Abstract
Background
Internationally, patient and public involvement (PPI) is core policy for health service quality improvement (QI). However, authentic QI partnerships are not commonplace. A lack of patient and staff capability to deliver successful partnerships may be a barrier to meaningful QI collaboration.
Objectives
The research questions for this scoping review were: What is known regarding the capabilities required for healthcare staff and patients to effectively partner in QI at the service level?; and What is known regarding the best practice learning and development strategies required to build and support those capabilities?
Methods
A six-stage scoping review was completed. Five electronic databases were searched for publications from January 2010 to February 2020. The database searches incorporated relevant terms for the following concepts: capabilities for PPI in healthcare QI; and best practice learning and development strategies to support those capabilities. Data were analysed using descriptive statistics and qualitative content analysis.
Results
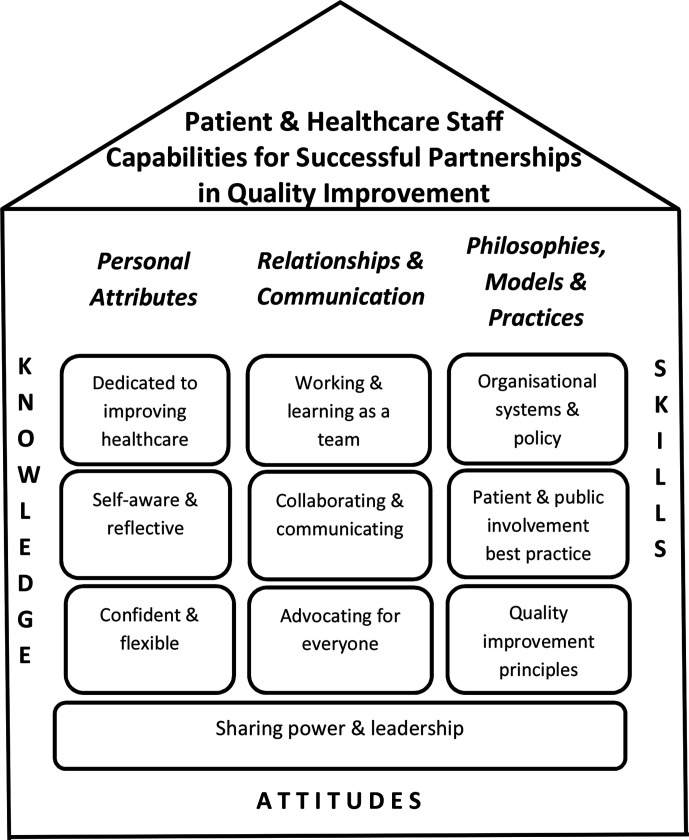
Forty-nine papers were included. Very little peer-reviewed literature focused explicitly on capabilities for QI partnerships and thus implicit paper content was analysed. A Capability framework for successful partnerships in healthcare quality improvement was developed. It includes knowledge, skills and attitudes across three capability domains: Personal Attributes; Relationships and Communication; and Philosophies, Models and Practices, and incorporates 10 capabilities. Sharing power and leadership was discussed in many papers as fundamental and was positioned across all of the domains. Most papers discussed staff and patients’ co-learning (n=28, 57.14%). Workshops or shorter structured training sessions (n=36, 73.47%), and face-to-face learning (n=34, 69.38%) were frequently reported.
Conclusion
The framework developed here could guide individualised development or learning plans for patient partners and staff, or could assist organisations to review learning topics and approaches such as training content, mentoring guidelines or community of practice agendas. Future directions include refining and evaluating the framework. Development approaches such as self-reflection, communities of practice, and remote learning need to be expanded and evaluated.
Keywords: attitudes, continuing education, continuing professional development, healthcare quality improvement, patient-centred care
Background
The WHO1 highlights the increasing complexity of healthcare and the critical role patient engagement plays in safety and quality improvement (QI). In addition, internationally, patient and public involvement (PPI) has become a core policy requirement for health service QI across the continuum of care. It is integral to accreditation,2–4 funding,5 and is a legislative requirement4 6 7 in many jurisdictions. PPI has been described as an ethical imperative which embraces the principles of inclusivity and mutual respect,8 and a political necessity due to the expectations of the public.9 In addition to the rightful role patients have in contributing to the quality of the design and delivery of services, they also have the necessary expertise given their lived experience of those services.10 The use of the term ‘patient’ in PPI initiatives is not universally endorsed.11 However, given there is no international agreement on terminology, this paper uses ‘patient’ to be inclusive of health service consumers, their families and carers, and members of the public.
PPI in health service QI may occur at three levels: direct care; organisational design and governance; or policymaking.12 13 Patient engagement at the direct care level includes communication, decision-making and partnerships that occur between individual clinicians and individual patients related to that specific patient’s healthcare journey.13 This paper will focus on PPI in QI for organisational design and governance, which is termed the service level here. Organisational design is defined as the planning, design, delivery, measurement and evaluation of systems and services.14 It includes patient: membership on governance or quality advisory committees; involvement in strategic or operational planning and priority setting; accreditation assessors; inclusion in QI project teams; and contribution to service evaluation through focus groups, surveys or interviews. The policymaking level refers to public agency policy development that governs healthcare systems rather than organisational policy which occurs at the service level and is within scope for this review.13 The service level was chosen as the focus for this review as, in the authors’ view, this is the level of PPI where patients, through the mechanisms described above, may have the most influence across an organisation which in turn may shape both direct care and high-level public policy.
The International Association for Public Participation (IAP2) Public Participation Spectrum15 is useful for understanding types of patient engagement across five levels from Inform to Consult to Involve to Collaborate to Empower. Patient–staff partnerships in QI can be mapped to the IAP2 Collaborate level as, in true partnerships, decisions incorporate patient recommendations to the maximum extent possible.15 Despite patient partnerships in health service QI being high on the international policy agenda, uptake has been limited across the healthcare continuum.5 16–19 Current efforts have been criticised as tokenistic,20 21 and with limited application due to health professional resistance or lack of knowledge about how to redress power disparities.18 Negative beliefs17 22 and insufficient understanding of successful PPI models5 and tools16 have also been discussed. The importance of education and training for both staff and patients to deliver a broader and more effective approach to QI partnerships has been highlighted.3 4 23 24
When considering education and training initiatives, the terms competency and capability are often used interchangeably, but there are fundamental differences. Capability is the ability to adapt to change, generate new knowledge and continuously improve performance within unfamiliar contexts (p799).25 Competencies are task focused and are usually measurable technical or procedural skills performed within a stable, predictable situation. In contrast, capabilities build on existing competencies, embrace the complexity of healthcare environments, incorporate self-esteem and confidence, and are more compatible with adult learning principles and lifelong learning.26 Thus, the term capability is used throughout this paper.
Preliminary searches identified a lack of literature directly discussing capabilities for successful QI partnerships, and so a formal literature review was warranted. Thus, the primary aim of this paper is to present the results of a scoping review which have been used to co-produce a patient and healthcare staff capability framework for successful partnerships in QI at the service level. The secondary aim is to provide recommendations regarding best practice learning and development strategies for building and supporting these capabilities.
Methods
The scoping review, on which the capability framework is based, was co-produced by a research team inclusive of two patients (service users and family/carers of patients: one an experienced patient advisor, and the other a hospital volunteer) and three health professionals (an academic, a research specialist based in community disability healthcare and a hospital clinical manager). In line with the policy, ethical and political imperatives included in the introduction, patient engagement in this research was essential. Including an academic and a research specialist in the team ensured research rigour with the addition of teaching and learning expertise from the academic. Inclusion of a hospital department manager with extensive experience in PPI in QI added a clinical perspective. The foundational principles and best practice activities for patient stakeholder engagement in research described by Harrison et al 27 were integral to the co-production approach used. The team regularly reviewed this framework, discussed examples of best practice implemented and brainstormed strategies for improvement.
The research questions were:
What is known regarding the capabilities required for healthcare staff and patients to effectively partner in QI at the service level?
What is known regarding the best practice learning and development strategies required to build and support those capabilities?
A scoping review methodology was suitable as the research question was exploratory with heterogeneous paper designs and settings, and there is insufficient evidence for interventions to be assessed through a systematic review.28 The EQUATOR (Enhancing the QUAlity and Transparency Of health Research), PRISMA-ScR (PRISMA extension for Scoping Reviews)29 and GRIPP2-SF (Guidance for Reporting Involvement of Patients and the Public‐Short Format)30 checklists were used to facilitate quality reporting. An audit trail and research team meeting records were maintained.
The research team, inclusive of the patients, had collaborated on a previous scoping review. The associated publication details patient learning and development processes including sharing expectations, role clarification, best practice research engagement principles, scoping review methodology and qualitative data analysis.31 The research team built on the learning and met 13 times, over 10 months for approximately 23 hours in total for the current review. Patient learning and development was flexible, occurred as required, and addressed their expressed and anticipated learning needs. ‘On-the-job training’, coaching and peer support were provided at team meetings. Other learning included a health librarian-led electronic database orientation and an initial paper screening session with the first author.
Five databases were searched: Medline Complete, CINAHL Complete, APA PsycINFO, EMBASE and SCOPUS. Grey literature was not searched due to the reported high risk of bias22 and the aim to build a framework based on the best available evidence and expert opinion. All papers were in English and published between 01 January 2010 and 29 February 2020 in order to capture contemporary research and practice. Due to the challenge of terminology variations in the PPI literature, language used in key papers such as engagement, involvement, participation and partnering helped guide search terms as recommended elsewhere.10 A health librarian provided advice and the PPI and research experiences of the authors also informed the development of search terms. Four key concepts (each with multiple search terms) were included: (1) capability and/or learning and development; (2) PPI; (3) organisational design or QI at the service level; (4) hospital or healthcare. For transparency and repeatability, the SCOPUS and EMBASE search terms and methods are included in online supplemental appendix A. Papers were downloaded to reference management software and then uploaded to the Covidence web-based systematic review platform.32
bmjqs-2020-012729supp001.pdf (71.4KB, pdf)
The title and abstract of all papers were independently screened by two authors with the first author reviewing all papers. The patients screened approximately 40 papers and then decided not to continue due to the high time commitment and not feeling confident in their decisions. The other authors completed the screening. Any discrepancies or uncertainties were resolved through discussion with one or more additional health professional authors. A full-text review was conducted on remaining articles by the health professional authors to determine eligibility. Inclusion criteria were: (1) contains discussion or implementation of PPI in healthcare QI at the service level; and (2) original research, or a literature review, or an opinion/conceptual paper; and (3) contains information regarding training, education, learning, development, capabilities and/or competencies to support PPI; and (4) originates from a comparable health context (ie, UK, USA, Australia, Canada, New Zealand, Europe). Exclusion criteria were: (1) topic is exclusively about research processes; and/or (2) focus is only at the direct care or policy level; and/or (3) study protocol, or abstract only, or book (chapter), or thesis, or letter to the editor; and/or (4) not clearly peer reviewed; and/or (5) regarding oral health. Oral health was not included as these are mainly private sector services in Australia (where the review was conducted), and the focus on PPI for QI may be different.
Using the same eligibility criteria, snowball searching of citations through Google Scholar and ancestry searching of reference lists were conducted for all papers included from the database searches. These steps were not repeated for papers included via snowball and ancestry searching. All volumes of the Patient Experience Journal were searched within the date parameters as a patient research team member identified papers from this journal as relevant, and it was not indexed in the searched databases.
A data extraction spreadsheet was developed and modified as required. It included: paper source; year of publication; country; aim/purpose; paper method; stakeholders included; health service context; health condition; description of QI activities discussed; and whether the paper had a PPI in QI capability and/or learning and development focus, or if this information was incidentally reported. Similar to other authors,24 verbatim text data on themes, concepts, and categories relevant to the research questions were copied and pasted into the spreadsheet for qualitative content analysis including: capabilities; learning and development strategies; facilitators and challenges to successful PPI in QI; and recommendations for future PPI initiatives and/or research. Data extraction for all papers was completed by the first author. Fourteen randomly selected papers (approximately 30%) were checked by an additional author, with the patients completing 10 of these checks. A high level of agreement was achieved, and so further independent review was not warranted.
Data analysis
Descriptive statistics were used to analyse main paper characteristics. Qualitative data were analysed using qualitative content analysis as this method is suitable for inductive qualitative analysis and where interpretation of latent content is required.33 The first author completed preliminary inductive open coding for patient and healthcare staff capabilities using all qualitative data including where papers inferred capabilities through discussion of training content, role descriptions, barriers, facilitators and recommendations. The preliminary codes were then revised and refined by all authors and similar codes placed into categories. Categories were then grouped, revised and refined until the final capability categories were agreed on and domains developed. The capabilities for successful partnerships in QI were then defined and a framework was developed. Categories were also mapped across patient and staff capabilities. Analysis of the capability data required considerable research team discussion and interpretation due to the substantial latent content. The research team’s strong commitment to meaningful partnerships in research and health service QI influenced data analysis and interpretation. Critical discussion and reflection regarding research team PPI experiences and attitudes occurred throughout the planning and execution of this study in order to raise awareness of individual biases and to enhance reflexivity. As recommended for qualitative research,34 the first author facilitated this process by keeping a reflexive diary and taking field notes during meetings. This enabled reflection and discussion regarding unspoken elements and emotional aspects of interactions which assisted the first author to lead reflective discussions during research team meetings.
Results
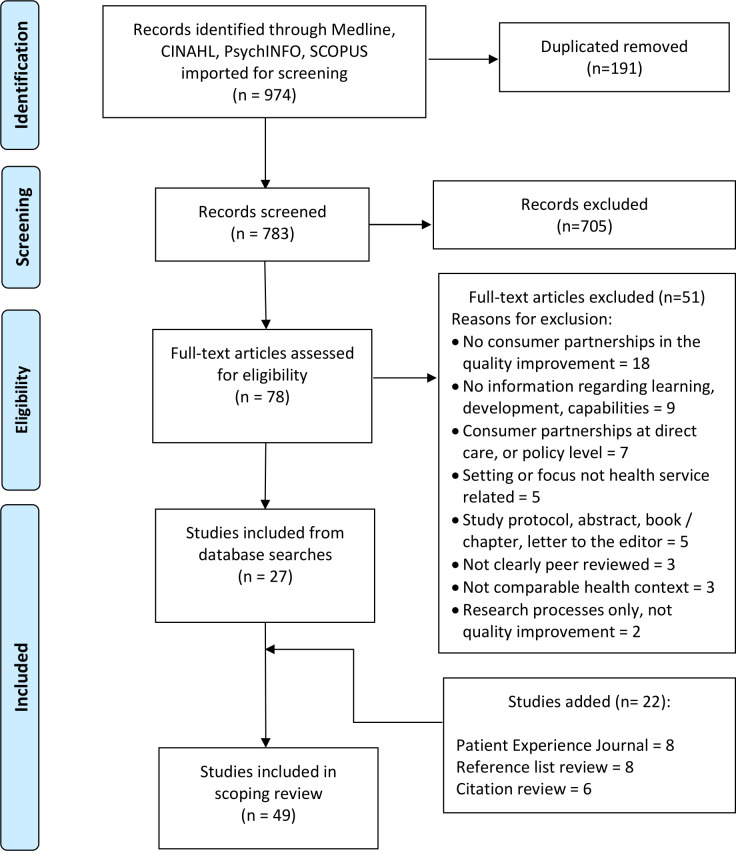
Forty-nine (49) papers were included (see figure 1 for the PRISMA study selection flow chart).35 Online supplemental appendix B includes a summary table of all papers including aim, method, stakeholders, setting, focus relevant to the research questions, and description or examples of QI discussed. The types of QI activities described in the papers were varied across service planning, design, delivery, measurement and evaluation (see online supplemental appendix B) for details. Many papers described specific QI initiatives such as streamlining patient bookings,36 improving bedside rounding,37 redesigning clinic physical layout,38 improving understanding of advance care planning,39 optimising timing of paediatric immunisations40 and developing staff training regarding preventing harm.41 Other papers were less specific and reported that patients worked on projects to improve general practitioner services for patients with back pain,42 assisted teams to meet falls-related accreditation standards43 or participated in audits regarding best practice for chronic disease.44 PPI in QI governance such as patient inclusion on health service boards,10 45 strategic planning committees,46 47 and standing QI or patient advisory committees48–50 were also discussed. Both healthcare staff and patients were included as stakeholders for 75.51% (n=37) of papers. Table 1 summarises the main characteristics of each included paper. Approximately half (n=27, 55.10%) of the papers were identified through the database searches. Papers tended to be published more recently (n=37, 75.51% in 2015 and later) and originated from Canada (n=19, 38.76%), the USA (n=10, 20.40%) and seven other countries. Qualitative research was the most frequent method (n=19, 38.78%). Most papers focused on more than one service context in the care continuum (n=29, 59.18%) and more than half were generalist in scope (n=27, 55.10%). Capabilities and/or learning and development for PPI in QI were incidentally reported for most papers (n=34, 69.38%).
Figure 1.
Study selection flow diagram.
Table 1.
Main characteristics of included papers
| Paper characteristic | Categories | Results | |
| n | % | ||
| Paper source | Citation | 6 | 12.24 |
| Patient Experience Journal search | 8 | 16.33 | |
| Reference list | 8 | 16.33 | |
| Database search | 27 | 55.10 | |
| Year of publication | 2010 | 0 | 0.00 |
| 2011 | 1 | 2.04 | |
| 2013 | 2 | 4.08 | |
| 2014 | 4 | 8.16 | |
| 2015 | 5 | 10.20 | |
| 2016 | 6 | 12.24 | |
| 2017 | 5 | 10.20 | |
| 2018 | 11 | 22.45 | |
| 2019 | 13 | 26.53 | |
| 2020* | 2 | 4.08 | |
| Country of origin | France | 1 | 2.04 |
| Netherlands | 1 | 2.04 | |
| Norway | 1 | 2.04 | |
| New Zealand | 2 | 4.08 | |
| Ireland | 2 | 4.08 | |
| Australia | 6 | 12.24 | |
| UK | 7 | 14.29 | |
| USA | 10 | 20.41 | |
| Canada | 19 | 38.78 | |
| Method | Quantitative research | 2 | 4.08 |
| Case study | 3 | 6.12 | |
| Opinion piece | 3 | 6.12 | |
| Literature review | 4 | 8.16 | |
| Reflection | 8 | 16.33 | |
| Mixed methods | 10 | 20.41 | |
| Qualitative research | 19 | 38.78 | |
| Health service context | Other | 2 | 4.08 |
| General practice/primary care | 8 | 16.33 | |
| Hospital | 10 | 20.41 | |
| More than one, for example, hospital and community | 29 | 59.18 | |
| Health condition | Mental health | 4 | 8.16 |
| Chronic disease | 5 | 10.20 | |
| More than one | 5 | 10.20 | |
| Other (eg, cancer care, older persons, paediatrics and youth) | 8 | 16.32 | |
| Generalised scope | 27 | 55.10 | |
| Capabilities and/or learning and development focus | Capabilities only | 1 | 2.04 |
| Both capabilities, and learning and development | 4 | 8.16 | |
| Learning and development only | 10 | 20.41 | |
| Incidental reporting of both | 34 | 69.39 | |
*Search conducted on 29 February 2020.
bmjqs-2020-012729supp002.pdf (257.2KB, pdf)
Capability framework for successful partnerships in QI
The qualitative content analysis revealed codes which consisted of specific capabilities and descriptors. These capabilities were further refined into capability categories and then grouped into domains. The research team used these data to co-produce a Capability framework for successful partnerships in QI (see table 2). Online supplemental appendix C includes all references against each capability descriptor and delineates papers which discussed each capability for staff or patients, or both. The data revealed that all of the capabilities were applicable to both staff and patients, as there were papers that discussed each capability in relation to both groups. As discussed below, some capabilities were discussed more frequently for one group or the other. The following results include individual capabilities in italics and describe each with examples and indicative references.
Table 2.
Capability framework for successful partnerships in healthcare quality improvement
| Domain | Capability and description |
| Personal Attributes |
Dedicated to improving healthcare
|
Self-aware and reflective
| |
Confident and flexible
| |
| Relationships and Communication |
Working and learning as a team
|
Collaborating and communicating
| |
Advocating for everyone
| |
| Philosophies, Models and Practices |
Organisational systems and policies
|
Patient and public involvement (PPI) best practice
| |
Quality improvement (QI) principles and processes
| |
| Across all Domains |
Sharing power and leadership
|
bmjqs-2020-012729supp003.pdf (157.4KB, pdf)
Personal Attributes domain
The Personal Attributes domain includes knowledge, skills and attitudes (capabilities) which reside within the individual. Many papers discussed the importance of staff and patients being Dedicated to improving healthcare. For example, papers reported that the desire of both patients and staff to improve services was essential to success24 51 52 and was often personally rewarding.53–55 This motivation led to a sustained commitment to QI partnerships9 51 53 and increasingly sophisticated levels of engagement.53 The importance of patients and staff being Self-aware and reflective was also discussed. To be effective QI partners, patients needed to reflect on and share their personal experiences while also keeping some distance from them.47 51 56 In addition, patients and staff needed to be in tune with their emotional reactions and behaviours and how these may influence others.42 46 52 The Confident and flexible capability included actively engaging in constructive dialogue in a group, inclusive of all stakeholders, and was primarily reported with respect to patients.3 37 42 47 51 52 57–65 A need to be flexible in unfamiliar and evolving situations was also reported, including dealing with uncertainty as QI initiatives progress66; patients collaborating when unsure about what was involved39 and staff accepting that roles may evolve in unpredictable ways.67
Relationships and Communication domain
The Relationships and Communication domain includes capabilities for working effectively with others. Many papers referred to the QI ‘team’, inclusive of patients,3 39 57 68 69 and the importance of Working and learning as a team. Being an active and effective team member, including contributing to quality team functioning was described as essential.43 52 Recognising the unique and valuable contributions of each team member, including understanding that all members had their own expertise, was also considered necessary.6 70 The capability to embrace co-learning was important24 as this contributed to personal growth,54 coalition building6 42 and the co-creation of knowledge.64 Collaborating and communicating were additional capabilities for productive QI partnerships including building consensus by listening and speaking constructively,58 67 finding common ground10 and creating valuable connections.66 71 Strong conflict resolution and negotiation skills were viewed as paramount both for patients and staff.4 9 22 58 66 Building respectful, constructive and reciprocal relationships was highlighted,10 50 66 with honesty,42 patient avoidance of a combative approach63 and a virtuous cycle of a shared journey67 emphasised. Advocating for everyone rather than personal interests was also considered valuable. This included influencing change to improve PPI by embracing lived experience knowledge,9 of patients, their families55 and the community.47 Promoting the needs of marginalised peoples7 38 48 64 including representing those without a voice,61 63 and the role of senior leadership in advocacating for disadvantaged groups3 10 38 were also emphasised. There was a reported need for capabilities regarding sharing success, networking and linking diverse stakeholders across geographical areas and organisations59 66; educating others regarding the valuable patient role in QI6 69 and systems advocacy,22 60 especially by organisational leaders.38 56 69
Philosophies, Models and Practices domain
The Philosophies, Models and Practices domain focuses on capabilities which enable patients and staff to work effectively within an organisational context and with the requisite practical skills. Works within organisational priorities, governance, policies, resources and constraints was viewed as an essential capability as this reduced patient frustration,67 and enabled shared insights into the changes needed.38 70 Abilities to work within confidentiality requirements,3 47 50 57 committee procedures45 48 58 60 and patient reimbursement and compensation guidelines4 39 54 56 were also discussed. Organisational knowledge facilitated development of sustainable solutions by patients and staff.9 58 66 Being aware of relevant clinical processes and having sufficient health literacy were noted as essential for effective collaboration mainly for patients.41 48 58 60 68 The value of understanding and implementing PPI best practice was seen as a requirement for QI partnership success including a commitment to the inherent value of PPI, especially for staff.5 40 44 54 60 65 71–73 This capability included implementing a variety of PPI principles and practices such as experience-based co-design,9 71 developing lay content,41 70 recruiting and retaining consumer partners,44 60 68 and evaluating engagement initiatives.6 9 66 Effectively conveying one’s own experience in order to positively influence QI was seen as key not only for patients but also for staff.3 39 42 47 56 73 The requirement to facilitate teaching and learning for productive QI partnerships, including coaching and mentoring, was mainly reported as a specialised skill for paid or experienced patient advisors and staff.9 43 57 60 61 67 Similarly, provision of ongoing support and feedback, particularly to patient partners, was deemed essential as this kept communication channels open,36 39 enhanced engagement capacity,10 66 facilitated safe transition out of engagement projects,3 24 and prevented potential negative impacts on health and well-being.61 72 The practical skills of understanding and implementing QI principles and processes across service planning, design, delivery and evaluation were discussed. In particular, the papers discussed the role of coaches,9 67 specialist QI teams57 63 or organisational leaders9 51 56 74 in supporting transformation of services through QI practical expertise.
Sharing power and leadership
The Sharing power and leadership capability was described as fundamental to all successful QI partnerships and is therefore positioned across all domains. Enhancing staff understanding and ability to address the traditional power differential of health services was frequently discussed.6 10 44 47 75 Additionally, patients were reported as needing to reconceptualise their expectations from being ‘users and choosers’ to being ‘makers and shapers’ of healthcare services.53 62 The need for organisational leaders to actively encourage this dynamic was reported.45 46 52 The necessity to intentionally prioritise shared decision-making and joint leadership, with staff having the courage to relinquish control42 and their paternalistic attitudes,24 and include patients from the beginning52 55 was discussed. The support of patient-led leadership models was noted as important53 73 with an active investment in patient leadership capability being required.45 64
A summary diagram was co-developed by the research team, inclusive of the patients, over two meetings, and with additional email and telephone correspondence. It provides a simplified and clear depiction of the capability domains and corresponding capabilities. This image emphasises the foundational nature of power sharing as the base and that capabilities include knowledge, skills and attitudes (see figure 2).
Figure 2.
Summary diagram of the Capability framework for successful partnerships in quality improvement.
Learning and development for partnerships in QI
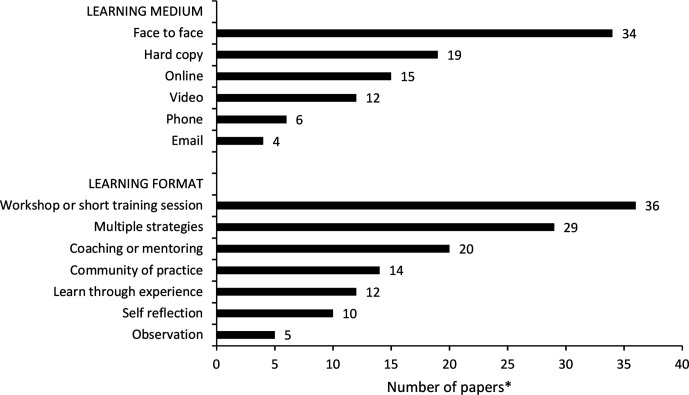
With respect to learning and development, many papers did not clearly describe specific strategies and so their data were not able to be categorised. Figure 3 summarises the learning and development media and formats reported. Most papers recommended that healthcare staff and patients learn together (n=28, 57.14%). Face to face was the most frequent learning medium described (n=34, 69.38%) and structured workshops or shorter training sessions were the most common learning format (n=36, 73.47%). Workshops and training sessions incorporated role-plays, small group discussions, case studies, quizzes and individual reflection. Multiple learning strategies were discussed in many papers (n=29, 34.48%), and coaching/mentoring was frequently discussed (n=20, 40.82%). Where specified, duration of learning varied from a half day orientation session to a 240-hour internship over 1 year.
Figure 3.
Learning medium and format for each paper (*many papers used more than one learning medium and format).
In addition to the details included in the methodology, and in line with best practice reporting for PPI in research,30 box 1 includes a summary of the extent of patient influence on the scoping review plus benefits and challenges of the patient engagement. The GRIPP2-SF checklist30 is included in online supplemental appendix D.
Box 1. Summary of the extent of the patient influence on the scoping review plus benefits and challenges of the patient engagement.
Extent of patient influence on study
Patients were core members of the research team and integral to all decisions.
Added a hand search of the Patient Experience Journal to the review which yielded eight additional papers.
Supplemented search terms based on patient experiences and their reading of patient-focused literature.
Added an emphasis on carers.
Stressed the importance of organisational leaders and culture in supporting patient engagement in quality improvement.
Focused attention on the need for the capability framework and diagram to be clear, simple and familiar, resulting in a house image.
Benefits of the patient research collaboration
Co-production was consistent with the philosophical paradigm of the research.
Clarifying questions from the patients ensured that health professionals’ assumptions and tacit knowledge were made explicit, discussed, evaluated and actioned accordingly.
Both patients were able to provide considerable time and attention to detail to data extraction and analysis.
A novel, hard copy, socially distanced method for independent data coding to accommodate patient preferences was developed.
Lively debate regarding patient and public involvement experiences resulted in enhanced team reflexivity.
Substantial co-learning by all authors resulted in enhanced research partnership capability for future projects.
Challenges of the patient research collaboration
Use of the term ‘patient’, while agreed as relevant to an international audience, did not sit comfortably with the consumer co-researchers’ role and identity given collaboration in this scoping review did not focus on them as recipients of healthcare.
Tailored learning and development strategies were required to ensure meaningful collaboration which required additional time from the first author.
A lack of confidence regarding the paper screening stage was expressed by the patients despite the support and training that was provided.
The patient preference not to perform coding on a computer screen meant that qualitative data were printed which added to the time required and research costs.
Negotiation with the patients was required to ensure that the focus of the research was international rather than based on local experiences.
The level of detail and time taken for a rigorous literature review resulted in some frustration for one of the patients who was action focused.
A lack of funding resulted in no hourly payment for patient time. However, expenses were reimbursed and there was a budget available for patient conference travel and accommodation as a strategy to recognise the valuable patient contributions.
Safety guidelines due to COVID-19 meant that some meetings were conducted via video-conferencing while the patients preferred face-to-face interactions.
bmjqs-2020-012729supp004.pdf (79.1KB, pdf)
Discussion
This scoping review examined the capabilities, including knowledge, skills and attitudes required for successful QI partnerships in healthcare at the service level. Results indicated that there was very little peer-reviewed literature focused explicitly on this topic and thus implicit paper content was analysed. The high proportion of recent papers incorporating qualitative or mixed methods research, author reflection or literature review demonstrates the emerging and exploratory nature of the topic and that guidance is required to support staff and patient development. The Capability framework for successful partnerships in QI which has been co-produced from this review may provide this structure and direction. An accompanying summary diagram (see figure 2) aims to make the framework user friendly. To our knowledge, the framework is the first to be developed from the international peer-reviewed literature regarding this concept. The framework adds to our current understanding of the breadth of capabilities required across the three framework domains which incorporate the dynamic interplay between the individual, social and organisational aspects of PPI described elsewhere.62 Interestingly, no capabilities were discussed exclusively in relation to patients or staff. This is reflected in the framework in that all capabilities are presented as important for both groups. Literature was reviewed from nine countries, across the healthcare continuum, including different health conditions and a variety of PPI stakeholders. Thus, the framework is flexible enough to accommodate local needs.
In particular, the capability to build and support a strong foundation of sharing power and leadership was reported as necessary for QI partnerships to flourish. This core requirement to address historical power imbalances has been emphasised21 76 but potentially has not been discussed as a capability that requires development. To be truly transformative, empowerment of patients to lead change in healthcare is needed,24 and the framework reflects this paradigm shift towards the Empower IAP2 level.15 Building on positive views, raising self-awareness and influencing negative perceptions through authentic interactions between stakeholders, as well as formal learning opportunities, have been recommended to support attitude change and capability development for QI partnerships.77 Participatory processes to achieve this may include values and beliefs, exercises and democratic dialogue10; sense-giving activities77 and dialogical ethics approaches.9 The framework could be used to structure and guide these initiatives.
In addition, team co-learning, rather than learning in silos, may improve quality and safety78 and is fundamental to the framework. Building consensus, conflict resolution, respect and reciprocal relationships are included in other interprofessional healthcare capability frameworks.79 80 The current framework goes further by including patient partners as part of the team. Of note, there is only one capability description for QI principles and processes in the framework. This reinforces the research team’s view, and that of others,44 62 67 that practical or technical skills, while important, are just one small contributor to authentic partnerships in QI. The key influence of organisational leaders in supporting capability development across all of the domains to ensure strategic alignment and organisational sustainability of co-produced QIs was discussed as essential.3 7 10 74
Implementing the framework
The framework could be used across many adult learning pedagogies to support capability development through individual learning plans based on self-reflection and/or feedback from peers, mentors or coaches. These strategies are compatible with experiential, reflective and transformative learning theories, for example.81 A personalised learning approach that encompasses humanistic and self-directed learning theory,81 including the use of learning plans with patient partners, in particular, is worthy of future examination. Implementing new practices in a complex system such as health services requires ‘deliberate learning’ which is conscious and goal directed.25 The framework could support this process if used as a template for mapping current learning resources, to identify strengths and gaps, and also in training needs analyses. At the organisational level, the framework could guide documentation of role statements and selection criteria for QI project teams and committees. Universities could also refer to the framework when developing curricula.
Best practice learning and development approaches
Patients are part of the QI team and so co-learning is critical4 6 43 44 67 as reflected in the framework. There was, however, limited consideration of learning strategies and theory in the literature. The main approaches used were pre-prepared and structured face-to-face learning, through workshops or short education sessions. These modes may not reflect current best practice given adult learners require individualised approaches that build on what they already know, their experiences and their motivations to learn.81 Recently, authors recommended health professional team reflexivity as a developmental strategy to support patient safety and high-quality care.78 This reflective and experiential learning approach was discussed in a number of papers as useful to enhance QI partnerships.5 36 42 43 50 64 75 Many papers alluded to communities of practice (CoP) as a knowledge creation strategy for partnerships in QI but did not elaborate on, nor evaluate this approach. CoP are best practice in contemporary healthcare education as they are collaborative, involve problem-solving in a specific, shared context, are focused on development of expertise,82 and are underpinned by the social theory of learning.81 Alternatives to structured workshops should be expanded and evaluated to better meet the needs of adult learners.
Limitations
The inconsistent definition and reporting of PPI concepts in the literature, as described previously,9 10 resulted in challenges locating relevant literature. There was also a tendency for papers to inadequately separate PPI for QI at the individual patient care, service and policy levels. Papers were included if most of the content was describing the service level. An additional limitation is that opinion pieces, reflective papers and literature reviews were included, rather than only original research. This may have resulted in inclusion of lower level evidence. However, much like clinical practice guidelines, expert opinion is warranted when there is insufficient high-level evidence. Oral health was not included which may have excluded papers from countries where this sector may have a strong PPI focus. Non-English-language papers were also excluded, which may have resulted in missed data. In addition, the focus on literature from Western high-income countries, with only one paper inclusive of First Nation Peoples’ perspectives,44 may limit generalisability. Finally, qualitative analysis, by definition, is a subjective process. However, the diversity of the research team, which included two patients and three health professionals, enhanced trustworthiness.
Future directions
The next step is to refine the framework which may involve qualitative interviews, Delphi surveys or observational studies of high performing QI partnerships. Implementation studies could follow, and these would explore application of the framework in practice. Comparison of findings internationally and across healthcare settings would be useful to ascertain contextual factors which influence partnership capabilities. Evaluation of learning and development approaches is also needed, particularly for non-traditional strategies such as self-reflection and reflexivity, CoP and remote learning.
Conclusions
Authentic and effective patient–staff partnerships in QI at the healthcare service level require specific capabilities which incorporate adaptation to change, generation of new knowledge and continuous improvement of performance. The novel Capability framework for successful partnerships in QI described here has been co-produced from a scoping review. It includes three domains and 10 capabilities. This framework could be used to support individual learning planning, gap analysis of organisational learning resources and training needs analyses.
Footnotes
Twitter: @RuthCox_OccThy, @mmolineux
Contributors: RC conceptualised the study as part of her doctoral research which was supervised by MM and MK. All authors contributed to all aspects of the study across the research cycle. RC developed the first draft of the manuscript and all authors reviewed and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement statement: This was a co-produced scoping review in full partnership with two consumer co-authors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Approval was necessary for detailed publication of the results of the patient co-researcher partnership. Approval was granted by the Metro South Health Human Research Ethics Committee (MS HREC/2019/QMS/52675) and the Griffith University Human Research Ethics Committee (GU Ref No: 2019/659).
References
- 1. World Health Organization . Patients for patient safety: partnerships for safer health care. Geneva, Switzerland: WHO Press, 2013. [Google Scholar]
- 2. Australian Commission on Safety and Quality in Health Care . Partnering with consumers standard. Sydney, NSW: Australian Commission on Safety and Quality in Health Care, 2019. http://nationalstandards.safetyandquality.gov.au/2.-partnering-consumers [Accessed 24 Oct 2020] [Google Scholar]
- 3. Clavel N, Pomey M-P, Ghadiri DPS. Partnering with patients in quality improvement: towards renewed practices for healthcare organization managers? BMC Health Serv Res 2019;19:815. 10.1186/s12913-019-4618-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kuluski K, Kokorelias KM, Peckham A, et al. Twelve principles to support caregiver engagement in health care systems and health research. Patient Exp J 2019;6:141–8. 10.35680/2372-0247.1338 [DOI] [Google Scholar]
- 5. Pandhi N, Jacobson N, Crowder M, et al. Engaging patients in primary care quality improvement initiatives: facilitators and barriers. Am J Med Qual 2020;35:52–62. 10.1177/1062860619842938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fancott C, Baker GR, Judd M, et al. Supporting patient and family engagement for healthcare improvement: reflections on "engagement-capable environments" in Pan-Canadian learning collaboratives. Healthc Q 2018;21:12–30. 10.12927/hcq.2018.25642 [DOI] [PubMed] [Google Scholar]
- 7. Rise MB, Solbjør M, Steinsbekk A. Experiences from the implementation of a comprehensive development plan for user involvement in a mental health hospital: a qualitative case study. Int J Soc Psychiatry 2014;60:387–95. 10.1177/0020764013491739 [DOI] [PubMed] [Google Scholar]
- 8. Holroyd-Leduc J, Resin J, Ashley L, et al. Giving voice to older adults living with frailty and their family caregivers: engagement of older adults living with frailty in research, health care decision making, and in health policy. Res Involv Engagem 2016;2:19. 10.1186/s40900-016-0038-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dimopoulos-Bick T, Osten R, Shipway C, et al. Shared decision making implementation: a case study analysis to increase uptake in New South Wales. Aust Health Rev 2019;43:492–9. 10.1071/AH18138 [DOI] [PubMed] [Google Scholar]
- 10. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci 2018;13:22. 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morley R, Chapman S. Evidently Cochrane [Internet], 2017. Cochrane UK. Available: https://www.evidentlycochrane.net/patients-people-power-of-words/#:~:text=Patients%2C%20people%20and%20the%20power%20of%20words,-By%20Richard%20Morley&text=Here%2C%20Cochrane’s%20Richard%20Morley%20and,to%20the%20work%20in%20hand
- 12. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff 2013;32:223–31. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 13. Carman KL, Workman TA. Engaging patients and consumers in research evidence: applying the conceptual model of patient and family engagement. Patient Educ Couns 2017;100:25–9. 10.1016/j.pec.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 14. Australian Commission on Safety and Quality in Health Care . National safety and quality health service standards. 2nd ed. Sydney, NSW: Australian Commission on Safety and Quality in Health Care, 2017. [Google Scholar]
- 15. International Association for Public Participation Australasia . IAP2’s public participation spectrum. Toowong, Queensland: International Association for Public Participation Australasia, 2014. https://www.iap2.org.au/resources/spectrum/ [Google Scholar]
- 16. Farmer J, Bigby C, Davis H, et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services. BMC Health Serv Res 2018;18:1–13. 10.1186/s12913-018-3433-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sarrami-Foroushani P, Travaglia J, Debono D, et al. Implementing strategies in consumer and community engagement in health care: results of a large-scale, scoping meta-review. BMC Health Serv Res 2014;14:16. 10.1186/1472-6963-14-402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Scholz B, Bocking J, Platania-Phung C, et al. "Not an afterthought": power imbalances in systemic partnerships between health service providers and consumers in a hospital setting. Health Policy 2018;122:922–8. 10.1016/j.healthpol.2018.06.007 [DOI] [PubMed] [Google Scholar]
- 19. Zaga C, Leggat S, Hill S. Partnering with consumers in the public reporting of quality of care: review of the Victorian quality of care reports. Aust Health Rev 2018;42:550–6. 10.1071/AH16272 [DOI] [PubMed] [Google Scholar]
- 20. Armstrong N, Herbert G, Aveling E-L, et al. Optimizing patient involvement in quality improvement. Health Expect 2013;16:e36–47. 10.1111/hex.12039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf 2016;25:626–32. 10.1136/bmjqs-2015-004839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liang L, Cako A, Urquhart R, et al. Patient engagement in hospital health service planning and improvement: a scoping review. BMJ Open 2018;8:e018263-e. 10.1136/bmjopen-2017-018263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kovacs Burns K, Bellows M, Eigenseher C, et al. ‘Practical’ resources to support patient and family engagement in healthcare decisions: a scoping review. BMC Health Serv Res 2014;14:1–25. 10.1186/1472-6963-14-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Majid U, Gagliardi A. Clarifying the degrees, modes, and muddles of "meaningful" patient engagement in health services planning and designing. Patient Educ Couns 2019;102:1581–9. 10.1016/j.pec.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 25. Fraser SW, Greenhalgh T. Coping with complexity: educating for capability. BMJ 2001;323:799–803. 10.1136/bmj.323.7316.799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Connell J, Gardner G, Coyer F. Beyond competencies: using a capability framework in developing practice standards for advanced practice nursing. J Adv Nurs 2014;70:2728–35. 10.1111/jan.12475 [DOI] [PubMed] [Google Scholar]
- 27. Harrison JD, Auerbach AD, Anderson W, et al. Patient stakeholder engagement in research: a narrative review to describe foundational principles and best practice activities. Health Expect 2019;22:307–16. 10.1111/hex.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:9. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 30. Staniszewska S, Brett J, Simera I, Seers K, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3:11. 10.1186/s40900-017-0062-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cox R, Kendall M, Molineux M, et al. Consumer engagement in occupational therapy health-related research: a scoping review of the Australian Occupational Therapy Journal and a call to action. Aust Occup Ther J 2021;68:180–92. 10.1111/1440-1630.12704 [DOI] [PubMed] [Google Scholar]
- 32. Covidence systematic revew software [Internet], 2019. Veritas Health Innovation. Available: www.covidence.org [Accessed 14 Oct 2020].
- 33. Cho JY, Lee E-H. Reducing confusion about grounded theory and qualitative content analysis: similarities and differences. Qual Rep 2014;19:1–20. 10.46743/2160-3715/2014.1028 [DOI] [Google Scholar]
- 34. Elliott H, Ryan J, Hollway W. Research encounters, reflexivity and supervision. Int J Soc Res Methodol 2012;15:433–44. 10.1080/13645579.2011.610157 [DOI] [Google Scholar]
- 35. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bak K, Macdougall L, Green E, et al. Hindsight is 20/20: lessons learned after implementing experience based design. Patient Exp J 2014;1:12–19. 10.35680/2372-0247.1035 [DOI] [Google Scholar]
- 37. Lavallee DC, Blakeney EA-R, Yu Y, et al. Engaging patients and families to transform heart failure care. J Interprof Care 2020;34:1–4. 10.1080/13561820.2019.1696286 [DOI] [PubMed] [Google Scholar]
- 38. Bar S, Grant K, Asuri S, et al. British Columbia Ministry of Health Patients as Partners: a transformational approach. Healthc Manage Forum 2018;31:51–6. 10.1177/0840470417744569 [DOI] [PubMed] [Google Scholar]
- 39. Maher LM, Hayward B, Hayward P, et al. Increasing patient engagement in healthcare service design: a qualitative evaluation of a co-design programme in New Zealand. Patient Exp J 2017;4:23–32. 10.35680/2372-0247.1149 [DOI] [Google Scholar]
- 40. Davis S, Berkson S, Gaines ME, et al. Implementation science workshop: engaging patients in team-based practice redesign - critical reflections on program design. J Gen Intern Med 2016;31:688–95. 10.1007/s11606-016-3656-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kirby J, Cannon C, Darrah L, Milliman-Richard Y, et al. Partnering with pediatric patients and families in high reliability to identify and reduce preventable safety events. Patient Exp J 2018;5:76–90. 10.35680/2372-0247.1287 [DOI] [Google Scholar]
- 42. Worswick L, Little C, Ryan K, et al. Interprofessional learning in primary care: an exploration of the service user experience leads to a new model for co-learning. Nurse Educ Today 2015;35:283–7. 10.1016/j.nedt.2014.05.007 [DOI] [PubMed] [Google Scholar]
- 43. Miller W, Asselbergs M, Bank J, et al. Homecare safety virtual quality improvement collaboratives. Healthc Q 2020;22:100–11. 10.12927/hcq.2020.26042 [DOI] [PubMed] [Google Scholar]
- 44. Larkins S, Carlisle K, Turner N, et al. 'At the grass roots level it's about sitting down and talking': exploring quality improvement through case studies with high-improving Aboriginal and Torres Strait Islander primary healthcare services. BMJ Open 2019;9:e027568. 10.1136/bmjopen-2018-027568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scholz B, Bocking J, Happell B. How do consumer leaders co-create value in mental health organisations? Aust Health Rev 2017;41:505–10. 10.1071/AH16105 [DOI] [PubMed] [Google Scholar]
- 46. Pomey M-P, Morin E, Neault C, et al. Patient advisors: how to implement a process for involvement at all levels of governance in a healthcare organization. Patient Exp J 2016;3:99–112. 10.35680/2372-0247.1134 [DOI] [Google Scholar]
- 47. Nathan S, Johnston L, Braithwaite J. The role of community representatives on health service committees: staff expectations vs. reality. Health Expect 2011;14:272–84. 10.1111/j.1369-7625.2010.00628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hwang A, Warshaw G. Joint AGS-CCEHI survey offers insights into patient engagement in geriatric clinical settings. J Am Geriatr Soc 2019;67:1791–4. 10.1111/jgs.16016 [DOI] [PubMed] [Google Scholar]
- 49. Sharma AE, Grumbach K. Engaging patients in primary care practice transformation: theory, evidence and practice. Fam Pract 2017;34:262. 10.1093/fampra/cmw128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kratchman A, Barkman D, Conaboy K, et al. The Children’s Hospital of Philadelphia Family Partners Program: promoting child and family-centered care in pediatrics. Patient Exp J 2015;2:50–60. 10.35680/2372-0247.1063 [DOI] [Google Scholar]
- 51. Pomey M-P, Hihat H, Khalifa M, et al. Patient partnership in quality improvement of healthcare services: patients’ inputs and challenges faced. Patient Exp J 2015;2:29–42. 10.35680/2372-0247.1064 [DOI] [Google Scholar]
- 52. Pougheon Bertrand D, Minguet G, Gagnayre R. Lessons from patient and parent involvement (P&PI) in a quality improvement program in cystic fibrosis care in France. Orphanet J Rare Dis 2018;13:85–102. 10.1186/s13023-017-0751-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Blignault I, Aspinall D, Reay L, et al. Realisation of a joint consumer engagement strategy in the Nepean Blue Mountains region. Aust J Prim Health 2017;23:531–5. 10.1071/PY16103 [DOI] [PubMed] [Google Scholar]
- 54. Hertel E, Cheadle A, Matthys J, et al. Engaging patients in primary care design: an evaluation of a novel approach to codesigning care. Health Expect 2019;22:609–16. 10.1111/hex.12909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lavoie-Tremblay M, O'Connor P, Biron A, et al. The experience of patients engaged in co-designing care processes. Health Care Manag 2016;35:284–93. 10.1097/HCM.0000000000000132 [DOI] [PubMed] [Google Scholar]
- 56. O’Donnell D, É Ní Shé, McCarthy M. Enabling public, patient and practitioner involvement in co-designing frailty pathways in the acute care setting. BMC Health Serv Res 2019;19:1–11. 10.1186/s12913-019-4626-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Caplan W, Davis S, Kraft S, et al. Engaging patients at the front lines of primary care redesign: operational lessons for an effective program. Jt Comm J Qual Patient Saf 2014;40:533–40. 10.1016/s1553-7250(14)40069-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Frawley T, Carroll L, Casey M, et al. Evaluation of a national training programme to support engagement in mental health services: learning enablers and learning gains. J Psychiatr Ment Health Nurs 2019;26:323–36. 10.1111/jpm.12535 [DOI] [PubMed] [Google Scholar]
- 59. Holland-Hart DM, Addis SM, Edwards A, et al. Coproduction and health: public and clinicians' perceptions of the barriers and facilitators. Health Expect 2019;22:93–101. 10.1111/hex.12834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jenkinson BM, Smethurst J, Boorman R, et al. Effect of a maternity consumer representative training program on participants' confidence and engagement. Aust Health Rev 2014;38:306–11. 10.1071/AH13183 [DOI] [PubMed] [Google Scholar]
- 61. Neech SGB, Scott H, Priest HM, et al. Experiences of user involvement in mental health settings: user motivations and benefits. J Psychiatr Ment Health Nurs 2018;25:327–37. 10.1111/jpm.12466 [DOI] [PubMed] [Google Scholar]
- 62. Renedo A, Marston CA, Spyridonidis D, et al. Patient and public involvement in healthcare quality improvement: how organizations can help patients and professionals to collaborate. Public Manag Rev 2015;17:17–34. 10.1080/14719037.2014.881535 [DOI] [Google Scholar]
- 63. Sharma AE, Willard-Grace R, Willis A, et al. "How can we talk about patient-centered care without patients at the table?" Lessons learned from patient advisory councils. J Am Board Fam Med 2016;29:775–84. 10.3122/jabfm.2016.06.150380 [DOI] [PubMed] [Google Scholar]
- 64. Shklarov S, Marshall DA, Wasylak T, et al. "Part of the team": mapping the outcomes of training patients for new roles in health research and planning. Health Expect 2017;20:1428–36. 10.1111/hex.12591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Vennik FD, van de Bovenkamp HM, Putters K, et al. Co-production in healthcare: rhetoric and practice. Int Rev Adm Sci 2016;82:150–68. 10.1177/0020852315570553 [DOI] [Google Scholar]
- 66. Boivin A, Dumez V, Fancott C, et al. Growing a healthy ecosystem for patient and citizen partnerships. Healthc Q 2018;21:73–82. 10.12927/hcq.2018.25634 [DOI] [PubMed] [Google Scholar]
- 67. Alidina S, Martelli PF, J Singer S, et al. Optimizing patient partnership in primary care improvement: a qualitative study. Health Care Manage Rev 2021;46:123–34. 10.1097/HMR.0000000000000250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Loud F, Jain N, Thomas N. How to develop a patient and carer advisory group in a quality improvement study. J Ren Care 2013;39 Suppl 2:2–9. 10.1111/j.1755-6686.2013.12032.x [DOI] [PubMed] [Google Scholar]
- 69. Maher LM, Hayward B, Hayward P, et al. Increasing sustainability in co-design projects: a qualitative evaluation of a co-design programme in New Zealand. Patient Exp J 2017;4:44–52. 10.35680/2372-0247.1150 [DOI] [Google Scholar]
- 70. Marshall C, Zambeaux A, Ainley E, et al. NHS England Always Events® program: developing a national model for co-production. Patient Exp J 2019;6:154–65. 10.35680/2372-0247.1340 [DOI] [Google Scholar]
- 71. Bak K, Moody L, Wheeler SM, et al. Patient and staff engagement in health system improvement: a qualitative evaluation of the experience-based co-design approach in Canada. Healthc Q 2018;21:24–9. 10.12927/hcq.2018.25626 [DOI] [PubMed] [Google Scholar]
- 72. McCarron TL, Moffat K, Wilkinson G, et al. Understanding patient engagement in health system decision-making: a co-designed scoping review. Syst Rev 2019;8:10. 10.1186/s13643-019-0994-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. McGhee I, Gleicher Y. Developing capacity to do improvement science work. Anesthesiol Clin 2018;36:117–26. 10.1016/j.anclin.2017.11.001 [DOI] [PubMed] [Google Scholar]
- 74. O'Connor P, Di Carlo M, Rouleau J-L. The leadership and organizational context required to support patient partnerships. Healthc Q 2018;21:31–7. 10.12927/hcq.2018.25641 [DOI] [PubMed] [Google Scholar]
- 75. Singh S, Burns KK, Rees J, et al. Patient and family engagement in Alberta Health Services: improving care delivery and research outcomes. Healthc Manage Forum 2018;31:57–61. 10.1177/0840470417747003 [DOI] [PubMed] [Google Scholar]
- 76. Majid U, Gagliardi A. Conceptual frameworks and degrees of patient engagement in the planning and designing of health services: a scoping review of qualitative studies. Patient Exp J 2019;6:82–90. 10.35680/2372-0247.1356 [DOI] [Google Scholar]
- 77. Farrington C, Burt J, Boiko O, et al. Doctors' engagements with patient experience surveys in primary and secondary care: a qualitative study. Health Expect 2017;20:385–94. 10.1111/hex.12465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. McHugh SK, Lawton R, O'Hara JK, et al. Does team reflexivity impact teamwork and communication in interprofessional hospital-based healthcare teams? A systematic review and narrative synthesis. BMJ Qual Saf 2020;29:672–83. 10.1136/bmjqs-2019-009921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Brewer M. Exploring the potential of a capability framework as a vision and "sensemaking" tool for leaders of interprofessional education. J Interprof Care 2016;30:574–81. 10.1080/13561820.2016.1182969 [DOI] [PubMed] [Google Scholar]
- 80. Thistlethwaite JE, Forman D, Matthews LR, et al. Competencies and frameworks in interprofessional education: a comparative analysis. Acad Med 2014;89:869–75. 10.1097/ACM.0000000000000249 [DOI] [PubMed] [Google Scholar]
- 81. Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. J Med Educ Curric Dev 2019;6:1–10. 10.1177/2382120519840332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. de Carvalho-Filho MA, Tio RA, Steinert Y. Twelve tips for implementing a community of practice for faculty development. Med Teach 2020;42:143–9. 10.1080/0142159X.2018.1552782 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqs-2020-012729supp001.pdf (71.4KB, pdf)
bmjqs-2020-012729supp002.pdf (257.2KB, pdf)
bmjqs-2020-012729supp003.pdf (157.4KB, pdf)
bmjqs-2020-012729supp004.pdf (79.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.