Abstract
Background
The current COVID-19 pandemic is unprecedented; under resource-constrained settings, predictive algorithms can help to stratify disease severity, alerting physicians of high-risk patients; however, there are only few risk scores derived from a substantially large electronic health record (EHR) data set, using simplified predictors as input.
Objective
The objectives of this study were to develop and validate simplified machine learning algorithms that predict COVID-19 adverse outcomes; to evaluate the area under the receiver operating characteristic curve (AUC), sensitivity, specificity, and calibration of the algorithms; and to derive clinically meaningful thresholds.
Methods
We performed machine learning model development and validation via a cohort study using multicenter, patient-level, longitudinal EHRs from the Optum COVID-19 database that provides anonymized, longitudinal EHR from across the United States. The models were developed based on clinical characteristics to predict 28-day in-hospital mortality, intensive care unit (ICU) admission, respiratory failure, and mechanical ventilator usages at inpatient setting. Data from patients who were admitted from February 1, 2020, to September 7, 2020, were randomly sampled into development, validation, and test data sets; data collected from September 7, 2020, to November 15, 2020, were reserved as the postdevelopment prospective test data set.
Results
Of the 3.7 million patients in the analysis, 585,867 patients were diagnosed or tested positive for SARS-CoV-2, and 50,703 adult patients were hospitalized with COVID-19 between February 1 and November 15, 2020. Among the study cohort (n=50,703), there were 6204 deaths, 9564 ICU admissions, 6478 mechanically ventilated or EMCO patients, and 25,169 patients developed acute respiratory distress syndrome or respiratory failure within 28 days since hospital admission. The algorithms demonstrated high accuracy (AUC 0.89, 95% CI 0.89-0.89 on the test data set [n=10,752]), consistent prediction through the second wave of the pandemic from September to November (AUC 0.85, 95% CI 0.85-0.86) on the postdevelopment prospective test data set [n=14,863], great clinical relevance, and utility. Besides, a comprehensive set of 386 input covariates from baseline or at admission were included in the analysis; the end-to-end pipeline automates feature selection and model development. The parsimonious model with only 10 input predictors produced comparably accurate predictions; these 10 predictors (age, blood urea nitrogen, SpO2, systolic and diastolic blood pressures, respiration rate, pulse, temperature, albumin, and major cognitive disorder excluding stroke) are commonly measured and concordant with recognized risk factors for COVID-19.
Conclusions
The systematic approach and rigorous validation demonstrate consistent model performance to predict even beyond the period of data collection, with satisfactory discriminatory power and great clinical utility. Overall, the study offers an accurate, validated, and reliable prediction model based on only 10 clinical features as a prognostic tool to stratifying patients with COVID-19 into intermediate-, high-, and very high-risk groups. This simple predictive tool is shared with a wider health care community, to enable service as an early warning system to alert physicians of possible high-risk patients, or as a resource triaging tool to optimize health care resources.
Keywords: COVID-19, predictive algorithm, prognostic model, machine learning
Introduction
The COVID-19 pandemic has impacted more than 200 countries, claimed more than 3 million lives, presenting an urgent threat to global health. Under resource-constrained settings, a validated model using large-scale real-world data to predict COVID-19 prognosis can rapidly identify the individuals who are at risk of COVID-19 adverse outcomes and mortality, so they could benefit from early interventions.
Several studies have derived prognostic predictors for COVID-19; however, currently there are only few COVID-19 risk calculation tools with simplified predictors for stratification that leverage on a substantially large US electronic health record (EHR) data set of statistically meaningful size [1,2]. The Acute Physiology and Chronic Health Evaluation (APACHE) II score [3] has been widely used to predict in-hospital mortality, and has been found to predict mortality in patients with COVID-19, outperforming Sequential Organ Failure Assessment (SOFA) [4] and CURB-65 [5] scores in a retrospective study of 154 patients in China [6]. COVID-GRAM [2] is a web-based calculator to estimate the occurrence of ICU admission, mechanical ventilation, or death in hospitalized patients with COVID-19; it has been validated in a study of nearly 1600 patients in China. The Coronavirus Clinical Characterization Consortium (4C) Mortality Score [1] developed by the International Severe Acute Respiratory and Emerging Infections Consortium (ISARIC) World Health Organization (WHO) Clinical Characterisation Protocol UK (CCP-UK) study is a risk stratification tool to predict in-hospital mortality by categorizing patients at low, intermediate, high, or very high risk of death. Separately, an accurate, machine learning–based COVID-19 mortality prediction model has been developed based on data from the Mount Sinai Health System; however, its validation data set is limited in size [7].
The objective of this paper is to develop and validate simplified and parsimonious predictive algorithms, leveraging large size, near real-time real-world data as a risk stratification methodology to identify patients who are at heightened risk of (1) mortality; (2) ICU admission; (3) composite of invasive mechanical ventilation/extracorporeal membrane oxygenation (ECMO); (4) composite of acute respiratory distress syndrome (ARDS)/respiratory failure, which can be easily integrated into the hospital electronic medical record system as a risk stratification and triaging tool.
Methods
Data Source
This is a retrospective observational cohort analysis of multicenter, longitudinal, anonymized patient-level data from the Optum EHR COVID-19 database. It includes demographics, insurance status, medication prescription, vital signs, coded diagnoses, procedures, laboratory results, visits, encounters, and providers. Currently, there are 3,702,050 patients in the data release dated January 27, 2021. As deidentified data are used for the study, it was exempt from Institutional Review Board approval.
Study Period
The study period was from February 1, 2020, to January 27, 2021. A baseline of up to 1 year prior to and including index date was used for assessment of demographics, lifestyle factors, and comorbidity at baseline. Patients were followed up to 28 days from admission, unless they were censored by in-hospital mortality or discharged.
Participants
Study cohort consists of patients hospitalized with COVID-19 aged 18 and older, with a confirmed diagnosis or positive test of COVID-19 infection. A COVID-19 diagnosis was defined as the first occurrence on or after February 1, 2020, of any of the following: (1) positive result from SARS-CoV-2 viral RNA or antigen tests; (2) International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes U07.1 (COVID-19, virus identified), J12.81 (pneumonia due to SARS-associated coronavirus), J12.89 (other viral pneumonia), or J80 (ARDS); and (3) ICD-10-CM code B97.29 (other coronavirus as the cause of disease) or B34.20 (coronavirus infection, unspecified) occurring on or before April 30, 2020. The expanded diagnosis code list, beyond COVID-19–specific diagnosis code (U07.1), was used because U07.1 was either unavailable (pre-April 2020) or was being implemented (April 2020), resulting in the use of alternative codes for COVID-19 in early pandemic. Other codes such as J20.3 (acute bronchitis due to coxsackievirus) were excluded due to very few uses (<10 patients) in the study period.
Patients were excluded for any of the following: (1) missing age or sex; (2) under the age of 18; (3) diagnosis or procedure codes for labor and delivery during hospitalization; (4) diagnosis codes for trauma, injury, fracture, or poisoning during the first 2 days of hospitalization; (5) admitted to hospital more than 10 days prior to COVID-19 diagnosis or 28 days after COVID-19 diagnosis; (6) diagnosed or admitted to hospital after November 16, 2020, therefore with less than 10 weeks between their first COVID-19 diagnosis date or hospital admission date, and the last database refresh date (January 27, 2021; Figure 1). Additional sensitivity analysis was conducted between the final study cohort (n=50,703) and patients who tested positive for SARS-CoV-2 (n=38,277), a subset of the former.
Figure 1.
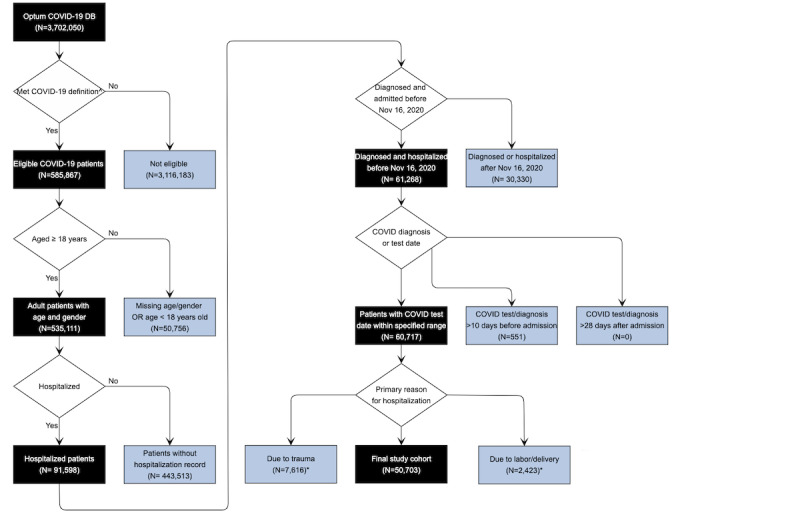
Patient attrition diagram. ∧With relevant COVID-19 diagnosis codes or tested positive for SARS-CoV-2. *Non-exclusive critera: overlapping was allowed.
Sampling
In the final cohort that satisfied the study criteria (n=50,703), data from patients with an index date prior to September 7, 2020, were referred to as model development data set (n=35,840), which was randomly sampled without replacement using 28-day in-hospital mortality as stratification factor into 40% training data set (n=14,336), 30% validation data set (n=10,752) for hyperparameter tuning and threshold calculation, and 30% test data set (n=10,752). The sampling ratio is determined such that the validation or test data set alone can satisfy the sample size requirement; the minimum sample size is estimated to be 8605, assuming a predetermined sensitivity of 0.7 and the prevalence of all-cause mortality of 15% with 95% CI and maximum marginal error of estimate of 2.5% [8]. Furthermore, an independent validation consisting of patients with index date from September 7 to November 15, 2020, was referred to as postdevelopment prospective test data set (n=14,863).
Index Date
The index date was defined as hospital admission date.
Sample Size
The initial anonymized data for 3,702,050 patients from 885,677 providers and 2465 delivery networks for the study period February 1, 2020, to January 27, 2021, were transferred from Optum, among which 585,867 patients were diagnosed or tested positive for SARS-CoV-2 infection.
Outcome
The outcomes were 28-day in-hospital (1) all-cause mortality; (2) ICU admission; (3) composite of invasive mechanical ventilation or ECMO; (4) composite of ARDS and respiratory failure. These were assessed as dichotomous outcomes and individually modeled. Outcome-specific exclusions were applied as appropriate to include only incident outcomes.
Covariates
A total of 386 study covariates (with a minimum 70% [35,493/50,703 patients] coverage among study cohort) consisting of patients’ baseline demographics (age, sex, census division, insurance status, race, ethnicity), lifestyle factors (smoking status, BMI), comorbidities (including atrial fibrillation cancer history, cerebrovascular disease, chronic kidney disease stage I-V, chronic obstructive pulmonary disease, coronary artery disease, Type I/II diabetes mellitus, HIV, stroke, etc.), baseline medication (including antidiabetics, anticoagulants, antihypertensives, antiplatelets, steroids, etc.) within 12 months prior to index date, vital signs (blood pressures, heart rate, pulse, respiration rate, temperature), laboratory values (including albumin, alanine transaminase, aspartate aminotransferase, total bilirubin, B-type natriuretic peptide, blood urea nitrogen (BUN), chloride, creatinine, C-reactive protein, D-dimer, fibrinogen, hemoglobin, lymphocyte, monocyte, neutrophil, oxygen saturation platelet count, arterial blood pH, etc.), and treatment (including diuretics, disease-modifying antirheumatic drugs, steroids, etc.) administered on the day of hospital admission were included in the analysis. Concretely, baseline medication, comorbidity, and postadmission treatment were expressed as dichotomous variables; categorical variables were converted to dummy variables; numerical variables were used without standardization, unless when fitting to penalized (Lasso or Ridge) logistic regression models, while numerical covariates were normalized using a min–max standardization to speed up convergence.
Missing Data
One of the challenges of working with real-world data is the missing covariates. Assuming covariates are missing at random, multiple imputation by chained equations via random forest [9] was used to impute covariates with missing values. Ten complete data sets each with 10 iterations were imputed with predictive mean matching using available covariates while excluding the outcome variables. The prediction performances of sparsity-aware models (XGB [10]) between imputed and nonimputed data set were compared in the sensitivity analysis.
Given the intention to develop an algorithm of great relevance to as many patients as possible, we have restricted the model input to covariates with a minimum of 70% coverage in the study cohort. Overall, the proportion of missing values among the vital and laboratory variables ranges from 10.44% (5295/50,703) to 99.36% (50,381/50,703) out of 50,703 patients; 45 of 431 variables were not included as input to the model due to more than 30% (15,211/50,703) of missingness (Multimedia Appendices 1 and 2). Sensitivity analysis was conducted to evaluate whether inclusion of additional covariates with higher degrees of missingness (ie, varying the cutoffs from 10% to 90%) aids in improving model performance, though it may increase the sensitivity of the models to biases due to nonignorable missingness in the data.
Model Development
We have applied a systematic approach to model development and validation. A framework of 6 machine learning algorithms (XGB [10,11], penalized logistic regression [12,13] with Lasso [14] or Ridge loss [11], random forest [11,15,16], decision tree [17], and LightGBM [18]) has been adopted to develop interpretable models to predict the prognosis of COVID-19.
In the preliminary analysis, the most performant algorithm was selected from the candidate algorithms; prior to model training, hyperparameter optimization via grid search, ranging from 96 to 243 folds, was performed on 6 candidate algorithms individually for full and simplified models. The full model uses all the available 386 input features after extraction and transformation in preliminary analysis, while the simplified model recursively eliminates the aforementioned input to yield a maximum of 20 variables [19]. The algorithm with best performance (area under the receiver operating characteristic curve [AUC], Brier score [20], and calibration [21]) on the test data set was selected for the final analysis.
In the final analysis, model input is further iteratively reduced to a maximum of 5 variables with a step size of 1; 100 individual runs were performed at each step, with retuned model parameters every 5 steps. The selected features were pooled and plotted in frequency heatmap with the corresponding AUC.
The model performance is evaluated against outcome variables in the test and postdevelopment prospective test data sets via AUC, Brier score, and calibration curve. The 95% CIs for AUC and Brier score were calculated based on percentiles from bootstrapped resampling with replacement (bootstrap sample size = 2000) without bias correction or acceleration [22]. The calibration curves (number of discretized bins = 10) were plotted for all the runs.
Model Validation
Rigorous validation analysis was performed to ensure robustness and reliability of the predictions. Both full and simplified models of 6 candidate algorithms were trained and validated during the model development phase with data from February 1 to September 6, where the test data set was held out from model training and used solely for reporting the performance. Furthermore, the model has been additionally validated externally, using the postdevelopment prospective test data set collected from September 7 to November 15, 2020, to demonstrate consistent model performance through the subsequent wave of the pandemic. Model discrimination was performed on the imputed test data set by assessing AUC on the stratified analysis by sex, age, and racial groups.
Model Benchmark
The performance of the risk prediction models has been benchmarked to (1) the baseline model and (2) published COVID-19 prognostic scores. The baseline model was developed using XGB with optimized hyperparameters on age and sex only. Evaluation metrics including AUC, sensitivity, specificity, and decision curve analysis were assessed to compare the performance and utility of prognostic scores (APACHE II [3,23], CURB-65 [5,24,25], E-CURB [26], The National Early Warning [NEWS] 2 score [25,27-29], Respiratory Rate-Oxygenation [ROX] index [29,30], ISARIC 4C mortality score [1,25]). AUC is reported based on complete case data from test and postdevelopment prospective test data sets, and no imputation was performed.
Predictors
Feature importance is ranked by Shapley values [31] from test and postdevelopment prospective test data sets in the SHapley Additive exPlanations (SHAP) summary plot. Shapley value calculates fair contribution and the extent of predictors toward the model output [32]. It measures feature importance by the magnitude and the direction of contributions. The dependence between model prediction and age is plotted with age on the x-axis and its impact on prediction represented by Shapley value on the y-axis for every patient, colored by the magnitude of a second feature (BUN, respiration rate, pulse, lymphocyte count) individually.
Receiver Operating Characteristic Curve Analysis
We adopted two approaches in determining the optimal threshold on the receiver operating characteristic curve. Assuming the sensitivity and specificity were weighted equally without ethical, cost, and prevalence constraints, the optimal cutoff is at the location where the Youden index (sum of specificity and sensitivity – 1) is maximized at the test data set [33-36]. This approach relies solely on the predictive accuracy of a model, and consequences of the predictions (ie, cost of false positives and false negatives) are not considered. In the second approach, clinical utility–based decision theory was used in developing a cost-sensitive threshold, where it builds in disease prevalence and costs of false positive and false negatives of specific diagnostic scenario [33,37].
Decision curve analysis assists in clinical judgment and comparison about the relative value of benefits associated with the use of a clinical prediction tool [38,39]. The standardized net benefit of full model, simplified model (with 10 input variables), and selected benchmark prognostic scores was calculated and plotted across probabilities. The benchmark models that use point scores were calibrated to test data prior to decision curve analysis.
Results
Patient Characteristics
Figure 1 shows patient attrition flowchart, and the workflow of model development and validation is in Figure 2. Patients’ baseline and clinical characteristics at admission are summarized in Table 1. Validation and test data sets are largely homogeneous to the training data set; however, the postdevelopment prospective test data set that was collected later in the pandemic from September to November presents more differences in geographic locations (a decline in the proportion of patients in Middle Atlantic from 22.69% [8132/35,840] to 8.68% [1290/14,863] after September 7, and an increase in West North Central from 9.83% [3523/35,840] to 24.18% [3594/14,863]) and racial distribution (the proportion of White increased from 53.87% [19,308/35,840] to 72.88% [10,832/14,863]). However, the overall mortality remains consistent. Hypertension (57.55% [29,179/50,703]), obesity (47.51% [24,089/50,703]), diabetes mellitus (34.44% [17,461/50,703]), chronic kidney disease (19.79% [10,033/50,703]), and coronary artery disease (17.74% [8996/50,703]) were the common comorbidities among the cohort.
Figure 2.
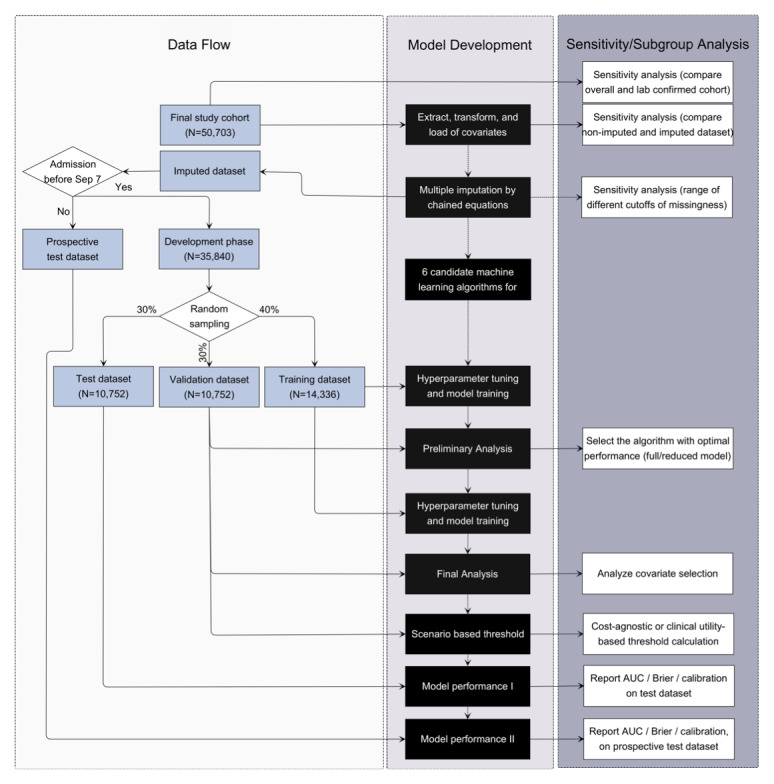
Model development and validation framework including data sampling and corresponding sensitivity analyses.
Table 1.
Demographic and clinical characteristics of hospitalized patients with COVID-19 at baseline and admission.
| Characteristic | Training data set (n=14,336) | Validation data set (n=10,752) | Test data set (n=10,752) | Prospective test data set (n=14,863) | ||
| Mean (SD) age at baseline, years | 60.9 (17.2) | 60.9 (17.2) | 60.8 (17.1) | 63.8 (16.8) | ||
| Distribution, n (%) |
|
|
|
|
||
|
|
18-34 | 1231 (8.59) | 920 (8.56) | 911 (8.47) | 1015 (6.83) | |
|
|
35-49 | 2383 (16.62) | 1780 (16.56) | 1840 (17.11) | 1893 (12.74) | |
|
|
50-64 | 4337 (30.25) | 3193 (29.70) | 3293 (30.63) | 4110 (27.65) | |
|
|
65-74 | 2922 (20.38) | 2296 (21.35) | 2141 (19.91) | 3325 (22.37) | |
|
|
75-84 | 2165 (15.10) | 1589 (14.78) | 1606 (14.94) | 2943 (19.80) | |
|
|
85+ | 1298 (9.05) | 974 (9.06) | 961 (8.94) | 1577 (10.61) | |
| Sex at baseline, n (%) | ||||||
|
|
Male | 7473 (52.13) | 5619 (52.26) | 5629 (52.35) | 7645 (51.44) | |
|
|
Female | 6863 (47.87) | 5133 (47.74) | 5123 (47.65) | 7218 (48.56) | |
| Race at baseline, n (%) | ||||||
|
|
African American | 3466 (24.18) | 2669 (24.82) | 2668 (24.81) | 1867 (12.56) | |
|
|
Asian | 368 (2.57) | 268 (2.49) | 276 (2.57) | 216 (1.45) | |
|
|
White | 7779 (54.26) | 5734 (53.33) | 5795 (53.90) | 10,832 (72.88) | |
|
|
Other/Unknown | 2723 (18.99) | 2081 (19.35) | 2013 (18.72) | 1948 (13.11) | |
| Census division at baseline, n (%) | ||||||
|
|
East North Central | 3778 (26.35) | 2942 (27.36) | 2908 (27.05) | 4174 (28.08) | |
|
|
East South Central | 1010 (7.05) | 708 (6.58) | 754 (7.01) | 1205 (8.11) | |
|
|
Middle Atlantic | 3221 (22.47) | 2488 (23.14) | 2423 (22.54) | 1290 (8.68) | |
|
|
Mountain | 496 (3.46) | 355 (3.30) | 363 (3.38) | 923 (6.21) | |
|
|
New England | 1042 (7.27) | 705 (6.56) | 763 (7.10) | 769 (5.17) | |
|
|
Pacific | 475 (3.31) | 331 (3.08) | 317 (2.95) | 345 (2.32) | |
|
|
South Atlantic/West South Central | 2454 (17.12) | 1802 (16.76) | 1810 (16.83) | 2120 (14.26) | |
|
|
West North Central | 1396 (9.74) | 1067 (9.92) | 1060 (9.86) | 3594 (24.18) | |
|
|
Other/Unknown | 464 (3.24) | 354 (3.29) | 354 (3.29) | 443 (2.98) | |
| BMI at baseline (kg/m2), mean (SD) | 31.0 (8.5) | 30.9 (8.3) | 31.2 (8.6) | 31.6 (8.7) | ||
| Distribution, n (%) |
|
|
|
|
||
|
|
Underweight | 352 (2.46) | 235 (2.19) | 221 (2.06) | 304 (2.05) | |
|
|
Healthy weight | 2526 (17.62) | 1873 (17.42) | 1833 (17.05) | 2283 (15.36) | |
|
|
Overweight | 3697 (25.79) | 2878 (26.77) | 2838 (26.40) | 3679 (24.75) | |
|
|
Obese | 3041 (21.21) | 2247 (20.90) | 2344 (21.80) | 3228 (21.72) | |
|
|
Morbidly obese | 3679 (25.66) | 2739 (25.47) | 2742 (25.50) | 4069 (27.38) | |
|
|
Unknown | 1041 (7.26) | 780 (7.25) | 774 (7.20) | 1300 (8.75) | |
| Comorbidity at baselinea, n (%) | ||||||
|
|
Cerebrovascular disease | 676 (4.72) | 502 (4.67) | 501 (4.66) | 894 (6.01) | |
|
|
Chronic kidney disease | 2808 (19.59) | 2058 (19.14) | 2040 (18.97) | 3127 (21.04) | |
|
|
Congestive heart failure | 2137 (14.91) | 1534 (14.27) | 1553 (14.44) | 2369 (15.94) | |
|
|
Coronary artery disease | 2430 (16.95) | 1797 (16.71) | 1800 (16.74) | 2969 (19.98) | |
|
|
Diabetes mellitus | 4831 (33.70) | 3636 (33.82) | 3586 (33.35) | 5408 (36.39) | |
|
|
Hypertension | 8173 (57.01) | 6091 (56.65) | 6063 (56.39) | 8852 (59.56) | |
|
|
Solid tumor | 830 (5.79) | 606 (5.64) | 619 (5.76) | 1052 (7.08) | |
|
|
Transplant history | 28 (0.20) | 16 (0.15) | 20 (0.19) | 12 (0.08) | |
| 28-day outcomes, n (%) | ||||||
|
|
All-cause mortality | 1769 (12.34) | 1326 (12.33) | 1327 (12.34) | 1782 (11.99) | |
|
|
Intensive care unit admission | 2813 (19.62) | 2181 (20.28) | 2148 (19.98) | 2422 (16.30) | |
|
|
Acute respiratory distress syndrome (respiratory failure) | 7276 (50.75) | 5500 (51.15) | 5384 (50.07) | 7009 (47.16) | |
|
|
Extracorporeal membrane oxygenation (mechanical ventilation) | 1962 (13.69) | 1535 (14.28) | 1498 (13.93) | 1483 (9.98) | |
| Vitals at admission, median (10th-90th percentile) | ||||||
|
|
Diastolic blood pressure (mmHg)b | 73.0 (56.0-90.0) | 73.0 (56.0-90.0) | 73.0 (56.0-90.0) | 73.0 (56.0-90.0) | |
|
|
Systolic blood pressure (mmHg)b | 125.0 (100.0-154.0) | 125.0 (101.0-155.0) | 125.0 (101.0-154.0) | 128.0 (103.0-159.0) | |
|
|
Pulse (bpm)b | 85.0 (64.0-110.0) | 85.0 (64.0-110.0) | 85.0 (64.0-110.0) | 81.0 (61.0-107.6) | |
|
|
Respiratory rate (breaths/minute)b | 19.0 (16.0-28.0) | 19.0 (16.0-28.0) | 19.0 (16.0-28.0) | 18.0 (16.0-25.0) | |
|
|
Temperature (oC)b | 36.8 (36.3-37.9) | 36.8 (36.3-37.9) | 36.8 (36.3-37.8) | 36.7 (36.2-37.7) | |
| Laboratory valuesa at admission, median (10th percentile-90th percentile) |
|
|||||
|
|
Alkaline phosphatase (IU/L) | 77.0 (49.0-137.0) | 76.0 (49.0-136.0) | 76.0 (48.0-135.0) | 78.0 (50.0-134.0) | |
|
|
Alanine aminotransferase (IU/L) | 28.0 (12.0-79.0) | 29.0 (12.0-80.0) | 28.0 (12.0-79.0) | 27.0 (12.0-68.0) | |
|
|
Aspartate aminotransferase (IU/L) | 37.0 (18.0-95.0) | 36.0 (18.0-97.0) | 36.0 (18.0-95.0) | 34.0 (18.0-80.0) | |
|
|
Albumin (g/dL) | 3.5 (2.7-4.2) | 3.6 (2.7-4.2) | 3.6 (2.7-4.2) | 3.6 (2.8-4.2) | |
|
|
Anion gap (mEq/L) | 12.0 (7.0-17.0) | 12.0 (7.0-17.0) | 12.0 (7.0-17.0) | 12.0 (7.0-16.0) | |
|
|
Blood urea nitrogen (mg/dL) | 16.0 (8.0-47.0) | 17.0 (8.0-46.0) | 16.0 (8.0-47.0) | 18.0 (9.0-44.0) | |
|
|
Bicarbonate (mmol/L) | 24.0 (19.0-29.0) | 24.0 (19.0-29.0) | 24.0 (19.0-29.0) | 24.0 (19.0-29.0) | |
|
|
Bilirubin total (mg/dL) | 0.6 (0.3-1.2) | 0.6 (0.3-1.2) | 0.6 (0.3-1.2) | 0.6 (0.3-1.1) | |
|
|
C-reactive protein (mg/dL) | 85.0 (10.3-229.0) | 82.2 (11.0-218.0) | 82.0 (10.2-220.0) | 73.0 (10.0-206.6) | |
|
|
Chloride (mmol/L) | 101.0 (94.0-108.0) | 101.0 (94.0-108.0) | 101.0 (94.0-108.0) | 101.0 (94.0-107.0) | |
|
|
Glucose (mg/dL) | 120.0 (91.0-242.0) | 121.0 (92.0-236.0) | 121.0 (92.0-240.6) | 122.0 (91.2-244.0) | |
|
|
Hemoglobin (g/dL) | 13.2 (10.0-15.5) | 13.2 (10.1-15.6) | 13.2 (10.2-15.7) | 13.2 (10.1-15.6) | |
|
|
Lymphocyte (%) | 14.1 (5.4-30.0) | 14.8 (5.6-30.7) | 14.6 (5.8-30.2) | 14.1 (5.3-30.0) | |
|
|
Monocyte (%) | 7.1 (3.1-12.9) | 7.0 (3.2-12.6) | 7.1 (3.2-12.7) | 7.8 (3.6-13.1) | |
|
|
Neutrophil (%) | 75.8 (57.0-88.0) | 75.0 (57.0-88.0) | 75.2 (57.0-88.0) | 75.0 (57.0-88.0) | |
|
|
Platelet count (x109/L) | 210.0 (125.0-351.0) | 210.0 (127.0-348.0) | 211.0 (126.0-351.0) | 205.0 (124.0-335.0) | |
|
|
Potassium (mmol/L) | 3.9 (3.3-4.8) | 3.9 (3.3-4.8) | 3.9 (3.3-4.8) | 3.9 (3.3-4.7) | |
|
|
Protein total (g/dL) | 7.2 (6.2-8.2) | 7.2 (6.2-8.2) | 7.3 (6.2-8.2) | 7.1 (6.2-8.0) | |
|
|
Red cell distribution width coefficient of variation (%) | 13.9 (12.4-17.0) | 13.8 (12.4-16.9) | 13.8 (12.4-17.0) | 13.8 (12.4-16.7) | |
|
|
Sodium (mmol/L) | 136.0 (130.0-141.0) | 136.0 (131.0-142.0) | 136.0 (131.0-141.0) | 136.0 (131.0-141.0) | |
|
|
Oxygen saturation pulse oximeter (%) | 96.0 (91.0-99.0) | 96.0 (90.0-99.0) | 96.0 (91.0-99.0) | 95.0 (90.0-99.0) | |
|
|
Oxygen saturation pulse oximeterb (%) | 95.0 (87.0-99.0) | 95.0 (87.0-99.0) | 95.0 (87.0-99.0) | 95.0 (87.0-99.0) | |
|
|
Oxygen saturation pulse oximeterc (%) | 93.0 (84.0-97.0) | 93.0 (84.0-97.0) | 93.0 (84.0-97.0) | 92.0 (83.0-97.0) | |
|
|
White blood cell count (x109/L) | 7.1 (4.0-14.1) | 7.1 (4.0-13.9) | 7.0 (4.0-13.8) | 6.9 (3.9-13.5) | |
aNon-exhaustive list.
bFirst measurement on the day of hospital admission.
cMinimum measurement on the day of hospital admission.
The study cohort is defined as hospitalized adult patients with COVID-19 who were either diagnosed with relevant diagnosis codes or tested positive for SARS-CoV-2 viral RNA or antigen tests. In the subgroup analysis of patients who tested positive for SARS-CoV-2, model performances of these 2 groups (ie, overall cohort and tested positive subgroup) were largely similar with less than 1% difference in AUC across all outcomes for full and simplified models (Multimedia Appendix 3).
Model Performance
We have adopted a systematic framework of model development, including a variety of tree-, boosting-, and ensemble-based machine learning models, combined with rigorous validation on statistically meaningful sample size. The model performances (AUC and Brier score) on test and prospective test data sets are summarized in Table 2 and Figure 3. AUC is a widely used metric for performance measurement of classification; Brier score is a proper scoring rule, measuring mean squared error between prediction and outcome, impacted by both discrimination and calibration. Calibration of the algorithm is further assessed by plotting the predicted proportion against the observed proportion of outcome in each decile of risk (Figure 4).
Table 2.
Summary of model performances (AUCa and Brier Score) on test data set and postdevelopment prospective test data set in the final analysis. The full model uses all the available 210 covariates with less than 30% (15,211/50,703) missingness (excluding postadmission treatment) among the study cohort (n=50,703); the parsimonious N10 model only uses 10 predictors prefiltered from the automatic predictor selection.
| Outcome and model | AUCa (95% CI) | Brier score (95% CI) | ||||
|
|
Test data set, % | Prospective test data set, % | Test data set | Prospective test data set | ||
| All-cause mortality |
|
|
|
|
||
|
|
Full model | 88.7 (88.4-89.0) | 85.4 (85.1-85.7) | 0.071 (0.070-0.072) | 0.079 (0.078-0.080) | |
| N10 model | 87.6 (87.2-87.9) | 84.3 (84.0-84.6) | 0.074 (0.073-0.075) | 0.081 (0.080-0.081) | ||
| Intensive care unit admission |
|
|
|
|
||
|
|
Full model | 79.7 (79.4-80.1) | 77.7 (77.3-78.0) | 0.123 (0.122-0.124) | 0.115 (0.114-0.115) | |
| N10 model | 73.6 (73.2-74.0) | 73.5 (73.2-73.9) | 0.138 (0.137-0.139) | 0.123 (0.122-0.124) | ||
| Respiratory failureb |
|
|
|
|
||
|
|
Full model | 82.3 (82.0-82.5) | 80.7 (80.5-80.9) | 0.172 (0.171-0.173) | 0.180 (0.179-0.181) | |
| N10 model | 79.5 (79.2-79.7) | 78.1 (77.9-78.3) | 0.185 (0.184-0.186) | 0.192 (0.191-0.193) | ||
| Mechanical ventilationc |
|
|
|
|
||
|
|
Full model | 83.6 (83.3-84.0) | 81.1 (80.8-81.5) | 0.090 (0.089-0.091) | 0.074 (0.074-0.075) | |
| N10 model | 78.1 (77.7-78.5) | 76.6 (76.2-77.1) | 0.101 (0.100-0.101) | 0.081 (0.081-0.082) | ||
aAUC: area under the receiver operating characteristic curve.
bRefers to composite of respiratory failure and acute respiratory distress syndrome.
cRefers to composite of invasive mechanical ventilation and extracorporeal membrane oxygenation.
Figure 3.
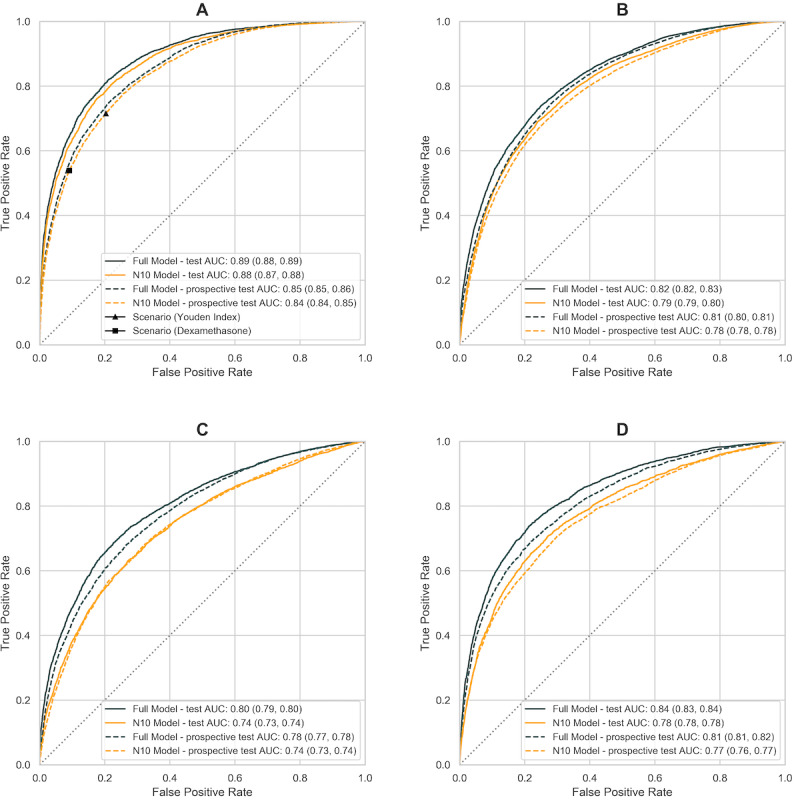
Receiver operating characteristics (AUROC) curves on four prediction outcomes in final analysis: (a) all-cause mortality; (b) respiratory failure including ARDS; (c) ICU admission; (d) invasive mechanical ventilation including ECMO. Full model is colored in black, parsimonious model with ten input variables is colored in orange. Solid line represents model performance on test dataset (n=10,752); dashed line represents post-development prospective test dataset (n=14,863). ARDS: acute respiratory distress syndrome. ECMO: extracorporeal membrane oxygenation.
Figure 4.
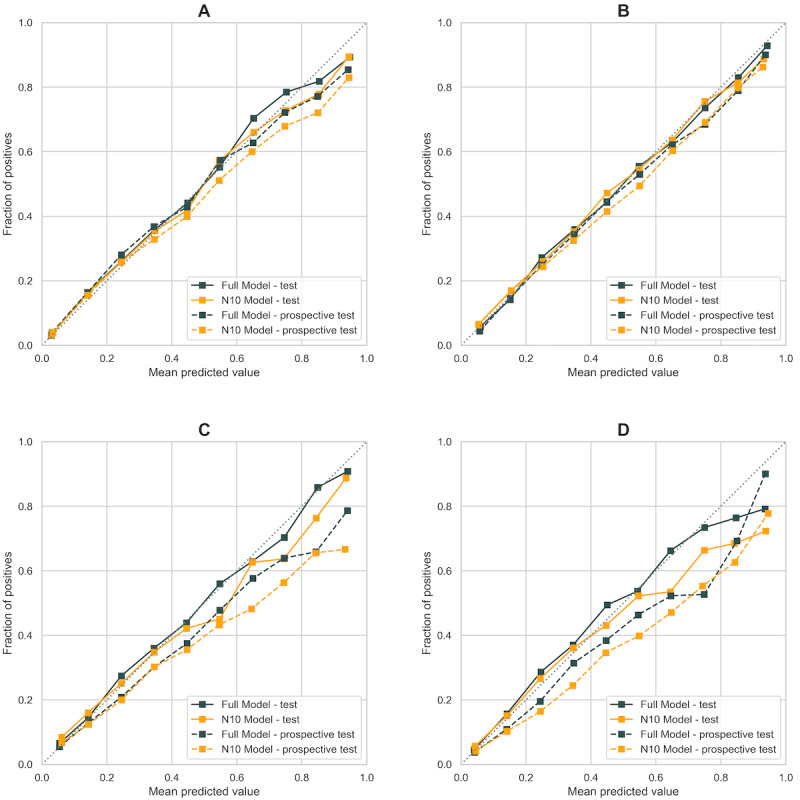
Calibration curve (number of bins = 10) on four prediction outcomes in final analysis: (a) all-cause mortality; (b) respiratory failure including ARDS; (c) ICU admission; (d) invasive mechanical ventilation including ECMO. Full model is colored in black, parsimonious model with ten input variables is colored in orange. Solid line represents calibration on test dataset (n=10,752); dashed line represents calibration on post-development prospective test dataset (n=14,863). ARDS: acute respiratory distress syndrome. ECMO: extracorporeal membrane oxygenation.
The model predicts 28-day in-hospital mortality accurately (AUC 0.88, 95% CI 0.87-0.88 on the test data set) and reliably through the second wave of pandemic (AUC 0.84, 95% CI 0.84-0.85 on the prospective test data set). Given this data set was acquired later in time from September to November and more likely to suffer from data lag, the completeness and accuracy of outcome data are hypothesized to contribute to the decrease in model performance; a subgroup analysis on patients with the complete clinical features shows an improved performance (AUC 0.89, 95% CI 0.88-0.90; Table 3).
Table 3.
Comparison with existing risk scores evaluated on test data sets to predict 28-day all-cause mortality. Sensitivity and specificity were evaluated at 2 different thresholds.
| Risk score | AUCa (95% CI), % | Threshold 1b | Threshold 2c | nd | ||
| Sensitivity, % | Specificity, % | Sensitivity, % | Specificity, % |
|
||
| Acute Physiology and Chronic Health Evaluation II | 72.3 (69.5-74.9) | 66.2 | 68.5 | 92.4 | 26.0 | 1769 |
| Respiratory Rate-Oxygenation Index | 68.5 (67.0-70.0) | 28.2 | 92.7 | 54.2 | 78.3 | 16,640 |
| CURB-65 | 78.7 (77.6-79.7) | 36.2 | 92.4 | 77.2 | 69.1 | 15,001 |
| E-CURB | 81.9 (80.3-83.3) | 63.4 | 83.4 | 87.3 | 61.3 | 5772 |
| National Early Warning Score 2 score | 82.9 (81.7-84.2) | 51.6 | 91.2 | 75.0 | 77.0 | 14,112 |
| Coronavirus Clinical Characterization Consortium Mortality score | 82.2 (80.7-83.5) | 62.3 | 83.8 | 71.8 | 75.7 | 6979 |
| Baseline model | 73.8 (73.2-74.5) | 44.8 | 83.4 | 80.2 | 54.9 | 25,615 |
| Full model | 89.2 (88.1-90.3) | 63.1 | 92.2 | 85.2 | 76.4 | 8493 |
| N10 model | 88.9 (88.0-90.0) | 65.9 | 90.9 | 81.4 | 79.3 | 10,688 |
aAUC: area under the receiver operating characteristic curve.
bThreshold 1 is a clinically relevant threshold that identifies patients for dexamethasone treatment; costs of FP and FN are expressed in terms of mortality risk.
cThreshold 2 is derived from a cost-agnostic approach and is located at the point on the area under the receiver operating characteristic curve that maximizes the Youden index.
dNumber of hospitalized patients in the test data set and the postdevelopment test data set with complete case.
We also examined discriminatory capacity in subgroups stratified by sex, race, and age group separately. It predicts all-cause mortality similarly among men (AUC 0.84, 95% CI 0.84-0.84) and women (AUC 0.84, 95% CI 0.84-0.85) and is marginally more predictive among Asians (AUC 0.86, 95% CI 0.85-0.87) compared with African Americans (AUC 0.83, 95% CI 0.83-0.84) and Whites (AUC 0.84, 95% CI 0.84-0.84). Given age is an important predictor, the model is more sensitive toward elderly cohort (more accurately ruling out negative cases) and conversely more specific toward younger cohort (more accurately ruling in the positive cases).
Algorithm Selection
In the preliminary analysis, all the candidate algorithms perform comparably on test and prospective test data sets, with less than 3% difference in AUC for all outcomes between full and simplified models (Multimedia Appendix 4). Of the 6 candidate machine learning algorithms, boosting-based algorithms (XGB [10] and LightGBM [18]) performed consistently better [40] for both full and preliminary simplified models (n=20) with less computation time and produced well-calibrated probabilities (Multimedia Appendices 5 and 6); XGB was selected given it has been validated in a similar approach [7,41,42]. With adequate model calibration and low Brier score, no adjustment or calibration was subsequently performed.
Predictor Selection
Predictors were selected in the development pipeline; specifically, 100 individual runs of recursive predictor elimination are pooled at each step between 5- and 20-input model with an increment of 1. The selection of predictors was analyzed in the frequency heatmap (Multimedia Appendix 7) and automated from the pipeline while nonmodifiable factors such as diagnosis month or census division were precluded.
With only 10 predictors, the final parsimonious model (N10) still predicts COVID-19 adverse outcomes accurately and similarly to the full model (Table 2); for instance, the final parsimonious model consisting of age, systolic and diastolic blood pressures, respiration rate, pulse, temperature, BUN, SpO2, albumin, and presence of any major cognitive disorder (including dementia, Parkinson disease, and Alzheimer disease) as input predicts all-cause mortality accurately with AUC of 0.88 (95% CI 0.87-0.88).
The magnitude and direction of individual feature contribution to prediction are inferred from the summary plot of Shapley values sorted by the descending order of feature impact (Multimedia Appendix 8); an increase in age [43-45], respiration rate [46], BUN [45,47,48], and aspartate transaminase [45,49], and a decrease in oxygen saturation [7,50], platelet count [26,51,52], and albumin [45,53] are associated with the increase in mortality risk.
Comparison With Existing Benchmark
The model shares commonalities (eg, age, respiration rate, blood pressures, pulse, BUN, SpO2, albumin) with existing prognostic scores for community-acquired pneumonia or COVID-19 [5,26,27]; however, with automated feature selection from comprehensive input covariates, and machine learning algorithm, it compares favorably with existing scores across diagnostic statistics (Table 3) and shows greater clinical utility across a wide range of probability thresholds (Figure 5) in decision curve analysis.
Figure 5.
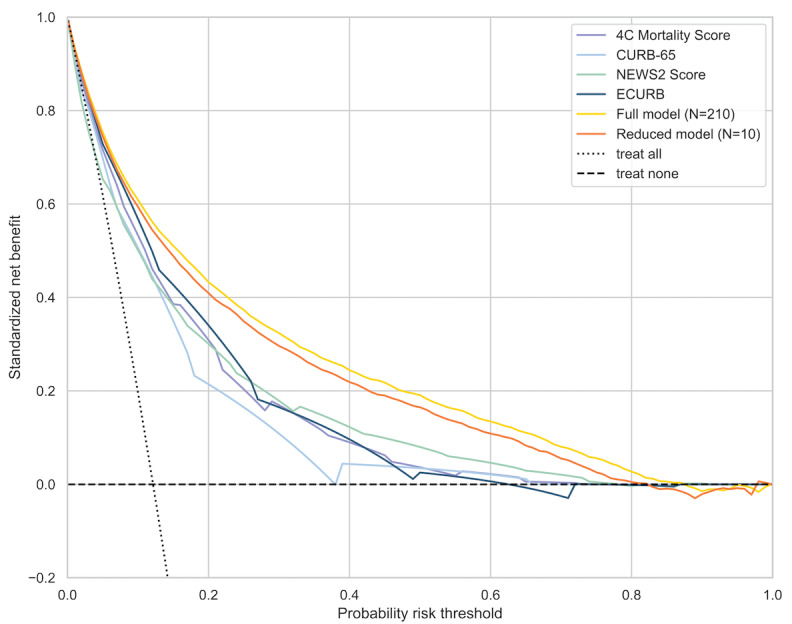
Decision curve analysis of standardized net benefit across different risk thresholds. Dotted line represents the scenario if everyone is treated; dashed line represents the scenario if none is treated.
Discussion
Summary of Principal Findings
In this paper, we have adopted a systematic framework of developing and evaluating various machine learning techniques in predicting COVID-19 prognosis on near real-time, large-size EHR data in the United States. Boosting-based algorithms (XGBoost and LightGBM) have consistently outperformed other machine learning algorithms and COVID-19 benchmark risk scores with higher accuracy on the test data set (AUC 0.89, 95% CI 0.88-0.89) and on the prospective test data set (AUC 0.85, 95% CI 0.85-0.86), and better clinical utility on decision curve analysis. After further simplification of the model to only 10 clinical features, relative to full model it provides comparable discriminatory performance (AUC 0.88 95% CI 0.87-0.88) and clinical utility.
Predictors
A major strength of this study is the use of near real-time, large-size EHR data, resulting in predictors that are highly representative and relevant to clinical practice. We have restricted the analysis to commonly measured covariates with less than 30% (15,211/50,703) of missing values among the cohort. A higher coverage cutoff precludes key predictors such as oxygen saturation [7,50], respiration rate [46], and BUN [47,48] leading to degradation of model performance (Multimedia Appendices 9 and 10).
Postadmission treatment is not a major predictor of model performance; they are not included in the final analysis, which results in minimal impact of the model performance on all-cause mortality. Patients are presented at different disease trajectories when admitted to hospital, with some being in critical condition; for instance, among 9564 ICU patients, 4745 (49.61%) were admitted to ICU on day 1 of hospital admission. The relationship between treatment type and outcome is therefore confounded by the stages of the disease course.
Age is identified as a crucial predictor for adverse outcomes [44]. It increases almost monotonically with health outcomes such as mortality and ARDS, but nonmonotonically with resource-dependent outcomes, such as ICU admission and invasive mechanical ventilation/ECMO, as these outcomes are closely associated with the availability of health care resources such as ventilator and ICU rooms. This is more noticeable for elderly patients over 75 years, who are disadvantaged for mechanical ventilation and ICU, presumably due to the scarcity of health care resources during the pandemic, though they are at highest mortality risk (Multimedia Appendix 11).
Clinical Application
When applying the model to clinical setting, threshold selection is of great practical importance in producing dichotomous predictions. In the data-driven, cost-agnostic approach, threshold is derived numerically from the AUC curve (Figure 3), which maximizes the Youden index [34] (P=.13). When the model is applied to inform clinical decision making, such as identifying patients for dexamethasone treatment, insights from relevant clinical trials could guide threshold calculation. For instance, the findings from the Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial [54], a large-enrollment, randomized controlled trial of dexamethasone, indicate a mortality risk reduction of 4.84% among patients who received oxygen therapy or were mechanically ventilated (393/1603, 24.52%) compared with the control group (965/3287, 29.36%); conversely, there was an increase in mortality risk of 3.74% among patients who require no oxygen (dexamethasone group [89/501, 17.76%] vs usual care group [145/1034, 14.02%]). When the model is applied clinically as a prognostic tool to identify patients who will receive dexamethasone, cost of false negatives (ie, misclassifying patients as low risk, and therefore they missed dexamethasone treatment) is 4.84%, and cost of false positive (ie, misclassifying patients as high risk) is 3.74% when cost of misclassification is expressed as an increase in mortality risk. Given the mortality rate of 1592/6425 (24.78%) from the RECOVERY trial [54], the threshold is found from the AUC curve at P=.33, where the slope of curve [33,37] is (0.0374/0.0484) x (1 – 0.248)/(0.248) = 2.35. Model performances are evaluated at these 2 thresholds in Table 3.
These 2 thresholds (P=.13 and .24) are similar to the intermediate- and high-risk cutoffs used to define the severity of pneumonia [1,55,56]. Based on these approaches, we derived 2 clinically meaningful thresholds (Table 4), stratifying patients into (1) low-to-intermediate risk (P≤.13, observed mortality rate = 315/8065, 3.91%); (2) high risk (0.13<P≤.24, observed mortality rate = 225/1170, 19.23%); and (3) very high risk (P>.24, observed mortality rate = 787/1517, 51.88%). Scenario-based threshold can be substituted with appropriate clinical trial insights according to different treatment options.
Table 4.
Mortality rate comparison across different risk groups on the test and postdevelopment prospective test data sets. Three risk groups were defined as (1) low-to-intermediate–risk group (P≤.13), (2) high risk (.13<P≤.24), and (3) very high risk (P>.24). The threshold probabilities are obtained from receiver operating characteristic analysis, which (1) maximizes the Youden index (P=.13), or (2) defined by clinical utility of dexamethasone (P=.24) from the RECOVERYa trial.
| Risk group | Test data set | Prospective test data set | ||
| Patients, n (%) (n=10,752) |
Deaths, n (%) (n=1327) |
Patients, n (%) (n=14,863) |
Deaths, n (%) (n=1782) |
|
| Low–intermediate | 8065 (75.01) | 315 (3.91) | 11,049 (74.34) | 512 (4.63) |
| High | 1170 (10.88) | 225 (19.23) | 1743 (11.73) | 327 (18.76) |
| Very high | 1517 (14.11) | 787 (51.88) | 2071 (13.93) | 943 (45.53) |
aRECOVERY: Randomised Evaluation of COVID-19 Therapy.
Strengths
The strengths of this research include the large size of data set, longitudinal nature, and near real-time update of the data release. The Optum database provides patient-level information with a diverse mix of geographic regions, insurance types, socioeconomic status, and ethnicity. A comprehensive list of 386 input covariates from baseline and at admission was included in the analysis based on epidemiological and clinical characteristics of COVID-19 cases; the end-to-end pipeline automates feature selection and model development process, producing risk factors that are both commonly measured at admission with wide coverage among study cohort and concordant with similar risk scores. This helps to improve the usability of the model without extensive electronic medical record integration or feeding the model with continuous data streams. The systematic approach and rigorous validations demonstrate consistent model performance to predict even beyond the period of data collection, with satisfactory discriminatory power and great clinical utility. Overall, the study offers an accurate, validated, and reliable prediction model based on only 10 clinical features as a prognostic tool for stratifying patients with COVID-19 into intermediate-, high-, and very high-risk groups. We envision this model to be used on the day of hospital admission at an inpatient setting where resource triaging is most relevant and early identification of high-risk patient is the key.
Limitations
There are several limitations in our study. First, the Optum COVID-19 database, being an EHR database, may not capture patients’ entire interaction with health care systems because patients can switch between different hospitals or health care systems. This impacts several aspects of the study, from assessment of baseline comorbidity and comedication, to capture of outcomes during follow-up. Although we have identified a minimum of 10-week period from database refresh date to COVID-19 diagnosis date to allow for capture of follow-up data and outcomes, it is possible additional data lag is still present, challenging the completeness and accuracy of outcome assessment.
Because of Health Insurance Portability and Accountability Act (HIPAA)–compliance protection, patients over 89 years were included as a single category of age in the data set, with age being an important risk predictor of mortality. This can potentially lead to some performance degradation for patients aged over 89 years. Additional data, such as symptoms since onset, could aid in early prediction of aggressive COVID-19 progression, but these were available for less than 70% (35,493/50,703) of patients in the data set; if we had adequate data on patient symptoms and the use of oxygen therapies, model performance would likely improve. Similarly, this negatively impacts the evaluation of existing prognostic scores that require FiO2. We have referred to the best currently available information on clinical trial for threshold calculation, and there could still exist differences in patient population between the RECOVERY trial and this work. Additional work is required for validating the results on vaccinated population.
Conclusions
In this study, we presented a systematic framework of model development based on a variety of machine learning techniques, combined with rigorous validation on statistically meaningful sample size. The model demonstrates consistent performance to predict even beyond the period of data collection. The parsimonious model with only 10 clinical features (age, systolic and diastolic blood pressures, respiration rate, pulse, temperature, BUN, SpO2, albumin, and presence of major cognitive disorder) offers an accurate, validated, and calibrated prediction to stratifying COVID-19 patients into intermediate-, high-, and very high-risk groups. This simple predictive tool is shared with a wider health care community (Multimedia Appendix 12), to enable service as an early warning system to alert physicians of possible high-risk patients.
Acknowledgments
We acknowledge the extensive programming and planning work of the Amgen Center for Observational Research (Oana Abrahamian, Bagmeet Behera, Corinne Brooks, and Kimberly A Roehl), initial feasibility analysis and model hosting by Amgen Digital Health & Innovation - Data Science and Engineering team (Maxim Ivanov). We also acknowledge the health care professionals whose tireless efforts in this unprecedented pandemic have provided critical knowledge, as well as the patients from whom we continue to learn so much.
Model input and variable transformation. In the preliminary analysis, a total of 386 covariates with <30% missingness are incorporated as model input.
Summary of missingness of vital and lab variables among the study cohort.
Sensitivity analysis on model performances (AUC, 95% CI) between study cohort (n=50,703 in orange) and lab confirmed cohort (n=38,277 in blue) which is a subset of study cohort; (a) model performances on test dataset; (b) on post-development prospective test dataset.
Model performance (AUC) during preliminary analysis (top: test dataset (N=10,752); bottom: post-development prospective test dataset (N=14,863). In the preliminary analysis, a total of 386 covariates (with <30% missingness) are incorporated as model input.
Calibration curve during preliminary analysis (top panel: test dataset (N=10,752); bottom panel: post-development prospective test dataset (N=14,863)). In the preliminary analysis, a total of 386 covariates (with <30% missingness) are incorporated as model input.
Runtime comparison among 6 candidate algorithms.
Frequency heatmap of top 20 features at 5-variable to 20-variable algorithms (step size = 1). (a) all-cause mortality; (b) mechanical ventilation including ECMO; (c) ARDS including respiratory failure; (d) ICU admission during final analysis, excluding covariates of post-admission treatment.
SHAP summary plot on 28-day mortality on aggregated datasets (test dataset and post-development prospective test dataset).
Sensitivity analysis on model performances (AUC) between non-imputed (in orange) and imputed data (in blue); (a) 28-day mortality; (b) 28-day ICU admission; (c) composite of 28-day ARDS and respiratory failure; (d) composite of 28-day ECMO and invasive ventilation usage. Left – test dataset; right – post-development prospective test dataset.
Sensitivity analysis on model performances (AUC) on non-imputed dataset with different thresholds of covariate coverage (10%, 30%, 50%, 70%, 80%, 90%) among the study cohort; (a) all-cause mortality; (b) ICU admission; (c) respiratory failure including ARDS; (d) invasive mechanical ventilation including ECMO. Left panel – test dataset; right panel – post-development prospective test dataset.
SHAP dependence plot between age and four outcomes (top left: 28-day mortality; top right: composite of 28-day ARDS and respiratory failure; bottom left: 28-day ICU admission; bottom right: 28-day ECMO or ventilator. The features are colored by (a) minimum SpO2 on admission; (b) respiration rate; (c) lymphocyte count; (d) BUN.
Gitlab repository.
Footnotes
Authors' Contributions: All the authors participated in literature search, conceptualization, data interpretation, reviewing, and editing the manuscript. JHP and FH were responsible for study design and methodology. FH performed the formal analysis and produced formatted tables and figures, and the original draft. KRW and AM conducted the initial feasibility analysis. All the authors have full access to the data in the study and accept responsibility to submit for publication.
Conflicts of Interest: FH, JHP, and AM are employees and stockholders of Amgen, Inc. KRW, an employee of League Inc, was formerly an employee of Amgen, Inc and owns stock in Amgen, Inc.
References
- 1.Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, Dunning J, Fairfield CJ, Gamble C, Green CA, Gupta R, Halpin S, Hardwick HE, Holden KA, Horby PW, Jackson C, Mclean KA, Merson L, Nguyen-Van-Tam JS, Norman L, Noursadeghi M, Olliaro PL, Pritchard MG, Russell CD, Shaw CA, Sheikh A, Solomon T, Sudlow C, Swann OV, Turtle LC, Openshaw PJ, Baillie JK, Semple MG, Docherty AB, Harrison EM, ISARIC4C investigators Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020 Sep 09;370:m3339. doi: 10.1136/bmj.m3339. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=32907855 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang W, Liang H, Ou L, Chen B, Chen A, Li C, Li Y, Guan W, Sang L, Lu J, Xu Y, Chen G, Guo H, Guo J, Chen Z, Zhao Y, Li S, Zhang N, Zhong N, He J, China Medical Treatment Expert Group for COVID-19 Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern Med. 2020 Aug 01;180(8):1081–1089. doi: 10.1001/jamainternmed.2020.2033. http://europepmc.org/abstract/MED/32396163 .2766086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818–29. [PubMed] [Google Scholar]
- 4.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996 Jul;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 5.Chen J, Chang S, Liu JJ, Chan R, Wu J, Wang W, Lee S, Lee C. Comparison of clinical characteristics and performance of pneumonia severity score and CURB-65 among younger adults, elderly and very old subjects. Thorax. 2010 Nov 21;65(11):971–7. doi: 10.1136/thx.2009.129627.65/11/971 [DOI] [PubMed] [Google Scholar]
- 6.Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, Yu S, Jing L, Li D, Huang J. Acute Physiology and Chronic Health Evaluation II Score as a Predictor of Hospital Mortality in Patients of Coronavirus Disease 2019. Crit Care Med. 2020 Aug;48(8):e657–e665. doi: 10.1097/CCM.0000000000004411. http://europepmc.org/abstract/MED/32697506 .00003246-202008000-00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yadaw A, Li YC, Bose S, Iyengar R, Bunyavanich S, Pandey G. Clinical features of COVID-19 mortality: development and validation of a clinical prediction model. The Lancet Digital Health. 2020 Oct;2(10):e516–e525. doi: 10.1016/S2589-7500(20)30217-X. https://linkinghub.elsevier.com/retrieve/pii/S2589-7500(20)30217-X .S2589-7500(20)30217-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014 Apr;48:193–204. doi: 10.1016/j.jbi.2014.02.013. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(14)00050-1 .S1532-0464(14)00050-1 [DOI] [PubMed] [Google Scholar]
- 9.Buuren SV, Groothuis-Oudshoorn K : Multivariate Imputation by Chained Equations in. J. Stat. Soft. 2011;45(3):1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- 10.Chen T, Guestrin C. XGBoost: A scalable tree boosting system. KDD '16: The 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining; August 13-17, 2016; San Francisco, CA, USA. 2016. Aug 13, pp. 785–794. [Google Scholar]
- 11.Li WT, Ma J, Shende N, Castaneda G, Chakladar J, Tsai JC, Apostol L, Honda CO, Xu J, Wong LM, Zhang T, Lee A, Gnanasekar A, Honda TK, Kuo SZ, Yu MA, Chang EY, Rajasekaran MR, Ongkeko WM. Using machine learning of clinical data to diagnose COVID-19: a systematic review and meta-analysis. BMC Med Inform Decis Mak. 2020 Sep 29;20(1):247. doi: 10.1186/s12911-020-01266-z. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-020-01266-z .10.1186/s12911-020-01266-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu C, Lei Q, Li W, Wang X, Liu W, Fan X, Li W. Clinical Characteristics, Associated Factors, and Predicting COVID-19 Mortality Risk: A Retrospective Study in Wuhan, China. Am J Prev Med. 2020 Aug;59(2):168–175. doi: 10.1016/j.amepre.2020.05.002. http://europepmc.org/abstract/MED/32564974 .S0749-3797(20)30218-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patrício André, Costa RS, Henriques R. Predictability of COVID-19 Hospitalizations, Intensive Care Unit Admissions, and Respiratory Assistance in Portugal: Longitudinal Cohort Study. J Med Internet Res. 2021 Apr 28;23(4):e26075. doi: 10.2196/26075. https://www.jmir.org/2021/4/e26075/ v23i4e26075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaid A, Jaladanki SK, Xu J, Teng S, Kumar A, Lee S, Somani S, Paranjpe I, De Freitas JK, Wanyan T, Johnson KW, Bicak M, Klang E, Kwon YJ, Costa A, Zhao S, Miotto R, Charney AW, Böttinger Erwin, Fayad ZA, Nadkarni GN, Wang F, Glicksberg BS. Federated Learning of Electronic Health Records to Improve Mortality Prediction in Hospitalized Patients With COVID-19: Machine Learning Approach. JMIR Med Inform. 2021 Jan 27;9(1):e24207. doi: 10.2196/24207. https://medinform.jmir.org/2021/1/e24207/ v9i1e24207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng F, Joshi H, Tandon P, Freeman R, Reich DL, Mazumdar M, Kohli-Seth R, Levin M, Timsina P, Kia A. Using Machine Learning to Predict ICU Transfer in Hospitalized COVID-19 Patients. J Clin Med. 2020 Jun 01;9(6):1668–1679. doi: 10.3390/jcm9061668. https://www.mdpi.com/resolver?pii=jcm9061668 .jcm9061668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parchure P, Joshi H, Dharmarajan K, Freeman R, Reich DL, Mazumdar M, Timsina P, Kia A. Development and validation of a machine learning-based prediction model for near-term in-hospital mortality among patients with COVID-19. BMJ Support Palliat Care. 2020 Sep 22;:1–8. doi: 10.1136/bmjspcare-2020-002602.bmjspcare-2020-002602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Z, Wang L, Huang L, Zhang M, Cai X, Xu F, Wu F, Li H, Huang W, Zhou Q, Yao J, Liang Y, Liu G. Efficient management strategy of COVID-19 patients based on cluster analysis and clinical decision tree classification. Sci Rep. 2021 May 05;11(1):9626. doi: 10.1038/s41598-021-89187-3. doi: 10.1038/s41598-021-89187-3.10.1038/s41598-021-89187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ke G, Meng Q, Finley T, Wang T, Chen W, Ma W, Ye Q, Liu T. A highly efficient gradient boosting decision tree. Adv Neural Inf Process Syst 2017; 31st Conference on Neural Information Processing Systems (NIPS 2017); Dec 4 - 7, 2017; Long Beach, CA, USA. LightGBM: 2017. pp. 3146–3154. [Google Scholar]
- 19.Guyon I, Weston J, Barnhill S, Vapnik V. Gene Selection for Cancer Classification using Support Vector Machines. Machine Learning. 2002;46(1):389–422. doi: 10.1023/A:1012487302797. [DOI] [Google Scholar]
- 20.Brier GW. Verification of Forecasts Expressed in Terms of Probability. Monthly Weather Review. 1950 Jan;78(1):1–3. doi: 10.1175/1520-0493(1950)078<0001:vofeit>2.0.co;2. [DOI] [Google Scholar]
- 21.Niculescu-Mizil A, Caruana R. Predicting Good Probabilities with Supervised Learning. Proceedings of the 22 nd International Conference on Machine Learning; Proceedings of the 22nd International Conference on Machine Learning; Aug 7 - 11, 2005; New York, NY. USA: Association for Computing Machinery; 2005. pp. 625–632. [DOI] [Google Scholar]
- 22.Goodhue. Lewis. Thompson Does PLS Have Advantages for Small Sample Size or Non-Normal Data? MIS Quarterly. 2012;36(3):981. doi: 10.2307/41703490. [DOI] [Google Scholar]
- 23.Stephens JR, Stümpfle Richard, Patel P, Brett S, Broomhead R, Baharlo B, Soni S. Analysis of Critical Care Severity of Illness Scoring Systems in Patients With Coronavirus Disease 2019: A Retrospective Analysis of Three U.K. ICUs. Crit Care Med. 2021 Jan 01;49(1):e105–e107. doi: 10.1097/CCM.0000000000004674. http://europepmc.org/abstract/MED/32991357 .00003246-202101000-00032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Capelastegui A, España P P, Quintana JM, Areitio I, Gorordo I, Egurrola M, Bilbao A. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006 Jan;27(1):151–7. doi: 10.1183/09031936.06.00062505. http://erj.ersjournals.com/cgi/pmidlookup?view=long&pmid=16387948 .27/1/151 [DOI] [PubMed] [Google Scholar]
- 25.Wellbelove Z, Walsh C, Perinpanathan T, Lillie P, Barlow G. Comparing the 4C mortality score for COVID-19 to established scores (CURB65, CRB65, qSOFA, NEWS) for respiratory infection patients. J Infect. 2021 Mar;82(3):414–451. doi: 10.1016/j.jinf.2020.10.015. http://europepmc.org/abstract/MED/33115655 .S0163-4453(20)30673-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu J, Xu F, Hui Zhou. Wu X, Shi L, Lu R, Farcomeni A, Venditti M, Zhao Y, Luo S, Dong X, Falcone M. Expanded CURB-65: a new score system predicts severity of community-acquired pneumonia with superior efficiency. Sci Rep. 2016 Mar 18;6(1):22911. doi: 10.1038/srep22911. doi: 10.1038/srep22911.srep22911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Early Warning Score (NEWS) 2. [2020-11-17]. https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 .
- 28.Carr E, Bendayan R, Bean D, O´Gallagher K, Pickles A, Stahl D, Zakeri R, Searle T, Shek A, Kraljevic Z, Teo Jt, Shah Am, Dobson Rj, Galloway Jb. Evaluation and improvement of the National Early Warning Score (NEWS2) for COVID-19: a multi-hospital study. BMC Med. 2021 Jan 21;19(1):23. doi: 10.1186/s12916-020-01893-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prower E, Grant D, Bisquera A, Breen CP, Camporota L, Gavrilovski M, Pontin M, Douiri A, Glover GW. The ROX index has greater predictive validity than NEWS2 for deterioration in Covid-19. EClinicalMedicine. 2021 May;35:100828. doi: 10.1016/j.eclinm.2021.100828. https://linkinghub.elsevier.com/retrieve/pii/S2589-5370(21)00108-5 .S2589-5370(21)00108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roca O, Messika J, Caralt B, García-de-Acilu Marina, Sztrymf B, Ricard J, Masclans J. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016 Oct;35:200–5. doi: 10.1016/j.jcrc.2016.05.022. doi: 10.1016/j.jcrc.2016.05.022.S0883-9441(16)30094-6 [DOI] [PubMed] [Google Scholar]
- 31.Lundberg SM, Erion G, Chen H, DeGrave A, Prutkin JM, Nair B, Katz R, Himmelfarb J, Bansal N, Lee S. From Local Explanations to Global Understanding with Explainable AI for Trees. Nat Mach Intell. 2020 Jan;2(1):56–67. doi: 10.1038/s42256-019-0138-9. http://europepmc.org/abstract/MED/32607472 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lundberg S, Lee S. A Unified Approach to Interpreting Model Predictions. 31st Conference on Neural Information Processing Systems (NIPS 2017); Dec 4 - 9, 2017; Long Beach, CA, USA. 2017. https://proceedings.neurips.cc/paper/2017/file/8a20a8621978632d76c43dfd28b67767-Paper.pdf . [Google Scholar]
- 33.Habibzadeh F, Habibzadeh P, Yadollahie M. On determining the most appropriate test cut-off value: the case of tests with continuous results. Biochem Med (Zagreb) 2016 Oct 15;26(3):297–307. doi: 10.11613/BM.2016.034. http://www.biochemia-medica.com/2016/26/297 .bm-26-297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Youden Wj. Index for rating diagnostic tests. Cancer. 1950 Jan;3(1):32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 35.Schisterman EF, Perkins NJ, Liu A, Bondell H. Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology. 2005 Jan;16(1):73–81. doi: 10.1097/01.ede.0000147512.81966.ba.00001648-200501000-00011 [DOI] [PubMed] [Google Scholar]
- 36.Shapiro DE. The interpretation of diagnostic tests. Stat Methods Med Res. 1999 Jun;8(2):113–34. doi: 10.1177/096228029900800203. [DOI] [PubMed] [Google Scholar]
- 37.Greiner M, Pfeiffer D, Smith R. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Preventive Veterinary Medicine. 2000 May;45(1-2):23–41. doi: 10.1016/S0167-5877(00)00115-XGet. doi: 10.1016/S0167-5877(00)00115-XGet. [DOI] [PubMed] [Google Scholar]
- 38.Vickers AJ, Van Calster B, Steyerberg EW. Net benefit approaches to the evaluation of prediction models, molecular markers, and diagnostic tests. BMJ. 2016 Jan 25;352:i6. doi: 10.1136/bmj.i6. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=26810254 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vickers AJ, van Calster B, Steyerberg EW. A simple, step-by-step guide to interpreting decision curve analysis. Diagn Progn Res. 2019;3:18. doi: 10.1186/s41512-019-0064-7. http://europepmc.org/abstract/MED/31592444 .64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subudhi S, Verma A, Patel AB, Hardin CC, Khandekar MJ, Lee H, McEvoy D, Stylianopoulos T, Munn LL, Dutta S, Jain RK. Comparing machine learning algorithms for predicting ICU admission and mortality in COVID-19. NPJ Digit Med. 2021 May 21;4(1):87. doi: 10.1038/s41746-021-00456-x. doi: 10.1038/s41746-021-00456-x.10.1038/s41746-021-00456-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bolourani S, Brenner M, Wang P, McGinn T, Hirsch JS, Barnaby D, Zanos TP, Northwell COVID-19 Research Consortium A Machine Learning Prediction Model of Respiratory Failure Within 48 Hours of Patient Admission for COVID-19: Model Development and Validation. J Med Internet Res. 2021 Feb 10;23(2):e24246. doi: 10.2196/24246. https://www.jmir.org/2021/2/e24246/ v23i2e24246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim H, Han D, Kim J, Kim D, Ha B, Seog W, Lee Y, Lim D, Hong SO, Park M, Heo J. An Easy-to-Use Machine Learning Model to Predict the Prognosis of Patients With COVID-19: Retrospective Cohort Study. J Med Internet Res. 2020 Nov 09;22(11):e24225. doi: 10.2196/24225. https://www.jmir.org/2020/11/e24225/ v22i11e24225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. 2021 Mar 09;372:n579. doi: 10.1136/bmj.n579. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33687922 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Driscoll Megan, Ribeiro Dos Santos Gabriel, Wang L, Cummings DAT, Azman AS, Paireau J, Fontanet A, Cauchemez S, Salje H. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021 Feb;590(7844):140–145. doi: 10.1038/s41586-020-2918-0.10.1038/s41586-020-2918-0 [DOI] [PubMed] [Google Scholar]
- 45.Zhou J, Lee S, Wang X, Li Y, Wu WKK, Liu T, Cao Z, Zeng DD, Leung KSK, Wai AKC, Wong ICK, Cheung BMY, Zhang Q, Tse G. Development of a multivariable prediction model for severe COVID-19 disease: a population-based study from Hong Kong. NPJ Digit Med. 2021 Apr 08;4(1):66. doi: 10.1038/s41746-021-00433-4. doi: 10.1038/s41746-021-00433-4.10.1038/s41746-021-00433-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Natarajan A, Su H, Heneghan C. Assessment of physiological signs associated with COVID-19 measured using wearable devices. NPJ Digit Med. 2020 Nov 30;3(1):156. doi: 10.1038/s41746-020-00363-7. doi: 10.1038/s41746-020-00363-7.10.1038/s41746-020-00363-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ok F, Erdogan O, Durmus E, Carkci S, Canik A. Predictive values of blood urea nitrogen/creatinine ratio and other routine blood parameters on disease severity and survival of COVID-19 patients. J Med Virol. 2021 Feb;93(2):786–793. doi: 10.1002/jmv.26300. http://europepmc.org/abstract/MED/32662893 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cheng A, Hu L, Wang Y, Huang L, Zhao L, Zhang C, Liu X, Xu R, Liu F, Li J, Ye D, Wang T, Lv Y, Liu Q. Diagnostic performance of initial blood urea nitrogen combined with D-dimer levels for predicting in-hospital mortality in COVID-19 patients. Int J Antimicrob Agents. 2020 Sep;56(3):106110. doi: 10.1016/j.ijantimicag.2020.106110. http://europepmc.org/abstract/MED/32712332 .S0924-8579(20)30293-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marjot T, Webb GJ, Barritt AS, Moon AM, Stamataki Z, Wong VW, Barnes E. COVID-19 and liver disease: mechanistic and clinical perspectives. Nat Rev Gastroenterol Hepatol. 2021 May;18(5):348–364. doi: 10.1038/s41575-021-00426-4. http://europepmc.org/abstract/MED/33692570 .10.1038/s41575-021-00426-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Razavian N, Major VJ, Sudarshan M, Burk-Rafel J, Stella P, Randhawa H, Bilaloglu S, Chen J, Nguy V, Wang W, Zhang H, Reinstein I, Kudlowitz D, Zenger C, Cao M, Zhang R, Dogra S, Harish KB, Bosworth B, Francois F, Horwitz LI, Ranganath R, Austrian J, Aphinyanaphongs Y. A validated, real-time prediction model for favorable outcomes in hospitalized COVID-19 patients. NPJ Digit Med. 2020;3:130. doi: 10.1038/s41746-020-00343-x. doi: 10.1038/s41746-020-00343-x.10.1038/s41746-020-00343-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu H, Chen J, Yang Q, Lei F, Zhang C, Qin J, Chen Z, Zhu L, Song X, Bai L, Huang X, Liu W, Zhou F, Chen M, Zhao Y, Zhang X, She Z, Xu Q, Ma X, Zhang P, Ji Y, Zhang X, Yang J, Xie J, Ye P, Azzolini E, Aghemo A, Ciccarelli M, Condorelli G, Stefanini GG, Xia J, Zhang B, Yuan Y, Wei X, Wang Y, Cai J, Li H. Development and validation of a risk score using complete blood count to predict in-hospital mortality in COVID-19 patients. Med (NY) 2021 Apr 09;2(4):435–447.e4. doi: 10.1016/j.medj.2020.12.013. http://europepmc.org/abstract/MED/33521746 .S2666-6340(20)30079-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bi X, Su Z, Yan H, Du J, Wang J, Chen L, Peng M, Chen S, Shen B, Li J. Prediction of severe illness due to COVID-19 based on an analysis of initial Fibrinogen to Albumin Ratio and Platelet count. Platelets. 2020 Jul 03;31(5):674–679. doi: 10.1080/09537104.2020.1760230. http://europepmc.org/abstract/MED/32367765 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kheir M, Saleem F, Wang C, Mann A, Chua J. Higher albumin levels on admission predict better prognosis in patients with confirmed COVID-19. PLoS One. 2021;16(3):e0248358. doi: 10.1371/journal.pone.0248358. https://dx.plos.org/10.1371/journal.pone.0248358 .PONE-D-20-38657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021 Feb 25;384(8):693–704. doi: 10.1056/NEJMoa2021436. http://europepmc.org/abstract/MED/32678530 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lim W S, van der Eerden M M, Laing R, Boersma W G, Karalus N, Town G I, Lewis S A, Macfarlane J T. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003 May;58(5):377–82. doi: 10.1136/thorax.58.5.377. https://thorax.bmj.com/lookup/pmidlookup?view=long&pmid=12728155 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaysin A, Viera AJ. Community-Acquired Pneumonia in Adults: Diagnosis and Management. Am Fam Physician. 2016 Nov 01;94(9):698–706. https://www.aafp.org/link_out?pmid=27929242 .d12810 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Model input and variable transformation. In the preliminary analysis, a total of 386 covariates with <30% missingness are incorporated as model input.
Summary of missingness of vital and lab variables among the study cohort.
Sensitivity analysis on model performances (AUC, 95% CI) between study cohort (n=50,703 in orange) and lab confirmed cohort (n=38,277 in blue) which is a subset of study cohort; (a) model performances on test dataset; (b) on post-development prospective test dataset.
Model performance (AUC) during preliminary analysis (top: test dataset (N=10,752); bottom: post-development prospective test dataset (N=14,863). In the preliminary analysis, a total of 386 covariates (with <30% missingness) are incorporated as model input.
Calibration curve during preliminary analysis (top panel: test dataset (N=10,752); bottom panel: post-development prospective test dataset (N=14,863)). In the preliminary analysis, a total of 386 covariates (with <30% missingness) are incorporated as model input.
Runtime comparison among 6 candidate algorithms.
Frequency heatmap of top 20 features at 5-variable to 20-variable algorithms (step size = 1). (a) all-cause mortality; (b) mechanical ventilation including ECMO; (c) ARDS including respiratory failure; (d) ICU admission during final analysis, excluding covariates of post-admission treatment.
SHAP summary plot on 28-day mortality on aggregated datasets (test dataset and post-development prospective test dataset).
Sensitivity analysis on model performances (AUC) between non-imputed (in orange) and imputed data (in blue); (a) 28-day mortality; (b) 28-day ICU admission; (c) composite of 28-day ARDS and respiratory failure; (d) composite of 28-day ECMO and invasive ventilation usage. Left – test dataset; right – post-development prospective test dataset.
Sensitivity analysis on model performances (AUC) on non-imputed dataset with different thresholds of covariate coverage (10%, 30%, 50%, 70%, 80%, 90%) among the study cohort; (a) all-cause mortality; (b) ICU admission; (c) respiratory failure including ARDS; (d) invasive mechanical ventilation including ECMO. Left panel – test dataset; right panel – post-development prospective test dataset.
SHAP dependence plot between age and four outcomes (top left: 28-day mortality; top right: composite of 28-day ARDS and respiratory failure; bottom left: 28-day ICU admission; bottom right: 28-day ECMO or ventilator. The features are colored by (a) minimum SpO2 on admission; (b) respiration rate; (c) lymphocyte count; (d) BUN.
Gitlab repository.


