Abstract
Background
Crowded teeth develop when there is not enough space in the jaws into which the teeth can erupt. Crowding can affect baby teeth (deciduous dentititon), adult teeth (permanent dentition), or both, and is a common reason for referral to an orthodontist. Crowded teeth can affect a child's self‐esteem and quality of life. Early loss of baby teeth as a result of tooth decay or trauma, can lead to crowded permanent teeth. Crowding tends to increase with age, especially in the lower jaw.
Objectives
To assess the effects of orthodontic intervention for preventing or correcting crowded teeth in children.
To test the null hypothesis that there are no differences in outcomes between different orthodontic interventions for preventing or correcting crowded teeth in children.
Search methods
Cochrane Oral Health's Information Specialist searched four bibliographic databases up to 11 January 2021 and used additional search methods to identify published, unpublished and ongoing studies.
Selection criteria
We included randomised controlled trials (RCTs) that evaluated any active interventions to prevent or correct dental crowding in children and adolescents, such as orthodontic braces or extractions, compared to no or delayed treatment, placebo treatment or another active intervention. The studies had to include at least 80% of participants aged 16 years and under.
Data collection and analysis
Two review authors, independently and in duplicate, extracted information regarding methods, participants, interventions, outcomes, harms and results. We resolved any disagreements by liaising with a third review author. We used the Cochrane risk of bias tool to assess the risk of bias in the studies. We calculated mean differences (MDs) with 95% confidence intervals (CI) for continuous data and odds ratios (ORs) with 95% CIs for dichotomous data. We undertook meta‐analysis when studies of similar comparisons reported comparable outcome measures, using the random‐effects model. We used the I2 statistic as a measure of statistical heterogeneity.
Main results
Our search identified 24 RCTs that included 1512 participants, 1314 of whom were included in analyses. We assessed 23 studies as being at high risk of bias and one as unclear.
The studies investigated 17 comparisons. Twenty studies evaluated fixed appliances and auxiliaries (lower lingual arch, lower lip bumper, brackets, archwires, lacebacks, headgear and adjunctive vibrational appliances); two studies evaluated removable appliances and auxiliaries (Schwarz appliance, eruption guidance appliance); and two studies evaluated dental extractions (lower deciduous canines or third molars).
The evidence should be interpreted cautiously as it is of very low certainty. Most interventions were evaluated by a single study.
Fixed appliances and auxiliaries
One study found that use of a lip bumper may reduce crowding in the early permanent dentition (MD −4.39 mm, 95% CI −5.07 to −3.71; 34 participants). One study evaluated lower lingual arch but did not measure amount of crowding.
One study concluded that coaxial nickel‐titanium (NiTi) archwires may cause more tooth movement in the lower arch than single‐stranded NiTi archwires (MD 6.77 mm, 95% CI 5.55 to 7.99; 24 participants). Another study, comparing copper NiTi versus NiTi archwires, found NiTi to be more effective for reducing crowding (MD 0.49 mm, 95% CI 0.35 to 0.63, 66 participants). Single studies did not show evidence of one type of archwire being better than another for Titinol versus Nitinol; nickel‐titanium versus stainless steel or multistrand stainless steel; and multistranded stainless steel versus stainless steel.
Nor did single studies find evidence of a difference in amount of crowding between self‐ligating and conventional brackets, active and passive self‐ligating brackets, lacebacks added to fixed appliances versus fixed appliances alone, or cervical pull headgear versus minor interceptive procedures.
Meta‐analysis of two studies showed no evidence that adding vibrational appliances to fixed appliances reduces crowding at 8 to 10 weeks (MD 0.24 mm, 95% CI −0.81 to 1.30; 119 participants).
Removable appliances and auxiliaries
One study found use of the Schwarz appliance may be effective at treating dental crowding in the lower arch (MD ‐2.14 mm, 95% CI −2.79 to −1.49; 28 participants). Another study found an eruption guidance appliance may reduce the number of children with crowded teeth after one year of treatment (OR 0.19, 95% CI 0.05 to 0.68; 46 participants); however, this may have been due to an increase in lower incisor proclination in the treated group. Whether these gains were maintained in the longer term was not assessed.
Dental extractions
One study found that extracting children's lower deciduous canines had more effect on crowding after one year than no treatment (MD −4.76 mm, 95 CI −6.24 to −3.28; 83 participants), but this was alongside a reduction in arch length. One study found that extracting wisdom teeth did not seem to reduce crowding any more than leaving them in the mouth (MD −0.30 mm, 95% CI −1.30 to 0.70; 77 participants).
Authors' conclusions
Most interventions were assessed by single, small studies. We found very low‐certainty evidence that lip bumper, used in the mixed dentition, may be effective for preventing crowding in the early permanent dentition, and a Schwarz appliance may reduce crowding in the lower arch. We also found very low‐certainty evidence that coaxial NiTi may be better at reducing crowding than single‐stranded NiTi, and that NiTi may be better than copper NiTi. As the current evidence is of very low certainty, our findings may change with future research.
Plain language summary
What is the best treatment for children with crowded teeth?
What are crowded teeth?
When teeth erupt (come through the gum into the mouth), they may twist, stick out, drop back, or overlap if there is not enough space in the mouth. Losing baby teeth early from tooth decay or trauma can lead to crowded permanent teeth. If crowded teeth affect a child's self‐esteem or cause pain, damage or chewing problems, the child may be referred to a specialist dentist known as an orthodontist to correct them. Orthodontics is about the growth of the jaws and face, and development of the teeth and bite.
What is orthodontic treatment?
Crowded teeth can be prevented or corrected using braces if crowding is mild (less than 4 mm). Removal of some teeth (extraction) may also be needed if crowding is moderate (4 to 8 mm) or severe (more than 8 mm). Fixed braces are used on permanent teeth. Removable braces can be used on baby or permanent teeth, or both. Baby or permanent teeth can be extracted.
Fixed braces
Fixed braces attach parts to each tooth using dental glue, with brackets holding a wire that puts a force on the teeth, to move and straighten them. The wire is secured with metal ties, small rubber bands or a clip that is built into the bracket ('self‐ligating').
A lower lingual arch (LLA) or lip bumper (LB) retains the lower back teeth (molars) while allowing the lower front teeth to straighten and move forwards. To remove pressure on the teeth, a LLA wire lies on the inner side of the teeth; a LB wire lies on the outer side. The 0.9 mm stainless steel wires are attached to metal bands around the back (molar) teeth at either end, with the LB wire having a plastic coating at the front.
Sometimes extra items are used with fixed braces, such as headgear (straps attached to a frame outside the mouth), vibrating plates or lacebacks (thin wires holding teeth together).
Removable braces
Removable braces are usually made from hard plastic that joins together active parts that move the teeth and clips that secure the brace. Some removable braces are made from moulded flexible plastic.
The Schwarz appliance has a screw that is turned once a week by parents, to widen the arch of the lower jaw and make more space into which the permanant teeth can move.
The eruption guidance appliance guides permanent teeth into a better position as they erupt. It is a combined upper and lower brace that holds the lower jaw forwards, and has guiding slots to align the front teeth and improve the side teeth bite.
Extraction
Baby eye teeth (canines) are extracted when children have a mix of adult and baby teeth, to provide space into which other teeth can move.
Wisdom teeth (third molars) may be removed any time from when they form (early teenage years) until adulthood, to help prevent them putting forward pressure on the other teeth.
What did we want to know?
We aimed to evaluate scientific research on the effectiveness of orthodontic treatments (fixed braces, removable braces, tooth extraction) used to prevent or correct crowded teeth in children aged 16 years old or younger. We searched for studies that compared these treatments against no treatment, delayed treatment, placebo (pretend treatment) or another orthodontic treatment.
What studies did we find?
We included 24 studies that presented results from 1314 children aged from 7 to 16 years in different countries. Twenty studies tested fixed braces, two tested removable braces and two tested extractions.
What were the main results?
Fixed braces and related items
A lower lip bumper may prevent crowding when the adult teeth are starting to come through. Nickel‐titanium wires may correct crowding better than wires made of copper nickel‐titanium, and twisted multi‐stranded (co‐axial) nickel‐titanium archwires may be better than single‐stranded ones. However, we cannot be sure of these findings.
For the other comparisons evaluated, it was not possible to show that one group did better or worse than the other for reducing crowding.
Removeable braces and related items
The Schwarz appliance may reduce crowding in the lower arch, when measured at nine months. Use of an eruption guidance appliance, for a year, may reduce likelihood of crowding, but there may be other explanations for this. Again, we cannot be sure of these findings.
Extraction
Taking out wisdom teeth (third molars) does not seem to affect crowding later in life, while taking out the pointy baby teeth (canines) from the lower jaw, may reduce crowding in the short term, but we cannot be sure of this. There are probably other explanations for this finding.
What are the limitations of the evidence?
The evidence is uncertain. It consists of small, individual studies testing different treatments. Some of them have problems with how they were carried out. We cannot be sure about our findings and future research may change them.
How up to date is the evidence?
The evidence is up to date to January 2021.
Summary of findings
Background
Description of the condition
Crowded teeth develop when there is not enough space in the jaws into which the teeth can erupt. This gives the child crooked or 'wonky' teeth that may be the focus of teasing at school (Shaw 1980; Shaw 1981), or later in life (Shaw 1985), and can result in low self‐esteem (Jung 2010). Crowded teeth is the problem seen most commonly by orthodontists. Prevalence of crowding varies, but it affects nearly half of 12‐year‐old children in the UK (Holmes 1992).
Crowding can affect baby teeth (deciduous dentition) or adult teeth (permanent dentition). Crowding tends to increase with age, especially in the lower jaw, so that only a third of adults have well‐aligned lower front teeth (incisors) (Proffit 1998). Crowding occurs when there is a difference between the size of the jaws and teeth, for example, the jaws are too small to hold the teeth. Crowding of the adult teeth can also occur when space is lost following the early loss of baby teeth, either as a result of tooth decay or trauma (Bhujel 2014; Bhujel 2016).
Description of the intervention
Orthodontics is the branch of dentistry concerned with the growth of the jaws and face, the development of the teeth and the way the teeth and jaws bite together. It also involves treatment of the teeth and jaws when they are irregular or bite in an abnormal way, or both. There are many reasons why the teeth may not bite together correctly. These include the position of the teeth, jaws, lips, tongue or cheeks, or may be due to a habit or the way people breathe. The need for treatment can be decided by looking at the effect of any particular tooth position on the life expectancy of the teeth, the function of the teeth or the effect that the appearance of the teeth has on how people feel about themselves (Shaw 1991).
There are many different orthodontic interventions that can be used to prevent or correct crowded teeth. The purpose of this review is to assess the current body of available evidence and determine which intervention or interventions are the most effective.
Several dental brace (orthodontic) treatments have been proposed to correct or prevent crowding. Some treatments use braces to expand the teeth or jaws. These treatments can be carried out early, before children are six years of age, when only baby teeth are present. Other treatments can be carried out when children have a mixture of baby and adult teeth (around 7 to 11 years of age). Treatments carried out at this stage use braces to maintain the space that arises when the baby back teeth (molars) are lost and replaced by smaller adult sized teeth (premolars).
Other treatments can be used later when all the adult teeth have come into the mouth (around 12 to 16 years of age), either using braces to expand the teeth or jaws, or removing teeth to create space so that the remaining teeth can be straightened using a brace. Braces can either be removed from the mouth or fixed to the teeth with special glue. Other types of brace are attached, via the teeth, to devices (headgear) that allow a force to be applied to the teeth and jaws from the back of the head.
Interventions to prevent or correct dental crowding in children can be divided into the following categories: fixed braces and auxiliaries, removable braces and auxiliaries, and extraction of teeth.
How the intervention might work
Fixed appliances and auxiliaries
Several interventions have been used to prevent or correct dental crowding in children using fixed appliances and auxiliaries.
The lip bumper and lingual arch maintain the space resulting from the total width of the adult eye teeth (canines) and side teeth (premolars) being less than the baby eye teeth (canine) and back teeth (molars) that they are replacing. The crowded teeth can then move into this extra (leeway) space, which allows the crowding to reduce.
Cervical pull headgear is attached to the back teeth (molars) and used to move them backwards to make more space nearer the front of the mouth into which crowded teeth can be aligned.
Different orthodontic bracket designs (self‐ligating versus conventional; active self‐ligating versus passive) claim to provide less resistance (friction) to tooth movement, allowing the teeth to move and align more quickly.
Different orthodontic archwires (copper nickel‐titanium versus nickel‐titanium; coaxial nickel‐titanium versus nickel‐titanium; nitinol versus titinol; nickel‐titanium versus multistranded stainless steel; nickel‐titanium versus stainless steel; multistranded stainless steel versus stainless steel) claim to move the teeth more gently or more consistently, or both, over a longer period of time, depending on the characteristics of the wires, allowing the teeth to move and align more efficiently.
The use of lacebacks, with fixed appliances, has also been claimed to help align the teeth more quickly and reduce the amount of crowding by influencing the position of the front teeth (incisors).
Vibrational appliances are used with fixed appliances. It is claimed that the vibrations increase the rate of tooth movement so the teeth straighten more quickly.
Removable appliances and auxiliaries
The Schwarz appliance is used to expand the lower teeth and provide extra space into which crowded teeth can be aligned.
The eruption guidance appliance again uses the difference between the size of the baby back (molar) teeth and adult side (premolar) teeth to provide extra space space into which the erupting adult teeth can be guided and to relieve any crowding.
Extractions
The lower deciduous eye teeth (canines) can be extracted to provide space into which the permanent front teeth (incisors) can spread and align.
Extraction of wisdom teeth (third molars) has been claimed to prevent the development of crowding of the front teeth (incisors) in later life.
Why it is important to do this review
As dental crowding has been found to affect oral health‐related quality of life (Jung 2015), and self‐esteem (Jung 2010) significantly, it is reasoned that treating crowding in children will improve psychological health, well‐being and body image in adulthood (Javidi 2017). Dentists, orthodontists, parents and children need guidance on whether and how best to intervene to prevent or correct crowded teeth.
Objectives
To assess the effects of orthodontic interventions for preventing or correcting crowded teeth in children.
To test the null hypothesis that there are no differences in outcomes between different orthodontic interventions for preventing or correcting crowded teeth in children.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled clinical trials (RCTs) of orthodontic treatments to prevent or correct crowded teeth where one intervention was compared concurrently to a placebo, no intervention or another method to prevent or correct dental crowding.
Types of participants
Studies were eligible for inclusion in the review if they had recruited children (aged 16 years old or under) receiving orthodontic treatment to prevent or correct crowded teeth.
We excluded studies involving participants with a cleft lip or palate or other craniofacial syndromes. We excluded studies where less than 80% of participants were aged 16 years old or less.
Types of interventions
We assessed the following active interventions to prevent or correct dental crowding:
fixed appliances and auxiliaries;
removable appliances and auxiliaries;
extractions.
We evaluated any intervention or combination of treatments, at any time during treatment.
Controls
Control conditions could be: no treatment, delayed treatment, placebo or another active intervention.
Types of outcome measures
We recorded clinically important outcomes at the most common endpoints that were reported for all ages. If harms were identified, we recorded them and reported them in descriptive terms.
Primary outcomes
Amount of crowding (measured in mm or by any index of malocclusion)
Secondary outcomes
Size of the upper jaw (arch length)
Size of the lower jaw (arch length)
Upper incisors to maxilla
Lower incisors to mandible
Lower molars to mandible
Time to alignment
Time for ligation
Self‐esteem
Participant satisfaction
Jaw joint problems
Other outcomes
Harms (recorded and reported in descriptive terms)
Health of the gums
Damage to the teeth (such as tooth decay)
Pain (including the use of analgesia)
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year or publication status restrictions:
Cochrane Oral Health’s Trials Register (searched 11 January 2021; Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 12) in the Cochrane Library (searched 11 January 2021; Appendix 2);
MEDLINE Ovid (1946 to 11 January 2021; Appendix 3);
Embase Ovid (1980 to 11 January 2021; Appendix 4);
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategies designed by Cochrane for identifying RCTs and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions, Version 6.1, (Lefebvre 2020)).
Searching other resources
Ww searched the following trials registries for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 11 January 2021; Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 11 January 2021; Appendix 6).
We handsearched the British (BJO), European (EJO), and American (AJO‐DO) journals of orthodontics and the Angle Orthodontist (AO), from 1994‐1998. However, these journals are now indexed on MEDLINE so we discontinued the handsearching from 1998 onwards. We searched the bibliographies of papers identified in this search for relevant studies.
We contacted the first‐named authors of all study reports in an attempt to identify unpublished studies and to obtain any further information about the studies.
We searched the reference lists of included studies and relevant systematic reviews, for further appropriate studies.
We did not perform a separate search for harms of interventions used; we considered adverse effects described in included studies only.
We checked that none of the included studies in this review were retracted due to error or fraud.
Data collection and analysis
Selection of studies
Two review authors (JH and DM or JH and FS or ST and DO), independently and in duplicate, assessed the titles and abstracts (when available) of all reports that were identified as potentially relevant by the search. The search was designed to be sensitive and include controlled clinical trials, these were filtered out early in the selection process if they were not randomised.
We obtained the full text of studies that were potentially relevant, studies that had insufficient information in the title and abstract to make a decision about inclusion, and studies where the review authors disagreed about eligibility. At least two review authors then assessed these full‐text papers, independently and in duplicate, to establish whether or not the studies met the inclusion criteria. The review authors were not blinded to study author(s), institution or site of publication. We resolved disagreements by discussion between JH and DM or JH and FS or ST and DO with JH. We kept a record of all decisions made about the potentially eligible studies.
Data extraction and management
At least two review authors independently extracted data including the year of publication, interventions assessed, outcomes, sample size and age of participants. The primary outcome was the amount of crowding and secondary outcomes were size of the upper and lower jaws (arch length); relationship of the upper front teeth (incisors) to the upper jaw (maxilla); relationship of the lower front teeth (incisors) and lower back teeth (molars) to the lower jaw (mandible); self‐esteem; participant satisfaction; jaw joint problems; time to alignment and time for ligation.
We recorded other outcomes, such as harms. For example, we recorded health of the gums or damage to the teeth (such as tooth decay) and pain, and reported the results in descriptive terms.
We extracted outcome data at all time points and reported the most common time points.
Assessment of risk of bias in included studies
At least two review authors assessed the risk of bias independently and in duplicate using the Cochrane risk of bias tool (RoB 1), as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We assessed the risk of bias in seven domains: random sequence generation; allocation concealment; blinding of participants and personnel, blinding of outcome assessment; incomplete outcome data; selective outcome reporting and 'other sources of bias'. For each domain, we assigned a judgement of high, low or unclear risk of bias according to the following criteria:
low risk of bias if plausible bias unlikely to seriously alter the results;
high risk of bias if plausible bias that seriously weakens confidence in the results;
unclear risk of bias if plausible bias that raises some doubt about the results.
We assessed sequence generation, allocation concealment and selective outcome reporting for the study as a whole. We assessed blinding and incomplete outcome data on the level of the study and for each outcome as appropriate.
We considered the overall risk of bias in each study as 'low' if we assessed all seven domains as low risk; unclear if all domains were at low or unclear risk of bias; and high if we assessed at least one domain as being at high risk of bias.
Measures of treatment effect
For continuous outcomes (e.g. amount of crowding (mm) or arch length) measured using the same scale, we used the mean values and standard deviations (SDs) reported in the studies in order to express the estimate of effect as mean difference (MD) with 95% confidence interval (CI). Where available, we used the change in the outcome measured from baseline.
For dichotomous outcomes (e.g. harm: yes or no), we expressed the estimate of effect as a risk ratio (RR) with 95% CI.
Unit of analysis issues
The unit of analysis was the participant. For multi‐arm studies, we selected the most appropriate arms to compare, or combined arms, using methods described in where possible and appropriate.
Dealing with missing data
We attempted to contact the study author(s) in cases of missing data for all included studies, when feasible, in order to gather details of outcomes that were measured but not reported, or for clarification and details. We did not need to use the methods described in Chapter 5 of the Cochrane Handbook for Systematic Reviews of Interventions to estimate missing standard deviations due to unclear or unavailable data (Li 2021). We used the RevMan calculator to combine continuous outcomes of different arms in multi‐arm parallel trials comparing two or more active treatments against a control. We did not use any other statistical methods or perform any further imputation to account for missing data.
Assessment of heterogeneity
We assessed clinical heterogeneity by identifying the participants, interventions and outcomes and considering whether a meaningful summary would be produced by combining the results. We also assessed heterogeneity statistically using a Chi2 test, where a P value less than 0.1 indicates statistically significant heterogeneity. We quantified heterogeneity using the I2 statistic (Higgins 2003). A guide to interpretation of the I2 statistic given in Section 10.10.2 of the Cochrane Handbook for Systematic Reviews of Interventions is as follows (Deeks 2021):
0% to 40% might not be important;
30% to 60% may represent moderate heterogeneity;
50% to 90% may represent substantial heterogeneity;
75% to 100% represents considerable heterogeneity.
Assessment of reporting biases
We had planned to assess reporting bias via funnel plot asymmetry if more than 10 studies were to be included in a meta‐analysis, as described in section 10.10.4.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2021). Whilst we had a sufficient number of studies included in this review for the primary outcome, the results were diluted due to the multiple different interventions and comparisons undertaken; we were therefore unable to use funnel plots to assess publication bias.
Data synthesis
We only carried out meta‐analyses when there were studies of similar comparisons reporting the same outcomes. We combined mean differences (MDs) for continuous data, and RRs for dichotomous data. Our general approach was to use a random‐effects model. With this approach, the CIs for the average intervention effect were wider than those that would have been obtained using a fixed‐effect approach, leading to a more conservative interpretation. We presented the results of single studies where a comparison and outcome was measured in only one study.
Subgroup analysis and investigation of heterogeneity
Had sufficient relevant data been available, we would have carried out a subgroup analysis on the age (stage of dental development) at which treatment was undertaken.
Sensitivity analysis
We did not plan or carry out any sensitivity analyses.
Summary of findings and assessment of the certainty of the evidence
We created a summary of findings table for each type of intervention (fixed appliances and auxiliaries, removable appliances and auxiliaries, and extractions). We presented summary information for the amount of crowding as this was our primary and most clinically relevant outcome. Two review authors independently assessed the certainty of the evidence using GRADE criteria (GRADE 2004; Schünemann 2021).
Results
Description of studies
Results of the search
The electronic search identified 2225 references to studies after the removal of duplicates. We identified nine additional articles from additional sources. We screened all titles and abstracts, where available, and discarded 2123. For the remaining 111 articles, we obtained full‐text articles where possible, and excluded 62 records at this stage (see Excluded studies). Ten studies were systematic reviews whose reference lists we searched (Afzal 2020; Chen 2019; El‐Angbawi 2015; Ke 2019; Papageorgiou 2019; Song 2009; Vieira 2018; Wang 2018; Wazwaz 2021; Yu 2013). Of the remaining studies, we were able to include 32 records of 24 studies, five studies await classification and two studies are ongoing (see Studies awaiting classification and Ongoing studies). Figure 1 summarises our study selection process.
1.
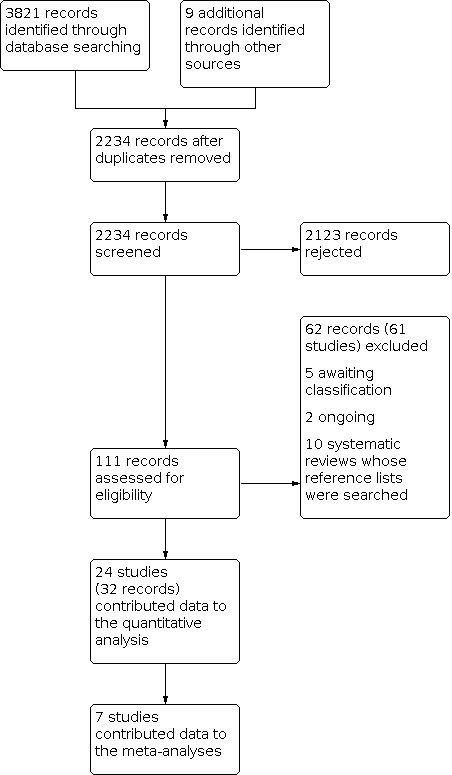
Study flow diagram
Included studies
We included 24 RCTs, involving a total of 1512 participants in this review of whom they included 1314 in analyses. All 24 studies provided data for the review. However, two of these studies only provided data for harms; we have reported these data descriptively. The studies investigated 17 different comparisons.
Characteristics of the study designs and settings
Design
All studies were of parallel design. Four studies had three arms (Gravina 2013; Ong 2011; Songra 2014; Woodhouse 2015). The remaining studies had two arms.
Setting
Five studies took place in the UK (Harradine 1998; Irvine 2004; O'Brien 1990; Songra 2014; Woodhouse 2015); four studies were conducted in Australia (Miles 2010; Miles 2012; Miles 2016; Ong 2011); three in Corfu, Greece (Pandis 2009; Pandis 2010a; Pandis 2011); three in Turkey (Aras 2018; Atik 2014; Aydin 2018); two in India (Sandhu 2013; Sebastian 2012), and one in each in Brazil (Gravina 2013); Finland (Finland 2004); Japan (Tai 2010); Norway (Myrlund 2015); and the USA (Davidovitch 1997). The setting for one study is unknown (Rebellato 1997). One study was multinational, being conducted in Wales, Italy and Germany (Kau 2004).
Centres
There were two studies with three centres (Kau 2004; Woodhouse 2015). Myrlund 2015 recruited across two centres, but all treatment was carried out in one centre. The other studies involved a single centre.
Funding
Seven studies reported their funding source: one received independent funding from government (Kau 2004), four from charity (Aydin 2018; Finland 2004; Miles 2016; Ong 2011), and two from orthodontic companies (Myrlund 2015; O'Brien 1990). The remaining studies did not report any funding source.
Conflict of interest
In five studies, the authors declared that they had no commercial or financial conflicts of interest (Aras 2018; Aydin 2018; Songra 2014; Tai 2010; Woodhouse 2015). However, one of these studies later acknowledged an engineering company for developing the software that the authors used to disprove their null hypothesis (Tai 2010). Another study declared that their appliances were supplied by the company that developed the appliance (Woodhouse 2015). Two other studies declared that commercial companies supplied them with materials or appliances (Myrlund 2015; O'Brien 1990). The remaining 15 studies did not report on any conflicts of interest.
Characteristics of the participants
We included 24 studies, which randomised a total of 1512 participants and analysed data from 1314 participants (see Characteristics of included studies). The mean age of participants within the studies ranged from 7.6 years to 15.3 years. Fifteen studies reported the number of male and female participants (Aras 2018; Atik 2014; Aydin 2018; Finland 2004; Gravina 2013; Harradine 1998; Irvine 2004; Myrlund 2015; Ong 2011; Pandis 2009; Pandis 2011; Sebastian 2012; Songra 2014; Tai 2010; Woodhouse 2015). The percentage of male participants ranged from 23.3% to 58.8% in these studies, other than in two that included female participants only (Atik 2014; Sebastian 2012).
Characteristics of the interventions and comparisons
We identified studies that compared interventions to prevent the perpetuation of crowding from the mixed dentition into the permanent dentition or to correct crowding in the permanent dentition. The interventions could be broadly divided into the following three categories: fixed appliances and auxiliaries; removable appliances and auxiliaries; and extractions.
Fixed appliances and auxiliaries
Twenty studies evaluated fixed appliances and auxiliaries. These interventions included: lip bumper (Davidovitch 1997), cervical pull headgear (Finland 2004), lingual arch (Rebellato 1997), brackets (Aras 2018; Atik 2014; Miles 2010; Pandis 2010a; Pandis 2011; Songra 2014), archwires (Aydin 2018; Gravina 2013; O'Brien 1990; Ong 2011; Pandis 2009; Sandhu 2013; Sebastian 2012), lacebacks (Irvine 2004), and adjunctive vibrational appliances (Miles 2012; Miles 2016; Woodhouse 2015).
Lower lip bumper
One study compared treatment with a lip bumper therapy to a control group, which did not receive any active treatment, to assess changes in the arch perimeter changes (Davidovitch 1997).
Cervical pull headgear
One study compared cervical pull headgear to a control group, which received interceptive procedures during the study duration to improve the alignment of the anterior teeth if deemed necessary (Finland 2004). The interceptive procedures consisted of extraction of the upper deciduous canines, extraction of the lower deciduous canines or interdental stripping. We identified three reports to this study that reported different outcomes at different time points.
Lower lingual arch
One study compared the passive lower lingual arch appliance against a control group that did not receive any active treatment during the study period. The aim was assess changes in arch length and lower incisor inclination arch length and incisor inclinational changes (Rebellato 1997).
Brackets
Six studies compared different types of orthodontic brackets.
Three studies compared a combination of conventional brackets with passive or active, or both, self‐ligating metal brackets (Atik 2014; Pandis 2011; Songra 2014). In Atik 2014, the conventional group underwent treatment with a quad‐helix before fixed appliance therapy.
One study compared ceramic self‐ligating brackets with conventional ceramic brackets (Miles 2010), one study compared active and passive self‐ligating brackets (Pandis 2010a), and one study compared metal self‐ligating brackets with conventional metal brackets (Aras 2018).
Archwires
Seven studies compared different archwire types against one another.
Two studies had three parallel arms. One compared two different nickel‐titanium archwire sequences (for which we combined the data) and a copper nickel‐titanium archwire sequence (Ong 2011), and one compared stainless steel, multistranded stainless steel and nickel‐titanium archwires (Gravina 2013).
The remaining five studies had two parallel arms. One study compared stabilised nickel‐titanium (Nitinol) against super–elastic nickel‐titanium (Titinol; O'Brien 1990); two compared nickel‐titanium against copper nickel titanium (Aydin 2018; Pandis 2009), one compared nickel‐titanium to multistranded stainless steel (Sandhu 2013), and one study compared coaxial nickel‐titanium against single stranded nickel‐titanium (Sebastian 2012).
Lacebacks
One study compared the use of lacebacks with fixed appliances to a control group where only fixed appliances were used (Irvine 2004).
Vibrational appliances
Three studies investigated the effects of vibrational appliances on crowding.
Two studies had two parallel arms: one study compared the vibrational appliance (Tooth Masseuse) and fixed appliances with fixed appliances alone (Miles 2012); the other compared a vibrational appliance (AcceleDent) and fixed appliances to fixed appliances alone (Miles 2016). The third study had three parallel arms consisting of participants who underwent mandibular first premolar extractions and received the vibrational appliance (AcceleDent) and fixed appliances versus fixed appliances only (Woodhouse 2015). There was an arm with a sham AcceleDent device and fixed appliances that we did not use in our review.
Removable appliances and auxiliaries
Two studies evaluated removable appliances and auxiliaries: the Schwarz appliance (Tai 2010), and the eruption guidance appliance (Myrlund 2015).
Schwarz appliance
One study compared the use of the Schwarz appliance to expand the upper and lower arches against a control group where the participants received no treatment (Tai 2010).
Eruption guidance appliance
One study compared the use of an eruption guidance appliance for both the upper and lower arches to a control group where the participants received no treatment (Myrlund 2015).
Extractions
Two studies looked at extracting teeth in order to prevent or correct dental crowding in children. The two extraction patterns were: extraction of lower deciduous canines (Kau 2004) and extraction of wisdom teeth (Harradine 1998).
Extraction of lower deciduous canines
One study compared the extraction of lower deciduous canines against a control group that received no treatment during the study period in order to treat dental crowding in the mixed dentition (Kau 2004).
Extraction of wisdom teeth
One study compared extraction of wisdom teeth to a control group that received no treatment during the study period to prevent dental crowding from developing in later life (Harradine 1998).
Characteristics of the outcomes
Primary outcome
The primary outcome was crowding, measured in millimetres or by any index of malocclusion.
Twelve of the studies used Little’s Irregularity Index to assess crowding in the mandible (Aras 2018; Aydin 2018; Finland 2004; Harradine 1998; Kau 2004; Miles 2012; Myrlund 2015; Ong 2011; Pandis 2009; Sebastian 2012; Songra 2014; Woodhouse 2015), one study used a 3D irregularity index (Gravina 2013), one study reported on mandibular crowding in the lower labial segment by comparing the amount of available space to the mesio‐distal widths of the teeth in the lower labial segment (Irvine 2004), and two studies were not clear as to what method they used to measure crowding (Davidovitch 1997; Tai 2010). Five studies reported on maxillary crowding (Harradine 1998; Miles 2010; Myrlund 2015; O'Brien 1990; Pandis 2010a). All of the studies that reported crowding used millimetres and recorded crowding in the anterior region of the maxilla or mandible.
Nineteen different time points were recorded across these studies, which ranged from pre‐treatment records to one study with a 13‐year follow‐up (Finland 2004). These time points varied greatly, with some readings in days, some in weeks or months and a few in years.
For most interventions, there was only one study available, but for the comparison of vibrational appliances against a control, we combined data from two studies by converting the time points into weeks (Miles 2012; Woodhouse 2015). This was considered to be the most clinically relevant time descriptor for the reduction of irregularity and also a reliable unit, as the days in a month can vary.
Secondary outcomes
Upon data extraction, we decided that certain outcomes were of interest and clinically relevant. The data for these were extracted as an amendment to the original protocol and include upper incisors to maxilla, lower incisors to mandible, arch length, time to alignment and ligation time (Harrison 2002). Abbreviations used in these studies are outlined in Table 4.
1. Abbreviations and measures used to assess outcomes.
| 1. Relationship of the top front teeth (incisors) to the upper jaw (maxilla) | |
| U1‐CT (°) | Angle formed between the upper incisor axis and the CT horizontal plane |
| U1–Vp | Distance from the vertical plane to the upper incisor crown tip |
| U1–CT | Distance from the CT horizontal plane to the upper incisor crown tip |
| 2. Relationship of the top back teeth (molars) to the upper jaw (maxilla) | |
| U6–CT (°) | Angle formed between the upper first molar axis and the CT horizontal plane |
| U6d–Vp | Distance from the vertical plane to the upper first molar distal point |
| U6–CT | Distance from the CT horizontal plane to the upper first molar mesiobuccal crown tip |
A‐P: antero‐posterior; APog: A‐point to pogonion line; SN: sella‐nasion
Arch length
Seven studies reported this as the change in arch length but for differing comparisons, so it was not appropriate to combine the results (Davidovitch 1997; Finland 2004; Harradine 1998; Irvine 2004; Kau 2004; Rebellato 1997; Tai 2010). Changes occurring between the start and the end of the individual studies were measured.
Upper incisors to maxilla
Three studies reported on the position of the upper incisor position relative to the maxilla but for differing comparisons, so it was not appropriate to combine the results of these studies (Finland 2004; Myrlund 2015; Tai 2010). Two studies reported on the angle formed between the upper incisors and the line between sella and nasion (Myrlund 2015; Tai 2010). One study reported on the angle of the upper incisor to the maxillary plane (line between anterior and posterior nasal spines; Finland 2004).
Lower incisors to mandible
Six studies reported on the position of the lower incisor position relative to the mandible (Davidovitch 1997; Finland 2004; Kau 2004; Myrlund 2015; Rebellato 1997; Tai 2010), but each study investigated a different comparison and so it was not appropriate to combine the results.
Lower molars to mandible
Two studies reported on the relationship of the lower molars to the mandible and investigated two different comparisons: lip bumper (Davidovitch 1997), and lingual arch (Rebellato 1997), versus control. The studies measured the molar position in two different ways; molar inclinational change in degrees and molar anterior‐posterior movement change in millimetres. Rebellato 1997 measured angular change relative to the functional occlusal plane, which they described as a line drawn through maximum inter‐cuspation of the occlusion, whereas Davidovitch 1997 measured it relative to the mandibular plane, described as the line drawn between gnathion and pogonion.
Time to alignment
Eight studies reported on time to alignment of the teeth; two of which were for copper nickel‐titanium versus nickel‐titanium archwires ( Ong 2011; Pandis 2009), two were for self‐ligating brackets versus conventional brackets (Pandis 2011; Songra 2014), and two were for vibrational appliances compared to fixed appliances only (Miles 2016; Woodhouse 2015), so the results were combined. The other two studies compared different comparisons so it was not appropriate to combine the results (Pandis 2010a; Pandis 2011).
Ligation time
One study reported on the ligation time for the two different types of brackets investigated (Miles 2010).
Self‐esteem
No study reported on this outcome.
Patient satisfaction
No study reported on this outcome.
Jaw joint problems
No study reported on this outcome
Other outcomes
Harms
Six studies reported on the discomfort experienced for differing comparisons.
Two studies used a 7‐point Likert Scale (Miles 2010; Ong 2011), and four used a 100 millimetre visual analogue scale (VAS; Atik 2014; Miles 2012; Sandhu 2013; Woodhouse 2015).
One study reported on Plaque Index, Gingival Index and probing depths (Atik 2014).
One study reported on root resorption (Aras 2018).
Excluded studies
We excluded 61 studies from this review for the following reasons (see Characteristics of excluded studies).
15 were not RCTs
18 because participants were not primarily receiving treatment to prevent or correct dental crowding
25 did not fulfil the eligibility criteria for age
1 did not fulfil criteria for participant crowding
2 had insufficient information to allow inclusion of data
Risk of bias in included studies
We assessed 23 studies as being at high risk of bias and one study as being at an unclear risk of bias. We determined all but one study as being at a high risk of bias due to the nature of the interventions, meaning that the participants and personnel could not be blinded. See Figure 2 and Figure 3 for a graphical representation of our assessments.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We assessed 13 studies as being at low risk of selection bias because they described an adequate method of random sequence generation and allocation concealment based on information published in the papers and further information received via correspondence with the study authors when required (Aydin 2018; Finland 2004; Kau 2004; Miles 2016; Myrlund 2015; Ong 2011; Pandis 2009; Pandis 2010a; Pandis 2011; Sandhu 2013; Sebastian 2012; Songra 2014; Woodhouse 2015). Despite being at a low risk of selection bias, the two groups described by Kau 2004 had differences in the amount of baseline crowding. The remaining 11 studies did not mention any method used to conceal the random sequence or allocation, and we assessed them as being at unclear risk of selection bias; Tai 2010 also described a longer pre‐treatment arch length in the Schwarz appliance group compared to the control.
Blinding
Performance bias
One study described adequate methods of blinding of participants and personnel and we therefore assessed it as being a low risk of bias for this domain (Pandis 2009). We assessed the other 23 studies as being at high risk of performance bias as it was either not possible to blind participants or clinicians, or both, or the study did not mention having done so.
Detection bias
We assessed 12 studies as low risk of detection bias as assessors were blinded (Harradine 1998; Kau 2004; Miles 2010; Miles 2016; Myrlund 2015; Ong 2011; Pandis 2011; Sandhu 2013; Sebastian 2012; Songra 2014; Tai 2010; Woodhouse 2015). We assessed 10 studies as unclear because information about the blinding of assessors was not reported (Atik 2014; Aydin 2018; Davidovitch 1997; Finland 2004; Gravina 2013; Irvine 2004; O'Brien 1990; Pandis 2009; Pandis 2010a; Rebellato 1997). We also deemed an additional study as being at unclear risk of detection bias (Miles 2012); although the assessors were blinded when measuring crowding and measuring the VAS scores, the participants had not been blinded to the intervention when they were measuring their own discomfort. We deemed Aras 2018 at a high risk of bias as the assessor could not be blinded.
Incomplete outcome data
We assessed 15 studies as being at low risk of attrition bias as dropout was less than 20 per cent (Atik 2014; Aydin 2018; Irvine 2004; Kau 2004; Miles 2012; Miles 2016; Myrlund 2015; O'Brien 1990; Pandis 2009; Pandis 2010a; Pandis 2011; Sandhu 2013; Sebastian 2012; Songra 2014; Woodhouse 2015).
We considered two studies to be at high risk due to high level of attrition across the studies (Finland 2004; Harradine 1998). However, these studies had long follow‐up periods.
The remaining seven studies did not report on dropouts and so we assessed them as being at unclear risk (Aras 2018; Davidovitch 1997; Gravina 2013; Miles 2010; Ong 2011; Rebellato 1997; Tai 2010).
Selective reporting
We assessed one study as being at unclear risk of selective reporting bias as it did not state any specific outcomes in the methods section, though it did report on appropriate outcomes in the results (Tai 2010). O'Brien 1990 was also unclear as they did not report final contact point displacement. The other studies were at low risk of bias.
Other potential sources of bias
We assessed three studies as having a high risk of other sources of bias (Aydin 2018; Irvine 2004; Woodhouse 2015). For Irvine 2004, it was unclear who or how many examiners took the measurements and they did not report intra/inter‐rater reliability. For Woodhouse 2015, in the follow‐up study looking at the secondary outcome of root resorption, the study was under‐powered (20% to 30%). For Aydin 2018, the participants were treated in a single centre by one clinician so the results may not be generalisable. In addition, their sample size calculation was based on one of the secondary outcomes rather than the primary outcome. It is worth noting that two studies (Atik 2014; Sebastian 2012), had gender bias in their sampling, having recruited only female participants; this, however, is a source of diversity or applicability rather than bias.
We considered 11 studies to have unclear risk of bias for this domain. One was because there was a clear difference in the baseline crowding between the two groups of participants (Kau 2004). Another study had clear differences for the same outcome, measured by two different methods, in the same study (Davidovitch 1997). Harradine 1998 had an unclear risk of bias due to the recall rate and O'Brien 1990 and Gravina 2013 did not report a sample size calculation. Two studies (Pandis 2010a; Pandis 2011), were conducted in a single‐centre, private practice with a per protocol analysis. In one study, participants in the control group received a variety of interceptive procedures, which were active treatments but not received by all participants in the group, as prescribed in the protocol, whilst comparing against the main intervention (Finland 2004). Another study removed the results for two participants in order to balance the two groups for numbers (Miles 2010). Rebellato 1997 had no sample size calculation, no mention of source of participants, proportion of male and female participants, or allocation concealment. Sebastian 2012 based their sample size just on the pilot study data.
We did not consider the remaining 10 studies to have any other potential sources of bias and we therefore assessed them as being at low risk of bias for this domain.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings 1. Fixed appliances and auxiliaries to prevent or correct dental crowding in children.
| Fixed appliances and auxiliaries versus other treatment or no treatment to prevent or correct dental crowding in children | ||||||
|
Population: children or adolescents, or both (age ≤ 16 years) having treatment to prevent or correct dental crowding Settings: Australia, Brazil, Finland, India, Turkey, UK, USA Intervention: fixed appliances and auxiliaries (lip bumper, headgear, lower lingual arch, brackets, archwires, lacebacks, vibrational appliances) Comparison: control (brackets, archwires, fixed appliances only, minor interceptive procedures, no active treatment) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) |
Relative effect
(95% CI) |
Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Fixed appliances and auxiliaries | |||||
| Lower lip bumper ‐ lower lip bumper versus no active treatment (control) | ||||||
| Change in the amount of crowding at 6 months | Mean change −0.7 mm | Mean change −5.09 mm ± 0.97 mm | 34 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was less crowding in the lip bumper group (MD −4.39 mm, 95% CI −5.07 to −3.71). | |
| Headgear ‐ cervical pull headgear versus minor interceptive procedures (control) | ||||||
| Amount of crowding at 2 years | Mean change 2.45 mm | Mean change 2.78 mm ± 1.91 mm | 64 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the amount of crowding at 2 years (MD 0.33 mm (95% CI −0.60 to 1.26). There was also no difference at 13 years follow‐up of the remaining 34 participants (MD 0.26, 95% CI −1.35 to 1.87). |
|
| Lower lingual arch ‐ lower lingual arch versus no active treatment (control) | ||||||
| Amount of crowding | Not measured | |||||
| Brackets ‐ self‐ligating brackets versus conventional brackets | ||||||
| Amount of crowding at 10 weeks | Mean amount of crowding 2.7 mm | Mean amount of crowding was 0.40 mm less (0.93 mm less to 0.13 mm more) | 60 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the amount of crowding. | |
| Archwires ‐ coaxial nickel‐titanium archwire versus nickel‐titanium archwire | ||||||
| Amount of tooth movement at 12 weeks | Mean amount of tooth movement 3.1 mm | Mean amount of tooth movement was 6.77 mm more (5.55 mm to 7.99 mm more) | 24 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was more tooth movement with the coaxial nickel‐titanium archwire than the nickel‐titanium archwire. | |
| Archwires ‐ copper nickel‐titanium archwire versus nickel‐titanium archwire | ||||||
| Amount of crowding at 12 weeks | Mean amount of crowding 6.33 mm | Mean amount of crowding was 0.49 mm more (0.35 mm to 0.63 mm more) | 66 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was less residual crowding with the nickel‐titanium archwire than the copper‐nickel titanium archwire. | |
| Archwires ‐ Titanol versus Nitinol | ||||||
| Change in the amount of crowding up to 37 weeks | Mean change 1.42 mm ± 0.79 mm | Mean change 1.7 mm ± 1.15 mm | 40 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the change in the amount of crowding (MD −0.28 mm, 95% CI −0.89 to 0.33). | |
| Archwires ‐ nickel‐titanium archwire versus multistranded stainless steel archwire | ||||||
| Change in the amount of crowding at 8 weeks | Mean change −29.2 mm | Mean change −27.6 mm ± 26.5 mm | 25 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the overall change in the amount of crowding (MD 1.60 mm, 95% CI −22.16 to 25.36). | |
| Archwires ‐ nickel‐titanium archwire versus stainless steel archwire | ||||||
| Change in the amount of crowding at 8 weeks | Mean change −10.8 mm | Mean change −27.6 mm ± 26.5 mm | 24 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the overall change in the amount of crowding (MD 16.80 mm, 95% CI −42.79 to 9.19). | |
| Archwires ‐ multistranded stainless steel archwire versus stainless steel archwire | ||||||
| Change in the amount of crowding at 8 weeks | Mean change −10.8 mm | Mean change −29.2 mm ± 33.4 mm | 23 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the overall change in the amount of crowding (MD −18.40 mm, 95% CI −47.12 to 10.32). | |
| Lacebacks ‐ lacebacks and fixed appliances versus fixed appliances only (control) | ||||||
| Change in the amount of crowding at 6 months | Mean change −2.67 mm | Mean change −3.00 mm ± 8.94 mm | 62 (1) | ⊕⊝⊝⊝ Very lowa,b |
There was no difference between groups in the change in the amount of crowding (MD −0.33 mm, 95% CI −5.90 to 5.24). | |
| Vibrational appliances ‐ vibrational appliances with fixed appliances versus fixed appliances only (control) | ||||||
| Change in the amount of crowding at 10 to 30 weeks | Mean change −0.7 mm | Mean change ranged from 4.0 mm to 5.5 mm | 119 (2) | ⊕⊝⊝⊝ Very lowc,d |
There was no difference between groups in the change in the amount of crowding (MD 0.24, 95% CI −0.81 to 1.30). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; mm: millimetre | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level as study at high risk of bias. bDowngraded twice as only one small study reported on this. cDowngraded twice as both studies at high risk of bias. dDowngraded one level as studies were potentially underpowered.
Summary of findings 2. Removable appliances and auxiliaries to prevent or correct dental crowding in children.
| Removable appliances and auxiliaries to prevent or correct dental crowding in children | ||||||
|
Population: children or adolescents (age ≤ 16 years) having treatment to prevent or correct dental crowding Setting: Japan, Norway Intervention: removable appliances, e.g. Schwarz appliance Comparison: fixed appliances only, no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| Schwarz appliance ‐ Schwarz appliance versus no active treatment (control) | ||||||
| Change in the amount of crowding at 9 months (after 6 months treatment) | Mean change −0.66 mm | Mean change −2.80 mm ± 1.14 mm |
28 (1) | ⊕⊝⊝⊝ Very lowa,b |
Use of a Schwarz appliance reduced crowding (MD −2.14, 95% CI −2.79 to −1.49). | |
| Eruption guidance appliance (EGA) ‐ EGA versus no active treatment (control) | ||||||
| Number of children with crowding after 1 year | 14 out of 22 children | 6 out of 24 children | OR 0.19 (95% CI 0.05 to 0.68) | 46 (1) | ⊕⊝⊝⊝ Very lowa,b |
Use of an EGA reduced the number of children with dental crowding after a year. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval;MD: mean difference; mm: millimetre; OR: odds ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded as study at high risk of bias. bDowngraded twice as only one small study reported on this.
Summary of findings 3. Extractions to prevent or correct dental crowding in children.
| Extractions to prevent or correct dental crowding in children | ||||||
|
Population: children or adolescents (age ≤ 16 years) having treatment to prevent or correct dental crowding Settings: Italy, Germany, Wales, UK Intervention: extraction of wisdom teeth or deciduous canines Comparison: no active treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| Extraction of wisdom teeth ‐ extraction of wisdom teeth versus no active treatment (control) | ||||||
| Change in the amount of crowding at 5 years | Mean change 1.1 mm | Mean change 0.8 mm ± 1.23 mm | 77(1) | ⊕⊝⊝⊝ Very low a,b |
There was no difference between extracting wisdom teeth and not extracting them in terms of the mean change in the amount of crowding (MD −0.30 mm (95% CI −1.30 to 0.70). | |
| Extraction of deciduous canines ‐ extraction of deciduous canines versus no active treatment (control) | ||||||
| Change in the amount of crowding at 1‐2 years | Mean change −1.27 mm | Mean change −6.03 mm ± 4.44 mm | 83(1) | ⊕⊝⊝⊝ Very low a,b |
There was a greater change in the amount of crowding when lower canines were extracted compared to when they were not (MD −4.76 mm (95% CI −6.24 to −3.28). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; mm: millimetre | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level as study at high both studies were at unclear risk of bias. bDowngraded as only one small study reported on this.
See Table 1 Fixed appliances and auxiliaries versus other treatment or no treatment to prevent or correct dental crowding in children; Table 2 Removable appliances and auxiliaries to prevent or correct dental crowding in children; Table 3 Extractions to prevent or correct dental crowding in children.
Fixed appliances and auxiliaries
Comparison 1: Lower lip bumper versus no active treatment (control)
We assessed Davidovitch 1997 as being at overall high risk of bias as it was not possible to blind personnel and participants.
Crowding
Davidovitch 1997 investigated change in mandibular incisor crowding, in millimetres, for a six‐month follow‐up period. They measured crowding at baseline and six months into treatment. In total, data from 34 participants were used for this outcome.
There was evidence of a greater reduction in lower incisor crowding of 4.39 mm in the lip bumper group, when compared to the control group, at six months (95% CI −5.07 to −3.71; P < 0.001; Analysis 1.1).
1.1. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 1: Change in mandibular crowding
Arch length
Davidovitch 1997 investigated arch length change in the mandible, in millimetres, up to a six‐month follow‐up period. They measured crowding at baseline and six months into treatment. In total, data from 34 participants were used for this outcome.
There was evidence of a greater increase in arch length of 3.34 mm in the lip bumper group (95% CI 2.71 to 3.97, P < 0.001) when compared with the control group, at six months (Analysis 1.2).
1.2. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 2: Change in arch length
Lower incisors to mandible
Davidovitch 1997 reported on the relationship on the lower incisors to the mandible, in degrees to the mandibular plane and in millimetres to A‐Pogonion, for up to a six‐month follow‐up period. In total, data from 34 participants were used for this outcome.
There was less labial movement of the lower incisors (0.49 mm) between baseline and six months, in the control group (95% CI 0.09 to 0.89; Analysis 1.3).
1.3. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 3: Change in mandibular incisor A‐P position
The lower incisors proclined 3.14 degrees more in the lip bumper group than the control (95% CI 1.73 to 4.55; Analysis 1.4).
1.4. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 4: Change in mandibular incisor inclination
Lower molars to mandible
Davidovitch 1997 reported on the lower molar to the mandibular plane, in degrees and in millimetres, for up to a six‐month follow‐up period. In total, data from 34 participants were used for this outcome.
The lower molar moved distally by 0.61 mm in the lip bumper group, compared to a 0.3 mm mesial movement in the control group. This difference of 0.91 mm (95% CI −1.58 to −0.24) favoured the lip bumper group (Analysis 1.5).
1.5. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 5: Change in mandibular molar A‐P position
The lower molars tipped distally by 3.38 degrees in the lip bumper group, compared to 0.75 degrees of mesial tipping in the control group. This difference of 4.13 degrees (95% CI −6.09 to −2.17) favoured the lip bumper group (Analysis 1.6).
1.6. Analysis.

Comparison 1: Lower lip bumper versus no active treatment (control), Outcome 6: Change in mandibular molar inclination
Harms
No harms were reported.
Other outcomes
Time to alignment and ligation time were not relevant for this comparison.
Upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 2: Cervical pull headgear versus minor interceptive procedures (control)
We assessed Finland 2004 as being at overall high risk of performance and attrition bias.
Crowding
Finland 2004 investigated lower incisor crowding, in millimetres, measured at baseline, two, four, eight and 13 years post‐treatment. At the one‐year recall, only 53 per cent of participants were included, meaning that there was high attrition bias. In total, 64 participants began the study and their data were used for this outcome for up to four years; 54 participants provided data for the eight‐year recall; but only 34 returned for the final recall at 13 years. There was no baseline imbalance in the characteristics of participants in each group.
The study found no evidence of a difference in the amount of lower incisor crowding between the two groups at any time point or comparing the change in crowding from baseline (Analysis 2.1; Analysis 2.4)
2.1. Analysis.

Comparison 2: Cervical pull headgear versus minor interceptive procedures (control), Outcome 1: Mandibular incisor crowding (pre‐treatment, 2 years, 4 years, 8 years, 13 years)
2.4. Analysis.

Comparison 2: Cervical pull headgear versus minor interceptive procedures (control), Outcome 4: Change in lower incisor to mandibular plane (0‐1 years and 0‐2 years)
Arch length
Finland 2004 reported on maxillary and mandibular arch length change, in millimetres, over an eight‐year period. Arch length was measured at baseline, two years and eight years and the changes occurring between these time points and baseline were reported.
For maxillary arch length, between baseline and the two‐year recall, arch length increased more in the headgear group (MD 1.98 mm) compared to the control group (95% CI 1.80 to 2.16: P < 0.00001). At the eight‐year recall, the results still favoured the headgear group (MD 2.28 mm, 95% CI 2.05 to 2.15mm; P < 0.001; Analysis 2.2).
2.2. Analysis.

Comparison 2: Cervical pull headgear versus minor interceptive procedures (control), Outcome 2: Change in maxillary arch length
For mandibular arch length, between baseline and the two‐year recall, arch length increased more in the headgear group compared to the control group (MD 1.3 mm, 95% CI 1.17 to 1.43 mm; P < 0.001), and was greater at 8 years (MD 1.52 mm) compared to the control group (95% CI 1.3 to 1.74; P < 0.001; Analysis 2.3).
2.3. Analysis.

Comparison 2: Cervical pull headgear versus minor interceptive procedures (control), Outcome 3: Change in mandibular arch length
Lower incisors to mandible
Finland 2004 reported on the lower incisor inclination, in degrees, over a two‐year period. The time points at which the change in lower incisor inclination was measured were baseline, baseline to one year and baseline to two years. In total, 64 participants were included in the analysis.
The characteristics of participants in the headgear and control groups were balanced at baseline with no evidence of a difference between the proclination of the lower incisors (P = 0.47). There was more proclination of the lower incisors (MD 2.3 degrees) in the headgear group compared to the control group at one year (95% CI 0.67 to 3.93; P = 0.006); however, at two years, this difference was lost (MD 1.4 degrees, 95% CI ‐0.42 to 3.22; P = 0.13; Analysis 2.4).
Upper incisors to maxilla
Finland 2004 reported on the upper incisor inclination, in degrees, over a two‐year period. The time points at which the upper incisor change was measured were baseline to one year and baseline to two years. In total, 64 participants were included in the analysis.
The groups were balanced at baseline with no evidence of a difference between their upper incisor inclination (P = 0.10).
Between baseline and one year, there was more proclination of the upper incisors in the headgear group compared to the control group (MD 4 degrees, 95% CI 1.97 to 6.03; P = 0.01). This difference was maintained at two years (MD 4.5 degrees, 95% CI 1.36 to 7.64; P < 0.001; Analysis 2.5).
2.5. Analysis.

Comparison 2: Cervical pull headgear versus minor interceptive procedures (control), Outcome 5: Change in upper incisor to maxillary plane
Harms
No harms were reported.
Other outcomes
The study did not measure the relationship of the lower molars to mandible, self‐esteem, participant satisfaction or jaw joint problems.
Time to alignment and ligation time were irrelevant for this comparison.
Comparison 3: Lower lingual arch versus no active treatment (control)
We assessed Rebellato 1997 as being at overall high risk of bias as it was not possible to blind personnel and participants; the method of randomisation was also unclear.
Crowding
This outcome was not reported.
Arch length
Rebellato 1997 investigated arch length change in the mandible, in millimetres, up to a one‐year follow‐up period. Crowding was measured at baseline and at 10 to 12 months post‐treatment. In total, data from 30 participants were used for this outcome.
The arch length increased more in the lower lingual arch appliance (LLA) group (MD 2.61 mm; 95% CI 1.83 to 3.39; P < 0.001; Analysis 3.1).
3.1. Analysis.

Comparison 3: Lower lingual arch versus no active treatment (control), Outcome 1: Change in mandibular arch length
Lower incisors to mandible
Rebellato 1997 reported on the lower incisors to the mandibular plane, in degrees and in millimetres, for up to a one‐year follow‐up period.
The lower incisors moved mesially by 0.32 mm in the LLA group, compared to a 0.34 mm distal movement in the control group, a clear difference of 0.66 mm (95% CI 0.46 to 0.86, P < 0.001; Analysis 3.2).
3.2. Analysis.

Comparison 3: Lower lingual arch versus no active treatment (control), Outcome 2: Change in mandibular incisor A‐P position
The lower incisors proclined by 0.73 degrees in the LLA group, compared to 2.28 degrees of retroclination in the control group and this difference of 3.01 degrees was clearly different (95% CI 1.71 to 4.31, P < 0.001; Analysis 3.3).
3.3. Analysis.

Comparison 3: Lower lingual arch versus no active treatment (control), Outcome 3: Change in mandibular incisor inclination
Lower molars to mandible
Rebellato 1997 reported on the lower molar to the mandibular plane, in degrees and in millimetres, for up to a one‐year follow‐up period.
The lower molar moved mesially by 0.33 mm in the LLA, compared to 1.44 mm in the control group and this difference of −1.11 mm was clearly different (95% CI −1.51 to −0.71, P < 0.001; Analysis 3.4).
3.4. Analysis.

Comparison 3: Lower lingual arch versus no active treatment (control), Outcome 4: Change in mandibular molar A‐P position
The lower molars tipped distally by 0.54 degrees in the LLA, compared to 2.19 degrees of mesial tipping in the control group and this difference of −2.73 degrees was clearly different (95% CI −4.29 to −1.17, P < 0.001; Analysis 3.5 ).
3.5. Analysis.

Comparison 3: Lower lingual arch versus no active treatment (control), Outcome 5: Change in mandibular molar inclination
Harms
No harms were reported.
Other outcomes
Time to alignment and ligation time were not relevant for this comparison.
Upper incisors to maxilla, harms, self‐esteem and participant satisfaction were not reported.
Comparison 4: Self‐ligating brackets versus conventional brackets
Five studies assessed this comparison, all of which we assessed as being at high risk of bias (Aras 2018; Atik 2014; Miles 2010; Pandis 2011; Songra 2014).
Crowding
One study investigated incisor crowding in the anterior maxilla, in millimetres, for a 10‐week period (Miles 2010). Crowding was measured at baseline and 10 weeks into treatment. We assessed this study as being at overall high risk of bias as although blinding of participants was carried out, blinding of personnel was not possible due to the type of intervention. The study states that participants were randomly allocated but no further details on the methods used were given. Additionally, there were dropouts in the conventional ligation group, so analysis was not performed on two of the self‐ligating group participants. In total, 68 participants provided baseline information and 60 (88.2%) were analysed at follow‐up.
There was no evidence of baseline imbalance between the groups with regards to the pre‐treatment degree of crowding (MD ‐0.17 mm, 95% CI ‐1.49 to 1.15; P = 0.8; Analysis 4.1).
4.1. Analysis.

Comparison 4: Self‐ligating brackets versus conventional brackets, Outcome 1: Maxillary incisor crowding (pre‐treatment and 10 weeks)
There was no evidence of a difference in lower incisor crowding between the self‐ligating and conventional groups at 10 weeks (MD −0.40 mm, 95% CI −0.93 to 0.13; P = 0.14; Analysis 4.1).
Time to alignment
Two studies reported on time to alignment, in days (Pandis 2011; Songra 2014). The time points reported were the mean number of days it took for alignment in each group. Alignment is described as the point at which a rectangular (0.019 inch x 0.025 inch) copper nickel‐titanium (Pandis 2011), or stainless steel (Songra 2014), archwire could be placed passively. The studies were considered to be at a high overall level of bias as it was not possible to blind participants and personnel as to which bracket type each participant received. In total, data from 148 participants were used for this outcome.
There was no evidence of a difference in time to alignment between the groups (MD 89.64 days; 95% CI −45.89 to 225.17; P = 0.19; Analysis 4.2). However, there was definite heterogeneity (I2 = 94%) in the treatment effect, which can be explained by the difference in the point at which alignment was assessed.
4.2. Analysis.

Comparison 4: Self‐ligating brackets versus conventional brackets, Outcome 2: Time to alignment
Ligation time
One study reported on the time to tie, ligate and untie six brackets, in seconds (Miles 2010). This study was assessed as being at overall unclear risk of bias, as the methods of randomisation and allocation concealment were not described; the participants were blinded but the clinicians were not; and not all the participants who completed the study were analysed, in order to keep the groups equal in size at the follow‐up. In total, data from 68 participants were used for the outcome of the time taken to untie, and data from 60 participants were used for the outcome of the time taken to ligate six brackets.
Untying was quicker (MD −22.3 seconds) in the self‐ligating group (95% CI −25.83 to −18.77, P < 0.001; Analysis 4.3).
4.3. Analysis.

Comparison 4: Self‐ligating brackets versus conventional brackets, Outcome 3: Ligation time
Ligation was quicker (MD −78.8 seconds) in the self‐ligating group (95% CI −81.86 to −75.74, P < 0.001; Analysis 4.3).
Lower incisors to mandible
Atik 2014 reported on the lower incisors to the mandibular plane, in degrees until the stage of treatment when a 0.019” x 0.025” stainless steel archwire was placed. We assessed Atik 2014 as being at overall high risk of bias as neither the participants nor the clinicians were blinded and the entire sample consisted of female participants. A total of 33 participants' data were used for the outcome of lower incisor inclination.
There was no evidence of baseline imbalance in lower incisor inclination despite there being 3.38 degrees less proclination in the conventional bracket group (95% CI −0.04 to 6.80; P = 0.05).
Post‐treatment, the change in lower incisor inclination in the conventional bracket group was 1.29 degrees less than the self‐ligating group, but no clear difference between the groups was seen (95% CI −1.77 to 4.35; P = 0.41; Analysis 4.4).
4.4. Analysis.

Comparison 4: Self‐ligating brackets versus conventional brackets, Outcome 4: Change in lower incisor to mandibular plane
Harms
Atik 2014 and Miles 2010 reported on discomfort. Atik 2014 reported on plaque index, gingival index and probing depth. Aras 2018 reported on root resorption of the maxillary incisors.
Atik 2014 described discomfort using a 100 mm VAS over the first month. The participants were asked to keep a diary and record discomfort in the maxilla and mandible at 4 hours, 24 hours, 3 days, 1 week, and 1 month using the terms “very comfortable” and “very uncomfortable” at the ends of the scale. No evidence of a difference in discomfort scores between self‐ligating and conventional brackets, was found.
Miles 2010 described discomfort using a 7‐point Likert scale for the first week. The participants were given a questionnaire and asked to record discomfort in the upper arch at 4 hours, 24 hours, 3 days and 1 week. Again, no evidence of a difference for discomfort scores between self‐ligating and conventional brackets, was found.
Atik 2014 described the periodontal and gingival health of all 24 maxillary and mandibular teeth and estimated the mean value per participant. They did not find evidence of differences in any of the scores between self‐ligating and conventional brackets, from the baseline measurement to the end of the study.
Aras 2018 measured the amount of root resorption of the maxillary incisors using cone beam computed tomography (CBCT) scans for 32 participants before treatment and nine months into treatment. There was no evidence of differences in root resorption between self‐ligating and conventional brackets.
Other outcomes
Lower molars to mandible, upper incisors to maxilla, arch length, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 5: Active versus passive self‐ligating brackets
Two studies assessed this outcome (Pandis 2010a; Songra 2014), and we considered both as being at overall high risk of bias because it was not possible to blind personnel and participants. However, in Pandis 2010a, there was evidence of a difference between groups, in the amount of baseline crowding.
Crowding
Pandis 2010a investigated baseline upper anterior crowding in millimetres. In total, data from 70 participants were used for this outcome.
There was evidence of a difference in crowding at baseline between the two bracket groups (P = 0.04), putting the study at a high risk of bias.
Time to alignment
Both studies (Pandis 2010a; Songra 2014), reported on this outcome. Pandis 2010a considered alignment complete when the maxillary incisors were visually regarded as aligned whereas for Songra 2014, it was when a rectangular (0.019 inch x 0.025 inch) stainless steel archwire could be placed passively. In total, 144 participants completed the study and their data were used for this outcome.
There was no evidence of a difference in the time to alignment between the two bracket groups (MD −13.11 days, 95% CI −28.76 to 2.53; P = 0.10; Analysis 5.2).
5.2. Analysis.

Comparison 5: Active self‐ligating brackets versus passive self‐ligating brackets, Outcome 2: Time to alignment
Harms
No harms were reported.
Other outcomes
Ligation time, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, patient satisfaction and jaw joint problems were not reported.
Comparison 6: Copper nickel‐titanium versus nickel‐titanium archwires
Three studies assessed this comparison (Aydin 2018; Ong 2011; Pandis 2009). We assessed Aydin 2018 and Ong 2011 as being at high risk of bias and Pandis 2009 as being at an unclear risk of bias overall.
Crowding
All three studies reported baseline mandibular anterior crowding in millimetres. We combined them in a meta‐analysis and found no difference in baseline crowding between the groups (MD −0.34 mm, 95% CI −1.27 to 0.58; P = 0.47; 254 participants; Analysis 6.1).
6.1. Analysis.

Comparison 6: Copper nickel‐titanium versus nickel‐titanium archwires, Outcome 1: Mandibular incisor crowding (pre‐treatment)
Aydin 2018 reported Little's Irregularity Index in millimetres at 2, 4, 6, 8, 10 and 12 weeks. Data after 12 weeks' treatment are reported and showed evidence of a difference favouring nickel‐titanium (NiTi )(MD 0.49 mm, 95% CI 0.35 to 0.63; P < 0.00001; Analysis 6.2).
6.2. Analysis.

Comparison 6: Copper nickel‐titanium versus nickel‐titanium archwires, Outcome 2: Little's Irregularity Index at 12‐weeks
Time to alignment
We combined two studies in a meta‐analysis to assess time to alignment in days (Ong 2011; Pandis 2009). Data from 191 participants were analysed and revealed that overall, there was no evidence of a difference in time to alignment based on either the copper NiTi or NiTi archwire sequence (MD −2.63 days, 95% CI −14.50 to 9.24; P = 0.66; Analysis 6.3).
6.3. Analysis.

Comparison 6: Copper nickel‐titanium versus nickel‐titanium archwires, Outcome 3: Time to alignment
Harms
One study investigated the discomfort experienced on a 7‐point Likert scale (Ong 2011). The participants were given a questionnaire and asked to record discomfort in the upper arch at four hours, 24 hours, three days and one week after each archwire was changed. There was no evidence of a difference in the overall discomfort levels between the copper NiTi and NiTi archwire sequences.
Other outcomes
Ligation time was not relevant to this comparison. Arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 7: Coaxial nickel‐titanium versus nickel‐titanium archwires
We assessed Sebastian 2012 as being at overall high risk of bias as they did not carry out blinding of personnel and participants; in addition, the sample consisted of female participants only.
Crowding
One study investigated lower anterior crowding in millimetres for up to eight weeks (Sebastian 2012). The time points at which reduction in crowding, or tooth movement was reported were 4, 8 and 12 weeks. In total, data from 24 participants were used for this outcome.
There was baseline equivalence in crowding between coaxial nickel‐titanium (NiTi) and NiTi groups (MD 0.10 mm, 95% CI −1.14 to 1.34; P = 0.87).
More tooth movement, or reduction in crowding, was found in the coaxial NiTi group compared to the NiTi group at 4, 8 and 12 weeks. The greatest difference was seen at 12 weeks (MD 6.77mm, 95% CI 5.55 to 7.99; P < 0.001; Analysis 7.2), with the difference having clearly increased over time from 4 to 12 weeks (P < 0.001).
7.2. Analysis.

Comparison 7: Coaxial nickel‐titanium versus nickel‐titanium archwires, Outcome 2: Total amount of tooth movement
Harms
No harms were reported.
Other outcomes
Ligation time was not relevant to this comparison. Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 8: Nitinol versus titinol archwires
We assessed O'Brien 1990 as being at overall high risk of bias as they did not report blinding of personnel and participants.
Crowding
O'Brien 1990 investigated baseline upper anterior crowding in millimetres for up to 37 days. In total, data from 40 participants were used for this outcome.
There was baseline equivalence in the amount of crowding between nitinol and titinol groups (MD 3.31 mm, 95% CI −0.73 to 7.35; P = 0.11).
There was no evidence of a difference in the change in crowding between the nitinol and titinol groups (MD −0.28 mm, 95% CI −0.89 to 0.33; P = 0.37; Analysis 8.1).
8.1. Analysis.

Comparison 8: Titanol versus nitinol archwires, Outcome 1: Change in maxillary incisor crowding
Harms
No harms were reported.
Other outcomes
Ligation time was not relevant to this comparison. Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 9: Nickel‐titanium versus multistranded stainless steel archwires
We deemed both Gravina 2013 and Sandhu 2013 at high risk of bias as they did not report blinding of participants and personnel. Gravina 2013 was also potentially under‐powered.
Crowding
Gravina 2013 investigated the change in mandibular crowding in millimetres from baseline to eight weeks. In total, data from 25 participants were used for this outcome. They found that there was no difference between the two archwires (MD 1.60, 95% CI −22.16 to 25.36; P = 0.90).
Harms
Sandhu 2013 reported on pain perception during the initial levelling and aligning phase of orthodontic treatment between nickel titanium archwires and multistranded stainless steel archwires. They found no evidence of a difference for overall pain. However, participants did definately experienced more pain with nickel titanium archwires at 12 hours and during day 1 in the morning, afternoon and at bedtime, when compared to those with the multistranded stainless steel archwires.
Other outcomes
Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw‐joint problems were not reported. Ligation time was not relevant to this comparison.
Comparison 10: Nickel‐titanium versus stainless steel archwires
We deemed Gravina 2013 at a high risk of bias as they did not report blinding of participants and personnel. The study was also potentially underpowered.
Crowding
Gravina 2013 investigated the change in mandibular crowding in millimetres from baseline to eight weeks. In total, data from 24 participants were used for this outcome. They found that there was no difference between the two archwires (MD −16.80, 95% CI −42.79 to 9.19; P = 0.21).
Harms
No study in this subgroup presented data in a way that facilitated assessment of this outcome.
Other outcomes
Ligation time was not relevant to this comparison. Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 11: Multistranded stainless steel versus stainless steel archwires
We deemed Gravina 2013 at a high risk of bias as they did not report blinding of participants and personnel. The study was also potentially underpowered.
Crowding
Gravina 2013 investigated the change in mandibular crowding in millimetres from baseline to eight weeks. In total, data from 23 participants were used for this outcome. They found that there was no difference between the two archwires (MD −18.40, 95% CI −47.12 to 10.32; P = 0.21).
Harms
No study in this subgroup presented data in a way that facilitated assessment of this outcome.
Other outcomes
Ligation time was not relevant to this comparison. Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 12: Lacebacks with fixed appliances versus fixed appliances only (control)
We assessed Irvine 2004 as being at high risk of bias.
Crowding
Irvine 2004 reported the amount of lower labial segment crowding at the time when the fixed appliances were placed and when sufficient levelling had taken place with a 0.018" stainless steel archwire. This was done by comparing the amount of available space and the combined mesio‐distal widths of the teeth. In total, data from 62 participants were analysed.
No evidence of baseline imbalance between the two groups was reported. There were no differences in the mean change in the amount of crowding between the fixed appliance only and the fixed appliance with lacebacks groups, at six months (MD −0.33 mm, 95% CI −5.90 to 5.24; P = 0.91; Analysis 12.1).
12.1. Analysis.

Comparison 12: Lacebacks with fixed appliances versus fixed appliances only (control), Outcome 1: Change in mandibular incisor crowding
Arch length
Irvine 2004 also reported on the change in arch length between the two groups. They measured this bilaterally as a straight line between the marginal ridge of the lower first molar and the mesio‐incisal edge of the most prominent central incisor and added the two values together.
There was no evidence of a difference in the arch length between the fixed appliance only and the fixed appliance with lacebacks groups (MD 0.83 mm, 95% CI −6.41 to 8.07; P = 0.82; Analysis 12.2).
12.2. Analysis.

Comparison 12: Lacebacks with fixed appliances versus fixed appliances only (control), Outcome 2: Change in mandibular arch length
Harms
No harms were reported.
Other outcomes
Time to alignment, ligation time, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw‐joint problems were not reported.
Comparison 13: Vibrational appliance versus no vibrational appliance (control)
Crowding
Three studies investigated mandibular anterior crowding in millimetres and but we combined only two of them in a meta‐analysis (Miles 2012; Woodhouse 2015). We assessed Miles 2016 as being at overall high risk of bias and we were unable to obtain appropriate data for this outcome. Woodhouse 2015 was also at a high risk of bias, mainly as they did not blind the clinicians and participants to the intervention, and Miles 2012 was at a high risk of bias as they could not blind participants and they reported on discomfort using a 100 mm VAS. In total, data from 119 participants were used for the outcome of the change in crowding. There was no evidence of baseline imbalance in irregularity between the two groups in each study and between the studies (P = 0.7; Analysis 13.1).
13.1. Analysis.

Comparison 13: Vibrational appliances with fixed appliances versus fixed appliances only (control), Outcome 1: Mandibular incisor crowding (pre‐treatment and after initial alignment)
Overall, there was no evidence of a difference in the change in crowding in either group as reported in Miles 2012 and Woodhouse 2015 (MD 0.24, 95% CI −0.81 to 1.30; P = 0.65). There was no heterogeneity (I2= 0%; Analysis 13.2).
13.2. Analysis.

Comparison 13: Vibrational appliances with fixed appliances versus fixed appliances only (control), Outcome 2: Change in mandibular incisor crowding
Time to alignment
We combined results from Miles 2016 and Woodhouse 2015 in a meta‐analysis that showed that there was no evidence of a difference between the two groups for the time to alignment (MD −3.70, 95% CI −26.29 to 18.89; P = 0.75). There was no heterogeneity (I2 = 0%; Analysis 13.3).
13.3. Analysis.

Comparison 13: Vibrational appliances with fixed appliances versus fixed appliances only (control), Outcome 3: Time to alignment
Harms
Two studies reported on discomfort using a 100 mm VAS over the first week (Miles 2012; Miles 2016). The participants were asked to keep a diary and record discomfort at four time points: bond‐up, six to eight hours after appliance placement, one day after, three days after and seven days after at the appliances were placed. There was no clear difference in discomfort scores between those participants in the vibrational appliance and those in the control groups.
Woodhouse 2015 reported pain intensity using a 100 mm VAS over the first week following insertion of fixed appliances, as well as analgesia consumption. Recordings were taken at bond‐up, four hours, 24 hours, 72 hours and at one week. The use of a vibrational appliance made no clear difference in the pain intensity experienced by the participants or the amount of analgesics they took.
Root resorption
Woodhouse 2015 also reported orthodontically‐induced inflammatory root resorption by taking a long‐cone periapical radiograph of the upper right central incisor for 81 participants at the start of treatment and at the end of alignment when a 0.019 x 0.025‐inch stainless steel archwire was placed. For the 72 participants included in the analysis, the study found that using a vibrational appliance did not affect the amount of root resorption when compared to the control.
Other outcomes
Time to alignment, arch length, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw‐joint problems were not reported. Ligation time was not relevant to this comparison.
Removable appliances and auxiliaries
Comparison 14: Schwarz appliance versus no active treatment (control)
We assessed Tai 2010 as being at overall high risk of bias as it was not possible to blind personnel and participants.
Crowding
Tai 2010 investigated lower arch crowding, in millimetres, over a nine‐month post‐treatment follow‐up period. Time‐points measured were baseline and nine months after expansion of the arches with a Schwarz appliance for six months. In total, 28 participants were included in this study.
There was no evidence of baseline imbalance in the degree of crowding between the Schwarz appliance and control groups (P = 0.48).
There was more reduction in lower arch crowding (MD −2.14 mm) in the Schwarz appliance group at the nine‐month follow‐up (95% CI −2.79 to −1.49, P < 0.00001; Analysis 14.1).
14.1. Analysis.

Comparison 14: Schwarz appliance versus no active treatment (control), Outcome 1: Change in mandibular incisor crowding
Arch length
Tai 2010 reported mandibular arch length, in millimetres, as reported above. Twenty‐eight participants were included in this analysis.
There was evidence of imbalance in baseline arch length (MD 1.86 mm) with the Schwarz appliance group having a longer pre‐treatment arch length than the control group (95% CI 0.23 to 3.49; P = 0.03).
There was no evidence of a difference in the change in arch length (MD 0.11 mm) between baseline and the nine‐month follow‐up between the Schwarz appliance group and the control (95% CI −0.46 to 0.68; P = 0.71; Analysis 14.2).
14.2. Analysis.

Comparison 14: Schwarz appliance versus no active treatment (control), Outcome 2: Change in mandibular arch length
Lower incisors to mandible
Tai 2010 reported on lower incisor position, in millimetres. The time points at which lower incisor position was measured are as above. In total, 28 participants were included in the analysis.
There was no evidence of baseline imbalance in the lower incisor position of the groups (P = 0.89).
There was evidence of a difference in the change in lower incisor position relative to the mandible (MD 0.39 mm; 95% CI 0.11 to 0.67; P = 0.006) with the lower incisors being more advanced in the Schwarz appliance group (Analysis 14.3).
14.3. Analysis.

Comparison 14: Schwarz appliance versus no active treatment (control), Outcome 3: Change in lower incisor to APog
Upper incisors to maxilla
Tai 2010 reported on upper incisor position, in degrees. The time points and risk of bias have been discussed earlier. In total, 28 participants were included in the analysis.
There was no evidence of baseline imbalance, between the groups, in the incisor inclination (P = 0.94).
There was no evidence of a difference between the Schwarz appliance group and the control group in the change in upper incisor inclination at the nine‐month follow‐up (MD 0.33 degrees, 95% CI −2.26 to 2.92; P = 0.8; Analysis 14.4).
14.4. Analysis.

Comparison 14: Schwarz appliance versus no active treatment (control), Outcome 4: Change in upper incisor to SN
Harms
No harms were reported.
Other outcomes
Time to alignment and ligation time were not relevant for this comparison.
Lower molars to mandible, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 15: Eruption guidance appliance versus no active treatment (control)
We assessed Myrlund 2015 as being at overall high risk of bias as it was not possible to blind personnel and participants.
Crowding
Myrlund 2015 investigated incisor crowding in the maxilla and the mandible, in millimetres, for a one‐year follow‐up period. They measured crowding at baseline and one‐year post‐treatment. In total, 46 participants began the study and their data were used for this outcome.
There was no evidence of baseline imbalance in crowding between the eruption guidance appliance (EGA) and the control groups for maxillary (upper) and mandibular (lower) anterior crowding (P = 0.15 in maxilla; P = 0.26 in mandible).
In the maxilla, there was no evidence of a difference in the number of children with crowding between the EGA and control groups at one‐year post‐treatment (OR 0.82 mm, 95% CI 0.25 to 2.63; P = 0.74; Analysis 15.1).
15.1. Analysis.

Comparison 15: Eruption guidance appliance versus no active treatment (control), Outcome 1: Maxillary incisor crowding (pre‐treatment and 1 year)
In the mandible, there were fewer children with crowding in the EGA group than the control group at one‐year post‐treatment (OR 0.19, 95% CI 0.05 to 0.68; P = 0.01; Analysis 15.2).
15.2. Analysis.

Comparison 15: Eruption guidance appliance versus no active treatment (control), Outcome 2: Mandibular incisor crowding (pre‐treatment and 1 year)
Lower incisors to mandible
Myrlund 2015 reported on lower incisor inclination to the mandible, in degrees, for a one‐year follow‐up in the EGA group. No data for the control group were reported for the one‐year post‐treatment follow‐up.
Upper incisors to maxilla
Myrlund 2015 reported on upper incisor inclination to the maxilla, in degrees, for a one‐year follow‐up in the EGA group. No data for the control group were reported for the one‐year post‐treatment follow‐up.
Harms
No harms were reported.
Other outcomes
Ligation time was not relevant. Arch length, lower molars to mandible, self‐esteem, participant satisfaction, jaw joint problems, and time to alignment were not reported.
Extractions
Comparison 16: Extraction of lower deciduous canines versus no active treatment (control)
We assessed Kau 2004 as being at overall high risk of bias as it was not possible to blind the assessors and there was a definate difference in the amount of dental crowding at baseline.
Crowding
Kau 2004 investigated lower incisor crowding in millimetres at baseline and one to two years post‐treatment. In total, 97 participants began the study and their data were used for the outcome of crowding at baseline, and 85 (85.6%) participants attended the recall appointment.
At baseline, there was evidence of less lower incisor crowding (1.8 mm) in the non‐extraction group (95% CI 0.39 to 3.21; P = 0.01).
The reduction in lower incisor crowding in the extraction group, between baseline and 1 to 2 years post‐treatment, was greater than in the control group (MD −4.76 mm, 95% CI −6.24 to −3.28; P = 0.00001; Analysis 16.1).
16.1. Analysis.

Comparison 16: Extraction lower deciduous canines versus no active treatment (control), Outcome 1: Change in mandibular incisor crowding
Arch length
Kau 2004 reported on arch length, in mm, at one to two years post‐treatment. The change in arch length was measured at baseline and one year post‐treatment. In total, data from 97 participants were used for the outcome of arch length at baseline and 83 participants presented at the one‐year recall.
There was a greater reduction in arch length in the extraction group compared to the non‐extraction group (MD −2.73 mm, 95% CI −3.69 to −1.77, P < 0.001; Analysis 16.2).
16.2. Analysis.

Comparison 16: Extraction lower deciduous canines versus no active treatment (control), Outcome 2: Change in mandibular arch length
Lower incisors to mandible
Kau 2004 reported on lower incisor inclination, in degrees, for up to one year post‐treatment. The change in lower incisor inclination was measured at baseline and one year post‐treatment. In total, 97 participants began the study and their data were used for the outcome of crowding at baseline and 83 participants presented at the one‐year recall.
There was no evidence of a difference in the change in lower incisor inclinational between baseline and one year post‐treatment, between the extraction and the non‐extraction groups (MD 0.08 degrees, 95% CI −0.55 to 0.71; P = 0.8; Analysis 16.3).
16.3. Analysis.

Comparison 16: Extraction lower deciduous canines versus no active treatment (control), Outcome 3: Change in mandibular incisor inclination
Harms
No harms were reported.
Other outcomes
Time to alignment and ligation time were not relevant for this comparison.
Lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw joint problems were not reported.
Comparison 17: Extraction of third molars versus no active treatment (control)
We assessed Harradine 1998 as being at a high risk of bias due to a high number of dropouts and participants and personnel not blinded due to the nature of the intervention.
Crowding
Harradine 1998 reported the amount of crowding using Little's Irregularity Index. For the 77 participants who completed the study, no baseline imbalances were reported. There was no evidence of a difference in the change in the amount of crowding between the two groups (MD −0.30 mm, 95% CI −1.30 to 0.70; P = 0.56; Analysis 17.1).
17.1. Analysis.

Comparison 17: Extraction of third molars versus no active treatment (control), Outcome 1: Change in mandibular incisor crowding
Arch length
Harradine 1998 also reported the change in arch length between the two groups as the sum of the distances measured bilaterally between the mesial contact of the first molars and the midline contact point. There was evidence of a clear difference between the two groups (MD 1.03, 95% CI 0.56 to 1.50, P < 0.0001) with a greater decrease in arch length for the non‐extraction group (Analysis 17.2).
17.2. Analysis.

Comparison 17: Extraction of third molars versus no active treatment (control), Outcome 2: Change in mandibular arch length
Harms
No harms were reported
Other outcomes
Time to alignment, ligation time, lower incisors to mandible, lower molars to mandible, upper incisors to maxilla, self‐esteem, participant satisfaction and jaw‐joint problems were not reported.
Discussion
Summary of main results
We included 24 RCTs with 1512 participants, of whom 1314 were analysed in this review. The studies evaluated 17 comparisons. We were able to perform meta‐analyses for four comparisons.
Fixed appliances and auxiliaries
Lower lip bumper versus no active treatment (control)
The lower lip bumper reduced crowding by 4.39 mm more than the control group and increased the arch length by 3.34 mm. Both these findings are clearly different and clinically important.
The increase in arch length for the lip bumper group appeared to be due to incisor advancement (0.69 mm) and distal movement of the molar (0.61 mm), thus potentially gaining 1.3 mm of arch length. Additionally, in the lip bumper group, the lower incisors proclined by 3.14 degrees and the molars tipped distally by 4.13 degrees more than in the control group.
These findings suggest that the lip bumper keeps the molars upright and increases arch length at the expense of lower labial segment advancement. Whilst these findings showed differences with lip bumper, their clinical importance would have to be assessed on a case‐by‐case basis. Additionally, as there was only one available study that was at high risk of bias, the evidence is of very low certainty.
These findings were similar to those resulting from treatment with the lower lingual arch. Both appliances increased the arch length by around 3 mm, resulted in lower labial segment advancement of about 0.5 mm and prevented mesial movement of the molars by causing them to tip distally compared to the control groups.
Cervical headgear versus minor interceptive procedures (control)
We found that, in the one available study, headgear increased arch length in the upper arch by up to 2.28 mm more than the control group, but this was at the expense of 2.5 degrees of upper incisor proclination, therefore resulting in anterior anchorage loss. Subgroup analysis revealed that there was no clear difference in the change in proclinations seen, between baseline and one year or between baseline and two years, so the majority of the proclination occurred in the first year.
Lower arch length also increased by up to 1.52 mm and the majority of the increase was in the first two years, as subgroup analysis did not reveal a clear difference between two and eight years. The lower incisors also initially proclined, but this effect was not maintained at two years, indicating that cervical pull headgear therapy does not result in long‐term lower incisor proclination. It was also found not to affect lower incisor crowding. Upper incisor crowding was not examined, but this would be an outcome worth investigating to determine whether cervical pull headgear does alleviate crowding and if so, whether this is by increasing the maxillary arch length by incisor proclination, by distal movement of the buccal segments or a combination of both.
Lower lingual arch (LLA) versus no active treatment (control)
The LLA is traditionally passive so is used to maintain arch length and maintain leeway space following the loss of deciduous molar(s). Our analysis, from the one available study, revealed that the LLA prevented mesial movement (1.11 mm) and tipping (2.73 degrees) of the molar compared with the control group. The clinical importance of these findings may be limited. More detailed analysis revealed that the LLA only permitted 0.33 mm of mesial movement of the molar and resulted in 0.54 degrees of distal tipping, which would be 0.66 mm for the entire lower arch. In comparison, the control group had 1.44mm of mesial movement, giving a total of 2.88 mm for the arch and 2.19 degrees of mesial inclination.
Anteriorly, in the LLA group, the lower incisors advanced by 0.66 mm and 3.01 degrees more than the control group, which can be interpreted as anterior anchorage loss. However, upon closer inspection, the advancement in LLA was only 0.32 mm and by 0.73 degrees. In contrast, the control group had retroclination and distal movement of the anterior teeth, so whilst there was a difference, it may not be clinically important.
Overall, it seems that the LLA keeps the molars upright and preserves space, despite a small amount of anterior anchorage loss, compared to the control group, who had mesial movement of the lower molars and retroclination of the lower incisors. These findings were confirmed by the clear difference in the arch lengths: the LLA increased mandibular arch length by 0.07 mm, whereas the control group had a 2.54 mm reduction. The 2.61 mm difference may be clinically important.
The LLA could be considered a method of preserving the leeway space and helping to prevent crowding in the mixed dentition from being perpetuated into the permanent dentition. This may be even more relevant if deciduous molars are lost early and could be the focus of future clinical studies. However, the evidence is of very low certainty with only one available study at a high risk of bias.
Brackets
Self‐ligating versus conventional brackets
Our analysis, of three studies, revealed that there was no evidence of a difference in the relief of crowding (Analysis 4.1), or time to alignment (Analysis 4.2), between the self‐ligating and conventional brackets (Miles 2010; Pandis 2011; Songra 2014). However, there was significant heterogeneity (I2 = 94%) in the time to alignment with the time taken being much longer in Songra 2014. This can be explained by the difference in the point at which alignment was assessed. Pandis 2011 took the point to be when a rectangular (0.019" x 0.025") copper nickel‐titanium archwire was inserted passively whereas for Songra 2014, it was when a rectangular (0.019" x 0.025") stainless steel archwire was placed.
Whilst the lower incisors definitely appeared to show more proclination in the self‐ligation group, no difference was found between the two groups in the periodontal index, gingival index or pocketing depths, from the start to end of the study. However, this could be attributed to differences between the groups at baseline, with the self‐ligation group already having greater incisor proclination (Atik 2014). Further confirmation was provided by no difference being found in the change in inclination of the lower incisors, between the groups.
There was, however, a clear and clinically important difference between self‐ligating and conventional brackets, in the time taken to ligate and untie the brackets (Miles 2010). Overall, self‐ligating brackets saved over a minute and a half per treatment episode (where we assume a participant has an archwire change and so requires untying and ligation). If this is extrapolated to 30 patients, which is an estimation of the number of patients seen in an orthodontic practice per day, this is potentially a saving of approximately 45 minutes per day. This is clinically significant as this time could be used to see more patients, take a break or undertake other activities; however, the increased cost of the self‐ligating bracket systems also needs to be considered.
No evidence of a difference was found in the discomfort experienced by participants, with each of the two types of brackets, from four hours to one month after bond‐up (Atik 2014; Miles 2010).
No evidence of a difference found between the periodontal index, gingival index or pocketing depths between both groups of participants between the start and end of the study (Atik 2014).
There was also no difference in the amount of root resorption between the two groups measured between the start of treatment and nine months into treatment (Aras 2018).
These data suggest that self‐ligating brackets have no clinical advantages; however, they did result in some time saving, which has to be balanced against their increased cost. However, the evidence is of very low certainty and based on three available studies at a high risk of bias.
Active versus passive self‐ligating brackets
Two studies contributed data to this comparison (Pandis 2010a; Songra 2014). Our analysis showed that there was no evidence of a difference in the time to alignment between active and passive self‐ligating brackets. The results were consistent (I2 = 0%). The lack of significance may be attributed to the studies having relatively small sample sizes and relatively large SDs and wide CIs (Analysis 5.2). Additionally, in Pandis 2010a, there was evidence of less crowding (MD −1.0 mm; 95% CI −1.96 to −0.04; P = 0.04) in the active self‐ligation group at baseline, so alignment in this group may have been quicker, causing the difference in treatment effect to have been overestimated.
Archwires
Copper nickel‐titanium versus nickel‐titanium
We combined data from three studies in meta‐analyses to assess differences in baseline crowding and time to alignment (Aydin 2018; Ong 2011; Pandis 2009). This revealed that overall, there was baseline equivalence with regards to pre‐treatment crowding (Analysis 6.1).
For crowding at 12 weeks, a difference between groups was found in favour of the nickel‐titanium sequence (Analysis 6.2).
For time to alignment, no evidence of a difference was found between the groups in the meta‐analysis (Analysis 6.3). There was very limited heterogeneity with I2 statistic at 2%.
When investigating discomfort, there was no difference found between the archwire groups for up to one week after the archwire was changed (Ong 2011).
Coaxial nickel‐titanium versus nickel‐titanium
One study provided evidence that there is greater resolution of crowding with coaxial NiTi than NiTi and that the treatment effect increases over time for up to 12 weeks, which was the end point of the study (Sebastian 2012). However, all the participants were female so the results of the study may not be generalisable.
Titanol versus Nitinol
After demonstrating baseline equivalence in crowding between the groups, one study found no difference in the relief in crowding between the archwires (O'Brien 1990). Again, this would suggest that there is no advantage to using one wire or the other for faster alignment of the teeth; however, the level of certainty of the evidence is very low.
Nickel‐titanium versus multistranded stainless steel
We assessed one study for this comparison and found no difference in the change in crowding over time; however, this could potentially be a false negative due to the small sample size (Gravina 2013). Sandhu 2013 demonstrated that there was no difference in overall pain experience; however, NiTi archwires did cause significantly more pain at 12 hours and during day 1, than the multistranded stainless steel. The study was deemed to be at a high risk of bias.
Nickel‐titanium versus stainless steel
We assessed one study for this comparison and found that whilst initially there appeared to be a benefit to using NiTi between baseline and eight weeks, there was no clear difference in the change in crowding over time, however the study was small and likely to be under‐powered (Gravina 2013).
Multistranded stainless steel versus stainless steel
Gravina 2013 showed that there was no difference in the change in the amount of mandibular incisor crowding between the two archwires from baseline to eight weeks, but this may again be attributed to this study being small and potentially under‐powered.
Lacebacks and fixed appliances versus fixed appliances only (control)
Irvine 2004 reported that there were no clear differences in the amount of crowding or arch length between the two groups. In both groups, the lower incisors retroclined and extruded. The mandibular first molar, however, migrated mesially in the laceback group by 0.75 mm compared to the non‐laceback group, which moved distally by 0.08 mm. This mean difference of 0.83 mm could be deemed clinically significant in terms of anchorage control and space closure.
Therefore, while the use of lacebacks may not affect crowding, arch length or the position of the lower labial segment, they may be useful if anchorage loss, by mesial migration of the first permanent molars, is required posteriorly. However, This is based on one study and the evidence is of low certainty.
Vibrational appliances with fixed appliances versus fixed appliances only (control)
Two studies were identified for this comparison and combined in a meta‐analysis (Miles 2012; Woodhouse 2015).
Baseline equivalence of crowding was demonstrated (Analysis 13.1). No difference in the change in irregularity between the start and at 8 to 10 weeks (Analysis 13.2, or any subgroup differences were found between the vibrational appliance group and the control group (Analysis 13.2); however, the studies were potentially under‐powered. Additionally, there was no clear difference in the time to alignment (Analysis 13.3), reduction in discomfort or root resorption when using the vibrational appliances, so overall they provided no benefit with regards to relief of crowding, analgesia consumption, pain reduction or root resorption.
Removable appliances and auxiliaries
Schwarz appliance versus no active treatment (control)
Our analysis found that the Schwarz appliance reduced lower arch crowding by 2.14 mm more than in the control group. However, there were clear differences in baseline arch lengths, favouring the Schwarz group, and overall, no difference was seen in the change in arch length. There was also no difference in maxillary incisor advancement, but subgroup analysis revealed that the change in mandibular incisor advancement was double in the Schwarz appliance group compared to the control group. However, whilst there was a difference in the amount of advancement seen, (P = 0.006), at only 0.39 mm, it was not thought to be clinically important and could also be attributed to tracing error.
While the available evidence suggests that the Schwarz appliance is an effective treatment option for the alleviation of crowding in the mandibular arch in the short‐term, the evidence is of very low certainty with only one available study that was deemed at high risk of bias. Also, there was no follow‐up beyond nine months so it is not possible to say whether this improvement in crowding was maintained into the permanent dentition.
Eruption guidance appliance versus no active treatment (control)
The eruption guidance appliance (EGA) improved crowding in the lower labial segment with an odds ratio of 0.19, so that the likelihood of remaining crowded in the control group was 5.3 times more than in the treatment group. This was also confirmed by subgroup analysis that demonstrated a clear difference in crowding levels post‐treatment, despite baseline equivalence. However, the treated group also had 4.1 degrees of lower incisor proclination post‐treatment, which would suggest that resolution of crowding was, in part, due to the space gained from proclination. As the control group’s incisor inclination was not reported, we are unable to determine if this effect is due to the appliance.
In the maxilla, the appliance made no difference to crowding or to upper incisor proclination.
Further research, with data for the control group and long‐term follow‐up, is required for this appliance. There is a very low level of certainty in the results because they were based on one available study, which was at a high risk of bias.
Extractions
Extraction of lower deciduous canines versus no active treatment (control)
Extracting the lower deciduous canines definitely reduced crowding of the lower incisors by 4.76 mm more, but the arch length was reduced by 2.73 mm when compared to the observation group. There was no difference in the inclination of the lower incisors between the extraction and observation groups, so relief of crowding did not occur by proclination of the lower labial segment and was more likely to be as a direct result of alignment into the extraction space. However, as arch length was also reduced in the extraction group, this would imply that space is then lost for either the permanent canines or the premolars, thus transferring and increasing the crowding into the adult dentition.
The study, Kau 2004, discusses the impact of the crowding in more detail; crowding was considered to have improved if there was a 50% reduction, or if there was an irregularity score of less than 2.5 mm at the end of the study. In the extraction group, only 28% of cases demonstrated an improvement against these criteria. In fact, when arch length loss was considered alongside the crowding, only 6% of cases showed an improvement, meaning that overall there was only a 5% chance of improving crowding by extracting the lower deciduous canines.
These results should be interpreted with caution, as there was a definite difference in baseline crowding between the groups, with the extraction group having more crowding pre‐treatment. This suggests that the treatment effect may have been overestimated, as the more severely crowded teeth were able to align into the available space.
Extraction of third molars versus no active treatment (control)
Extraction of the third molars did not affect the amount of lower incisor crowding that developed; the difference between the extraction and non‐extraction groups was only 1.1 mm, which was not thought to be clinically significant. The study also reported that there were no clear differences between the two groups for upper arch crowding (Harradine 1998).
Extraction of the third molars did significantly affect the mandibular arch length, with a greater decrease in the non‐extraction group of 2.1 mm compared to the extraction group of 1.1 mm. Harradine 1998 discussed that they looked back at the study models as they could not understand why the arch length was significantly affected but not the level of crowding; they found that 23 cases had some residual space where they had had premolar extractions, despite absence of space being part of the inclusion criteria. However, when they further analysed the data by excluding these cases, they found that there was still not definate difference in crowding but that the difference in arch length was still clearly different. The study discussed that this disparity may be due to third molars having a greater impact on arch form, rather than anterior alignment.
These results should be interpreted carefully due to the high dropout rate, with only 47% of the original recruited participants completing this study. The results suggest that while extraction of wisdom teeth may have some effect on mandibular arch length, it does not significantly affect anterior crowding.
Overall completeness and applicability of evidence
Overall, we found 24 studies that investigated orthodontic interventions used to prevent or correct crowding of teeth in children.
Twenty studies compared the use of fixed appliances and auxiliaries to a control, including the use of a lower lip bumper, cervical pull headgear, lower lingual arch, different types of brackets, different types of archwire, lacebacks and vibrational appliances. Two studies compared the use of removable appliances to a control, including the Schwarz appliance and eruption guidance appliance. Two studies compared extracting teeth to a control, including extracting deciduous canines and third molars.
Two studies had high levels of attrition (Finland 2004; Harradine 1998), and four studies were potentially under‐powered (Gravina 2013; Miles 2012; Miles 2016; Woodhouse 2015). We assessed 23 studies as being at a high risk of bias and one study as being at an unclear risk of bias. The results for most outcomes were of very low certainty and therefore their results should be interpreted with caution.
We included only RCTs in this review, which we recognise is only a fraction of the total available body of evidence investigating interventions to prevent and correct dental crowding in children. However, it does represent the most reliable evidence for treatment of this clinical condition (Baumgartner 2014; Gibson 2011).
This review aimed to assess the different interventions used to prevent and correct dental crowding in children; hence we included only studies where at least 80% of participants were aged 16 years old or younger.
Most orthodontic treatment is carried out in high street private practices. Some countries may have state‐funded care, however, the criteria for patients to be deemed eligible for this care, is variable. While some of the studies included in this review were carried out in private practice, most were carried out in a university or hospital setting and therefore may have limited external validity. Additionally, while some of the interventions may require input from clinicians with specialist training, some may be appropriate for general dental practitioners to provide for their patients.
Quality of the evidence
We assessed 23 studies as being at high risk of bias and one study as being at unclear risk of bias. However, most of the studies that we deemed to be at high risk of bias, were assessed as such because, due to the nature of the interventions, participants and personnel could not be blinded, which is the same for most orthodontic interventions.
Whilst many different treatment options were identified for both the prevention and correction of crowding, there was a lack of good‐quality RCTs available for each comparison. This meant that, in many instances, there was only one study included per comparison. There was also a variety of outcome measures reported, making it difficult to draw parallels between the outcomes of different comparisons. As a result, we carried out only four meta‐analyses, with each including two studies.
Several studies had small sample sizes or had not carried out a priori sample size calculations, or both (Gravina 2013; Ong 2011; Pandis 2009; Pandis 2010a). Four studies were also potentially under‐powered (Gravina 2013; Miles 2012; Miles 2016; Woodhouse 2015). Additionally, two studies suffered high levels of dropouts, which led to attrition bias (Finland 2004; Harradine 1998).
Overall, the evidence was deemed to have a very low level of certainty, and therefore the results and conclusions should be interpreted with caution.
Potential biases in the review process
The original protocol for the review was published before the year 2000 and since then treatment modalities have changed and additional outcomes have been considered relevant. Additionally, as this review was carried out over a long period of time, three review teams have been involved over its duration, with one consistent link (JH).
Agreements and disagreements with other studies or reviews
We found seven other reviews that reported on similar comparisons and outcomes to this review (Chen 2019; El‐Angbawi 2015; Fleming 2016; Papageorgiou 2019; Wang 2018; Wazwaz 2021; Yu 2013). It was difficult to compare most of them with this review as they had no upper age limit whereas our review considers treatment for children (80% participants aged 16 years old or younger).
Chen 2019 investigated the use of a lower lingual arch to treat mandibular incisor crowding and the effects on arch dimensions and also assessed Rebellato 1997. They found that a lower lingual arch was useful to relieve mandibular incisor crowding without any significant changes in the arch dimensions. Our review showed that arch length does significantly increase, but at the expense of proclination of the lower incisors.
El‐Angbawi 2015 investigated non‐surgical adjunctive interventions for accelerating tooth movement in people undergoing fixed orthodontic treatment and also assessed Miles 2012. They also found that there was no clear difference between the two groups.
Fleming 2016 investigated non‐pharmacological interventions for alleviating pain during orthodontic treatment and assessed Miles 2012 as part of their review. They agreed with our findings that vibrational appliances do not reduce discomfort or pain at any of the time points investigated.
Papageorgiou 2019 investigated the evidence of the use of myofunctional appliances and also assessed Myrlund 2015 as part of their review. They agreed with our findings that appliances such as the eruption guidance appliance can help to treat dental crowding; however, the crowding is often alleviated by proclination of the lower incisors.
Wang 2018 evaluated initial archwires for alignment during orthodontic treatment with fixed appliances and compared stabilised NiTi against superelastic NiTi. As part of this comparison, they assessed O'Brien 1990 and agreed with our findings: there was no definite difference between nitinol and titinol in terms of tooth movement. Additionally, Wang 2018 compared single‐stranded NiTi against other types of NiTi and concluded that there was very weak evidence from one study (Sebastian 2012), that coaxial NiTi produces greater tooth movement than single‐stranded NiTi. Again, this is in agreement with our findings.
Wazwaz 2021's main outcome was time to alignment rather than crowding. Twenty of their included studies were not eligible for this review due to the age of the participants, two assessed surgical interventions, one was not an RCT and two of the interventions were not relevant to this review; we had eight studies in common but their meta‐analysis was difficult to compare to ours. It also included studies involving older participants.
Yu 2013 investigated interventions for managing relapse of the lower front teeth after orthodontic treatment and did not find any relevant studies during their searches.
Authors' conclusions
Implications for practice.
Overall, the certainty of the evidence for the prevention and correction of crowding in children was very low, with many comparisons evaluated in single small studies, therefore the conclusions below may not be generalisable, are subject to change with future research and should be interpreted with caution.
The lower lingual arch and the lower lip bumper were both effective at maintaining space by increasing the arch length by around 3 mm and preventing mesial movement of the molars, but this was at the expense of advancing the lower labial segment and anterior anchorage loss of around 0.5 mm. The lower lip bumper was also effective in reducing the amount of crowding in the six‐month follow‐up period when compared to the group that received no active treatment. However, for each intervention, only a single study was available, both of which we deemed at a high risk of bias.
For initial alignment, the use of coaxial mickel‐titanium archwiresc(NiTi) was more effective than single‐stranded NiTi to relieve dental crowding, and NiTi archwires were more effective than copper NiTi archwires. We also found that self‐ligating brackets were quicker to untie and ligate than conventional brackets by over a minute and a half per case per treatment episode but this time advantage has to be weighed against the increased cost of the brackets. However, again, both interventions each had a single available study at high risk of bias for analysis,. Other archwire comparisons showed no evidence of a difference in treatment effect.
The Schwarz appliance reduced incisor crowding in the mandible by expanding the arch, without causing clinically significant proclination of the lower incisors; however, there was no evidence on its long‐term impact and there was only one included study, which was at a high risk of bias.
Use of the eruption guidance appliance reduced the number of children with crowding; however, the lower incisor proclination of the treated group increased. Again, there was no long‐term follow‐up and only one study, at high risk of bias, was available.
Extraction of deciduous canines reduced the amount of lower labial segment crowding significantly, but overall, reduced the arch length by 2.7 mm. The study was at high risk of bias.
Extracting lower wisdom teeth in the mid‐teenage years did not reduce the amount of crowding that developed by adulthood.
Implications for research.
As the overall level of certainty of the evidence was very low, the results highlight the need for a uniform and systematic way of assessing, recording and measuring crowding in future research. This would allow comparison and combination of the results in meta‐analysis and provide a stronger level of evidence.
The results of this review show that there is a need for more long‐term, well‐designed and reported randomised controlled clinical trials to assess the preventive interventions and treatment options for crowded teeth in children. This is particularly pertinent for interventions that are used in the mixed dentition with the aim of preventing or reducing crowding in the permanent dentition.
When designing future studies, the following should be included.
Clear inclusion and exclusion criteria
Core outcome(s) for crowding
An a priori sample size calculation based on the primary outcome
Longer follow‐up times, especially when interventions are carried out in the mixed dentition
-
Reporting of outcomes in a format that is clinically useful and relevant to patients. We suggest the following:
changes in irregularity or angulation of teeth, as well as raw values alone of irregularity at different time points;
time to alignment, and time for ligation and untying, particularly for interventions such as different archwires or brackets;
pain and other adverse effects or the absence of them should be reported in all studies.
Reports of randomised clinical studies would be improved by following the guidelines produced by the CONSORT group to ensure that all relevant information is provided and reported in a consistent way (Schulz 2010) and using core outcome measures for crowding (Tsichlaki 2020).
What's new
| Date | Event | Description |
|---|---|---|
| 4 January 2022 | Amended | Edits to Acknowledgements |
History
Protocol first published: Issue 1, 2002 Review first published: Issue 12, 2021
| Date | Event | Description |
|---|---|---|
| 23 June 2008 | Amended | Converted to new review format. |
Acknowledgements
We would like to acknowledge the contribution of Professor Helen Worthington to the protocol of this review and her ongoing support.
We would like to thank Laura MacDonald (Managing Editor, Cochrane Oral Health) for assistance in the development of the review and managing the editorial process, Anne Littlewood (Information Specialist, Cochrane Oral Health) for developing the search strategy and running the searches, and Janet Lear (Cochrane Oral Health) for her support with locating papers and co‐ordinating translations. We also thank Fang Hua, Trevor Johnson, Anne‐Marie Glenny, Philip Riley, Samer Faisal Mheissen, Denise Mitchell, Jo Weldon and Luisa Fernandez‐Mauleffinch.
We are grateful to the following for translation of studies that were not in English: Professor Chengge Hua, Tian Ye, Chunjie Li, Fang Hua, Sedigheh Shahnavaz.
We would also express our sincere thanks to the following study authors who provided extra information that contributed to the review: Victorija Krusinskiene, Nik Pandis, Peter Miles, Marcio Campos, Chihiro Tanikawa, Vinay Chugh, Asli Baysal, Satpal Sandhu, Biju Sebastian, Isil Aras, Toru Deguchi, Kutalmis Buyuk, Mehak Bansal, Yassir Yassir, Mohammed Al‐Zainal, Tony Ireland.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
#1 (("class i" and (angle* or malocclusion or bite))) AND (INREGISTER) #2 (("class ii" and (angle* or malocclusion or bite))) AND (INREGISTER) #3 (("class iii" and (angle* or malocclusion or bite))) AND (INREGISTER) #4 ((crowd* AND teeth)) AND (INREGISTER) #5 (#1 or #2 or #3 or #4) AND (INREGISTER) #6 (orthodontic*) AND (INREGISTER) #7 (appliance*) AND (INREGISTER) #8 (("lip bumper*" OR lip‐bumper*)) AND (INREGISTER) #9 (("arch develop*" AND (jaw* OR mandib* OR maxill*))) AND (INREGISTER) #10 (((expansion OR expand) AND (jaw* OR maxill*))) AND (INREGISTER) #11 ("leeway space*") AND (INREGISTER) #12 (("two‐phase treatment*" OR "two‐phase therap*" or "space maintain*" OR "space maintenance")) AND (INREGISTER) #13 (#6 or #7 or #8 or #9 or #10 or #11 or #12) AND (INREGISTER) #14 (#5 and #13) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 MALOCCLUSION ANGLE CLASS I Single term (MeSH) #2 MALOCCLUSION ANGLE CLASS II Single term (MeSH) #3 MALOCCLUSION ANGLE CLASS III Single term (MeSH) #4 ((class next i) and ((angle or angle*) or malocclusion or bite)) #5 ((class next ii) and ((angle or angle*) or malocclusion or bite)) #6 ((class next iii) and ((angle or angle*) or malocclusion or bite)) #7 (crowd* near teeth) #8 (#1 or #2 or #3 or #4 or #5 or #6 or #7) #9 ORTHODONTIC APPLIANCES, FUNCTIONAL Explode all trees (MeSH) #10 ORTHODONTIC APPLIANCES, REMOVABLE Explode all trees (MeSH) #11 ORTHODONTICS PREVENTIVE, Explode all trees (MeSH) #12 ORTHODONTICS INTERCEPTIVE, Explode all trees (MeSH) #13 TOOTH EXTRACTION Explode all trees (MeSH) #14 (leeway next space*) #15 ((extraoral or (extra next oral) or extra‐oral) and appliance*) #16 (lip next bumper*) #17 (((two next phase next treatment) or (two next phase next therapy)) and (orthodontic* or malocclusion)) #18 ((arch next development) and (jaw* or mandible or maxilla*)) #19 ((extraction* and (dental or teeth or tooth)) and orthodontic*) #20 (expansion and (jaw or maxilla*)) #21 ((serial next extract*) and (teeth or orthodontic*)) #22 ((space next maintenance) and orthodontic*) #23 (#9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22) #24 (#8 and #23)
Appendix 3. MEDLINE Ovid search strategy
1. exp MALOCCLUSION, ANGLE CLASS I/ 2. exp MALOCCLUSION, ANGLE CLASS II/ 3. exp MALOCCLUSION, ANGLE CLASS III/ 4. (("Class 1" or "Class I") and (Angle or Angle's or Angles or malocclusion$ or bite$)).mp. 5. (("Class 2" or "Class II") and (Angle or Angle's or Angles or malocclusion$ or bite$)).mp. 6. (("Class 3" or "Class III") and (Angle or Angle's or Angles or malocclusion$ or bite$)).mp. 7. ((crowd$ or overcrowd$) adj6 (teeth or dentition)).mp. 8. or/1‐7 9. exp Orthodontic Appliances, Functional/ 10. exp Orthodontic Appliances, Removable/ 11. exp Orthodontics, Preventive/ 12. exp Orthodontics, Interceptive/ 13. exp Tooth Extraction/ 14. ((extraoral or "extra oral" or extra‐oral) and appliance$).mp 15. ("Lip bumper$" or lip‐bumper$).mp. 16. ("arch develop$" and (jaw or mandib$ or maxill$)).mp. 17. (extract$ and (dental or teeth or tooth) and orthodontic$).mp. 18. ((expansion or expand) and (jaw$ or maxill$)).mp. 19. ("serial extract$" and (teeth or orthodontic$)).mp. 20. "leeway space$".mp. 21. ("two‐phase" adj3 treat$).mp. 22. ("two‐phase" adj3 therap$).mp. 23. (21 or 22) and (orthodontic$ or malocclusion$).mp. 24. ((space adj maintenance) and orthodontic$).mp. 25. ((space adj3 maintain$) and orthodontic$).mp. 26. 24 or 25 27. (orthodontic$ and (functional or removable) and appliance$).mp. 28. ((interceptive or preventive) and orthodontic$).mp. 29. ((activator adj4 appliance$) and orthodontic$).mp. 30. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 23 or 26 or 27 or 28 or 29 31. 8 and 30
The above subject search was linked with the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials in MEDLINE (as described in Lefebvre 2020, box 3b).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. MALOCCLUSION/ 2. (("Class 1" or "class I") and (Angle or Angle's or Angles or malocclusion$ or bite$)).mp. 3. (("Class 2" or "Class II") and (Angle or Angles or Angle's or malocclusion$ or bite$)).mp. 4. (("Class 3" or "Class III") and (Angle or Angle's or Angles or Malocclusion$ or bite$)).mp. 5. ((crowd$ or overcrowd$) adj6 teeth).mp. 6. or/1‐5 7. exp Orthodontic Device/ 8. orthodontics.mp. or exp ORTHODONTICS/ 9. 8 and ((removable or functional) and appliance$).mp. 10. 8 and (preventive or interceptive).mp. 11. Tooth Extraction/ 12. "leeway space$".mp. 13. ((extraoral or "extra oral" or extra‐oral) and appliance$).mp. 14. ("lip bumper$" or lip‐bumper$).mp. 15. ("arch develop$" and (jaw$ or mandib$ or maxilla$)).mp. 16. (extract$ and (dental or teeth or tooth) and orthodontic$).mp. 17. ((expansion or expand$) and (jaw$ or maxilla$)).mp. 18. ("serial extraction$" and (teeth or orthodontic$)).mp. 19. ("two‐phase" adj3 treat$).mp. 20. ("two‐phase" adj3 therap$).mp. 21. (19 or 20) and (orthodontic$ or malocclusion$).mp. 22. ("space maintenance" and orthodontic$).mp. 23. ((space adj3 Maintain$) and orthodontic$).mp. 24. 7 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 21 or 22 or 23 25. 6 and 24
The above subject search was linked with the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials in Embase (as described in Lefebvre 2020, box 3e).
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
crowded and teeth
Appendix 6. World Health Organization International Clinical Trials Registry Platform search strategy
crowded and teeth
Data and analyses
Comparison 1. Lower lip bumper versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Change in mandibular crowding | 1 | 34 | Mean Difference (IV, Random, 95% CI) | ‐4.39 [‐5.07, ‐3.71] |
| 1.2 Change in arch length | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 3.34 [2.71, 3.97] |
| 1.3 Change in mandibular incisor A‐P position | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.09, 0.89] |
| 1.4 Change in mandibular incisor inclination | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 3.14 [1.73, 4.55] |
| 1.5 Change in mandibular molar A‐P position | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐0.91 [‐1.58, ‐0.24] |
| 1.6 Change in mandibular molar inclination | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐4.13 [‐6.09, ‐2.17] |
Comparison 2. Cervical pull headgear versus minor interceptive procedures (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Mandibular incisor crowding (pre‐treatment, 2 years, 4 years, 8 years, 13 years) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Pre‐treatment | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐2.53, 0.35] |
| 2.1.2 2 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐0.60, 1.26] |
| 2.1.3 4 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.86, 0.80] |
| 2.1.4 8 years | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [‐0.35, 1.39] |
| 2.1.5 13 years | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 0.26 [‐1.35, 1.87] |
| 2.2 Change in maxillary arch length | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.2.1 2 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.98 [1.80, 2.16] |
| 2.2.2 8 years | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 2.28 [2.05, 2.51] |
| 2.3 Change in mandibular arch length | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.3.1 2 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [1.17, 1.43] |
| 2.3.2 8 years | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 1.52 [1.30, 1.74] |
| 2.4 Change in lower incisor to mandibular plane (0‐1 years and 0‐2 years) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.4.1 0 to 1 year | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 2.30 [0.67, 3.93] |
| 2.4.2 0 to 2 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [‐0.42, 3.22] |
| 2.5 Change in upper incisor to maxillary plane | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.5.1 0 to 1 year | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 4.00 [1.97, 6.03] |
| 2.5.2 0 to 2 years | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 4.50 [1.36, 7.64] |
Comparison 3. Lower lingual arch versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Change in mandibular arch length | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 2.61 [1.83, 3.39] |
| 3.2 Change in mandibular incisor A‐P position | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.66 [0.46, 0.86] |
| 3.3 Change in mandibular incisor inclination | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 3.01 [1.71, 4.31] |
| 3.4 Change in mandibular molar A‐P position | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐1.11 [‐1.51, ‐0.71] |
| 3.5 Change in mandibular molar inclination | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐2.73 [‐4.29, ‐1.17] |
Comparison 4. Self‐ligating brackets versus conventional brackets.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Maxillary incisor crowding (pre‐treatment and 10 weeks) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1.1 Pre‐treatment | 2 | 166 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐1.49, 1.15] |
| 4.1.2 10 weeks | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.93, 0.13] |
| 4.2 Time to alignment | 2 | 148 | Mean Difference (IV, Random, 95% CI) | 89.64 [‐45.89, 225.17] |
| 4.3 Ligation time | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.3.1 Untying | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐22.30 [‐25.83, ‐18.77] |
| 4.3.2 Ligating | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐78.80 [‐81.86, ‐75.74] |
| 4.4 Change in lower incisor to mandibular plane | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.4.1 Change | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 1.29 [‐1.77, 4.35] |
Comparison 5. Active self‐ligating brackets versus passive self‐ligating brackets.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Maxillary incisor crowding (pre‐treatment) | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐1.96, ‐0.04] |
| 5.1.1 Pre‐treatment | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐1.96, ‐0.04] |
| 5.2 Time to alignment | 2 | 144 | Mean Difference (IV, Fixed, 95% CI) | ‐13.11 [‐28.76, 2.53] |
5.1. Analysis.

Comparison 5: Active self‐ligating brackets versus passive self‐ligating brackets, Outcome 1: Maxillary incisor crowding (pre‐treatment)
Comparison 6. Copper nickel‐titanium versus nickel‐titanium archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Mandibular incisor crowding (pre‐treatment) | 3 | 254 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.27, 0.58] |
| 6.2 Little's Irregularity Index at 12‐weeks | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.35, 0.63] |
| 6.3 Time to alignment | 2 | 191 | Mean Difference (IV, Random, 95% CI) | ‐2.63 [‐14.50, 9.24] |
Comparison 7. Coaxial nickel‐titanium versus nickel‐titanium archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Mandibular incisor crowding (pre‐treatment) | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.14, 1.34] |
| 7.2 Total amount of tooth movement | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.2.1 4 weeks | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 3.33 [2.72, 3.94] |
| 7.2.2 8 weeks | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 5.07 [4.16, 5.98] |
| 7.2.3 12 weeks | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | 6.77 [5.55, 7.99] |
7.1. Analysis.

Comparison 7: Coaxial nickel‐titanium versus nickel‐titanium archwires, Outcome 1: Mandibular incisor crowding (pre‐treatment)
Comparison 8. Titanol versus nitinol archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Change in maxillary incisor crowding | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.33, 0.89] |
| 8.1.1 Change in maxillary incisor crowding | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.33, 0.89] |
Comparison 9. Nickel‐titanium versus multistranded stainless steel archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Change in mandibular incisor crowding | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 1.60 [‐22.16, 25.36] |
9.1. Analysis.

Comparison 9: Nickel‐titanium versus multistranded stainless steel archwires, Outcome 1: Change in mandibular incisor crowding
Comparison 10. Nickel‐titanium versus stainless steel archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Change in mandibular incisor crowding | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐16.80 [‐42.79, 9.19] |
10.1. Analysis.

Comparison 10: Nickel‐titanium versus stainless steel archwires, Outcome 1: Change in mandibular incisor crowding
Comparison 11. Multistranded stainless steel versus stainless steel archwires.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 11.1 Change in mandibular incisor crowding | 1 | 23 | Mean Difference (IV, Fixed, 95% CI) | ‐18.40 [‐47.12, 10.32] |
11.1. Analysis.

Comparison 11: Multistranded stainless steel versus stainless steel archwires, Outcome 1: Change in mandibular incisor crowding
Comparison 12. Lacebacks with fixed appliances versus fixed appliances only (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 12.1 Change in mandibular incisor crowding | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐5.90, 5.24] |
| 12.1.1 Amount of crowding (mean change) | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐5.90, 5.24] |
| 12.2 Change in mandibular arch length | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [‐6.41, 8.07] |
| 12.2.1 Arch length (mean change) | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [‐6.41, 8.07] |
Comparison 13. Vibrational appliances with fixed appliances versus fixed appliances only (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 13.1 Mandibular incisor crowding (pre‐treatment and after initial alignment) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1.1 Irregularity at baseline | 2 | 122 | Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐2.54, 1.70] |
| 13.1.2 Irregularity at initial alignment | 2 | 119 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.05, 0.90] |
| 13.2 Change in mandibular incisor crowding | 2 | 119 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [‐0.81, 1.30] |
| 13.3 Time to alignment | 2 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐3.70 [‐26.29, 18.89] |
Comparison 14. Schwarz appliance versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 14.1 Change in mandibular incisor crowding | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐2.79, ‐1.49] |
| 14.1.1 Change in mandibular incisor crowding | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐2.79, ‐1.49] |
| 14.2 Change in mandibular arch length | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.46, 0.68] |
| 14.2.1 Change in mandibular arch length | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.46, 0.68] |
| 14.3 Change in lower incisor to APog | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.3.1 Change in lower incisor to APog | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.11, 0.67] |
| 14.4 Change in upper incisor to SN | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐2.26, 2.92] |
| 14.4.1 Change in upper incisor to SN | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐2.26, 2.92] |
Comparison 15. Eruption guidance appliance versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 15.1 Maxillary incisor crowding (pre‐treatment and 1 year) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1.1 Pre‐treatment | 1 | 46 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [0.73, 7.92] |
| 15.1.2 1 year post‐treatment | 1 | 46 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.25, 2.63] |
| 15.2 Mandibular incisor crowding (pre‐treatment and 1 year) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.2.1 Pre‐treatment | 1 | 46 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.60, 6.83] |
| 15.2.2 1 year post‐treatment | 1 | 46 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.05, 0.68] |
Comparison 16. Extraction lower deciduous canines versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 16.1 Change in mandibular incisor crowding | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐6.24, ‐3.28] |
| 16.1.1 Change between baseline and 1 year | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐6.24, ‐3.28] |
| 16.2 Change in mandibular arch length | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐2.73 [‐3.69, ‐1.77] |
| 16.3 Change in mandibular incisor inclination | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.55, 0.71] |
| 16.3.1 LR1 Incisor change | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.55, 0.71] |
Comparison 17. Extraction of third molars versus no active treatment (control).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 17.1 Change in mandibular incisor crowding | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐1.30, 0.70] |
| 17.2 Change in mandibular arch length | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | 1.03 [0.56, 1.50] |
| 17.3 Change in maxillary incisor crowding | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | 0.44 [‐0.52, 1.40] |
17.3. Analysis.

Comparison 17: Extraction of third molars versus no active treatment (control), Outcome 3: Change in maxillary incisor crowding
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aras 2018.
| Study characteristics | ||
| Methods | Setting: Ege University, Turkey Design: parallel (2 arms) No. of centres: 1 Study duration: 9 months |
|
| Participants | Inclusion criteria: "Angle class I malocclusion, 4–10 mm of anterior crowding in both arches, 2–4 mm of overjet and overbite, complete permanent dentition except third molars, no evident root resorption in maxillary incisor teeth, no history of restorative or endodontic treatment of these incisors, no dilacerated incisor roots or peg laterals, no systemic diseases or periodic medications, and no history of previous orthodontic treatment." Exclusion criteria: not reported Participant sampling: N = 32 selected Group 1 (n = 16): 12 female, 4 male (mean age of 15.0 ± 1.03 years) Group 2 (n = 16): 10 female, 6 male (mean age of 14.94 ± 1.06 years) Sex: 22 female, 10 male Dropouts: not reported |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Self‐ligating brackets versus conventional brackets |
|
| Outcomes | Loss of root volume in maxillary incisor teeth | |
| Notes | The number of teeth affected by root resorption Group 1: 4 teeth had palatal root resorption (6.25%); 4 teeth had proximal root resorption (6.25%) Group 2: 14 teeth had palatal root resorption (21.87%); 13 teeth had proximal root resorption (20.31%) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning adolescents to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Blinding was not possible due to the groups being potentially distinguishable via the bracket images" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Quote: "Reproducibility of the measurements was high, with an ICC of 0.988 (95% confidence interval [CI] 0.0980–0.992)" |
Atik 2014.
| Study characteristics | ||
| Methods | Setting: Department of Orthodontics, Hacettepe University, Ankara, Turkey Design: parallel (2 arms) No. of centres: 1 Study duration: not reported. Mean treatment duration for intervention group 13.2 months and control group 15.3 months |
|
| Participants | Inclusion criteria: “between 13 and 17 years of age at the start of the treatment, moderate maxillary and mandibular crowding, a Class I malocclusion, and a dentally constricted maxillary arch.” Exclusion criteria: not reported Participant sampling: N = 33 selected Group 1 (n = 17): 17 female (mean age of 14.5 + 1.2 years) Group 2 (n = 16): 16 female (mean age of 14.8 + 1.0 years) Sex: 100% female Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Self‐ligating brackets versus conventional brackets |
|
| Outcomes | Lower incisors to mandible, harms (discomfort, plaque index, gingival index and probing depth) | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "The pre‐treatment and post‐treatment lateral cephalograms of each patient were traced by one examiner." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None noted |
Aydin 2018.
| Study characteristics | ||
| Methods | Setting: Suleyman Demirel, University, Faculty of Medicine, Isparta, Turkey Design: parallel (2 arms) No. of centres: 1 Study duration: recruitment October 2014‐August 2015 |
|
| Participants | Inclusion criteria: "(1) mandibular anterior dental crowding (Little's Irregularity Index [LII] > 6 mm); (2) 12 to 18 years of age; (3) permanent dentition; (4) treatment requiring no extraction of premolars or any other teeth; (5) skeletal and dental Class I relationships; (6) normal overjet and overbite; and (7) systemically and periodontally healthy." Exclusion criteria: "(1) unwilling to be assigned to any of the treatment options; (2) caries and impacted or missing teeth except for third molars; (3) orthodontic treatment history; (4) posterior crossbite; (5) craniofacial syndrome or skeletal asymmetry; and (6) periodic non‐steroidal anti‐inflammatory drug use." Participant sampling: N = 76 randomised; 66 analysed Group 1 NiTi (n = 36): 26 female, 10 male (mean age of 14.71 ± 1.79 years) Group 2 Copper NiTi (n = 30): 20 female, 10 male (mean age of 15.86 ± 1.58 years) Sex: 46 female, 20 male Dropouts: 10 |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Copper nickel‐titanium versus nickel‐titanium archwires |
|
| Outcomes | Crowding | |
| Notes | Sample size calculation not carried on primary outcome measure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The two study groups were designated using simple randomization (coin method)." |
| Allocation concealment (selection bias) | Low risk | Quote: "The two study groups were designated using simple randomization (coin method)." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "During the single‐blind study, the allocation of wires was concealed from the participants, but the clinician had this information." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "LII and mandibular arch dimensions were measured on three‐dimensional digital dental models at 2‐week intervals." "...the mandibular dental arch of each patient was scanned using an intraoral 3D scanner." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 80 patients eligible; 76 randomised; data available for 66 |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported |
| Other bias | High risk | Quote: "To achieve 95% power, the study included 36 patients per group (for alveolar inter‐first molar width feature; mean, 50 mm; standard deviation, 0.35; alpha level, 0.05)." Quote: "In this single‐center study, the treatments were performed by a single clinician." Quote: "After a 2‐week interval, 20 study models were randomly selected and re‐measured for reproducibility of the measurements (r: Cronbach's alpha, 0.871–0.963)." |
Davidovitch 1997.
| Study characteristics | ||
| Methods | Setting: Medical College of Virginia, USA, postgraduate orthodontic clinic Design: parallel (2 arms) No. of centres: 1 Study duration: 6 months |
|
| Participants | Inclusion criteria: "(1) white ethnicity, (2) 3 to 8 mm mandibular arch length deficiency, (3) presence of the mandibular deciduous second molars, and (4) Class I, Division 2 malocclusion" Exclusion criteria: not reported Participant sampling: N = 34 selected Group 1 (n = 16): sex and mean age of group not reported Group 2 (n = 18): sex and mean age of group not reported Overall age reported across both groups: 7.9‐13.1 years (mean = 10.2 years) Sex: not reported Dropouts: not reported |
|
| Interventions | Orthodontic intervention group: fixed appliances and auxiliaries Lip bumper versus no active treatment (observation) |
|
| Outcomes | Crowding, arch length, lower incisors to mandible, lower molars to mandible | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specifically reported whether lip bumper removed for impressions or radiographs |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | There was a large difference between tomographic and lateral ceph measurements Quote: "Tomographic data (‐6.31° ± 1.28°) showed approximately twice the angulation change as that measured from lateral cephalometric radiographs (‐3.38° ± 3.67°). The average change in molar angulation of experimental versus control subjects was found to be statistically significant when observed tomographically (p < 0.02)". |
Finland 2004.
| Study characteristics | ||
| Methods | Setting: Department of Oral Development and Orthodontics, Institute of Dentristry, Oulu, Finland Design: parallel (2 arms) No. of centres: 1 Study duration: 13 years |
|
| Participants | Inclusion criteria: "need for orthodontic treatment due to moderate crowding and a Class II tendency. The crowding was clinically diagnosed as moderate, based on the degree of space deficiency in the anterior regions of the dental arches". Exclusion criteria: not reported Participant sampling: N = 68 selected Group 1 (n = 34): sex and mean age of group not reported Group 2 (n = 34): sex and mean age of group not reported Overall age reported across both groups: mean age of 7.6 ± 3 years Overall sex reported across both groups: 28 female, 40 male Dropouts at the 13‐year follow‐up: "Thirty‐four subjects (53 per cent of the total study group) attended a recall appointment at T4 at the mean age of 20.6 years" |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Cervical pull headgear versus minor interceptive procedures (control) |
|
| Outcomes | Crowding, arch length, lower incisors to mandible, upper incisors to maxilla | |
| Notes | Funding source: research grant from the European Orthodontic Society | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomly allocated to 2 groups |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment Quote: “To conceal the allocation, most of the practitioners who undertook the treatment were not given information concerning the aim or rationale of the study.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessor was blinded: Quote: “All measurements were made by one author (VK) directly on dental casts using a digital calliper with an accuracy of 0.01 mm. Dental aesthetics was evaluated in the patients by two calibrated observers (PK and ASS) using the AC of IOTN scores (Evans and Shaw, 1987) at the last follow‐up (T4).” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Low response rate Quote: "Fifty‐three patients (83 per cent of the total study group) who continued to the second phase of treatment at T2 completed the follow‐up at T3 and full records were available. Thirty‐four subjects (53 per cent of the total study group) attended a recall appointment at T4 at the mean age of 20.6 years.” |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Impact of the various different interceptive treatments used in the control group was unclear |
Gravina 2013.
| Study characteristics | ||
| Methods | Setting: Brazil, Rio de Janeiro Design: parallel (3 arms) No. of centres: 1 Study duration: 8 weeks |
|
| Participants | Inclusion criteria: "presence of all erupted permanent teeth except for second and third molars; no previous orthodontic treatment; no indications for tooth extraction; overbite and overjet that allowed brackets to be placed on the lower teeth without occlusal interferences; level of crowding and teeth position that allowed a maximum deflection of 2 mm in the archwire when inserted in the bracket slots, and good conditions of oral hygiene and health". Exclusion criteria: not reported Participant sampling: N = 36 selected Group 1 (n = 11): sex and mean age of group not reported Group 2 (n = 12): sex and mean age of group not reported Group 3 (n = 13): sex and mean age of group not reported Overall age reported across groups: mean age of 14 ± 2 years Overall sex reported across both groups: 18 male, 18 female Dropouts: not reported |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Stainless steel versus multi stranded stainless steel versus nickel‐titanium |
|
| Outcomes | Crowding | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Possible measurement bias |
Harradine 1998.
| Study characteristics | ||
| Methods | Setting: Bristol Dental Hospital, UK Design: parallel (2 arms) No. of centres: 1 Study duration: 5.5 years (best estimate) |
|
| Participants | Inclusion criteria: "All patients had previously undergone orthodontic treatment, but on entry into the study were no longer wearing any orthodontic appliances or retainers. Orthodontic treatment comprised active treatment in the upper arch only with either removable appliances or a single arch fixed appliance, with no treatment or premolar extractions only being carried out in the lower arch. All patients had crowded third molars." Exclusion criteria: not reported Patient sampling: N = 164 selected Group 1 (only numbers of those available at follow‐up reported, n = 44): sex and mean age of group not reported Group 2 (only numbers of those available at follow‐up reported, n= 33): sex and mean age of group not reported Overall age reported across both groups at start: 14.1 years ± 16.2 months Overall sex reported across both groups at start: 90 female, 74 male Dropouts: 87 (55%) |
|
| Interventions | Orthodontic intervention: extractions Extraction of third molars versus no active treatment (control) |
|
| Outcomes | Crowding, arch length | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor Quote: "The third molar status was unknown to the digitizer" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate with only 45% of the original participants completing the study |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Unclear due to recall rate |
Irvine 2004.
| Study characteristics | ||
| Methods | Setting: Royal Bournemouth Hospital Design: parallel (2 arms) No. of centres: 1 Study duration: 6 months |
|
| Participants | Inclusion criteria: "A malocclusion requiring the extraction of all first premolars, no previous orthodontic treatment, lateral cephalometric radiographs to have been taken
of the patient within the previous 12 months at the start of treatment." Exclusion criteria: not reported Participant sampling: N = 71 selected Group 1 (n = 30): 12 male, 18 female (mean age of 13.6 ± 1.5 years) Group 2 (n = 32): 14 male, 18 female (mean age of 13.8 ± 1.5 years) Sex: 26 male, 36 female Dropouts: Group 1 = 3 withdrew, 2 lost to follow‐up Group 2 = 4 withdrew Total = 9 |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Lacebacks with fixed appliances versus fixed appliances only |
|
| Outcomes | Crowding, arch length | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | Unclear who/how many examiners took the measurements and intra/inter‐rater reliability not reported |
Kau 2004.
| Study characteristics | ||
| Methods | Setting: dental clinics in Italy, Germany, Wales Design: parallel (2 arms) No. of centres: 3 Study duration: 1 year, follow‐up 2 years |
|
| Participants | Inclusion criteria: "Caucasian children aged between 8 and 9 years old; crowding of the lower incisors greater than or equal to 6 mm, according to the irregularity index of Little (1975); Class I type occlusion as indicated by the molar relationship; the lower molars should have a good long‐term prognosis; overbite should be within normal limits". Exclusion criteria: not reported Participant sampling: N = 97 selected Group 1 (n = 55): sex and mean age of group not reported Group 2 (n = 42): sex and mean age of group not reported Age: "Caucasian children aged between 8 and 9 years old" (mean age and SD not reported) Sex: not reported Dropouts: 14 |
|
| Interventions | Orthodontic intervention: extractions Extraction of lower deciduous canines versus no active treatment (control) |
|
| Outcomes | Crowding, arch length, lower incisors to mandible | |
| Notes | Funding source: “This study was supported by a general research grant from the Wales Office of Research and Development for Health and Social Care.” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation Quote: "Simple randomization was the method of allocation treatment. A restricted randomization of allocation was used in blocks of 50 to ensure that equal numbers of patients were allocated to each of the treatment groups." |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment Quote: "The random allocation was then concealed in envelopes labelled with the study identification number and held in a central place." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessors Quote: "Observer bias was reduced by ensuring that the examiner was blind to whether the patient had received an extraction or non‐extraction treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate Quote: "53/55 (96%) extraction group; 30/42 (71%) non‐extraction group followed up; overall 83/97 (86%)" |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Unclear how many participants came from each centre and what the characteristics were of the participants from each centre |
Miles 2010.
| Study characteristics | ||
| Methods |
Setting: Caloundra, Queensland, Australia Design: parallel (2 arms) No. of centres: 1 Study duration: 10 weeks |
|
| Participants | Inclusion criteria: "consecutive subjects scheduled for non‐extraction treatment in the upper arch" Exclusion criteria: not reported Participant sampling: N = 68 selected Group 1 (n = 34): sex and mean age of group at start not reported Group 2 (n = 34): sex and mean age of group at start not reported Overall age reported across both groups at the end of the study: 13.5 ± 1.5 years Sex at the end of the study: Group 1 = 19 female, 11 male Group 2 = 19 female, 11 male Dropouts: Group 1 = 4 (11.7%) Group 2 = 4 (11.7%) |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Self‐ligating brackets versus conventional brackets |
|
| Outcomes | Crowding, ligation time, harms (discomfort) | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear impact of missing data Quote: "Of the 68 patients enrolled in the study, follow‐up impressions were missed for two subjects in Group 1 and four subjects in Group 2"; "...42 (70%) returned the discomfort questionnaires." |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Unclear impact of missing data Quote: “Two subjects, matched for age, gender and incisor irregularity, with two subjects in Group 2, were dropped from Group 1 to keep the same number of subjects in each group." |
Miles 2012.
| Study characteristics | ||
| Methods | Setting: Caloundra and University of Queensland Department of Orthodontics, Australia Design: parallel (2 arms) No. of centres: 1 Study duration: 10 weeks |
|
| Participants | Inclusion criteria: "children aged between 11 to 15 years, a non‐extraction treatment plan in the lower arch, no impactions/unerupted teeth, fixed appliances bonded from first molar to first molar in both arches, and living locally to allow for additional appointments for impressions" Exclusion criteria: not reported Participant sampling: N = 66 selected Group 1 (n = 33 for irregularity, 31 for discomfort): 19 female, 14 male (mean age of 13.1 ± 0.18 years) Group 2 (n = 33 for irregularity, 29 for discomfort): 21 female, 12 male (mean age of 13.0 ± 0.18 years) Sex: 40 female, 26 male Dropouts: Group 1 = irregularity 0 (0%); discomfort 1 (4%) Group 2 = irregularity 2 (6%); discomfort 1 (3%) |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Vibrational appliance versus no vibrational appliance (control) |
|
| Outcomes | Crowding, harms (discomfort) | |
| Notes | Funding source not cited | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinicians blinded, however not possible to blind participants due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessor blinded, however not possible to blind participants, who assessed their own pain levels, due to the different interventions used. Quote: "A staff member who was blinded to the study groups and trained in the use of a micrometer measured the VAS data." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate Quote: “Sixty‐six patients were enrolled in the study, of whom 64 patients reported for all 4 impression appointments. Pain scores were recorded by 60 patients, with 58 completing all 5 time points” |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
Miles 2016.
| Study characteristics | ||
| Methods | Setting: Caloundra, Queensland, Australia, private practice Design: parallel (2 arms) No. of centres: 1 Study duration: 10 weeks |
|
| Participants | Inclusion criteria: "(1) children up to age 16, (2) a fully erupted dentition from first molar forward, (3) erupted or erupting second molars, (4) no missing or previously extracted permanent teeth, (5) undergoing comprehensive orthodontic treatment with full fixed appliances, and (6) a Class II malocclusion requiring extraction of 2 maxillary premolars but no mandibular extractions". Exclusion criteria: not reported Participant sampling: N = 40 selected Group 1 (n = 20): 12 female, 8 male (mean age of 13.0 ± 1.5 years) Group 2 (n = 20): 14 female, 6 male (mean age of 12.7 ± 1.2 years) Sex: 26 female, 14 male Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Vibrational appliance versus no vibrational appliance (control) |
|
| Outcomes | Crowding, time to alignment, harms (discomfort) | |
| Notes | Funding source: "a special research grant was obtained from the Australian Society of Orthodontists Foundation for Research and Education to purchase the AcceleDent Aura appliances and to fund the statistical analysis" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation “Randomization was performed using permuted blocks of 10 randomly generated numbers with the random generation function in Excel (Microsoft, Redmond, Wash)" |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment Quote: “The numbers were sealed in opaque envelopes and shuffled by a staff member." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinician blinded, however not possible to blind participants due to the different interventions used “A clinical assistant opened an envelope for the group assignment after a patient's brackets were bonded and gave routine instructions in a closed consultation room to ensure that the operator (P.M.) was blinded.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor “And the model assessor (E.F.) was blinded to the treatment group and the model time point” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts "All subjects, once assigned, completed the trial with no lost data." |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
Myrlund 2015.
| Study characteristics | ||
| Methods | Setting: "Patients recruited from Tromsø, Norway; Public Dental Service Competence Centre of Northern Norway (TkNN) and the University student clinic (UTK). All treatment carried out at TkNN". Design: parallel (2 arms) No. of centres: 1 Study duration: 1 year |
|
| Participants | Inclusion criteria: "early mixed dentition with upper central incisors and first molars fully erupted; Angle Class I or Class II occlusion with one or more of the following characteristics: deep bite (≥2/3 overlapping of the incisors), increased overjet ≥5 mm, moderate anterior crowding in combination with an overjet of ≥4 mm". Exclusion criteria: children with Angle Class III malocclusion, crossbites, or retroclined upper incisors Participant sampling: N = 48 selected Group 1 (n = 25): 12 female, 13 male (mean age of 7.7 ± 0.6 years) Group 2 (n = 13): 11 female, 12 male (mean age of 7.7 ± 0.5 years) Sex: 23 female, 25 male Dropouts: 2 (4.2%); 1 from each group |
|
| Interventions | Orthodontic intervention: removable appliances and auxiliaries Eruption guidance appliance versus no active treatment (control) |
|
| Outcomes | Crowding, lower incisors to mandible, upper incisors to maxilla | |
| Notes | Funding source: “LM‐Instruments Oy, Finland, has supplied the study with free LM activators for the patients” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisaton “For the randomization, each subject was given an identification number. The numbers were written on a closed raffle ticket and put in a hat from where 25 subjects were blindly drawn to the experimental group, the remaining 23 subjects comprising the control group. Drawing was performed by an independent person (HK)." |
| Allocation concealment (selection bias) | Low risk | Adequate allocation concealment “To avoid any allocation bias, all clinical characteristics and personal data of the patients were concealed at this point.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessors “Before measuring, all study casts were pooled together and labelled by only numbers to hide any identification of group, patient name, or date of the model from the investigator. Similarly, all cephalograms were blinded before tracing by numbering the X‐rays randomly.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate “After 1 year, one boy from the treatment group (refused treatment after 6 months) and one girl from the control group (moved) had dropped out, resulting in 24 and 22 subjects in the treatment and control groups, respectively.” |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
O'Brien 1990.
| Study characteristics | ||
| Methods | Setting: Manchester, UK Design: parallel (2 arms) No. of centres: 1 Study duration: up to 37 days |
|
| Participants | Inclusion criteria: "...patients who were attending for routine Edgewise fixed appliance therapy..." Exclusion criteria: not reported Orthodontic intervention: 0.016" super‐elastic titinol or 0.016" nitinol archwire; all fitted with identical edgewise brackets Participant sampling: N = 40 selected Group 1 (n = 20): 11 female, 9 male (mean age of 12.95 ± 3.2 years) Group 2 (n = 20): sex of group not reported (mean age of 13.4 ± 3.12 years) Sex: overall sex across both groups not reported Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Nitinol versus titinol archwires |
|
| Outcomes | Crowding | |
| Notes | Funding source: “Thomas Bolton & Johnson Limited, Stoke‐on‐Trent, England, for supplying the archwires.” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Inadequate information on how randomisation was carried out "Forty patients who were attending for routine Edgewise fixed appliance therapy were randomly allocated". |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | Only contact point movement reported; final contact point displacement not reported "Initial contact point displacement measured and contact point movement following archwire placement in mm." |
| Other bias | Unclear risk | No sample size calculation |
Ong 2011.
| Study characteristics | ||
| Methods | Setting: private orthodontic practice, Caloundra, Queensland, Australia Design: parallel (3 arms) No. of centres: 1 Study duration: 1 year |
|
| Participants | Inclusion criteria: "all patients who required both upper and lower orthodontic appliances were included. There were no restrictions regarding age, previous orthodontic experience, or extraction/non‐extraction treatment. No patients had craniofacial abnormalities" Exclusion criteria: "children were excluded if they had asymmetrically missing or extracted premolars, missing or unerupted lower incisors or canines, or teeth blocked out that did not allow for placement of all brackets at the initial bonding appointment" Participant sampling: N = 132 selected Group 1 (n = 44): 30 female, 14 male (mean age of 14.4 ± 4.4 years) Group 2 (n = 44): 25 female, 19 male (mean age of 15.5 ± 6.4 years) Group 3 (n = 44): 25 female, 19 male (mean age of 16.1 ± 8.3 years) Sex: 80 female, 52 male Dropouts: 1 dropout from group 3; however, missing data due to missing or broken models and discomfort questionnaires not being returned |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Copper nickel‐titanium versus nickel‐titanium archwires |
|
| Outcomes | Crowding, time to alignment, harms (discomfort) | |
| Notes | Funding source: “This study was supported by a grant from the Australian Society of Orthodontists’ Foundation for Research and Education” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomly allocated to 3 groups "A restricted randomization process was employed, where patients were randomized in blocks of 12 to ensure equal allocation of patients to the treatment groups. Randomization was performed using computer generated numbers." |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment "A list of numbers was kept by the laboratory staff, who on the day of bracket placement would then assign them to the appropriate group, so the treating clinician was not involved" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants blinded, however not possible to blind personnel due to the different interventions used "The patients were blinded to their group allocation throughout treatment; however, the treating clinician could not be masked." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor "The clinician’s staff assigned an identification number to each model prior to measurement in order to mask the principal researcher (EO) to the patient name, treatment allocation, time‐point and archwire group during study model analysis. The models were rematched to the patient and archwire group after data collection was complete." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 dropout, however missing data due to missing or broken models and discomfort questionnaires not being returned. "One patient transferred and was lost to follow up; therefore, 131 patients completed the trial. Some of the irregularity data were lost because nine study models were missing and two were broken. Some discomfort data were also lost because 63 questionnaires were not returned. The data were checked for non‐response bias and there were no significant differences in the number of returned forms between the archwire groups, therefore, this is unlikely to have affected the results." |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
Pandis 2009.
| Study characteristics | ||
| Methods | Setting: Corfu, Greece, private practice of study author Design: parallel (2 arms) No. of centres: 1 Study duration: 6 months |
|
| Participants | Inclusion criteria: "non‐extraction treatment on the mandible, eruption of all mandibular teeth, no spaces in the mandibular arch, no crowding in the posterior segments, mandibular irregularity index greater than 2, and no therapeutic intervention planned involving intermaxillary or other intraoral or extraoral appliances including intra‐arch or interarch elastics, lip bumpers, maxillary expansion appliances, or headgears". Exclusion criteria: not reported Participant sampling: N = 60 selected Group 1 (n = 30): 70% female, 30% male (mean age of 13.4 ± 1.8 years) Group 2 (n = 30): 83.4% female, 16.6% male (mean age of 12.8 ± 1.7 years) Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Copper nickel‐titanium versus nickel‐titanium archwires |
|
| Outcomes | Crowding, time to alignment | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation “Randomization was done using random permuted blocks of size 6.” |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment "Opaque envelopes were used to allocate treatment.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Adequate blinding of participants and personnel "Allocation of wires was concealed from the investigator and the participants during the observation period, and no other wire was used throughout the study” "The type of wire selected for each patient was not disclosed to the provider or the patient" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessor was blinded "Measurements were made intraorally twice by the same clinician using a fine‐tip digital caliber (Digimatic NTD12‐6‐in C, Mitutoyo, Kanagawa, Japan), and the means of the 2 measurements were entered into an Excel spreadsheet (Microsoft, Redmond, Wash).” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
Pandis 2010a.
| Study characteristics | ||
| Methods | Setting: Corfu, Greece, private practice of study author Design: parallel (2 arms) No. of centres: 1 Study duration: 175 days |
|
| Participants | Inclusion criteria: "non‐extraction treatment in both arches, eruption of all maxillary teeth, no spaces in the maxillary arch, no high canines, maxillary irregularity index greater than 4 mm, and no therapeutic intervention planned involving intermaxillary or other intraoral or extraoral appliances including elastics, maxillary expansion appliances, or headgear". Exclusion criteria: not reported Participant sampling: N = 70 selected Group 1 (n = 35): 60% female, 40% male (mean age of 13.8 ± 1.8 years) Group 2 (n = 35): 57% female, 43% male (mean age of 13.8 ± 1.7 years) Sex: 58.6% female, 41.4% male Dropouts: 4 (2 per group) |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Active versus passive self‐ligating brackets |
|
| Outcomes | Crowding, time to alignment | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation "Randomization was accomplished by generating random permuted blocks of variable size; this ensured equal patient distribution between the 2 trial arms." |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment "Numbered, opaque, sealed envelopes were prepared before the trial containing the treatment allocation card. After patient selection, the secretary of the practice was responsible for opening the next envelope in sequence." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear if assessor was blinded "Measurements were made twice on the initial casts by the first author with a digital caliper (Digimatic NTD12‐6’’C, Mitutoyo, Tokyo, Japan)." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 dropouts (2 per group) = 6% |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Single centre, private practice; per‐protocol analysis |
Pandis 2011.
| Study characteristics | ||
| Methods | Setting: Corfu, Greece, private practice of study author Design: parallel (2 arms) No. of centres: 1 Study duration: 16 months |
|
| Participants | Inclusion criteria: "non‐extraction treatment on both arches, eruption of all mandibular teeth, no spaces in the mandibular arch, mandibular irregularity index greater than 2 mm (canine to canine), and no therapeutic intervention planned involving intermaxillary or other intraoral or extraoral appliances including elastics, maxillary expansion appliances, or headgears before the end of the observation period". Exclusion criteria: not reported Participant sampling: N = 50 selected Group 1 (n = 25): 64% female, 36% male (mean age of 13.4 ± 1.6 years) Group 2 (n = 25): 68% female, 32% male (mean age of 13.2 ± 1.6 years) Sex: 66% female, 34% male Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Self‐ligating brackets versus conventional brackets |
|
| Outcomes | Time to alignment | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation “Fifty patients were randomized to either a conventional or a self‐ligating appliance. The statistical software package was used by the first author, and the user‐written ralloc command was implemented to generate the random allocation sequence. Randomization was accomplished by generating random permuted blocks of variable size (2 and 4), which assured equal patient distribution between the 2 trial arms.” |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment “Sequentially numbered, opaque, sealed envelopes were prepared before the trial containing the treatment allocation cards. After patient selection and recording of baseline information, the secretary in the practice was responsible for opening the next envelope in sequence and allocation.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor “Impressions were taken, plaster models were prepared, and the brackets from second premolar to second premolar were scraped off with a curving knife by the laboratory technician to facilitate blind measurements. Each model had an identification number so that the measurements could be correctly entered into the spreadsheet” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Single centre, private practice |
Rebellato 1997.
| Study characteristics | ||
| Methods | Setting: not reported Design: parallel (2 arms) No. of centres: 1 Study duration: 10.5 months for lingual arch, 12.5 months for control |
|
| Participants | Inclusion criteria: "(1) both mandibular second deciduous molars were present with some clinical mobility, (2) mandibular crowding was 3 mm or more, (3) permanent molar relationships were end‐on to Class I (end‐on molars would have flush mesial planes and Class I mandibular molars were up to 4 mm mesial of flush mesial plane15), (4) overbite was 1 mm or greater, (5) mandibular plane inclination was average (MP‐SN) of 32 ° + 6 °, and (6) the lower lip was less than 4 mm ahead of Rickett's E line". Exclusion criteria: "patients were excluded from the study if they had any congenitally or prematurely missing teeth. Only European American patients were selected, because ethnic differences in mean skeletal patterns and mean differences in arch length and tooth sizes between European Americans and African Americans have been reported". Participant sampling: N = 30 selected Group 1 (n = 14): sex of group not reported (mean age 11.5 years; SD not reported) Group 2 (n = 16): sex of group not reported (mean age of 11.3 years; SD not reported) Sex: not reported Dropouts: not reported |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Lower lingual arch versus no active treatment (control) All participants were observed at least monthly |
|
| Outcomes | Arch length, lower incisors to mandible, lower molars to mandible | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear method of randomisation “Subjects were randomly assigned to two groups” |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether the lingual arches were removed prior to record collection and the assessors were truly blinded Quote: "The presence of the lingual arches prevented totally blind measurements, so a technician unfamiliar with the study made the measurements." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | No sample size calculation, no mention of source of participants, proportion of male and female, or allocation concealment. Due to this poor reporting, we had concerns about the study so we assessed it as unclear risk. |
Sandhu 2013.
| Study characteristics | ||
| Methods | Setting: single centre in India Design: parallel (2 arms) No. of centres: 1 Study duration: December 2010‐June 2012 |
|
| Participants | Inclusion criteria: "(1) 11‐ to ‐17‐year‐old male and female who required fixed orthodontic treatment; (2) moderate‐to‐severe crowding (4–9 mm) in the mandibular anterior segment that was not severe enough to prevent bracket engagement, patients with severe crowding related to one or two teeth (such as blocked out lateral incisors) were not included; (3) eruption of all mandibular anterior teeth; (4) no history of medical problems/medication that could influence pain perception; and (5) informed and witnessed consent from the minor participant and their parent/guardian". Exclusion criteria: "(1) presence of a severe deep bite that could affect bracket placement on the mandibular anterior teeth; (2) malocclusion correction required treatment procedures other than continuous arch wire mechanics; (3) participants taking pain medications for chronic pain; (4) participants with a positive history of dental pain or pain in the orofacial region; (5) a medical condition that precluded the use of a fixed orthodontic appliance (e.g. allergy to nickel, recent history of epileptic seizure or physician’s consent could not be obtained, etc.)" Participant sampling: N = 96 selected Group 1: 21 female, 21 male (mean age of 14.2 ± 1.9 years) Group 2: 22 female, 21 male (mean age of 13.9 ± 2.0 years) Sex: 43 female, 42 male Dropouts: "One participant was lost to follow up and 10 were excluded from the analysis due to bond failure or incomplete questionnaire answers". |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Nickel‐titanium versus multistranded stainless steel archwires |
|
| Outcomes | Harms (pain perception) | |
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation "The randomization schedule was prepared by using ralloc procedure (Stata/SE 10.0 software) to enrol 96 participants into superelastic nickel titanium and multi‐ stranded stainless steel groups using stratified block (size 4) randomization." |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment "A statistician generated the random allocation sequence, and the dental assistant helped enrol and conceal participant allocation using the opaque sealed envelope method." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants blinded, however not possible to blind personnel due to the different interventions |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessors "The VAS score was measured by trained dental assistants (blinded to the study) using a manual 0.1‐ mm calibrated Vernier caliper (manual type)." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts reported and sample size calculation completed "One participant was lost to follow up and 10 were excluded from the analysis due to bond failure or incomplete questionnaire answers." |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None identified |
Sebastian 2012.
| Study characteristics | ||
| Methods | Setting: Noorul Islam College of Dental Sciences, Trivandrum, Kerala, India Design: parallel (2 arms) No. of centres: 1 Study duration: 12 weeks |
|
| Participants | Inclusion criteria: "female patients in postmenarche period between 13 and 15 years of age with crowding in the lower anterior segment and having a mandibular irregularity index greater than 6, Class I skeletal pattern, extraction treatment in mandibular arch, all mandibular teeth erupted with no spacing between them, no relevant medical history, no recent history of intake of drugs such as nonsteroidal anti‐inflammatory drugs (NSAIDs). No previous active orthodontic treatment. Receiving full arch mechanics, preadjusted edgewise appliance therapy and no therapeutic intervention planned involving intermaxillary or other intraoral or extraoral appliances during the study period". Exclusion criteria: "recruitment of patients who may have experienced periodontal disease and hence loss of attachment, was avoided; participants who had taken any drugs because of unavoidable circumstances" Participant sampling: N = 24 selected Group 1 (n = 12): 12 female, no male (mean age of 13.8 ± 0.7 years) Group 2 (n = 12): 12 female, no male (mean age of 13.6 ± 0.6 years) Sex: 100% female Dropouts: none |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Coaxial nickel‐titanium versus nickel‐titanium archwires |
|
| Outcomes | Crowding | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation “Randomization was done using computer software–generated numbers” |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment “Opaque envelopes were used to allocate the archwires to two groups, each consisting of 12 participants. Allocation thus was concealed from the investigator and from participants during the study.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor “All readings were measured by an expert single operator, who was not aware of the archwire specimen used for the arches being measured.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | All participants female; sample size based on pilot study |
Songra 2014.
| Study characteristics | ||
| Methods | Setting: Musgrove Park Hospital, Taunton, UK Design: parallel (3 arms) No. of centres: 1 Allocation ratio: 2:2:1 Study duration: recruitment span 2006‐2010; last debond 2011 |
|
| Participants | Inclusion criteria: "Less than 18 years of age, ready to commence maxillary and mandibular fixed appliance treatment, intact labial segments, and premolar extractions required in all 4 quadrants." Exclusion criteria: "...could not understand English, had learning difficulties, and had incomplete labial segments." Participant sampling: N = 100 randomised; 98 analysed Group 1 Damon 3MX passive self‐ligating brackets (n = 41): 25 female, 17 male (mean age of 14.2 ± 1.09 years) Group 2 In‐Ovation R active self‐ligating brackets (n = 37): 20 female, 10 male (mean age of 13.9 ± 1.49 years) Group 3 Omni conventional brackets (n = 20): 12 female, 8 male (mean age of 13.5 ± 1.0 years) Sex: 47 female, 63 male Dropouts: 2 (2%) |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Self‐ligating brackets versus conventional brackets |
|
| Outcomes | Crowding, time to alignment | |
| Notes | We combined the data from the Damon 3MX and In‐Ovation R bracket groups as they are both self‐ligating brackets | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomization was carried out by the local research and development office, which was contacted by telephone before the bond‐up of each participant." |
| Allocation concealment (selection bias) | Low risk | "The randomization was carried out by the local research and development office, which was contacted by telephone before the bond‐up of each participant. This process allowed allocation concealment from the researchers and prevented the possibility of prediction of the next randomization in each block." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The brackets had different physical appearance so participants and personnel could not be blinded to the interventions. "The patients and the operators carrying out the treatment (N.E.A., G.S., and others) could not be blinded." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "This was done to facilitate easy removal of the impression and to ensure that the bracket type would remain concealed on the study models during subsequent measurements. Therefore, only the model assessor (G.S.) was blinded during the study." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "In total, 100 patients were recruited into the trial, and 98 were followed to completion of treatment, with 2 dropouts." |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | A priori power calculation undertaken; reliability testing undertaken; measurements undertaken in standardised conditions; single centre but multiple operators; standardised archwire sequence |
Tai 2010.
| Study characteristics | ||
| Methods | Setting: Tai orthodontic office (private) Osaka, Japan Design: parallel (2 arms) No. of centres: 1 Study duration: up to 21 months |
|
| Participants | Inclusion criteria: "Angle Class I malocclusions with crowding and normal vertical dimensions and no posterior crossbites" Exclusion criteria: "no posterior crossbites" Participant sampling: N = 28 selected Group 1 (n = 14): 8 female, 6 male (7 years 11 months at T0; 9 years 1 month at T1 ‐ mean age not reported) Group 2 (n = 14): 8 female, 6 male (8 years at T0; 9 years 8 months at T1 ‐ mean age not reported) Dropouts: none |
|
| Interventions | Orthodontic intervention: removable appliances and auxiliaries Schwarz appliance versus no active treatment (control) |
|
| Outcomes | Crowding, arch length, lower incisors to mandible, upper incisors to maxilla | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Inadequate information on how randomisation was carried out “After initial recording of the data, the patients were randomized to 2 groups.” |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation sequence concealed from those assigning patients to participant groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor “To prevent bias in the measurement of the expanded and nonexpanded groups, the investigator was blinded.” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts not reported |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported |
| Other bias | Low risk | Sample size based on pilot study |
Woodhouse 2015.
| Study characteristics | ||
| Methods | Setting: King’s College London Dental Institute (Guy’s Hospital); the Royal Alexander Children’s Hospital, Brighton, Sussex; and William Harvey Hospital, Ashford, Kent, UK Design: parallel (3 arms) No. of centres: 3 Study duration: 209 ± 65 days |
|
| Participants | Inclusion criteria: "(1) < 20 years old at start of treatment, (2) no medical contraindications, (3) in the permanent dentition, (4) mandibular arch incisor irregularity, and (5) extraction of mandibular first premolars included in the orthodontic treatment plan" Exclusion criteria: "no posterior crossbites" Participant sampling: N = 81 selected Group 1 (n = 29): sex of group not reported (mean age of 13.9 ± 1.6 years) Group 2 (n = 25): sex of group not reported (mean age of 14.1 ± 1.9 years) Group 3 (n =27): sex of group not reported (mean age of 14.4 ± 1.8 years) Overall sex reported across groups: 40 male, 41 female Overall age reported across groups: mean age of 14.06 ± 1.7 years Dropouts: 4 (Group 1 = 1, Group 2 = 2, Group 3 = 1) |
|
| Interventions | Orthodontic intervention: fixed appliances and auxiliaries Vibrational appliance versus control |
|
| Outcomes | Crowding, time to alignment, harms (pain, root resorption) | |
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate method of randomisation “The randomization sequence was generated using GraphPad online software (http://www.graphpad.com/quickcalcs/index.cfm)” |
| Allocation concealment (selection bias) | Low risk | Adequate method of allocation concealment "Participant allocation undertaken centrally at King’s College London, independently from the clinical operators, following recruitment.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel due to the different interventions used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Adequate blinding of assessor “Dental casts were coded so that measurements were undertaken blind”. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout rate ‐ less than 10% drop‐out at final alignment. "At initial alignment, a full data set was obtained except for 1 case allocated to fixed only, where the mandibular cast was lost." |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | High risk | For the secondary outcome of root resorption (DiBiase 2016), the study was underpowered (20%‐30%) |
A‐P: antero‐posterior;APog: A‐point to pogonion line; LII: Little's Irregularity Index; n: number; NiTi: nickel‐titanium; SD: standard deviation; SN: sella‐nasion
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdelrahman 2015 | Did not meet age range specified for review |
| Agarwal 2021 | Did not meet age range specified for review |
| Akyalcin 2007 | Not RCT |
| Alcan 2006 | Did not report on crowding |
| Almeida 2015 | Did not meet age range specified for review |
| Altug 2005 | Did not report on crowding |
| Angelieri 2008 | Not RCT |
| Atik 2018 | Did not report on crowding; retrospective |
| Atik 2019 | Does not meet age range specified for review |
| Bansal 2019 | Did not meet age range specified for review |
| Battagel 1998 | Not RCT |
| Baumrind 1996 | Not RCT |
| Bennett 1999 | Did not report on crowding |
| Bhasin 2017 | Did not report on crowding |
| Bhavra 2002 | Did not report on crowding |
| Bondemark 2005 | Did not report on crowding |
| Bondemark 2007 | Not RCT |
| Caprioglio 2014 | Not RCT |
| Celebi 2019 | Unclear if meets age range specified for review; study authors contacted, but no response |
| Cerruto 2017 | Did not report on crowding |
| CTRI/2018/05/014070 | 25% of participants > 16 years old |
| CTRI/2018/10/016038 | Did not meet age range specified for review |
| Dmitrenko 2016 | Not RCT |
| Fan 2009 | Did not meet age range specified for review |
| Feldmann 2008 | Did not report on crowding |
| Fleming 2009a | Did not meet age range specified for review |
| Fleming 2009b | Did not meet age range specified for review |
| Fleming 2010 | Did not report on crowding |
| Germec 2008 | Not RCT and did not meet age range specified for review |
| Germec‐Cakan 2010 | Did not meet age range specified for review |
| Gibreal 2019 | Did not meet age range specified for review |
| IRCT2016042427577N1 | Did not meet age range specified for review |
| Kaklamanos 2017 | Did not report on crowding |
| Keski‐Nisula 2008a | Not RCT |
| Keski‐Nisula 2008b | Not RCT |
| Krishna 2016 | Not RCT |
| Lombardo 2018 | Did not meet age range specified for review |
| Mahmoudzadeh 2018 | Did not meet age range specified for review |
| Mateu 2018 | Did not report on crowding |
| Miles 2018 (AJO‐DO) | Did not report on crowding |
| Mittal 2020 | Did not meet age range specified for review. Surgical procedure |
| Murakami 2016 | Not RCT |
| Nabbat 2020 | Does not meet age range specified for review |
| NCT03645356 | Did not report on crowding |
| NCT03652454 | Does not meet age range specified for review |
| NCT04106141 | Did not meet age range specified for review |
| Nordstrom 2018 | Did not meet age range specified for review |
| Pandis 2007 | Not RCT |
| Pandis 2010b | Not RCT |
| Scott 2008 | Did not meet age range specified for review |
| Silva 2012 | Did not report on crowding |
| Silvola 2009 | Did not report on crowding |
| Soldanova 2012 | Did not meet age range specified for review |
| Taner 2003 | Did not report on crowding |
| Virkkula 2009 | Did not report on crowding |
| Wasserman 2009 | No contact from study author to gain further study information |
| West 1995 | Data not available; results were pooled |
| Xu 2010 | > 60% of participants had < 3 mm crowding |
| Yavuz 2018 | Did not meet age range specified for review |
| Yildirim 2018 | Unclear if age range matches that specified by review ‐ unsuccessful contact with study authors |
| Yu 2008 | Not RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
CTRI/2017/08/009333.
| Methods | Parallel‐group RCT Method of generating randomisation sequence: adaptive randomisation, such as minimisation Method of allocation concealment: sequentially numbered, sealed, opaque envelopes Blinding: participant and investigator blinded |
| Participants | Target sample size: 54 Inclusion criteria: between 11‐20 years of age, requiring both upper and lower or lower fixed orthodontic treatment, moderate (Little's irregularity index (LLI) score 4mm to 6mm) to severe crowding (LII score 6mm to 9mm) in mandibular anterior segment, requiring both extraction or non‐extraction treatment (except lower anterior extraction), malocclusion treatment requiring continuous archwire system, no history of previous orthodontic treatment, all mandibular teeth erupted except second or third molars, no relevant medical history, no analgesics taken prior to procedure, no/mild crowding in the posterior segments Exclusion criteria: patients with a blocked out tooth that will not allow for placement of the bracket at initial bonding appointment, those whose treatment plan includes extraction of lower incisor, those with missing or extracted lower incisor, people with craniofacial syndrome, those with poor oral hygiene or periodontally compromised teeth, those with a medical condition that precluded the use of a fixed orthodontic appliance (e.g. allergy to nickel, recent history of epileptic seizure or physician's consent could not be obtained), those with spacing in lower anterior region, with anterior cross bite or having deep bite |
| Interventions | Fixed appliances (archwires): nickel titanium versus superelastic nickel titanium Intervention: conventional nickel titanium archwire (0.016 inch conventional nickel titanium wire) Control: superelastic nickel titanium wire (0.016 inch superelastic nickel titanium wire) |
| Outcomes | Mandibular anterior irregularity achieved by 0.016 inch conventional nitinol versus 0.016 inch superelastic nickel titanium wire over a period of 12 weeks Timepoints for measurement: before placement of fixed orthodontic appliance in lower arch After 12 weeks of mandibular aligning wire placement in lower arch |
| Notes | Emailed author; awaiting contact |
CTRI/2018/04/013037.
| Methods | Parallel‐group RCT Allocation concealment: sequentially numbered, sealed, opaque envelopes Participant and outcome assessor blinded |
| Participants | Target sample size: 20 Inclusion criteria: Class I malocclusion, fully erupted permanent dentition, no missing teeth, between 14‐35 years of age Exclusion criteria: children with a history of previous orthodontic treatment, missing teeth, history of trauma, syndromes or extensive cuspal wear |
| Interventions | Fixed appliances: ordinary orthodontic bracket versus newer generation ceramic brackets |
| Outcomes | Changes in tooth position ("to achieve initial leveling and aligning in 6 months") "Correct the facial profile" |
| Notes | Dr Balakrishna Shetty, Department of Orthodontics and Dentofacial Orthopedics, Karnataka, India dr_bkshetty@yahoo.com |
CTRI/2018/05/014220.
| Methods | Unknown |
| Participants | Children with malocclusion requiring extraction of premolars for treatment Inclusion criteria: patients reporting to the department for orthodontic treatment, no history of previous orthodontic treatment, crowding less than 5 mm, no other therapeutic intervention, no medical contraindications |
| Interventions | Different methods of ligation: continuous bracket ligation technique versus conventional bracket ligation technique 17x25 inch stainless steel wire in situ for at least 6 weeks |
| Outcomes | Proclination and vertical changes in the position of the incisors, and mesial movement of the molars as measured on a lateral cephalogram and study models Secondary: alleviation of crowding measured with Little's Index, arch length, chairside time needed for both the ligation techniques, changes in the Inter‐canine width and inter‐molar width, oral hygiene status ‐ Gingival Index and Plaque Index will be recorded |
| Notes | Emailed author; awaiting contact |
NCT02996292.
| Methods | Setting: Syrian Arab Republic Design: 3‐arm parallel RCT No. of centres: unclear Study duration: unclear |
| Participants | Age 14‐24 years Inclusion criteria:
Exclusion criteria:
|
| Interventions | Orthodontic intervention: fixed appliances Conventional brackets versus active self‐ligating brackets versus passive self‐ligating brackets |
| Outcomes | Primary outcome: speed of alignment Secondary outcomes:
|
| Notes | Emailed author; awaiting contact |
UMIN000036836.
| Methods | Setting: Department of Orthodontics and Dentofacial Orthopedics, Osaka University Dental Hospital Funder: Align Technology Japan |
| Participants | Minimum age of 12 years |
| Interventions | Clear aligners |
| Outcomes | Treatment period, teeth alignment |
| Notes | Contacted study authors ‐ awaiting response Author email: ctanika@dent.osaka‐u.ac.jp |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT04347018.
| Study name | NCT04347018 |
| Methods | Setting: unclear Design: parallel RCT (2 arms) No. of centres: unclear Study duration: unclear |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Orthodontic intervention: fixed appliances BRIUS appliance versus preadjusted edgewise full fixed appliance |
| Outcomes | Primary outcome: Little's Irregularity Index Secondary outcomes: pain and discomfort |
| Starting date | July 2020 |
| Contact information | malzaina@buffalo.edu |
| Notes | Emailed study author for further information |
RBR‐9kvw9t.
| Study name | Evaluation of efficacy and efficiency of a removable esthetic appliance for solving teeth crowding in the childhood: a randomized clinical trial |
| Methods | 2‐arm parallel RCT |
| Participants | Target: 40 participants, 20 in each group Inclusion criteria: 7 to 11 years old, mixed dentition phase, with definitive primary crowding of at least 3 mm Exclusion criteria: presence of agenesis of one or more upper incisors, need for the use of extraoral or extraction mechanics, presence of caries lesions, history of orthodontic treatment, cleft lip and palate, syndromes or any type of systemic or neurological alteration that makes it impossible to perform interventions and presence of white spot lesion or caries already established |
| Interventions | Invisible aligners versus fixed partial 4 x 2 mechanical appliances |
| Outcomes | "Primary outcome: primary anterior and superior crowding correction in the mixed dentition ‐ at least 2mm Little's index change. Secondary outcome: better white spot lesion prevention during the appliance use". |
| Starting date | 21 August 2019 |
| Contact information | Vinicius Augustus Merino da Silva, Faculdade de Odontologia de Bauru/FOB/USP, Brazil vinisilva@usp.br |
| Notes | Emailed author; awaiting contact |
RCT: randomised controlled trial
Differences between protocol and review
The author team has changed since the protocol and there is a new lead author.
We clarified the categorisation of treatments in the Type of interventions section of the Methods.
We updated and edited the Background.
When completing data extraction, we found that some of the studies reported on arch length (upper and lower jaw), ligation time, time to alignment and pain (including the use of analgesia). We decided that these are important clinical outcomes so we added them as secondary outcomes to our Methods section and reported on them in this review.
We did not undertake the handsearching we had originally planned.
Contributions of authors
The review was conceived by Jayne Harrison (JEH), Kevin O'Brien (KDO'B) and Bill Shaw (WCS). Previous work, which was the foundation of current study, was undertaken by Sylvia Bickley (SRB), JEH and KDO’B. The protocol was written by JEH, SRB, Helen V Worthington, KDO’B, WCS and Fyeza Janjua Sharif (FJS).
The review was co‐ordinated by JEH. FJS and JEH or JEH and DM or ST and DO screened the results, retrieved papers and appraised the risk of bias and quality of the papers and extracted data from them. DM or JEH checked any papers that were disputed between FJS and JEH or ST and DO. FJS and JEH or ST and DO analysed and interpreted the data. ST, DO and JEH wrote the review.
Sources of support
Internal sources
-
The Liverpool University Hospitals NHS Trust, UK
Salary support JEH
-
School of Dentistry, The University of Manchester; Manchester Academic Health Sciences Centre (MAHSC); and the NIHR Manchester Biomedical Research Centre, UK
Support to Cochrane Oral Health
External sources
-
NHS National Primary Dental Care R&D (Research and Development) Programme, UK
Grant funding for scoping and pilot projects for orthodontic reviews
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (ohg.cochrane.org/partnerships-alliances). Contributors over recent years have been: British Association for the Study of Community Dentistry, UK; British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; Centre for Dental Education and Research at All India Institute of Medical Sciences, India; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; Swiss Society for Endondontology, Switzerland.
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Sarah Turner: none known Jayne E Harrison: none known. I am an Editor with Cochrane Oral Health Fyeza NJ Sharif: none known Darren Owens: none known Declan T Millett: none known
Edited (no change to conclusions)
References
References to studies included in this review
Aras 2018 {published data only}
- Aras I, Unal I, Huniler G, Aras A. Root resorption due to orthodontic treatment using self-ligating and conventional brackets. Journal of Orofacial Orthopedics 2018;79(3):181-90. [DOI] [PubMed] [Google Scholar]
Atik 2014 {published data only}
- Atik E, Ciger S. An assessment of conventional and self-ligating brackets in Class I maxillary constriction patients. Angle Orthodontist 2014;84(4):615-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aydin 2018 {published data only}
- Aydin B, Senisik NE, Koskan O. Evaluation of the alignment efficiency of nickel-titanium and copper-nickel-titanium archwires in patients undergoing orthodontic treatment over a 12-week period: a single-center, randomized controlled clinical trial. Korean Journal of Orthodontics 2018;48(3):153-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davidovitch 1997 {published data only}
- Davidovitch M, McInnis D, Lindauer SJ. The effects of lip bumper therapy in the mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics 1997;111(1):52-8. [DOI] [PubMed] [Google Scholar]
Finland 2004 {published and unpublished data}
- Hadler-Olsen S, Pirttiniemi P, Kerosuo H, Sjögren A, Pesonen P, Julku J, et al. Does headgear treatment in young children affect the maxillary canine eruption path? European Journal of Orthodontics 2018;40(6):583-91. [DOI] [PubMed] [Google Scholar]
- Krusinskiene V, Kiuttu P, Julku J, Silvola AS, Kantomaa T, Pirttiniemi P. A randomized controlled study of early headgear treatment on occlusal stability--a 13 year follow-up. European Journal of Orthodontics 2008;30(4):418-24. [DOI] [PubMed]
- Mantysaari R, Kantomaa T, Pirttiniemi P, Pykalainen A. The effects of early headgear treatment on dental arches and craniofacial morphology: a report of a 2 year randomized study. European Journal of Orthodontics 2004;26(1):59-64. [DOI] [PubMed] [Google Scholar]
- Pirttiniemi P, Kantomaa T, Mantysaari R, Pykalainen A, Krusinskiene V, Laitala T, et al. The effects of early headgear treatment on dental arches and craniofacial morphology: an 8 year report of a randomized study. European Journal of Orthodontics 2005;27(5):429-36. [DOI] [PubMed] [Google Scholar]
Gravina 2013 {published data only}
- Gravina MA, Brunharo IH, Fraga MR, Artese F, Campos MJ, Vitral RW, et al. Clinical evaluation of dental alignment and leveling with three different types of orthodontic wires. Dental Press Journal of Orthodontics 2013;18(6):31-7. [DOI] [PubMed] [Google Scholar]
- Quintão CC, Jones ML, Menezes LM, Koo D, Elias CN. A prospective clinical trial to compare the performance of four initial orthodontic archwires. Korean Journal of Orthodontics 2005;35(5):381-7. [Google Scholar]
Harradine 1998 {published data only}
- Harradine N, Pearson M, Toth B. The effect of extraction of third molars on late lower incisor crowding: a randomized controlled trial. British Journal of Orthodontics 1998;25:117-22. [DOI] [PubMed] [Google Scholar]
Irvine 2004 {published data only}
- Irvine R, Power S, McDonald F. The effectiveness of laceback ligatures: a randomized controlled clinical trial. Journal of Orthodontics 2004;31(4):303-11. [DOI] [PubMed] [Google Scholar]
Kau 2004 {published data only}
- Kau CH, Durning P, Richmond S, Miotti FA, Harzer W. Extractions as a form of interception in the developing dentition: a randomized controlled trial. Journal of Orthodontics 2004;31(2):107-14. [DOI] [PubMed] [Google Scholar]
Miles 2010 {published data only}
- Miles P, Weyant R. Porcelain brackets during initial alignment: are self-ligating cosmetic brackets more efficient? Australian Orthodontic Journal 2010;26(1):21-6. [PubMed] [Google Scholar]
Miles 2012 {published data only}
- Miles P, Smith H, Weyant R, Rinchuse DJ. The effects of a vibrational appliance on tooth movement and patient discomfort: a prospective randomised clinical trial. Australian Orthodontic Journal 2012;28(2):213-8. [PubMed] [Google Scholar]
Miles 2016 {published data only}
- Miles P, Fisher E. Assessment of the changes in arch perimeter and irregularity in the mandibular arch during initial alignment with the AcceleDent Aura appliance vs no appliance in adolescents: a single-blind randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2016;150(6):928-36. [DOI] [PubMed] [Google Scholar]
- Miles P. Does microvibration accelerate leveling and alignment? A randomized controlled trial. Journal of Clinical Orthodontics 2018;52(6-7):342-5. [PubMed] [Google Scholar]
Myrlund 2015 {published data only}
- Myrlund R, Dubland M, Keski-Nisula K, Kerosuo H. One year treatment effects of the eruption guidance appliance in 7- to 8-year-old children: a randomized clinical trial. European Journal of Orthodontics 2015;37(2):128-34. [DOI] [PubMed] [Google Scholar]
- Myrlund R, Keski-Nisula K, Kerosuo H. Stability of orthodontic treatment outcomes after 1-year treatment with the eruption guidance appliance in the early mixed dentition: a follow-up study. Angle Orthodontist 2019;89(3):206-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Brien 1990 {published data only}
- O'Brien K, Lewis D, Shaw W, Combe E. A clinical trial of aligning archwires. European Journal of Orthodontics 1990;12:380-4. [DOI] [PubMed] [Google Scholar]
Ong 2011 {published data only}
- Ong E, Ho C, Miles P. Alignment efficiency and discomfort of three orthodontic archwire sequences: a randomized clinical trial. Journal of Orthodontics 2011;38:32-9. [DOI] [PubMed] [Google Scholar]
Pandis 2009 {published and unpublished data}
Pandis 2010a {published data only}
- Pandis N, Polychronopoulou A, Eliades T. Active or passive self-ligating brackets? A randomized controlled trial of comparative efficiency in resolving maxillary anterior crowding in adolescents. American Journal of Orthodontics & Dentofacial Orthopedics 2010;137(1):12.e1-6; discussion 12-3. [DOI] [PubMed]
Pandis 2011 {published data only}
- Pandis N, Polychronopoulou A, Katsaros C, Eliades T. Comparative assessment of conventional and self-ligating appliances on the effect of mandibular intermolar distance in adolescent non-extraction patients: a single-center randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopaedics 2011;140(3):99-105. [DOI] [PubMed] [Google Scholar]
Rebellato 1997 {published data only}
- Rebellato J, Lindauer SJ, Rubenstein LK, Isaacson RJ, Davidovitch M, Vroom K. Lower arch perimeter preservation using the lingual arch. American Journal of Orthodontics and Dentofacial Orthopedics 1997;112(4):449-56. [DOI] [PubMed] [Google Scholar]
Sandhu 2013 {published data only}
- Sandhu S, Sandhu J. A randomized clinical trial investigating pain associated with superelastic nickel–titanium and multistranded stainless steel archwires during the initial leveling and aligning phase of orthodontic treatment. Journal of Orthodontics 2013;40:276-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sebastian 2012 {published data only}
- Sebastian B. Alignment efficiency of superelastic coaxial nickel-titanium vs superelastic single-stranded nickel-titanium in relieving mandibular anterior crowding: a randomized controlled prospective study. Angle Orthodontics 2012;82(4):703-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Songra 2014 {published and unpublished data}
- Songra G, Clover M, Atack NE, Ewings P, Sherriff M, Sandy JR, et al. Comparative assessment of alignment efficiency and space closure of active and passive self-ligating vs conventional appliances in adolescents: a single-center randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2014;145(5):569-78. [DOI: 10.1016/j.ajodo.2013.12.024] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tai 2010 {published data only}
- Tai K, Hotokezaka H, Park JH, Tai H, Miyajima K, Choi M, et al. Preliminary cone-beam computed tomography study evaluating dental and skeletal changes after treatment with a mandibular Schwarz appliance. American Journal of Orthodontics & Dentofacial Orthopedics 2010;138(3):262.e1-11; discussion 262-3. [DOI] [PubMed]
Woodhouse 2015 {published data only}
- DiBiase A, Woodhouse N, Papageorgiou S, Johnson N, Slipper C, Grant J, et al. Effect of supplemental vibrational force on orthodontically induced inflammatory root resorption: a multicenter randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2016;150:918-27. [DOI] [PubMed] [Google Scholar]
- Woodhouse N, DiBiase A, Papageorgiou S, Johnson N, Slipper C, Grant J, et al. Supplemental vibrational force does not reduce pain experience during initial alignment with fixed orthodontic appliances: a multicenter randomized clinical trial. Scientific Reports - Nature 2015;27:17224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodhouse NR, DiBiase AT, Johnson N, Slipper C, Grant J, Alsaleh M, et al. Supplemental vibrational force during orthodontic alignment: a randomized trial. Journal of Dental Research 2015;94(5):682-9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdelrahman 2015 {published data only}
- Abdelrahman R, Al-Nimrib KS, Al Maaitah EF. A clinical comparison of three aligning archwires in terms of alignment efficiency: a prospective clinical trial. Angle Orthodontist 2015;85(3):434-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdelrahman R, Al-Nimrib KS, Al Maaitah EF. Pain experience during initial alignment with three types of nickel-titanium archwires: a prospective clinical trial. Angle Orthodontist 2015;85(6):1021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Agarwal 2021 {published data only}
- Agarwal SS, Datana S, Kumar MPP, Sharma M, Andhare P. Comparison of efficacy between MBT preadjusted edgewise appliance and clear aligner therapy among class I crowding cases: a randomized controlled trial. Medical Journal Armed Forces India 2021. [DOI: 10.1016/j.mjafi.2021.09.006] [ISSN: 0377-1237] [DOI] [PMC free article] [PubMed] [Google Scholar]
Akyalcin 2007 {published data only}
- Akyalcin S, Hazar S, Guneri P, Gogus S, Erdinc AM. Extraction versus non-extraction: evaluation by digital subtraction radiography. European Journal of Orthodontics 2007;29(6):639-47. [DOI] [PubMed] [Google Scholar]
Alcan 2006 {published data only}
- Alcan T, Ceylanoglu C. Upper midline correction in conjunction with rapid maxillary expansion. American Journal of Orthodontics and Dentofacial Orthopedics 2006;130(5):671-5. [DOI] [PubMed] [Google Scholar]
Almeida 2015 {published data only}
- Valli de Almeida N, Silveira GS, Pereira DM, Mattos CT, Mucha JN. Interproximal wear versus incisors extraction to solve anterior lower crowding: a systematic review. Journal of Orthodontics 2015;20(1):66-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Altug 2005 {published data only}
- Altug H, Bengi AO, Akin E, Karacay S. Dentofacial effects of asymmetric headgear and cervical headgear with removable plate on unilateral molar distalization. Angle Orthodontist 2005;75(4):584-92. [DOI] [PubMed] [Google Scholar]
Angelieri 2008 {published data only}
- Angelieri F, De Almeida RR, Janson G, Castanha Henriques JF, Pinzan A. Comparison of the effects produced by headgear and pendulum appliances followed by fixed orthodontic treatment. European Journal of Orthodontics 2008;30(6):572-9. [DOI] [PubMed] [Google Scholar]
Atik 2018 {published data only}
- Atik E, Akarsu-Guven B, Kocadereli I. Mandibular dental arch changes with active self-ligating brackets combined with different archwires. Nigerian Journal of Clinical Practice 2018;21(5):566-72. [DOI] [PubMed] [Google Scholar]
Atik 2019 {published data only}
- Atik E, Gorucu-Coskuner H, Akarsu-Guven B, Taner T. A comparative assessment of clinical efficiency between premium heat-activated copper nickel-titanium and superelastic nickel-titanium archwires during initial orthodontic alignment in adolescents: a randomized clinical trial. Progress in Orthodontics 2019;20(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bansal 2019 {published data only}
- Bansal M, Sharma R, Kumar D, Gupta A. Effects of mini‐implant facilitated micro‐osteoperforations in alleviating mandibular anterior crowding: a randomized controlled clinical trial. Journal of Orthodontic Science 2019;8(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Battagel 1998 {published data only}
- Battagel J, Ryan A. Spontaneous lower arch changes with and without second molar extractions. American Journal of Orthodontics and Dentofacial Orthodpaedics 1998;113(2):133-43. [DOI] [PubMed] [Google Scholar]
Baumrind 1996 {published data only}
- Baumrind S, Korn EL, Boyd RL, Maxwell R. The decision to extract: part II. Analysis of clinicians' stated reasons for extraction. American Journal of Orthodontics and Dentofacial Orthodpaedics 1996;109(4):393-402. [DOI] [PubMed] [Google Scholar]
Bennett 1999 {published data only}
- Bennett GR, Weinstein M, Borislow AJ. Efficacy of open-bite treatment with the Thera-spoon. Journal of Clinical Orthodontics 1999;33(9):531. [PubMed] [Google Scholar]
Bhasin 2017 {published data only}
- Bhasin V, Singh M, Goutam M, Singh S, Nigam AS, Joshi A. Comparative evaluation of myeloperoxidase enzymatic activity in gingival crevicular fluid of subjects having orthodontic treatment by different aligning arch wires. Journal of Contemporary Dental Practice 2017;18(10):977-80. [DOI] [PubMed] [Google Scholar]
Bhavra 2002 {published data only}
- Bhavra GS. A prospective RCT comparing straight-wire and tip-edge fixed appliance systems. Journal of Orthodontics 2002;29(3):230-6. [Google Scholar]
Bondemark 2005 {published data only}
- Bondemark L, Karlsson I. Extraoral vs intraoral appliance for distal movement of maxillary first molars: a randomized controlled trial. Angle Orthodontist 2005;75(5):699-706. [DOI] [PubMed] [Google Scholar]
Bondemark 2007 {published data only}
- Bondemark L, Holm AK, Hansen K, Axelsson S, Mohlin B, Brattstrom V, et al. Long-term stability of orthodontic treatment and patient satisfaction. A systematic review. Angle Orthodontist 2007;77(1):181-91. [DOI] [PubMed] [Google Scholar]
Caprioglio 2014 {published data only}
- Caprioglio A, Cozzani M, Fontana M. Comparative evaluation of molar distalization therapy with erupted second molar: segmented versus quad pendulum appliance. Progress in Orthodontics 2014;15(49):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Celebi 2019 {published data only}
- Celebi F, Turk T, Bicakci A. Effects of low-level laser therapy and mechanical vibration on orthodontic pain caused by initial archwire. American Journal of Orthodontics and Dentofacial Orthopedics 2019;156:87-93. [DOI] [PubMed] [Google Scholar]
Cerruto 2017 {published data only}
- Cerruto C, Ugolini A, Di Vece L, Doldo T, Caprioglio A, Silvestrini-Biavati A. Cephalometric and dental arch changes to Haas-type rapid maxillary expander anchored to deciduous vs permanent molars: a multicenter, randomized controlled trial. Journal of Orofacial Orthopedics 2017;78(5):385-93. [DOI] [PubMed] [Google Scholar]
CTRI/2018/05/014070 {unpublished data only}
- CTRI/2018/05/014070. A clinical trial to compare the alignment efficiency of two types of nickel titanium archwires in relieving lower anterior crowding. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/05/014070.
CTRI/2018/10/016038 {unpublished data only}
- CTRI/2018/10/016038. Success of two arch wires to relieve irregularity of teeth. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/10/016038 2018.
Dmitrenko 2016 {published data only}
- Dmitrenko M, Pisarenko E. Analysis of orthodontic treatment efficiency in children with dental crowding. Wiadomosci Lekarskie 2016;69(2):252-7. [PubMed] [Google Scholar]
Fan 2009 {published data only}
- Fan CX, Sun R, Wu LP. The effect of first premolar extraction on vertical dimension in skeletal Class I patients. Shanghai Kou Qiang Yi Xue [Shanghai Journal of Stomatology] 2009;18(6):592-5. [PubMed] [Google Scholar]
Feldmann 2008 {published data only}
- Feldmann I, Bondemark L. Anchorage capacity of osseointegrated and conventional anchorage systems: a randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(3):339.e19-28. [DOI] [PubMed] [Google Scholar]
Fleming 2009a {published data only}
Fleming 2009b {published data only}
- Fleming PS, DiBiase AT, Sarri G, Lee RT. Efficiency of mandibular arch alignment with 2 preadjusted edgewise appliances. American Journal of Orthodontics and Dentofacial Orthopedics 2009;135(5):597-602. [DOI] [PubMed] [Google Scholar]
Fleming 2010 {published data only}
- Fleming PS, DiBiase AT, Lee RT. Randomized clinical trial of orthodontic treatment efficiency with self-ligating and conventional fixed orthodontic appliances. American Journal of Orthodontics and Dentofacial Orthopedics 2010;137(6):738-42. [DOI] [PubMed] [Google Scholar]
Germec 2008 {published data only}
- Germec D, Taner TU. Effects of extraction and nonextraction therapy with air-rotor stripping on facial esthetics in postadolescent borderline patients. American Journal of Orthodontics & Dentofacial Orthopedics 2008;133(4):539-49. [DOI] [PubMed] [Google Scholar]
Germec‐Cakan 2010 {published data only}
- Germec-Cakan D, Taner TU, Akan S. Arch-width and perimeter changes in patients with borderline Class I malocclusion treated with extractions or without extractions with air-rotor stripping. American Journal of Orthodontics & Dentofacial Orthopedics 2010;137(6):734.e1-7; discussion 734-5. [DOI] [PubMed] [Google Scholar]
Gibreal 2019 {published data only}
- Gibreal O, Hajeer M, Brad B. Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: a randomized controlled trial. European Journal of Orthodontics 2019;41(2):188-95. [DOI] [PubMed] [Google Scholar]
IRCT2016042427577N1 {unpublished data only}
- IRCT2016042427577N1. Comparison of tooth alignment and pain perception of different sizes of nickle-titanium archwires in the initial phase of fixed orthodontic treatment: randomized clinical trial. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2016042427577N1.
Kaklamanos 2017 {published data only}
- Kaklamanos EG, Mavreas D, Tsalikis L, Karagiannis V, Athanasiou AE. Treatment duration and gingival inflammation in Angle's Class I malocclusion patients treated with the conventional straight-wire method and the Damon technique: a single-centre, randomised clinical trial. Journal of Orthodontics 2017;44(2):75-81. [DOI] [PubMed] [Google Scholar]
Keski‐Nisula 2008a {published data only}
- Keski-Nisula K, Hernesniemi R, Heiskanen M, Keski-Nisula L, Varrela J. Orthodontic intervention in the early mixed dentition: a prospective, controlled study on the effects of the eruption guidance appliance. American Journal of Orthodontics & Dentofacial Orthopedics 2008;133(2):254-60; quiz 328.e2. [DOI] [PubMed] [Google Scholar]
Keski‐Nisula 2008b {published data only}
- Keski-Nisula K, Keski-Nisula L, Salo H, Voipio K, Varrela J. Dentofacial changes after orthodontic intervention with eruption guidance appliance in the early mixed dentition. Angle Orthodontist 2008;78(2):324-31. [DOI] [PubMed] [Google Scholar]
Krishna 2016 {published and unpublished data}
- Krishna NK, Farhan A, Issar R, Subramanian S, Muniyappa MP, Ranjan S, et al. Clinical evaluation of proclination of lower anterior teeth during alignment using a single width bracket - a pilot study. Journal of Clinical and Diagnostic Research 2016;10(6):113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lombardo 2018 {published data only}
- Lombardo L, Arreghini A, Ghislanzoni LT, Siciliani G. Accelerating aligner treatment using low-frequency vibration: a single-centre, randomized controlled clinical trial. European Journal of Orthodontics 2018;41(4):1-10. [Google Scholar]
Mahmoudzadeh 2018 {published data only}
- Mahmoudzadeh M, Farhadian M, Alijani S, Azizi F. Clinical comparison of two initial arch wires (A-NiTi and Heat Activated NiTi) for amount of tooth alignment and perception of pain: a randomized clinical trial. International Orthodontics 2018;16(1):60-72. [DOI] [PubMed] [Google Scholar]
Mateu 2018 {published data only}
- Mateu ME, Benitez-Roge S, Iglesias M, Calabrese D, Lumi M, Solla M, et al. Increased interpremolar development with self-ligating orthodontics. A prospective randomized clinical trial. Acta Odontologica Latinoamericana 2018;31(2):104-9. [PubMed] [Google Scholar]
Miles 2018 (AJO‐DO) {published data only}
- Miles P, Fisher E, Pandis N. Assessment of the rate of premolar extraction space closure in the maxillary arch with the AcceleDent Aura appliance vs no appliance in adolescents: a single-blind randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2018;153:8-14. [DOI] [PubMed] [Google Scholar]
Mittal 2020 {published data only}
- Mittal R, Attri S, Batra P, Sonar S, Sharma K, Raghavan S. Comparison of orthodontic space closure using micro-osteoperforation and passive self-ligating appliances or conventional fixed appliances. Angle Orthodontist 2020;90(5):634-9. [DOI: 10.2319/111119-712.1] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murakami 2016 {published data only}
- Murakamia T, Kawanabeb N, Kataokab T, Hoshijimab M, Komorib H, Fujisawab A, et al. A single-center, open-label, randomized controlled clinical trial to evaluate the efficacy and safety of the indirect bonding technique. Acta Medica Okayama 2016;70(5):413-6. [DOI] [PubMed] [Google Scholar]
Nabbat 2020 {published data only}
- Nabbat S, Yassir Y. A clinical comparison of the effectiveness of two types of orthodontic aligning archwire materials: a multicentre randomized clinical trial. European Journal of Orthodontics 2020;42(6):626–34. [DOI] [PubMed] [Google Scholar]
NCT03645356 {unpublished data only}
- NCT03645356. Comparison between clear aligners and traditional fixed appliances in the treatment of four-premolar-extraction cases. clinicaltrials.gov/show/nct03645356.
NCT03652454 {unpublished data only}
- NCT03652454. The evaluation of the efficiency of micro-osteoperforation. clinicaltrials.gov/show/nct03652454.
NCT04106141 {published data only}
- NCT04106141. Effect of changing the activation frequency of the arch wires on the rate of leveling and alignment in moderate crowding cases. clinicaltrials.gov/show/nct04106141.
Nordstrom 2018 {published data only}
- Nordstrom B, Shoji T, Anderson W, Fields HW, Beck F, Kim D, et al. Comparison of changes in irregularity and transverse width with nickel-titanium and niobium-titanium-tantalum-zirconium archwires during initial orthodontic alignment in adolescents: a double-blind randomized clinical trial. Angle Orthodontist 2018;88(3):348-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pandis 2007 {published data only}
- Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. American Journal of Orthodontics and Dentofacial Orthopaedics 2007;132(2):208-15. [DOI] [PubMed] [Google Scholar]
Pandis 2010b {published data only}
- Pandis N, Polychronopoulou A, Makou M, Eliades T. Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets. European Journal of Orthodontics 2010;32(3):248-53. [DOI] [PubMed] [Google Scholar]
Scott 2008 {published data only}
- Scott P, DiBiase AT, Sherriff M, Cobourne MT. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;134(4):470.e1-8. [DOI] [PubMed] [Google Scholar]
Silva 2012 {published data only}
- Silva RG, Kaieda AK, Paranhos LR, Angelieri F, Torres FC, Scanavini MA. A comparative study between lip bumper and headgear as maxillary molar retainers following distalization. International Journal of Orthodontics (Milwaukee, Wis.) 2012;23(3):29-34. [PubMed] [Google Scholar]
Silvola 2009 {published data only}
- Silvola AS, Arvonen P, Julku J, Lahdesmaki R, Kantomaa T, Pirttiniemi P. Early headgear effects on the eruption pattern of the maxillary canines. Angle Orthodontist 2009;79(3):540-5. [DOI] [PubMed] [Google Scholar]
Soldanova 2012 {published data only}
- Soldanova M, Leseticky O, Komarkova L, Dostalova T, Smutny V, Spidlen M. Effectiveness of treatment of adult patients with the straightwire technique and the lingual two-dimensional appliance. European Journal of Orthodontics 2012;34:674–80. [DOI] [PubMed] [Google Scholar]
Taner 2003 {published data only}
- Taner TU, Yukay F, Pehlivanoglu M, Cakirer B. A comparative analysis of maxillary tooth movement produced by cervical headgear and pend-x appliance. Angle Orthodontist 2003;73(6):686-91. [DOI] [PubMed] [Google Scholar]
Virkkula 2009 {published data only}
- Virkkula T, Kantomaa T, Julku J, Pirttiniemi P. Long-term soft-tissue response to orthodontic treatment with early cervical headgear--a randomized study. American Journal of Orthodontics & Dentofacial Orthopedics 2009;135(5):586-96. [DOI] [PubMed] [Google Scholar]
Wasserman 2009 {published data only}
- Wasserman I. Effects of expansion in class I: evaluation one year follow-up. In: 87th General Session and Exhibition of IADR/AADR/CADR. Vol. Apr 1-4. 2009:927.
West 1995 {published data only}
- West AE, Jones ML, Newcombe RG. Multiflex versus superelastic: a randomized clinical trial of the tooth alignment ability of initial arch wires. American Journal of Orthodontics and Dentofacial Orthopaedics 1995;108(5):464-71. [DOI] [PubMed] [Google Scholar]
Xu 2010 {published data only}
- Xu TM, Zhang X, Oh HS, Boyd RL, Korn EL, Baumrind S. Randomized clinical trial comparing control of maxillary anchorage with 2 retraction techniques. American Journal of Orthodontics & Dentofacial Orthopedics 2010;138(5):544.e1-9; discussion 544-5. [DOI] [PubMed] [Google Scholar]
Yavuz 2018 {published data only}
- Yavuz M, Sunar O, Buyuk S, Kantarci A. Comparison of piezocision and discision methods in orthodontic treatment. Progress in Orthodontics 2018;19(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildirim 2018 {published data only}
- Yildirim K, Saglam-Aydinatay B. Comparative assessment of treatment efficacy and adverse effects during nonextraction orthodontic treatment of Class I malocclusion patients with direct and indirect bonding: a parallel randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2018;154(1):26-34. [DOI] [PubMed] [Google Scholar]
Yu 2008 {published data only}
- Yu YL, Tang GH, Gong FF, Chen LL, Qian YF. A comparison of rapid palatal expansion and Damon appliance on non-extraction correction of dental crowding. Shanghai Kou Qiang Yi Xue [Shanghai Journal of Stomatology] 2008;17(3):237-42. [PubMed] [Google Scholar]
References to studies awaiting assessment
CTRI/2017/08/009333 {published data only (unpublished sought but not used)}
- CTRI/2017/08/009333. Which wire is most efficient in correcting irregularly placed lower front teeth? Conventional nickel titanium or superelastic nickel titanium. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/08/009333 (first received 31 March 2019).
CTRI/2018/04/013037 {unpublished data only}
- CTRI/2018/04/013037. Comparison of changes in tooth position while using ordinary orthodontic bracket and newer generation ceramic brackets. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/04/013037 (first received 4 April 2018).
CTRI/2018/05/014220 {published data only (unpublished sought but not used)}
- CTRI/2018/05/014220. To compare the effect of two different methods of tying braces on the position of front and back teeth. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/05/014220 (first received 31 March 2019).
NCT02996292 {unpublished data only}
- NCT02996292. Assessment of dentoalveolar changes resulting from orthodontic treatment of crowding with self-ligating brackets using CBCT randomized controlled trial. clinicaltrials.gov/show/nct02996292 (first received 19 December 2016).
UMIN000036836 {published data only (unpublished sought but not used)}
- UMIN000036836#. The efficacy of clear aligners. rctportal.niph.go.jp/en/detail?trial_id=UMIN000036836# (first received 1 June 2019).
References to ongoing studies
NCT04347018 {published data only}
- Al-Zainal M. Alignment and discomfort using non-sliding lingual orthodontic technique (BRIUS) and conventional bracket systems: a single-center randomized clinical trial. clinicaltrials.gov/show/NCT04347018 (first received 15 April 2020).
RBR‐9kvw9t {published data only (unpublished sought but not used)}
- RBR-9kvw9t. Evaluation of efficacy and efficiency of a removable esthetic appliance for solving teeth crowding in the childhood: a randomized clinical trial. www.who.int/trialsearch/Trial2.aspx?TrialID=RBR-9kvw9t (first received 4 June 2020).
Additional references
Afzal 2020
- Afzal E, Fida M, Malik D, Irfan S, Gul M. Comparison between conventional and piezocision-assisted orthodontics in relieving anterior crowding: a systematic review and meta-analysis. European Journal of Orthodontics 2020;19(1):1-7. [DOI] [PubMed] [Google Scholar]
Baumgartner 2014
- Baumgartner S, Pandis N, Eliades T. Exploring the publications in three major orthodontic journals: a comparative analysis of two 5-year periods. Angle Orthodontist 2014;84(3):397-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhujel 2014
- Bhujel N, Duggal M, Munyombwe T, Godson J, Day P. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. European Archives of Paediatric Dentistry 2014;15(6):393-400. [DOI] [PubMed] [Google Scholar]
Bhujel 2016
- Bhujel N, Duggal MS, Saini P, Day PF. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. European Archives of Pediatric Dentistry 2016;17(6):423-34. [DOI] [PubMed] [Google Scholar]
Chen 2019
- Chen C, Hsu KC, Marghalani AA, Dhar V, Coll JA. Systematic review and meta-analysis of passive lower lingual arch for resolving mandibular incisor crowding and effects on arch dimension. Pediatric Dentistry 2019;41(1):9-22. [PubMed] [Google Scholar]
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
El‐Angbawi 2015
- El-Angbawi A, McIntyre GT, Fleming PS, Bearn DR. Non-surgical adjunctive interventions for accelerating tooth movement in patients undergoing fixed orthodontic treatment. Cochrane Database of Systematic Reviews 2015, Issue 11. Art. No: CD010887. [DOI: 10.1002/14651858.CD010887.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fleming 2016
- Fleming PS, Strydom H, Katsaros C, MacDonald L, Curatolo M, Fudalej P, et al. Non-pharmacological interventions for alleviating pain during orthodontic treatment. Cochrane Database of Systematic Reviews 2016, Issue 12. Art. No: CD010263. [DOI: 10.1002/14651858.CD010263.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibson 2011
- Gibson R, Harrison J. What are we reading? An analysis of the orthodontic literature 1999 to 2008. American Journal of Orthodontics and Dentofacial Orthopedics 2011;139(5):471-84. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- The GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017), Cochrane, 2017. Available from training.cochrane.org/handbook/PDF/v5.2/chapter-08.
Holmes 1992
- Holmes A. The prevalence of orthodontic treatment need. British Journal of Orthodontics 1992;19(3):177-82. [DOI] [PubMed] [Google Scholar]
Javidi 2017
- Javidi H, Vettore M, Benson PE. Does orthodontic treatment before the age of 18 years improve oral health-related quality of life? A systematic review and meta-analysis. American Journal of Orthodontics and Dentofacial Orthopaedics 2017;151(4):644-55. [DOI] [PubMed] [Google Scholar]
Jung 2010
- Jung M. Evaluation of the effects of malocclusion and orthodontic treatment on self-esteem in an adolescent population. American Journal of Orthodontics and Dentofacial Orthopaedics 2010;138(2):160-6. [DOI] [PubMed] [Google Scholar]
Jung 2015
- Jung M. An evaluation of self-esteem and quality of life in orthodontic patients: effects of crowding and protrusion. Angle Orthodontist 2015;85(5):812-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ke 2019
- Ke Y, Zhu Y, Zhu M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health 2019;19(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2020
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical supplement to chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Li 2021
- Li T, Higgins JP, Deeks JJ editor(s). Chapter 5: Collecting data. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Papageorgiou 2019
- Papageorgiou S, Koletsi D, Eliades T. What evidence exists for myofunctional therapy with prefabricated appliances? A systematic review with meta-analyses of randomised trials. Journal of Orthodontics 2019;1:1-14. [DOI] [PubMed] [Google Scholar]
Proffit 1998
- Proffit WR, Fields HW Jr, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. International Journal of Adult Orthodontics and Orthognathic Surgery 1998;13(2):97-106. [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Journal of Clinical Epidemiology 2010;63(8):834-40. [DOI] [PubMed] [Google Scholar]
Schünemann 2021
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Shaw 1980
- Shaw WC, Addy M, Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dentistry and Oral Epidemiology 1980;8(1):36-45. [DOI] [PubMed] [Google Scholar]
Shaw 1981
- Shaw WC. The influence of children's dentofacial appearance on their social attractiveness as judged by peers and lay adults. American Journal of Orthodontics 1981;79(4):399-415. [DOI] [PubMed] [Google Scholar]
Shaw 1985
- Shaw WC, Rees G, Dawe M, Charles CR. The influence of dentofacial appearance on the social attractiveness of young adults. American Journal of Orthodontics 1985;87(1):21-6. [DOI] [PubMed] [Google Scholar]
Shaw 1991
- Shaw WC, Richmond S, O'Brien KD, Brook P, Stephens CD. Quality control in orthodontics: indices of treatment need and treatment standards. British Dental Journal 1991;170(3):107-12. [DOI] [PubMed] [Google Scholar]
Song 2009
- Song F, O'Meara S, Wilson P, Golder S, Kleijnen J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technology Assessment 2000;4(15):1-55. [PubMed] [Google Scholar]
Tsichlaki 2020
- Tsichlaki A, O'Brien K, Benson PE, Marshman Z, Johal A, Colonio-Salazar FB, Harman NL, Fleming PS. Development of a core outcome set for use in routine orthodontic clinical trials. American Journal of Orthodontics and Dentofacial Orthopedics 2020;158(5):650-660. [DOI: 10.1016/j.ajodo.2020.05.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vieira 2018
- Vieira E, Watanabe B, Pontes L, Mattos J, Maia L, Normando D. The effect of bracket slot size on the effectiveness of orthodontic treatment: a systematic review. Angle Orthodontist 2018;88(1):100-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2018
- Wang Y, Liu C, Jian F, McIntyre GT, Millett DT, Hickman J, Lai W. Initial arch wires used in orthodontic treatment with fixed appliances. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No: CD007859. [DOI: 10.1002/14651858.CD007859.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wazwaz 2021
- Wazwaz F, Seehra J, Carpenter GH, Ireland AJ, Papageorgiou SN, Cobourne MT. Duration of tooth alignment with fixed appliances: a systematic review and meta-analysis. American Journal of Orthodontics and Dentofacial Orthopedics 16 November 2021 [Epub ahead of print];S0889-5406(21):00560-6. [DOI: 10.1016/j.ajodo.2021.06.016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yu 2013
- Yu Y, Sun J, Lai W, Wu T, Koshy S, Shi Z. Interventions for managing relapse of the lower front teeth after orthodontic treatment. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No: CD008734. [DOI: 10.1002/14651858.CD008734.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Harrison 2002
- Harrison JE, Scholey J, Worthington HV, Bickley S, O'Brien KD, Shaw BC. Orthodontic treatment for crowded teeth in children. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No: CD003453. [DOI: 10.1002/14651858.CD003453] [DOI] [PMC free article] [PubMed] [Google Scholar]


