Abstract
Point-of-care ultrasonography (POCUS) is a limited ultrasound study performed by the clinician at the bedside as a component or an adjunct to physical examination. POCUS has multiple applications in nephrology practice, including evaluation of obstructive uropathy, objective assessment of volume status, arteriovenous access assessment, and procedural guidance. However, unlike specialties such as emergency medicine, POCUS training is not yet integrated into most nephrology fellowship curricula, and the sonographic applications taught vary widely among fellowship programs. In this article, we have used our institutional experience to provide a roadmap or blueprint for nephrology programs looking to create a POCUS program. We provide an overview of the curriculum, including the basic organization, applications taught, online resources, milestone development, and quality assessment. We also discuss the nuances of POCUS workflow and perspectives on billing for these limited studies. In addition, we share the evaluation forms and sample documentation we use in our program. Future support, in the form of endorsed nephrology society guidelines, is needed before POCUS training is universally incorporated across nephrology fellowship programs.
Keywords: clinical nephrology, billing, curriculum, nephrology, POCUS, point-of-care ultrasound, quality assessment
Introduction
Point-of-care ultrasonography (POCUS) is a focused ultrasound examination performed and interpreted by the clinician at the patient’s bedside as a diagnostic aid or to guide procedures. Diagnostic POCUS is intended to answer focused clinical questions and serve as an adjunct to conventional physical examination in formulating a management plan. POCUS training is well established in specialties such as emergency medicine, where it is a core component of Accreditation Council for Graduate Medical Education program requirements for residency training (1). With increased recognition of its feasibility and clinical utility, POCUS is increasingly integrated into internal medicine residency training and undergraduate medical curricula (2,3). Once confined to procedural guidance such as dialysis catheter placement, the adoption of diagnostic POCUS has been expanding in nephrology, partly sparked by the data supporting the role of lung ultrasound in patients with ESKD (4,5). Multiorgan POCUS also aids in the objective assessment of hemodynamics, which is critical when caring for patients with complex fluid and electrolyte aberrancies (6). Despite the stated applications and learners’ desires for additional instruction in sonography, POCUS training in nephrology fellowship programs largely remains a work in progress (7). Scarcity of POCUS-trained faulty, lack of formal guidelines on the scope of practice, and unfamiliarity with program administration among educators are among the barriers for incorporation of this skill. We have previously proposed a model POCUS curriculum for nephrology fellows on the basis of our institutional experience (8). Building on that framework and lessons learned from internal quality assessment, we have created a structured collaborative curriculum in two nephrology divisions namely, the Medical College of Wisconsin (MCW) and University of Florida (UF). In this article, we outline the content and execution of our longitudinal POCUS curriculum to serve as a guide for nephrology fellowship programs relatively new to this terrain.
The Curricular Framework and Rationale
Because there is no universally accepted POCUS curriculum, and sonographic applications that are taught vary significantly among specialties, there exists a huge heterogeneity in the duration of training (9–11). Previously, we demonstrated that two half-day teaching sessions can significantly increase the confidence of internal medicine residents to identify common abnormalities on renal ultrasound (12). However, the retention of knowledge is poor after short introductory courses if the initial training is not followed by continued practice (13). Learning POCUS is similar to that of acquiring physical examination skills, where the learner is not only expected to recognize the findings, but also use them to inform patient care. As such, it is conceivable that a longitudinal training coupled with hands-on experience may result in better proficiency. Therefore, our curriculum spans the 2-year nephrology fellowship and incorporates a variety of teaching methods including didactic lectures, online material, and hands-on training. We adopted the indication, acquisition, interpretation, and medical decision-making (I-AIM) model as a guide to develop the content of these individual components and competency assessment (14). Indication means the learner must be able to formulate an appropriate focused question to be answered by the scan; acquisition represents obtaining high-quality images by using proper scanning protocols; interpretation involves using a systematic approach to identify and describe the findings; and medical decision making signifies integration of these sonographic findings with history and clinical signs to guide management.
Implementation
Curricula at both institutions (MCW and UF) follow the same overall structure, albeit with minor variations in execution contingent on the local workflow. The following description of the key components reflects how the program is implemented at MCW.
Lectures
The didactics include a series of ten 45–60-minute lectures spread out over 6 months delivered in person and/or through an online platform (Zoom). These lectures are standardized to cover the core nephrology-related sonography topics as listed below and are repeated every academic year. Integration of the online platform helps diversify the lecturers with a variety of backgrounds and expertise, and to strengthen interinstitutional collaborative efforts that will facilitate the exchange of knowledge and experience.
-
1.
Ultrasound physics and knobology
Ultrasound wave properties, transducer types
Introduction to modes: B, M, color flow, power Doppler, spectral Doppler
Image optimization: depth, zoom, gain, time gain compensation
Image orientation: organ presets, standard conventions
Basics of image interpretation: acoustic impedance, relative echogenicity of various tissues
Common ultrasound artifacts, including acoustic shadowing, acoustic enhancement, mirror image, reverberation, ring-down, and twinkle artifacts
-
2.
Renal ultrasound
Technique: probe selection, positioning, and description of movements
Organ anatomy: gross and sonographic correlation in long and short axes
Kidney size and appearance: length, cortical and parenchymal thickness, cortical echogenicity
Core pathologies: hydronephrosis, stone, cyst, mass, free fluid in hepatorenal and splenorenal recesses
Less common abnormalities: infections, vascular malformations, congenital abnormalities, and anatomic variants
-
3.
Renal allograft and urinary bladder ultrasound
Technique: probe selection, positioning, and description of movements
Allograft anatomy: expected differences compared with native kidney (e.g., prominent collecting system), proximity to bladder and pelvic organs
Allograft core pathologies: hydronephrosis, perinephric collections, basic evaluation of vascular anastomosis, and resistive index
Urinary bladder anatomy: gross and sonographic correlation in long and short axes
Bladder volume calculation, urinary retention, Foley catheter malposition, differentiating pelvic ascites from urine, prostatomegaly
-
4.
Lung ultrasound
Technique: probe selection, positioning, and description of movements
Sonographic zones of evaluation: rationale behind the existence of multiple scanning systems, correlation between various techniques
A and B lines: physics underlying artifact generation, i.e., reverberations and ring-down, cardiogenic versus pneumogenic B lines
Pleural effusion: simple effusion, spine sign, recognition of complex/exudative effusions
Consolidations: differentiating lobar pneumonia and atelectasis, static and dynamic air bronchograms, subpleural consolidations
-
5.
Focused cardiac ultrasound
Rationale and limitations
Technique: probe and preset selection, probe positioning to acquire basic cardiac views namely, parasternal long axis, parasternal short axis, apical 4 and 5 chamber, subxiphoid 4 chamber, and inferior vena cava
Utility of M-mode and color Doppler
Cardiac anatomy: gross and sonographic correlation of the basic views
Evaluation of 5 Es: ejection (left and right ventricular systolic function including M-mode parameters), effusion (pericardial effusion from different windows, quantification), equality (identification of gross alterations in cardiac chamber size), entrance (estimation of right atrial pressure using inferior vena cava), and exit (evaluation of the aortic root in a patient who is hemodynamically unstable) (15)
Pitfalls of isolated inferior vena cava ultrasound
-
6.
Integrative assessment of fluid volume status
Rationale behind using multiorgan POCUS for objective evaluation of fluid status
Patient studies illustrating the role of integrating findings from focused cardiac ultrasound, lung ultrasound, and limited abdomen to assess fluid status
Limitations of basic POCUS and introduction to hemodynamic assessment using Doppler ultrasound
-
7.
Sonographic evaluation of the dialysis access
Principles of spectral Doppler focusing on pulsed wave Doppler, scale adjustment, aliasing, angle correction
Anatomy of vascular access: gross and sonographic correlation in long and short axes
Technique: probe selection, measurement of depth, diameter, volume flow
Core pathologies: pseudoaneurysm, hematoma, thrombosis, narrowing and turbulent flow; assessment of maturity of a newly placed access. Detailed assessment of stenosis/vein mapping is beyond the scope of POCUS
Peritoneal dialysis access: abdominal wall anatomy, sonographic appearance of normal catheter and cuff, tunnel infection, abscess, pericatheter leaks
-
8.
Limited Doppler echocardiography
Principles of cardiac Doppler: continuous and pulsed wave Doppler, tissue velocity imaging
Technique: appropriate cardiac view and correct placement of Doppler gate and/or cursor to obtain the chosen parameter
Doppler parameters: left ventricular outflow tract velocity time integral, cardiac output, right ventricular outflow tract velocity time integral and waveform assessment, pulmonary artery systolic pressure, mitral inflow Doppler including E/A ratio, E-wave deceleration time, mitral annular E’, tricuspid annular S’
-
9.
Quantification of venous congestion using Doppler ultrasound
-
•
Rationale behind venous congestion assessment, effect of fluid overload on downstream organs, overview of venous excess Doppler ultrasound (VExUS)
-
•
Technique: probe selection, preset, positioning, standard, and alternative imaging windows
-
•
Components of VExUS:
-
o
Hepatic vein waveform: genesis, nomenclature of normal waves, transformation with increasing right atrial pressure, pitfalls, utility of simultaneous electrocardiographic trace
-
o
Portal vein waveform: normal appearance, transformation with increasing right atrial pressure, pitfalls
-
o
Renal parenchymal vessels waveform: normal appearance, transformation with increasing right atrial pressure, pitfalls
-
o
-
•
Three to four patient studies illustrating the role of integrating findings from Doppler echocardiography, VExUS, and lung ultrasound
-
•
-
10.
Ultrasound-guided procedures and others
Temporary hemodialysis catheter placement: probe selection, vessel selection, visualization of the needle tip, technique of catheter insertion, confirmation of correct placement by cardiac ultrasound (rapid atrial swirl sign)
Renal biopsy (native and transplant): probe selection, site selection, visualization of the renal cortex, vasculature, needle tip and surrounding anatomy (e.g., bowel loop interference in the case of allograft), evaluation of postbiopsy hematoma/Doppler signs of active bleeding along the needle track
Others: brief overview of ocular, soft tissue, musculoskeletal ultrasound pertinent to nephrology including evaluation of papilledema, cellulitis/abscess, deep vein thrombosis, and crystalline arthropathies
Online Resources
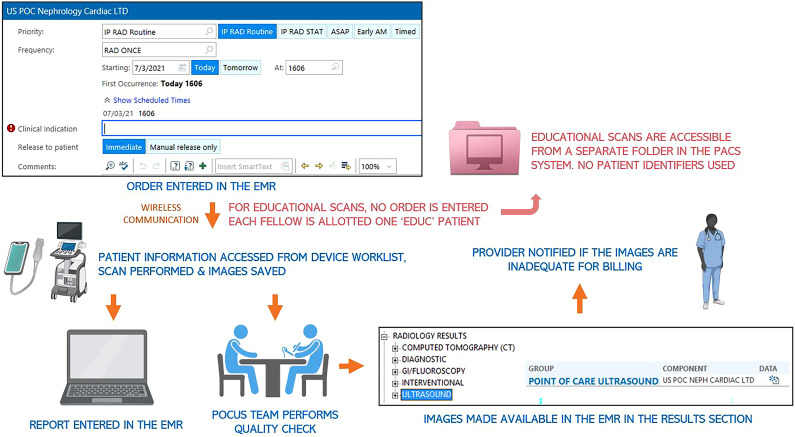
NephroPOCUS.com, a nephrologist-designed website recognized by the American Society of Nephrology as an innovative teaching tool, is used as a primary resource to supplement the didactics (16,17). It consists of recorded lectures, short videos discussing POCUS pearls and pitfalls, self-assessment quizzes, infographics, and brief clinical vignettes organized by the topic (Figure 1). In addition, literature relevant to POCUS is presented in the form of visual abstracts, which provide a concise, pictorial, and visual summary of each article. Once familiar with the basics, trainees are encouraged to take advantage of the multitude of open-access POCUS-learning resources geared toward various specialties (18).
Figure 1.
Pictorial representation of the online point-of-care ultrasonography learning tool, NephroPOCUS.com. POCUS, point-of-care ultrasonography.
Ultrasound Equipment
The division of nephrology has a dedicated cart-based portable ultrasound machine equipped with the necessary options for the sonographic applications taught including spectral Doppler, tissue velocity imaging, and electrocardiogram cables. In addition, two ultraportable/hand-held ultrasound (HHU) devices are available for use by fellows on clinical rotations.
It is of note that although HHU devices are gaining popularity because of the lower pricing and user-friendly interfaces, their image quality could be suboptimal for certain sonographic applications (19). Most such devices do not offer a reliable spectral Doppler option, which is essential for evaluation of venous congestion, cardiac output, and dialysis vascular access volume flow. Moreover, because most of these devices can be connected to personal phones and tablets, concerns about patient privacy may arise. Therefore, it would be prudent for the division leadership to review institutional policies and discuss with the hospital information technology department before investing in such devices. The advantage of HHU devices is their enhanced portability; they can be carried to outpatient dialysis units and outreach clinics. The image quality is adequate for basic applications, such as the detection of extravascular lung water, pleural effusion, excluding hydronephrosis, pericardial effusion etc.
Hands-on Training
Regardless of how well the lectures are designed, the scanning technique is best taught at the bedside. Introductory scanning sessions are held in a clinic room or medical school simulation laboratory when feasible, where fellows practice on volunteers or standardized patients. Fellows are then allowed to scan patients under direct supervision of the POCUS faculty until they complete ≥10 examinations per application, and on their own thereafter. This is an arbitrary number to ensure basic image acquisition skills, not a measure of competence. Supervision is then provided on as-needed basis, tailored to the needs of individual fellows. For example, fellows with some ultrasound training received during their residency or at medical school may require less direct supervision compared with a POCUS-naïve fellow. Review of the images acquired by fellows also helps to provide feedback about correct transducer positioning and assess their progress.
Most of the hands-on exposure occurs when the fellow is on a renal consulting service, where they can ask focused clinical questions, obtain answers using POCUS, and directly integrate the findings into their management plan. In addition, 1-week POCUS electives are offered to those interested in further solidifying their skills. These electives are typically dedicated to the practice of Doppler echocardiography and venous congestion assessment. Elective rotations are arranged with vascular access surgeons to provide exposure to complications of arteriovenous access and their sonographic assessment. Because most of the fellows are trained in ultrasound-guided temporary dialysis catheter placement during internal medicine residency, graded supervision is provided after an initial assessment. At both MCW and UF, renal biopsies are performed in the radiology suite assisted by a sonographer; the fellows perform biopsy without having to simultaneously operate the ultrasound machine.
Personnel
Availability of ultrasound-skilled faculty within the division is vital for a successful POCUS program. We have two core POCUS faculty entrusted with administration of the program at each institution, one of them designated as the POCUS director. Their time is protected by a full time equivalent of 0.15–0.3 to be able to lead this initiative. The duties of the director broadly include development of educational material, direct and indirect supervision, maintaining equipment, performing quality assessment, providing learner feedback, ensuring proper documentation, guiding scholarly activity, and training other faculty in the division.
Nephrology divisions with no ultrasound expertise should consider collaborating with other POCUS-performing specialties within the institution such as emergency medicine, anesthesiology, critical care medicine, etc. Identifying nephrology faculty with an interest in POCUS and providing them with time to complete a rotation/mini fellowship with institutional experts is a more viable option than completely relying on other specialists to train nephrology fellows. In our experience, rotating with sonographers is also a beneficial approach to enhance the practice and acquire confidence in scanning. Regardless of baseline expertise, POCUS faculty are expected to continuously improve their knowledge and skills through continuing medical education activities.
Quality Assessment and Milestones
Quality assessment is an essential component of a POCUS program to ensure diagnostic quality of the images and to monitor the progress of trainees. We require fellows to save all of the images, whether they perform educational or clinically indicated scans. Educational scan is a study performed for learning purposes with patients’ permission, usually to replicate abnormal findings reported on a radiology-performed scan. Saving images helps the faculty to review them later and provide constructive feedback about the acquisition aspects, such as anatomy, gain, depth, orientation, Doppler settings, etc. A five-point feedback scale is used to rate the image quality and provide feedback, which is partially on the basis of the American College of Emergency Physicians guidelines (20). In addition to formal image archiving, fellows are encouraged to maintain individual portfolios by saving the deidentified images to SonoClipShare, a cloud-based image storing platform, which could prove helpful when applying for external certifications (21). This system allows sharing the images with the faculty and the receipt of feedback. By the end of the fellowship training, each fellow is expected to have performed a minimum of 40–50 scans per application. This number has been synthesized from the recommendations of various professional societies as we outlined before (8). It is of special note that although meeting the minimum criteria facilitates certification and hospital credentialing, it does not guarantee competence. Similar to any other skill, continued practice is the key to mastery. In addition to image review, a formal direct observation feedback is provided every 6 months for basic applications, and at the end of 18 months for Doppler applications. The forms we use can be found in the Supplemental Appendix 1.
We use a simplified milestone system to assess the progress and provide periodic learner feedback (Table 1). Briefly, the learning objectives are divided into three levels of increasing proficiency. Fellows are expected to attain level I approximately 6 months into their fellowship training (or 9 months if POCUS is not a part of the orientation schedule), level II by the next 6 months, and level III by the end of fellowship training.
Table 1.
Expected milestones according to level of proficiency in point-of-care ultrasonography
| Competency | Level I | Level II | Level III |
|---|---|---|---|
| Technical skills and image interpretation | • Acquire optimal greyscale (+ color Doppler where indicated) images of kidney, lung, vascular access • Guide internal jugular/femoral temporary dialysis access placement • Distinguish normal from abnormal structures |
• Acquire optimal greyscale and color Doppler images of the heart, including IVC • Identify common abnormalities |
• Acquire optimal spectral Doppler images of the heart, abdominal veins, vascular access • Identify less commonly encountered findings |
| Practice-based learning and professionalism | • Demonstrate respect for patients and families, their privacy and explain indication(s) for scanning • Notify POCUS faculty of the scans being performed in a timely manner • Solicit feedback from staff and colleagues to improve performance • Appropriately handle and store the equipment |
• Identify gaps in knowledge and skills, actively seek opportunities to improve performance • Present patients who are POCUS based and relevant literature in nephrology conference/journal club • Take responsibility for scans, communicate incidental findings to POCUS faculty/consulting teams in a timely manner |
• Apply clinical practice guidelines and available data to formulate management plan using POCUS findings • Document POCUS findings in the chart in accordance with billing compliance and policies • Present POCUS-based research (including case reports) in a professional meeting and/or publish in a medical journal |
IVC, inferior vena cava; POCUS, point-of-care ultrasonography.
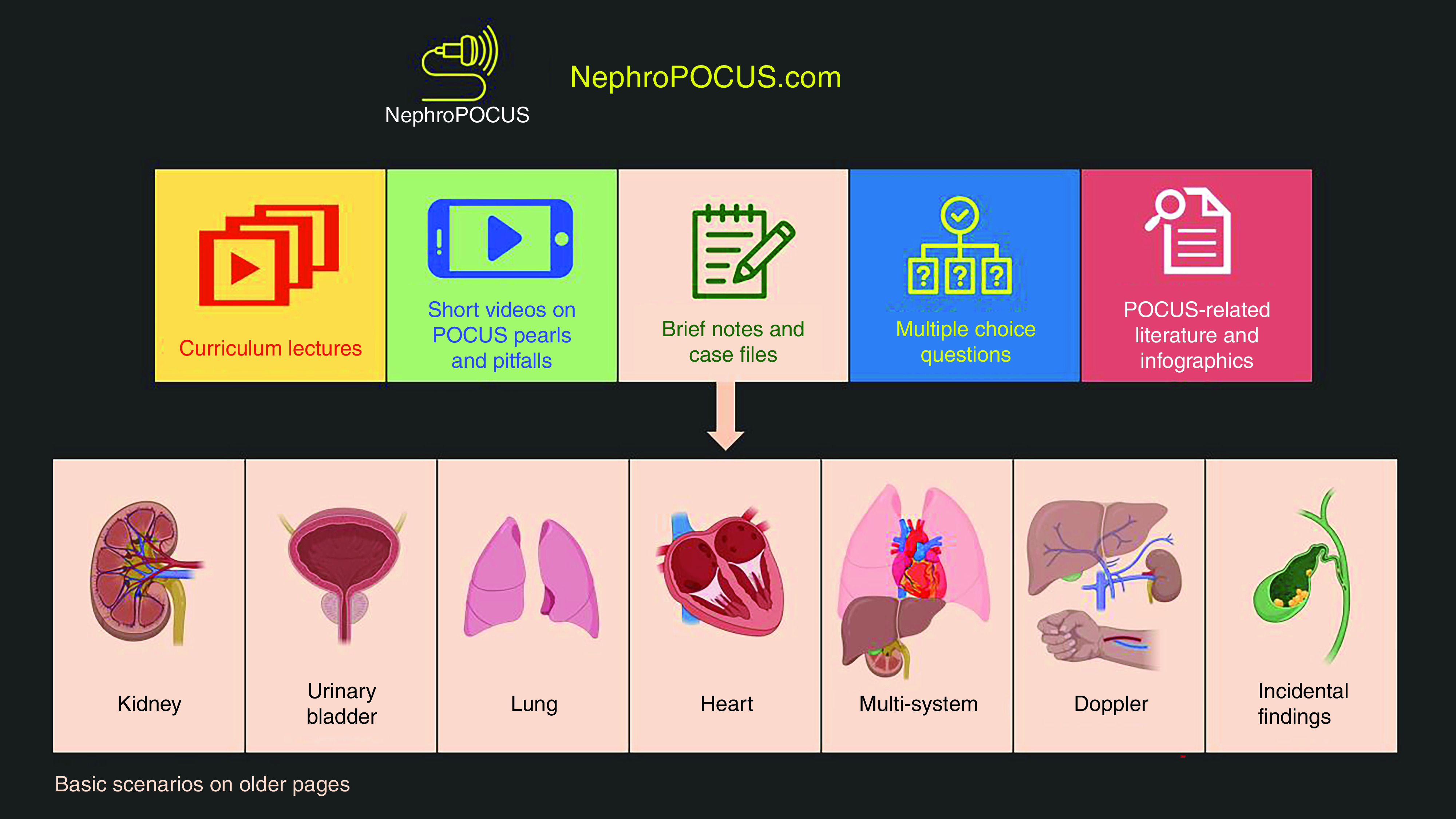
Workflow and Billing
We have designed a dedicated image archiving system that is necessary for billing compliance (22). Clinically indicated POCUS studies are billable as limited scans with proper documentation; the revenue generated may help offset the cost of equipment over time. Our workflow is illustrated in Figure 2. Briefly, a customized nephrology-specific POCUS order is placed in the patient’s electronic chart, which is wirelessly transmitted to the ultrasound machines we use (including HHU devices). This allows us to find the patient information from the device worklist, perform the scan, and save images, which are then transmitted to the picture archiving and communication system (PACS). A separate POCUS note is placed in the chart that contains indications for the scan(s), operator name, findings, and interpretation. A sample note is shown in Supplemental Appendix 2. Froedtert Hospital, which is the primary teaching affiliate of MCW has a dedicated POCUS team comprising of experienced sonographers who review all of the POCUS images performed in the hospital to ensure they meet billing requirements before uploading in the patient’s chart. Images are available in the results section of the chart analogous to radiology-performed scans.
Figure 2.
Workflow of point-of-care ultrasound examinations at our institution. Educ patient indicates space with sham-patient identifier unique to each fellow, under which multiple educational scans can be saved. EMR, electronic medical record; PACS, picture archiving and communication system.
The Current Procedural Terminology codes we commonly use and their descriptors are summarized below (Box 1).
Box 1. Commonly used Current Procedural Terminology codes
76604 Ultrasound, chest (includes mediastinum).
-
93308 Echocardiography, transthoracic (two-dimensional) includes M-mode recording; when performed, follow-up, or limited study.
+93321 (add-on) Doppler echocardiography, pulsed wave and/or continuous wave with spectral display; follow-up or limited.
+93325 (add-on) Doppler echocardiography color flow velocity mapping; limited.
76705 Abdominal ultrasound; limited (e.g., single organ, quadrant, follow-up).
76775 Ultrasound retroperitoneal (e.g., renal, aorta, nodes); limited.
93976 Duplex scan of arterial inflow and venous outflow of abdominal, pelvic, scrotal contents, and/or retroperitoneal organs; limited (used for venous congestion assessment in selected patients).
93990 Duplex scan of hemodialysis access (including arterial inflow, body of access, and venous outflow).
+76937 (add-on to dialysis catheter insertion procedure code) Ultrasound guidance for vascular access requiring ultrasound evaluation of potential access sites, documentation of selected vessel patency, real time visualization of vascular needle entry, with permanent recording and reporting.
As previously mentioned, we perform renal biopsies in the radiology suite and hence do not bill for ultrasound guidance. We also do not bill at the outpatient dialysis units.
The POCUS director and the core faculty are credentialed to perform and bill for the images. Because there are no uniform certification standards for nephrology-related POCUS currently, hospitals typically rely on the American College of Emergency Physicians guidelines and external certifications to grant privileges. In some patients, “conditional” privileges may be granted, where the renewal is contingent on periodic quality assessment by institutional experts. At MCW, the POCUS director has completed the Examination of Special Competence in Critical Care Echocardiography administered by National Board of Echocardiography, which facilitated credentialing, particularly for the Doppler applications.
Although some clinicians express concerns about missed findings and consequent legal implications as a barrier to wide application of POCUS (23), so far, there is no indication in the literature that missed findings on focused or limited ultrasound examinations resulted in an adverse legal action against physicians. Instead, failure to perform POCUS in a timely manner has led to lawsuits (24–27). We believe that saving the images and billing stewardship will promote a culture of responsible documentation and seeking timely expert consultation when there is uncertainty about the findings.
Future Directions
POCUS is an invaluable addition to the armamentarium of a nephrologist. It provides insights into pathophysiology at the bedside, enhances patient care and satisfaction, and has the potential to reduce the health care cost burden (28–33). Moreover, a longitudinal POCUS curriculum can serve as a complement to other evolving subspecialties within nephrology, such as cardiorenal medicine (34,35). Having formal guidelines and support from the professional societies governing nephrology specialty is vital for development of universal standards in POCUS training. To address this need, American Society of Diagnostic and Interventional Nephrology will release certification requirements for POCUS in nephrology in the later part of 2021. We believe that establishing a taskforce to achieve consensus on the scope of POCUS in nephrology and competency evaluation would streamline the standardization process. Future research should focus on studying the effect of POCUS curriculum and various teaching techniques on trainee competence. It would also be interesting to explore whether incorporation of POCUS into nephrology electives will have a salutary effect on the interest level of medical students/residents in the specialty.
Disclosures
A. Kazory reports consultancy agreements with CHF Solutions (NuWellis), Inc.; reports being on the Scientific Advisory Board of Baxter, a consultant for Horizon, Relypsa, and W.L. Gore; reports receiving honoraria from Baxter, CHF Solutions (NuWellis), Horizon, Relypsa, and W.L. Gore; reports being a scientific advisor or member of CHF Solutions, the International Academy of Cardiology, and the World Congress on Heart Disease, and the Medical Advisory Board of W.L. Gore Inc.; and reports other interests/relationships as DCI Inc., as Medical Director. All remaining authors have nothing to disclose.
Funding
None.
Author Contributions
B. Bhasin, A. Kazory, A. Koratala, and O. Olaoye conceptualized the study; A. Kazory and A. Koratala were responsible for the investigation; B. Bhasin, A. Koratala, and O. Olaoye were responsible for the methodology; A. Koratala and O. Olaoye were responsible for the project administration; A. Kazory and A. Koratala were responsible for the resources; A. Kazory provided supervision; B. Bhasin, A. Kazory, and O. Olaoye reviewed and edited the manuscript; and A. Koratala was responsible for the data curation, validation, and wrote the original draft.
Supplemental Material
This article contains the following supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0005082021/-/DCSupplemental.
POCUS image quality and direct observation feedback forms. Download Supplemental Appendix 1, PDF file, 174 KB (173KB, pdf)
Nephrology point-of-care ultrasonography note sample. Download Supplemental Appendix 2, PDF file, 174 KB (173KB, pdf)
References
- 1.The Accreditation Council for Graduate Medical Education: ACGME Program Requirements for Graduate Medical Education in Emergency Medicine. Available at: https://acgme.org/Portals/0/PFAssets/ProgramRequirements/110_EmergencyMedicine_2020_TCC.pdf?ver=2020-06-26-125900-147. Accessed July 4, 2021
- 2.Bahner DP, Goldman E, Way D, Royall NA, Liu YT: The state of ultrasound education in U.S. medical schools: Results of a national survey. Acad Med 89: 1681–1686, 2014 [DOI] [PubMed] [Google Scholar]
- 3.LoPresti CM, Schnobrich DJ, Dversdal RK, Schembri F: A road map for point-of-care ultrasound training in internal medicine residency. Ultrasound J 11: 10, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koratala A, Teodorescu V, Niyyar VD: The nephrologist as an ultrasonographer. Adv Chronic Kidney Dis 27: 243–252, 2020 [DOI] [PubMed] [Google Scholar]
- 5.Koratala A, Ronco C, Kazory A: The promising role of lung ultrasound in assessment of volume status for patients receiving maintenance renal replacement therapy. Blood Purif 49: 643–646, 2020 [DOI] [PubMed] [Google Scholar]
- 6.Koratala A, Kazory A: Point of care ultrasonography for objective assessment of heart failure: Integration of cardiac, vascular, and extravascular determinants of volume status. Cardiorenal Med 11: 5–17, 2021 [DOI] [PubMed] [Google Scholar]
- 7.Rope RW, Pivert KA, Parker MG, Sozio SM, Merell SB: Education in nephrology fellowship: A survey-based needs assessment. J Am Soc Nephrol 28: 1983–1990, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koratala A, Segal MS, Kazory A: Integrating point-of-care ultrasonography into nephrology fellowship training: A model curriculum. Am J Kidney Dis 74: 1–5, 2019 [DOI] [PubMed] [Google Scholar]
- 9.Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB: Point-of-care ultrasound in general practice: A systematic review. Ann Fam Med 17: 61–69, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hellmann DB, Whiting-O’Keefe Q, Shapiro EP, Martin LD, Martire C, Ziegelstein RC: The rate at which residents learn to use hand-held echocardiography at the bedside. Am J Med 118: 1010–1018, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Schnobrich DJ, Olson AP, Broccard A, Duran-Nelson A: Feasibility and acceptability of a structured curriculum in teaching procedural and basic diagnostic ultrasound skills to internal medicine residents. J Grad Med Educ 5: 493–497, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koratala A, Bhattacharya D, Kazory A: Helping patients and the profession: Nephrology-oriented point-of-care ultrasound program for internal medicine residents. Clin Nephrol 91: 321–322, 2019 [DOI] [PubMed] [Google Scholar]
- 13.Hempel D, Stenger T, Campo dell' Orto M, Stenger D, Seibel A, Röhrig S, Heringer F, Walcher F, Breitkreutz R: Analysis of trainees’ memory after classroom presentations of didactical ultrasound courses. Crit Ultrasound J 6: 10, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahner DP, Hughes D, Royall NA: I-AIM: A novel model for teaching and performing focused sonography. J Ultrasound Med 31: 295–300, 2012 [DOI] [PubMed] [Google Scholar]
- 15.Kennedy Hall M, Coffey EC, Herbst M, Liu R, Pare JR, Andrew Taylor R, Thomas S, Moore CL: The “5Es” of emergency physician-performed focused cardiac ultrasound: A protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med 22: 583–593, 2015 [DOI] [PubMed] [Google Scholar]
- 16.Online POCUS teaching tool, NephroPOCUS.com. Available at: https://nephropocus.com/about/. Accessed July 4, 2021
- 17.American Society of Nephrology : ASN Innovations in Kidney Education. Available at: https://www.asn-online.org/education/contest/. Accessed July 4, 2021
- 18.The Society of Point of Care Ultrasound : FOAM-US Resources. Available at: https://spocus.org/resources-programs/foamed/. Accessed July 4, 2021
- 19.Malik AN, Rowland J, Haber BD, Thom S, Jackson B, Volk B, Ehrman RR: The use of handheld ultrasound devices in emergency medicine [published online ahead of print May 11, 2021] Curr Emerg Hosp Med Rep [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emergency ACEP : Point-of-Care, and Clinical Ultrasound Guidelines in Medicine. Available at: https://www.acep.org/patient-care/policy-statements/ultrasound-guidelines-emergency-point-of--care-and-clinical-ultrasound-guidelines-in-medicine/. Accessed July 4, 2021
- 21.SonoClipShare Ultrasound Image Sharing Platform. Available at: https://wiki.sonoclipshare.com/. Accessed July 4, 2021
- 22.Koenig SJ, Lou BX, Moskowitz Y, Narasimhan M, Mayo PH: Ultrasound billing for intensivists. Chest 156: 792–801, 2019 [DOI] [PubMed] [Google Scholar]
- 23.Koratala A, Bhattacharya D, Kazory A: Harnessing twitter polls for multi-specialty collaboration in standardizing point-of-care ultrasonography in nephrology. Clin Nephrol 94: 50–52, 2020 [DOI] [PubMed] [Google Scholar]
- 24.Blaivas M, Pawl R: Analysis of lawsuits filed against emergency physicians for point-of-care emergency ultrasound examination performance and interpretation over a 20-year period. Am J Emerg Med 30: 338–341, 2012 [DOI] [PubMed] [Google Scholar]
- 25.Stolz L, O'Brien K, Miller M, Winters-Brown N, Blaivas M, Adhikari S: A review of lawsuits related to point-of-care emergency ultrasound applications. West J Emerg Med 16: 1–4, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen J, Cascione M, Noori S: Analysis of lawsuits related to point-of-care ultrasonography in neonatology and pediatric subspecialties. J Perinatol 36: 784–786, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Reaume M, Farishta M, Costello JA, Gibb T, Melgar TA: Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. Postgrad Med J 97: 55–58, 2021 [DOI] [PubMed] [Google Scholar]
- 28.Koratala A, Sturgill D: Point-of-care venous Doppler ultrasound in the management of heart failure and hyponatremia. Clin Nephrol 96: 63–66, 2021 [DOI] [PubMed] [Google Scholar]
- 29.Argaiz ER, Koratala A, Reisinger N: Comprehensive assessment of fluid status by point-of-care ultrasonography. Kidney360 2: 1326-1338, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mathews BK, Miller PE, Olson APJ: Point-of-care ultrasound improves shared diagnostic understanding between patients and providers. South Med J 111: 395–400, 2018 [DOI] [PubMed] [Google Scholar]
- 31.Andersen CA, Brodersen J, Rudbæk TR, Jensen MB: Patients’ experiences of the use of point-of-care ultrasound in general practice: A cross-sectional study. BMC Fam Pract 22: 116, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barchiesi M, Bulgheroni M, Federici C, Casella F, Medico MD, Torzillo D, Janu VP, Tarricone R, Cogliati C: Impact of point of care ultrasound on the number of diagnostic examinations in elderly patients admitted to an internal medicine ward. Eur J Intern Med 79: 88–92, 2020 [DOI] [PubMed] [Google Scholar]
- 33.Van Schaik GWW, Van Schaik KD, Murphy MC: Point-of-Care ultrasonography (POCUS) in a community emergency department: An analysis of decision making and cost savings associated with POCUS. J Ultrasound Med 38: 2133–2140, 2019 [DOI] [PubMed] [Google Scholar]
- 34.Koratala A: Utilizing point-of-care ultrasound in the cardiorenal clinic to enhance patient care. Braz J Nephrol 43: 135–136, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kazory A, McCullough PA, Rangaswami J, Ronco C: Cardionephrology: Proposal for a futuristic educational approach to a contemporary need. Cardiorenal Med 8: 296–301, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
POCUS image quality and direct observation feedback forms. Download Supplemental Appendix 1, PDF file, 174 KB (173KB, pdf)
Nephrology point-of-care ultrasonography note sample. Download Supplemental Appendix 2, PDF file, 174 KB (173KB, pdf)