Abstract
Objective:
The COVID-19 outbreak created numerous multidimensional stressors, to which people show different levels of vulnerability. The current paper examines whether symptoms of ADHD are associated with poorer adaptation.
Method:
After the first quarantine in Israel, 2,055 adults participated in an online survey. Participants completed scales probing adaptation indicators: financial status, adherence to preventive measures, mental health, and COVID-19 related perceptions. Background measures, including the level of symptoms of ADHD, were collected.
Results:
Adaptation indicators negatively correlated with the level of symptoms of ADHD. Financial decline explained a small portion of the link between ADHD and decreased mental health. Background risk-taking, anti-social, and pro-social behavior partially explained the link between ADHD and non-adherence to preventive measures. COVID-19 related perceptions also partially explained that link.
Conclusion:
This study suggests that people with ADHD are more vulnerable to the challenges created by the COVID-19 pandemic and therefore deserve special attention and care.
Keywords: ADHD, COVID-19, health, well-being, pandemic
The novel coronavirus 2019 (COVID-19) pandemic is a public health and global economy breakdown affecting every facet of society. At the individual level, the pandemic has created a myriad of long-term and multidimensional psychosocial stressors such as lockdown and social distancing, unemployment, as well as decreased family and social support that are important for financial security and emotion regulation (Gruber et al., 2021). As a result, harmful effects on physical and mental health and life satisfaction are likely. International organizations advocate integration of mental health and psychosocial support into the COVID-19 response (Moreno et al., 2020).
Different people will respond to the challenges of the pandemic by various behaviors and perceptions, thus demonstrating variable degree of adaptation. Vulnerable people might be at increased risk and are expected to show lower levels of adaptation. Indeed, a recent study demonstrated substantial increases in distress during the emergence of the COVID-19 crisis. Importantly, those with preexisting mental health conditions were more likely to show a rise in distress (Daly & Robinson, 2020).
Attention deficit/hyperactivity disorder (ADHD) is a neurodevelopmental condition characterized by inattention, hyperactivity, and impulsivity leading to functional impairment (American Psychiatric Association [APA], 2013). ADHD is one of the earliest reliable predictors of long-term poor health outcomes, including various psychiatric and physical disorders, smoking and substance use, risky behavior, and accidental injury (Nigg, 2013). The current paper examines whether ADHD also predicts increased vulnerability to the significant life transitions and challenges that have been recently presented by the COVID-19 pandemic.
Life transitions are common and experienced by most if not all people. Such transitions challenge people’s perceptions and beliefs, behavioral habits, and emotional well-being and demand adaptation to a new reality. For instance, the onset of a serious health condition, transition to college life or to military service, grief after a loss of a beloved person, etc., all demand adaptation of cognitive and behavioral functions.
Research has shown that adaptability, the capacity to constructively adapt to new or changing situations, relates to behavioral, cognitive, and emotional regulation (Martin et al., 2012). Therefore, individuals who are deficient in behavioral, cognitive, and emotional regulatory functions might show lower adaptability and greater vulnerability to higher stress in times of change. Indeed, ADHD that has long been linked to lower behavioral, cognitive, and emotional regulatory functions (Barkley, 1997), has also been associated with more difficulties in managing increased stress levels (Hirvikoski et al., 2011; Lackschewitz et al., 2008). The following are several instances: Faced with stressful episodes, individuals with ADHD more frequently use maladaptive coping strategies such as escape-avoidance (wishful thinking and behavioral efforts to escape or avoid the situation), confrontational (aggressive efforts to alter the situation), and unplanned problem-solving (lack of deliberate problem-focused efforts to alter the situation) (Hampel et al., 2008; Oster et al., 2020; Young, 2005). Individuals with ADHD reported greater stress in transition to college, demonstrating unhealthy coping skills and lower adaptability (Martin & Burns, 2014). In transition to military service in countries such as Korea, Singapore, and the US, individuals with ADHD experience higher emotional distress, more alcohol and caffeine use, and reduced quality of life (Cipollone et al., 2020; Noh et al., 2018). Finally, the high prevalence of ADHD among patients with post-traumatic stress disorder (PTSD) suggests that ADHD is a vulnerability factor for developing PTSD following exposure to stress (Adler et al., 2004). All these instances suggest that ADHD is a vulnerability factor for poor adaptation to life transitions and stressors.
In line with the suggestion that ADHD is a vulnerability factor to adaptation, the present study aimed to examine the links between ADHD and adaptation indicators during the COVID-19 outbreak. Specifically, the links between symptoms of ADHD and financial decline, adherence to preventive measures, psychological distress and life satisfaction, as well as to COVID-19 related perceptions, were examined. We hypothesized that a higher level of symptoms of ADHD will correlate with greater financial decline and psychological distress, and with lower life satisfaction and adherence to preventive measures.
Methods
Data from a study that detected risk factors for non-adherence to preventive measures were re-analyzed for the purpose of the current research. The methods of the study have been described extensively in the manuscript summarizing the primary findings of the study (Pollak et al., 2020). Below is a full description of all methods that were used for the current paper.
The study was approved by the ethics committee of the Seymour Fox School of Education at the Hebrew University of Jerusalem. From May 13 to 23, 2020, a sample of 2,055 online panel respondents was recruited. The respondents have been registered in the Panel4All system (https://www.panel4all.co.il) and paid for completing surveys. The sample represented both the typicality and the variety of the adult Israeli population. The average age of the sample was 39.8 ± 15.1, 55.4% of the respondents were women, 89.7% identified as Jewish, 73.7% identified as religious, 63.8% were married or in a relationship, 51.7% had higher education, 83.4% lived in cities and towns, and 87.3% were born in Israel. Concerning economic pre-outbreak position, 51.9% reported having below or much below average income, and 54.6% reported having full-time jobs.
Measures
For the current study, the main outcome variables were financial decline, low adherence to preventive measures, psychological distress, and illness-related perceptions.
Financial decline was measured by a one-item five-point question concerning the level of decrease in income since the onset of the outbreak (1 = no decrease at all, 5 = a sharp decrease). In addition, participants reported their pre-outbreak and current full/part time position on a five-point scale (0%, 25%, 50%, 75%, 100%) and a difference (current - pre-outbreak) score was computed. The difference score was further categorized into a binary variable (0 = no decrease, for a positive or null difference score, and 1 = decrease, for a negative difference score).
Low adherence to preventive measures was probed by a 13-item questionnaire. Participants rated the extent to which they adhered to each of the 13 preventive measures that were released by the Israeli Ministry of Health at the corresponding period (focusing on social distancing, personal hygiene practicing, facemask wearing). A five-point Likert scale was used: 1 = “Not at all,” 2 = “Somewhat,” 3 = “Moderately,” 4 = “Strictly,” and 5 = “Very strictly.” Individual mean response scores were calculated. In this sample, the scale had excellent internal consistency (Cronbach’s α = .91).
An adapted version of the Kessler Screening Scale for Psychological Distress (K6) was used to probe for non-specific psychological distress (Kessler et al., 2002). For the purpose of the current study, only the first part of the scale was used, in which respondents rated on a five-level Likert scale (1 = “All the time,” 5 = “None of the time”) the level of six psychiatric common symptoms during the COVID-19 crisis. The questionnaire is sensitive to high levels of mental distress (Kessler et al., 2002, 2010) and is used in the annual US National Health Interview Survey (Kessler et al., 2010). Life satisfaction was probed by two questions concerning the current level of happiness and satisfaction from life. A four-point Likert scale was used: 1 = “Not at all,” 2 = “Somewhat,” 3 = “Moderately,” 4 = “Very much.” Individual mean response scores were calculated.
COVID-19-related perception factors: Perceptions regarding the COVID-19 and the preventive measures were assessed using several five-point Likert scales: Perceived risk of COVID-19 was assessed by a nine-item self-report questionnaire that was designed for this study based on the risk perception literature (Sjoberg, 2000). For example, “How likely are you to get COVID-19?.” In this sample, the scale had good internal consistency (Cronbach’s α = .80). Perceived efficacy of the preventive measures was measured by a self-report questionnaire designed for this study. The scale consisted of five items and was composed for measuring participants’ perceived efficacy of the preventive measures. For example, “To what extent do you think that adhering to the preventive measures will reduce the chances that you or your loved ones will get COVID-19?.” In this sample, the scale had good internal consistency (Cronbach’s α = .83). Another scale composed for this study, consisted of seven items probing for the perceived costs of adherence to preventive measures, including the perceived cost on different domains of well-being (e.g., financial, social, spiritual). For example, “To what extent adhering to the preventive measures will impair your interpersonal relationships?.” In this sample, the scale had good internal consistency (Cronbach’s α = .84). Perceived norms regarding adherence to preventive measures were measured by four questions regarding the descriptive (i.e., the prevalence of non-adherence) and the injunctive (i.e., the tolerance toward non-adherence) norms of family/friends and community/workplace they are embedded in.
The independent variable, the level of symptoms of ADHD, was measured by the Hebrew version of the Adult ADHD Self-Report Scale (Kessler et al., 2005). A total score of ASRS was created by averaging the responses to all 18 items. The original scale has high internal consistency (Cronbach’s α = .88) assessing ADHD in adults. Its sensitivity is 68.4% and specificity 99.6% (Adler et al., 2006). The Hebrew version of the scale has shown good reliability (Cronbach’s α = .89) and reasonable sensitivity (62.7%), and specificity (68%) (Zohar & Konfortes, 2010).
Other background measures consisted of sociodemographic and behavioral characteristics.
Sociodemographic factors: Respondents completed a questionnaire consisting of items regarding age, gender, marital status, number of children, ethnicity, religious affiliation and level of observance, the type of education, place of living (country region, and type of community), and background migration. In addition, respondents reported their pre-outbreak level of income (much above average, above average, average, below average, much below average).
Behavioral factors: The pro-social subscale of the young adult Strengths and Difficulties Questionnaire (SDQ) (Brann et al., 2018; Goodman & Scott, 1999) was used for measuring pro-sociality. The scale’s inter-scale correlations, internal consistency, and inter-rater agreement were confirmed (Brann et al., 2018). Respondents rated the extent to which a series of six attributes described them during a 6-month reference period on a three-level response scale (0 = “not true,” 1 = “somewhat true,” or 2 = “certainly true”). In this sample, the scale had acceptable internal consistency (Cronbach’s α = .71).
A short form of the Adult Risk-Taking Inventory (ARTI) was used to measure past engagement in risky behavior. The tool was validated in previous studies (Shoham et al., 2020, 2021). The short form consisted of 14 items probing for the frequency of engagement in relatively frequent activities (e.g., sunbathing without sunscreen, smoking marijuana) with respect to their frequency during the preceding year on a rating scale, ranging from 1 = “Not at all” to 7 = “On a daily basis.” Previous work has shown that the ARTI has good reliability and validity. In this sample, the scale had acceptable internal consistency (Cronbach’s α = .75).
Past anti-social behavior was assessed using a 15-item 4-point frequency scale, ranging from 1 = “Not at all” to 4 = “More than five times,” adapted from Cho et al. (2010). In this sample, the scale had good internal consistency (Cronbach’s α = .80).
Other health-related variables were measured but were not analyzed for the current study. These include daily hours of sleep, frequency of physical activity, smoking habits, background chronic health conditions that are considered risk factors for COVID-19 (Jordan et al., 2020), whether they were confirmed COVID-19 cases, and general subjective health.
Statistical Analysis
Descriptive statistics included mean, standard deviations, medians, and ranges of the continuous variables and frequency and percentage of categorical variables. Spearman correlations were used to measure the links between the ASRS score and the different adaptation indicators. Linear regression analyses were used to covariate for demographic variables (gender, age, religiousness, marital status) and for examining the specific contributions of symptoms of ADHD clusters (inattention, hyperactivity/impulsivity) to the prediction of the continuous outcome measures. The direct and indirect effects of symptoms of ADHD on the outcome measures through financial decline, behavioral characteristics, and COVID-19-related perceptions were calculated using the multiple mediation approach and SPSS macro (PROCESS, Model 4) provided by Hayes (2017). Though collinearity testing revealed small VIF score (<3), the significance of the regression and mediation analyses’ effects was tested via a commonly performed bootstrap analysis (bias-corrected and accelerated, 5,000 samples), which allows for greater statistical power in multiple mediator analyses and does not have distributional assumptions (e.g., lack of multicollinearity). All analyses were conducted using SPSS 25.0, including an SPSS macro designed for assessing multiple mediation models (Preacher & Hayes, 2008).
Results
Descriptive Statistics
Table 1 presents the sociodemographic, clinical, and behavioral characteristics and COVID-19-related perceptions of the sample.
Table 1.
Demographic and Clinical Characteristics.
| Categorical variables | n | % | ||
|---|---|---|---|---|
| Gender | ||||
| Females | 1,128 | 55.4 | ||
| Males | 909 | 44.6 | ||
| Religiousness | ||||
| Non-religious | 1,501 | 73.7 | ||
| Religious | 535 | 26.3 | ||
| Marital status | ||||
| Not married | 740 | 36.2 | ||
| Married | 1,302 | 63.8 | ||
| Having children | ||||
| No | 582 | 31.7 | ||
| Yes | 1,253 | 68.3 | ||
| Higher education | ||||
| No | 983 | 48.3 | ||
| Yes | 1,054 | 51.7 | ||
| Pre-outbreak level of income | ||||
| Much more than average | 78 | 3.8 | ||
| More than average | 292 | 14.3 | ||
| Average | 611 | 30.0 | ||
| Less than average | 498 | 24.4 | ||
| Much less than average | 561 | 27.5 | ||
| Decrease in percent of position | ||||
| No | 1,231 | 62.8 | ||
| Yes | 729 | 37.2 | ||
| Continuous variables | Mdn | (25%–75%) | Mean | SD |
| Age | 37.0 | (27.0–52.0) | 39.81 | 15.13 |
| Decline in income (1–5 scale) | 2.00 | (1.00–4.00) | 2.49 | 1.51 |
| Adherence to preventive measures (1–5 scale) | 4.15 | (3.62–4.62) | 4.04 | 0.75 |
| Mental health measures | ||||
| Life satisfaction | 3.00 | (2.00–3.00) | 2.82 | 0.72 |
| Psychological distress (K6) | 1.83 | (1.50–2.50) | 2.07 | 0.82 |
| Behavioral and personality | ||||
| ARTI | 1.57 | (1.29–2.00) | 1.74 | 0.64 |
| Antisocial | 1.13 | (1.07–1.33) | 1.25 | 0.30 |
| Prosocial | 2.80 | (2.40–3.00) | 2.67 | 0.35 |
| COVID-19-related perception measures | ||||
| Efficacy | 4.00 | (3.40–4.50) | 3.85 | 0.85 |
| Norm | 4.00 | (3.25–4.50) | 3.78 | 0.83 |
| Cost | 2.71 | (2.14–3.43) | 2.78 | 0.92 |
| Risk | 3.00 | (2.64–3.45) | 3.03 | 0.62 |
| ADHD symptoms—mean ASRS score (1–5 scale) | ||||
| Total | 2.17 | (1.78–2.56) | 2.20 | 0.61 |
| Inattention | 2.22 | (1.78–2.67) | 2.22 | 0.67 |
| Hyperactivity | 2.11 | (1.67–2.56) | 2.17 | 0.66 |
Note. ADHD = attention deficit/hyperactive disorder; Antisocial = past anti-social behavior; ARTI = a short form of the Adult Risk-Taking Inventory; ASRS = the Hebrew version of the Adult ADHD Self-Report Scale; Cost = the perceived costs of adherence to preventive measures; Efficacy = the perceived efficacy of the preventive measures; Norm = the perceived norms regarding adherence to preventive measures; Prosocial = pro-social subscale of the young adult Strengths and Difficulties Questionnaire (SDQ); Psychological Distress (K6) = Kessler Screening Scale for Psychological Distress, Risk = perceived risk of COVID-19.
We hypothesized that a higher level of symptoms of ADHD will be associated with greater financial decline and psychological distress, and with lower life satisfaction and adherence to preventive measures. All these hypotheses were confirmed. Table 2 presents the Spearman’s correlations between the level of symptoms of ADHD and each of the adaptation indicators. Small size correlation was found between symptoms of ADHD and greater financial decline measures (r = .110–.135) and with higher perceived risk of COVID-19 (r = .101), small-to-moderate correlation with lower adherence to preventive measures (r = −.226) and with perceptions about the efficacy, cost, and norms concerning the preventive measures (−.203, .279, and −.212, respectively), and moderate and large size correlations with lower life satisfaction and higher psychological distress (−.309 and .535, respectively).
Table 2.
Spearman’s Rho Correlations between ADHD Symptoms and Outcome Variables.
| ADHD symptoms | Finance | Mental health measures | Behavioral and personality | COVID-19-related perception measures | Adherence to preventive measures | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
| ADHD symptoms | |||||||||||||||
| 1 Mean ASRS | — | ||||||||||||||
| 2 Inattention | .913** | — | |||||||||||||
| 3 Hyperactivity | .912** | .679** | — | ||||||||||||
| Finance | |||||||||||||||
| 4 Decrease in income | .135** | .127** | .120** | — | |||||||||||
| 5 Decrease in percent of position | .110** | .107** | .094** | .608** | — | ||||||||||
| Mental health measures | |||||||||||||||
| 6 Psychological Distress (K6) | .535** | .468** | .519** | .214** | .154** | — | |||||||||
| 7 Life satisfaction | −.309** | −.299** | −.274** | −.160** | −.125** | −.569** | — | ||||||||
| Behavioral and personality | |||||||||||||||
| 8 Prosocial | −.098** | −.095** | −.082** | .015 | .008 | −.102** | .201** | — | |||||||
| 9 Antisocial | .315** | .309** | .276** | −.004 | .028 | −.142** | −.118** | −.132** | — | ||||||
| 10 ARTI | .347** | .302** | .332** | .094** | .074** | −.223** | −.113** | −.066** | .477** | — | |||||
| COVID-19-related perception measures | |||||||||||||||
| 11 Risk | .101** | .084** | .108** | .073** | .010 | −.180** | −.117** | .029 | −.128** | −.100** | — | ||||
| 12 Efficacy | −.203** | −.190** | −.184** | −.039 | −.031 | .162** | .156** | .166** | −.215** | −.216** | .362** | — | |||
| 13 Cost | .279** | .245** | .269** | .289** | .240** | −.345** | −.253** | −.063** | .088** | .155** | .247** | −.099** | — | ||
| 14 Norm | −.212** | −.206** | −.188** | .002 | .001 | .185** | .119** | .194** | −.163** | −.199** | .135** | .453** | −.074** | — | |
| 15 Adherence to preventive measures | −.226** | −.227** | −.193** | .035 | .010 | .121** | .105** | .164** | −.324** | −.306** | .315** | .420** | −.067** | .347** | — |
Note. ADHD = attention deficit/hyperactive disorder; ARTI = a short form of the Adult Risk-Taking Inventory; ASRS = the Hebrew version of the Adult ADHD Self-Report Scale; Cost = the perceived costs of adherence to preventive measures; Decrease in income = decrease in income since the onset of the outbreak; Decrease in percent of position = pre-outbreak level of income; Efficacy = the perceived efficacy of the preventive measures; Norm = the perceived norms regarding adherence to preventive measures; Psychological Distress K6 = Kessler Screening Scale for Psychological Distress; Risk = perceived risk of COVID-19.
p < .01.
A set of regression analyses included all demographic variables in the first block and the intention and hyperactivity/impulsivity subscales scores of ASRS in the second block. Symptoms of ADHD remained a significant predictor of all outcome variables above and beyond the demographic variables (see Table 3). Inattention symptoms predicted decrease in income above and beyond hyperactivity symptoms, but not vice versa. Hyperactivity/impulsivity symptoms predicted increase in perceived risk and decrease in perceived efficacy above and beyond inattention symptoms, but not vice versa. Both inattention and hyperactivity predicted mental health outcome (K6 and life satisfaction scores), adherence to preventive measures, and perceived norms and costs of adherence to preventive measures above and beyond each other (see Table 3).
Table 3.
Prediction of Financial Decline, Adherence to Preventive Measures, Psychological Distress, Life Satisfaction, and COVID-19 Related Perceptions by Demographics and ADHD Symptoms.
| Predictor | Financial decline | Adherence to preventive measures | Psychological distress | Life satisfaction | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β | |
| Block 1 | .034* | .050* | .070* | .055* | ||||||||||||
| Age | −.012 | −.017 – −.006 | −.117 | .008 | .006–.011 | .171 | −.009 | −.012 - −.006 | −.173 | −.004 | −.007 - −.001 | −.082 | ||||
| Gender | .031 | −.118–.184 | .010 | .153 | .082–.224 | .103 | .176 | .101 - .254 | .110 | −.084 | −.154 - −.014 | −.059 | ||||
| Marital status | .046 | −.150–.241 | .014 | .072 | −.016–.162 | .046 | .007 | −.094 - .107 | .004 | .180 | .094 - .268 | .120 | ||||
| Having children | .092 | −.140–.320 | .029 | .031 | −.067–.129 | .020 | −.078 | −.209 - .051 | −.046 | .071 | −.029 - .171 | .047 | ||||
| Religiousness | −.156 | −.315 - −.003 | −.046 | .013 | −.063–.093 | .008 | −.140 | −.221 - −.052 | −.007 | .214 | .139 - .287 | .133 | ||||
| Higher education | −.107 | −.255–.041 | −.035 | −.002 | −.072–.070 | −.001 | .019 | −.055 - .094 | .012 | .002 | −.065 - .071 | .002 | ||||
| Income | −.157 | −.223 - −.092 | −.120 | −.031 | −.064–.000 | −.049 | −.052 | −.088 - −.016 | −.075 | .040 | .010 - .071 | −.066 | ||||
| Block 2 | .012* | .035* | .229* | .096* | ||||||||||||
| Age | −.010 | −.016 - −.005 | −.100 | .007 | .004–.010 | .141 | −.005 | −.008 - −.002 | −.093 | −.006 | −.009 - −.004 | −.132 | ||||
| Gender | .024 | −.129 -–.177 | .008 | .159 | .087–.228 | .107 | .145 | .079 - .211 | .090 | −.076 | −.144 - −.008 | −.053 | ||||
| Marital status | .055 | −.140–.248 | .017 | .063 | −.023–.150 | .041 | .032 | − .056 - .119 | .019 | .168 | .086 - .247 | .112 | ||||
| Having children | .105 | −.125–.326 | .032 | .022 | −.075–.122 | .014 | −.049 | −.158 - .052 | −.029 | .054 | −.041 - .150 | .036 | ||||
| Religiousness | −.158 | −.316 - −.006 | −.046 | .014 | −.062–.094 | .008 | −.143 | −.215 - −.067 | −.079 | .215 | .143 - .286 | .134 | ||||
| Higher education | −.114 | −.261–.031 | −.038 | .006 | −.065–.078 | .004 | .007 | −.059 - .074 | .004 | .015 | −.049 - .081 | .011 | ||||
| Income | −.151 | −.217 - −.085 | −.116 | −.037 | −.069 –−.005 | −.057 | −.041 | −.073 - −.009 | −.059 | .032 | .003 - .061 | .051 | ||||
| Inattention | .183 | .018–.349 | .079 | −.153 | −.225 - −.082 | −.136 | .205 | .127 - .283 | .168 | −.242 | −.313 - −.170 | −.224 | ||||
| Hyperactivity | .091 | −.074–.252 | .039 | −.078 | −.151 - −.004 | −.069 | .440 | .359 - .520 | .358 | −.127 | −.201 - .052 | −.117 | ||||
| Perceived risk | Perceived norms | Perceived efficacy | Perceived cost | |||||||||||||
| Predictor | ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β | ΔR 2 | B | 95% CI | β |
| Block 1 | .049* | .042* | .040* | .020* | ||||||||||||
| Age | .005 | .003–.007 | .117 | .008 | .006–.011 | .153 | .009 | .006–.012 | .154 | −.007 | −.010 - −.003 | −.107 | ||||
| Gender | .140 | .079–.199 | .112 | .128 | .053–.207 | .078 | .105 | .024–.183 | .062 | −.034 | −.122–.051 | −.018 | ||||
| Marital status | .097 | .020–.174 | .074 | .010 | −.088–.108 | .005 | .058 | −.049–.166 | .032 | −.008 | −.133–.117 | −.004 | ||||
| Having children | .013 | −.075–.105 | .010 | .011 | −.106–.131 | .006 | .020 | −.101–.149 | .011 | .003 | −.137–.150 | .002 | ||||
| Religious | −.116 | −.183 - −.051 | −.083 | −.190 | −.277 - −.105 | −.102 | −.103 | −.191 - −.011 | −.054 | −.035 | −.131–.064 | −.017 | ||||
| Higher education | −.019 | −.076–.039 | −.016 | −.106 | −.182 - −.030 | −.064 | −.128 | −.207 - −.044 | −.076 | .135 | .042–.227 | .074 | ||||
| Income | −.054 | −.081 - −.026 | .100 | .005 | −.032 -.042 | .007 | .018 | −.019–.056 | .025 | .040 | −.001–.083 | .050 | ||||
| Block 2 | .019* | .035* | .026* | .077* | ||||||||||||
| Age | .006 | .003–.008 | .140 | .007 | .004–.010 | .123 | .007 | .004–.010 | .128 | −.004 | −.007 –.000 | −.062 | ||||
| Gender | .134 | .074–.193 | .108 | .135 | .061–.213 | .082 | .114 | .035–.189 | .067 | −.053 | −.139 –.029 | −.029 | ||||
| Marital status | .103 | .027–.178 | .078 | .000 | −.096–.098 | .000 | .049 | −.054–.153 | .027 | .010 | −.107 –.131 | .005 | ||||
| Having children | .021 | −.069–.114 | .016 | −.001 | −.116–.116 | −.001 | .009 | −.112–.134 | .005 | .025 | −.108 –.168 | .013 | ||||
| Religious | −.117 | −.183 - −.054 | −.084 | .192 | .109–.277 | .103 | .105 | .014–.195 | .055 | −.039 | −.133 –.055 | −.019 | ||||
| Higher education | −.023 | −.079–.035 | −.018 | −.098 | −.173 - −.023 | −.060 | −.122 | −.201 - −.040 | −.073 | .126 | .039 –.213 | .069 | ||||
| Income | −.051 | −.079 - −.024 | −.095 | −.011 | −.047–.026 | −.015 | −.023 | −.060–.014 | −.031 | −.033 | −.074–.008 | −.041 | ||||
| Inattention | .057 | −.011–.121 | .060 | −.158 | −.247 - −.068 | −.126 | −.092 | −.189–.003 | −.072 | .142 | .050 –.237 | .101 | ||||
| Hyperactivity | .090 | .021–.156 | .094 | −.101 | −.189 - −.015 | −.080 | −.137 | −.235 - −.037 | −.106 | .287 | .192–.382 | .203 | ||||
Note. ADHD = attention deficit/hyperactive disorder; ASRS = the Hebrew version of the Adult ADHD Self-Report Scale; Cost = the perceived costs of adherence to preventive measures; Decrease in income = decrease in income since the onset of the outbreak; Efficacy = the perceived efficacy of the preventive measures; Norm = the perceived norms regarding adherence to preventive measures; Psychological Distress = Kessler Screening Scale for Psychological Distress (K6) score; Risk = perceived risk of COVID-19. Bold faced values indicate statistical significance (the respective 95% bias-corrected confidence intervals did not contain zero in bootstrap analyses).
p < .001.
Notably, some sociodemographic variables, especially the age, gender, religiousness, and pre-outbreak level of income, were also significant predictors of several adaptation indices. Older age was associated with lower financial decline, higher adherence to preventive measures, and lower psychological distress. Female gender predicted higher adherence to preventive measures and higher psychological distress; and religiousness and pre-outbreak level of income predicted lower financial decline and lower psychological distress (see Table 3).
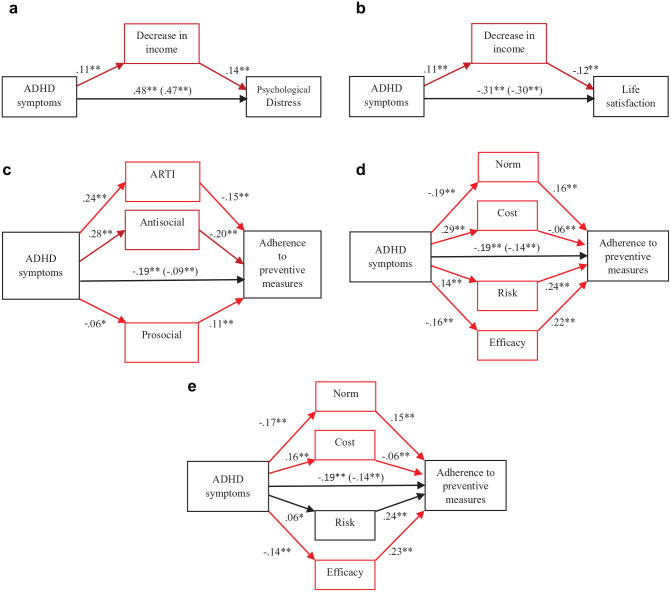
In an additional set of analyses, indirect pathways between symptoms of ADHD and different outcome variables were examined. The first two mediation models examined whether the link between symptoms of ADHD (ASRS score) and decrease in income explains the increase in psychological distress (K6 score) and decrease in life satisfaction. The first model demonstrated that the ASRS score predicted greater decrease in income and that the level of decrease in income predicted higher psychological distress (K6 scores) (see Figure 1(a) for the standardized regression coefficients). The standardized indirect pathway between symptoms of ADHD (ASRS score) and psychological distress (K6 scores) through the level of decrease in income was small but significant (see Table 4). In a similar vein, the second model revealed that the level of decrease in income predicted lower life satisfaction scores (see Figure 1(b) for the standardized regression coefficients). The standardized indirect pathway between symptoms of ADHD (ASRS score) and life satisfaction scores through the level of decrease in income was small but significant (see Table 4).
Figure 1.
(a) Path analyses predicting psychological distress (K6) score from ADHD with the covariates of age, gender, marital status, child, religious, higher education, and income, (b) path analyses predicting life satisfaction score from ADHD, (c) path analyses predicting adherence to preventive measures score from ADHD, (d) path analyses predicting adherence to preventive measures score from ADHD, and (e) path analyses predicting adherence to preventive measures score from ADHD with additional covariate of psychological distress (K6).
Note. Final mediation path analysis predicting three different variables: psychological distress, life satisfaction, and adherence to preventive measures. The values shown are the standardized regression coefficients of the indirect and direct effects (taking into account other mediators) of ADHD symptoms upon (a) psychological distress, (b) life satisfaction, and (c and d) adherence to preventive measures. The covariates of age, gender, marital status, child, religious, higher education, and income for all figures and the covariate psychological distress (K6) for Figure 1(e) are not shown in the table for the sake of brevity. ADHD = attention deficit/hyperactive disorder; ARTI = a short form of the Adult Risk-Taking Inventory; Cost = the perceived costs of adherence to preventive measures; Decrease in income = decrease in income since the onset of the outbreak; Efficacy = the perceived efficacy of the preventive measures; Norm = the perceived norms regarding adherence to preventive measures; Psychological Distress = Kessler Screening Scale for Psychological Distress (K6) score; Risk = perceived risk of COVID-19.
*p < .05. **p < .01.
Table 4.
Mediation Coefficients and Confidence Intervals (CIs).
| Dependent variable | Model R2 | Indirect effect | Direct effect | |||
|---|---|---|---|---|---|---|
| Decrease in income | ||||||
| K6 | 29.49 | 0.015 | 0.469 | |||
| 95% CI [0.007, 0.024] | 95% CI [0.428, 0.509] | |||||
| Decrease in income | ||||||
| Life satisfaction | 14.70 | −0.013 | −0.301 | |||
| 95% CI [0.06, 0.022] | 95% CI [0.257, 0.346] | |||||
| Behavioral and personality | ||||||
| ARTI | Antisocial | Prosocial | ||||
| Adherence to preventive measures | 8.33 | −0.036 | −0.057 | −0.007 | −0.088 | |
| 95% CI [−0.054, −0.021] | 95% CI [−0.075, −0.038] | 95% CI [−0.014, −0.001] | 95% CI [−0.134, −0.041] | |||
| COVID-19-related perception measures | ||||||
| Norm | Cost | Risk | Efficacy | |||
| Adherence to preventive measures | 8.33 | −0.030 | −0.017 | 0.035 | −0.037 | −0.140 |
| 95% CI [−0.045, −0.018] | 95% CI [−0.031, −0.004] | 95% CI [0.021, 0.050] | 95% CI [−0.053, −0.022] | 95% CI [−0.184, −0.096] | ||
| COVID-19-related perception measures with Psychological Distress (K6) covariated | ||||||
| Norm | Cost | Risk | Efficacy | |||
| Adherence to preventive measures | 8.19 | −0.026 | −0.010 | 0.014 | −0.031 | −0.141 |
| 95% CI [−0.085, −0.022] | 95% CI [−0.019, −0.002] | 95% CI [−0.000, 0.015] | 95% CI [−0.048, −0.015] | 95% CI [−0.189, −0.093] | ||
Note. Final mediation path analysis predicting adherence to preventive measures. The values shown are the standardized regression coefficients of the indirect and direct effects (considering other mediators) of ADHD symptoms upon adherence to preventive measures. Bold faced values indicate statistical significance (the respective 95% bias-corrected confidence intervals did not contain zero in bootstrap analyses). The covariates of age, gender, marital status, child, religious, higher education, and income are not shown in the table for the sake of brevity.
The next models examined indirect pathways between symptoms of ADHD and lower adherence to preventive measures. The third model revealed that the symptoms of ADHD (ASRS score) predicted higher risk-taking behavior and anti-social behavior scores and lower pro-social behavior scores. Risk-taking behavior and anti-social behavior scores predicted lower adherence to preventive measures, whereas pro-social behavior predicted higher adherence (see Figure 1(c) for the standardized regression coefficients). The standardized indirect pathways between the ASRS and lower adherence to preventive measures through increased risk-taking behavior and antisocial behavior and decreased pro-social behavior were significant (see Table 4).
The fourth model revealed that the ASRS score predicted increased perceived risk of the COVID-19 illness, increased perceived cost of the preventive measures, decreased perceived efficacy of the preventive measures, and decreased adherence norms. Perceived risk of the COVID-19 illness, perceived efficacy of the preventive measures, and perceived adherence norms predicted adherence to the preventive measures, whereas perceived cost of the preventive measures predicted non-adherence (see Figure 1(d) for the standardized regression coefficients). The standardized significant indirect pathways between the ASRS and lower adherence to preventive measures through increased perceived cost of the preventive measures, decreased perceived efficacy of the preventive measures, and decreased perceived adherence norms to the preventive measures were significant. However, an indirect pathway through increased perceived risk of the COVID-19 illness diminished the negative link between ADHD and adherence. Interestingly, adding psychological distress (K6 score) as a covariate to the model reduced the indirect pathway through the perceived risk (see Table 4).
Discussion
The current paper examined the link between symptoms of ADHD and adaptation to the COVID-19 pandemic indicators in several domains. It was found that higher levels of symptoms of ADHD predicted lower economic outcome, mental health indices, and adherence to preventive measures. In addition, symptoms of ADHD correlated with higher perceived risk of COVID-19 but also with perceptions that encourage non-adherence to preventive measures. These findings suggest that high symptoms of ADHD are associated with poor adaptation reflected by less optimal behavioral, emotional, and perceptual responses.
Symptoms of ADHD Predict Financial Decline
The level of symptoms of ADHD correlated with a decrease in percent of position and in income. Furthermore, this correlation explained a small but significant proportion of the variance in the link between ADHD and psychological distress. Inattention rather than hyperactivity/impulsivity symptoms predicted financial decline, in line with a study reporting that persisting high levels of ADHD inattention symptoms in adulthood predicted occupational outcome (Fredriksen et al., 2014; Gjervan et al., 2012). Interestingly, economic decline correlated with COVID-19 related perceptions, such that participants who experienced greater financial problems perceived the illness as more severe and the preventive measures as more costly and less effective.
Symptoms of ADHD Predict Lower Adherence to Preventive Measures
The level of symptoms of ADHD correlated with lower level of adherence to preventive measures, in line with a previous study (Pollak et al., 2020). Non-adherence to preventive measures reflects risk-taking behavior as it increases the likelihood of infection. Indeed, ADHD was found to be a risk factor for COVID-19 infection (Merzon et al., 2020). Also, as the preventive measures were mandatory in Israel at the time of the study, non-adherence may also be considered as anti-social behavior. Importantly, both risk-taking and anti-social behavior are closely related to ADHD (Pollak et al., 2019; Retz et al., 2021). Accordingly, the link between ADHD and non-adherence was partially explained by high levels of risk-taking and anti-social behavior.
Non-adherence to preventive measures correlated with illness-related perceptions, namely, with lower perceived severity of the illness, lower perceived efficacy of and lower perceived norms of adhering to the preventive measures, and higher perceived cost of adherence. In our sample, level of symptoms of ADHD correlated with lower perceived efficacy and norms and with higher perceived cost of adherence to the preventive measures, explaining part of the link between ADHD and non-adherence. On the other hand, levels of symptoms of ADHD also correlated with higher perceived illness severity, tempering the tendency toward non-adherence. Interestingly, the link between ADHD and perceived illness severity was fully nullified by controlling for psychological distress, suggesting a common source for ADHD-related increase in perceived illness severity and psychological distress.
Symptoms of ADHD Predict Higher Psychological Distress
Level of symptoms of ADHD also predicted higher psychological distress and lower life satisfaction. Notably, these links are not unique to the COVID-19 outbreak era (APA, 2013). Therefore, the findings may indicate that during the period of the study people with high levels of symptoms of ADHD were more likely to experience distress, but not necessarily that these people experienced more distress than they had experienced before the outbreak. Importantly, part of the link between ADHD and psychological distress was accounted for by financial decline, suggesting that at least some of the negative consequences of the pandemic aggravated pre-outbreak levels of distress of people with high levels of symptoms of ADHD.
Other Predictors of Adaptation
Several sociodemographic variables were also significant predictors of adaptation. Older age was associated with lower financial decline and higher adherence to preventive measures, as well as lower psychological distress. This profile is in line with the low rate of employment among the elderly and the recognized fact that age is a major risk factor for COVID-19 illness and mortality (Bonanad et al., 2020). Female gender predicted higher adherence to preventive measures and higher psychological distress, consistent with other studies demonstrating that women showed higher levels of stress and negative health outcomes during the COVID-19 outbreak (Szabo et al., 2020; Valiente et al., 2021) Religiousness and pre-outbreak level of income predicted lower financial decline and lower psychological distress. These findings are in line with studies reporting that gross annual income and religiosity/spirituality are predictors of better mental health during the pandemic (Lucchetti et al., 2020; Valiente et al., 2021).
Limitations
The study has limitations. ADHD was dimensionally defined and did not focus on a comparison between people who meet the DSM-5 criteria of ADHD. All measures were based on self-report and not on objective observations. The study did not examine interactions between ADHD and individual differences, such as age and gender. Financial decline was measured on the basis of only one-item question. The focus on the Israeli public and the timing of the survey in a relatively early period of the pandemic might limit the generalization of the findings to other places and times. The respondents were paid for their survey completion, which might affect their response concerning financial decline.
Clinical implications
The COVID-19 outbreak’s harmful effects on individual’s financial security and health are well recognized, and international organizations advocate for integration of mental health and psychosocial support into the COVID-19 response (Moreno et al., 2020). The current study suggests that people with elevated symptoms of inattention and/or hyperactivity-impulsivity are even more vulnerable to the challenges created by the COVID-19 pandemic and therefore deserve special attention and care. Specifically, vocational and mental counseling is important, as well as fostering a healthy lifestyle that includes optimal adherence to preventive measures.
The documented vulnerability among people with elevated symptoms of ADHD to the challenges of the COVID-19 pandemic is a matter of concern since it leads them to undesirable consequences. This study highlights the difficulty of people with elevated symptoms of ADHD to adopt a new lifestyle of preventive measures and offers new insights into this tendency. In treating people with elevated symptoms of ADHD who show adaptation problems, clinicians should attend to the ways their patients view the positive outcomes of non-adherence and the perceived low efficacy of the adherence, and not only on how they assess the potential risks of the illness. Therapeutic discourse could thus focus on the benefits attained from non-adherence, in attempt to help patients develop more adaptive decision-making skills.
Author Biographies
Yehuda Pollak is an associate professor at the Seymour Fox School of Education, the Hebrew University of Jerusalem, Jerusalem, Israel.
Rachel Shoham is a senior lecturer at the Department of Special Education, The Talpiot College, Holon, Israel.
Haym Dayan is a PhD student at the Paul Baerwald School of Social Work and Social Welfare, The Hebrew University of Jerusalem, Jerusalem, Israel.
Ortal Gabrieli-Seri is a PhD student at the Seymour Fox School of Education, the Hebrew University of Jerusalem, Jerusalem, Israel.
Itai Berger is a professor at the Paul Baerwald School of Social Work and Social Welfare, The Hebrew University of Jerusalem, Jerusalem, Israel, and the head of the Pediatric Neurology Service, Assuta Ashdod University Medical Center, Ashdod, Israel.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This research was supported by the Ministry of Science, Technology, and Space, Israel.
ORCID iDs: Yehuda Pollak  https://orcid.org/0000-0002-1293-499X
https://orcid.org/0000-0002-1293-499X
Ortal Gabrieli-Seri  https://orcid.org/0000-0002-4264-4205
https://orcid.org/0000-0002-4264-4205
Itai Berger  https://orcid.org/0000-0002-7577-4444
https://orcid.org/0000-0002-7577-4444
References
- Adler L. A., Kunz M., Chua H. C., Rotrosen J., Resnick S. G. (2004). Attention-deficit/hyperactivity disorder in adult patients with posttraumatic stress disorder (PTSD): Is ADHD a vulnerability factor? Journal of Attention Disorders, 8(1), 11–16. [DOI] [PubMed] [Google Scholar]
- Adler N. E., Boyce T., Chesney M. A., Cohen S., Folkman S., Kahn R. L., Syme S. L. (1994). Socioeconomic status and health: the challenge of the gradient. American Psychologist, 49(1), 15–24. 10.1037/0003-066X.49.1.15 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. American Psychiatric Association. [Google Scholar]
- Barkley R. A. (1997). Attention-deficit/hyperactivity disorder, self-regulation, and time: Toward a more comprehensive theory. Journal of Developmental and Behavioral Pediatrics, 18(4), 271–279. [PubMed] [Google Scholar]
- Bonanad C., García-Blas S., Tarazona-Santabalbina F., Sanchis J., Bertomeu-González V., Fácila L., Ariza A., Núñez J., Cordero A. (2020). The effect of age on mortality in patients with COVID-19: A meta-analysis with 611,583 subjects. Journal of the American Medical Directors Association, 21(7), 915–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brann P., Lethbridge M. J., Mildred H. (2018). The young adult Strengths and Difficulties Questionnaire (SDQ) in routine clinical practice. Psychiatry Research, 264, 340–345. [DOI] [PubMed] [Google Scholar]
- Cho Y. I., Martin M. J., Conger R. D., Widaman K. F. (2010). Differential item functioning on antisocial behavior scale items for adolescents and young adults from single-parent and two-parent families. Journal of Psychopathology and Behavioral Assessment, 32(2), 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipollone G., Gehrman P., Manni C., Pallucchini A., Maremmani A. G. I., Palagini L., Perugi G., Maremmani I. (2020). Exploring the role of caffeine use in adult-ADHD symptom severity of US army soldiers. Journal of Clinical Medicine, 9(11), 3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. (2020). Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research, 136, 603–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen M., Dahl A. A., Martinsen E. W., Klungsoyr O., Faraone S. V., Peleikis D. E. (2014). Childhood and persistent ADHD symptoms associated with educational failure and long-term occupational disability in adult ADHD. ADHD Attention Deficit and Hyperactivity Disorders, 6(2), 87–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjervan B., Torgersen T., Nordahl H. M., Rasmussen K. (2012). Functional impairment and occupational outcome in adults with ADHD. Journal of Attention Disorders, 16(7), 544–552. [DOI] [PubMed] [Google Scholar]
- Goodman R., Scott S. (1999). Comparing the Strengths and Difficulties Questionnaire and the child behavior checklist: Is small beautiful? Journal of Abnormal Child Psychology, 27(1), 17–24. [DOI] [PubMed] [Google Scholar]
- Gruber J., Prinstein M. J., Clark L. A., Rottenberg J., Abramowitz J. S., Albano A. M., Aldao A., Borelli J. L., Chung T., Davila J., Forbes E. E., Gee D. G., Hall G. C. N., Hallion L. S., Hinshaw S. P., Hofmann S. G., Hollon S. D., Joormann J., Kazdin A. E., . . . Weinstock L. M. (2021). Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist, 76(3), 409–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel P., Manhal S., Roos T., Desman C. (2008). Interpersonal coping among boys with ADHD. Journal of Attention Disorder, 11(4), 427–436. [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Publications. [Google Scholar]
- Hirvikoski T., Olsson E. M., Nordenstrom A., Lindholm T., Nordstrom A. L., Lajic S. (2011). Deficient cardiovascular stress reactivity predicts poor executive functions in adults with attention-deficit/hyperactivity disorder. Journal of Clinical and Experimental Neuropsychology, 33(1), 63–73. [DOI] [PubMed] [Google Scholar]
- Jordan R. E., Adab P., Cheng K. K. (2020). Covid-19: Risk factors for severe disease and death. BMJ, 368, m1198. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Adler L., Ames M., Demler O., Faraone S., Hiripi E., Howes M. J., Jin R., Secnik K., Spencer T., Ustun T. B., Walters E. E. (2005). The World Health Organization adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychological Medicine, 35(2), 245–256. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Andrews G., Colpe L. J., Hiripi E., Mroczek D. K., Normand S. L., Walters E. E, Zaslavskymonitor A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Green J. G., Gruber M. J., Sampson N. A., Bromet E., Cuitan M., Furukawa T. A., Gureje O., Hinkov H., Hu C. Y., Lara C., Lee S., Mneimneh Z., Myer L., Oakley-Browne M., Posada-Villa J., Sagar R., Viana M. C., Zaslavsky A. M. (2010). Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19 Suppl 1, 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackschewitz H., Hüther G., Kröner-Herwig B. (2008). Physiological and psychological stress responses in adults with attention-deficit/hyperactivity disorder (ADHD). Psychoneuroendocrinology, 33(5), 612–624. [DOI] [PubMed] [Google Scholar]
- Lucchetti G., Góes L. G., Amaral S. G., Ganadjian G. T., Andrade I., Almeida P. O. D. A., do Carmo V. M., Manso M. E. G. (2020). Spirituality, religiosity and the mental health consequences of social isolation during Covid-19 pandemic. International Journal of Social Psychiatry. Advance online publication. 10.1177/0020764020970996 [DOI] [PMC free article] [PubMed]
- Martin A. J., Burns E. C. (2014). Academic buoyancy, resilience, and adaptability in students with ADHD. The ADHD Report, 22, 1–9. [Google Scholar]
- Martin A. J., Nejad H., Colmar S., Liem G. A. D. (2012). Adaptability: Conceptual and empirical perspectives on responses to change, novelty and uncertainty. Australian Journal of Guidance and Counselling, 22, 58–81. [Google Scholar]
- Merzon E., Manor I., Rotem A., Schneider T., Vinker S., Golan Cohen A., Lauden A., Weizman A., Green I. (2020). ADHD as a risk factor for infection with Covid-19. Journal of Attention Disorders. Advance online publication. 10.1177/1087054720943271 [DOI] [PMC free article] [PubMed]
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., Cannon M., Correll C. U., Byrne L., Carr S., Chen E. Y. H., Gorwood P., Johnson S., Kärkkäinen H., Krystal J. H., Lee J., Lieberman J., López-Jaramillo C., Männikkö M., . . . Arango C. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry, 7(9), 813–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg J. T. (2013). Attention-deficit/hyperactivity disorder and adverse health outcomes. Clinical Psychology Review, 33(2), 215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh G. M., Lee S. M., Bahn G. H. (2018). Social function of adult men with attention-deficit/hyperactivity disorder in the context of military service. Neuropsychiatric Disease and Treatment, 14, 3349–3354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster C., Ramklint M., Meyer J., Isaksson J. (2020). How do adolescents with ADHD perceive and experience stress? An interview study. Nordic Journal of Psychiatry, 74(2), 123–130. [DOI] [PubMed] [Google Scholar]
- Pollak Y., Dayan H., Shoham R., Berger I. (2020). Predictors of non-adherence to public health instructions during the COVID-19 pandemic. Psychiatry and Clinical Neurosciences, 74(11), 602–604. [DOI] [PubMed] [Google Scholar]
- Pollak Y., Dekkers T. J., Shoham R., Huizenga H. M. (2019). Risk-taking behavior in attention deficit/hyperactivity disorder (ADHD): A review of potential underlying mechanisms and of interventions. Current Psychiatry Reports, 21(5), 33. [DOI] [PubMed] [Google Scholar]
- Pollak Y., Shoham R., Dayan H., Gabrieli Seri O., Berger I. (2020). Background and concurrent factors predicting non-adherence to public health preventive measures during the chronic phase of the COVID-19 pandemic. medRxiv. [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Retz W., Ginsberg Y., Turner D., Barra S., Retz-Junginger P., Larsson H., Asherson P. (2021). Attention-deficit/hyperactivity disorder (ADHD), antisociality and delinquent behavior over the lifespan. Neuroscience & Biobehavioral Reviews, 120, 236–248. [DOI] [PubMed] [Google Scholar]
- Shoham R., Sonuga-Barke E., Yaniv I., Pollak Y. (2020). What drives risky behavior in ADHD: Insensitivity to its risk or fascination with its potential benefits? Journal of Attention Disorders. Advance online publication. 10.1177/1087054720950820 [DOI] [PubMed]
- Shoham R., Sonuga-Barke E., Yaniv I., Pollak Y. (2021). ADHD is associated with a widespread pattern of risky behavior across activity domains. Journal of Attention Disorders, 25(7), 989–1000. [DOI] [PubMed] [Google Scholar]
- Sjoberg L. (2000). Factors in risk perception. Risk Analysis, 20(1), 1–11. [PubMed] [Google Scholar]
- Szabo A., Ábel K., Boros S. (2020). Attitudes toward COVID-19 and stress levels in Hungary: Effects of age, perceived health status, and gender. Psychological Trauma: Theory, Research, Practice, and Policy, 12(6), 572–575. [DOI] [PubMed] [Google Scholar]
- Valiente C., Contreras A., Peinado V., Trucharte A., Martínez A. P., Vázquez C. (2021). Psychological adjustment in Spain during the COVID-19 pandemic: Positive and negative mental health outcomes in the general population. The Spanish Journal of Psychology, 24, e8. [DOI] [PubMed] [Google Scholar]
- Young S. (2005). Coping strategies used by adults with ADHD. Personality and Individual Differences, 38, 809–816. [Google Scholar]
- Zohar A. H., Konfortes H. (2010). Diagnosing ADHD in Israeli adults: The psychometric properties of the adult ADHD Self Report Scale (ASRS) in Hebrew. The Israeli Journal of Psychiatry and Related Sciences, 47(4), 308–315. [PubMed] [Google Scholar]