Introduction
The first renal transplant in Turkey was performed in 1968 at the Ista nbul University Medical School (1). However, the patient died due to ventricular fibrillation at the seventh postoperative hour (1). The first successful renal transplant in Turkey was performed at Hacettepe University by Dr. Mehmet Haberal and his colleagues in 1975, which involved a transplant from a mother to her child. This was followed by the first deceased-donor kidney transplantation in 1978, using an organ supplied by Eurotransplant (2). The law on harvesting, storage, and transplantation of organs and tissues was enacted in 1979; later that year, the first local deceased-donor kidney transplantation was performed by the same team. In 2001, the Turkish Ministry of Health established the National Coordination Center to promote transplantation activities and deceased-donor organ procurement ( 3). Currently, the Organ Transplantation Regulatory Unit is a subdivision of the Ministry of Health. From 2008 to 2020, a total of 33,028 renal transplants and 13,135 liver transplants have been performed, as compared with 728 heart transplants, 276 lung transplants, 65 pancreas transplants, according to the publicly available online registry of the Ministry of Health (4). Despite the large number of living-donor renal and liver transplants performed in Turkey, the number of heart, lung, pancreas, and intestinal operations and overall deceased-donor transplants are quite behind due to various factors, including low rates of deceased donation compared with Europe or the United States. According to the most recent reports from the International Organ Registry in Organ Donation and Transplantation, Turkey ranked first globally for the overall living-donor transplant rate (53.02 per million population [pmp]) and for living-donor renal transplant activity (36.64 pmp); however, Turkey was 42nd for overall deceased-donor transplant rates (at only 7.54 pmp), compared with the top three countries (Unites States, Spain and Portugal; 38.35, 37.40, and 33.80 pmp, respectively) (5,6). The deceased-donor kidney transplant rate for Turkey was 10.45 pmp (6).
Current Status of Renal Transplant in Turkey
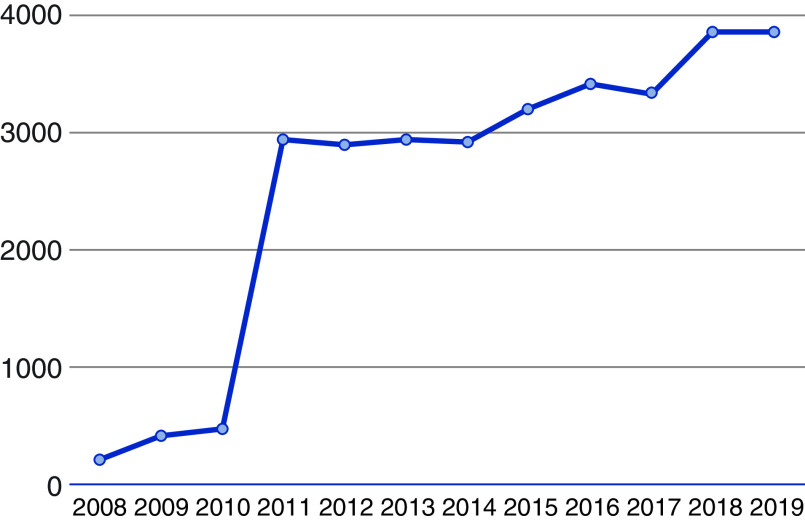
The annual number of renal transplants has been increasing steadily in Turkey (Figure 1). There were 20,857 patients listed for renal transplant as of 2020 (4). As of 2021, there were 78 renal transplant programs and six pancreas transplants programs listed in the country (4). There have been some major changes in the Turkish transplant regulations. First, during 2008–2010, the Ministry of Health made substantial increases in financial incentives for kidney tr ansplants. Second, the Ministry of Health gave permission for the private hospitals to perform kidney transplants. Before these regulations, only state hospitals and state universities were eligible to perform transplants. Third, there has been increase in education, for medical providers and the public, regarding organ donation. Because of these changes, the annual number of renal transplants has increased dramatically since around 2010 (Figure 1). All transplant programs and activities are closely monitored and strictly reported to the Ministry of Health. Another important data source is the Turkish Society of Nephrology (TND), which was founded in 1970. The TND initiated a reporting system in 1990 and collects data from participating centers, and their annual reports are publicly available. A caveat to the TND reports is that they do not include all centers in the country.
Figure 1.
Trend of renal transplant activity in Turkey. Data obtained from the websites of the Turkish Ministry of Health and the Turkish Society of Nephrology (7).
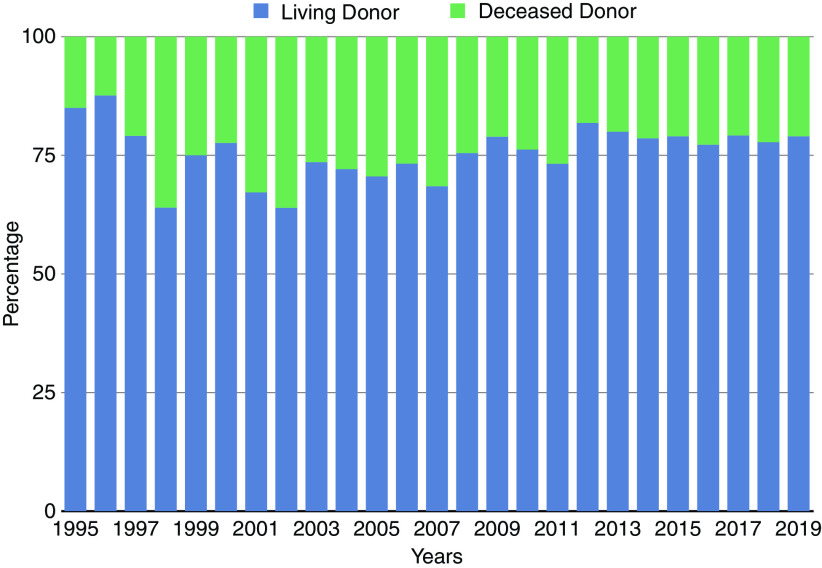
With all of these limitations in mind, the 1-year renal graft survival was 94%, acc ording the latest TND report from 2019 (7); survival was 96% for living-donor renal transplants and 86% for deceased-donor renal transplants (Table 1). Of all of the renal transplants in 2019, only 805 (21%) were from deceased donors, whereas the remaining 3053 (79%) were from living donors; the majority (63%) of the living donations were from relatives, and 22% were from unrelated donors (7). The distribution of living- and deceased-donor renal transplants for the last two decades is shown in Figure 2. Deceased-donor rates decreased further in 2020 due to the coronavirus disease 2019 pandemic and increased rates of organ discard.
Table 1.
Outcomes of renal transplants performed in 2019
| Outcome | n | % |
| Functioning graft (all transplants) | 3632 | 94 |
| Returned to dialysis | 45 | 1 |
| Retransplant | 16 | 0.41 |
| Death | 165 | 4 |
| Total | 3858 | 100 |
| Functioning graft (living donor) | 2937 | 96 |
| Returned to dialysis | 26 | 0.85 |
| Retransplant | 3 | 0.10 |
| Death | 87 | 3 |
| Total | 3053 | 100 |
| Functioning graft (deceased donor) | 695 | 86 |
| Returned to dialysis | 19 | 2 |
| Retransplant | 13 | 2 |
| Death | 78 | 10 |
| Total | 805 | 100 |
Adapted from the Turkish Society of Nephrology (7).
Figure 2.
Distribution of living- and deceased-donor renal transplants since 1995. Adapted from ref. 7, with permission.
Donor exchange is legally allowed in Turkey, but a national, paired exchange program is still under preparation and is not active as of 2021. Individual kidney exchange is possible between families and is facilitated within each individual transplant program. The rate of paired exchange in 2019 was 6%, which was similar to that in 2018 (7).
The rate of pre-emptive transplantation was higher in 2019 compared with 2018 (46% versus 44%, respectively). The TND report stated that the high rates of pre-emptive renal transplant raise concerns about the timing of transplantation (7). Half of the patients were on hemodialysis and only 4% were on peritoneal dialysis.
Pediatric Renal Transplant
According to the TND report, 13 centers participated in the pediatric transplant registry in 2019 (7). There were 89 pediatric patients who underwent renal transplants in 2019. In contrast, the Ministry of Health data state that there were 329 total pediatric renal transplants for 2019, which means only 27% of all pediatric cases were captured in the TND report. Despite this sampling limitation, the TND report also includes the following information: of the 89 pediatric patients, 91% were living-donor transplants, and 29% were pre-emptive transplants. Although there were three graft losses, patient survival was 100% at 1 year. The top three etiologies of renal failure in pediatric patients were vesicoureteral reflux and recurrent urinary tract infections (23%), primary GN (20%), and the “other” category (27%) (7).
Trends of ESKD
Turkey is ranked 23rd for the incidence of ESKD according to the most recent United States Renal Data System Annual Data Report (8). The average annual change in incidence of treated ESKD by country or region, for 2009–2010 versus 2017–2018, showed that the incidence of ESKD decreased in Israel, Norway, Sweden, Italy, Bosnia and Herzegovina, Colombia, Chile, and Turkey (6). The primary etiologies of ESKD in Turkey were classified as follows: diabetes (21%), GN (20%), hypertension (18%), polycystic kidney disease (6%), obstructive nephropathy (5%), tubulointerstitial nephritis (3%), amyloidosis (3%), and unknown etiology (16 %) (7).
Transplant Surgery and Post-Transplant Care
Kidney transplants are primarily performed by urologists at 16 of the 78 (20%) centers in Turkey. High-volume centers (i.e., 100 renal transplants per year) constitute ≤20% of all programs. The training certification process for renal transplant surgery is undertaken through the Ministry of Health. General surgeons, urologists, or pediatric surgeons can apply for any institution listed by the Ministry of Health. Surgeons collect points in the following criteria for the certification process: (1) working for a minimum of 6 months at a center where at least 15 renal transplants per year are performed; (2) working in the first assistant and primary surgeon role for the recipient operation; (3) participating in a donor nephrectomy surgery; and (4) carrying out academic activities (publishing peer-reviewed article, review, or book chapter) with a foc us on renal transplant. Each category is associated with a different number of points which contributes toward certification, and final approval is given by the Ministry of Health. Transplant nephrology remains a rotation within the nephrology fellowship of the internal medicine specialty, which also has a similar certification system. The follow-up of patients who have received a renal transplant is mainly performed by transplant nephrologists. Recipient and donor costs, including lifelong immunosuppression, are covered by the universal health care system, but lodging and travel expenses are not included.
Conclusion
Despite the limited access to long-term patient and graft survival data, the 1-year graft and patient survival is excellent after living-donor kidney transplants and is good after deceased-donor renal transplants in Turkey. Turkey ranks first globally for rates of living-donor renal transplants. Countries that need to expand their living-donor transplant numbers could focus on incentivizing transplant programs. Although this may not be an easily achievable goal, there could be other external resources for this purpose (i.e., private funds or donations). Turkey has significant experience in living-donor transplants; however, the deceased-donor system should be augmented, prioritized, and perhaps incentivized in financial and nonfinancial ways. The possible areas for improvement could be summarized as a need for increased public awareness, increased training and education among medical providers and medical staff, the formation of independent personnel to approach families, the implementation of regulations facilitating or promoting deceased donation, and consideration for specific donor management teams (either within the same institute or independent teams). This would also allow us to expand other lifesaving organ transplants, including those of the heart, lung, pancreas, and intestine. These improvements would require a systematic, long-term commitment from both the Ministry of Health and the transplant providers. We can further strengthen the system with publicly available, long-term graft and patient outcomes. This will not only allow patients to be able to choose where they wish to have their transplants performed, but will also increase the quality of the centers by pushing them to reach better long-term outcomes and decrease the outcome variations among centers. Lastly, a standardized national transplant fellowship curriculum, structured by professional transplant societies and formal board certifications, and recognition of transplantation as a formal subspecialty, both in medicine and surgery, are mandatory. We believe this would further raise the bar in transplant quality nationally.
Disclosures
All authors have nothing to disclose.
Funding
None.
Acknowledgments
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
The authors thank the editorial team of Kidney360 sincerely for their support and assistance for the language edits.
Author Contributions
F.T. Aki provided supervision; F.T. Aki and O. Andacoglu were responsible for methodology and reviewed and edited the manuscript; and O. Andacoglu conceptualized the study, wrote the original draft, and was responsible for data curation and investigation.
Footnotes
This article contains a podcast at https://dts.podtrac.com/redirect.mp3/www.asn-online.org/media/podcast/K360/2021_07_29_KID0002542021.mp3
References
- 1.San A, editor: Turk Nefroloji Tarihi, Ankara, Turkey, Anadolu Bobrek Vakfi, 2002 [Google Scholar]
- 2.Karakayali H, Haberal M: The history and activities of transplantation in Turkey. Transplant Proc 37: 2905–2908, 2005. 10.1016/j.transproceed.2005.07.025 [DOI] [PubMed] [Google Scholar]
- 3.Haberal M: Transplantation in Turkey. Clin Transpl 175–180, 2013 [PubMed] [Google Scholar]
- 4.Turkish Ministry of Health: TDIS KDS Public Information Pages, Organ Transplant Registry. Available at: https://organkds.saglik.gov.tr/dss/PUBLIC/Transplant_Solid_Organ.aspx. Accessed May 21, 2021
- 5.Donation and Transplantation Institute: International Registry in Organ Donation and Transplantation. Available at: https://www.irodat.org/?p=publications. Accessed May 21, 2021
- 6.Donation and Transplantation Institute: International Registry in Organ Donation and Transplantation: Final numbers 2019, 2020. Available at: https://www.irodat.org/img/database/pdf/Newsletter%20Dec%202020%20.pdf. Accessed May 21, 2021
- 7.Turkish Society of Nephrology: Registry of the Nephrology, Dialysis and Transplantation in Turkey: Registry 2018, 2019. Available at: http://www.nefroloji.org.tr/folders/file/REGISTRY_2018.pdf. Accessed May 21, 2021
- 8.United States Renal Data System: Chapter 11: International Comparisons. In: 2020 Annual Data Report, 2020. Available at: https://adr.usrds.org/2020/end-stage-renal-disease/11-international-comparisons. Accessed May 21, 2021