Training healthcare workers in disaster preparedness has been shown to increase their willingness and ability to report to work during emergencies. This article assesses the perceived need for additional disaster preparedness training among clinicians and nonclinicians at the US Department of Veterans Affairs for three types of disasters (natural, pandemic, manmade) and examines the determinants, including sociodemographic, household, and workforce characteristics, that influence the desire for such training. Identifying which factors influence participation in preparedness trainings will guide national training efforts and improve hospital operations and health services delivery before, during, and after disasters.
Key Words: continuing education, disasters, emergency preparedness, healthcare providers, US Department of Veterans Affairs
Abstract
Objectives
Training healthcare workers in disaster preparedness has been shown to increase their willingness and ability to report to work during disasters. Little is known, however, about the relation between sociodemographic, household, and workforce characteristics and the desire for such training. Accordingly, this study aimed to assess healthcare workers’ desire for additional workforce preparedness training, and the determinants that influence the need for such training, for three types of disasters (natural, pandemic, manmade).
Methods
The US Department of Veterans Affairs (VA) Preparedness Survey was a random, anonymous, Web-based questionnaire fielded nationwide (October–December 2018). Multivariate, logistic regression analyses were conducted.
Results
In total, 4026 VA employees, clinical and nonclinical, responded. A total of 61% of respondents wanted additional training for natural, 63% for pandemic, and 68% for manmade disasters. VA supervisors (natural: odds ratio [OR] 1.28, pandemic: OR 1.33, manmade: OR 1.25, P < 0.05) and clinicians (natural: OR 1.24, pandemic: OR 1.24, manmade: OR 1.24, P < 0.05) were more likely to report the need for additional training. Those who reported that they understood their role in disaster response were less likely to report the need for training (natural: OR 0.25, pandemic: OR 0.27, manmade: OR 0.28, P < 0.001), whereas those who perceived their role to be important during response (natural: OR 2.20, pandemic: OR 2.78, manmade: OR 3.13, P < 0.001), and those who reported not being prepared at home for major disasters (natural: OR 1.85, pandemic: OR 1.92, manmade: OR 1.94, P < 0.001), were more likely to indicate a need for training.
Conclusions
Identifying which factors encourage participation in disaster preparedness training can help hospitals and other healthcare providers create targeted training and educational materials to better prepare all hospital staff for future disasters.
Key Points
In total, 61% want training to prepare for natural disasters, 63% for pandemics, and 68% for manmade disasters.
Supervisors and clinicians were more likely to report the need for additional training to prepare for disasters.
Employees who understand their role during disaster response were less likely to want additional training.
Employees who perceive their role during disaster response as important were more likely to want additional training.
Those not prepared at home for disasters more likely to want additional training.
Before 2001, few US healthcare workers had formal disaster preparedness education, and those who did likely worked in emergency departments, had served in the military, or had previous disaster relief experience.1 A significant change occurred following the events of September 11, 2001, with the release of stricter standards from The Joint Commission (TJC) and the creation of the Office of the Assistant Secretary for Preparedness and Response within the US Department of Health and Human Services.2 In 2004, the US Department of Veterans Affairs (VA) Office of Emergency Management developed and implemented the Comprehensive Emergency Management Program aimed at ensuring the resiliency, continuity, and rapid recovery of VA healthcare services and facilities during disasters.3 TJC and the Centers for Medicare & Medicaid Services require that their accredited healthcare organizations conduct an exercise to test their emergency plan at least annually, including a full-scale community-based exercise or facility-based functional exercise every other year, and then conduct a mock disaster drill or a tabletop exercise the following year.4,5 Approximately 77% of US hospitals are accredited by TJC,6 including all VA facilities, and thus meet their emergency preparedness requirements. There are also state-level training requirements for clinicians set by professional standards boards.
Although there is no consensus regarding the most effective methods of training healthcare workers in disaster preparedness,1,7–9 disaster training has been shown to improve preparedness knowledge8,10,11 and increase the ability and willingness of healthcare workers to report to work during disasters.1,12–15 Such findings point toward the need to better understand which factors encourage healthcare workers to participate in disaster training. There is, however, a gap in the literature regarding the relation between sociodemographic, household, or workforce characteristics and the desire for additional disaster preparedness training. A better understanding of the various factors that may influence healthcare workers’ desire for additional training would help hospitals create targeted disaster preparedness trainings that will better prepare nurses, physicians, and hospital support staff for disasters. The current coronavirus disease 2019 (COVID-19) pandemic stresses the need for additional training for future infectious disease outbreaks and other major disasters.
The VA provides care to >9 million veterans at 1255 facilities and has a large healthcare staff, including the largest nursing workforce in the United States.16 One of the missions of the VA is to provide medical resources and care to both veterans and nonveterans during major disasters and thus has responded to numerous national emergencies,17–19 including the COVID-19 pandemic.19 Because the VA plays an important role in the nation’s disaster response, understanding the perceptions of workplace preparedness and training needs for all VA healthcare employees is critical to ensure the continued delivery of care to US military veterans and local communities during times of crisis.
Accordingly, the first nationwide survey to examine the disaster preparedness of VA healthcare employees was developed and conducted across the United States in late 2018. The VA All Employee Disaster Preparedness Survey (VA Preparedness Survey) focused on perceptions about workforce preparedness, the need for additional training to prepare for disasters, and understanding of individual response roles and their perceived importance of their roles during three types of major disasters: natural, pandemic, and manmade. This article examines the determinants of the perceived need for additional disaster preparedness training among VA staff, and focuses on employees’ understanding and perception of the importance of their role during their facility’s response to the aforementioned types of disasters.
Methods
The VA Preparedness Survey was a random, anonymous, 10-minute Web-based survey of all full-time and part-time employees at VA medical facilities nationwide. The survey was fielded from October through December 2018, and both clinical and nonclinical staff were invited to participate. Additional details regarding the study design, questionnaire, and study population are available elsewhere.20,21 This study was determined by the local institutional review board to be a quality-improvement, nonresearch project.
Statistical Analyses
Descriptive statistical analyses were conducted to illustrate the sociodemographic, work-related, general health, and household-related characteristics of the study population, and the percent distribution of key study variables, including perceptions of workforce preparedness during natural, pandemic, and manmade types of major disasters. For this article, the determinants of additional training to prepare for the three types of disasters were examined, in which each dependent variable was dichotomized by combining the “strongly agree/agree” responses into one category and the remaining responses (“strongly disagree,” “disagree,” and “neutral”) into another category, given that this study aims to identify the predictors of workforce preparedness training. The analyses included three multivariate logistic regressions, one for each disaster type. The following covariates were included in the multivariate logistic regression models: sociodemographic characteristics (sex, age, race, marital status, education, and military background), overall general health status, work-related characteristics (clinical duties, supervisory responsibilities, number of years at the VA, and whether the respondent previously experienced one or more disasters while at the VA), and household characteristics (dependents younger than 18 years, household preparedness, has plans to meet family’s healthcare needs during major disasters, and responsible for assisting someone who does not live at home). The main independent variables were related to perceptions of workforce preparedness; for each disaster type (natural, pandemic, manmade), survey respondents were asked to rate the following two items using a 5-point (strongly agree to strongly disagree) Likert scale: I understand my role in my facility’s overall disaster response and my role in my facility’s overall disaster response is important. The response categories for these independent variables were dichotomized by combining the “strongly agree/agree” responses into one category, and the remaining responses (“strongly disagree,” “disagree,” and “neutral”) into another category. In addition, to account for the survey design weights, the svy command in STATA (version 15, StataCorp, College Station, TX) was used when conducting the logistics regression analyses. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to determine the statistically significant predictors of workforce preparedness training for three types of disasters. Statistical significance was set at P < 0.05.
Results
Characteristics of Participants
Details about the sociodemographic characteristics of the study participants are available elsewhere.22
Perceptions of Workforce Disaster Preparedness
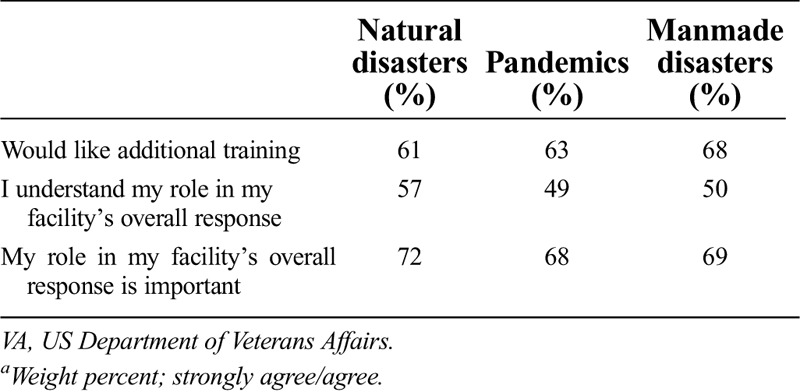
Table 1 presents the weighted percent distribution of responses for the three workforce disaster preparedness variables. For the dependent variable I would like additional trainings to prepare, 61% strongly agreed/agreed wanting additional training for natural disasters, 63% for pandemics, and 68% for manmade disasters. For the first set of independent variables, I understand my role in my facility’s overall response, the weighted percent distributions of strongly agree/agree were 57% for natural disasters, 49% for pandemics, and 50% for manmade disasters. For the second set of independent variables, My role in my facility’s overall response is important, the weighted percent distributions of strongly agree/agree were 72% for natural disasters, 68% for pandemics, and 69% for manmade disasters.
Table 1.
Perceptions of VA workforce preparednessa during major disasters (N = 4026)
Determinants of Workforce Disaster Preparedness Trainings
Table 2 shows the ORs and 95% CIs for all of the study covariates and the two main independent variables, predicting the desire for additional disaster preparedness training for natural disasters, pandemics, and manmade disasters. The findings indicate that VA employees with supervisory responsibilities, compared with employees with no supervisory responsibilities, were more likely to report the need for additional training (natural disasters OR 1.28, 95% CI 1.78–2.74; pandemics OR 1.33, 95% CI 1.11–1.60; manmade disasters OR 1.25, 95% CI 1.04–1.51). Similarly, VA employees with clinical duties were more likely to report the need for additional disaster preparedness training (natural disasters OR 1.24, 95% CI 1.04–1.47; pandemics OR 1.24, 95% CI 1.04–1.46; manmade disasters OR 1.24, 95% CI 1.04–1.47). Furthermore, respondents who have been employed at the VA for a longer period of time were less likely to report the need for additional training for natural disasters (OR 0.93, 95% CI 0.88–0.99) and pandemics (OR 0.92, 95% CI 0.86–0.98). For demographic characteristics, race and age were the two statistically significant covariates. Whites compared with non-Whites were less likely to report the need for additional disaster preparedness trainings: natural disasters (OR 0.54, 95% CI 0.45–0.65; pandemics OR 0.60, 95% CI 0.50–0.73; OR 0.57, 95% CI 0.46–0.69). For age, the two oldest age categories (55–64 and ≥ 65) compared with the youngest age group (18–44) were less likely to report the need for training. In terms of household characteristics, there were three statistically significant predictors. VA employees who reported that they were “not prepared at all” at home for any major disaster were more likely to report the need for additional training at work compared with those who reported that they were “well prepared” at home (natural disasters OR 1.85, 95% CI 1.39–2.46, pandemics OR 1.92, 95% CI 1.45–2.55, manmade disasters OR 1.94, 95% CI 1.44–2.61). VA employees who had plans to meet their family's healthcare needs in a major disaster and those responsible for assisting someone not living in their household were also more likely to report the need for additional disaster preparedness training at home. Finally, for the two main independent variables in this study, VA employees who reported that they understood their role in their facility’s overall disaster response, compared with those who reported that they do not understand their role, were less likely to report the need for additional disaster preparedness training for all types of disasters (natural disasters OR 0.25, 95% CI 0.21–0.31, pandemics OR 0.27, 95% CI 0.22–0.34, manmade disasters OR 0.28, 95% CI 0.22–0.34). VA employees who perceived their role in their facility’s overall disaster response to be important were more likely to report the need for additional trainings (natural disasters OR 2.20, 95% CI 1.78–2.74, pandemics OR 2.78, 95% CI 2.24–3.44, manmade disasters OR 3.13, 95% CI 2.50–3.92), however.
Table 2.
Determinants of workforce preparedness training for major disasters aWeight percent; strongly agree/agree.

Discussion
Few studies have examined the relation between sociodemographic and household characteristics and a desire for training; however, it has been found that healthcare workers with postgraduate education and those who have been employed for longer periods were more eager for training and the implementation of an emergency plan.23 Several studies have found that younger healthcare workers were more likely to be absent from work during disasters than their older colleagues.1,12 In contrast, clinicians23,24 and hospital staff with a military background1,23 and prior disaster experience1,15,25 have been shown to be more likely to respond or else felt better prepared to respond to a disaster. Improving household preparedness also has been shown to increase the willingness to respond or improve workforce preparedness.1,22 Furthermore, healthcare workers have expressed their desire for personal and family preparedness training.26
In this study, we found that VA employees who were “not prepared” at home were more likely to want additional training to prepare for major disasters; only 23% felt “well prepared at home” and 41% had a “plan to meet their family’s healthcare needs during a disaster.” As such, healthcare facilities should strongly consider personal preparedness training that encourages employees to put together basic disaster kits at home as well as written household disaster plans that address the needs of dependents and others whom they may be responsible for in the event that they have to report to work during a disaster. As US military veterans have been cited as having better household preparedness than the general population,27 employees who are veterans could be a valuable resource28 to lead training sessions for their colleagues on how to prepare their home for various disasters. Lastly, because supervisors, clinicians, and those who have been employed at the VA for a shorter period of time expressed their desire for additional training to prepare, annual education exercises and drills should be offered shortly after onboarding and should be both tailored to outline their specific response roles and designed to fit their busy schedules.
Healthcare workers who underwent disaster training or else believed that they were prepared to respond, have been reported to be more likely to report to work during a major disaster.1,12–15,24 Advanced training also has been shown to have a significant association with preparedness knowledge,7,10,11,29 such as improved understanding of the hospital’s disaster plan, incident command system, communication strategies, and their individual response roles, as well as increased confidence in self-protection practices and use of firefighting equipment.9,30 Most of the hospitals that did not report experiencing any substantial challenges during Hurricane Sandy in 2012 attributed their lack of problems to successful emergency planning and participation in preparedness activities.31 The majority of healthcare professionals have expressed their desire for additional training to prepare for a major disaster,12,14,22,23,26 including >60% of VA employees surveyed in this study. The most frequently cited training needs include information about their specific response roles,26,32 the incident command structure,8,26 their hospital’s disaster plan,7 infection control,15,26 personal preparedness,26 and triage.15 Large-scale exercises and disaster drills have been found to be an effective means of improving knowledge of disaster procedures and identifying problems with incident command, communications, triage, patient flow, security, and more.8,15 In addition, “just-in-time” training can be valuable for rapidly equipping healthcare workers with disaster-specific skills and improving knowledge just before or during disaster response.33,34
In particular, VA employees from this study want additional training to prepare for pandemics (63%) and manmade disasters (68%). Our finding about pandemics underscores the need for training about the novel coronavirus that causes COVID-19 as well as other emerging infectious diseases. The finding also is consistent with previous studies that found that healthcare workers are more willing and able to respond to natural disasters and less likely to respond to infectious outbreaks and chemical, biological, radiological, nuclear, or explosive events.13 The literature exploring chemical, biological, radiological, nuclear, or explosive events found that there were significant deficiencies in healthcare personnel training,8,14,35 and many hospitals did not have emergency plans or guidelines specific to radiological threats.35 Furthermore, many healthcare workers have reported that they have not received any, or very little, pandemic-related training,12–14 and the fear of becoming ill or contaminated12,13,35 and fear of unknown agents35 have been widely cited as a common influencer regarding the willingness to respond during a disaster. As such, future training should strive to improve knowledge and skills in disaster preparedness and response, with an emphasis on pandemics and manmade disasters. Our findings support recommendations for healthcare facilities to broadly disseminate their disaster plan, which should include specific information and instructions for each disaster type, to all employees. Annual education should refamiliarize healthcare workers with these plans and, as generally recommended, address common biological, chemical, and radiological agents and emerging infectious diseases. It also should include information regarding how to protect themselves and their family members, so that they become less fearful and more likely to report to work. Although just-in-time training can be an efficient solution for rapidly addressing competencies, knowledge, and skills during disaster response, training for a pandemic may require continued, periodic refresher courses, as infectious disease outbreaks often have uncertain and prolonged timelines.
One of the most significant factors associated with an increased likelihood of reporting to work during a disaster is having an individual response role.1,14,26,36 For example, one study found that pediatric nurse practitioners with a specified role in the workplace disaster plan were three to five times more likely to respond during a disaster than those without a specified role.1 Healthcare workers with a higher perceived importance in an emergency response role also were more willing to report to work during a disaster.24,26 In fact, one element of performance standards for TJC accreditation is that hospital staff be “trained and knowledgeable about their roles in the hospital’s programs for fire safety, security, hazardous materials, and emergencies.”37 Furthermore, the World Health Organization’s guide to preparing hospitals for epidemics recommends that all staff members, particularly those involved in infection prevention and control, prepare “job action sheets,” which describe their roles and tasks in an emergency situation.38 This study found that those who were less likely to “understand their role” in their medical facility’s response to a disaster were more likely to want additional training, and those who believed their role in disaster response was important were more likely to want training to prepare. Because only approximately half of all VA employees reported understanding their role during response to a disaster, training should outline individual response roles, especially when responding to a pandemic or manmade disaster. Annual education also should stress the importance of their roles during disaster response. Although it may be difficult to assign specific, predetermined roles for all of the possible disasters, a set of potential roles should be defined and clearly communicated to all employees. The use of simulations and drills has been shown to help define individual response roles and improve self-efficacy, collegiality, and perceived role importance.25,36
The results of this study may not be generalizable outside the VA; however, the VA healthcare workforce is similar to other healthcare workers in terms of its sociodemographic characteristics as well as the type, amount, and scope of disaster preparedness training. For example, the applicability of emergency preparedness requirements set by TJC and state-level professional standards boards would be the same for both VA and non-VA healthcare employees. In addition, perceptions of workforce preparedness may not reflect objective readiness for disasters, so future surveys should examine perceptions in relation to actual response metrics; in VA, such studies could focus on the Comprehensive Emergency Management Program’s “mission areas” of hospital preparedness.39,40
Conclusions
Clinicians and nonclinical staff play important roles in disaster response; accordingly, improving knowledge and skills about preparedness for both groups is essential for a nation’s effective response to a major disaster. VA employees in this study expressed a desire for additional disaster preparedness training for all three types of disasters (natural, pandemic, manmade). The findings point to the need for additional hospital-based education and training strategies to boost employees’ willingness and ability to respond.
This study suggests that training should better define employees’ individual response roles and the importance of their roles during response, particularly during pandemics and manmade disasters. Interventions also should aim to improve hospital staff’s household preparedness, which could include instructions about preparing disaster kits and developing written disaster plans to address the needs of their dependents. Understanding what factors influence the desire for additional training can assist hospitals and other healthcare facilities to create targeted trainings and educational materials to better prepare the ability of the healthcare system to respond effectively and efficiently during crises.
Acknowledgment
The authors thank Advanced Survey Design for their contributions to this project.
Footnotes
This material is based upon work supported by the US Department of Veterans Affairs, Veterans Health Administration, Office of Patient Care Services. The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the US Department of Veterans Affairs or the United States government.
Funding for the Veterans Emergency Management Evaluation Center is provided by the US Department of Veterans Affairs (XVA 65-077). The funder did not participate in the design of the study, collection, analysis, and interpretation of data or writing this manuscript, but will support open access publishing.
The authors did not report any financial relationships or conflicts of interest.
Contributor Information
Claudia Der-Martirosian, Email: Claudia.Der-Martirosian@va.gov.
Aram Dobalian, Email: Aram.Dobalian@va.gov.
References
- 1.Goodhue CJ Burke RV Ferrer RR, et al. Willingness to respond in a disaster: a pediatric nurse practitioner national survey. J Pediatr Health Care 2012;26:e7–e20. [DOI] [PubMed] [Google Scholar]
- 2.Toner E. Healthcare preparedness: saving lives. Health Secur 2017;15:8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dobalian A, Callis R, Davey VJ. Evolution of the Veterans Health Administration’s role in emergency management since September 11, 2001. Disaster Med Public Health Prep 2011;5(suppl 2):S182–S184. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services . State Operations Manual: Appendix Z- Emergency Preparedness for All Provider and Certified Supplier Types Interpretive Guidance. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_z_emergprep.pdf. Published February 2, 2020. Accessed June 2, 2020.
- 5.The Joint Commission . Revised Emergency Preparedness Standards for Federally Qualified Health Centers. https://www.jointcommission.org/-/media/ff56866a5b7b4ca886f3c401ede0b103.ashx. Published March 2020. Accessed July 24, 2020.
- 6.Di Marco J . Hospital Accreditation Facts to Know. https://www.chthealthcare.com/blog/hospital-accreditation. Published March 9, 2017. Accessed July 24, 2020.
- 7.Bistaraki A, Waddington K, Galanis P. The effectiveness of a disaster training programme for healthcare workers in Greece. Int Nurs Rev 2011;58:341–346. [DOI] [PubMed] [Google Scholar]
- 8.Hsu CE Mas FS Jacobson H, et al. Assessing the readiness and training needs of non-urban physicians in public health emergency and response. Disaster Manag Response 2005;3:106–111. [DOI] [PubMed] [Google Scholar]
- 9.Williams J, Nocera M, Casteel C. The effectiveness of disaster training for health care workers: a systematic review. Ann Emerg Med 2008;52:211–222, 222.e1–222.e2. [DOI] [PubMed] [Google Scholar]
- 10.Henning KJ Brennan PJ Hoegg C, et al. Health system preparedness for bioterrorism: bringing the tabletop to the hospital. Infect Control Hosp Epidemiol 2004;25:146–155. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs-Wingo JL Schlegelmilch J Berliner M, et al. Emergency preparedness training for hospital nursing staff, New York City, 2012–2016. J Nurs Scholarsh 2019;51:81–87. [DOI] [PubMed] [Google Scholar]
- 12.Bell MA Dake JA Price JH, et al. A national survey of emergency nurses and avian influenza threat. J Emerg Nurs 2014;40:212–295. [DOI] [PubMed] [Google Scholar]
- 13.Gershon RR Magda LA Qureshi KA, et al. Factors associated with the ability and willingness of essential workers to report to duty during a pandemic. J Occup Environ Med 2010;52:995–1003. [DOI] [PubMed] [Google Scholar]
- 14.Hayanga HK Barnett DJ Shallow NR, et al. Anesthesiologists and disaster medicine: a needs assessment for education and training and reported willingness to respond. Anesth Analg 2017;124:1662–1669. [DOI] [PubMed] [Google Scholar]
- 15.Labrague LJ Hammad K Gloe DS, et al. Disaster preparedness among nurses: a systematic review of literature. Int Nurs Rev 2018;65:41–53. [DOI] [PubMed] [Google Scholar]
- 16.US Department of Veterans Affairs . Office of Nursing Services (ONS). http://www.va.gov/nursing/workforce/workforce.asp. Published March 25, 2020. Accessed June 5, 2020.
- 17.Bossert WH, Dobalian A. VA’s involvement in the aftermath of the 9/11 attacks. Disaster Med Public Health Prep 2011;5(suppl 2):S167. [DOI] [PubMed] [Google Scholar]
- 18.Claver M Friedman D Dobalian A, et al. The role of Veterans Affairs in emergency management: a systematic literature review. PLoS Curr 2012;4:e198d344bc40a75f927c9bc5024279815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Department of Veterans Affairs . VA fourth mission summary. https://www.va.gov/health/coronavirus/statesupport.asp. Published June 5, 2020. Accessed June 6, 2020.
- 20.Dobalian A, Balut MD, Der-Martirosian C. Workforce preparedness for disasters: perceptions of clinical and non-clinical staff at the U.S. Department of Veterans Affairs. BMC Public Health 2020;20:1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balut MD, Der-Martirosian C, Dobalian A. Determinants of workforce preparedness during pandemics among healthcare workers at the U.S. Department of Veterans Affairs. J Prim Care Community Health 2021;12:21501327211004738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Der-Martirosian C, Balut MD, Dobalian A. Household preparedness and perceptions of workforce preparedness during pandemics: a healthcare employee survey at the U.S. Department of Veterans Affairs. Disaster Med Public Health Prep 2021. DOI: 10.1017/dmp.2021.198. [DOI] [PubMed] [Google Scholar]
- 23.Naser WN, Saleem HB. Emergency and disaster management training; knowledge and attitude of Yemeni health professionals—a cross-sectional study. BMC Emerg Med 2018;18:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma X He Z Wang Y, et al. Knowledge and attitudes of healthcare workers in Chinese intensive care units regarding 2009 H1N1 influenza pandemic. BMC Infect Dis 2011;11:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baack S, Alfred D. Nurses’ preparedness and perceived competence in managing disasters. J Nurs Scholarsh 2013;45:281–287. [DOI] [PubMed] [Google Scholar]
- 26.Stergachis A Garberson L Lien O, et al. Health care workers’ ability and willingness to report to work during public health emergencies. Disaster Med Public Health Prep 2011;5:300–308. [DOI] [PubMed] [Google Scholar]
- 27.Der-Martirosian C Strine T Atia M, et al. General household emergency preparedness: a comparison between veterans and nonveterans. Prehosp Disaster Med 2014;29:134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Der-Martirosian C Schmitz S Wyte-Lake T, et al. US military veterans: an untapped resource as disaster volunteers. Am J Public Health 2019;109(S4):S263–S264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qureshi KA Merrill JA Gershon RR, et al. Emergency preparedness training for public health nurses: a pilot study. J Urban Health 2002;79:413–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blessman J Skupski J Jamil M, et al. Barriers to at-home-preparedness in public health employees: implications for disaster preparedness training. J Occup Environ Med 2007;49:318–326. [DOI] [PubMed] [Google Scholar]
- 31.US Department of Health and Human Services, Office of the Inspector General . Hospital emergency preparedness and response during Superstorm Sandy. https://www.hsdl.org/?view&did=757768. Published September 16, 2014. Accessed June 6, 2020.
- 32.Niska RW, Shimizu IM. Hospital preparedness for emergency response: United States, 2008. Natl Health Stat Rep 2011;(37):1–14. [PubMed] [Google Scholar]
- 33.Ragazzoni L Barco A Echeverri L, et al. Just-in-time training in a tertiary referral hospital during the COVID-19 pandemic in Italy. Acad Med 2021;96:336–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stoler GB Johnston JR Stevenson JA, et al. Preparing emergency personnel in dialysis: a just-in-time training program for additional staffing during disasters. Disaster Med Public Health Prep 2013;7:272–277. [DOI] [PubMed] [Google Scholar]
- 35.Becker SM, Middleton SA. Improving hospital preparedness for radiological terrorism: perspectives from emergency department physicians and nurses. Disaster Med Public Health Prep. 2008;2:174–184. [DOI] [PubMed] [Google Scholar]
- 36.Whetzel E Walker-Cillo G Chan GK, et al. Emergency nurse perceptions of individual and facility emergency preparedness. J Emerg Nurs 2013;39:46–52. [DOI] [PubMed] [Google Scholar]
- 37.Joint Commission International . Joint Commission International Accreditation Standards for Hospitals: including standards for academic medical center hospitals, 6th edition. https://www.jointcommissioninternational.org/-/media/jci/jci-documents/accreditation/hospital-and-amc/learn/jci_standards_only_6th_ed_hospital.pdf?db=web&hash=E2D36799998C7EE27C59CFF3131EE0A7&hash=E2D36799998C7EE27C59CFF3131EE0A7. Published July 1, 2017. Accessed June 5, 2020.
- 38.World Health Organization . Hospital preparedness for epidemics. https://www.who.int/publications/i/item/hospital-preparedness-for-epidemics. Published April 4, 2014. Accessed June 10, 2020.
- 39.Der-Martirosian C Radcliff TA Gable AR, et al. Assessing hospital disaster readiness over time at the US Department of Veterans Affairs. Prehosp Disaster Med 2017;32:46–57. [DOI] [PubMed] [Google Scholar]
- 40.Dobalian A Stein JA Radcliff TA, et al. Developing valid measures of emergency management capabilities within US Department of Veterans Affairs hospitals. Prehosp Disaster Med 2016;31:475–84. [DOI] [PubMed] [Google Scholar]


