Abstract
Background:
Mental health stigma is a major barrier to seeking help, and leads to poor quality of life and social withdrawal for individuals living with mental illness. These concerns are especially severe in low-income and middle-income countries (LMICs) that face a disproportionate share of the global burden of mental illnesses. With growing access to digital technologies in LMICs, there may be new opportunities to address mental health stigma. This review considers the potential for emerging digital technologies to advance efforts to challenge mental health stigma in LMICs.
Methods:
Promising digital strategies to reduce mental health stigma were identified through searching the peer-reviewed literature. Drawing from the Mental Illness Stigma Framework, these studies of digital strategies were grouped into three categories: 1) protest; 2) education, and 3) contact.
Results:
These three categories align with established stigma reduction programs. Digital strategies could expand the reach of or complement existing efforts. There are challenges with digital stigma reduction strategies, including the need for cultural adaptation of these programs to diverse contexts and settings, consideration of reliable measurement of mental health related stigma, and risks that digital media could perpetuate the spread of misinformation and exacerbate concerns pertaining to mental health stigma.
Conclusion:
This review highlights the promise of technology for addressing mental health stigma in LMICs. This is imperative in the face of growing demand for mental health services owing to the economic and social impacts of the COVID-19 pandemic, and the increasing reliance on digital platforms among individuals in most countries.
Keywords: Digital technology, Low-income and middle-income countries, Mental illness, Stigma
BACKGROUND
Mental illnesses are a leading cause of disability worldwide, and efforts to support prevention, early intervention, and recovery represent a critical public health priority [1]. Alarmingly, few individuals living with mental illness have access to basic mental health services. It is estimated that roughly 80% of people who live with a mental illness worldwide reside in low-income and middle-income countries (LMICs) [2], where over 90% of these individuals do not have access to evidence-based care [1]. This dramatic disparity between those who receive mental health care and those who require care but do not receive it is referred to as the mental health care gap [3], and is one of the contributing factors to dramatically shortened life expectancy observed among persons living with mental illness when compared to the general population [4]. This early mortality disparity is further compounded by a range of intersecting social and economic factors, including poverty, high rates of unemployment, increased risk of homelessness, and importantly, the impact of stigma and discrimination [4]. Stigma refers to the negative public opinions and discrimination against certain groups of people due to their distinct characteristics [5, 6]. For those facing the challenges of mental illness, the consequences of stigma and discrimination are profound, resulting in low self-confidence and social isolation. Stigma also represents a significant barrier to advancing prevention and treatment initiatives, and exacerbates the already significant gap in available mental health services because many individuals are reluctant to seek help due to fears of victimization or shame, concerns that are particularly pronounced in low-resource settings [7]. Therefore, there is urgent need and an ethical imperative to develop and implement innovative approaches to overcome the challenges of mental health stigma.
There has been increasing research showing that digital technologies, ranging from smartphones, social media, and mobile apps represent a collection of promising approaches for augmenting mental health services and improving quality and access to care [8]. Given the widespread reach of mobile devices and popularity of social media, online platforms, and apps, these technologies form an integral part of the daily lives of most individuals [9]. Additionally, digital technologies could play an especially important role for individuals living with mental illness who may be reluctant to seek care due to stigma, as they could potentially access digital mental health programs through their personal mobile devices and do so discreetly and at their own leisure [10]. The coronavirus (COVID-19) pandemic has further highlighted the promise of digital technologies for mental health, as digital devices have emerged as being especially critical for enabling access to mental health services, particularly in settings where in-person contact is restricted and for individuals facing strict quarantine and lockdowns [11], including in LMICs [12, 13].
In this paper, we consider the role that technology can play as a potential strategy for challenging and overcoming mental health-related stigma, with emphasis on the application of technology in LMICs. Specifically, we illustrate the potential for emerging digital technologies to advance mental health outreach and advocacy campaigns, to challenge stigmatizing attitudes and misinformation about mental illness, and to promote recovery through peer connection and social support. We apply the Mental Health Stigma Framework [5] to conceptualize how these different examples could address mental health related stigma, with consideration of promising examples in LMICs, where there has been recent rapid expansion of digital mental health efforts [14-16]. The examples described in this paper are not exhaustive; rather, our goal is to contribute to growing recognition of the opportunities surrounding the use of technology, while considering the potential risks, towards promoting the dignity and autonomy of persons living with mental illness globally.
STIGMA AND MENTAL HEALTH: A GLOBAL CHALLENGE
The varying components of stigma are conceptualized as part of the Mental Illness Stigma Framework (MISF), which emphasizes cognitive, affective, and behavioural aspects of stigma [5, 17]. These three components correspond to stereotype, prejudice, and discrimination, respectively, and can collectively shape the impact of stigma on those living with mental illnesses. In general, such impact is understood in terms of three aspects: experienced stigma [18], which refers to external stereotypes, prejudice and discrimination; anticipated stigma [19], which refers to the expectation of being the subject of experienced stigma; and self-stigma [20], which refers to the endorsement and internalization of the stigmatizing ideas by the stigmatized. Mental health-related stigma contributes to increased symptom severity among individuals living with mental illness, as well as decreased treatment seeking and increased treatment non-adherence [21]. Additional repercussions include greater public avoidance, susceptibility to coercive treatment, and a history of segregated clinical practices, use of restraints, and institutionalization of patients with mental health problems [17, 22, 23]. Internalized stigma can also lead to lower self-esteem or increased anger and resentment among those who are stigmatized in response to the prejudice they experience [17].
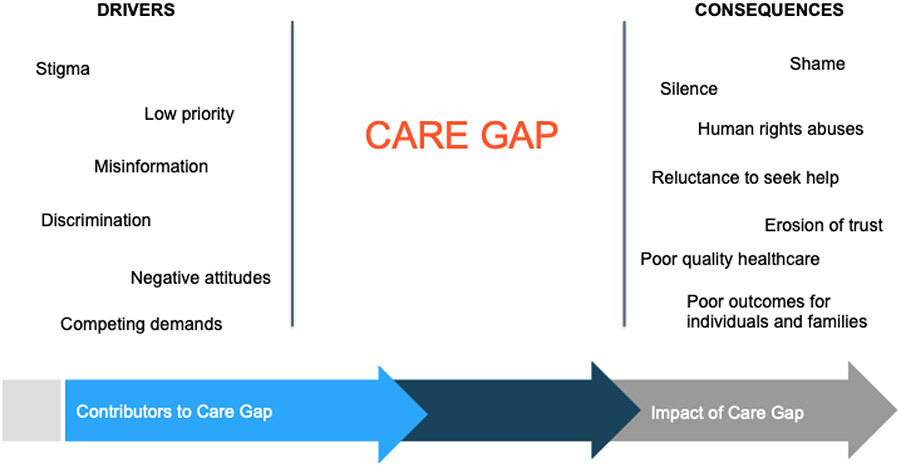
Research on mental health stigma has also shifted from individual-level interactions to greater recognition of societal-level factors, referred to as structural stigma, encompassing the culture and policies that may limit and marginalize the opportunities and well-being of the stigmatized individual [24-26]. Structural stigma synergistically amplifies other types of stigma and deepens the health inequalities and adverse health consequences for the stigmatized individuals, ranging from dysregulated physiological stress responses to premature mortality [27]. The consequences of stigma among individuals living with mental illness have even been described as being worse than the mental health conditions themselves [28], and represent a major driver of the mental health care gap, as depicted in Figure 1. Stigma contributes to worsening of disabilities through loss of social and economic opportunities, disadvantages across multiple personal and professional life domains, and direct threats of discrimination and negative attitudes [7].
Figure 1.
Mental health stigma is one of the key underlying drivers of the global mental health care gap with resulting consequences for individuals
In LMICs, mental health stigma can manifest itself differently between cultures and contexts. For example, in Eastern countries, moral attributions in the form of social exclusion, or perception of dangerousness are more common, but in Western countries, prejudice and discrimination against mental illnesses in racial and ethnic minority groups are more common [29]. Furthermore, the ways in which individuals may feel comfortable seeking support can differ between cultures, where in some instances traditional healers, spiritual practitioners, and others from faith-based communities can be the preferred resource during a crisis [30]. Despite these differences, the resulting detrimental impact for the individual is often consistent [31]. Moreover, in many LMICs where there may be fewer protections implemented for persons with disabilities, many people with mental illnesses are the subject of abuses, extreme poverty and social exclusion, making mental health stigma not only a public health issue but also a human rights issue [7]. There is also often limited priority for stigma reduction methods in LMICs, and these efforts are typically under-funded and under-studied [31]. It is often unclear how applicable and generalizable the stigma reduction study results from high-income countries are to populations in LMICs [32]. Despite these concerns, there have been an increasing number of effective stigma reduction interventions tested in LMICs, with several focusing on recovery and strengths among persons living with mental illness [33]. However, these existing programs are limited by the inadequate involvement of communities and locals in the intervention design and evaluation, as well as concentration in only a few LMICs, which limits generalizability across diverse settings [33]. Given that the wide-ranging detrimental effects of stigma are a global challenge, it is critical to conceptualize, develop and evaluate novel stigma reduction interventions that can be widely implemented and scaled up, and that may be particularly suitable for under-resourced settings where there have been fewer prior efforts to address mental health stigma such as in LMICs.
DIGITAL TECHNOLOGY AND OPPORTUNITIES FOR COMBATING STIGMA
Emerging digital technologies, including the recent rapid rise of social media use and mobile apps has quickly taken on an important role in the lives of individuals across the globe, many of whom suffer from mental health challenges [14]. It is estimated from studies in high income countries that people living with mental illnesses are equally likely to engage in social media platforms as the general population [34], even though in the offline world individuals living with mental illness are often less likely to have adequate social support networks [35]. Digital platforms combine features of anonymity and use of asynchronous communication, which does not require immediate response or interpretation of non-verbal cues, and could potentially overcome fears of in-person social interaction or communication deficits consistent with many illnesses [35-37]. As a result, digital mental health may have important implications as a prominent way of facilitating social interactions and support networks necessary for raising mental health awareness [35].
Digital platforms could also protect patient’s anonymity and allow communication without the fear of being identified; therefore, the features of digital platforms could be of particular relevance to the treatment for severe mental illnesses, which are often among the most stigmatizing illnesses [34, 38]. Studies have suggested that social media could be a valuable avenue for patients with schizophrenia to seek help for mental health concerns, connect with others, feel less alone, and engage with community supports [39]. Digital platforms also allow opportunities for self-disclosing personal narratives, and sharing painful thoughts or feelings that may otherwise be difficult to convey in real life [40]. Naturally occurring peer-to-peer support on online platforms could minimize the sense of isolation and provide hope and strategies necessary for coping [41]. These peer exchanges are often found to be positive and can potentially serve as a strong force to oppose stigmatizing and hostile comments. Furthermore, these online peer exchanges could help promote treatment engagement, reach a wider audience and serve as a link between community-level and primary-care level support [35, 41].
Development of digital programs has allowed changes in mental health literacy, stigma and increasing willingness to seek help, particularly in younger generations. For example, in Australia, a randomized controlled trial of three brief fully automated internet-based mental health help-seeking interventions for young athletes showed a reduction in depression and anxiety stigma at 3-month follow-up [42]. However, in contrast, not all digital platforms have shown equally impressive results. Studies on the Reach Out Central online game among people ages 16-25 found that although mental health literacy and help-seeking attitudes improved, there did not appear to be any changes in mental health stigma [43, 44]. Additionally, entertainment-education has been used to reduce stigma and model appropriate help-seeking behaviours in both high-income and low-income countries [6]. This approach incorporates educational messaging into popular entertainment such as fotonovela, soap opera and sitcoms to inform the public about mental health issues in an interesting and engaging way [45]. Use of technologies for stigma reduction has grown markedly over recent years, a trend that is expected to continue as the availability and use of digital technologies continues to expand to most regions of the globe, and as digital avenues appear to hold promise for delivering anti-stigma information [6].
With many important opportunities for leveraging popular and increasingly widely available digital technologies for combating stigma, and mounting evidence highlighting the reach and impact of these technologies for mental health in LMICs [10, 14, 46, 47], this is an area that is ripe for innovation. In particular, there may be opportunities to draw from existing successful stigma reduction efforts [7], and to adapt these effective programs for digital platforms in order to expand the reach and impact of these programs in LMICs. Furthermore, this is an especially timely research focus given the increasing reliance on digital technologies during the COVID-19 pandemic [11], and the extensive reach across most regions of the globe and in particular in LMICs [13].
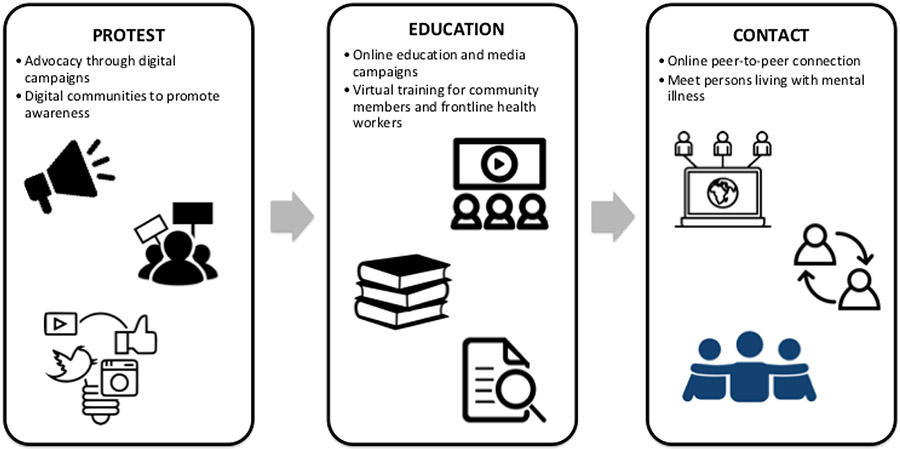
For this review, we grouped promising strategies to reduce mental health related stigma that hold potential for widespread reach in LMICs using emerging digital technologies into three broad categories: 1) protest; 2) education, and 3) contact [48]. These categories were selected as they form part of the Mental Illness Stigma Framework (MISF) [5], and because they align with established stigma reduction strategies from the literature [48]. Digital technologies may offer important opportunities for expanding the reach of these three types of approaches. We consider how these approaches could support global stigma reduction efforts, and draw from a combination of promising examples from the published peer-reviewed literature in LMICs as well as from high-income settings. The different strategies are illustrated in Figure 2 and described in detail in the sections that follow.
Figure 2.
Conceptualizing different approaches for digital technology to advance stigma prevention efforts through protest, education, and contact
1). Protest
Protest focuses on addressing inaccurate misinformation or representation of mental illness, both by combatting negative media portrayals of mental illness and the spread of stigmatizing images, and through tackling public belief in negative viewpoints. Among the three strategies identified above, protest typically receives inadequate attention as a viable approach for challenging mental health stigma [49]. As part of the HIV/AIDS movement, efforts such as the AIDS Coalition to Unleash Power (ACT UP), are often cited as important models for understanding the immensely important destigmatizing impact of protest [50]. Inspired by HIV/AIDS activism, the Movement for Global Mental Health was established in 2008 to provide platforms for members from around the world to promote shared visions of closing the mental health treatment gap in LMICs [51]. This movement organized a large digital community, many of whom identified as living with mental illnesses, where they are able to participate in and support each other’s initiatives and activities with the common goal of improving availability, accessibility and quality of services for people struggling with mental illnesses. Other than structured virtual programs, the increasing visible presence of blogging and microblogging has also been extensively used for advocacy and encouragement of “joining the conversation” from the public [52]. StigmaBusters is a group from the National Alliance on Mental Illness (NAMI) that aims to report and speak out against stigmatizing media representation of mental illnesses and has successfully deterred several disrespectful media stories from being published and disseminated on screens and has praised media that endorse anti-stigma images [53]. Even though StigmaBusters is based in the United States, this approach is especially relevant for tackling mental health related-stigma in LMICs, where several studies have highlighted the detrimental effects of exaggerated and sensational media portrayals of mental illness and suicide [54-56].
Protest is also occasionally defined in the literature more narrowly as directly suppressing negative representations or attitudes by objecting to inappropriate media outlets that portray a negative stereotype of mental illness [57]. Examples include public rallies and boycotting certain businesses if they refuse to rectify stigmatizing comments, products, or images [58]. Under this framework, it often becomes controversial whether it is truly effective or potentially harmful. Some important changes were observed among opinion leaders such as politicians, journalists or other leading media outlets; however, evidence in changing the perceptions within the general public is lacking and remains understudied. There has been concern over the polarizing effects of direct suppression with the unanticipated consequence of further deepening isolating and divisive sentiments [57]. Given the very different features of protest, it is important to distinguish different ways of protest in the context of reducing mental health stigma and to remain mindful of the psychological reactions that might be elicited from the public when initiating a protest or advocacy program.
2). Education
Education aims to provide truthful information to the public to make more informed decisions and judgements about mental illness. It has been shown that groups with better understanding of mental illnesses are less likely to endorse discriminatory views, and that education that focuses on provision of accurate information is able to improve positive attitudes about patients with mental illness. Digital technologies also have the potential to be a powerful tool for extending the reach and impact of anti-stigma campaigns on a population level in both high and low-income countries. In one example from Bangladesh, a popular and successful televised animation program called Meena Communication Initiative (MCI) was implemented as an educational initiative to build knowledge capacity for girls in rural and underserved areas [59]. A short episode of Meena and interactive play were developed to raise awareness and reduce stigma for autism and was disseminated across 158 subdistricts across the country where plays were aired. Even though the effectiveness of this effort of mass media intervention was not rigorously evaluated, and the effort was not replicated for other types of mental illnesses, it nonetheless offers valuable insights regarding the role that media platforms could serve as a potential avenue to address stigma in mental health by changing mental health-related behaviours such as help seeking and improving public understanding [59]. Despite its positive influences, these mass media campaigns can often be expensive if it involves purchasing media time. Therefore, a multitude of grassroot digital platforms, and use of social media, have also been developed to address the issues more locally.
The Systematic Medical Appraisal, Referral and Treatment (SMART) mental health project was developed to focus on mental health services delivery model to screen, diagnose and manage common mental illnesses in rural India [60]. It involves a stigma reduction campaign that aims to increase mental health knowledge across rural villages. The campaign consists of sharing brochures and posters on mental health, showing filmed videos of actors talking about mental illnesses and dramatization that features seeking help for mental illnesses. In subsequent outcome evaluation studies, a total of 1576 and 2100 participants were interviewed at pre- and post- campaign, respectively [60, 61]. It was reported that the campaign resulted in significantly lower level of stigma related to help-seeking behaviours, and a significant increase in positive attitudes towards mental health. A longitudinal study over the span of 24 months demonstrated that attitude and behaviour scores towards mental health maintained a statistically significant increase compared to pre-campaign, further substantiating the beneficial and long-lasting effects of the anti-stigma campaign [61].
In another example from India, Atmiyata is a rural community-led intervention program that uses digital platforms such as smartphone technology and films to promote well-being and reduce the burden of mental illness in rural villages. A proof-of-concept study demonstrated that 59 community volunteers called Atmiyata champions were able to help identify more than one thousand people with mental illnesses and were able to help raised awareness to more than seven thousand people [62]. One of the main benefits of Atmiyata is that it was designed to embed the intevention within existing community development programs in the region and thus create a more integrated program with less stigma than a separate standalone mental health program [62].
3). Contact
Lastly, contact encompasses opportunities for connecting with someone with mental illness, which appear to reduce stigmatizing attitudes as reflected in many prior studies in higher income countries, though many prior studies lack methodological rigor and may not generalize to all settings [63], such as LMICs. Contact-based interventions could also encompass opportunities for peer connection whereby persons with mental illness can connect with and support each other in overcoming challenges attributed to stigma. In contact-based anti-stigma interventions, persons living with mental illnesses can openly share with the public their struggle, challenges and success to overcome the interpersonal segregations that often foster fear and distrust. Social psychology research shows that contact-based behavioural interventions can both reduce external public stigma but also benefit internal self-stigma by means of empowerment and self-esteem [48]. This further emphasizes the potential benefit of leveraging technology to enable social contact.
One promising example is the It’s Ok To Talk campaign that was launched in 2017 in New Delhi, India as an initiative to facilitate public disclosure of mental health problems and reduction in self-stigma among young people [64]. The campaign showed that breaking stigma is one of the four central themes of the narratives that people share on the platform. Interestingly, although the platform emphasized the option of anonymity, most participants chose to include some personally identifying information, which reflects a strong desire to be heard and understood. Furthermore, the campaign emphasized the importance of self-acceptance on the journeys to recovery for many participants and it is consistent with previous research that has shown that online sharing can increase self-confidence and facilitate interpersonal connections [64]. In an example from China, research into the self-organized online community of people on a popular online forum for mental illnesses called Sunshine showed that the platform was able to facilitate information exchange regarding medication and coping skills, peer therapy, storytelling and peer emotional support [65]. These results suggest decreased stigma through important benefits such as enhanced self-efficacy and self-esteem and elevated sense of belonging [65].
DISCUSSION
By applying the Mental Illness Stigma Framework (MISF) [5, 17], we classified promising digital approaches for addressing stigma into the three broad categories of protest, education, and contact [48]. An important strength with conceptualizing digital approaches to stigma reduction in this way is that it can guide the design and implementation of new initiatives, while also informing outcome measurement and assessment of impact. Additionally, standardized, easily interpretable measurements for mental health stigma of all types, particularly those that address the confounding effects of social desirability bias in self-reports, would greatly strengthen the development and subsequent rigorous evaluation of digital stigma reduction programs.
Despite the promising approaches described in this review, there remains a large need for future stigma research, especially in LMICs. More research should focus on examining the impact of protest as a means to challenge stigma. For instance, this topic is largely understudied topic, and it is necessary to better understand the differences in outcomes from past protest efforts, and the particular relevance of these approaches for LMICs where there may be different regulations guiding the open sharing of information or opinions regardless of the topic. With regards to education, new campaigns that involve the use of digital technology appear particularly important for decreasing mental health-related stigma and promoting help seeking behaviours in LMICs where its scalability and economic sustainability are especially valuable. Careful attention will be needed to ensure equitable distribution of education efforts, specifically within marginalized and underserved communities where the harmful effects mental health stigma may go largely unaddressed. Further, while social contact is a powerful tool for addressing mental health related stigma as reflected in the studies summarized here, as well as preliminary research suggesting the benefits of digital programs for promoting social contact, there have been few studies of comparable efforts in the context of LMICs [33]. Specifically, more initiatives with rigorous evaluative methods are needed in LMICs to demonstrate a lasting effect of digitally enabled contact-based interventions for addressing mental health related stigma.
THREATS AND CHALLENGES
Digital platforms have become an important vector for public messaging and spread of information and could yield opportunities to advance efforts to address mental health stigma in LMICs; however, consideration of the challenges posed by these emerging technologies is also warranted. For instance, the internet and the media have great potential in reducing stigmatization of mental illnesses, they can also be used to perpetuate the spread of misinformation, fake news, harmful stereotypes and deep-rooted discriminations regarding mental illnesses that could severely threaten the quality of life of these populations [66]. Television news, entertainment programs, films and newspapers have all played a central role in crystalizing the biased images of persons facing the challenges of mental illnesses. Notably, the media often portray individuals with mental illness as dangerous, reckless, prone to committing crimes and burdensome to the functions of society, and often in the context of mediagenic and sensational news [67]. The overgeneralized framing of mental illnesses as an individual character flaw rather than in the context of societal causes and environmental factors contributes to the perpetuation of inaccurate public understanding of mental health and mental illness. For example, simplifying and trivializing the symptoms of a mental illness, such as obsessive compulsive disorder being viewed as quirky behaviours, or attributing blame on the individual for their condition, such as in the case of addiction and substance use disorders.
There are also inherent risks with using digital technology that warrant consideration, such as the detrimental effects of prolonged screen exposure, social isolation due to reduction in in-person contact, exposure to harmful or discriminatory content online, and risks to privacy [34]. In many LMICs, there lack adequate data protection laws, which could have the unintended consequence of an individual’s mental health-related data being exploited, and potentially resulting in greater harm and stigmatization [10]. Careful attention to these concerns will be essential, to ensure that the benefits outweigh potential risks with leveraging novel technologies for combating stigma.
Research in many LMICs has focused on the public health threats of inadequate media reporting of suicides. For instance, studies have highlighted that most reporting fails to follow key WHO recommendations for suicide reporting by portraying inaccurate information, describing the methods used for suicide, and presenting sensational headlines as reflected in countries such as India [55, 56], Nigeria [68], or Indonesia [69]. This type of dramatic media reporting perpetuates negative sentiments and stigmatizing attitudes about suicide, and can risk triggering suicidal behaviours rather than educating the public or offering opportunities for individuals to seek help and address the underlying mental health problems associated with suicide risk [70]. This is alarming as suicide represents a significant cause of death globally, with suicide rates increasing in some countries and particularly in many LMICs [71].
Collective stigmatizing assumptions have powerfully reinforced public stigma that often draws immediate associations to mental illnesses whenever a negative or violent event is caused by a human or technical failure [72]. In a study analyzing printed media images of psychological disorders in European countries, it was found that more than half of all articles contained negative sentiments towards persons with mental illnesses, with severe mental illnesses such as psychosis being the most stigmatized [73]. It was also found that most of the highly stigmatizing articles do not have professional sources of information and the voices of the patients along with mental health professionals are generally not sought after [74]. In contrast, the role of media in generating self-stigma is less clearly defined; yet, a recent study found that stereotype agreement, one of the 4 subscales of self-stigma, significantly increased after the participants watched a highly stigmatizing video about depression, pointing to the possibility that mass media can also contributed to internalized stigma [66]. Media coverage, as an important influencer of public opinions, therefore, need to utilize its power to deliver healthy understanding of mental health conditions instead of spreading misinformation that risks propagating the marginalization of people living with mental illnesses.
Another important yet challenging consideration for technology-enabled stigma interventions is the understanding of mental health and its stigma in specific contexts of cultural variations. There are several studies that have documented the cultural differences in the expression of mental illnesses and mental health problems, as well as the understanding of the causes of these concerns, and the decision to seek help [75]. Other studies have found that attitudes towards mental illness can also vary among ethnicities, cultures and countries, particularly according to the influence of different religious or spiritual beliefs [76, 77]. These different attributions of mental illnesses between different cultures can also result in differences in stigma and prejudice towards individuals living with mental illness [29]. In low-resource settings that lack adequate mental health services, family members often represent the only form of support that individuals facing mental health problems have [78]. In these circumstances, the impact of stigma can be especially severe, as it can manifest in the form of neglect of the patient, or fear of abandonment of the patient by families and communities, which is a persistent threat to help seeking [78, 79]. It is also important to note that formal mental health providers, such as psychiatrists, may not be ideally positioned to address mental health stigma in some LMICs. Recognition of this challenge is especially important in settings where psychiatric care retains a colonial legacy and is historically associated with oppression of marginalized groups [80], as well as in settings where there is widespread mistrust of the formal health care system [81-83]. This further emphasizes the importance of cultural adaptation of digitally-enabled stigma reduction campaigns across different LMICs, where program implementers need to carefully study the ethnocultural beliefs prior to selecting the most appropriate methods for combating stigma [84]. Such efforts should also be guided by relevant frameworks and rigorous methods to ensure acceptability, reach, and sustained engagement within the target setting [85].
Another important challenge in determining the impact of digital approaches to stigma reduction will be the reliable measurement of mental health related stigma. The measurement of stigma continues to be a controversial topic in academic research, with more than 400 different measures used in literature since 2004 [5]. Strikingly over 66% of these measures have not undergone any systematic psychometric validation and are often developed solely for the particular study in which it appeared [5]. Challenges with establishing standardized stigma measures likely stem from the lack of an unified conceptual framework that defines mental illness stigma, as well as the multitude of varying factors that contribute to stigma as well as differing representation of mental health stigma across cultures and contexts [29]. With emerging digital technologies poised to play an increasingly important role in addressing stigma, future work should consider how user data captured from these platforms could yield insights about the perceptions of stigma. These novel data streams could supplement existing measures of stigma to determine the benefits of new stigma reduction initiatives.
FUTURE DIRECTIONS AND GLOBAL IMPACT
Stigma has detrimental effects on those facing the challenges of mental illness, and represents a serious challenge for advancing the treatment and prevention of mental illnesses. These concerns are especially severe in LMICs that face a disproportionate share of the global burden of mental illness, and where systematic efforts to address stigma are a nascent area of research [32]. For one thing, while social stigma appears to hurt many people living with mental illness, it also appears to energize some to react to injustice. It has been proposed that the perception of the stigma as well as the person’s identification within the stigmatized community can moderate these differences in response [86], and research is necessary to illustrate a situational model that can help people cope with self-stigma in the clinic. Another important yet understudied area of research is structural stigma [21], encompassing societal-level factors, cultural norms, and institutional policies that have detrimental effects on those living with mental illness and their life opportunities and ability to seek care [87]. Future research needs to bridge the gap and study the interactions between structural, social, and self-stigma and explain how structural stigma can moderate (and often worsen) the detrimental psychosocial outcomes of stigma. Importantly, exploration of how digital technology could be used to intervene to mitigate or reverse these detrimental effects is necessary. Suggestions to combine health equity principles with technology to overcome structural barriers could also potentially address structural stigma through innovative approaches. As highlighted in this review, the emergence of digital technologies offers new opportunities to accelerate anti-stigma efforts, especially in LMICs where there has been rapid growth in access to and use of smartphones and other mobile technologies in recent years [9]. Novel digital interventions could be used to break down misconceptions, misinformation and misguided views towards mental illness, and further extend the reach of efforts aimed at tackling mental health related stigma.
Acknowledgements:
Dr. Naslund reports receiving funding from the National Institute of Mental Health (Grant number: 5U19MH113211). The funder played no role in the study design; collection, analysis, or interpretation of data; writing of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Declaration of Interest: The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Patel V, Saxena S, Lund C, thornicroft G, Bingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018; 392: 1553–98. [DOI] [PubMed] [Google Scholar]
- 2.Rathod S, Pinniti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights 2017; 10:1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pathare S, Brazinova A,Levav I. Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiol Psychiatr Sci 2018; 27: 463–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu NH, Daumit GL, Dua T, Aquila R, Charlson F, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatr 2017; 16: 30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma: The mental illness stigma framework and critical review of measures. Stigma Health 2018; 3: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parcesepe AM, Cabassa LJ. Public stigma of mental illness in the United States: A systematic literature review. Adm Pol Ment Health 2013; 40: 384–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. , Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 2016; 387: 1123–32. [DOI] [PubMed] [Google Scholar]
- 8.Schueller SM, Torous J. Scaling evidence-based treatments through digital mental health. Am Psychol 2020; 75: 1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.We Are Social. Digital in 2021. 2021. [cited 2021 March 15]; Available from: https://wearesocial.com/global-digital-report-2019.
- 10.Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, et al. Digital innovations for global mental health: opportunities for data science, task sharing, and early intervention. Curr Treat Options Psychiatry 2019; 6: 337–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torous J, Myrick KJ, Rauseo-Ricupero N, Firht J. Digital mental health and COVID-19: Using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health 2020; 7: e18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodriguez-Villa E, Naslund J, Keshavan M, Patel V, Torous J. Making mental health more accessible in light of COVID-19: Scalable digital health with digital navigators in low and middle-income countries. Asian J Psychiatr 2020; 54: 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kola L, Kohrt BA, Hanlon C, Naslund J, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry 2021;8 : 535–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter H, Araya R, Anjur K, Deng D, Naslund J. The emergence of digital mental health in low-income and middle-income countries: A review of recent advances and implications for the treatment and prevention of mental disorders. J Psychiatric Res 2021; 133: 233–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merchant R, Torous J, Rodriguez-Villa E, Naslund J. Digital technology for management of severe mental disorders in low-income and middle-income countries. Curr Opin Psychiatry 2020; 33: 501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naslund JA, Shidhaye R, Patel V. Digital technology for building capacity of nonspecialist health workers for task sharing and scaling up mental health care globally. Harvard Rev Psychiatry 2019: p. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002;1: 16. [PMC free article] [PubMed] [Google Scholar]
- 18.Brohan E, Clement S, Rose D, Sartorius N, Slade M, et al. Development and psychometric evaluation of the Discrimination and Stigma Scale (DISC). Psychiatry Res 2013; 208: 33–40. [DOI] [PubMed] [Google Scholar]
- 19.Thornicroft G, Rose D, Kassam A. Discrimination in health care against people with mental illness. Int Rev Psychiatry 2007; 19: 113–22. [DOI] [PubMed] [Google Scholar]
- 20.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res 2003; 121: 31–49. [DOI] [PubMed] [Google Scholar]
- 21.Hatzenbuehler ML. Structural stigma: Research evidence and implications for psychological science. Am Psychol 2016; 71: 742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Personality Soc Psychol 1988; 55: 738. [DOI] [PubMed] [Google Scholar]
- 23.Martin JK, Pescosolido BA, Tuch SA. Of fear and loathing: The role of'disturbing behavior,'labels, and causal attributions in shaping public attitudes toward people with mental illness. J Health Soc Behav 2000; 41: 208–23. [Google Scholar]
- 24.Corrigan PW, Rao D. On the self-stigma of mental illness: Stages, disclosure, and strategies for change. Can J Psychiatry 2012; 57: 464–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pugh T, Hatzenbuehler M, Link B. Structural stigma and mental illness. Commissioned Paper for Committee on the Science of Changing Behavioral Health Social Norms, Mailman School of Public, Columbia University (August 2015), 2015. [Google Scholar]
- 26.Livingston JD. Mental illness-related structural stigma: The downward spiral of systemic exclusion final report. 2014: Mental Health Commission of Canada. [Google Scholar]
- 27.Hatzenbuehler ML, McLaughlin KA. Structural stigma and hypothalamic–pituitary–adrenocortical axis reactivity in lesbian, gay, and bisexual young adults. Ann Behav Med 2014; 47: 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henderson C, Thornicroft G. Stigma and discrimination in mental illness: Time to Change. Lancet 2009; 373: 1928–30. [DOI] [PubMed] [Google Scholar]
- 29.Krendl AC, Pescosolido BA. Countries and cultural differences in the stigma of mental illness: the east–west divide. J Cross-Cultural Psychol 2020; 51: 149–67. [Google Scholar]
- 30.Javed A, Lee C, Zakaria H, Buenaventura RD, Cetkovich-Bakmas M, et al. , Reducing the stigma of mental health disorders with a focus on low-and middle-income countries. Asian J Psychiatry 2021;58: 102601. [DOI] [PubMed] [Google Scholar]
- 31.Mascayano F, Armijo JE, Yang LH. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry 2015. 6: p. 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kemp CG, Jarrett BA, Kwon CS, Song L, Jetté N, Sapag JC, et al. Implementation science and stigma reduction interventions in low-and middle-income countries: a systematic review. BMC Med 2019; 17: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clay J, Eaton J, Gronholm PC, Semrau M, Votruba N. Core components of mental health stigma reduction interventions in low-and middle-income countries: a systematic review. Epidemiol Psychiatric Sci 2020; 29:e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naslund JA, Bondre A, Torous J, Aschbrenner KA. Social media and mental health: Benefits, risks, and opportunities for research and practice. J Technol Behav Sci 2020; 5: 245–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatric Sci 2016; 25: 113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Batterham PJ, Calear AL. Preferences for internet-based mental health interventions in an adult online sample: findings from an online community survey. JMIR Mental Health 2017; 4: e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brusilovskiy E, Townley G, Snethen G, Salzer MS. Social media use, community participation and psychological well-being among individuals with serious mental illnesses. Computers Hum Behav 2016; 65: 232–40. [Google Scholar]
- 38.Highton-Williamson E, Priebe S, Giacco D. Online social networking in people with psychosis: a systematic review. Int J Soc Psychiatry 2015; 61: 92–101. [DOI] [PubMed] [Google Scholar]
- 39.Miller BJ, Stewart A, Schrimsher J, Peeples D, Buckley PF. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res 2015; 225: 458–63. [DOI] [PubMed] [Google Scholar]
- 40.Indian M, Grieve R. When Facebook is easier than face-to-face: social support denned from Facebook in socially anxious individuals. Personal Indiv Differences 2014; 59: 102–6. [Google Scholar]
- 41.Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One 2014; 9: e110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gulliver A, Griffiths KM, Christensen H, Mackinnon A, Calear AL, Parsons A, et al. Internet-based interventions to promote mental health help-seeking in elite athletes: an exploratory randomized controlled trial. J Med Internet Res 2012; 14: e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shandley K, Austin D, Klein B, Kyrios M. An evaluation of ‘Reach Out Central’: an online gaming program for supporting the mental health of young people. Health Educ Res 2010; 25: 563–74. [DOI] [PubMed] [Google Scholar]
- 44.Burns JM, Durkin LA, Nicholas J. Mental health of young people in the United States: what role can the internet play in reducing stigma and promoting help seeking? J Adolescent Health 2009; 45: 95–7. [DOI] [PubMed] [Google Scholar]
- 45.Unger JB, Cabassa LJ, Molina GB, Contreras S, Baron M. Evaluation of a fotonovela to increase depression knowledge and reduce stigma among Hispanic adults. J Immigrant Minority Health 2013; 15: 398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Naslund JA, Bartels SM, Marsch LA. Digital technology, including telemedicine, in the management of mental illness. In Atkinson K & Mabey D (Eds.), Revolutionizing Tropical Medicine: Point-of-Care Tests, New Imaging Technologies and Digital Health (pp. 505–530). Wiley. [Google Scholar]
- 47.Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer JPatel V, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry 2017; 4: 486–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. Stigma Health 2015; 1: 2. [DOI] [PubMed] [Google Scholar]
- 49.Griffiths KM, Carron-Arthur B, Parsons A, Reid R. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta- analysis of randomized controlled trials. World Psychiatry 2014; 13: 161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.DeParle J. Rude, rash, effective, Act-Up shifts AIDS policy. The New York Times, 1990: p. B1. [Google Scholar]
- 51.Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature 2011; 475: 27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peek HS, Richards M, Muir O, Chan SR, Caton M, MacMillan C. Blogging and social media for mental health education and advocacy: a review for psychiatrists. Curr Psychiatry Rep 2015; 17: 88. [DOI] [PubMed] [Google Scholar]
- 53.Corrigan P, Gelb B. Three programs that use mass approaches to challenge the stigma of mental illness. Psychiatric Serv 2006; 57: 393–8. [DOI] [PubMed] [Google Scholar]
- 54.Armstrong G, Vijayakumar L, Pirkis J, Jayaseelan M, Cherian A, Soerensen JB, et al. Mass media representation of suicide in a high suicide state in India: an epidemiological comparison with suicide deaths in the population. BMJ open 2019; 9: e030836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ganesh R, Singh S, Mishra R, Sagar R. The quality of online media reporting of celebrity suicide in India and its association with subsequent online suicide-related search behaviour among general population: An infodemiology study. Asian J Psychiatr 2020; 53: 102380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Menon V, Kar SK, Varadharajan N, Kalaimoorthy C, Pattnaik JI, Sharma G, et al. Quality of media reporting following a celebrity suicide in India. J Public Health 2020:fdaa161. [DOI] [PubMed] [Google Scholar]
- 57.Corrigan PW, River LP, Lunin RK, Penn DL, Uphoff-Wasowski K, Campion J, et al. Three strategies for changing attributions about severe mental illness. Schizophr Bull 2001; 27: 187–95. [DOI] [PubMed] [Google Scholar]
- 58.Arboleda-Flórez J, Stuart H. From sin to science: fighting the stigmatization of mental illnesses. Can J Psychiatry 2012; 57: 457–63. [DOI] [PubMed] [Google Scholar]
- 59.Hasan MT, Thornicroft G. Mass media campaigns to reduce mental health stigma in Bangladesh. Lancet Psychiatry 2018; 5: 616. [DOI] [PubMed] [Google Scholar]
- 60.Maulik PK, Devarapalli S, Kallakuri S, Tewari A, Chilappagari S, Koschorke M, et al. Evaluation of an anti-stigma campaign related to common mental disorders in rural India: a mixed methods approach. Psychol Med 2017; 47: 565–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maulik PK, Devarapalli S, Kallakuri S, Tripathi AP, Koschorke M, et al. Longitudinal assessment of an anti-stigma campaign related to common mental disorders in rural India. Br J Psychiatry 2019; 214: 90–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shields-Zeeman L, Pathare S, Walters BH, Kapadia-Kundu N, Joag K. Promoting wellbeing and improving access to mental health care through community champions in rural India: the Atmiyata intervention approach. Int J Mental Health Syst 2017; 11: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jorm AF. Effect of contact-based interventions on stigma and discrimination: A critical examination of the evidence. Psychiatric Serv 2020; 71: 735–7. [DOI] [PubMed] [Google Scholar]
- 64.Gonsalves PP, Hodgso ES, Michelson D, Pal S, Naslund J, Sharma R, et al. What are young Indians saying about mental health? A content analysis of blogs on the It’s Ok To Talk website. BMJ Open 2019; 9: e028244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang R, Eschler J, Reddy M. Online support groups for depression in China: Culturally shaped interactions and motivations. Computer Supported Cooperative Work (CSCW), 2018; 27: 327–54. [Google Scholar]
- 66.Goepfert NC, von Heydendorff SC, Dressing H, Bailer J. Effects of stigmatizing media coverage on stigma measures, self-esteem, and affectivity in persons with depression–an experimental controlled trial. BMC pPsychiatr 2019; 19: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Aragonès E, Lopez-Muntaner J, Ceruelo S, Basora J. Reinforcing stigmatization: coverage of mental illness in Spanish newspapers. J Health Commun 2014; 19: 1248–58. [DOI] [PubMed] [Google Scholar]
- 68.Olushola O, Bolanle O, Olurotimi C, Abiodun A, Akintayo O. Analysis of media reporting of suicidal behavior in Nigeria. Mental Health Prevention 2021: p. 200197. [Google Scholar]
- 69.Nisa N, Arifin M, Nur MF, Adella S, Marthoenis M. Indonesian online newspaper reporting of suicidal behavior: Compliance with World Health Organization media guidelines. Int J Soc Psychiatry 2020; 66: 259–62. [DOI] [PubMed] [Google Scholar]
- 70.Pirkis J. Suicide and the media. Psychiatry 2009; 8: 269–71. [Google Scholar]
- 71.Sinyor M, TseR, Pirkis J. Global trends in suicide epidemiology. Current Opin Psychiatry 2017; 30: 1–6. [DOI] [PubMed] [Google Scholar]
- 72.Chan G, Yanos PT. Media depictions and the priming of mental illness stigma. Stigma Health 2018; 3: 253. [Google Scholar]
- 73.Angermeyer MC, Matschinger H. The effect of violent attacks by schizophrenic persons on the attitude of the public towards the mentally ill. Soc Sci Med 1996; 43: 1721–8. [DOI] [PubMed] [Google Scholar]
- 74.Nawková L, Nawka A, Adamkova T, Rukavina TV, Holcnerova P, Kuzman MR, et al. The picture of mental health illness in the printed media in three central European countries. J Health Commun 2012; 17: 22–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kohrt BA, Rasmussen A, Kaiser BN, Haroz EE, Mahajan SM, Mutamba BB, et al. Cultural concepts of distress and psychiatric disorders: literature review and research recommendations for global mental health epidemiology. Int J Epidemiol 2014; 43: 365–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nieuwsma JA, Pepper CM, Maack DJ, Birgenheir DG. Indigenous perspectives on depression in rural regions of India and the United States. Transcult Psychiatry 2011; 48: 539–68. [DOI] [PubMed] [Google Scholar]
- 77.Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clin Psychol Rev 2011; 31: 934–48. [DOI] [PubMed] [Google Scholar]
- 78.Gopalkrishnan N Cultural diversity and mental health: Considerations for policy and practice. Fron Public Health 2018; 6: 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Javed A, Herrman H. Involving patients, carers andfamilies: an international perspective on emerging priorities. B J Psych Int 2017; 14: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sweetland AC, Oquendo MA, Carlson C, Magidson JF, Wainberg ML. Mental health research in the global era: training the next generation. Acad Psychiatry 2016; 40: 715–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nsereko JR, Kizza D, Kigozi F, Ssebunnya J, Ndyanabangi S, Flicher AJ, et al. Stakeholder's perceptions of help-seeking behaviour among people with mental health problems in Uganda. Int J Mental Health Syst 2011; 5: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Akol A, Moland KM, Babirye J, Engebretsen IMS. “We are like co-wives”: Traditional healers' views on collaborating with the formal Child and Adolescent Mental Health System in Uganda. BMC Health Serv Res 2018; 18: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hays K, Costello J. Reflections on the cultural adaptations and implementation challenges of mental health first aid in Uganda: A case study. Psychol Serv 2021.doi101037. [DOI] [PubMed] [Google Scholar]
- 84.WonPat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol 2012; 47: 145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Heim E, Kohrt BA. Cultural Adaptation of Scalable Psychological Interventions. Clin Psychol Europe 2019; 1: 1–22. [Google Scholar]
- 86.Corrigan PW, Watson AC. The paradox of self - stigma and mental illness. Clin Psychol Sci Pract 2002; 9: 35–53. [Google Scholar]
- 87.Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psychiatric Serv 2007; 58:1547–54. [DOI] [PubMed] [Google Scholar]