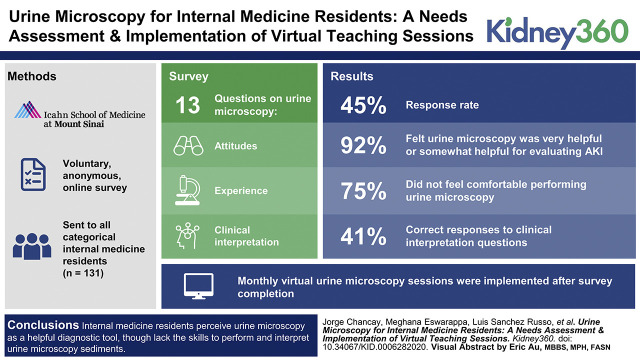
Visual Abstract
Keywords: clinical nephrology, acute kidney injury, internal medicine residents, medical education, nephrology, residents, trainees, urine, urine microscopy, video conferencing, virtual
Abstract
Background
Although urine microscopy is an important step in the initial evaluation of a patient with kidney disease, internal medicine residents have minimal exposure to this technique during their training. The goal of this study was to understand knowledge of and attitudes toward urine microscopy among internal medicine residents and to implement virtual urine microscopy teaching sessions.
Methods
A voluntary, anonymous, online survey was sent to all of the categorical internal medicine residents (n=131) training at the Icahn School of Medicine at Mount Sinai (ISMMS). The survey included 13 questions to assess attitudes toward, experience with, and clinical interpretation of urine microscopy specimens. In response to the survey results, we implemented virtual urine microscopy teaching sessions using video conferencing software that incorporated real-time urine sediment analysis with nephrology fellows and attending nephrologists.
Results
The survey response rate was 45% (59 of 131). Forty-seven percent (28 of 59) of respondents reported performing urine microscopy at least once during their training, and 75% (44 of 59) of respondents did not feel comfortable performing urine microscopy. The majority of residents (92%; 54 of 59) reported they felt urine microscopy was very helpful or somewhat helpful in the evaluation of patients with AKI. Overall, 41% of responses to clinical interpretation questions were considered correct. Following survey completion, virtual urine microscopy sessions were held monthly and well received by the participants.
Conclusions
Our study found that internal medicine residents perceive urine microscopy as a helpful diagnostic tool, although lack the skills to perform and interpret urine microscopy sediments. Virtual educational sessions using video conferencing software are a technically feasible approach to teaching urine microscopy to internal medicine residents. Future studies include a study of the effect of these sessions on learning of urine microscopy.
Podcast
This article contains a podcast at https://www.asn-online.org/media/podcast/K360/2021_01_28_KID0006282020.mp3.
Introduction
Urine microscopy is an important step in the diagnostic evaluation of a wide range of kidney pathologies (1–4). Although urine microscopy is often performed via automated methods on the basis of flow cytometry or software recognition, a thorough manual evaluation of the urine sediment has been shown to be a low-cost and clinically useful tool in the diagnosis of kidney disease (1,4,5). Its utility as a diagnostic aid ranges from glomerular, tubular, and metabolic disorders to toxin ingestions and hemodynamic kidney injury (1–4,6,7). Urine microscopy has also been shown to be a useful prognostic tool, specifically in acute tubular necrosis (6,7) and it is both inexpensive and noninvasive (1–4). With the current prevalence of AKI reported as high as 20% in hospitalized patients, education on how to perform this procedure should be available to clinicians caring for patients with AKI (8–10).
Despite urine microscopy findings being taught during preclinical training, internal medicine trainees generally do not receive formal education on performance and interpretation of urine microscopy—unless they happen to learn this during their nephrology rotation. Previous reports on potential reasons to explain the low interest in nephrology as a specialty choice consistently highlight lack of diverse exposure to the field and the paucity of procedures (11,12). In addition to improving clinical reasoning skills and patient management, exposure to and teaching of urine microscopy to trainees during internal medicine residency have the potential to increase interest in nephrology as a future career choice. Moreover, studies have found interobserver variability while analyzing urine microscopy, even between attending nephrologists, indicating a need for enhanced education on urine microscopy analysis at all training levels (13,14).
In this study, we administered an anonymous survey to assess internal medicine residents’ knowledge of and attitudes toward urine microscopy. The results of this assessment were used to develop virtual urine microscopy teaching sessions for internal medicine residents, during which participants viewed urine sediment analysis in real time with attending nephrologists and nephrology fellows.
Materials and Methods
Survey
An anonymous, online, voluntary survey (Google Forms, Mountain View, CA) was sent to all categorical internal medicine residents (n=131) enrolled at the Icahn School of Medicine at Mount Sinai (ISMMS). The survey (Supplemental Material) included 13 questions that addressed demographics and both attitudes toward and experience with urine microscopy. Three content questions asked for clinical interpretation of an image of a white blood cell cast, uric acid crystals, and acanthocytes. A five-point Likert scale was used to assess attitudes and experiences. These clinical interpretation questions were validated by two nephrologists who did not participate in the study.
Virtual Urine Microscopy Teaching Sessions
After survey completion, voluntary urine microscopy teaching sessions were scheduled every month for all internal medicine residents after discussion with residency program leadership. Sessions were held via video conferencing software (Zoom Video Communications, San Jose, CA). A mobile device (iPhone 5C; Apple Inc., Cupertino, CA), installed with the Zoom application, was connected to an Olympus BH-2 microscope via microscope adapter (iDu Optics) (Figure 1). This device was then connected via lightning cable to a computer to share the microscope view with all participants (Figure 2). Fresh urine samples were collected from hospitalized patients shortly before the session, and urine sediment slides were prepared prior to the session using standard technique. Sessions were structured first with a 15-minute introduction to urine microscopy and then, 45 minutes of real-time viewing of the urine sediment with teaching of urine microscopy findings with clinical correlation that was led by nephrology fellows. Attending nephrologists were also in attendance. Urine sediments were viewed under light microscopy with different objectives (×4, ×10, and ×40), phase contrast (×40), and a polarizer. Sediments were also viewed after Sternheimer–Malbin staining. All participants were able to use the “Annotation” feature to draw or point to structures seen under the microscope.
Figure 1.
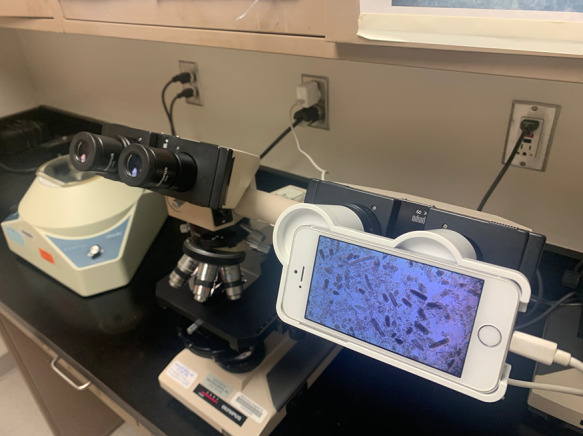
Centrifuge and microscope with mobile device and adapter.
Figure 2.
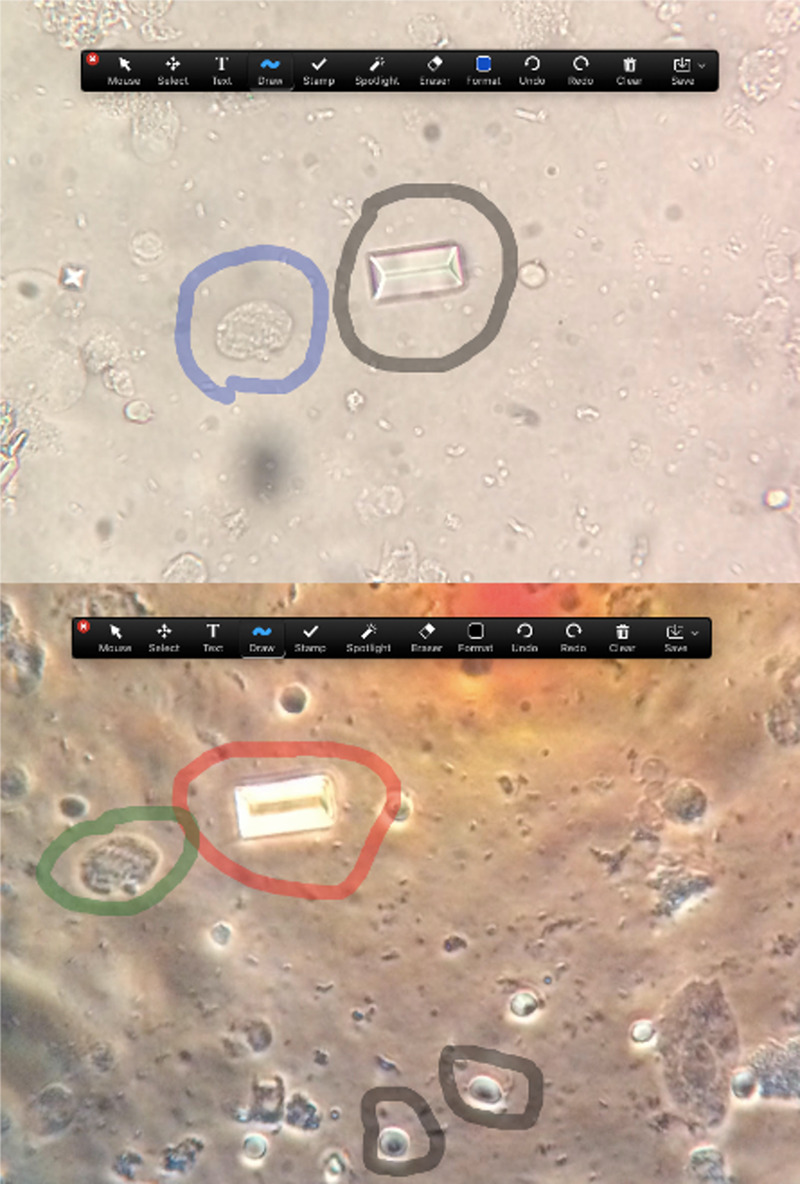
Screenshots of virtual urine microscopy session (via Zoom), with an annotation bar. (Upper panel) Light microscopy, ×40. Unstained sample with struvite stone (gray) and transitional epithelial cell (blue). (Lower panel) Phase contrast, ×40. Polarized sample with struvite stone (red), transitional epithelial cell (green), and monomorphic red blood cells (gray).
Statistical Analyses
Chi-squared analysis and t tests were used to compare survey results between postgraduate year (PGY) groups (PGY-1, PGY-2, and PGY-3). Comparison of postgraduate group means (PGY-1, PGY-2, and PGY-3) of Likert-scale questions was performed using Kruskal–Wallis one-way ANOVA with Dunn multiple comparisons post-test. All statistics were performed with GraphPad Prism 8 (San Diego, CA). P=0.05 were considered statistically significant.
This study was approved by the ISMMS Institutional Review Board.
Results
Demographics, Experience, and Comfort Level with Urine Microscopy
Survey response rate among categorical internal medicine residents was 45% (59 of 131). Of the respondents, 58% (34 of 59) identified as women, and 41% (24 of 59) identified as men. All respondents were between 25 and 36 years of age. Of the 59 respondents, 31% (18 of 59) were PGY-1, 42% (25 of 59) were PGY-2, and 27% (16 of 59) were PGY-3.
Survey question responses are summarized in Table 1. Forty-seven percent (28 of 59) of respondents reported performing urine microscopy at least once during their training. PGY-3 respondents were more likely (75%, 12 of 16, P=0.03) to have previously performed urine microscopy than PGY-2 (40%, ten of 25) or PGY-1 (33%, six of 18). Overall, 12% (seven of 59) felt “somewhat comfortable” performing this procedure, and none reported feeling “very comfortable” (Table 1). Seventy-five percent of respondents felt “not very comfortable” or “not at all comfortable” while performing urine microscopy.
Table 1.
Attitudes toward and comfort level with urine microscopy
| Survey Question | All, n=59 | Postgraduate Year 1, n=18 | Postgraduate Year 2, n=25 | Postgraduate Year 3, n=16 | P Value |
| How helpful do you think urine microscopy is? | |||||
| Very helpful (5) | 30 (51%) | 8 (47%) | 15 (58%) | 7 (44%) | |
| Somewhat helpful (4) | 24 (41%) | 5 (29%) | 10 (38%) | 9 (56%) | |
| Neutral (3) | 5 (9%) | 4 (24%) | 1 (4%) | 0 (0%) | |
| Not very helpful (2) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Not at all helpful (1) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Mean (SD) | 4.4 (0.7) | 4.3 (0.8) | 4.6 (0.6) | 4.4 (0.5) | 0.41 |
| How comfortable do you feel performing urine microscopy? | |||||
| Very comfortable (5) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Somewhat comfortable (4) | 7 (12%) | 1 (6%) | 3 (12%) | 3 (19%) | |
| Neutral (3) | 8 (14%) | 1 (6%) | 6 (23%) | 1 (6%) | |
| Not very comfortable (2) | 18 (31%) | 3 (18%) | 8 (30%) | 7 (44%) | |
| Not at all comfortable (1) | 26 (44%) | 12 (70%) | 9 (35%) | 5 (31%) | |
| Mean (SD) | 1.9 (1.1) | 1.5 (0.9) | 2.2 (0.2) | 2.1 (1.1) | 0.05 |
| Have you ever performed urine microscopy? | |||||
| Yes | 28 (48%) | 6 (35%) | 10 (38%) | 12 (75%) | |
| No | 29 (49%) | 11 (65%) | 15 (58%) | 3 (19%) | |
| Not sure | 2 (3%) | 0 (0%) | 1 (4%) | 1 (6%) |
Means between postgraduate year (PGY) groups were calculated and compared using the Kruskal–Wallis one-way ANOVA with Dunn multiple comparisons post-test. Post-test analysis for “How helpful do you think urine microscopy is?”: PGY-1 versus PGY-2, P=0.80; PGY-1 versus PGY-3, P>0.99; PGY-2 versus PGY-3, P=0.80. Post-test for “How comfortable do you feel performing urine microscopy?”: PGY-1 versus PGY-2, P=0.05; PGY-1 versus PGY-3, P=0.30; PGY-2 versus PGY-3, P>0.99.
Respondents entered qualitative comments, including “Would like to learn how to spin urine,” “I’ve never done it! I wish we learned more about it,” “I did a nephrology rotation in med school and we spun urine on all our consults. I found it super informative and interesting!,” and “It was a really cool experience that I was able to have thanks to the nephrology fellow. It helped crystallize my book learning with real world experience.” No negative comments were entered.
Perceived Utility and Performance on Clinical Interpretation Questions
When asked their perception of the utility of urine microscopy in the clinical workup of AKI, 92% (54 of 59) felt it was “very helpful” or “somewhat helpful” (Table 1). Higher training level was associated with a higher perceived value in urine microscopy, with 100% (16 of 16) of PGY-3 respondents, 96% (25 of 26) PGY-2 respondents, and 78% of PGY-1 (14 of 18) respondents feeling that it was either “very helpful” or “somewhat helpful” (P=0.03).
Overall, 40%, 37%, and 46% of clinical interpretation questions were answered correctly by PGY-1, PGY-2, and PGY-3 respondents, respectively (Figure 3A). Correct responses to the three questions did not correlate with PGY status (PGY-1, P=0.10; PGY-2, P=0.20; PGY-3, P=0.80). Percentages of correct responses to individual questions are summarized in Figure 3A. Prior experience with urine microscopy was not associated with higher performance on the content questions (Figure 3B). Similarly, comfort level with urine microscopy was not associated with higher performance on the content questions (Figure 3C).
Figure 3.
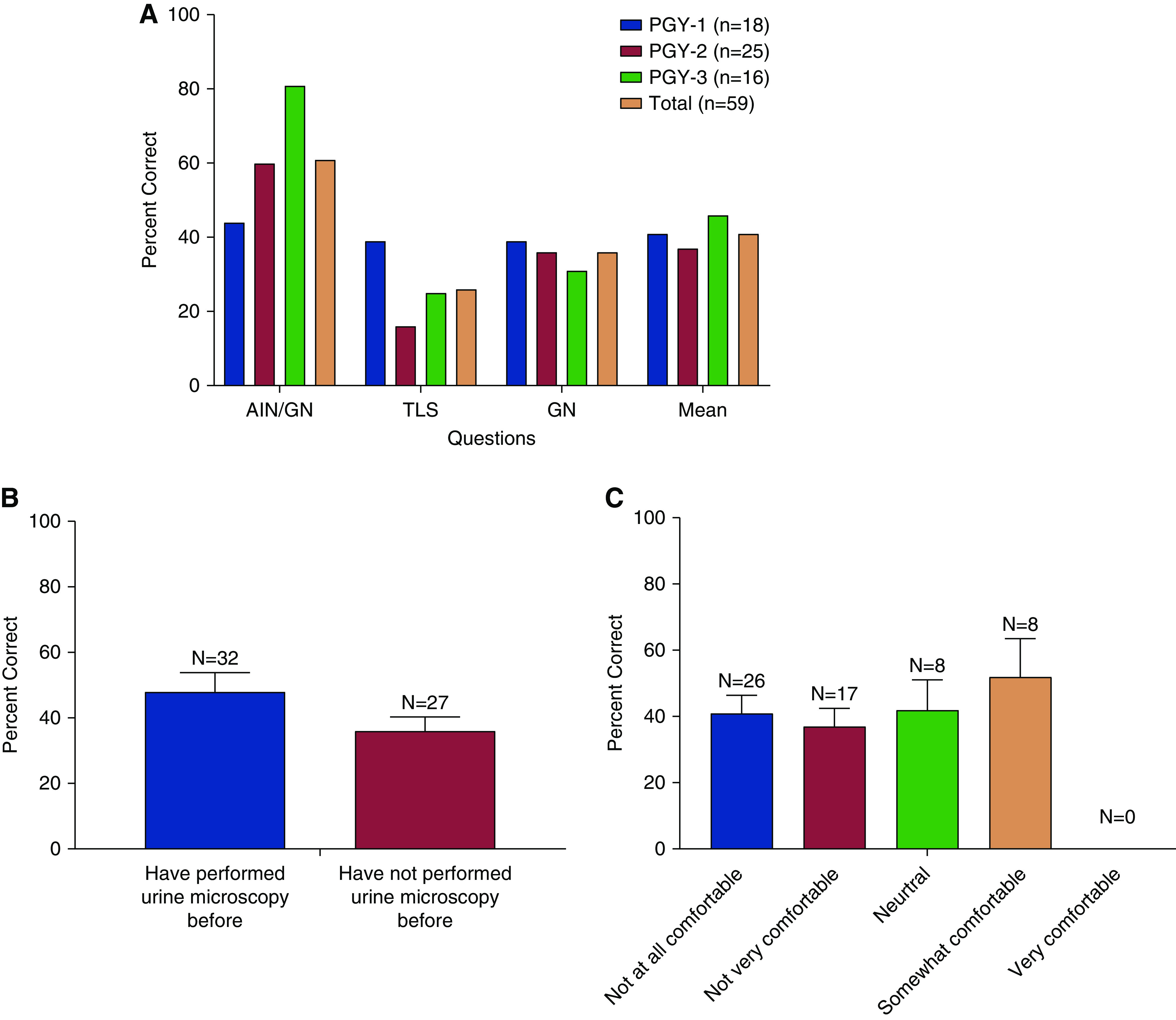
Performance on urine microscopy clinical correlation questions. (A) Mean percentage of urine microscopy clinical interpretation questions correctly answered by training level. Error bars represent SEM. Chi-squared analysis was used to compare performance by postgraduate year (PGY) group for each question. Acute interstitial nephritis (AIN), P=0.10; tumor lysis syndrome (TLS), P=0.20; GN, P=0.90. (B) The mean percentage of correct responses to all three questions were compared with whether or not the trainee had indicated that they had performed urine microscopy (“not sure” was included in the “no” group). No difference was seen in either group (unpaired t test, P=0.50). (C) The mean percentage of correct response was compared with the five different urine microscopy comfort levels (Likert scale). No differences were identified using Kruskal–Wallis test and Dunn multiple comparisons (P=0.80; all comparisons P>0.99).
Interest in Nephrology as a Career Choice
In response to a question about interest in nephrology as a career choice, 15% (nine of 59) of respondents reported feeling “very interested” or “somewhat interested,” whereas 73% reported feeling “not very interested” and “not at all interested” (43 of 59). Seven percent (four of 59) of the respondents reported nephrology as the current specialty of choice. The most popular specialties of interest within this cohort were cardiology, gastroenterology, pulmonary/critical care, and hospital medicine with 25%, 25%, 10%, and 10%, respectively. Of the 15% (nine of 59) of respondents who reported feeling “very interested” or “somewhat interested” in nephrology as a career choice, 55% (five of nine) reported having performed urine microscopy at least once during their training. Of those “not very interested,” “not at all interested,” or “neutral” regarding their interest in nephrology as a career choice, 46% (23 of 50) reported performing urine microscopy at least once during their training.
Virtual Urine Microscopy Sessions
Sessions were scheduled monthly and attended by 15 residents on average. Urine samples from at least three patients were reviewed at each session.
Discussion
Our survey results found that the majority of internal medicine residents feel that urine microscopy is an important tool to aid in the diagnosis of AKI, although they do not feel comfortable performing this skill. Somewhat surprisingly, residents’ comments suggest an interest in wanting to learn more about this procedure—despite a lack of interest in nephrology as a specialty. Residents with a higher level of training were more likely to view microscopy as an important diagnostic tool or have experience with this technique, which is likely a reflection of their clinical exposure. Responses to content questions revealed a significant knowledge gap in the clinical interpretation of urine microscopy sediments.
Responses and comments from our survey revealed an overall positive attitude toward urine microscopy, suggesting willingness to learn this skill. Of note, those with an interest in pursuing nephrology as a subspecialty did not report more experience in performance of urine microscopy when compared with the rest of the cohort. Our study found that 15% of respondents had some interest in nephrology, similar to previous reports (15).
Interest in nephrology as a career remains low, with only 60% of the offered positions filled in the match recently (11,12,15). Studies have shown a lack of diverse exposure to the field and dearth of procedures as potential reasons for low interest (11,12,15). Although procedures within a specialty generally may be attractive as a means for reimbursement, urine microscopy has the potential to improve understanding of nephrology pathophysiology, provide unique exposure to the field beyond traditional clinical experiences, and ultimately increase interest in nephrology as a career choice. Interestingly, the proportion of internal medicine residents who had performed urine microscopy in the past was similar between those with an interest in nephrology as a career and those without. Existing literature supports the use of virtual and online teaching tools in medical education, which has now been accelerated by the coronavirus disease 2019 pandemic that necessitates social distancing (16–19). We found that when necessary resources and technology are available, virtual urine microscopy teaching sessions are a feasible method to teach internal medicine residents a technique that can help with their clinical reasoning skills and management of patients with AKI —while increasing exposure to nephrology during the coronavirus disease 2019 pandemic. Other institutions may be able to replicate these virtual sessions to similarly teach trainees urine microscopy or other topics via microscopy (e.g., kidney pathology). Further, learning urine microscopy may be especially helpful for clinicians who plan to practice in primary care or settings with limited nephrology resources.
Limitations of this study include selection bias as our survey was voluntary. It is possible that our respondents were more interested in nephrology topics than those who did not answer the survey, although the majority did not indicate an interest in nephrology as a subspecialty choice. Data available for analysis were also limited as we only included three questions to assess clinical interpretation of urine microscopy images. Additional questions were not included to improve our survey response and completion rate. All respondents answered all questions before submission. As these clinical interpretation questions were multiple choice questions with five options, it is possible that respondents may have answered each question correctly by chance 20% of the time. Of note, knowledge questions on the survey asked for clinical interpretation of white blood cell casts, acanthocytes, and uric acid crystals rather than identification of urine sediment elements. Although it has been reported that white blood cell casts are highly sensitive for acute interstitial nephritis, they may not always reliably predict histologic diagnosis. As white blood cell casts may be present in exudative GN, both acute interstitial nephritis and GN (selected by eight of 59, 13.6%) were considered to be correct responses (4,20). Finally, our study is a single-center study at a large academic institution with available technology resources, and thus, generalizability may be limited.
In conclusion, we found that internal medicine residents perceive urine microscopy as a helpful diagnostic tool, although lack the skills to perform and interpret urine microscopy sediments. Implementation of virtual urine microscopy sessions with real-time viewing of urine microscopy samples has the potential to improve residents’ knowledge of this skill set and possibly, interest in nephrology as a specialty choice. Future studies include systematic evaluation of our sessions, including a reassessment of knowledge of and attitudes toward urine microscopy. Future plans also include expansion of these sessions to include trainees and nephrologists from around the world.
Disclosures
S.S. Farouk reports other interests/relationships with American Journal of Kidney Diseases (editorial board), Clinical Transplantation (editorial board), and Journal of Nephrology (editorial board). M.A. Sparks reports honoraria from Elsevier-Nephrology Secrets and scientific advisor of or membership with the American Board of Internal Medicine (nephrology board), NephJC (board of directors), American Society of Nephrology (media and communications committee), American Journal of Kidney Diseases (editorial board), Kidney360 (editorial board), Kidney Medicine (editorial board), American Heart Association (Kidney & Cardiovascular Disease Membership and Communications Committee and Kidney & Cardiovascular Disease Scientific and Clinical Education Lifelong Learning Committee), and the National Kidney Foundation North Carolina (medical advisory board). All remaining authors have nothing to disclose.
Funding
S.S. Farouk is funded by the American Society of Nephrology KidneyCure William and Sandra Bennett Clinical Scholars Program.
Author Contributions
J. Chancay and S.S. Farouk conceptualized the study; M. Eswarappa, S.S. Farouk, and M.A. Sparks were responsible for data curation; S.S. Farouk was responsible for visualization; J. Chancay, M. Eswarappa, S.S. Farouk, and M.A. Sparks were responsible for formal analysis; J. Chancay, S.S. Farouk, L. Sanchez Russo, and M.A. Sparks were responsible for investigation; J. Chancay, S.S. Farouk, L. Sanchez Russo, and M.A. Sparks were responsible for methodology; J. Chancay, S.S. Farouk, L. Sanchez Russo, and M.A. Sparks were responsible for project administration; S.S. Farouk and M.A. Sparks were responsible for resources; S.S. Farouk and M.A. Sparks provided supervision; J. Chancay and S.S. Farouk were responsible for validation; J. Chancay, S.S. Farouk, and M.A. Sparks wrote the original draft; and J. Chancay, S.S. Farouk, and M.A. Sparks reviewed and edited the manuscript.
Supplemental Material
This article contains supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0006282020/-/DCSupplemental.
Urine microscopy lecture series; Pre-survey. Download Supplemental Material, PDF file, 428 KB (427.1KB, pdf)
References
- 1.Becker GJ, Garigali G, Fogazzi GB: Advances in urine microscopy. Am J Kidney Dis 67: 954–964, 2016. 10.1053/j.ajkd.2015.11.011 [DOI] [PubMed] [Google Scholar]
- 2.Perazella MA, Coca SG, Kanbay M, Brewster UC, Parikh CR: Diagnostic value of urine microscopy for differential diagnosis of acute kidney injury in hospitalized patients. Clin J Am Soc Nephrol 3: 1615–1619, 2008. 10.2215/CJN.02860608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verdesca S, Brambilla C, Garigali G, Croci MD, Messa P, Fogazzi GB: How a skilful (correction of skilful) and motivated urinary sediment examination can save the kidneys. Nephrol Dial Transplant 22: 1778–1781, 2007. 10.1093/ndt/gfm142 [DOI] [PubMed] [Google Scholar]
- 4.Cavanaugh C, Perazella MA: Urine sediment examination in the diagnosis and management of kidney disease: Core curriculum 2019. Am J Kidney Dis 73: 258–272, 2019. 10.1053/j.ajkd.2018.07.012 [DOI] [PubMed] [Google Scholar]
- 5.Cho SY, Hur M: Advances in automated urinalysis systems, flow cytometry and digitized microscopy. Ann Lab Med 39: 1–2, 2019. 10.3343/alm.2019.39.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chawla LS, Dommu A, Berger A, Shih S, Patel SS: Urinary sediment cast scoring index for acute kidney injury: A pilot study. Nephron Clin Pract 110: c145–c150, 2008. 10.1159/000166605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perazella MA, Coca SG, Hall IE, Iyanam U, Koraishy M, Parikh CR: Urine microscopy is associated with severity and worsening of acute kidney injury in hospitalized patients. Clin J Am Soc Nephrol 5: 402–408, 2010. 10.2215/CJN.06960909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeng X, McMahon GM, Brunelli SM, Bates DW, Waikar SS: Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol 9: 12–20, 2014. 10.2215/CJN.02730313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA; Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators: Septic acute kidney injury in critically ill patients: Clinical characteristics and outcomes. Clin J Am Soc Nephrol 2: 431–439, 2007. 10.2215/CJN.03681106 [DOI] [PubMed] [Google Scholar]
- 10.Chan L, Coca SG: Acute kidney injury in the time of COVID-19. Kidney360 1: 588–590, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nair D, Pivert KA, Baudy A 4th, Thakar CV: Perceptions of nephrology among medical students and internal medicine residents: A national survey among institutions with nephrology exposure. BMC Nephrol 20: 146, 2019. 10.1186/s12882-019-1289-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sozio SM, Pivert KA, Shah HH, Chakkera HA, Asmar AR, Varma MR, Morrow BD, Patel AB, Leight K, Parker MG: Increasing medical student interest in nephrology. Am J Nephrol 50: 4–10, 2019. 10.1159/000501058 [DOI] [PubMed] [Google Scholar]
- 13.Wald R, Bell CM, Nisenbaum R, Perrone S, Liangos O, Laupacis A, Jaber BL: Interobserver reliability of urine sediment interpretation. Clin J Am Soc Nephrol 4: 567–571, 2009. 10.2215/CJN.05331008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palsson R, Colona MR, Hoenig MP, Lundquist AL, Novak JE, Perazella MA, Waikar SS: Assessment of interobserver reliability of nephrologist examination of urine sediment. JAMA Netw Open 3: e2013959, 2020. 10.1001/jamanetworkopen.2020.13959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daniels MN, Maynard S, Porter I, Kincaid H, Jain D, Aslam N: Career interest and perceptions of nephrology: A repeated cross-sectional survey of internal medicine residents. PLoS One 12: e0172167, 2017. 10.1371/journal.pone.0172167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hale LS, Mirakian EA, Day DB: Online vs classroom instruction: Student satisfaction and learning outcomes in an undergraduate Allied Health pharmacology course. J Allied Health 38: e36–e42, 2009 [PubMed] [Google Scholar]
- 17.Khogali SEO, Davies DA, Donnan PT, Gray A, Harden RM, McDonald J, Pippard MJ, Pringle SD, Yu N: Integration of e-learning resources into a medical school curriculum. Med Teach 33: 311–318, 2011. 10.3109/0142159X.2011.540270 [DOI] [PubMed] [Google Scholar]
- 18.Newman NA, Lattouf OM: Coalition for medical education-A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. J Card Surg 35: 1174–1175, 2020. 10.1111/jocs.14590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hilburg R, Patel N, Ambruso S, Biewald MA, Farouk SS: Medical education during the coronavirus disease 2019 pandemic: Learning from a distance [published online ahead of print June 23, 2020]. Adv Chronic Kidney Dis 10.1053/j.ackd.2020.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perazella MA: Diagnosing drug-induced AIN in the hospitalized patient: A challenge for the clinician. Clin Nephrol 81: 381–388, 2014. 10.5414/CN108301 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Urine microscopy lecture series; Pre-survey. Download Supplemental Material, PDF file, 428 KB (427.1KB, pdf)