Abstract
Introduction
Cholecystectomy is a standard treatment in the management of symptomatic gallstone disease. Current literature has contradicting views on the cost-effectiveness of different cholecystectomy treatments. We have conducted a systematic reappraisal of literature concerning the cost-effectiveness of cholecystectomy in management of gallstone disease.
Methods
We systematically searched for economic evaluation studies from PubMed, Embase and Scopus for eligible studies from inception up to July 2020. We pooled the incremental net benefit (INB) with a 95% CI using a random-effects model. We assessed the heterogeneity using the Cochrane-Q test, I2 statistic. We have used the modified economic evaluation bias (ECOBIAS) checklist for quality assessment of the selected studies. We assessed the possibility of publication bias using a funnel plot and Egger’s test.
Results
We have selected 28 studies for systematic review from a search that retrieved 8710 studies. Among them, seven studies were eligible for meta-analysis, all from high-income countries (HIC). Studies mainly reported comparisons between surgical treatments, but non-surgical gallstone disease management studies were limited. The early laparoscopic cholecystectomy (ELC) was significantly more cost-effective compared with the delayed laparoscopic cholecystectomy (DLC) with an INB of US$1221 (US$187 to US$2255) but with high heterogeneity (I2=73.32%). The subgroup and sensitivity analysis also supported that ELC is the most cost-effective option for managing gallstone disease or cholecystitis.
Conclusion
ELC is more cost-effective than DLC in the treatment of gallstone disease or cholecystitis in HICs. There was insufficient literature on comparison with other treatment options, such as conservative management and limited evidence from other economies.
PROSPERO registration number
CRD42020194052.
Keywords: cost-effectiveness, cholecystectomy, economic evaluation
Introduction
Gallstones constitute one of the most common and expensive gastrointestinal disorders and cause significant epidemiological and economic burdens worldwide. Approximately 20% of people with gallstones experience symptoms requiring medical attention or surgery, while the remaining 80% remain asymptomatic for many years.1 Treatment options for cholecystitis include surgical (cholecystectomy-open and laparoscopic) or conservative management. The treatment of gallstone disease is expensive and often engenders substantial economic and social burdens if symptoms or complications occur. The healthcare system in the USA alone reported treatment costs as US$6.5 billion per year.2
The optimal timing and the treatment choice for cholecystectomy in patients with acute cholecystitis have always been contentious.3 In earlier days, several weeks of hospital stay and an initial intense medical management were the norm before an open cholecystectomy (OC).4 Introducing early cholecystectomy (open or laparoscopic) reduced the overall treatment duration considerably.3 Performing early surgery for cholecystitis has the advantage of reducing hospital stay and circumvents the risk of emergency surgery in the wake of a non-resolved or recurrent issue.4
Delayed laparoscopic cholecystectomy (DLC) and OC require multiple hospital visits considering conservative treatment, surgery and recovery period. Hence, it was associated with a higher rate of morbidity, hospital stays, pain and time to return to work.5 Early laparoscopic cholecystectomy (ELC) was associated with a lower risk of wound infection, shorter hospital stay, better cost-effectiveness, and higher patient satisfaction and quality of life.4 Studies have confirmed that ELC also reduces treatment costs significantly.6–8 However, uncertainty still prevailed around the ELC as the standard of care, conceivably due to fear of complication. The unpredictability in health outcomes and costs makes comparison of the overall cost-effectiveness of ELC over DLC debatable as well as imperative.7
Most of the reported studies on gallstone disease management were clinical or partial economic evaluations. These studies covered the costs of treatments but failed to capture the combined measure of the cost and effectiveness of both interventions and comparators in terms of the monetary cost and a generic measure of health gain.9 Concurrently, even the reported cost-effectiveness studies depict conflicting results, as some studies have reported ELC as cost-effective (CE).7 10 11 In contrast, some others12 13 concluded it was only cost saving and not CE. The lack of existing evidence and its discord on the cost-effectiveness of cholecystectomy compared with other treatment options was evident; hence, a systematic reappraisal of the literature is critical. Therefore, we systemically reviewed the economic evaluation studies of cholecystitis and cholelithiasis management. Also, we synthesised the evidence on the cost-effectiveness of the various treatment options. This systematic review and meta-analysis summarise the cost-effectiveness of an intervention (early/open-laparoscopic Cholecystectomy (LC)) compared with a comparator intervention (delayed/open- LC, conservative management). Therefore, the results could provide appropriate information to choose the most CE method.
Methods
We conducted a systematic literature search in PubMed, Scopus and Embase databases in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).14 This study is part of a more extensive economic evaluation study.15
Data sources, screening and study selection
The search was performed from inception to 1 July 2020, in PubMed, Embase and Scopus databases. We followed the Population, Intervention, Comparator, Outcome approach to construct the search terms. The desired population for the study included all the adult patients presenting with cholelithiasis or acute cholecystitis who were being considered for a cholecystectomy. Surgical removal of the gallbladder using early, open or LC was the intervention, and non-surgical methods like conservative management, wait-and-watch or endoscopic management covered the comparator strategy. The possible economic outcomes included were incremental cost-effectiveness ratio (ICER), incremental net benefit (INB), quality-adjusted life-years (QALYs) gained, life years saved and costs saved.
The detailed search terms and search strategies are reported in online supplemental material 1. The total number of studies identified from the database search was 8710, including 2977 from PubMed, 3696 from Scopus and 2037 from Embase. After removing the duplicates (n=1414), 7296 studies were selected for an initial title and abstract screening.
bmjgast-2021-000779supp001.pdf (788.9KB, pdf)
Titles and abstracts of the studies listed from the electronic database search were screened independently by the authors (BSB, MN and AS) for potential inclusion using the Rayyan software.16 After screening, the authors (BSB, MN and AS) independently reviewed the full-text articles (n=660). The final list of studies that met the inclusion and exclusion criteria was prepared by the authors’ mutual consensus (BS, MN and AS).
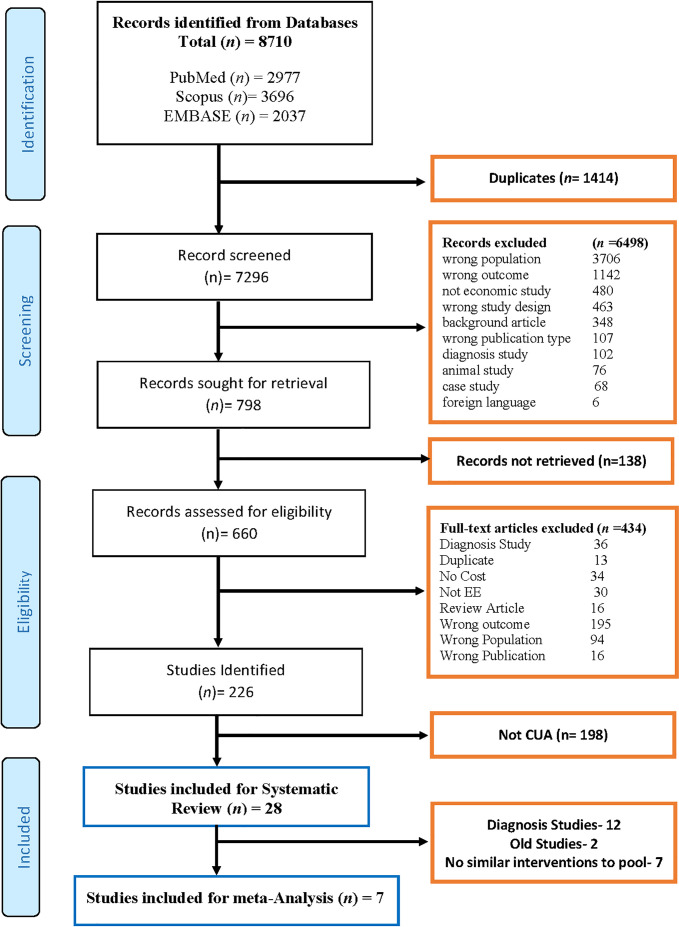
All full economic evaluation studies with a study population of cholelithiasis or cholecystitis that compared the costs and consequences of intervention with a comparator in terms of QALYs, ICERs or INBs were included in the study. Studies other than cost–utility analysis (CUA), reviews, letters, editorials, abstracts, books, reports, grey literature and methodological articles were excluded from the study. We identified 28 studies for systematic review based on these inclusion–exclusion criteria, and the data were extracted from these papers using a data extraction form. The PRISMA flow chart of the screening process is appended as figure 1.
Figure 1.
PRISMA flow chart of selection of studies. CUA, cost–utility analysis; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The data extraction form captured general study characteristics, characteristics of the studied population, economic input parameters—cost and incremental/delta costs (C and ΔC), clinical effectiveness and incremental/delta effectiveness (E and ΔE), ICERs, INB values and their measures of dispersion (ie, SD, SE or 95% CI), and willingness-to-pay (WTP) threshold (K) as well as details of intervention and comparator outcomes data for the pooling domain. From the CE plane graph, we have extracted ΔC and ΔE using WebPlotDigitizer software.17 The intervention of interest was early surgical removal (within 7 days of symptoms) of the gallbladder (OC or LC). The comparator delayed surgical removal (after 6–8 weeks) of the gallbladder (OC or LC) and included non-surgical methods like conservative management, wait-and-watch and endoscopic management. Three reviewers (BSB, AS and SKS) independently extracted the data from the finally selected 28 studies; any disagreement was resolved by consensus.
We assessed the risk of bias using the modified economic evaluation bias (ECOBIAS) checklist.18 It considers overall biases (11 items) and biases from model-specific aspects, that is, structure (4 items), data (6 items) and internal consistency (1 item). Each item was graded as yes, partly, unclear, no or not applicable (online supplemental figure 1).
The outcome of interest
The primary outcome parameter of interest was INB, defined as, INB=K*ΔE-ΔC, where K was the WTP threshold, ΔC-incremental cost (ie, the difference in costs between intervention and comparator), ΔE-incremental effectiveness (ie, the difference in effectiveness between intervention and comparator). The positive INB favours treatment, that i, the intervention was CE. In contrast, a negative INB suggests favouring the comparator, that is, the intervention was not CE. We used INB instead of ICER as the effect measure because of limitations with ICER and the ambiguity in interpreting them.19 20 In addition, since all monetary units were being reported in different currencies and at different periods (years), we converted them to purchasing power parity (PPP), adjusted to US$ for the year 2019.21
Data preparation and statistical analysis
We followed the data preparation method and analysis as detailed in Bagepally et al.22 In brief, to calculate the INB and its variance, mean values along with dispersions (SD, SE and 95% CI) of ΔC and ΔE were required. However, economic studies reported different parameters; therefore, we designed five scenarios to deal with the data available from different studies. Using the data as reported by the primary research publications and following the approach detailed in Bagepally et al, we calculated the INB and its variances for each intervention comparator duo.19
Following the data preparation, INBs were pooled across studies stratified by low-income, lower-middle-income (LMIC), upper-middle-income and high- income countries (HICs) as per the World Bank classification. A meta-analysis was applied to pool the INBs using a random-effects model if heterogeneity was present (ie, I2 ≥25% or Q, p<0.1). We did subgroup analysis wherever appropriate to explore the source of heterogeneity and provide subgroup-specific pooled INBs. Subsequently, we assessed the publication bias using funnel plots and Egger’s test. Furthermore, we explored the sources of asymmetry using contour-enhanced funnel plots. All data were prepared using Microsoft Excel version 2016 and analysed by Stata software V.16.23 Two-sided p<0.05 was considered statistically significant.
Results
We retrieved 8710 potentially relevant studies through our search. Twenty-eight studies were eligible for the systematic review, as shown in the PRISMA flow diagram (figure 1). Of the identified 28 studies, 12 were diagnostic,24–35 and the remaining 16 were therapeutic. Only 7 out of the16 therapeutic studies were included in the meta-analysis.8 11–13 36–38 The remaining nine studies were excluded because two39 40 of them were conducted before the year 2000 and had considerable variation in their cost data; and seven had no similar intervention comparator duos to pool (table 1).
Table 1.
Characteristics of studies included in the systematic review
| Author, year | Country | Setting | Study perspective | Target population | Time horizon (Year) | Discount rate (%) | Intervention | Comparator | Findings |
| Weinstein et al24 1990 | USA | Risk group | Societal | Biliary colic, non-calcified gallstones | NA | 5 | Elective Chole | Ursodiol with surgery | Not Cost effective |
| Bass et al25 1991 | USA | Others | Payers | Bile duct stones with gallstones | 5 | No | ESWL | Surgery | NA |
| Bass et al39 1993 | USA | Others | Payers | Acute/chronic biliary pain | 5 | 5 | LC | OC | Dominant |
| Cook et al40 1994 | Australia | Others | Payers | Underwent cholecystectomy | NA | No | LC, OC | LC, ESWL | LC dominant |
| Gregor et al30 1996 | Canada | Others | Third Party Payers | CBD patients | NA | 5 | ERCP | No ERCP | ERCP dominant |
| Teerawattananon et al43 2005 | Thailand | Country | Societal | Gallstone pancreatitis, bile duct stones | 3 | 3.5 | LC | OC | Not cost-effective |
| Howard et al34 2006 | Australia | NA | Health System | Post cholecystectomy patients with biliary obstruction | 1 | No | MRCP | ERCP | Dominant |
| Vergel et al32 2006 | UK | Risk group | Healthcare provider | CBD patients with biliary obstruction | 1 | No | MRCP | ERCP | Dominant |
| Poulose et al26 2007 | USA | Others | Payers | symptomatic Cholelithiasis and incidental CDL at the time of LC | 1 | No | LCBDE | ERCP | Dominant |
| Keränen et al41 2007 | Finland | Hospital | Healthcare Provider | Bile duct stone, diagnosed with cholelithiasis | 1 | No | From home to operation | Ward | Dominant |
| Macafee et al13 2009 | UK | Hospital | Societal | Acute Biliary Cholic | 1 | No | Early LC | Delayed LC | ELC cost-saving |
| Wilson et al37 2010 | UK | Country | Payers | Gallstone pancreatitis, cholecystitis | 1 | No | Emergency LC | Delayed LC | ELC dominant |
| Dageforde et al29 2012 | USA | Others | Societal | Underwent cholecystectomy | 1 | 3 | Early HBS | Late HBS, | Dominant |
| Gurusamy et al45 2012 | UK | Country | Payers | gall bladder stones with CBD stones | 3 | 3.5 | IOES | POES | Dominant |
| Johner et al38 2013 | Canada | Others | Healthcare Provider | Acute cholecystitis | 1 | No | Early LC | Delayed LC | Dominant |
| Parmar et al44 2014 | USA | NA | NA | bile duct stones/cholecholithiasis | 2 | No | CM | Elective LC | CM cost-effective |
| Morris et al12 2014 | UK | Others | UK NHS | LC for Mild, acute gallstone pancreatitis | 1 | No | Early LC | Late LC | ELC cost saving |
| Brazzelli et al7 2014 | UK | NA | UK NHS | symptomatic uncomplicated gallstone, cholecystitis | 5 | 3.5 | Surgery (LC) | CM | LC cost-effective |
| Morris et al31 2015 | UK | NA | UK NHS | CBD stone patients | 1 | No | EUS, MRCP | ERCP | MRCP cost-effective |
| Oliver et al33 2015 | USA | Others | Healthcare provider | Biliary stricture without mass | 5 | 3 | ERCP | EUS, Surgery | EUS cost-effective |
| Javid et al10 2016 | Iran | Hospital | Healthcare Provider | Undergone cholecystectomy | NA | No | LC | OC | Cost-effective |
| de Mestral et al8 2016 | Canada | Hospital | Third-party payer | Cholecystitis | 5 | 5 | Delayed LC | Early LC | ELC cost-saving |
| Sun et al35 2016 | USA | Others | NA | Intermediate bile duct stones | NA | No | IOUS, IOCP | EM | IOUS dominat |
| Sutton et al36 2016 | UK | NA | Payers | Bile duct stones with gallstones | 1 | No | Delayed LC | Early LC | ELC dominant |
| Rosenmüller et al42 2017 | Sweden | Others | Societal | Acute emergency gallstone pancreatitis bile duct stones | 1 | No | LC | SIOC | SIOC cost saving |
| Kang et al27 2017 | USA | Country | US health system | Symptomatic bile duct stones with gallstones | Lifetime | 3 | MRCP | ASGE | Cost-effective |
| Rystedt et al28 2017 | Sweden | Country | Payers | Symptomatic bile duct stones with gallstones | 10 | 3 | Routine IOCP | On demand IOCP | Not cost-effective |
| Kerwat et al11 2018 | UK | Country | Payers | Acute bile duct stones with gallstones | 2 | No | Early LC | Delayed LC | ELC cost-effective |
ASGE, American Society for Gastrointestinal Endoscopy; CBD, Common bile duct; CDL, choledocholithiasis; ELC, early laparoscopic cholecystectomy; ERCP, endoscopic retrograde cholangiopancreatography; ESWL, Extracorporeal Shock Wave Lithotripsy; HBS, Hepatobiliary surgeon; IOCP, Intra operative Cholangiography; IOUS, Intraoperative ultrasonography; LC, laparoscopic cholecystectomy; LCBDE, Laparoscopic common bile duct Exploration; MRCP, MR cholangiopancreatography; NA, not available; OC, open cholecystectomy; SIOC, Single Incision open cholecystectomy.
Based on analytical approach and design, 78.57% (N=22) studies were model- based, and the remaining 21.43% (N=6) studies were primary economic evaluations.10 13 28 40–42 The model-based techniques used in these studies were decision tree (N=19, 67.86%) and Markov model (N=3, 10.71%).7 8 39 Most studies (N=11, 39.29%) adopted the payer perspective, followed by the health system perspective (N=10, 35.71%). Four studies adopted a societal perspective,24 29 42 43 and the remaining three studies did not mention the study perspective.13 35 44
The time horizons used in these studies vary from 1 year to a lifetime. The majority of the studies used a 1-year time horizon (N=13, 46.43%), followed by 5 years (N=5, 17.86%). Two studies each used 2-year and 3-year time horizons,11 43–45 and only one study used lifetime horizons.27 Five studies failed to mention a time horizon, and three were from before the year 2000.10 24 30 35 40
All the diagnostic studies evaluating the effectiveness of endoscopic retrograde cholangiopancreatography and endoscopic ultrasound over MR cholangiopancreatography (MRCP) reported MRCP as the dominant strategy, either as CE or by providing more QALYs compared with the alternatives. The initial diagnosis with MRCP was reported as the most CE option, with the highest monetary net benefit.30–34
Among the three therapeutic studies7 8 44 that compared conservative management with surgery (LC), two studies reported that early detection and treatment of cholecystitis is cost saving and that ELC was less expensive and provided greater QALY gains compared with DLC and watchful waiting. Both these studies confirmed that DLC was the most expensive treatment and implied the need for early treatment.7 8 In contrast, the study conducted by Parmar et al reported that observation was the most CE approach.44 Similarly, three other studies comparing the cost-effectiveness of LC with OC also favoured laparoscopic surgery as it was less costly and more effective, concluding that LC dominates OC.10 39 40 Contrastingly, Teerawattananon and Mugford found that LC was not CE compared with OC.43
Risk of bias assessment
The ECOBIAS checklist shows that best current practice was chosen as a comparator for most of the studies, and all the comparators have been described in adequate detail. Studies also reported a clear presentation of the data used in the model, provided sufficient detail on the costs, applied recommended discount rates and outwardly disclosed details of funding received. Bias related to time horizon was high because most of the studies used a short-term horizon. Limited scope bias is very likely in almost all studies, and the internal consistency related to mathematical logic was unclear (see online supplemental figure 1).
Pooled INBs of early versus DLC
The INBs of ELC vs DLC varied across the seven studies,8 11–13 36–38 with high heterogeneity (I2=73.32) and a pooled INB of US$1221 (US$187 to US$2255) (figure 2). The calculated overall INB and 95% CI values of the selected studies favour the intervention; infers that ELC is CE compared with the DLC in HICs. We found that the meta-analysis results are dominated by two studies11 12 with 48% weightage each. We further conducted sensitivity analysis by omitting each of these studies one after the other, the results indicated these are source of heterogeneity but still ELC is CE; On omitting Kerwat et al, study the pooled INB US$1798 (US$1442 to US$2154, I2=0),11 while on omitting Morris et al, the pooled INB US$588 (US$232 to US$944, I2=0).12 However, on sensitivity analysis by omitting both the studies reduced the heterogeneity (US$2146 (US$−3427 to 7719), I2=0), but the statistical significance of ELC being CE is lost.
Figure 2.
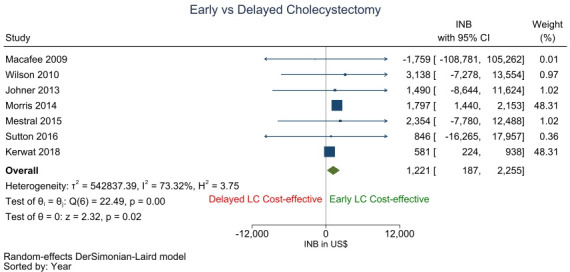
Comparision of incremental net benefit between early and delayed cholecystectomy. INB, incremental net benefit; LC, laparoscopic cholecystectomy.
Examination of the evidence of publication bias on the funnel plot shows evidence of asymmetry. Egger’s test with a p value of 0.912 also indicated a significant asymmetry. No study fell in the area of significance on contour enhanced funnel plot, making publication bias plausible (online supplemental figure 2). To distinguish between publication bias or other causes would be a challenge due to high between-study heterogeneity.
Subgroup analysis of the time horizon used for the study also indicates that ELC was significantly CE compared with DLC for 1-year and 5-year time frames. The pooled INBs of studies with 1-year and 5-year time horizon with 95% CI values was US$1797 (US$1441 to US$2154) and US$583 (US$227 to US$940), respectively (online supplemental figure 3). In addition, six out of the seven selected studies for meta-analysis were model-based studies, and the sensitivity analysis of these six studies also supports the Intervention (ELC) with a pooled INBs of US$1223 (US$161 to US$2285) (online supplemental figure 4).
The countrywise pooled INB statistic from the subgroup analysis revealed that intervention was not CE in Canada (US$1922 (−US$5244 to US$9088)), and there was no heterogeneity between these studies (I2=0). Conversely, ELC was CE in the UK with a positive pooled INB of US$1209 (US$106 to US$2311) but with substantial heterogeneity (I2=82.17%) (online supplemental figure 5). The study by Sutton, 2017 has examined cholecystectomy outcomes in both the UK and Ireland. However, to make a sufficient capacity to be pooled for INBs, we considered the country UK only in subgroup analysis.
All the selected studies followed the payer’s perspective, except Macafee et al13 which followed a societal perspective. The pooled INB values from the sensitivity analysis of all these studies, excluding the Macafee et al with a 95% CI, was US$$1221 (US$161 to US$2285) (online supplemental figure 6), depicts that ELC is CE over DLC.
Discussion
We conducted a systematic review and meta-analysis of various treatment options for gallstone diseases. On meta-analysis of CE evidence, the ELC was significantly more CE than the DLC. Subgroup analysis, as well as sensitivity analysis, strengthened the robustness of this finding. However, limited studies across different settings and lifetime horizons warrant the need for primary economic evaluation studies to fill the knowledge gap.
The subgroup analysis revealed that ELC was CE compared with DLC from the payer’s perspective. However, only one study reported non-cost effectiveness from a societal perspective, thus postulating unpredictability in the overall cost-effectiveness of the ELC with societal perspectives. Similarly, ELC was CE in studies from Canada but not from the UK; both are HICs, and this points out the high heterogeneity across available studies. Studies are limited in terms of different economies, mainly from LMICs, societal perspectives, and longer time horizons. Sensitivity analysis identified both Kerwat et al and Morris et al are the sources of heterogeneity, even though both of them had precise estimates or shorter 95% CI. Since, Kerwat et al is in scenario 5 and we used the variance from Morris et al (most similar study), hence, possibly the Morris et al study is the main source of heterogeneity. Further the study population of Morris et al study is mild acute gallstone disease with pancreatitis, which may the reason for heterogeneity, while most of the other studies were with only gallstone disease.
Many retrospectives46 47 and prospective studies48 reported ELC as the best treatment of choice for patients with acute cholecystitis. Updated Tokyo guidelines made ELC mandatory for patients with mild cholecystitis and DLC for moderate or severe cholecystitis patients.49 Overlapping meta-analysis has reported discordant results and conclusions. A systematic review of meta-analyses by Song et al suggested ELC as the standard treatment option and indicated a non-significant difference in mortality and complications, with a significant reduction in hospitalisation and improvement in quality of life when compared with DLC.50 Recent meta-analyses also suggested ELC as safe and effective against DLC for acute cholecystitis within 7 days from presentation51; also, ELC should be preferred to DLC when feasible within 72 hours of the onset of symptoms.52 In 2020, the World Society of Emergency Surgery recommended that ELC should be the standard of care whenever possible.53
Previous Randomised control trials have reported quality improvements and cost savings through same-day surgery (ELC) over preoperative admission.6 41 Model-based CUAs have reported ELC as the optimal management for uncomplicated gallstones and less expensive, with more significant QALY gains than DLC or watchful waiting.8 11 38 However, reported studies are mostly incongruous and clustered around the specific geography of HICs. Furthermore, it depends on the different study conditions and perspectives. Some studies have reported conflicting results, primarily because of different analytical perspectives or different healthcare contexts.54 Although early detection and treatment is clinically an effective strategy, synthesised economic evidence was limited. The present meta-analysis of cost-effectiveness evidence fills the knowledge gap in this regard.
The majority of the studies included in the analysis reported ELC as CE and superior to DLC, except for two studies.43 44 Full economic evaluation studies in people with gallstones or cholecystitis comparing the cost–utility effectiveness of cholecystectomy to other treatments, especially conservative management, were largely limited.
Our study has several limitations. Most of the selected studies were from HICs, either the UK or Canada, limiting results to other countries, especially the LMICs. We had only one study with a societal perspective, and studies with indirect cost would provide a real-world comparison scenario. Hence, synthesised findings have limited generalisability when extrapolating the results to all other healthcare contexts. The inadequacy of similar studies to be pooled for the INB values for intervention and comparators only permitted us to perform the meta-analysis with seven studies. Due to a lack of peer-reviewed published literature, the idea of meta-analysis with the conservative gallstone disease management was curtailed. Further, due to limited information in the primary literature, sensitivity and subgroup analysis to explore comorbidity-related costs, gender differences, patient’s age, etc could not be performed.
Future research from various economies, primarily LMICs, societal perspectives and longer time horizons are needed. Future research should be context-specific, include primary economic evaluations based on well-conducted clinical trials that provide a more accurate estimate of costs and benefits. Furthermore, timely cost-effectiveness evaluations of such interventions, will facilitate the incorporation of such health economic evidence into clinical practise. Thereby reducing barriers and overall poor uptake of economic evidence outside of health technology assessment and may positively influence the adoption and resource allocations for those interventions for greater societal benefit.
Conclusion
The synthesised results from the available studies showed ELC is a CE option compared with DLC in the treatment of gallstone disease or cholecystitis in HICs. There is a need to generate comparative economic evidence between surgical and conservative management as well as other aspects of gallstone disease management, such as endoscopic approaches and diagnostic aspects.
Footnotes
Twitter: @bshankara
Contributors: BBS: guarantor, conceptualisation, data curation, formal analysis, investigation, methodology, software, original draft, review and editing. SKS: data curation, formal analysis, original draft. AS: conceptualisation, data curation, formal analysis, original draft. MN: data curation, review and editing.
Funding: We received no specific funding for this work. However, the Dept. of Health Research, Govt. of India funds the Health Technology Assessment Resource Centre, ICMR-NIE. Grant Number: T.11011/08/2017-HR(Part-1)/E-office -8025571.
Disclaimer: Funders had no role in the conceptualisation, conduction and manuscript preparation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Brazzelli M, Cruickshank M, Kilonzo M, et al. Systematic review of the clinical and cost effectiveness of cholecystectomy versus observation/conservative management for uncomplicated symptomatic gallstones or cholecystitis. Surg Endosc 2015;29:637–47. 10.1007/s00464-014-3712-6 [DOI] [PubMed] [Google Scholar]
- 2.Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep 2005;7:132–40. 10.1007/s11894-005-0051-8 [DOI] [PubMed] [Google Scholar]
- 3.Papi C, Catarci M, D'Ambrosio L, et al. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol 2004;99:147–55. 10.1046/j.1572-0241.2003.04002.x [DOI] [PubMed] [Google Scholar]
- 4.Wu X-D, Tian X, Liu M-M, et al. Meta-Analysis comparing early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2015;102:1302–13. 10.1002/bjs.9886 [DOI] [PubMed] [Google Scholar]
- 5.Gurusamy K, Samraj K, Gluud C, et al. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2010;97:141–50. 10.1002/bjs.6870 [DOI] [PubMed] [Google Scholar]
- 6.Minutolo V, Licciardello A, Arena M, et al. Laparoscopic cholecystectomy in the treatment of acute cholecystitis: comparison of outcomes and costs between early and delayed cholecystectomy. Eur Rev Med Pharmacol Sci 2014;18:40–6. [PubMed] [Google Scholar]
- 7.Brazzelli M, Cruickshank M, Kilonzo M, et al. Clinical effectiveness and cost-effectiveness of cholecystectomy compared with observation/conservative management for preventing recurrent symptoms and complications in adults presenting with uncomplicated symptomatic gallstones or cholecystitis: a systematic review and economic evaluation. Health Technol Assess 2014;18:1–102. 10.3310/hta18550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Mestral C, Hoch JS, Laupacis A, et al. Early Cholecystectomy for Acute Cholecystitis Offers the Best Outcomes at the Least Cost: A Model-Based Cost-Utility Analysis. J Am Coll Surg 2016;222:185–94. 10.1016/j.jamcollsurg.2015.10.015 [DOI] [PubMed] [Google Scholar]
- 9.Gallagher TK, Kelly ME, Hoti E. Meta-analysis of the cost-effectiveness of early versus delayed cholecystectomy for acute cholecystitis. BJS Open 2019;3:146–52. 10.1002/bjs5.50120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Javid M, Hadian M, Rezapour A. Cost-Utility analysis of laparoscopic cholecystectomy and open cholecystectomy in Kashani Hospital, Shahr-e-Kord, Iran. Iranian Red Crescent Medical Journal 2018;20. [Google Scholar]
- 11.Kerwat Doa'a, Zargaran A, Bharamgoudar R, et al. Early laparoscopic cholecystectomy is more cost-effective than delayed laparoscopic cholecystectomy in the treatment of acute cholecystitis. Clinicoecon Outcomes Res 2018;10:119–25. 10.2147/CEOR.S149924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris S, Gurusamy KS, Patel N, et al. Cost-Effectiveness of early laparoscopic cholecystectomy for mild acute gallstone pancreatitis. Br J Surg 2014;101:828–35. 10.1002/bjs.9501 [DOI] [PubMed] [Google Scholar]
- 13.Macafee DAL, Humes DJ, Bouliotis G, et al. Prospective randomized trial using cost-utility analysis of early versus delayed laparoscopic cholecystectomy for acute gallbladder disease. Br J Surg 2009;96:1031–40. 10.1002/bjs.6685 [DOI] [PubMed] [Google Scholar]
- 14.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 15.Cost-Effective management of cholelithiasis or cholecystitis: a systematic review and meta-analysis of full economic evaluation studies. Available: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020194052
- 16.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile APP for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WebPlotDigitizer - Extract data from plots, images, and maps, 2018. Available: https://automeris.io/WebPlotDigitizer/download.html
- 18.Adarkwah CC, van Gils PF, Hiligsmann M, et al. Risk of bias in model-based economic evaluations: the ECOBIAS checklist. Expert Rev Pharmacoecon Outcomes Res 2016;16:513–23. 10.1586/14737167.2015.1103185 [DOI] [PubMed] [Google Scholar]
- 19.Bagepally BS, Gurav YK, Anothaisintawee T, et al. Cost utility of sodium-glucose cotransporter 2 inhibitors in the treatment of metformin monotherapy failed type 2 diabetes patients: a systematic review and meta-analysis. Value Health 2019;22:1458–69. 10.1016/j.jval.2019.09.2750 [DOI] [PubMed] [Google Scholar]
- 20.O’Mahony JF. The limitations of Icers in screening interventions and the relative net benefit alternative. Value in Health 2015;18. [Google Scholar]
- 21.World economic and financial surveys world economic outlook database, 2021. Available: https://www.imf.org/en/Publications/WEO/weo-database/2020/October/download-entire-database [Accessed 18 Apr 2021].
- 22.Bagepally BS, Chaikledkaew U, Gurav YK, et al. Glucagon-Like peptide 1 agonists for treatment of patients with type 2 diabetes who fail metformin monotherapy: systematic review and meta-analysis of economic evaluation studies. BMJ Open Diabetes Res Care 2020;8:e001020. 10.1136/bmjdrc-2019-001020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.StataCorp . Stata statistical software: release 14. College Station, TX: StataCorp LP, 2015. [Google Scholar]
- 24.Weinstein MC, Coley CM, Richter JM. Medical management of gallstones: a cost-effectiveness analysis. J Gen Intern Med 1990;5:277–84. 10.1007/BF02600391 [DOI] [PubMed] [Google Scholar]
- 25.Bass EB, Steinberg EP, Pitt HA, et al. Cost-Effectiveness of extracorporeal shock-wave lithotripsy versus cholecystectomy for symptomatic gallstones. Gastroenterology 1991;101:189–99. 10.1016/0016-5085(91)90477-3 [DOI] [PubMed] [Google Scholar]
- 26.Poulose BK, Speroff T, Holzman MD. Optimizing choledocholithiasis management: a cost-effectiveness analysis. Arch Surg 2007;142:43–8. 10.1001/archsurg.142.1.43 [DOI] [PubMed] [Google Scholar]
- 27.Kang SK, Hoffman D, Ferket B, et al. Risk-Stratified versus Non-Risk-stratified diagnostic testing for management of suspected acute biliary obstruction: comparative effectiveness, costs, and the role of Mr cholangiopancreatography. Radiology 2017;284:468–81. 10.1148/radiol.2017161714 [DOI] [PubMed] [Google Scholar]
- 28.Rystedt JML, Tingstedt B, Montgomery F, et al. Routine intraoperative cholangiography during cholecystectomy is a cost-effective approach when analysing the cost of iatrogenic bile duct injuries. HPB 2017;19:881–8. 10.1016/j.hpb.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 29.Dageforde LA, Landman MP, Feurer ID, et al. A cost-effectiveness analysis of early vs late reconstruction of iatrogenic bile duct injuries. J Am Coll Surg 2012;214:919–27. 10.1016/j.jamcollsurg.2012.01.054 [DOI] [PubMed] [Google Scholar]
- 30.Gregor JC, Ponich TP, Detsky AS. Should ERCP be routine after an episode of "idiopathic" pancreatitis? A cost-utility analysis. Gastrointest Endosc 1996;44:118–23. 10.1016/S0016-5107(96)70127-X [DOI] [PubMed] [Google Scholar]
- 31.Morris S, Gurusamy KS, Sheringham J, et al. Cost-effectiveness analysis of endoscopic ultrasound versus magnetic resonance cholangiopancreatography in patients with suspected common bile duct stones. PLoS One 2015;10:e0121699. 10.1371/journal.pone.0121699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vergel YB, Chilcott J, Kaltenthaler E, et al. Economic evaluation of Mr cholangiopancreatography compared to diagnostic ERCP for the investigation of biliary tree obstruction. Int J Surg 2006;4:12–19. 10.1016/j.ijsu.2006.01.007 [DOI] [PubMed] [Google Scholar]
- 33.Oliver JB, Burnett AS, Ahlawat S, et al. Cost-Effectiveness of the evaluation of a suspicious biliary stricture. J Surg Res 2015;195:52–60. 10.1016/j.jss.2014.12.037 [DOI] [PubMed] [Google Scholar]
- 34.Howard K, Lord SJ, Speer A, et al. Value of magnetic resonance cholangiopancreatography in the diagnosis of biliary abnormalities in postcholecystectomy patients: a probabilistic cost-effectiveness analysis of diagnostic strategies. Int J Technol Assess Health Care 2006;22:109–18. 10.1017/S0266462306050902 [DOI] [PubMed] [Google Scholar]
- 35.Sun SX, Kulaylat AN, Hollenbeak CS, et al. Cost-effective decisions in detecting silent common bile duct gallstones during laparoscopic cholecystectomy. Ann Surg 2016;263:1164–72. 10.1097/SLA.0000000000001348 [DOI] [PubMed] [Google Scholar]
- 36.Sutton AJ, Vohra RS, Hollyman M, et al. Cost-effectiveness of emergency versus delayed laparoscopic cholecystectomy for acute gallbladder pathology. Br J Surg 2017;104:98–107. 10.1002/bjs.10317 [DOI] [PubMed] [Google Scholar]
- 37.Wilson E, Gurusamy K, Gluud C, et al. Cost–utility and value-of-information analysis of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. British Journal of Surgery 2010;97:210–9. 10.1002/bjs.6872 [DOI] [PubMed] [Google Scholar]
- 38.Johner A, Raymakers A, Wiseman SM. Cost utility of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc 2013;27:256–62. 10.1007/s00464-012-2430-1 [DOI] [PubMed] [Google Scholar]
- 39.Bass EB, Pitt HA, Lillemoe KD. Cost-Effectiveness of laparoscopic cholecystectomy versus open cholecystectomy. Am J Surg 1993;165:466–71. 10.1016/S0002-9610(05)80942-0 [DOI] [PubMed] [Google Scholar]
- 40.Cook J, Richardson J, Street A. A cost utility analysis of treatment options for gallstone disease: methodological issues and results. Health Econ 1994;3:157–68. 10.1002/hec.4730030305 [DOI] [PubMed] [Google Scholar]
- 41.Keränen J, Soini EJO, Ryynänen O-P, et al. Economic evaluation comparing from home to operation same day admission and preoperative admission one day prior to the surgery process: a randomized, controlled trial of laparoscopic cholecystectomy. Curr Med Res Opin 2007;23:2775–84. 10.1185/030079907X233223 [DOI] [PubMed] [Google Scholar]
- 42.Rosenmüller MH, Nilsson E, Lindberg F, et al. Costs and quality of life of small-incision open cholecystectomy and laparoscopic cholecystectomy - an expertise-based randomised controlled trial. BMC Gastroenterol 2017;17:48. 10.1186/s12876-017-0601-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teerawattananon Y, Mugford M. Is it worth offering a routine laparoscopic cholecystectomy in developing countries? A Thailand case study. Cost Eff Resour Alloc 2005;3:10. 10.1186/1478-7547-3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parmar AD, Coutin MD, Vargas GM, et al. Cost-Effectiveness of elective laparoscopic cholecystectomy versus observation in older patients presenting with mild biliary disease. J Gastrointest Surg 2014;18:1616–22. 10.1007/s11605-014-2570-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gurusamy K, Wilson E, Burroughs AK, et al. Intra-operative vs pre-operative endoscopic sphincterotomy in patients with gallbladder and common bile duct stones: cost-utility and value-of-information analysis. Appl Health Econ Health Policy 2012;10:15–29. 10.2165/11594950-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 46.Serralta AS, Bueno JL, Planells MR, et al. Prospective evaluation of emergency versus delayed laparoscopic cholecystectomy for early cholecystitis. Surg Laparosc Endosc Percutan Tech 2003;13:71–5. 10.1097/00129689-200304000-00002 [DOI] [PubMed] [Google Scholar]
- 47.Pessaux P, Tuech JJ, Rouge C, et al. Laparoscopic cholecystectomy in acute cholecystitis. A prospective comparative study in patients with acute vs. chronic cholecystitis. Surg Endosc 2000;14:358–61. 10.1007/s004640020088 [DOI] [PubMed] [Google Scholar]
- 48.Skouras C, Jarral O, Deshpande R, et al. Is early laparoscopic cholecystectomy for acute cholecystitis preferable to delayed surgery?: best evidence topic (BET). Int J Surg 2012;10:250–8. 10.1016/j.ijsu.2012.04.012 [DOI] [PubMed] [Google Scholar]
- 49.Gomi H, Solomkin JS, Takada T. Tokyo guideline revision C. TG13 antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2013;20:60–70. [DOI] [PubMed] [Google Scholar]
- 50.Song G-M, Bian W, Zeng X-T, et al. Laparoscopic cholecystectomy for acute cholecystitis: early or delayed?: evidence from a systematic review of discordant meta-analyses. Medicine 2016;95:e3835. 10.1097/MD.0000000000003835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lyu Y, Cheng Y, Wang B, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: an up-to-date meta-analysis of randomized controlled trials. Surg Endosc 2018;32:4728–41. 10.1007/s00464-018-6400-0 [DOI] [PubMed] [Google Scholar]
- 52.Borzellino G, Khuri S, Pisano M, et al. Timing of early laparoscopic cholecystectomy for acute calculous cholecystitis: a meta-analysis of randomized clinical trials. World J Emerg Surg 2021;16:16. 10.1186/s13017-021-00360-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pisano M, Allievi N, Gurusamy K, et al. 2020 world Society of emergency surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg 2020;15:61. 10.1186/s13017-020-00336-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderson RE, Hunter JG. Laparoscopic cholecystectomy is less expensive than open cholecystectomy. Surg Laparosc Endosc 1991;1:82???84–4. 10.1097/00129689-199106000-00004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgast-2021-000779supp001.pdf (788.9KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.