Abstract
Cheerleading is a highly popular youth sport in the United States and has been increasingly recognized in recent years for its athleticism and competitive nature. The sport has changed dramatically since its inception. When the sport of cheerleading was first developed, its primary purpose was to entertain crowds and support other athletes. Today, cheerleaders are competitive athletes themselves. Cheerleaders, most of whom are in the pediatric age group, and their parents commonly approach orthopaedic surgeons and sports medicine physicians with questions regarding the risks associated with participation in the sport. Appropriate clinical guidance is especially important for athletes returning to the sport after an injury. However, unlike other popular sports (eg, football, basketball, and volleyball), the intricacies of cheerleading are not well-known to those outside the sport, including many health care providers. Previous studies have reported on the epidemiological patterns of injuries associated with cheerleading and how such aesthetic sports affect the body, finding that fractures and concussions are prevalent and that catastrophic injuries are more common than in most other sports. Here, we provide an evidence-based discussion of 10 pertinent topics regarding cheerleading and its risks to the musculoskeletal system. The purpose of this review is to provide a comprehensive resource for orthopaedic surgeons and sports medicine physicians who care for these athletes.
Keywords: athlete, cheerleading, concussion, injuries, injury prevention, return to sport
Cheerleading attracts approximately 4 million participants annually in the United States. 141 Despite its more than 100-year history, cheerleading has only recently been considered a sport by the public and regulatory organizations, as the athleticism required of its participants has become evident through social media and docuseries. 54,131 Cheerleading involves the performance of various complex skills that contribute to its categorization as a high-risk sport for injuries. 7
Each year, approximately 35,000 cheerleading-related injuries, most commonly involving the extremities, are treated in emergency departments across the United States. 172 Specifically, cheerleading accounts for 65% of all catastrophic injuries—defined as severe spinal, spinal cord, or cerebral injuries—occurring in female athletes. 9,102 Such catastrophic injuries present acutely, but most injuries sustained in cheerleading are chronic and related to overuse. 144 Most cheerleaders fall into the pediatric age group, and they and their parents often approach their medical teams with questions regarding the injury profile specific to cheerleading.
The purpose of this review was to synthesize the available literature and present evidence-based guidance to orthopaedic surgeons and sports medicine physicians for the treatment and counseling of cheerleaders. To improve understanding of the circumstances of injury and how to approach the cheerleader as a patient, we provide evidence-based discussion of 10 pertinent topics regarding cheerleading and its risks to the musculoskeletal system.
Understanding the Context of Cheerleading Injuries
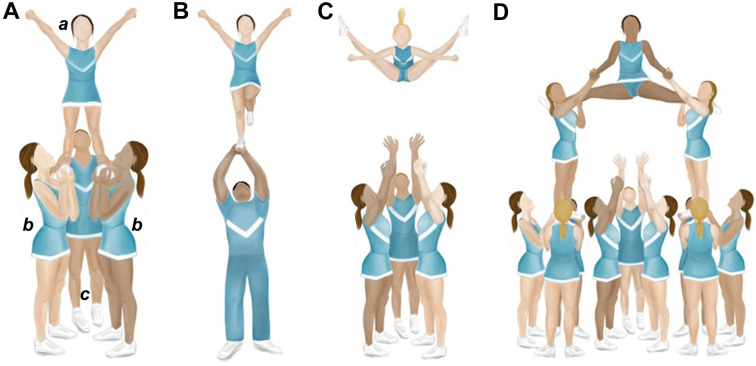
Cheerleading is uniquely defined by its combination of stunting and tumbling. A stunt is any skill in which a top person (flyer) is supported above the performance surface by 1 or more persons, commonly 2 bases and 1 backspot (Figure 1A). Stunts can be static, in which the flyer is held in one position (as in partner stunts) (Figure 1B), dynamic (as in airborne basket tosses) (Figure 1C), or both. Classically, pyramids that involve the connection of multiple stunts have both static and dynamic elements occurring in sequence (Figure 1D). Tumbling—or any hip-overhead skill not supported by a base that begins and ends on the performance surface—is an aspect shared with gymnastics. Skills vary in difficulty from cartwheels and handstands to combination passes involving the sequential performance of multiple skills. Routines also typically include coordinated dance movements and jumps (Appendix Table A1).
Figure 1.
Illustration of cheerleading stunts. (A) Prep-level group stunt demonstrating basic stunt positions: a, top person/flyer; b, bases; and c, backspot. (B) Extended, single-leg partner stunt involving 1 female flyer and 1 male base. (C) Airborne toe-touch basket toss. (D) Two-and-one-half-high pyramid.
Three main types of cheerleading exist: recreational, scholastic, and all-star. 158 Although all types involve similar skills, they differ in setting and primary focus. Recreational and scholastic (including collegiate) types of cheerleading are affiliated with community youth organizations, such as the Pop Warner Little Scholars and schools, respectively. 156 These types may be competition-based (competing against other cheerleading teams), gameday-based (supporting another athletic team, most commonly football or basketball), or a combination of both. 156,158 Meanwhile, all-star cheerleading is strictly competitive and practiced in private gymnasiums. 156
In addition to the required athleticism, several other factors inherent to cheerleading contribute to high risks for injury and reinjury. Similar to athletes of other aesthetic sports (ie, sports in which scoring depends on subjective evaluation of skill competency and presentation), cheerleaders generally reach their athletic peak in their teens, typically between ages 12 and 18 years. 47,68,80,154 Cheerleading is also unique in that opportunities to pursue the sport professionally are limited because most teams affiliated with professional sports organizations, such as the National Football League or National Basketball Association, are actually dance teams without the tumbling and stunting components of cheerleading. 31 These circumstances, along with the inability of a team to perform a coordinated routine in the absence of any single member, put cheerleaders on an accelerated timeline for skill acquisition and injury recovery. This timeline may lead to impatience regarding skill training and progression, lack of compliance with return-to-sport guidelines after injury, and initiation of the sport at a young age. Additionally, cheerleading is a year-round sport without an off-season. 167 Currently, >30 states classify competitive high school cheerleading as an official interscholastic sport, which enables consistent safety regulation, training for coaches, and access to resources 53,104 (such as athletic trainers) that reduce the risk of injury. A new form of competitive collegiate cheerleading, called STUNT, has been recently named an emerging sport by the National Collegiate Athletic Association (NCAA). 157 However, cheerleading itself is not currently sanctioned as an NCAA sport nor is it recognized by Title IX guidelines. 54,157
Sports Medicine Essentials for Cheerleaders
1. Health Benefits
The high level of athleticism demanded by cheerleading involves endurance and strength training. 3,148 This athleticism contributes to cardiovascular and muscle fitness, 148 leading to a healthier cardiovascular profile in adulthood and a lower rate of early death from chronic diseases. 16,123 Cheerleading also has positive effects on bone formation and bone strength. 111,118 Cheerleaders measure substantially higher in all bone strength outcomes, including cortical content, compared with adolescents not exposed to high-impact activities. Improving bone strength in adolescence may prevent age-related osteoporosis. 50,169 In addition, for women, the culture of a structured, female-dominated sport may reduce the risks of future substance dependence, learning and memory impairments, and unintentional injury or death. 22,92,95,97
Summary: Cheerleading involves a combination of high endurance and strength training, which contributes to benefits in cardiovascular and bone health.
2. Health Risks
The combination of high-impact activities, negative social pressures, and immature physiological characteristics of young athletes can put cheerleaders at risk for conditions that can predispose them to orthopaedic problems. Relative energy deficiency in sport (RED-S)—a syndrome resulting from low energy availability—presents more frequently in athletes participating in aesthetic sports, such as cheerleading, than in athletes participating in nonaesthetic sports. 105,147
Energy availability is a concern for all growing athletes and can be affected by disordered eating behaviors. 45 The appearance demands of cheerleading are well-recognized and embedded in the culture of the sport, with cheerleaders reporting high rates of body dissatisfaction (46%) and disordered eating (33%). †† Cheerleaders, particularly those competing at elite levels, are at higher risk of low energy availability. 93
In RED-S, the inadequacy of energy impairs physiological function, most pertinently menstrual function and bone health. 99 Up to 33% of female cheerleaders report some form of menstrual dysfunction, which can present as amenorrhea or oligomenorrhea. 147 The associated low-estrogen state in women may affect normal skeletal development by decreasing bone mineral density (BMD). 35,85,106 Eating disorders and low testosterone levels in men are similarly associated with low BMD, so cheerleaders of both sexes are susceptible. 96 Low BMD may negate the positive effects of weightbearing exercises on bone strength. 21,28,81 Building BMD is most crucial during childhood and adolescence because approximately 90% of peak bone mass is accrued before 18 years of age 2 ; therefore, any conditions that impair bone mass accrual can increase later risk for stress fractures, acute fractures, and osteoporosis. 49 Therefore, orthopaedic surgeons and sports medicine physicians should be cognizant of risk factors for low BMD and counsel patients on the importance of healthy eating habits, current bone health, and its implications for future musculoskeletal injury. 38,49 Cheerleaders who have low BMD or are at risk for developing low BMD should be referred to a sports medicine physician who understands this condition and its treatment.
Patients who present with dysmenorrhea (ie, painful menstrual cramps) should be evaluated for pelvic floor dysfunction, because cheerleaders are at risk from the performance of high-impact maneuvers. 17,23 Pelvic floor dysfunction is associated with urinary and anal incontinence, sexual dysfunction, and reduced quality of life. 94,145 Referral to a gynecologist, gastroenterologist, or specialized physical therapist may be recommended.
Summary: Cheerleaders are at risk for developing RED-S from the sport’s physical and social demands. Low BMD increases the risk of developing fractures and osteoporosis, with effects extending into adulthood.
3. Musculoskeletal Injury Patterns in Cheerleading
The incidence of cheerleading injuries is approximately 0.67 to 2.8 per 1000 athlete-exposures, with 1 athlete-exposure defined as 1 cheerleader participating in 1 cheerleading event. 128,136 Despite the low incidence of injury, mean sport participation time lost per injury is 29 days, with 78% of cheerleaders experiencing at least 1 injury during their athletic career. 1,67 Injuries occur more frequently during competition than during practice, and the most common mechanisms of injury are basing or spotting a stunt, falling, failing to complete a skill, tripping or twisting a body part, and colliding with another cheerleader. 163 Overuse injuries account for 66% of all cheerleading-related injuries treated at sports medicine clinics, 144 often presenting as a gradual onset of unspecified chronic pain. 20,33
The most common body areas injured are the ankle (22%-45%), wrist or hand (16%-21%), back (9.2%-16%), and knee (8.4%-15%). 39,66,67 The ankle is prone to sprains of the anterior talofibular or calcaneofibular ligaments and talar osteochondritis dissecans. Wrist and hand injuries often involve the interosseous ligaments, triangular fibrocartilage complex, distal radius (epiphysiolysis or gymnast’s wrist), or scaphoid (fractures). 59,62,66,67,110,128 The high frequency of ankle and wrist/hand injuries results from force overload on the joints given the weightbearing nature of tumbling and stunting. 24,39,136,162 The lower back is susceptible to muscle strains and pars interarticularis stress reactions, progressing to spondylolysis with or without spondylolisthesis, from the repetitive flexion, hyperextension, rotation, and compressive loading involved in tumbling and basing stunts. 59,87,98,121 One study 136 found that 66% of cheerleading-related recurrent injuries occurred around 1 of these 3 body areas. Knee injuries can present chronically as patellofemoral syndrome, Osgood-Schlatter disease, or patellar tendonitis or acutely as injury to the anterior or posterior cruciate ligaments (Appendix Table A2). 63,120
Overuse through large joint range of motion can result in shoulder pain or instability or hip flexor tendonitis caused by the increased muscle strength required to overcome soft tissue laxity associated with the joint hypermobility often seen in these athletes. 62,136,164 These conditions can manifest from cheerleading’s high range of motion and skill-landing strategies requiring joint control and force resistance. 46 The upper extremity weightbearing activities of cheerleading are further associated with stress fractures, with bones exposed to forces equal to as much as 12 times the cheerleader’s body weight. 81 Stress fractures most frequently occur in the upper extremity distal to the elbow. 139 Acute fractures also occur most commonly in the upper extremity, often secondary to falls on an outstretched arm. 68,90,126 Of cheerleading-related injuries treated at emergency departments nationwide, 14% to 17% were acute fractures; 62% of these fractures involved the upper extremity. 68,103,134 Other acute musculoskeletal presentations include soft tissue injuries (hematomas, contusions, crush injuries, and abrasions; 12%-22%), lacerations and avulsions (3.2%-6.0%), and acute dislocations (2.0%-2.2%). 62,68,103,128,134 The incidence of these injuries is likely higher than noted here because only approximately 28% of cheerleading injuries are treated in an emergency department. 55,128
Summary: The most commonly injured areas are the ankle, wrist, lower back, and knee. More than half of cheerleading injuries are caused by overuse, with the most common acute, noncatastrophic injuries being soft tissue sprains and strains and upper extremity fractures.
4. Catastrophic Injuries in Cheerleading
The National Center for Catastrophic Sport Injury Research defines a catastrophic injury as any severe spinal, spinal cord, or cerebral injury incurred during sports participation. A mean of 3.6 catastrophic injuries per year were reported for cheerleading between 2002 and 2017, increasing from 1.95 injuries per year between 1982 and 2002. 9,173 Although the incidence is low, cheerleading accounts for 54% of all direct catastrophic injuries to female high school athletes and 56% to female collegiate athletes. 101 These injuries most often occur in the setting of stunts, particularly pyramid and basket tosses, when flyers fall from heights and land on the floor or their bases. 5,57 More than half (52%) of catastrophic cheerleading injuries occur to the head, often resulting in cerebral edema, hematoma, or skull fracture. 9 Approximately 54% of these injuries lead to permanent disability. The next most common catastrophic injury involves the cervical spine (32%), with 29% of such injuries resulting in permanent disability. 9 These injuries include cervical fractures, severe ligament injury, or spinal cord injury. 9 Injuries to other sections of the spine and internal organs, such as the lungs and heart, are less common. 40,173 Fatal injuries are rare. 9,100,102
Summary: For cheerleading, the overall incidence of catastrophic injury is low. These injuries most commonly occur to the head and cervical spine as a result of falls from stunts.
5. Spotlight on Concussions
The incidence of concussions sustained by cheerleaders is 0.02 to 0.33 per 1000 athlete-exposures. 26,114,127 Similar to the risk of sustaining a catastrophic injury, the risk of sustaining a concussion in cheerleading has increased as the sport has evolved in difficulty and complexity. 103,134,172 This increase may also be related to greater reporting and awareness of concussions in recent years, as seen with other sports. 119 The national incidence of concussion has increased by >900% since 2000, from approximately 600 concussions that year (2.7% of all cheerleading injuries presenting to US emergency departments) to approximately 5500 concussions (18%) in 2019. 9,103,134,172 Of note, cheerleading’s concussion rate has continued to increase while the sport’s overall injury rate has decreased. 172,173
Concussions are the most common head injury in cheerleading, and 96% are secondary to stunt-related incidents. 132,133 When a stunt fails, flyers may fall from a height and hit their head on a hard surface, like a hardwood floor or concrete. Bases may similarly experience concussions if they are struck in the head by a falling flyer. 102 More concussions are reported during practices than during competitions, which may be explained by the lower regulation of practice surfaces and significantly higher proportion of time spent during practice each season. 68,103 Overall, cheerleaders are at high risk for repetitive head contact. Even subconcussive impacts are associated with lower neurocognitive functioning in adolescent athletes if they occur repeatedly. 151,153 Thus, it is essential to follow a graduated return-to-sport protocol to allow the brain to heal fully and minimize occurrence of second impact syndrome.
Summary: Cheerleading is associated with a high and increasing risk for concussion. Most concussions are sustained from head impact during stunts.
6. Risks of Starting Cheerleading at a Young Age
Participants can now begin cheerleading as young as 3 years of age, albeit at lower skill and competition levels than their older counterparts. Younger athletes (<12 years) have double the risk of moderate or severe injury, with 46% of their injuries falling into this category versus 28% for older athletes. 58 Cheerleaders younger than 12 are more susceptible to upper extremity fractures and dislocations than are their older counterparts. 76,122,134 The developmental stage of children younger than 12 years may explain their vulnerability to injury. Having not yet reached skeletal maturity, open physes are more susceptible to injury, and pediatric bone is structurally weaker and less dense than adult bone. 34,51 Increases in height and weight at this age may lead to a higher injury risk secondary to decreased proprioception and body awareness while performing demanding skills. 24 These athletes have not yet reached cognitive maturity, which is associated with decreased ability to plan movements and react to sensory stimuli. 14 Of note, the higher rates of severe injury in younger cheerleaders can be at least partially attributed to the learning curve associated with developing skills in a new athlete. Early specialization in a particular sport is further associated with higher risk for overall injury and overuse injury, a consideration for cheerleaders who hope to pursue the sport at high levels. 69,70,115
Summary: Cheerleaders younger than 12 years of age have double the risk of sustaining moderate or severe injuries, specifically upper extremity fractures, compared with older cheerleaders. In deciding at what age to introduce a child to cheerleading, parents must balance injury risk with future athletic aspirations.
7. Injury Profile of All-Star Versus Scholastic Cheerleading
The incidence of cheerleading injuries per 1000 athlete-exposures increases from 0.5 in middle school to 0.9 in high school and 2.4 in college. All-star cheerleading has an injury incidence of 0.8 per 1000 athlete-exposures. 133 Although all-star cheerleading is more competitive, collegiate athletes are 3 times as likely to sustain a concussion and 5 times as likely to experience a catastrophic injury than are other types of cheerleaders. 9,133,135 These differences may be explained by the collegiate level’s incorporation of more advanced stunts, such as flipping basket tosses and two-and-one-half-high pyramids, that are not allowed at lower scholastic levels and are used only at the highest all-star levels (Appendix Table A1). 132 Although stunts are the most common mechanism of injury for all types of cheerleading, all-star athletes are more likely to be injured via tumbling. 133,136 This greater risk may be explained by the incorporation of more complex tumbling skills attributable to the use of a spring floor, similar to a gymnastics floor, versus harder surfaces, such as a basketball court in scholastic cheerleading.
Summary: Although all-star cheerleaders are more likely to sustain injuries via tumbling compared with other types of cheerleaders, the risks of sustaining any injury and sustaining catastrophic injury are similar to those of high school cheerleaders.
8. Injury Profile of Bases Versus Flyers
Cheerleading requires every athlete to participate in stunts, tumbling, jumps, dance, and other aspects of a routine. Therefore, stunt position (base or flyer) is the main determinant of injury risk. Backspots are included as bases here. Contrary to common perceptions, bases have a higher rate of stunt-related injury (34%-46%) compared with flyers (30%-39%). 26,132,172 Injuries to bases most frequently occur to the head and neck (21%), knee (10%), and lower back (9%) as a result of improper technique in tossing, lifting, or catching. 132 Injuries to flyers most often occur to the head and neck (49%), followed by the upper extremity (20%), and result from falls. 135 Most concussions sustained by bases result from contact with another athlete, whereas most concussions sustained by flyers result from contact with the ground. 26 Because of their exposure to heights during stunts, flyers are at greater risk than bases for catastrophic injury. In fact, 70% of catastrophic injuries sustained during cheerleading occur to flyers. 173
Summary: For stunt-related injuries, flyers have a greater risk for catastrophic injury, but bases have a higher risk of injury overall.
9. Injury Profile of Cheerleading Versus Other Sports
Compared with other sports, cheerleading most closely resembles gymnastics. Both involve tumbling and substantial impact on the upper and lower extremities, leading to similar susceptibility to and patterns of injuries. 38,90,139,144 However, the added stunt component in cheerleading is associated with a higher risk for concussions and catastrophic injuries compared with gymnastics. 9,100,103,134,138
Regarding overall injury, cheerleading accounts for only 1.2% of annual sport-related injuries and ranks 18th of 22 high school sports for injury rate per 1000 athlete-exposures. 26,102 The risk of concussion was historically low, with rates similar to low-contact sports such as softball and track and field. 26,74,114,128,174 However, with increased reporting of injuries after formal recognition of cheerleading as a high school sport, recent data have indicated that cheerleading has surpassed football in concussion and catastrophic injury risk. 15,25,102,152,170 Cheerleading is associated with the highest number of direct catastrophic injuries, or those resulting directly from sports participation, for all high school and collegiate sports in which women participate. 5 Fewer data exist for male cheerleaders than for female cheerleaders or male athletes of other sports. Per proportion of overuse versus acute injuries, cheerleading ranks behind tennis, swimming, dance, running, and track and field. 144 Cheerleading presents a similar risk for lower extremity stress fractures as running and basketball, all 3 of which are higher risk than other high-impact sports. 38
Summary: Although cheerleading involves skills similar to gymnastics, the added stunt component and the involvement of multiple athletes in a routine put cheerleaders at higher risk for concussions and catastrophic injury than most other athletes.
10. Preventive Measures
Most methods to prevent injury and improve safety in cheerleading must occur at the administrative level from national cheerleading organizations and other institutions. These actions include establishing regulations for stunts and tumbling, hiring coaches with appropriate certification, ensuring facility safety, enforcing proper skill-technique training, designating cheerleading as an official sport, and providing access to appropriate medical resources. ‡‡
Athletes can take certain actions to reduce their risk of injury and reinjury. Patients should be advised on the following:
Understand the symptoms of concussion and be aware of the development, presentation, and timeline of concussions after a head injury.
Seek medical guidance after a musculoskeletal injury and perform rehabilitation exercises targeting the muscles around the joint to reduce laxity, increase stability, and avoid reinjury.
Incorporate appropriate rest and recovery into training schedules because excessive practicing increases injury from overuse, fatigue, and use of improper technique. Athletes should not practice more hours per week than their age (eg, no more than 5 hours per week for a 5-year-old cheerleader), and, if possible, they should take at least 1 month off from the sport per year. 69,70,115
Practice proper nutrition for adequate energy availability, including intake of protein, calcium, and vitamin D for bone and muscle healing.
Be patient with skill progression. Rapid progression or skipping simpler skills to compete at higher levels raises the risk of injury from poor technique.
Follow return-to-sport guidelines set by professionals after injury or surgery. Refer to Appendix Table A2 for evidence-based recommendations after common cheerleading injuries.
Obtain annual physical examinations and laboratory tests, if indicated, to screen for any predisposing factors to injury, such as low BMD.
Summary: Although the greatest improvements in cheerleading safety must be mandated from cheerleading organizations, individual athletes can take precautions in their own training to prevent injury or reinjury.
Conclusion
This review provides orthopaedic surgeons and sports medicine physicians a basic understanding of cheerleading and answers to potential patient questions regarding the sport. Although overall injury incidence is low, concussions and musculoskeletal injuries are common. Cheerleading also accounts for the highest number of catastrophic injuries to female athletes and carries an especially high risk for RED-S. Cheerleaders should be advised about the importance of appropriate training and health behaviors, as well as rehabilitation and return-to-sport guidelines after injury.
Acknowledgment
The authors thank Paul D. Sponseller, MD, MBA, for recognizing the importance of a review on cheerleading and recommending its creation. For editorial assistance, we thank Jenni Weems, MS, Kerry Kennedy, BA, and Rachel Box, MS, in the editorial services group of The Johns Hopkins Department of Orthopaedic Surgery.
APPENDIX
TABLE A1.
Definitions of Basic Cheerleading Terms a
| Term | Definition |
|---|---|
| Jump | An airborne position not involving hip-over-head rotation. |
| Stunt | Any skill in which a top person is supported above the performance surface by one or more persons. |
| Tumbling | Any hip-over-head skill that is not supported by a base that begins and ends on the performance surface. |
| Stunt Skills | |
| Basket toss | Two bases interlock wrists to form a platform. The flyer steps on this and is thrown; may or may not perform skills while suspended. |
| Dismount | The ending movement from a stunt to a cradle or the performance surface. |
| Extended stunt | When the flyer’s feet are positioned at an extended arm length over the base(s). |
| Half/prep | When the flyer’s feet are positioned at the shoulder level of the base(s). |
| Pyramid | Two or more connected stunts. |
| Two-and-one-half-high pyramid | A pyramid with multiple levels in which the flyer has weightbearing support by at least 1 other flyer and is free of contact from the base. |
| Stunt Positions | |
| Backspot | The cheerleader in direct contact with the performance surface (positioned behind the flyer, supporting their ankles/legs) who lifts, tosses, or supports the weight of another cheerleader. |
| Base | The cheerleader in direct contact with the performance surface (positioned to the sides of the flyer, supporting their feet) who lifts, tosses, or supports the weight of another cheerleader. |
| Flyer/top person | The cheerleader(s) being supported above the performance surface in a stunt, pyramid, or toss. |
| Spotter | Cheerleader whose primary responsibility is to prevent injuries by protecting the head and shoulders of a flyer during a stunt. |
| Tumbling Skills | |
| Full/double full | A single- or double-twist performed simultaneously with the layout. |
| Handspring | Performed forward or backward when a cheerleader flips by jumping from feet to hands and returning to feet, rotating through a handstand position. |
| Layout | Performed forward or backward when a cheerleader is in a straight, slightly hollow body position while rotating through the air. |
| Round-off | Similar to a cartwheel except the cheerleader lands with 2 feet placed together instead of 1 foot at a time. |
| Tuck | Performed forward or backward when a cheerleader rotates hip-over-head with knees drawn into the torso while suspended. |
| Walkover | Performed forward or backward when a cheerleader flips with legs in a split position, without losing contact with the performance surface. |
a Adapted with permission from the International Cheer Union glossary of terms. 64 Copyright 2018 International Cheer Union.
TABLE A2.
Common Cheerleading Injuries a
| Injury | Cause/Description | Treatment | Return to Sport |
|---|---|---|---|
| Head | |||
| Concussion | Although contact is not necessary, most concussions occur by head impact from contact with the ground or another athlete. Most commonly results from stunts. 132,133 | At least 24 h of rest followed by graduated 6-phase return-to-play protocol. 143,155 | 10 d to 3 wk 78,89 |
| Upper Extremity | |||
| Glenohumeral instability | Can result from forces on the shoulder during weightbearing maneuvers, 42 including basing and tumbling, which can cause glenohumeral sprains that may increase joint laxity and decrease stiffness, leading to instability. | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT. Surgery may be warranted after recurrent dislocations or first-time dislocation in young, active patients at high risk for recurrence. 161 | 3 wk 12 b to 6 mo 91 c |
| Subacromial impingement | Can result from the forces on the shoulder during weightbearing maneuvers. 4,60,113 Abnormal distribution of stress can compress the rotator cuff tendons, leading to chronic impingement syndrome with subacromial bursitis. | PT (with or without subacromial steroid injections) and NSAIDs, or surgery if unresponsive. 70%-90% of cases resolve with nonoperative treatment. 18,43 If untreated, subacromial impingement can lead to partial or complete tear of the rotator cuff. 146 | 4 wk 36 b to 6 mo 168 c |
| Distal radius epiphysiolysis (“gymnast’s wrist”) | Can result from repetitive compression loading and shearing forces on an extended wrist, such as when basing or performing handsprings or walkovers. Presents with physeal stress reactions on radiographic evaluation. 32,86 | Nonoperative treatment (rest, activity modification, and NSAIDs), period of immobilization, and then PT. Consider monitoring for growth disturbance. | 6-8 wk 72 |
| Wrist sprain or strain | Skills (eg, basing and tumbling) often require transmission of loads exceeding body weight through the wrist while dorsiflexed. Often presents with chronic, insidious pain. 32,33 | Nonoperative treatment (rest, activity modification, and NSAIDs). | Regain full ROM d |
| Back | |||
| Lower back strain | Repetitive hyperextension, flexion overload, forced rotation, and unbalanced shear forces from tumbling, jump landings, and stunts. Often presents with chronic, insidious pain. 11,44 | Nonoperative treatment (rest, activity modification, and NSAIDs) with or without lumbar bracing. 84 | Regain full ROM d |
| Pars interarticularis stress reaction (spondylolysis or spondylolisthesis) | Repetitive hyperextension, flexion overload, forced rotation, and unbalanced shear forces from tumbling, jump landings, and stunts can result in lumbar vertebral injury progressing from stress reaction to spondylolisthesis with time and continued high-impact activity. Poor technique can further contribute. 75,108 | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT with or without antilordotic bracing. Rarely requires surgical pars repair or spinal arthrodesis, 48,109 because 92% of injuries respond well to nonoperative therapy. | 4 wk 98 b to 12 mo 52 c |
| Lower Extremity | |||
| Femoroacetabular instability or impingement | Can result from repetitive training and compensatory soft tissue laxity, likely caused by strategic landings after jumps and tumbling skills. The extremes of ROM can lead to labral damage and cause intra-articular impingement (at posterior-superior acetabulum) or extra-articular impingement (between AIIS and distal femoral neck). 19,140,164 | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT. Symptomatic patients can be treated with labral repair, resection of arthroscopic cam deformity if present, and periacetabular osteotomy for symptoms associated with hip dysplasia. | 6 wk 171 b to 8 mo 41 c |
| ACL or PCL injury | Extensive training increases anterior knee laxity, leading to diminished postural stability and increased risk of ligament damage. 120 ACL injury most often occurs with twisting, valgus, and hyperextension or when landing skills are “short” or off-balance. 8,61 PCL injury can result from force applied to the lower leg while the knee is at a 90° angle, such as impact while basing. 77 | Surgical ACL reconstruction is favored for young athletes hoping to return to sport after injury. 88 PCL tears often can be treated nonoperatively. 65,112,130 | |
| Patellar tendonitis or Osgood-Schlatter disease | Repetitive high-impact movements, particularly jumping, can cause inflammation about the patellar tendon and tibial tubercle. 37,59,160 | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT with or without bracing. Rarely requires surgical excision of symptomatic, unfused ossicle after skeletal maturity. 165 | 8-12 wk 124 |
| Patellofemoral syndrome | Pressure up to 7 times the body weight can be transmitted through the knee with squatting and other high-impact positions involved in stunts, tumbling, and jumps. Presents with anterior knee pain. 10 | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT with or without bracing. 116 Surgery for select, recalcitrant cases if alignment issues are present. | 6-8 wk 56,71 |
| Talar osteochondral lesions | In addition to resulting from recurrent ankle sprains, these lesions also occur from short landings from underrotation while tumbling, in which the athlete impacts the floor with the ankle in hyperdorsiflexion. Lesions result from repetitive driving of the talus into the distal tibia. 110,159 | Nonoperative treatment (rest, activity modification, and NSAIDs) with or without CAM boot or crutches. Surgery should be considered if lesion is unstable. 59,107 | 5 wk to 6 mo 79,142 c |
| Ankle sprain or strain | Can be sustained from landing in an inverted or plantarflexed position, decreasing ability to absorb ground reaction forces on impact. Lateral ankle ligaments are most commonly affected. 29,136 | Nonoperative treatment (rest, activity modification, and NSAIDs) and PT with or without bracing. Surgery is an option for recurrent instability. | Regain full ROM, strength, and function d |
a ACL, anterior cruciate ligament; AIIS, anterior inferior iliac spine; CAM, controlled ankle movement; NSAIDs, nonsteroidal anti-inflammatory drugs; PCL, posterior cruciate ligament; PT, physical therapy; ROM, range of motion.
b Least conservative estimation of return-to-sport time with nonoperative treatment.
c Most conservative estimation of return-to-sport time with operative treatment.
d Return-to-sport time varies depending on severity of injury and specific component injured. Radiographs should be obtained to rule out fractures.
Final revision submitted September 1, 2021; accepted September 27, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.J.B. has received education payments from Arthrex and hospitality payments from Smith & Nephew. R.J.L. has received education payments from Arthrex and hospitality payments from Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Axe MJ, Newcomb WA, Warner D. Sports injuries and adolescent athletes. Del Med J. 1991;63(6):359–363. [PubMed] [Google Scholar]
- 2. Bachrach LK. Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab. 2001;12(1):22–28. [DOI] [PubMed] [Google Scholar]
- 3. Bagnulo A. Cheerleading injuries: a narrative review of the literature. J Can Chiropr Assoc. 2012;56(4):292–298. [PMC free article] [PubMed] [Google Scholar]
- 4. Bayley JC, Cochran TP, Sledge CB. The weight-bearing shoulder: the impingement syndrome in paraplegics. J Bone Joint Surg Am. 1987;69(5):676–678. [PubMed] [Google Scholar]
- 5. Boden BP. Direct catastrophic injury in sports. J Am Acad Orthop Surg. 2005;13(7):445–454. [DOI] [PubMed] [Google Scholar]
- 6. Boden BP, Jarvis CG. Spinal injuries in sports. Neurol Clin. 2008;26(1):63–78; viii. [DOI] [PubMed] [Google Scholar]
- 7. Boden BP, Prior C. Catastrophic spine injuries in sports. Curr Sports Med Rep. 2005;4(1):45–49. [DOI] [PubMed] [Google Scholar]
- 8. Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boden BP, Tacchetti R, Mueller FO. Catastrophic cheerleading injuries. Am J Sports Med. 2003;31(6):881–888. [DOI] [PubMed] [Google Scholar]
- 10. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86(2):382–396. [DOI] [PubMed] [Google Scholar]
- 12. Burns TC, Owens BD. Management of shoulder instability in in-season athletes. Phys Sportsmed. 2010;38(3):55–60. [DOI] [PubMed] [Google Scholar]
- 13. Byrne S, McLean N. Elite athletes: effects of the pressure to be thin. J Sci Med Sport. 2002;5(2):80–94. [DOI] [PubMed] [Google Scholar]
- 14. Canadian Sport Centres. Canadian Sport for Life Through Long-term Athlete Development Resource Paper V2. Accessed March 9, 2021.https://cdn3.sportngin.com/attachments/document/0108/6653/1._LTAD_2.1_EN_web.pdf
- 15. Carll KE, Park AE, Tortolani PJ. Epidemiology of catastrophic spine injuries in high school, college, and professional sports. Semin Spine Surg. 2010;22(4):168–172. [Google Scholar]
- 16. Carnethon MR, Gulati M, Greenland P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. JAMA. 2005;294(23):2981–2988. [DOI] [PubMed] [Google Scholar]
- 17. Carvalho C, da Silva Serrão PRM, Beleza ACS, Driusso P. Pelvic floor dysfunctions in female cheerleaders: a cross-sectional study. Int Urogynecol J. 2020;31(5):999–1006. [DOI] [PubMed] [Google Scholar]
- 18. Castagna A, Garofalo R, Cesari E, Markopoulos N, Borroni M, Conti M. Posterior superior internal impingement: an evidence-based review [corrected]. Br J Sports Med. 2010;44(5):382–388. [DOI] [PubMed] [Google Scholar]
- 19. Charbonnier C, Kolo FC, Duthon VB, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39(3):557–566. [DOI] [PubMed] [Google Scholar]
- 20. Chawla A, Wiesler ER. Nonspecific wrist pain in gymnasts and cheerleaders. Clin Sports Med. 2015;34(1):143–149. [DOI] [PubMed] [Google Scholar]
- 21. Christo K, Prabhakaran R, Lamparello B, et al. Bone metabolism in adolescent athletes with amenorrhea, athletes with eumenorrhea, and control subjects. Pediatrics. 2008;121(6):1127–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chun TH, Linakis JG. Interventions for adolescent alcohol use. Curr Opin Pediatr. 2012;24(2):238–242. [DOI] [PubMed] [Google Scholar]
- 23. Coco AS. Primary dysmenorrhea. Am Fam Physician. 1999;60(2):489–496. [PubMed] [Google Scholar]
- 24. Colvin AC, Lynn A. Sports-related injuries in the young female athlete. Mt Sinai J Med. 2010;77(3):307–314. [DOI] [PubMed] [Google Scholar]
- 25. Cooper MT, McGee KM, Anderson DG. Epidemiology of athletic head and neck injuries. Clin Sports Med. 2003;22(3):427–443, vii. [DOI] [PubMed] [Google Scholar]
- 26. Currie DW, Fields SK, Patterson MJ, Comstock RD. Cheerleading injuries in United States high schools. Pediatrics. 2016;137(1). [DOI] [PubMed] [Google Scholar]
- 27. Davison KK, Earnest MB, Birch LL. Participation in aesthetic sports and girls’ weight concerns at ages 5 and 7 years. Int J Eat Disord. 2002;31(3):312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. De La Torre DM, Snell BJ. Use of the preparticipation physical exam in screening for the female athlete triad among high school athletes. J Sch Nurs. 2005;21(6):340–345. [DOI] [PubMed] [Google Scholar]
- 29. Decker MJ, Torry MR, Wyland DJ, Sterett WI, Richard Steadman J. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon). 2003;18(7):662–669. [DOI] [PubMed] [Google Scholar]
- 30. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 31. Delp V. NFL/NBA Cheerleaders. Accessed March 10, 2021. https://cheerleading.lovetoknow.com
- 32. DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34(5):840–849. [DOI] [PubMed] [Google Scholar]
- 33. DiFiori JP, Puffer JC, Aish B, Dorey F. Wrist pain in young gymnasts: frequency and effects upon training over 1 year. Clin J Sport Med. 2002;12(6):348–353. [DOI] [PubMed] [Google Scholar]
- 34. Edwards T. Clinical sports medicine, 3rd edn. Br J Sports Med. 2007;41(3):183–184. [Google Scholar]
- 35. Eliakim A, Beyth Y. Exercise training, menstrual irregularities and bone development in children and adolescents. J Pediatr Adolesc Gynecol. 2003;16(4):201–206. [DOI] [PubMed] [Google Scholar]
- 36. Escamilla RF, Hooks TR, Wilk KE. Optimal management of shoulder impingement syndrome. Open Access J Sports Med. 2014;5:13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ferretti A. Epidemiology of jumper’s knee. Sports Med. 1986;3(4):289–295. [DOI] [PubMed] [Google Scholar]
- 38. Field AE, Gordon CM, Pierce LM, Ramappa A, Kocher MS. Prospective study of physical activity and risk of developing a stress fracture among preadolescent and adolescent girls. Arch Pediatr Adolesc Med. 2011;165(8):723–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Foley EC, Bird HA. “Extreme” or tariff sports: their injuries and their prevention (with particular reference to diving, cheerleading, gymnastics, and figure skating). Clin Rheumatol. 2013;32(4):463–467. [DOI] [PubMed] [Google Scholar]
- 40. Fort GG, Fort FG. Cheerleading as a cause of splenic rupture. Am J Emerg Med. 1999;17(4):432–433. [DOI] [PubMed] [Google Scholar]
- 41. Frank RM, Kunze KN, Beck EC, Neal WH, Bush-Joseph CA, Nho SJ. Do female athletes return to sports after hip preservation surgery for femoroacetabular impingement syndrome? A comparative analysis. Orthop J Sports Med. 2019;7(3):2325967119831758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Frank RM, Romeo AA, Provencher MT. Posterior glenohumeral instability: evidence-based treatment. J Am Acad Orthop Surg. 2017;25(9):610–623. [DOI] [PubMed] [Google Scholar]
- 43. Garofalo R, Conti M, Massazza G, Cesari E, Vinci E, Castagna A. Subcoracoid impingement syndrome: a painful shoulder condition related to different pathologic factors. Musculoskelet Surg. 2011;95(suppl 1):S25–S29. [DOI] [PubMed] [Google Scholar]
- 44. Garrick JG, Requa RK. Epidemiology of women’s gymnastics injuries. Am J Sports Med. 1980;8(4):261–264. [DOI] [PubMed] [Google Scholar]
- 45. Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117(2):544–559. [DOI] [PubMed] [Google Scholar]
- 46. Gittoes MJ, Irwin G, Kerwin DG. Kinematic landing strategy transference in backward rotating gymnastic dismounts. J Appl Biomech. 2013;29(3):253–260. [DOI] [PubMed] [Google Scholar]
- 47. Gladu A. Female gymnasts don’t have the luxury of aging. Accessed March 10, 2021. https://www.bustle.com/articles/172254-what-age-do-gymnasts-retire-its-a-lot-younger-than-you-might-think
- 48. Goetzinger S, Courtney S, Yee K, Welz M, Kalani M, Neal M. Spondylolysis in young athletes: an overview emphasizing nonoperative management. J Sports Med (Hindawi Publ Corp). 2020;2020:9235958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Golden NH, Abrams SA. Optimizing bone health in children and adolescents. Pediatrics. 2014;134(4):e1229–e1243. [DOI] [PubMed] [Google Scholar]
- 50. Goolsby MA, Boniquit N. Bone health in athletes. Sports Health. 2017;9(2):108–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Grady MF, Goodman A. Common lower extremity injuries in the skeletally immature athlete. Curr Probl Pediatr Adolesc Health Care. 2010;40(7):170–183. [DOI] [PubMed] [Google Scholar]
- 52. Grazina R, Andrade R, Santos FL, et al. Return to play after conservative and surgical treatment in athletes with spondylolysis: a systematic review. Phys Ther Sport. 2019;37:34–43. [DOI] [PubMed] [Google Scholar]
- 53. Green L. Impact of competitive cheer laws, regulations on Title IX compliance Accessed September 24, 2020. https://www.nfhs.org/articles/impact-of-competitive-cheer-laws-regulations-on-title-ix-compliance/
- 54. Greenspan RE. Cheer shows competitive cheerleading is almost as dangerous as football. So why isn’t it officially considered a sport? Accessed February 8, 2021. https://time.com/5782136/cheer-netflix-cheerleading-dangers/
- 55. Hage P. Cheerleading: new problems in a changing sport. Phys Sportsmed. 1981;9(2):140–145. [DOI] [PubMed] [Google Scholar]
- 56. Halabchi F, Abolhasani M, Mirshahi M, Alizadeh Z. Patellofemoral pain in athletes: clinical perspectives. Open Access J Sports Med. 2017;8:189–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hardy I, McFaull S, Saint-Vil D. Neck and spine injuries in Canadian cheerleaders: an increasing trend. J Pediatr Surg. 2015;50(5):790–792. [DOI] [PubMed] [Google Scholar]
- 58. Hardy I, McFaull SR, Beaudin M, St-Vil D, Rousseau É. Cheerleading injuries in children: what can be learned? Paediatr Child Health. 2017;22(3):130–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hart E, Meehan WP, III, Bae DS, d’Hemecourt P, Stracciolini A. The young injured gymnast: a literature review and discussion. Curr Sports Med Rep. 2018;17(11):366–375. [DOI] [PubMed] [Google Scholar]
- 60. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8(3):151–157; discussion 157-158. [DOI] [PubMed] [Google Scholar]
- 61. Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. [DOI] [PubMed] [Google Scholar]
- 62. Hutchinson MR. Cheerleading injuries: patterns, prevention, case reports. Phys Sportsmed. 1997;25(9):83–96. [DOI] [PubMed] [Google Scholar]
- 63. Hutchinson MR, Ireland ML. Knee injuries in female athletes. Sports Med. 1995;19(4):288–302. [DOI] [PubMed] [Google Scholar]
- 64. International Cheer Union. Glossary of terms. Accessed April 6, 2021.https://cheerunion.org/cheerleadingglossary/
- 65. Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace: a preliminary report. J Bone Joint Surg Br. 2010;92(10):1381–1384. [DOI] [PubMed] [Google Scholar]
- 66. Jacobson BH, Hubbard M, Redus B, et al. An assessment of high school cheerleading: injury distribution, frequency, and associated factors. J Orthop Sports Phys Ther. 2004;34(5):261–265. [DOI] [PubMed] [Google Scholar]
- 67. Jacobson BH, Redus B, Palmer T. An assessment of injuries in college cheerleading: distribution, frequency, and associated factors. Br J Sports Med. 2005;39(4):237–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jacobson NA, Morawa LG, Bir CA. Epidemiology of cheerleading injuries presenting to NEISS hospitals from 2002 to 2007. J Trauma Acute Care Surg. 2012;72(2):521–526. [DOI] [PubMed] [Google Scholar]
- 69. Jayanthi NA, LaBella CR, Fischer D, Pasulka J, Dugas LR. Sports-specialized intensive training and the risk of injury in young athletes: a clinical case-control study. Am J Sports Med. 2015;43(4):794–801. [DOI] [PubMed] [Google Scholar]
- 70. Jayanthi NA, Post EG, Laury TC, Fabricant PD. Health consequences of youth sport specialization. J Athl Train. 2019;54(10):1040–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Jones BQ, Covey CJ, Sineath MH, Jr. Nonsurgical management of knee pain in adults. Am Fam Physician. 2015;92(10):875–883. [PubMed] [Google Scholar]
- 72. Jones GL. Upper extremity stress fractures. Clin Sports Med. 2006;25(1):159–174, xi. [DOI] [PubMed] [Google Scholar]
- 73. Kaplan Y, Witvrouw E. When is it safe to return to sport after ACL reconstruction? Reviewing the criteria. Sports Health. 2019;11(4):301–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kerr ZY, Cortes N, Caswell AM, et al. Concussion rates in U.S. middle school athletes, 2015-2016 school year. Am J Prev Med. 2017;53(6):914–918. [DOI] [PubMed] [Google Scholar]
- 75. Kruse D, Lemmen B. Spine injuries in the sport of gymnastics. Curr Sports Med Rep. 2009;8(1):20–28. [DOI] [PubMed] [Google Scholar]
- 76. LaBella CR, Mjaanes J. Cheerleading injuries: epidemiology and recommendations for prevention. Pediatrics. 2012;130(5):966–971. [DOI] [PubMed] [Google Scholar]
- 77. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077–3092. [DOI] [PubMed] [Google Scholar]
- 78. Leddy JJ, Sandhu H, Sodhi V, Baker JG, Willer B. Rehabilitation of concussion and post-concussion syndrome. Sports Health. 2012;4(2):147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Letts M, Davidson D, Ahmer A. Osteochondritis dissecans of the talus in children. J Pediatr Orthop. 2003;23(5):617–625. [DOI] [PubMed] [Google Scholar]
- 80. Longo AF, Siffredi CR, Cardey ML, Aquilino GD, Lentini NA. Age of peak performance in Olympic sports: a comparative research among disciplines. J Hum Sport Exerc. 2016;11(1):31–41. [Google Scholar]
- 81. Loud KJ, Gordon CM, Micheli LJ, Field AE. Correlates of stress fractures among preadolescent and adolescent girls. Pediatrics. 2005;115(4):e399–406. [DOI] [PubMed] [Google Scholar]
- 82. Luckstead EF, Sr, Satran AL, Patel DR. Sport injury profiles, training and rehabilitation issues in American sports. Pediatr Clin North Am. 2002;49(4):753–767. [DOI] [PubMed] [Google Scholar]
- 83. Lundholm JK, Littrell JM. Desire for thinness among high school cheerleaders: relationship to disordered eating and weight control behaviors. Adolescence. 1986;21(83):573–579. [PubMed] [Google Scholar]
- 84. Malanga GA, Nadler SF. Nonoperative treatment of low back pain. Mayo Clin Proc. 1999;74(11):1135–1148. [DOI] [PubMed] [Google Scholar]
- 85. Mallinson RJ, De Souza MJ. Current perspectives on the etiology and manifestation of the “silent” component of the female athlete triad. Int J Womens Health. 2014;6:451–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mandelbaum BR, Bartolozzi AR, Davis CA, Teurlings L, Bragonier B. Wrist pain syndrome in the gymnast: pathogenetic, diagnostic, and therapeutic considerations. Am J Sports Med. 1989;17(3):305–317. [DOI] [PubMed] [Google Scholar]
- 87. Marshall SW, Covassin T, Dick R, Nassar LG, Agel J. Descriptive epidemiology of collegiate women’s gymnastics injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):234–240. [PMC free article] [PubMed] [Google Scholar]
- 88. Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. [DOI] [PubMed] [Google Scholar]
- 89. May KH, Marshall DL, Burns TG, Popoli DM, Polikandriotis JA. Pediatric sports specific return to play guidelines following concussion. Int J Sports Phys Ther. 2014;9(2):242–255. [PMC free article] [PubMed] [Google Scholar]
- 90. McCarthy MM, Bihl JH, Frank RM, Salem HS, McCarty EC, Comstock RD. Epidemiology of clavicle fractures among US high school athletes, 2008-2009 through 2016-2017. Orthop J Sports Med. 2019;7(7):2325967119861812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. McCarty EC, Ritchie P, Gill HS, McFarland EG. Shoulder instability: return to play. Clin Sports Med. 2004;23(3):335–351, vii-viii. [DOI] [PubMed] [Google Scholar]
- 92. Melnick MJ, Miller KE, Sabo DF, Farrell MP, Barnes GM. Tobacco use among high school athletes and nonathletes: results of the 1997 youth risk behavior survey. Adolescence. 2001;36(144):727–747. [PubMed] [Google Scholar]
- 93. Meng K, Qiu J, Benardot D, et al. The risk of low energy availability in Chinese elite and recreational female aesthetic sports athletes. J Int Soc Sports Nutr. 2020;17(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn. 2005;24(4):374–380. [DOI] [PubMed] [Google Scholar]
- 95. Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007;119(1):76–85. [DOI] [PubMed] [Google Scholar]
- 96. Misra M, Katzman DK, Cord J, et al. Bone metabolism in adolescent boys with anorexia nervosa. J Clin Endocrinol Metab. 2008;93(8):3029–3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Moore MJ, Werch CE. Sport and physical activity participation and substance use among adolescents. J Adolesc Health. 2005;36(6):486–493. [DOI] [PubMed] [Google Scholar]
- 98. Motley G, Nyland J, Jacobs J, Caborn DN. The pars interarticularis stress reaction, spondylolysis, and spondylolisthesis progression. J Athl Train. 1998;33(4):351–358. [PMC free article] [PubMed] [Google Scholar]
- 99. Mountjoy M, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond the female athlete triad—Relative Energy Deficiency in Sport (RED-S). Br J Sports Med. 2014;48(7):491–497. [DOI] [PubMed] [Google Scholar]
- 100. Mueller FO. Catastrophic head injuries in high school and collegiate sports. J Athl Train. 2001;36(3):312–315. [PMC free article] [PubMed] [Google Scholar]
- 101. Mueller FO. Cheerleading injuries and safety. J Athl Train. 2009;44(6):565–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Mueller FO, Kucera KL, Cox LM, Cantu RC. Catastrophic sports injury research: thirty-first annual report, fall 1982–spring 2013. Accessed April 14, 2021. https://nccsir.unc.edu/wp-content/uploads/sites/5614/2015/02/NCCSIR-31st-Annual-All-Sport-Report-1982_2013.pdf
- 103. Naiyer N, Chounthirath T, Smith GA. Pediatric cheerleading injuries treated in emergency departments in the United States. Clin Pediatr (Phila). 2017;56(11):985–992. [DOI] [PubMed] [Google Scholar]
- 104. National Federation of State High School Association. 2018-19 High school athletics participation survey. Accessed April 6, 2021. https://www.nfhs.org/media/1020412/2018-19_participation_survey.pdf
- 105. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–1882. [DOI] [PubMed] [Google Scholar]
- 106. Nichols JF, Rauh MJ, Barrack MT, Barkai HS. Bone mineral density in female high school athletes: interactions of menstrual function and type of mechanical loading. Bone. 2007;41(3):371–377. [DOI] [PubMed] [Google Scholar]
- 107. O’Farrell TA, Costello BG. Osteochondritis dissecans of the talus: the late results of surgical treatment. J Bone Joint Surg Br. 1982;64:494–497. [DOI] [PubMed] [Google Scholar]
- 108. Omey ML, Micheli LJ, Gerbino PG, II. Idiopathic scoliosis and spondylolysis in the female athlete: tips for treatment. Clin Orthop Relat Res. 2000;372:74–84. [DOI] [PubMed] [Google Scholar]
- 109. Overley SC, McAnany SJ, Andelman S, et al. Return to play in adolescent athletes with symptomatic spondylolysis without listhesis: a meta-analysis. Global Spine J. 2018;8(2):190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Overlin AJ, Chima B, Erickson S. Update on artistic gymnastics. Curr Sports Med Rep. 2011;10(5):304–309. [DOI] [PubMed] [Google Scholar]
- 111. Pashkova A, Hartman JM, Letuchy EM, Janz KF. Interscholastic athletics and bone strength: the Iowa Bone Development Study. J Strength Cond Res. Published online May 25, 2020. doi:10.1519/JSC.0000000000003646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3(2):137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Patel RM, Gelber JD, Schickendantz MS. The weight-bearing shoulder. J Am Acad Orthop Surg. 2018;26(1):3–13. [DOI] [PubMed] [Google Scholar]
- 114. Pfister T, Pfister K, Hagel B, Ghali WA, Ronksley PE. The incidence of concussion in youth sports: a systematic review and meta-analysis. Br J Sports Med. 2016;50(5):292–297. [DOI] [PubMed] [Google Scholar]
- 115. Post EG, Trigsted SM, Riekena JW, et al. The association of sport specialization and training volume with injury history in youth athletes. Am J Sports Med. 2017;45(6):1405–1412. [DOI] [PubMed] [Google Scholar]
- 116. Post WR. Patellofemoral pain: results of nonoperative treatment. Clin Orthop Relat Res. 2005;436:55–59. [PubMed] [Google Scholar]
- 117. Reel JJ, Gill DL. Psychosocial factors related to eating disorders among high school and college female cheerleaders. Sport Psychol. 1996;10(2):195–206. [Google Scholar]
- 118. Roberts D. Bone adaptations in male collegiate-level cheerleaders. Accessed March 10, 2021. https://soar.wichita.edu/bitstream/handle/10057/6838/t13040_Roberts.pdf?isAllowed=y&%20sequence=1
- 119. Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005-2006 to 2011-2012. Am J Sports Med. 2014;42(7):1710–1715. [DOI] [PubMed] [Google Scholar]
- 120. Rowe A, Wright S, Nyland J, Caborn DN, Kling R. Effects of a 2-hour cheerleading practice on dynamic postural stability, knee laxity, and hamstring extensibility. J Orthop Sports Phys Ther. 1999;29(8):455–462. [DOI] [PubMed] [Google Scholar]
- 121. Ruff AN, Cornelson SM, Wells CB, Kettner NW. Neural arch bone marrow edema and spondylolysis in adolescent cheerleaders: a case series. J Chiropr Med. 2019;18(4):335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Rui P, Ashman JJ, Akinseye A. Emergency department visits for injuries sustained during sports and recreational activities by patients aged 5-24 years, 2010-2016. Natl Health Stat Report. 2019;133:1–15. [PubMed] [Google Scholar]
- 123. Ruiz JR, Castro-Piñero J, Artero EG, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. 2009;43(12):909–923. [DOI] [PubMed] [Google Scholar]
- 124. Rutland M, O’Connell D, Brismée JM, Sizer P, Apte G, O’Connell J. Evidence-supported rehabilitation of patellar tendinopathy. N Am J Sports Phys Ther. 2010;5(3):166–178. [PMC free article] [PubMed] [Google Scholar]
- 125. Sachs CJ. Epidemiology of cheerleading injuries presenting to NEISS hospitals. J Trauma Acute Care Surg. 2012;72(4):1116. [DOI] [PubMed] [Google Scholar]
- 126. Sarraff LM, Haines CJ. Common orthopedic injuries in the pediatric ED. Pediatric Emergency Medicine Reports. July 1, 2010. [Google Scholar]
- 127. Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160(10):937–944. [DOI] [PubMed] [Google Scholar]
- 128. Schulz MR, Marshall SW, Yang J, Mueller FO, Weaver NL, Bowling JM. A prospective cohort study of injury incidence and risk factors in North Carolina high school competitive cheerleaders. Am J Sports Med. 2004;32(2):396–405. [DOI] [PubMed] [Google Scholar]
- 129. Senese M, Greenberg E, Todd Lawrence J, Ganley T. Rehabilitation following isolated posterior cruciate ligament reconstruction: a literature review of published protocols. Int J Sports Phys Ther. 2018;13(4):737–751. [PMC free article] [PubMed] [Google Scholar]
- 130. Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526–1533. [DOI] [PubMed] [Google Scholar]
- 131. Sherman E. Why don’t more people consider competitive cheerleading a sport? The rigorous activity is dominated by female athletes—and is growing in legitimacy and popularity. Accessed February 8, 2021. https://www.theatlantic.com/entertainment/archive/2017/05/why-dont-more-people-consider-competitive-cheerleading-a-sport/524940/
- 132. Shields BJ, Fernandez SA, Smith GA. Epidemiology of cheerleading stunt-related injuries in the United States. J Athl Train. 2009;44(6):586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Shields BJ, Smith GA. Cheerleading-related injuries in the United States: a prospective surveillance study. J Athl Train. 2009;44(6):567–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Shields BJ, Smith GA. Cheerleading-related injuries to children 5 to 18 years of age: United States, 1990-2002. Pediatrics. 2006;117(1):122–129. [DOI] [PubMed] [Google Scholar]
- 135. Shields BJ, Smith GA. Epidemiology of cheerleading fall-related injuries in the United States. J Athl Train. 2009;44(6):578–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Shields BJ, Smith GA. Epidemiology of strain/sprain injuries among cheerleaders in the United States. Am J Emerg Med. 2011;29(9):1003–1012. [DOI] [PubMed] [Google Scholar]
- 137. Shields BJ, Smith GA. The potential for brain injury on selected surfaces used by cheerleaders. J Athl Train. 2009;44(6):595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Singh S, Smith GA, Fields SK, McKenzie LB. Gymnastics-related injuries to children treated in emergency departments in the United States, 1990-2005. Pediatrics. 2008;121(4):e954–960. [DOI] [PubMed] [Google Scholar]
- 139. Sinha AK, Kaeding CC, Wadley GM. Upper extremity stress fractures in athletes: clinical features of 44 cases. Clin J Sport Med. 1999;9(4):199–202. [DOI] [PubMed] [Google Scholar]
- 140. Skendzel JG, Weber AE, Ross JR, et al. The approach to the evaluation and surgical treatment of mechanical hip pain in the young patient: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95(18):e133. [DOI] [PubMed] [Google Scholar]
- 141. Sports & Fitness Industry Association. Cheerleading participation report 2020. Accessed September 24, 2020. https://www.sfia.org/reports/808_Cheerleading-Participation-Report-2020
- 142. Steman JAH, Dahmen J, Lambers KTA, Kerkhoffs G. Return to sports after surgical treatment of osteochondral defects of the talus: a systematic review of 2347 cases. Orthop J Sports Med. 2019;7(10):2325967119876238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Stillman A, Alexander M, Mannix R, Madigan N, Pascual-Leone A, Meehan WP. Concussion: evaluation and management. Cleve Clin J Med. 2017;84(8):623–630. [DOI] [PubMed] [Google Scholar]
- 144. Stracciolini A, Casciano R, Friedman HL, Meehan WP, III, Micheli LJ. A closer look at overuse injuries in the pediatric athlete. Clin J Sport Med. 2015;25(1):30–35. [DOI] [PubMed] [Google Scholar]
- 145. Sung VW, Hampton BS. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 2009;36(3):421–443. [DOI] [PubMed] [Google Scholar]
- 146. Tarkin IS, Morganti CM, Zillmer DA, McFarland EG, Giangarra CE. Rotator cuff tears in adolescent athletes. Am J Sports Med. 2005;33(4):596–601. [DOI] [PubMed] [Google Scholar]
- 147. Thein-Nissenbaum JM, Rauh MJ, Carr KE, Loud KJ, McGuine TA. Menstrual irregularity and musculoskeletal injury in female high school athletes. J Athl Train. 2012;47(1):74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Thomas DQ, Seegmiller JG, Cook TL, Young BA. Physiologic profile of the fitness status of collegiate cheerleaders. J Strength Cond Res. 2004;18(2):252–254. [DOI] [PubMed] [Google Scholar]
- 149. Thompson SH, Digsby S. A preliminary survey of dieting, body dissatisfaction, and eating problems among high school cheerleaders. J Sch Health. 2004;74(3):85–90. [DOI] [PubMed] [Google Scholar]
- 150. Torres-McGehee TM, Monsma EV, Dompier TP, Washburn SA. Eating disorder risk and the role of clothing in collegiate cheerleaders’ body images. J Athl Train. 2012;47(5):541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Tsushima WT, Ahn HJ, Siu AM, Yoshinaga K, Choi SY, Murata NM. Effects of repetitive subconcussive head trauma on the neuropsychological test performance of high school athletes: a comparison of high, moderate, and low contact sports. Appl Neuropsychol Child. 2019;8(3):223–230. [DOI] [PubMed] [Google Scholar]
- 152. Tsushima WT, Siu AM, Ahn HJ, Chang BL, Murata NM. Incidence and risk of concussions in youth athletes: comparisons of age, sex, concussion history, sport, and football position. Arch Clin Neuropsychol. 2019;34(1):60–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Tsushima WT, Siu AM, Yamashita N, Oshiro RS, Murata NM. Comparison of neuropsychological test scores of high school athletes in high and low contact sports: a replication study. Appl Neuropsychol Child. 2018;7(1):14–20. [DOI] [PubMed] [Google Scholar]
- 154. US All Star Federation. 2020-2021 USASF cheer age grid. Accessed March 10, 2021. https://rules.usasfmembers.net/wp-content/uploads/2020/05/USASF_Cheer_Age-Grid_20-21.pdf
- 155. USA Cheer. Concussion management and return to play protocol. Accessed March 9, 2021. https://www.usacheer.org/safety/resources/concussion-management-return-to-play
- 156. USA Cheer. National governing body for sport cheering in the United States. Accessed March 10, 2021. https://www.usacheer.org/
- 157. USA Cheer. STUNT receives emerging sport recommendation from the NCAA’s committee on women’s athletics. Accessed March 10, 2021. https://www.usacheer.org/stunt-receives-emerging-sport-recommendation-from-the-ncaas-committee-on-womens-athletics
- 158. Varsity Spirit. Accessed March 10, 2021. https://www.varsity.com/
- 159. Vormittag K, Calonje R, Briner WW. Foot and ankle injuries in the barefoot sports. Curr Sports Med Rep. 2009;8(5):262–266. [DOI] [PubMed] [Google Scholar]
- 160. Wall EJ. Osgood-Schlatter disease: practical treatment for a self-limiting condition. Phys Sportsmed. 1998;26(3):29–34. [DOI] [PubMed] [Google Scholar]
- 161. Warme WJ, Arciero RA, Taylor DC. Anterior shoulder instability in sport: current management recommendations. Sports Med. 1999;28(3):209–220. [DOI] [PubMed] [Google Scholar]
- 162. Waterman BR, Belmont PJ, Jr, Cameron KL, Deberardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38(4):797–803. [DOI] [PubMed] [Google Scholar]
- 163. Waters N. What goes up must come down! A primary care approach to preventing injuries amongst highflying cheerleaders. J Am Assoc Nurse Pract. 2013;25(2):55–64. [DOI] [PubMed] [Google Scholar]
- 164. Weber AE, Bedi A, Tibor LM, Zaltz I, Larson CM. The hyperflexible hip: managing hip pain in the dancer and gymnast. Sports Health. 2015;7(4):346–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Weiss JM, Jordan SS, Andersen JS, Lee BM, Kocher M. Surgical treatment of unresolved Osgood-Schlatter disease: ossicle resection with tibial tubercleplasty. J Pediatr Orthop. 2007;27(7):844–847. [DOI] [PubMed] [Google Scholar]
- 166. Wells EK, Chin AD, Tacke JA, Bunn JA. Risk of disordered eating among Division I female college athletes. Int J Exerc Sci. 2015;8(3):256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Wendling S. What’s an off-season? Tips for pushing through a year-long sport. Accessed March 10, 2021. https://www.insidecheerleading.com/news-features/whats-an-off-season-tips-for-pushing-through-a-year-long-sport/
- 168. Williams GR, Kelley M. Management of rotator cuff and impingement injuries in the athlete. J Athl Train. 2000;35(3):300–315. [PMC free article] [PubMed] [Google Scholar]
- 169. Wilson DJ. Osteoporosis and sport. Eur J Radiol. 2019;110:169–174. [DOI] [PubMed] [Google Scholar]
- 170. Wolff CS, Cantu RC, Kucera KL. Catastrophic neurologic injuries in sport. Handb Clin Neurol. 2018;158:25–37. [DOI] [PubMed] [Google Scholar]
- 171. Wright AA, Hegedus EJ, Taylor JB, Dischiavi SL, Stubbs AJ. Non-operative management of femoroacetabular impingement: a prospective, randomized controlled clinical trial pilot study. J Sci Med Sport. 2016;19(9):716–721. [DOI] [PubMed] [Google Scholar]
- 172. Xu AL, Suresh KV, Lee RJ. Progress in cheerleading safety: update on the epidemiology of cheerleading injuries presenting to US emergency departments, 2010-2019. Orthop J Sports Med. Published online October 13, 2021. doi: 10.1177/23259671211038895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Yau RK, Dennis SG, Boden BP, Cantu RC, Lord JA, III, Kucera KL. Catastrophic high school and collegiate cheerleading injuries in the United States: an examination of the 2006-2007 basket toss rule change. Sports Health. 2019;11(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Young TE, Chen M. One-year concussion prevalence in Marion County, Florida high school athletes. J Chiropr Med. 2016;15(3):204–207. [DOI] [PMC free article] [PubMed] [Google Scholar]