Visual Abstract

Keywords: dialysis, animation, arteriovenous, catheter, education, fistula, graft, hemodialysis, mixed methods, stakeholder, vascular access, video
Key Points
Guided by 105 stakeholders, we developed mixed-media vascular access education materials that acknowledge common patient concerns.
Preliminary findings suggest that the education materials are promising to improve vascular access understanding among patients.
Abstract
Background
Initiating hemodialysis via an arteriovenous (AV) access is considered best practice for most patients. Despite the well-recognized advantages of AV access, 80% of US patients start hemodialysis with a catheter. Limited patient knowledge about vascular access, among other factors, may play a role in this high rate. We used iterative stakeholder input to develop novel, mixed media vascular access education materials and evaluated their preliminary acceptability.
Methods
We conducted preliminary focus groups and interviews with key stakeholders to assess patient vascular access understanding and elicit perspectives on existing education materials. We then used stakeholder input to inform initial development and iterative updates to the content and design of an animated video and complementary brochure. Video development (scripting, storyboarding, animation) was guided by an evidence-based framework and two health behavior change models. We assessed acceptability of the completed materials with patients and medical providers/personnel via interviews.
Results
Overall, 105 stakeholders participated in education materials development and review (80 patients/care partners, 25 medical providers/personnel). Preliminary qualitative work included 52 patients/care partners and 16 providers/personnel; video development included 28 patients/care partners and nine providers/personnel. The video script, storyboards, and animation underwent 14, four, and nine stakeholder-guided iterations, respectively. Responsive changes included aesthetic modifications, technical updates, and content additions (e.g., HD circuit, access self-monitoring, enhanced patient testimonials). The final 18-minute video and complementary brochure define vascular access types, describe care processes, outline potential complications, and address common patient concerns. Interviews with 28 patients/care partners and nine providers/personnel from diverse geographic regions revealed preliminary acceptability of, and enthusiasm for, the materials by patients and providers.
Conclusions
In collaboration with key stakeholders, we developed mixed media vascular access education materials that were well-received by patients and providers. Preliminary findings suggest that the materials are promising to improve vascular access understanding among patients.
Introduction
Initiating hemodialysis (HD) via an arteriovenous (AV) access is considered best practice for most patients. Compared with central venous catheters, AV accesses are associated with lower risk for infection, cardiovascular events, hospitalizations, and death (1–3). Despite the well-recognized advantages of AV access, 80% of US patients start HD with a catheter (4). Although complex barriers related to the health system (e.g., insufficient interprovider communication), the patient (e.g., emotional distress), and clinical status (e.g., uncertainty about time to kidney failure) contribute to this high rate (5–7), limited patient understanding of vascular access may also play a role.
Health education interventions have the potential to enhance understanding, improve self-management, and positively affect health outcomes among individuals with CKD (8). However, we lack standardized approaches to vascular access education and related care processes. Currently, such education is combined with programs about kidney failure treatment options, despite the unique emotional experiences and clinical complexities associated with vascular access. Although written education resources exist (9–12), their use is variable, and most materials do not directly address patient concerns, such as worries about dialysis, needles, and/or disfigurement. As such, there is a need for novel vascular access education approaches that are patient-centered and are delivered at an appropriate health literacy level. Emerging data suggest that animating health information can enhance learning and retention across literacy levels (13–16).
Accordingly, our objective was to develop mixed media vascular access education materials that acknowledge patient emotions (e.g., fear, reluctance) while providing realistic insight into the care steps and potential complications that may arise during the process of creating a viable AV access. Throughout the project, we used iterative stakeholder input to guide content, imagery, and tone. We then evaluated the preliminary acceptability of the developed materials with stakeholders.
Methods
Overview
Figure 1 depicts project activities. In preliminary focus groups and interviews, stakeholders identified the lack of mixed media, patient-centered education materials as a barrier to AV access-based HD initiation. In response, we developed a vascular access education brochure and produced an animated video. We used iterative stakeholder input to inform material content and design.
Figure 1.
The 7-step process of stakeholder-guided dialysis vascular access education materials development resulted in a final education package comprised of an animated video and complementary brochure. aPatients with advanced CKD and dialysis-dependent ESKD, medical providers, and clinic personnel with experience in vascular access creation and maintenance processes.
The preliminary focus groups, interviews, and draft education brochure assessment were conducted as part of a broader Geisinger Health quality improvement (QI) project, aiming to improve rates of AV access–based HD initiation (17). These activities were approved by the Duke Health Institutional Review Board (IRB; Pro00075488). Video development activities were approved by the University of North Carolina (UNC) IRB (20-0369). Participants provided informed consent.
Preliminary Focus Groups, Interviews, and Draft Brochure
We conducted focus groups and interviews with stakeholders from Geisinger Health in Danville, Pennsylvania, and UNC Health in Chapel Hill, North Carolina. Care partners and patients with nondialysis-dependent advanced CKD (eGFR ≤20 ml/min per 1.73 m2) and a preference for HD, or HD-dependent kidney failure who initiated HD within 1 year, were eligible for focus groups. Interviewees included nephrologists, surgeons, interventionalists, and clinic personnel. Research coordinators recruited patients and providers using IRB-approved in-person and over-the-telephone recruitment scripts. We used purposive sampling to recruit individuals with diverse vascular access care experiences and professional roles. Two research coordinators (one from each site) with prior experience in qualitative data collection completed joint training to ensure standardized use of this project’s moderator and interview guides (Supplemental Table 1). In addition, the research coordinators received training about vascular access from a CKD educator, nephrologist, and two patients with vascular access experience. Both coordinators performed a mock interview, observed by the principal investigator, before research data collection. All research interactions were recorded and professionally transcribed.
Findings were used to draft a preliminary vascular access education brochure for the Geisinger Health QI project (17). During the QI project, we collected user feedback (patient, medical provider/personnel) through semistructured interviews to inform brochure modifications and video development.
Video Development and Production
Strategy and Target Population
We used Williams et al.’s (18) adaptation of the Medical Research Council framework for the development of visually based interventions to guide video development. The framework has four stages: (1) selecting a theoretic basis, (2) developing a narrative to establish structure, (3) storyboarding and creating imagery, and (4) establishing acceptability and understanding. We aimed to develop a 15-minute video to balance the need to communicate detailed information without overtaxing the viewer. Our target audience is people planning for HD as a treatment for kidney failure and their social supports. Ideally, the materials would be used in the dialysis preparatory phase to support pre-emptive AV access creation. However, the information is also relevant to individuals who have already initiated HD.
Development Process
Selecting a Theoretic Basis
Our video objectives were to: (1) improve understanding of vascular access and potential complications, (2) increase the perceived benefits of AV access, (3) reduce uncertainty surrounding vascular access care processes, and (4) increase self-efficacy in navigating such processes. To guide video content and format, we drew upon two health behavior change models derived from social psychologic theories: the health belief model and Leventhal et al.’s self-regulation model (19–21).
Developing a Narrative
After selecting the theoretic bases, we worked with stakeholders to draft and iteratively refine the script, using the principles from Hill-Briggs et al.’s (22) five-step methodology for adaptation of patient health information to achieve a fifth-grade reading level. Specifically, we used short sentences with active (versus passive) voice, and defined essential medical terms (e.g., thrill, bruit, cannulation) (22). We used transitions between a professional narrator and a patient narrator to retain viewer attention and reinforce important concepts.
Storyboarding and Creating Imagery
A professional animator (T.O.) then drafted storyboards. The animator selected subway imagery to depict the “journey” and visually communicate the nonlinear aspects of associated care. This approach naturally supported the patient recommendation of content segmentation through subway stops. We incorporated photographs of real vascular accesses and ultrasound images to supplement animated graphics.
Animation and Sound Production
The animator then converted the static storyboard images into flowing video sequences, and a professional audio engineer added the narrations, background music, and supporting sound effects to create a cohesive narrative.
Acceptability and Understanding
We conducted stakeholder interviews to establish preliminary acceptability and understanding of the video content.
Stakeholder Input
Throughout video development, we gathered stakeholder input through semistructured interviews. Using the same recruitment criteria and strategies as for the preliminary data collection, we recruited participants from UNC Health–affiliated practices. In addition, we relied on a patient database to recruit patients from other health systems who had previously expressed interest in learning about research opportunities. All interviews were conducted by an experienced interviewer using standardized guides (Supplemental Table 1). The master’s trained interviewer has >4 years of experience performing semistructured research interviews with individuals with kidney disease, their providers, and other relevant stakeholders.
During script-related interviews, interviewees read along with an audio-recorded script; the interviewer sought input on content, narration style and pacing, and potential visual supports. The script underwent 14 stakeholder-driven iterative revisions. During storyboard and video interviews, interviewees examined storyboards or the video (in part or in whole); the interviewer sought feedback on graphics, sound effects, and flow. Interview questions focused on content completeness, technical accuracy, design, and patient-centeredness. In cases where we made responsive technical changes (e.g., thrombectomy animation, needle positioning) or content additions (e.g., HD circuit, access self-monitoring), we returned to the recommending stakeholders to affirm the updates. The storyboards and video underwent four and nine stakeholder-driven iterative revisions, respectively.
Alignment of Video and Written Materials
We then updated the content and aesthetics of the preliminary brochure to match the video by: (1) aligning wording and definitions, (2) adding stakeholder-recommended topics, and (3) incorporating video imagery. We assessed acceptability of the final materials with patients/care partners and medical providers/personnel via interviews.
Statistical Analysis
We used descriptive statistics (count with percentage, median with interquartile range [IQR] to report participant characteristics and materials’ acceptability. We imported preliminary focus group and interview data transcriptions into ATLAS.ti software (version 7, Berlin, Germany), and used directed content analysis to identify barriers to vascular access care (23–25), focusing on education-related gaps for this presented work. Three researchers used line-by-line coding to group text according to education-related deficiencies (e.g., content, style, reading level). Specifically, the data were split into smaller units, named on the basis of their content, and then grouped according to conceptual similarities (25). Through iterative discussion (i.e., triangulation), researchers resolved discrepancies and reached consensus on the coding scheme.
During video development and production, we analyzed stakeholder interviews to guide revisions to the script, storyboards, and video. Data were compiled in tables organized by video development stage, interviewee type, and material aspect (e.g., content, tone, imagery). Two researchers independently reviewed and coded the data to identify content for potential revision. When considering responsive changes, we weighted information provided by two or more interviewees. To ensure validity and credibility, we performed member checking (i.e., participant validation), where we asked participants to review the education material changes made in response to their initial interviews and confirm their accuracy (26). We considered development steps complete when member checking produced no suggested revisions. We deemed the materials final when acceptability testing yielded >90% acceptability and stakeholders suggested no further modifications.
Results
Participant Characteristics
Table 1 depicts project participants. Preliminary qualitative work, conducted to identify deficiencies in existing vascular access education materials, included four focus groups with 18 patients (nine patients on HD, nine patients with advanced CKD), six care partners, and 16 individual interviews with providers/personnel, all from Geisinger Health and UNC Health. During the Geisinger Health vascular access QI project, 28 people with advanced CKD (median [IQR] eGFR of 21 [17–24] ml/min per 1.73 m2) reviewed the preliminary education brochure.
Table 1.
Participant characteristics
| Characteristic | Focus Groups and Interviews (N=40) | Draft Brochure Review (N=28) | Animated Video Review (N=37)a |
| Patients and care partners, n | 24 | 28 | 28 |
| Participant type, n (%) | |||
| Patient on HD | 9 (38) | 0 | 6 (21) |
| Patient with a transplant | 0 | 0 | 1 (4) |
| Patient with CKD stage 4 | 5 (21) | 23 (82) | 6 (21) |
| Patient with CKD stage 5 | 3 (13) | 5 (18) | 12 (43) |
| Patient with unknown CKD stage | 1 (4) | 0 | 0 |
| Care partner | 6 (25) | 0 | 3 (11) |
| Geographic region, n (%) | |||
| Southeastern United States | 11 (46) | 0 | 10 (36) |
| Northeastern United States | 13 (54) | 28 (100) | 8 (29) |
| Midwestern United States | 0 | 0 | 3 (11) |
| Western United States | 0 | 0 | 5 (18) |
| Europe | 0 | 0 | 2 (7) |
| Age (yr), median (IQR) | 65 (60–73) | 63 (58–74) | 58 (52–77) |
| Female, n (%) | 12 (50) | 9 | 15 (54) |
| Race, n (%) | |||
| Black | 7 (29) | 0 | 12 (43) |
| White | 13 (47) | ||
| Other | 17 (71) | 28 (100) | 3 (11) |
| Highest level of education completed, n (%) | — | ||
| Some high school | 2 (8) | 2 (7) | |
| High school graduate or GED | 12 (50) | 10 (36) | |
| Some college | 3 (13) | 5 (18) | |
| ≥4 Year college degree | 7 (29) | 11 (39) | |
| Vascular access type, n (%) | |||
| Fistula | 16 (67) | 0 | 4 (14) |
| Graft | 1 (4) | 0 | 4 (14) |
| Catheter | 2 (8) | 0 | 3 (11) |
| Fistula and catheter b | 1 (4) | 0 | 2 (7) |
| None | 3 (13) | 28 (100) | 15 (54) |
| Missing | 1 (4) | 0 | 0 |
| Clinic personnel and medical providers, n | 16 | 0 | 9 |
| Professional role, n (%) | |||
| Nephrology provider c | 3 (19) | 4 (44) | |
| Surgeon | 2 (13) | 1 (11) | |
| Interventionalist | 2 (13) | 2 (22) | |
| Nurse | 8 (50) | 2 (22) | |
| Nephrology scheduler | 1 (6) | 0 | |
| Geographic region, n (%) | — | ||
| Southeastern United States | 8 (50) | 7 (78) | |
| Northeastern United States | 8 (50) | 2 (22) | |
| Age (yr), median (IQR) | 42 (38–51) | — | 46 (37–63) |
| Female, n (%) | 11 (69) | — | 6 (67) |
| Race, n (%) | |||
| Black | — | 1 (11) | |
| White | 12 (75) | 6 (67) | |
| Other | 4 (25) | 2 (22) | |
| Time worked in role (yr), median (IQR) | 7 (5–9) | — | 5 (4–11) |
HD, hemodialysis; IQR, interquartile range; GED, General Educational Development.
Of the 37 participants, eight individuals participated in more than one interview.
Individuals dialyzing via catheter while arteriovenous access was healing or maturing.
Nephrology provider includes physicians and advanced practice providers.
Video development and review participants included 28 patients (six with HD, 18 with advanced CKD, one with a transplant), three care partners, and nine providers/personnel. Among patient participants, the median (IQR) age was 58 (52–77) years, and 12 (43%) had a high school degree or less. Among provider participants, the median (IQR) time serving in their role was 5 (4–11) years.
Education-Related Findings from Preliminary Focus Groups and Interviews
In focus groups, patients and care partners reported feeling uncertain navigating vascular access care processes and identified the need for more comprehensive, patient-centered education materials (Supplemental Table 2). They also emphasized inclusion of patient testimonials to acknowledge and validate emotional experiences (e.g., reluctance, fear). Patients underscored the importance of frankly describing the variable experiences and potential complications associated with viable AV access creation. In interviews, providers affirmed the importance of the aforementioned points, reflecting on their own experiences with patients who were unprepared to participate in shared decision making or manage common complications due to limited understanding of vascular access. Patients and providers acknowledged that the breadth of information could overwhelm audiences, and therefore suggested segmenting the material by presenting vascular access care processes as a multistep “journey.” We used these findings to inform development of a preliminary vascular access education brochure.
Initial Testing of Draft Education Brochure
Overall, patients responded positively to the preliminary education brochure’s content, format, and length (Supplemental Table 3). Specifically, the “journey” concept clearly depicted the steps involved in getting a vascular access, and the provided definitions improved understanding of terminology. Of the 28 patients who reviewed the brochure, 27 (96%) would recommend it to other patients. Several patients suggested developing a video to reinforce and expand upon the brochure concepts, citing a desire for more in-depth information that could accommodate different learning styles.
Stakeholder-Informed Video Development
Supplemental Table 2 contains participant quotations from all stages of materials development. Table 2 displays a summary of the stakeholder input and responsive script, storyboard, and video changes. Specifically, input was obtained from 21 individual participants (12 patients, nine providers) across 47 unique interactions. Figure 2 provides examples of stakeholder-informed, patient-centered concepts applied during video development.
Table 2.
Stakeholder feedback on the video and responsive changes
| Script and Storyboarding Feedback | Responsive Change(s) | Video Feedback |
| Patients | ||
| Helpful information, but some details unnecessary | Shortened technical descriptions | Good overview that stimulates questions, equips patients for care team conversations |
| Patient-narrated portion is essential, well-timed, and relatable | Included patient’s voice and image throughout video | Patient story is influential, clarifies information, and eases fears/concerns |
| “Journey” concept is intuitive; subway imagery is clear; detours imply different experiences | Added more examples of potential detours to highlight variability in individual experiences | Steps to get an access are easy to follow; transparent content prepares individuals by providing a complete and truthful picture |
| Add more information about day-to- day life with a vascular access | Added patient-suggested daily activities, questions, and worries | Examples contextualize the information |
| Cartoons are effective at imparting complex information, but should be paired with real imagery | Added vascular access photographs and ultrasound images | Animation complements the script and is easy to understand; vibrant colors, pace, and tempo facilitate interest |
| Providers | ||
| Content is comprehensive, but ranges from too technical to too nonspecific | Removed excess detail (e.g., term “blood flow rate”); updated overly simplified concepts (e.g., added detail about access self-assessments) | Addresses common concerns and key topics at an appropriate health literacy level; relevant for both patients with advanced CKD and those who are HD dependent |
| Amount of information is difficult to digest, but topics are critical to include | Reordered information; summarized key concepts in patient-narrated portions | Good flow; summaries support learning and bring humanity to technical detail |
| Provide context to make animation clearer | Added orienting imagery and labels | Animations are accurate and support learning |
Figure 2.
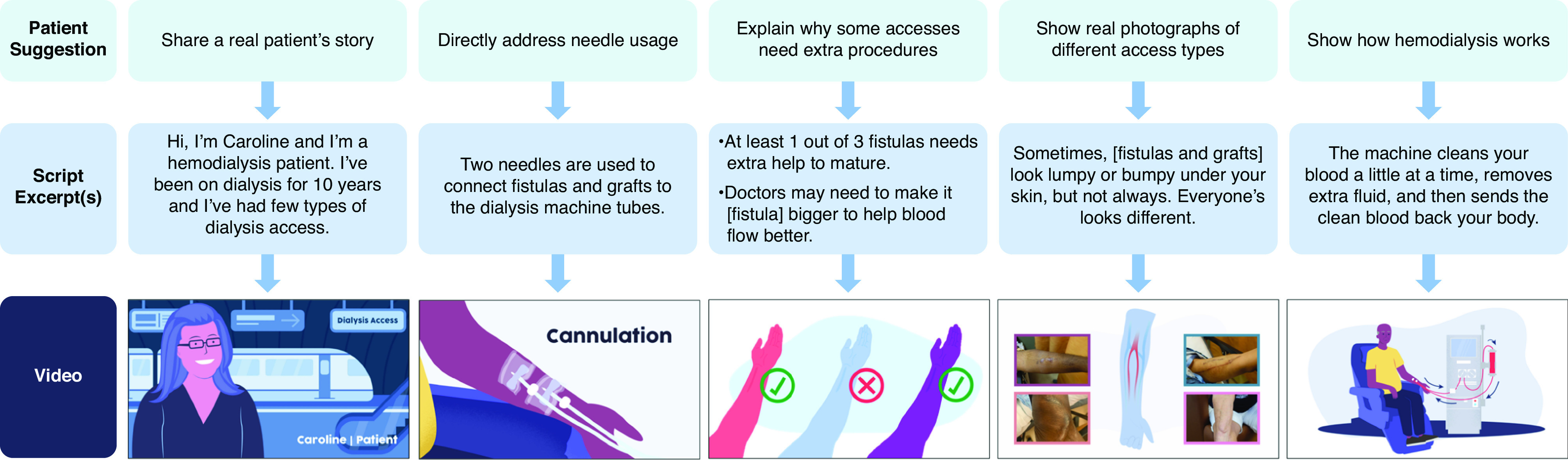
Stakeholder suggestions guided several modifications to the video script (e.g., content, tone), storyboards (e.g., color, identifying labels), and animation (e.g., procedures) to enhance patient-centeredness. We used patient suggestions from focus groups and interviews to guide patient-centered concept inclusion throughout video development.
Script Development
In early script interviews, stakeholders affirmed the importance of the included concepts, but suggested simplifying technical descriptions and elaborating on practical aspects (e.g., influence on the patient’s life, timeline). Patients and providers recommended adding information about vascular access maintenance procedures (e.g., angioplasty, catheter thrombolysis) and providing more detail about HD (e.g., cannulation, dialysis circuit). In general, interviewees appreciated repeated information to facilitate understanding, but a few considered the redundancy a distraction. In response, we shortened or spaced out repeat descriptions. Related, we consolidated the interspersed patient testimonials into summary sections at each “journey stop.” In near-final script interviews, stakeholders reported these changes effectively signaled content transitions, reinforced key information, and, most importantly, infused the script with humanity and “real-life” experiences. In addition, stakeholder input guided word changes to promote technical accuracy and an appropriate health literacy level (e.g., incorporating and defining terms such as “vessel mapping” and “maturing”). The script was deemed “final” upon interviewee approval of modifications during member checking.
Storyboard and Video Development
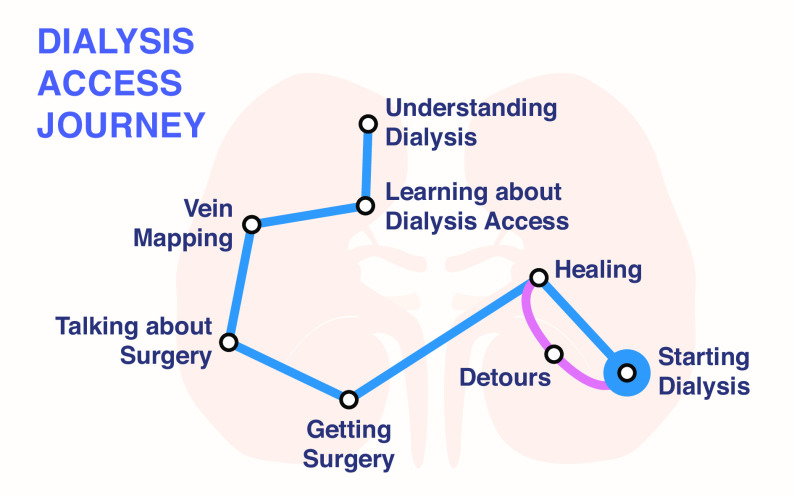
In storyboard and early video interviews, stakeholders suggested modifying the color palette to reflect more diverse skin tones, enlarging font size, adding real imagery, and using on-screen text to signal key terms. Many patients expressed concerns about body disfigurement. One woman said, “…I’m so concerned that my arm is gonna look like some incredible hulk.” In response, we added photographs of vascular accesses to showcase their variability in appearance. Patients preferred that procedures remain animated to avoid unnecessarily detailed depictions. Interviewees also suggested incorporating a “vascular access journey map” throughout the video to illustrate progress and depict the nonlinear nature of the experience (Figure 3).
Figure 3.
To help patients navigate their vascular access journeys, the video comprises eight “journey stops” (understanding dialysis, learning about dialysis access, vein mapping, talking about surgery, getting surgery, healing, detours, and starting dialysis). This animated map is coupled with audio aids and appears throughout the video to signal a new “stop,” or a change in the video content. It also serves as an indicator of video progress.
Final Video Production
In near-final video interviews, stakeholders reported satisfaction with animation updates, citing improvements in the depiction of content often perceived as dull and complex. Only minor refinements were suggested to support ease of viewership. For example, a few perceived the journey stops as “running together.” In response, we lengthened transitions and added audio indicators to cue the beginning of each “journey stop.” After these edits, the final video was 18 minutes long, which is 3 minutes more than the target duration. Despite the length, patients found the content neither burdensome nor boring, and described the video as empowering because of its comprehensive and realistic nature. In general, stakeholders found that the animation effectively imparted complex information, and that the two narrators, background music, and sound effects held their attention. One patient on HD commented, “It was visually interesting, and I wasn’t watching the clock thinking that it was taking forever,” and a patient with advanced CKD said, “…The video gave me lots of information that I can just sit with and ask questions later.”
In particular, the patient narrator’s story resonated across stakeholder types. A patient on HD commented, “[She] will reduce anxiety and make things clearer. You always can identify with someone who has been through what you’re going to go through.” This idea was evidenced when an individual who was just beginning their vascular access journey said, “I felt less tense and less worried because of her…” All patient and provider participants indicated they would recommend the video to their peers and patients, respectively.
Understanding and Acceptability of Postproduction Materials
The final education package (go.unc.edu/dialysisaccess; Supplemental Material) was evaluated by 25 patients, three care partners, and nine medical providers. Participants were from diverse geographic regions, and 13 (77%) of the patients had advanced CKD—the video target audience. Participants felt the aesthetics and content paralleled one another, effectively reinforcing important concepts (e.g., vascular access journey, terms), while providing helpful, medium-specific individualizations (e.g., space to write-in medical appointments, animated technical procedures). Patients called attention to the accessibility of mixed media, noting “…it’s great because you can watch the video and then take the brochure home and really think about it…,” and “…it gives you a chance to keep thinking about it [and] share it with family.” Similarly, a provider commented, “The repeated visuals help [the information] stick with you. Even if a patient is overwhelmed and teary eyed and mad, [they] can remember these pictures so [they] know how to ask questions.” All 37 (100%) interviewees endorsed use of the materials in practice, exceeding the 90% acceptability threshold.
Discussion
This article describes the stakeholder-guided process of developing a patient-centered vascular access education video and complementary brochure. The resultant materials use subway imagery to depict the “journey” of navigating vascular access care, include patient testimonials to acknowledge common emotions and concerns, and summarize key health information. Preliminary findings suggest the materials are acceptable to patients and providers, and have the potential to improve understanding of vascular access and associated care. This work highlights the importance of creating mixed media health education tools that are infused with patient experiences to enhance relatability and appeal.
A systematic review of qualitative studies found that patients often experience emotional vulnerability, unpreparedness, and loss of control during vascular access planning (27). Our focus group findings supported these data, with stakeholders reiterating the need for education that directly acknowledges patient anxiety, fear, and uncertainty. To do so, we incorporated a patient narrator who is currently receiving maintenance HD. In the video, she tells her own vascular access story, describing her reluctance to start the journey, fears of needles and pain, and medical complications. The patient’s story resonated with viewers, who described “Caroline” as the distinguishing video element, grounding the health information in an authentic voice. Patients found Caroline’s story comforting because they identified with her emotions and challenges. Such reactions are consistent with peer mentorship literature that highlights the role of shared patient experiences in normalizing emotions, promoting credibility, enhancing trust, and providing hope (28,29). The patient narrator also reiterated critical information relayed by the professional narrator, aiming to increase viewer understanding and retention. Stakeholders felt this approach was particularly important given the information complexity and volume.
However, the aforementioned elements would likely fall short without accommodating different learning styles and literacy levels. Limited health literacy affects more than a quarter of individuals with CKD and is associated with poorer health outcomes (e.g., more rapid kidney function decline, higher mortality) (30–34). Factors related to limited health literacy—including reduced self-management capacity, challenges navigating care processes, and difficulty effectively communicating with providers—may, in part, mediate these observed associations (35). Data suggest that animation can help overcome some limited health literacy challenges by improving comprehension and recall (13–15). For example, audiences with limited health literacy may have difficulty developing mental representations of static information (36,37). Incorporating dynamic animation and audio narration in colorectal education materials was shown to eliminate recall differences between audiences with lower and higher health literacy (13). Moreover, an animated video on kidney allocation provides precedent for using this medium to improve understanding and decisional self-efficacy in CKD populations (38). Therefore, we coupled static (brochure) and dynamic (video) media to enhance viewer information processing, emphasize key points, and improve recallability of vascular access information.
Strengths of our project include: (1) use of a validated framework for the development of visually based interventions and two health behavior change models to guide content and development; (2) reliance on a five-step methodology for lowering material reading level; (3) incorporation of both professional and patient narration; (4) guidance by diverse stakeholders; and (5) input from 80 patients/care partners, including perspectives from 54 individuals with advanced CKD (i.e., the target audience). We acknowledge project limitations. First, we only included participants who spoke English. Although we have translated the materials into Spanish, these require cultural validation and possibly cultural adaptation. Second, the video length could deter viewing. To address this potential limitation, we generated time-stamped video chapters within the 18-minute video and eight individual “journey-stop” video clips to facilitate segmented viewing. Third, we reported solely on the material development process. Future studies should assess the materials’ effectiveness at increasing knowledge and decisional self-efficacy, and improving clinical outcomes. Finally, no education product is ever truly finished. Although we used formal member checking and acceptability testing to guide our decision to end material editing, we acknowledge that future revisions may be warranted.
In conclusion, we present a vascular access education package comprising an animated video and complementary brochure. Together, these materials present key information about vascular access, care steps, and common patient concerns. Although future research is needed to evaluate their effectiveness, our data highlight the materials’ potential to improve patient understanding and experiences as they navigate dialysis vascular access care.
Disclosures
E.H. Chang reports receiving research funding from Lantheus Medical Imaging, and serving on the medical advisory board for the North Carolina chapter of the National Kidney Foundation (NKF). J.E. Flythe reports serving on the editorial board of American Journal of Kidney Diseases (2017–), CJASN (2017–), Kidney Medicine (2019–), and Nephrology Dialysis Transplantation (as the HD theme editor; 2018–), and as an associate editor for Kidney360 (2019–); receiving honoraria from American Renal Associates, American Society of Nephrology, Baxter, Dialysis Clinic Incorporated, Fresenius Medical Care North America, NKF, Renal Ventures, and numerous universities; having consultancy agreements with AstraZeneca and NxStage Medical Advisory Board; serving on the Kidney Disease Improving Global Outcomes Executive Committee (2020–) and Kidney Health Initiative (KHI) Board of Directors (2019–), and as the KHI Patient Preferences Project Chairperson (2019–); and receiving research funding from National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH/National Heart, Lung, and Blood Institute, Patient-Centered Outcomes Research Institute, Renal Research Institute (subsidiary of Fresenius Medical Care North America), and Robert Wood Johnson Foundation. A. Hegde reports serving on the research committee for the American Society of Diagnostic and Interventional Nephrology, and having consultancy agreements with Truepill. C. Wilkie reports having consultancy agreements with KHI, the UNC at Chapel Hill, University of Pennsylvania’s HOPE Consortium, and University of Pittsburgh; and having other interests in/relationships with NKF. All remaining authors have nothing to disclose.
Funding
This work was supported by NIDDK grant R21DK116115, and Renal Research Institute (RRI; a subsidiary of Fresenius Kidney Care North America) unrestricted, investigator-initiated research grant 20-0149. J.E. Flythe is supported by NIDDK grant K23DK109401.
Acknowledgments
The authors express gratitude to our Geisinger collaborators, Dr. Jamie Green and Ms. Christina Yule, for their work developing and implementing the QI project from which these education materials stemmed. The authors also thank Drs. Surya Manivannan and Shannon Murphy for their assistance with qualitative analyses of the preliminary focus groups and interviews, Ms. Linda York for her support with participant recruitment, and the numerous stakeholders who shared their experiences and feedback. Finally, we thank the patients who permitted inclusion of photographs of their dialysis accesses and ultrasound images.
The results presented in this article have not been published previously in whole or part, except in abstract form.
RRI played no role in study design; collection, analysis, and interpretation of data; writing the report; or in the decision to submit the report for publication.
Author Contributions
All authors were responsible for visualization; A. Dorough and J.E. Flythe wrote the original draft; A. Dorough, J.E. Flythe, and J.H. Narendra were responsible for formal analysis; A. Dorough, J.E. Flythe, and T. Oliver conceptualized the study; A. Dorough and J.H. Narendra were responsible for data curation and project administration; J.E. Flythe was responsible for funding acquisition and provided supervision; J.E. Flythe and T. Oliver were responsible for methodology and resources; T. Oliver was responsible for software; and all authors were responsible for investigation, and reviewed and edited the manuscript.
Supplemental Material
This article contains the following supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0002382021/-/DCSupplemental.
Representative interview guide questions. Download Supplemental Table 1, PDF file, 344 KB (343.8KB, pdf)
Stakeholder quotations. Download Supplemental Table 2, PDF file, 344 KB (343.8KB, pdf)
Stakeholder-informed vascular access educational brochure development. Download Supplemental Table 3, PDF file, 344 KB (343.8KB, pdf)
Education Package. Download Supplemental Material, PDF file, 344 KB (343.8KB, pdf)
References
- 1.Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, Pannu NI, Thomas C, Hemmelgarn BR, Craig JC, Manns B, Tonelli M, Strippoli GF, James MT: Associations between hemodialysis access type and clinical outcomes: A systematic review. J Am Soc Nephrol 24: 465–473, 2013. 10.1681/ASN.2012070643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Kidney Foundation : KDOQI clinical practice guideline for vascular access, 2019. Available at: https://www.kidney.org/professionals/guidelines/guidelines_commentaries/vascular-access. Accessed June 30, 2021 [DOI] [PubMed]
- 3.Ravani P, Gillespie BW, Quinn RR, MacRae J, Manns B, Mendelssohn D, Tonelli M, Hemmelgarn B, James M, Pannu N, Robinson BM, Zhang X, Pisoni R: Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol 24: 1668–1677, 2013. 10.1681/ASN.2012121234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Renal Data System 2018 annual data report: Epidemiology of kidney disease in the United States. Available at: https://www.usrds.org/annual-data-report. Accessed June 30, 2021 [DOI] [PMC free article] [PubMed]
- 5.Lopez-Vargas PA, Craig JC, Gallagher MP, Walker RG, Snelling PL, Pedagogos E, Gray NA, Divi MD, Gillies AH, Suranyi MG, Thein H, McDonald SP, Russell C, Polkinghorne KR: Barriers to timely arteriovenous fistula creation: A study of providers and patients. Am J Kidney Dis 57: 873–882, 2011. 10.1053/j.ajkd.2010.12.020 [DOI] [PubMed] [Google Scholar]
- 6.Woo K, Lok CE: New insights into dialysis vascular access: What is the optimal vascular access type and timing of access creation in CKD and dialysis patients? Clin J Am Soc Nephrol 11: 1487–1494, 2016. 10.2215/CJN.02190216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiaii M, MacRae JM: A dedicated vascular access program can improve arteriovenous fistula rates without increasing catheters. J Vasc Access 9: 254–259, 2008. 10.1177/112972980800900406 [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Vargas PA, Tong A, Howell M, Craig JC: Educational interventions for patients with CKD: A systematic review. Am J Kidney Dis 68: 353–370, 2016. 10.1053/j.ajkd.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 9.American Association of Kidney Patients: Understanding your hemodialysis access options. Available at: https://aakp.org/wp-content/uploads/2019/09/Hemo-Access-Options-Final.pdf. Accessed February 24, 2021
- 10.National Kidney Foundation: Hemodialysis access: What you need to know. Available at: https://www.kidney.org/sites/default/files/11-50-0216_va.pdf2006. Accessed February 24, 2021
- 11.Medical Education Institute: Vascular access: A lifeline for dialysis: Kidney school module 8. Available at: https://course.wcea.education/app/mei/elearning/nurse/medical-education-institute/192779/vascular-access-a-lifeline-for-dialysis-kidney-school-module-8. Accessed February 24, 2021
- 12.PeaceHealth: Vascular access failure. Available at: https://www.peacehealth.org/medical-topics/id/abo39242020. Accessed February 24, 2021
- 13.Meppelink CS, van Weert JC, Haven CJ, Smit EG: The effectiveness of health animations in audiences with different health literacy levels: an experimental study. J Med Internet Res 17: e11, 2015. 10.2196/jmir.3979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George S, Moran E, Duran N, Jenders RA: Using animation as an information tool to advance health research literacy among minority participants. AMIA Annu Symp Proc 2013: 475–484, 2013 [PMC free article] [PubMed] [Google Scholar]
- 15.Leiner M, Handal G, Williams D: Patient communication: A multidisciplinary approach using animated cartoons. Health Educ Res 19: 591–595, 2004. 10.1093/her/cyg079 [DOI] [PubMed] [Google Scholar]
- 16.Calderón JL, Shaheen M, Hays RD, Fleming ES, Norris KC, Baker RS: Improving diabetes health literacy by animation. Diabetes Educ 40: 361–372, 2014. 10.1177/0145721714527518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flythe JE, Narendra JH, Yule C, Manivannan S, Murphy S, Lee S-YD, Strigo TS, Peskoe S, Pendergast JF, Boulware LE, Green JA: Targeting patient and health system barriers to improve rates of hemodialysis initiation with an arteriovenous access. Kidney360 2: 708–720, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams B, Anderson AS, Barton K, McGhee J: Can theory be embedded in visual interventions to promote self-management? A proposed model and worked example. Int J Nurs Stud 49: 1598–1609, 2012. 10.1016/j.ijnurstu.2012.07.005 [DOI] [PubMed] [Google Scholar]
- 19.Leventhal H, Phillips LA, Burns E: The common-sense model of self-regulation (CSM): A dynamic framework for understanding illness self-management. J Behav Med 39: 935–946, 2016. 10.1007/s10865-016-9782-2 [DOI] [PubMed] [Google Scholar]
- 20.Hagger MS, Koch S, Chatzisarantis NLD, Orbell S: The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol Bull 143: 1117–1154, 2017. 10.1037/bul0000118 [DOI] [PubMed] [Google Scholar]
- 21.Karekla M, Karademas EC, Gloster AT: The common sense model of self-regulation and acceptance and commitment therapy: Integrating strategies to guide interventions for chronic illness. Health Psychol Rev 13: 490–503, 2019. 10.1080/17437199.2018.1437550 [DOI] [PubMed] [Google Scholar]
- 22.Hill-Briggs F, Schumann KP, Dike O: Five-step methodology for evaluation and adaptation of print patient health information to meet the < 5th grade readability criterion. Med Care 50: 294–301, 2012. 10.1097/MLR.0b013e318249d6c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsieh HF, Shannon SE: Three approaches to qualitative content analysis. Qual Health Res 15: 1277–1288, 2005. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 24.Moser A, Korstjens I: Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur J Gen Pract 24: 9–18, 2018. 10.1080/13814788.2017.1375091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elo S, Kyngäs H: The qualitative content analysis process. J Adv Nurs 62: 107–115, 2008. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 26.Birt L, Scott S, Cavers D, Campbell C, Walter F: Member checking: A tool to enhance trustworthiness or merely a nod to validation? Qual Health Res 26: 1802–1811, 2016. 10.1177/1049732316654870 [DOI] [PubMed] [Google Scholar]
- 27.Casey JR, Hanson CS, Winkelmayer WC, Craig JC, Palmer S, Strippoli GF, Tong A: Patients’ perspectives on hemodialysis vascular access: A systematic review of qualitative studies. Am J Kidney Dis 64: 937–953, 2014. 10.1053/j.ajkd.2014.06.024 [DOI] [PubMed] [Google Scholar]
- 28.Hughes J, Wood E, Smith G: Exploring kidney patients’ experiences of receiving individual peer support. Health Expect 12: 396–406, 2009. 10.1111/j.1369-7625.2009.00568.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bennett PN, St Clair Russell J, Atwal J, Brown L, Schiller B: Patient-to-patient peer mentor support in dialysis: Improving the patient experience. Semin Dial 31: 455–461, 2018. 10.1111/sdi.12703 [DOI] [PubMed] [Google Scholar]
- 30.Taylor DM, Fraser SDS, Bradley JA, Bradley C, Draper H, Metcalfe W, Oniscu GC, Tomson CRV, Ravanan R, Roderick PJ; ATTOM investigators: A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol 12: 1070–1084, 2017. 10.2215/CJN.12921216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor DM, Fraser S, Dudley C, Oniscu GC, Tomson C, Ravanan R, Roderick P; ATTOM investigators: Health literacy and patient outcomes in chronic kidney disease: A systematic review. Nephrol Dial Transplant 33: 1545–1558, 2018 [DOI] [PubMed] [Google Scholar]
- 32.Devraj R, Borrego M, Vilay AM, Gordon EJ, Pailden J, Horowitz B: Relationship between health literacy and kidney function. Nephrology (Carlton) 20: 360–367, 2015. 10.1111/nep.12425 [DOI] [PubMed] [Google Scholar]
- 33.Ricardo AC, Yang W, Lora CM, Gordon EJ, Diamantidis CJ, Ford V, Kusek JW, Lopez A, Lustigova E, Nessel L, Rosas SE, Steigerwalt S, Theurer J, Zhang X, Fischer MJ, Lash JP; CRIC Investigators: Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clin Nephrol 81: 30–37, 2014. 10.5414/CN108062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, Huizinga MM, Elasy TA, Rothman RL, Ikizler TA: Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 21: 1979–1985, 2010. 10.1681/ASN.2009111163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boonstra MD, Reijneveld SA, Foitzik EM, Westerhuis R, Navis G, de Winter AF: How to tackle health literacy problems in chronic kidney disease patients? A systematic review to identify promising intervention targets and strategies [published online ahead of print December 22, 2020]. Nephrol Dial Transplant 10.1093/ndt/gfaa273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Höffler TN, Leutner D: Instructional animation versus static pictures: A meta-analysis. Learn Instr 17: 722–738, 2007. 10.1016/j.learninstruc.2007.09.013 [DOI] [Google Scholar]
- 37.Mayer R, Moreno R: Animation as an aid to multimedia learning. Educ Psychol Rev 14: 87–99, 2002 [Google Scholar]
- 38.Kayler LK, Keller MM, Crenesse-Cozien N, Dolph B, Cadzow R, Feeley TH: Development and preliminary evaluation of ilearnKAS: An animated video about kidney allocation to support transplant decision-making. Clin Transplant 33: e13638, 2019. 10.1111/ctr.13638 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Representative interview guide questions. Download Supplemental Table 1, PDF file, 344 KB (343.8KB, pdf)
Stakeholder quotations. Download Supplemental Table 2, PDF file, 344 KB (343.8KB, pdf)
Stakeholder-informed vascular access educational brochure development. Download Supplemental Table 3, PDF file, 344 KB (343.8KB, pdf)
Education Package. Download Supplemental Material, PDF file, 344 KB (343.8KB, pdf)