, Labus T, Debeljak Z, Plavsic B, Miteva A, Alexandrov T, Pite L, Boci J, Marojevic D, Kondratenko V, Atanasov Z, Murati B, Acinger‐Rogic Z, Kohnle L, Calistri P and Broglia A, 2020. Field observations and experiences gained from the implementation of control measures against lumpy skin disease in South‐East Europe between 2015 and 2017. Preventive Veterinary Medicine, 181, 104600. 10.1016/j.prevetmed.2018.12.006 [DOI] [PubMed] [Google Scholar]
- Turan N, Yilmaz A, Tekelioglu BK and Yilmaz H, 2017. Lumpy Skin Disease: global and Turkish Perspectives. Approaches in Poultry, Dairy & Veterinary Sciences, 1. 10.31031/APDV.2017.01.000504 [DOI] [Google Scholar]
- Ularamu HG, Lefebvre DJ, Haegeman A, Wungak YS, Ehizibolo DO, Lazarus DD, De Vleeschauwer AR and De Clercq K, 2020. Complex circulation of foot‐and‐mouth disease virus in cattle in Nigeria. Front Vet Sci, 7, 466. 10.3389/fvets.2020.00466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss K, 1968. Lumpy skin disease virus. Cytomegaloviruses. Rinderpest Virus. Lumpy Skin Disease Virus. Springer. pp. 111–131. [Google Scholar]
- Wolff J, Krstevski K, Beer M and Hoffmann B, 2020. Minimum infective dose of a lumpy skin disease virus field strain from North Macedonia. Viruses, 12. 10.3390/v12070768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeruham I, Nir O, Braverman Y, Davidson M, Grinstein H, Haymovitch M and Zamir O, 1995. Spread of lumpy skin disease in Israeli dairy herds. Veterinary Record, 137, 91–93. 10.1136/vr.137.4.91 [DOI] [PubMed] [Google Scholar]
- Young E, Basson PA and Weiss KE, 1970. Experimental infection of game animals with lumpy skin disease virus (prototype strain Neethling). Onderstepoort Journal of Veterinary Research, 37, 79–87. [PubMed] [Google Scholar]


