Abstract
The present study aimed to compare psychological symptoms and coping strategies in 1480 preschoolers, schoolchildren, and adolescents during home confinement due to COVID-19. We enrolled parents from Italy, Portugal, and Spain who completed a survey between the second and fourth week of lockdown. The results showed that preschoolers displayed more sleeping difficulties, temper tantrums, and dependency while adolescents' reactions were more related to COVID-19 worries and uncertainty. Schoolchildren showed more difficulty in concentrating. Adolescent girls showed higher anxiety levels than schoolchildren boys. Schoolchildren relied more on emotion-oriented strategies, which were linked to increased internalizing and externalizing symptoms in all ages. Task-oriented strategies, regardless of the child's age, work best to cope with stress. Our findings provide information for professionals and parents about children's most common and adaptive coping strategies according to age. Furthermore, they contribute to the early detection of long-term psychological maladjustment in children.
Keywords: COVID-19, Quarantine, Psychological symptoms, Coping strategies, Children, Adolescents
The coronavirus outbreak (COVID-19) was declared a Public Health Emergency of International Concern on January 30, 2020, as the virus spread rapidly across many countries worldwide. In response to the growing number of COVID-19 positive cases, many countries implemented urgent measures such as mandatory quarantine to help contain the spread. Although evidence suggested that children could contract COVID-19, very few developed severe symptoms; however, the isolation brought about by contact with others with COVID-19, and the disruption to their daily lives put children at a higher risk of psychological stress and mental health problems (Novins et al., 2020; Orben, Tomova, & Blakemore, 2020).
In the past, studies on the effects of pandemics such as SARS and H1N1 on children focused on the long-term effects, such as post-traumatic stress disorder (Sprang & Silman, 2013). These studies showed that the psychological impacts of prolonged stressful events, such as social isolation and high uncertainty, caused the most distress in children (Silverman & La Greca, 2002). During the current COVID-19 pandemic, recent empirical studies have investigated the coping strategies employed by children and adolescents or the psychological impacts this social isolation brought. In one study from Hubei province, a region that was particularly affected by COVID-19, 22.6% of school-age children reported symptoms of depression, while 19.8% reported anxiety symptoms (Xie et al., 2020). In a similar study from Italy and Spain, 85.7% of Italian and Spanish parents described changes in their children's emotional state and behaviors (aged 3–18 years) during the first weeks of lockdown due to COVID-19 (Orgilés, Morales, Delvecchio, Mazzeschi, & Espada, 2020). These parents described symptoms such as difficulty concentrating, boredom, irritability, restlessness, nervousness, feelings of loneliness, and being more uneasy and more worried than usual. The present study aimed to compare psychological symptoms and coping strategies in preschoolers, schoolchildren, and adolescents during the first weeks of home confinement due to COVID-19.
Existing literature on children's reactions to other natural disasters, such as earthquakes and floods, suggested that preschoolers show less psychological distress and exhibit fewer cognitive problems than older children (Salmon & Bryant, 2002). However, the results were often contradictory, as other findings suggested that preschoolers suffer from a high incidence of generalized or specific fears, including separation anxiety, loss of language skills, and exhibit behavioral problems (e.g., temper tantrums and aggression), dependency, irritability, sleep problems, and specific regressive behaviors (e.g., thumb sucking, bedwetting, and tics) (Baggerly & Exum, 2007; Corrarino, 2008; Dyregrov & Yule, 2006).
As children get older and start school, they show more overall psychological distress than preschoolers but less than adolescents, with common reactions such as problems with sleeping, eating, and behavior. Adolescent symptoms include depression, anxiety, belligerence, and pessimistic views about the future (Korol, Green, & Gleser, 1999). However, few studies exist on adolescents and their psychological reactions to disasters. This is likely due to their more sophisticated cognitive understanding of situations and consequences, leading to them being considered more adult-like than child-like in their responses (Eth & Pynoos, 1985).
COVID-19 psychological impact: The effect of age and sex
A systemic review of the impact of COVID-19 on mental health showed the extent to which the literature either focused only on one age group (i.e., preschoolers or adolescents), compared children to college students or adults, and included only small sample sizes, which prevented conclusions from being generalized (Nearchou, Flinn, Niland, Subramaniam, & Hennessy, 2020). Another pilot study on a Chinese population compared preschool and older children during the early weeks of the COVID-19 pandemic and found that preschoolers were more dependent on their parents and had more fear of infection, whereas older children (6–18 years) were more distracted and posed persistent questions about COVID-19 (Jiao et al., 2020). Nevertheless, any findings should be interpreted with caution since all previous studies have considered children and adolescents as unique samples, whereas the effects of the pandemic may have different impacts between the age groups described. For example, schoolchildren may have faced particular difficulties dealing with remote learning and remote friendships (as they cannot access learning independently or enjoy play activities when not face-to-face) than adolescents, generating fear, frustration, and sadness. On the other hand, adolescents might be more challenged by the restrictions imposed by the lockdown, which impact their need for autonomy and social interaction (Waite et al., 2021), causing anger.
The impact of the pandemic will likely differ depending on other risk factors, such as sex. Generally speaking, school-age boys are more prone to develop psychological instabilities (most commonly displayed as behavioral problems) than girls. In contrast, in adolescence, boys and girls are equally likely to develop psychological issues, and girls have shown higher rates of emotional disorders (Davis et al., 2018). Overall, most of the literature on the effects of the pandemic focused on internalizing symptoms, with some studies showing that girls were struggling more (i.e., Chen et al., 2020; Ellis, Dumas, & Forbes, 2020; Zhou et al., 2020), and others reporting that boys struggled more (Francisco et al., 2020; Ravens-Sieberer et al., 2021). Conversely, other studies found no differences between the sexes (Liu, Liu, & Liu, 2020; Xie et al., 2020). The confounding effects described in these studies are likely due to the age groups investigated and the choice of reporters. For example, the studies reporting more difficulties for girls referred to adolescents' self-rated questionnaires (Chen et al., 2020; Ellis et al., 2020; Zhou et al., 2020), whereas those for boys were parent reports for children aged 3–18 (Francisco et al., 2020) and 7–17 (Ravens-Sieberer et al., 2021). Interestingly, the self-reports completed by primary school children revealed no significant differences. Moreover, Francisco et al. (2020) showed that being male was a significant predictor of behavioral difficulties and changes in eating patterns, and this agreed with a previous study in which boys experienced more mental health problems, increased hyperactivity, and more significant behavioral problems (Ravens-Sieberer et al., 2021).
The role of coping strategies
While most children start to behave normally again after stressful events, others are more susceptible to developing psychological issues (Orgilés et al., 2021), and their capability to overcome problems, and the strategies used for coping with these experiences will help us to understand why some children cope better than others. Coping as a strategy has been described as a conscious, deliberate attempt to regulate emotion, cognition, behavior, and the environment when facing stressful events (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001). There are three general dimensions of coping that encompass the overarching features of response to stress in childhood and adolescence: task-oriented coping (i.e., responses such as finding solutions and taking action to reduce or eliminate the stressor), emotion-oriented coping (i.e., the use of emotions to buffer stress and seeking support from others), and avoidant coping strategies (responses that disengage, deny, move away, or remove the individual from the stressor or the emotional and cognitive states related to it) (Skinner & Zimmer-Gembeck, 2016; VanMeter, Handley, & Cicchetti, 2020).
Coping strategies also depend on the nature of the stressors and the individual's developmental phase (Zimmer-Gembeck & Skinner, 2011). While some younger children with less developed comprehensive strategies may be more vulnerable when having to cope with a high number of stressors (Fields & Prinz, 1997), children of all ages have shown low-to-moderate consistency in their coping strategies across different types of stressors (Donaldson, Prinstein, Danovsky, & Spirito, 2000; Griffiths, Ravindran, Merali, & Anisman, 2000).
It was seen that preschoolers relied more on avoidance-oriented strategies than older children (Bernzweig, Eisenberg, & Fabes, 1993; Peterson, Harbeck, Chaney, & Farmer, 1990), whereas task-oriented coping strategies predominated in primary and junior school children (age 8–14) (Compas, Malcarne, & Fondacaro, 1988; Hampel & Petermann, 2005). In these preschoolers, the increased use of avoidance-oriented strategies was linked to reduced psychological distress in the short-term (Peterson, 1989), and a review of 41 relevant articles showed that task-oriented coping strategies were mainly learned during early childhood but changed qualitatively over time, with their use increasing with age (Skinner & Zimmer-Gembeck, 2016). As children age, emotion-focused coping strategies tend to come into play more, and these include role-play as a means to cope with stress. The core dimensions of stress management strategies include seeking support and emotion-expression (Lazarus & Folkman, 1984), with support-seeking being more likely to be used by preschoolers and talking about emotions occurring more frequently in older children (Skinner & Zimmer-Gembeck, 2016).
Some studies have also linked coping strategies to children's and adolescents' psychological well-being (MacIntosh & Whiffen, 2005; Orgilés, Morales, et al., 2021; Skinner & Zimmer-Gembeck, 2007; VanMeter et al., 2020), in which task-oriented strategies were linked to positive outcomes, and emotion-focused and avoidance-oriented strategies were linked to increased internalizing and externalizing symptoms, especially in adolescents (Carlo, Crockett, Wolff, & Beal, 2012; Delvecchio, Salcuni, Lis, Germani, & Di Riso, 2019; Fields & Prinz, 1997; VanMeter et al., 2020). A recent study based on a large sample of adults from the UK reported that all three types of coping strategies were significantly related to higher anxiety and depressive symptoms at the beginning of the lockdown (Fluharty, Bu, Steptoe, & Fancourt, 2021).
Overall, the pandemic resulted in children and adolescents having to face several psychological adjustment challenges (e.g., Ford, John, & Gunnell, 2021; Jiao et al., 2020; Meherali et al., 2021; Nearchou et al., 2020; Orgilés, Morales, et al., 2020). However, exactly how the different age groups cope remains unclear, and therefore, as previously stated, this study investigated the psychological symptoms experienced during home confinement due to COVID-19 and the coping strategies utilized by children across three age groups.
Study hypotheses
Due to the ongoing nature of the current pandemic, data is still in progress, and, therefore, our hypotheses are also based on past research on the responses to natural disasters and/or in regions with widespread illness. First, we analyzed differences in children's psychological symptoms by age group, including preschoolers (3–5 years), schoolchildren (6–12 years), and adolescents (13–18 years). We expected preschoolers to be more dependent on their parents, more irritable, and show increased sleep problems than older children (Baggerly & Exum, 2007; Corrarino, 2008; Jiao et al., 2020). We also anticipated that parents of schoolchildren would report greater cognitive and behavioral difficulties, such as difficulty concentrating, irritability, and arguing with family members (Nearchou et al., 2020, Orgilés, Morales, et al., 2020; Romero et al., 2020). We also hypothesized that adolescents would be more anxious, depressed, and aggressive (Dogan-Ates, 2010; Jiao et al., 2020) but that both preschoolers (Jiao et al., 2020) and adolescents (Tang et al., 2021) would fear COVID-19 infection.
We also assessed differences in children's coping strategies by age, where we hypothesized that preschoolers would show higher avoidance-oriented strategies than older children, who would rely more on task-oriented and emotion-focused strategies (Bernzweig et al., 1993; Fields & Prinz, 1997). Finally, we investigated the relationship between children's psychological symptoms and coping strategies regarding age and sex. We hypothesized that task-oriented strategies would be linked to more positive internalizing and externalizing outcomes for all age groups, whereas emotion-focused and avoidance-oriented strategies would correlate to more negative outcomes (Delvecchio et al., 2019; VanMeter et al., 2020). However, we did not expect preschoolers to show increased adverse outcomes due to avoidance-oriented strategies because, in this age group, avoidance-oriented strategies were hypothesized to be linked to reduced psychological maladjustment (Peterson, 1989). Interestingly, sex was hypothesized to be a predictor of changes in eating patterns, with boys scoring higher than girls (Francisco et al., 2020; Ravens-Sieberer et al., 2021), but adolescent girls were expected to experience higher anxiety than boys (Chen et al., 2020; Zhou et al., 2020). As a result, we hypothesized that boys would display more changes in their behavior and greater use of avoidance-oriented strategies (Eschenbeck, Kohlmann, & Lohaus, 2007; Francisco et al., 2020).
Materials and methods
Participants
Table 1 lists the sample characteristics and differences in the sociodemographic variables according to age group. We recruited parents of 1480 children from 94 Italian (48.1%), 84 Spanish (29.1%) and 94 Portuguese (22.8%) cities to participate in the project. Parents were allowed to complete measures for multiple children. They were required to fill in a new form for each child.
Table 1.
Sample characteristics and differences among children's age groups.
| Total (N = 1480) |
Preschoolers (1) (n = 385) | Schoolchildren (2) (n = 739) | Adolescents (3) (n = 356) |
Testa | Effect sizeb | Post -hocc |
|
|---|---|---|---|---|---|---|---|
| Parents | |||||||
| Females, N (%) | 1299 (87.8) | 354 (91.9) | 647 (87.6) | 298 (83.7) | 11.76** | 0.09 | 1 > 3 |
| Age, M (SD) | 42.26 (5.92) | 37.74 (4.61) | 42.40 (5.09) | 46.84 (5.08) | 477.15*** | 0.22 | 2 > 1 3 > 1 3 > 2 |
| Country | 26.01*** | 0.09 | |||||
| Italy | 712 (48.1) | 187 (48.6) | 333 (45) | 192 (53.9) | |||
| Spain | 431 (29.1) | 112 (29.1) | 251 (34) | 68 (19.1) | 2 > 3 | ||
| Portugal | 337 (22.8) | 86 (22.3) | 155 (21) | 96 (27) | |||
| Marital status | 11.02** | 0.10 | |||||
| Married | 1292 (87.3) | 349 (90.6) | 651 (88.1) | 292 (82) | 1 > 3 | ||
| Single | 183 (12.4) | 34 (8.9) | 87 (11.8) | 62 (17.4) | 3 > 1 | ||
| Others | 5 (0.3) | 2 (0.5) | 1 (0.1) | 2 (0.6) | – | ||
| Monthly family income (euros) | 8.71 | - - | |||||
| Up to 999 | 87 (6.6) | 26 (7.3) | 43 (6.5) | 18 (6) | |||
| Between 1000 and 1999 | 372 (28.2) | 103 (29.1) | 182 (27.4) | 87 (29.2) | |||
| Between 2000 and 2999 | 417 (31.8) | 118 (33.3) | 221 (33.2) | 78 (26.2) | |||
| Between 3000 and 4999 | 343 (26) | 86 (24.3) | 170 (25.5) | 87 (29.2) | |||
| 5000 or more | 98 (7.4) | 21 (6) | 49 (7.4) | 28 (9.4) | |||
| The house where you live has, N (%) | 3.83 | – | |||||
| Only windows | 158 (10.7) | 39 (10.1) | 82 (11.1) | 37 (10.4) | |||
| Garden | 559 (37.8) | 144 (37.4) | 274 (37.1) | 141 (39.6) | |||
| Terrace | 303 (20.5) | 77 (20) | 161 (21.8) | 65 (18.3) | |||
| Balcony | 416 (28) | 112 (29.1) | 199 (26.9) | 105 (29.5) | |||
| Another exit | 44 (3) | 13 (3.4) | 23 (3.1) | 8 (2.2) | |||
| People who live in my house during quarantine, N (%) | 1.95 | – | |||||
| They do not leave the house unless they have to buy groceries or other allowed activities | 934 (63.1) | 232 (60.3) | 471 (63.7) | 231 (64.9) | |||
| One or both parents still work outside the home | 546 (36.9) | 153 (39.7) | 268 (36.3) | 125 (35.1) | |||
| How many people live in at home during quarantine, M (SD) | 3.94 (0.94) | 3.87 (0.87) | 3.96 (0.91) | 4.01 (1.07) | 7.10* | 0.26 | 3 > 1 |
| Square meters home, M (SD) | 131.04 (67.70) | 119.70 (60.98) | 132.16 (67.97) |
140.93 (72.28) | 28.03*** | 0.23 | 2 > 1 3 > 1 3 > 2 |
| Children | |||||||
| Females, N (%) | 699 (47.2) | 193 (50.1) | 340 (46) | 166 (46.6) | 1.79 | – | |
| Physical or psychological problems, N (%) | 174 (11.8) | 30 (7.8) | 105 (14.2) | 39 (11) | 10.33** | 0.08 | 2 > 1 |
| Receive psychological treatment, N (%) | 128 (8.6) | 23 (6.0) | 74 (10.0) | 31 (8.7) | 1.90 | – | |
Note. M = Mean; SD = Standard Deviation.
*p < .05, **p < .01, ***p < .001.
- No post-hoc test was conducted.
Chi-square test (χ2) for categorical variables and Kruskal-Wallis (χ2) for continuous variables.
Effect size = Cramer's V for multi-categorical variables and Epsilon-squared for continuous variables.
Bonferroni correction applied to p values was used to reduce the risk of type I errors post hoc analysis of a chi-squared test.
At the time of data collection (between March and April 2020), Italy and Spain were two of the most affected EU countries in terms of morbidity and mortality (European Centre for Disease Prevention and Control, 2020). Mandatory quarantine to contain the spread of the virus was implemented in those countries (Francisco et al., 2020). Shutdown orders included the following measures: staying at home, restricted movement of the population except for necessities, and social distancing. Travel to districts outside of their own was forbidden. All non-essential commercial and retail businesses were closed. Children were banned from going outside for three (in Italy) and six (in Spain) weeks. Portugal, where voluntary quarantine was put in place, showed a considerable low number of infections and deaths over the same period. Schools across Italy, Portugal and Spain were closed.
Most participants were mothers of children aged 3–18 (M age = 9.15, SD = 4.27; 47.2% female). The sample included 385 preschoolers (3–5 years old; M age = 4.04, SD = 0.82), 739 schoolchildren (6–12 years old; M age = 8.91, SD = 1.94) and 356 adolescents (13–18 years old; M age = 15.20, SD = 1.62). Most of the children were not diagnosed with any physical or psychological problems (88.2%) before COVID-19. Schoolchildren reportedly showed significantly more physical or psychological problems than preschoolers.
The preschoolers' parents were the youngest (M age = 37.74, SD = 4.61), followed by those of the schoolchildren (M age = 37.74, SD = 4.61), and the adolescents (M age = 46.84, SD = 5.08). There were more married couples of the preschoolers than adolescents. However, the reverse was true for single parents. Most parents were married with a monthly family income between 2000 and 4999 euros (57.8%), representing the middle-class. Parents of adolescents reported to live with a higher number of people than parents of preschoolers. The latter were the ones with the lowest number of children living at home.
Procedures
Due to quarantine restrictions, participation in the study was solicited through social media groups, using a snowball sampling strategy. Before participation, parents were required to read and approve the informed consent, which described the study purposes and participant's rights. After approval, the participants were asked to complete an online survey to assess the psychosocial reactions during home confinement in the children and parents. It was emphasized that participation was anonymous, voluntary and that all participants could withdraw at any time. Confidentiality was ensured, and no incentive reward was given.
Data were collected for 15 days, starting from 15 days after lockdown (i.e., Italy from March 24 to April 7; Portugal and Spain from March 28 to April 11). Inclusion criteria for participation were (a) age 18 or above, (b) having one or more children between the ages of 3 and 18, and (c) living in Italy, Portugal or Spain. The study was approved by the Ethics Board Committee of the authors' institution.
Measures
Child psychological symptoms
Parents completed the Impact Scale of COVID-19 and lockdown on children and adolescents (Orgilés, Morales, et al., 2020). It includes 31 items relating to the general question, “During the past few days, compared to before lockdown, have you noticed that your child...”. Items were rated on a Likert scale ranging from 1 to 5 (1 = much less than before quarantine; 2 = slightly less than before quarantine; 3 = same as before quarantine; 4 = slightly more than before quarantine; and 5 = much more than before quarantine). The responses were categorized into six domains: 1. Anxiety/Activation (10 items; ordinal α = 0.90); 2. Mood (6 items; ordinal α = 0.84); 3. Sleep (5 items; ordinal α = 0.89); 4. Behavioral (6 items; ordinal α = 0.86); 5. Eating (2 items; ordinal α = 0.80); and 6. Cognitive alterations (2 items; ordinal α = 0.75) (see Table 2 ). The Internal Consistency for the total scale was adequate (ordinal α = 0.75).
Table 2.
Primary caregivers' perception of effects on their children's anxiety, mood, sleep, behavioral alterations, feeding and cognitive alterations during home confinement, and differences among preschoolers, schoolchildren and adolescents.
| Total (N = 1480) |
Preschoolers (1) (n = 385) |
Schoolchildren (2) (n = 739) |
Adolescents (3) (n = 356) |
χ2 Test |
Effect sizea |
Post-hocb |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N1 | % | n1 | % | n1 | % | n1 | % | ||||
| Anxiety/Activation | |||||||||||
| My child is worried | 495 | 33.4 | 76 | 19.7 | 268 | 36.3 | 151 | 42.4 | 47.99*** | 0.18 | 3 > 1 |
| My child is anxious | 446 | 30.1 | 113 | 29.4 | 230 | 31.1 | 103 | 28.9 | 0.70 | – | |
| My child is nervous | 543 | 36.7 | 161 | 41.8 | 277 | 37.5 | 105 | 29.5 | 12.49** | 0.09 | 1 > 3 |
| My child worries when one of us leaves the house | 350 | 23.6 | 77 | 20.0 | 185 | 25.0 | 88 | 24.7 | 3.85 | – | |
| My child is restless | 563 | 38.0 | 171 | 44.4 | 300 | 40.6 | 92 | 25.8 | 31.15*** | 0.14 | 1 > 3 |
| My child is afraid of COVID-19 infection | 403 | 27.2 | 56 | 14.5 | 224 | 30.3 | 123 | 34.6 | 44.43*** | 0.17 | 3 > 2 3 > 1 2 > 1 |
| My child is uneasy | 501 | 33.9 | 144 | 37.4 | 264 | 35.7 | 93 | 26.1 | 12.82** | 0.09 | |
| My child is easily alarmed | 214 | 14.5 | 42 | 10.9 | 122 | 16.5 | 50 | 14.0 | 6.48* | 0.06 | 2 > 1c |
| My child has physical complaints (headache, stomach ache ...) | 193 | 13.0 | 50 | 13.0 | 107 | 14.5 | 36 | 10.1 | 4.04 | – | |
| My child asks about death | 202 | 13.6 | 54 | 14.0 | 123 | 16.6 | 25 | 7.0 | 18.93*** | 0.11 | 2 > 3 |
| Mood | |||||||||||
| My child is sad | 351 | 23.7 | 80 | 20.8 | 177 | 24.0 | 94 | 26.4 | 3.28 | – | |
| My child is reluctant | 345 | 23.3 | 85 | 22.1 | 172 | 23.3 | 88 | 24.7 | 0.72 | – | |
| My child feels lonely | 491 | 33.2 | 120 | 31.2 | 242 | 32.7 | 129 | 36.2 | 2.26 | – | |
| My child cries easily | 261 | 17.6 | 107 | 27.8 | 133 | 18.0 | 21 | 5.9 | 61.17*** | 0.20 | 1 > 3 |
| My child feels frustrated | 328 | 22.2 | 74 | 19.2 | 182 | 24.6 | 72 | 20.2 | 5.31 | – | |
| My child is bored | 772 | 52.2 | 196 | 50.9 | 395 | 53.5 | 181 | 50.8 | 0.98 | – | |
| Sleep | |||||||||||
| My child wakes up frequently | 180 | 12.2 | 68 | 17.7 | 83 | 11.2 | 29 | 8.1 | 16.87*** | 0.10 | 1 > 3 |
| My child sleeps little | 189 | 12.8 | 63 | 16.4 | 80 | 10.8 | 46 | 12.9 | 6.97* | 0.07 | 1 > 2c |
| My child is afraid to sleep alone | 253 | 17.1 | 103 | 26.8 | 137 | 18.5 | 13 | 3.7 | 71.82*** | 0.22 | 1 > 3 |
| My child has nightmares | 169 | 11.4 | 59 | 15.3 | 90 | 12.2 | 20 | 5.6 | 18.07*** | 0.11 | 1 > 3 |
| My child has sleeping difficulties | 249 | 16.8 | 79 | 20.5 | 133 | 18.0 | 37 | 10.4 | 15.00** | 0.10 | 1 > 3 |
| Behavioral alterations | |||||||||||
| My child argues with the rest of the family | 447 | 30.2 | 116 | 30.1 | 242 | 32.7 | 89 | 25.0 | 6.84* | 0.06 | 2 > 3c |
| My child is irritable | 598 | 40.4 | 163 | 42.3 | 305 | 41.3 | 130 | 36.5 | 3.06 | – | |
| My child has behavioral problems | 246 | 16.6 | 77 | 20.0 | 134 | 18.1 | 35 | 9.8 | 16.23*** | 0.10 | 1 > 3 |
| My child is angry | 388 | 26.2 | 114 | 29.6 | 197 | 26.7 | 77 | 21.6 | 6.24* | 0.06 | 1 > 3c |
| My child is very quiet | 159 | 10.7 | 37 | 9.6 | 63 | 8.5 | 59 | 16.6 | 16.92*** | 0.10 | 3 > 2 |
| My child is very dependent on us | 394 | 26.6 | 148 | 38.4 | 211 | 28.6 | 35 | 9.8 | 80.32*** | 0.23 | 1 > 3 |
| Eating | |||||||||||
| My child eats a lot | 343 | 23.2 | 86 | 22.3 | 178 | 24.1 | 79 | 22.2 | 0.69 | – | |
| My child has no appetite | 138 | 9.3 | 36 | 9.4 | 69 | 9.3 | 33 | 9.3 | 0.01 | – | |
| Cognitive alterations | |||||||||||
| My child is very indecisive | 173 | 11.7 | 44 | 11.4 | 92 | 12.4 | 37 | 10.4 | 1.01 | – | |
| My child has difficulty concentrating | 353 | 23.9 | 71 | 18.4 | 211 | 28.6 | 71 | 19.9 | 18.18*** | 0.11 | 2 > 1 |
Note. *p < .05, **p < .01, ***p < .001.
- No post-hoc test was conducted.
Children whose mental health has worsened during quarantine.
Effect size = Cramer's V.
Bonferroni correction applied to p values was used to reduce the risk of type I errors post hoc analysis of a chi-square test.
Unadjusted p-value for post hoc analysis of a chi-square test.
Child coping strategies-COVID-19
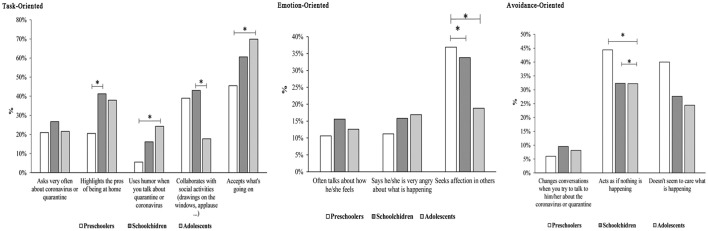
Child coping strategies were assessed through Child Coping Strategies-COVID-19 (Orgilés, Morales, et al., 2021), which includes 11 questions leading to three dimensions as suggested by Parker and Endler (1992): task-, emotion-, and avoidance-oriented strategies. Items were designed to capture the specificity of the COVID-19 context. They required binary “yes-no” responses (see Fig. 1 ) and were summed into Task-Oriented (5 items; ordinal α = 0.47); Emotion-Oriented (3 items; ordinal α = 0.50); and Avoidance-Oriented strategies (3 items; ordinal α = 0.49). Preliminary results on the structural validity of the Child Coping Strategies-COVID-19 in a Spanish sample showed adequate fit for the three-factor structure of the scale (Morales, Melero, Espada, & Orgilés, 2022).
Fig. 1.
Coping strategies among preschoolers, schoolchildren, and adolescents. Responses were yes/no binary, and the axis is % reported yes.
Sociodemographics
Table 1 lists the sociodemographic data for parents and children and questions about housing conditions (e.g., square meters, outdoor exits, number of people living at home).
Data analyses
The sociodemographic characteristics were examined using means and standard deviations for quantitative variables and proportions and percentages for categorical variables. To detect changes that occurred during the quarantine more easily, scores referring to the parents' perceptions of their children's symptoms were converted into dichotomous variables. Parents who indicated that their children had slightly more (rating scale = 4) and much more (rating scale = 5) of each symptom during quarantine (compared to before) were assigned to a new category called “children who have worsened during quarantine” and coded as 1. The rest were coded as 0. The children's ages were split into three groups to compare developmental differences: preschoolers (3–5 years old), schoolchildren (6–12 years old), and adolescents (13–18 years old).
We performed non-parametric tests for non-normally distributed data using the Kruskal–Wallis test to examine differences in young people's reactions during lockdown due to COVID-19. Epsilon-squared [ε2] was used to measure the effect size. Epsilon-squared was interpreted as follows: 0.01 to <0.08 (small), 0.08 to <0.26 (medium), and ≥ 0.26 (large). We used a chi-square test (χ 2) with Cramer's V to measure the effect size to assess differences at the item-level (e.g., psychological symptoms −31 tests were run- and coping strategies - 11 tests were run-) among the three age groups. Cramer's V was interpreted as follows: > 0.25 (very strong), > 0.15 (strong), > 0.10 (moderate), > 0.05 (weak), and > 0 (none or very weak) (Akoglu, 2018). Due to the high number of comparisons, a family-wise error rate (i.e., Bonferroni correction) was applied to control for type I errors (Armstrong, 2014). Adjusted residuals (post-hoc method) were calculated once the multi-group comparison was found to be significant at p < .05 (Beasley & Schumacker, 1995).
Spearman's coefficient was calculated to assess correlations between the children's symptoms and coping strategies. Correlation effect sizes were interpreted according to Cohen (1992), with correlation coefficients of 0.10, 0.30, and 0.50 representing low, medium, and high effect sizes, respectively. Finally, we performed multivariate analyses by generalized linear (GENLIN) modeling. For each group of symptoms (anxiety symptoms, mood symptoms, behavioral problems, changes in sleep patterns, changes in eating patterns, and cognitive alterations), we used GENLIN modeling to investigate differences by age (1 = 3–5 years old, 2 = 6–12 years old, and 3 = 13–18 years old), child's sex (0 = male and 1 = female) and coping strategies (task-, emotion-, and avoidance-oriented strategies). When the age and sex were statistically significant, the interaction was explored for each model. A total of 6 tests, one for each group of symptoms were run. The data was analyzed using SPSS 26 for Mac.
Results
Psychological symptoms during the lockdown in preschoolers, schoolchildren, and adolescents
We performed Kruskal–Wallis tests to analyze the differences in children's symptoms by age. Parents reported that schoolchildren were significantly more anxious than adolescents (χ 2 = 6.71, p ≤ 0.05, ε2 = 0.005; preschoolers: M = 2.45, SD = 2.34; schoolchildren: M = 2.84, SD = 2.65; adolescents: M = 2.43, SD = 2.44) and experienced more cognitive difficulties than preschoolers (χ 2 = 14.96, p ≤ 0.01, ε2 = 0.01; preschoolers: M = 0.29, SD = 0.57; schoolchildren: M = 0.41, SD = 0.62; adolescents: M = 0.30, SD = 0.57). Results showed that quarantine had the highest impact on preschoolers' sleep habits (M = 0.96, SD = 1.34), followed by schoolchildren (M = 0.70, SD = 1.23) and adolescents (M = 0.40, SD = 0.90) (χ 2 = 44.77, p ≤ 0.001, ε2 = 0.03). The latter showed the lowest behavioral alterations (χ 2 = 19.74, p ≤ 0.001, ε2 = 0.01; preschoolers: M = 1.70, SD = 1.67; schoolchildren: M = 1.55, SD = 1.63; adolescents: M = 1.19, SD = 1.46). No significant differences were found for mood and eating.
Table 2 lists the caregivers' perceptions of changes observed in their children at the item level. The chi-square tests showed that schoolchildren were more preoccupied with death than adolescents, more easily alarmed and had greater concentration problems than preschoolers. Preschoolers were considered more nervous, restless, dependent on parents, and cried more readily than adolescents, who were more worried and afraid of COVID-19 infection but showed fewer behavioral problems and anger than preschoolers.
Coping strategies used during the lockdown in preschoolers, schoolchildren, and adolescents
We showed that preschoolers used more avoidance-oriented strategies (χ 2 = 25.17, p ≤ 0.001, ε2 = 0.01; preschoolers: M = 0.90, SD = 0.83; schoolchildren: M = 0.69, SD = 0.83; adolescents: M = 0.64, SD = 0.80) and fewer task-oriented strategies than schoolchildren and adolescents (χ 2 = 64.96, p ≤ 0.001, ε2 = 0.03; preschoolers: M = 1.31, SD = 1.11; schoolchildren: M = 1.87, SD = 1.14; adolescents: M = 1.71, SD = 1.00) to cope with COVID-19. The use of emotion-oriented strategies was higher in schoolchildren than adolescents (χ 2 = 11.79, p ≤ 0.01, ε2 = 0.006; preschoolers: M = 0.58, SD = 0.71; schoolchildren: M = 0.65, SD = 0.79; adolescents: M = 0.48, SD = 0.70).
Chi-square tests with Cramer's V focusing on coping strategies revealed that preschoolers were less likely to highlight the benefits of staying at home than schoolchildren (χ 2 = 49.55, p ≤ 0.001, Cramer's V = 0.18), were less likely to accept the situation (χ 2 = 47.59, p ≤ 0.001, Cramer's V = 0.17), and were less likely to use humor while talking about the quarantine or coronavirus (χ 2 = 50.79, p ≤ 0.001, Cramer's V = 0.18) than adolescents. They acted as if nothing was happening (χ 2 = 18.18, p ≤ 0.001, Cramer's V = 0.11) or appeared not to care about what was happening (χ 2 = 25.56, p ≤ 0.001, Cramer's V = 0.13) more frequently than schoolchildren and adolescents. Schoolchildren collaborated more than adolescents in social activities (χ 2 = 69.17, p ≤ 0.001, Cramer's V = 0.21). Adolescents sought less affection from others (χ 2 = 33.67, p ≤ 0.001, Cramer's V = 0.15) than preschoolers and schoolchildren. Fig. 1 shows the coping strategies by age.
The relationship between psychological symptoms and coping strategies during the lockdown in preschoolers, schoolchildren, and adolescents
We conducted Spearman correlations to discover if task-oriented and avoidance-oriented strategies were linked to more positive internalizing and externalizing outcomes or whether emotion-focused strategies were correlated with more negative outcomes (Table 3 ). Several significant correlations emerged, although most displayed a low effect size.
Table 3.
Correlations with confidence intervals between psychological symptoms and coping strategies among the three groups: 3–5 years old, 6–12 years old, and 13–18 years old.
| Anxiety | Mood | Sleep | Behav. alterations | Eating | Cog. alterations | |
|---|---|---|---|---|---|---|
| 3–5 years old | ||||||
| Task-oriented | −0.00 | −0.14** | −0.08 | −0.13* | −0.02 | −0.07 |
| [−0.10, 0.10] | [−0.24, −0.04] | [−0.17, 0.02] | [−0.22, −0.03] | [−0.12, 0.08] | [−0.17, 0.03] | |
| Emotion-oriented | 0.31** | 0.23** | 0.14** | 0.22** | −0.09 | 0.12* |
| [0.22, 0.40] | [0.13, 0.32] | [0.04, 0.24] | [0.13, 0.32] | [−0.18, 0.01] | [0.02, 0.22] | |
| Avoidance-oriented | −0.21** | −0.14** | −0.16** | −0.05 | 0.02 | 0.04 |
| [−0.30, −0.11] | [−0.23, −0.04] | [−0.26, −0.06] | [−0.14, 0.06] | [−0.08, 0.12] | [−0.06, 0.14] | |
| 6–12 years old | ||||||
| Task-oriented | −0.10** | −0.21** | −0.12** | −0.16** | −0.07* | −0.14** |
| [−0.17, −0.03] | [−0.28, −0.14] | [−0.19, −0.05] | [−0.23, −0.09] | [−0.15, −0.00] | [−0.21, −0.07] | |
| Emotion-oriented | 0.25** | 0.20** | 0.18** | 0.20** | −0.03 | 0.10** |
| [0.18, 0.32] | [0.13, 0.27] | [0.11, 0.25] | [0.13, 0.27] | [−0.10, 0.04] | [0.03, 0.17] | |
| Avoidance-oriented | −0.20** | −0.10** | −0.08* | −0.04 | 0.04 | −0.01 |
| [−0.26, −0.12] | [−0.17, −0.03] | [−0.15, −0.01] | [−0.11, 0.04] | [−0.03, 0.11] | [−0.08, 0.07] | |
| 13–18 years old | ||||||
| Task-oriented | 0.03 | −0.14** | −0.10 | −0.12* | 0.03 | −0.03 |
| [−0.07, 0.13] | [−0.24, −0.03] | [−0.21, 0.00] | [−0.22, −0.02] | [−0.07, 0.13] | [−0.14, 0.07] | |
| Emotion-oriented | 0.28** | 0.25** | 0.05 | 0.15** | 0.02 | 0.12* |
| [0.18, 0.37] | [0.15, 0.35] | [−0.06, 0.15] | [0.04, 0.25] | [−0.08, 0.12] | [0.01, 0.22] | |
| Avoidance-oriented | −0.19** | 0.04 | 0.11* | 0.10 | 0.14** | 0.04 |
| [−0.29, −0.09] | [−0.07, 0.14] | [0.01, 0.21] | [−0.00, 0.20] | [0.03, 0.24] | [−0.06, 0.15] | |
Parents reported that preschoolers who used task-oriented strategies exhibited fewer changes in mood and behavior during quarantine. In preschoolers and schoolchildren, avoidance-oriented strategies were related to lower anxiety, mood, and changes in their sleeping patterns. Schoolchildren who used task-oriented strategies exhibited fewer symptoms in all the domains. Adolescents who used task-oriented strategies showed fewer changes in mood and behavior, whereas the use of avoidance-oriented strategies was associated with lower anxiety but increased changes in sleeping patterns and eating habits.
The relationship between psychological symptoms and age, sex and coping strategies
Table 4 shows the GENLIN models' results used to study the relationship between psychological symptoms (dependent variable) and age, sex, and coping strategies (independent variables). Children presenting with more anxiety symptoms were more likely to belong to the 6–12-year-old age group (compared to preschoolers and adolescents), to be male, were more likely to use emotion-oriented strategies, and less likely to use task-oriented and avoidance-oriented strategies. Interactions between coping strategies and sex and coping strategies and age were not significant, whereas the interaction between sex and age was significant (p = .001).
Table 4.
GENLIN models to predict psychological symptoms based on the child age group, child's sex, and coping strategies.
| Β (SE) | Wald χ2 | 95% CI | p-value | |
|---|---|---|---|---|
| Anxiety | ||||
| Age | ||||
| [3–5 years] | −0.02 (0.17) | 0.01 | −0.36, 0.32 | 0.90 |
| [6–12 years] | 0.32 (0.15) | 4.28 | 0.01 0.62 | 0.03 |
| [13–18 years] | – | – | – | – |
| Sex | ||||
| [Male] | 0.35 (0.12) | 8.14 | 0.11, 0.60 | 0.004 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.21 (0.06) | 12.28 | −0.32, −0.09 | < 0.001 |
| Emotion-oriented | 0.82 (0.10) | 66.81 | 0.62, 1.02 | < 0.001 |
| Avoidance-oriented | −0.45 (0.07) | 34.05 | −0.61, −0.30 | < 0.001 |
| Interaction sex × age | 0.99 (0.28) | 12.06 | 0.43, 1.56 | 0.001 |
| Mood | ||||
| Age | ||||
| [3–5 years] | −0.06 (0.12) | 0.31 | −0.31, 0.17 | 0.57 |
| [6–12 years] | 0.08 (0.09) | 0.81 | −0.10, 0.28 | 0.36 |
| [13–18 years] | – | – | – | – |
| Sex | – | – | – | – |
| [Male] | 0.02 (0.08) | 0.07 | −0.13, 0.17 | 0.79 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.30 (0.03) | 58.75 | −0.38, −0.22 | < 0.001 |
| Emotion-oriented | 0.48 (0.06) | 58.85 | 0.36, 0.61 | < 0.001 |
| Avoidance-oriented | −0.10 (0.05) | 3.70 | −0.20, 0.002 | 0.054 |
| Sleep | ||||
| Age | ||||
| [3–5 years] | 0.49 (0.08) | 33.61 | 0.33, 0.66 | < 0.001 |
| [6–12 years] | 0.28 (0.06) | 18.83 | 0.15, 0.41 | < 0.001 |
| [13–18 years] | – | – | – | – |
| Sex | ||||
| [Male] | 0.009 (0.06) | 0.020 | −0.11, 0.12 | 0.88 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.14 (0.02) | 22.90 | −0.19, −0.08 | < 0.001 |
| Emotion-oriented | 0.23 (0.04) | 23.28 | 0.13, 0.32 | < 0.001 |
| Avoidance-oriented | −0.07 (0.03) | 4.21 | −0.14, −0.003 | < 0.001 |
| Behavioral alterations | ||||
| Age | ||||
| [3–5 years] | 0.36 (0.11) | 9.61 | 0.13, 0.50 | 0.002 |
| [6–12 years] | 0.32 (0.09) | 11.05 | 0.13, 0.50 | 0.001 |
| [13–18 years] | – | – | – | – |
| Sex | ||||
| [Male] | 0.22 (0.08) | 7.85 | 0.06, 0.38 | 0.005 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.23 (0.03) | 34.21 | −0.30, −0.15 | < 0.001 |
| Emotion-oriented | 0.46 (0.06) | 53 | 0.34, 0.59 | < 0.001 |
| Avoidance-oriented | −04 (0.05) | 0.49 | −0.07, 0.15 | 0.48 |
| Interaction sex × age | 0.10 (0.35) | 0.08 | −0.59, 0.80 | 0.76 |
| Feeding alterations | ||||
| Age | ||||
| [3–5 years] | −0.007 (0.04) | 0.02 | −0.08, 0.07 | 0.86 |
| [6–12 years] | 0.02 (0.03) | 0.35 | −0.04, 0.09 | 0.55 |
| [13–18 years] | – | – | – | – |
| Sex | ||||
| [Male] | 0.06 (0.02) | 5.06 | 0.008, 0.12 | 0.02 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.01 (0.01) | 0.69 | −0.03, 0.01 | 0.40 |
| Emotion-oriented | −0.01 (0.01) | 0.24 | −0.04, 0.02 | 0.61 |
| Avoidance-oriented | 0.03 (0.01) | 2.81 | −0.005, 0.06 | 0.09 |
| Cognitive alterations | ||||
| Age | ||||
| [3–5 years] | −0.04 (0.04) | 0.95 | −0.13, 0.04 | 0.32 |
| [6–12 years] | 0.09 (0.03) | 5.98 | 0.01, 0.17 | 0.01 |
| [13–18 years] | – | – | – | – |
| Sex | ||||
| [Male] | 0.04 (0.03) | 2.09 | −0.08, −0.02 | 0.14 |
| [Female] | – | – | – | – |
| Coping strategies | ||||
| Task-oriented | −0.05 (0.01) | 15.57 | −0.08, −0.02 | < 0.001 |
| Emotion-oriented | 0.10 (0.02) | 20.33 | 0.06, 0.15 | < 0.001 |
| Avoidance-oriented | 0.02 (0.02) | 1.40 | −0.01, 0.06 | 0.23 |
CI = Confidence Interval; SE = Standard Error.
Children presenting with more mood symptoms were more likely to use emotion-focused strategies and fewer task-oriented strategies. Age and sex were not related to the number of mood symptoms (p > .05).
Children presenting with more changes in their sleep patterns were more likely to belong to the 3–5-year-old age group (compared to the rest) or the 6–12-year-old age group (compared to the 13–18-year-old age group) and were more likely to use emotion-oriented strategies and less likely to use the other coping strategies. The interaction between avoidance-oriented strategies and age was significant, suggesting that younger children were more likely to use avoidance-oriented strategies. Sex was unrelated to changes in sleeping patterns (p > .05).
Children presenting with more behavioral changes were more likely to belong to the 3–5-year-old age group (compared to the rest) and the 6–12-year-old age group (compared to the 13–18-year-old age group), to be male, and were more likely to use emotion-focused strategies and less likely to use task-oriented strategies. Interactions between coping strategies and age and coping strategies and sex were not significant as well as the interaction between age and sex (p > .05).
Children presenting with more changes in eating patterns were more likely to be male. Age and coping strategies were unrelated to changes in eating patterns (p > .05), and therefore, interactions across these variables were not explored.
Children presenting with more cognitive difficulties were more likely to belong to the 6–12-year-old age group (compared to the other two groups) and were more likely to use emotion-oriented strategies and less likely to use task-oriented strategies. Sex was unrelated to cognitive alterations. Interactions between coping strategies and sex and age were not significant (p > .05).
Discussion
This study aimed to assess psychological reactions to COVID-19 and coping strategies in preschoolers, schoolchildren, and adolescents. Assessing psychological well-being and coping strategies according to age is crucial to provide guidelines to reduce the impact of the quarantine on children and prevent long-term psychological consequences from COVID-19 and the related restrictions.
Preschoolers' parents mainly reported nervousness, restlessness, and irritability (over 40% of parents of children of this age); schoolchildren were also described as restless and irritable, whereas adolescents were more often described as worried. Boredom was a common reaction to lockdown across all age groups. In line with our hypotheses, we showed that preschoolers were more nervous, restless, irritable, angry, depended on their parents, and had more significant behavioral problems than adolescents. Furthermore, COVID-19 affected the sleeping habits of preschoolers more than older children.
On the other hand, adolescents were seen as more worried than preschoolers, angrier than schoolchildren, and the most afraid of COVID-19 infection. Schoolchildren showed greater difficulty concentrating, were more worried about COVID-19 infection, and more easily alarmed than preschoolers, and argued more with the rest of their family than adolescents. Most of these symptoms agreed with our hypotheses and the reactions reported by Jiao et al. (2020), except for being worried about COVID-19 infection, where our data showed that older children were more worried than preschoolers. A possible explanation may be that our survey asked about being worried in a more general sense about COVID-19 infection, whereas Jiao et al. (2020) referred to relatives being infected. Idoiaga, Berasategi, Eiguren, and Picaza (2020) reported that children aged 3–12 years were worried about being infected with the virus mainly because they were afraid to infect their family members, especially their grandparents.
Several studies have linked sleeping difficulties and dependency to anxiety (Forbes et al., 2008; Whalen, Gilbert, Barch, Luby, & Belden, 2017). At the same time, intolerance of uncertainty has been extensively related to generalized anxiety disorders in adolescence (Dugas, Marchand, & Ladouceur, 2005; Fialko, Bolton, & Perrin, 2012; Lin, Xie, Yan, & Yan, 2017). Thus, although schoolchildren scored higher for anxiety, the current data suggests preschoolers and adolescents were not exempt from feeling anxious during the COVID-19 pandemic. However, they expressed their worries in different ways, according to their ages. Preschoolers had more sleeping difficulties, temper tantrums and were more dependent on parents, while adolescents' reactions were more related to COVID-19 worries and uncertainty. Existing literature about the effects of disasters on adolescent mental health supports the hypothesis of an additional increased risk of anxiety and depression disorders in adolescence (Guessoum et al., 2020). Although our results did not find significant results for those domains, they alert health care professionals of the need to consider and identify ways to improve the assessment of a broader range of feelings and symptoms, such as uncertainty, which may be related to anxiety in adolescence. Parents' perceptions of schoolchildren's symptoms were based more on cognitive issues. Research has shown that parents struggle to keep schoolchildren focused on homeschooling and schoolwork during quarantine (Szabo, Richling, Embry, Biglan, & Wilson, 2020), which likely explains the parents' perceptions of increased cognitive problems, especially difficulties concentrating.
In terms of the differences related to sex, parents reported higher eating and behavioral changes in boys. Our findings mirrored those of Francisco et al. (2020) and Ravens-Sieberer et al. (2021), which were based on parents' perceptions. Changes in their daily routines and reduced physical activity levels due to lockdown may explain these results. The existing literature suggests that sport and physical activity have a positive impact on psychological adjustment (see Biddle, Ciaccioni, Thomas, & Vergeer, 2019 for review) and, at the same time, that boys are more physically active than girls during childhood (Francisco et al., 2020; Nielsen, Pfister, & Bo Andersen, 2011; Telford, Telford, Olive, Cochrane, & Davey, 2016). Furthermore, higher anxiety levels were reported in boys, in line with Francisco et al. (2020); however, the interaction between sex and age showed that anxiety was higher in boys at school age, whereas it peaked in adolescence in girls. Previous epidemiological studies on anxiety and research on the pandemic also confirmed this trend (Chen et al., 2020; Ellis et al., 2020; Zhou et al., 2020).
Our second aim was to assess differences in children's coping strategies by age. We showed that preschoolers were more likely to use avoidance-oriented strategies to cope with stress than older children. Parents might have perceived a greater use of such strategies simply because preschoolers have less developed abilities to comprehend the situation. Acting as if nothing was happening or as if they did not care might simply be due to their limited understanding of the pandemic rather than an active and conscious attempt to disengage, deny, or withdraw from it.
Our findings show that preschoolers sought more affection from others than older children. However, as Pfefferbaum, Noffsinger, Wind, and Allen (2014) reported and in line with our findings, preschoolers often rely on their parents and loved ones for comfort to cope during major events. They are also egocentric, viewing their actions as making events happen, which may lead them to feel guilty and blame themselves for provoking a disaster or not preventing it (Pfefferbaum et al., 2014). Thus, another possible explanation for our findings may be seen in preschoolers' use of avoidance-oriented strategies as a way to help them disengage and buffer any fears linked to those emotions. Finally, a further reason may be that our tool was primarily designed to assess behavioral techniques of avoidance that prevailed in younger children. Research on older children showed that they employed a mix of behavioral and cognitive (i.e., cognitive reappraisal) avoidance-oriented strategies (Skinner & Zimmer-Gembeck, 2016).
The literature emphasizes how task-oriented strategies are expected to be predominant in schoolchildren and late adolescents. Pincus and Friedman (2004) suggested that schoolchildren rely heavily on task-oriented strategies to cope with various stressful situations. Our study did not find any differences in 6 to 18 year-olds in terms of task-oriented strategies. Hampel and Petermann (2005) showed that the use of task-oriented strategies peaked between the ages of 8 and 14 years, and there were no age-related differences. The adolescents in this study had a mean age of approximately 14 years, which may have influenced our findings.
The parents in our study perceived that schoolchildren relied more on emotion-oriented strategies than adolescents, and this was echoed by Duan et al. (2020), whose results confirmed the hypothesis that emotion-oriented strategies are more widely used in childhood across all cultures. Schoolchildren's use of emotion-oriented strategies may be linked to their common reenactment in play, drawings, and stories of their fears and worries, which are normal activities at this stage. Moreover, due to their advanced cognitive abilities, schoolchildren refer to concrete operations and logic to understand events, their significance, and the consequences (Deering, 2000). Past research in disaster psychology highlights that schoolchildren are also attuned to others' perceptions during stressful situations and that they possibly enjoy collaborating with concrete social activities and relying on their parents for consolation. Our results confirmed that schoolchildren are more involved in social activities, such as putting rainbow drawings in windows, and responded more to praise than adolescents.
In adolescence, the ability to run formal operations enables teens to use abstract thinking, reflection and analysis, test alternatives, predict outcomes, and be empathic with others, increasing their acceptance of the situation they face (Deering, 2000; McNamara, 2000). Our findings also show increased acceptance of current events in adolescents. Terranova, Boxer, and Morris (2009) suggested that they face a greater risk during major events due to the possible interaction between normal adolescence-related distress and their more accurate, although not yet fully mature, perception of the seriousness of the situation.
Finally, in line with previous studies and our hypothesis, emotion-focused strategies were linked to higher internalizing (i.e., anxiety, mood, and sleep difficulties) and externalizing (i.e., behavioral and cognitive alterations) symptoms across all ages (Carlo et al., 2012). Our data indicated that children described as more anxious, with cognitive problems, and changes in their behavior and sleeping patterns, were more likely to employ emotion-oriented strategies. VanMeter et al. (2020) suggested that if a child perceives a situation to be hostile, they are more likely to use emotion-focused strategies (e.g., anger) to cope.
As expected, task-oriented activities in schoolchildren were related to fewer symptoms in all the domains considered. However, this association was valid only for mood and behavioral changes in preschoolers and adolescents. As mentioned previously, preschoolers might be less accustomed and not developmentally adept at using such strategies. Moreover, task-oriented strategies were listed as significant predictors for all the psychological domains considered in our study, other than changes in eating patterns.
We showed that avoidance-oriented strategies to disconnect from stressful COVID-19 stimuli were related to less anxiety, better mood, and fewer sleep difficulties in preschoolers and schoolchildren, whereas, unexpectedly, in adolescents, avoidance-oriented strategies correlated with fewer anxiety symptoms but more sleep and eating difficulties. Adolescents have higher developmental abilities than younger children to enable them to actively and consciously deny or avoid distress related to COVID-19. However, although these strategies appeared to buffer any immediate anxiety symptoms, they did not provide genuine relief from stressful COVID-19 situations since the use of avoidance-oriented strategies was linked to increased changes in health-related routines, such as eating and sleeping. Therefore, reduced use of avoidance-oriented strategies increased the risk of anxiety symptoms and changes in sleep habits.
Limitations and future research
Despite the significance of our findings, some limitations exist, and several important questions remain to be addressed in future research. First, although our study includes many cities in three European countries, the sample was relatively homogeneous, with the majority of participants being mothers and married. For example, single parents reported more externalizing behaviors in their children than married parents, and single mothers reported significantly more internalizing disorders than single fathers and married parents (Hilton & Devall, 1998). Alone or divorced parents showed less life satisfaction and reduced emotional well-being and vitality, affecting their perceptions of the children's psychological adjustments and reactions to COVID-19 (Jenkinson, Matsuo, & Matthys, 2020). Therefore, the findings may not be generalized to a broader, more diverse population.
Second, we relied on online data collection because of the quarantine restrictions, which excluded parents without mobile internet devices or social media. These parents might likely belong to the category with the lowest monthly income, which is underrepresented in our sample. These parents might also be less socially connected and supported. Due to the well-known association between socio-economic status and psychological maladjustment, further studies should develop a more inclusive approach to consider those variables to offer a more generalizable picture of our findings. Furthermore, parents with children who struggled might also be more interested in the study and more motivated to participate. This possible bias should be taken into account as a study limitation.
Moreover, although a multi-informant method would be desirable, we relied on parent-only reporting due to lockdown. Previous studies validated parent-proxy measures and are considered valid measures of preschool and school-age children's behavior, pain, psychological status, and psychosocial functioning (Achenbach, McConaughy, & Howell, 1987; Verhulst & van der Ende, 1992). However, there is less agreement on the validity of parent-proxy measures for adolescent children (Li, Delvecchio, Di Riso, Lis, & Salcuni, 2017). For example, preschoolers were reported to have more problems sleeping. However, parents are likely to be more in tune with the sleep patterns of younger children than adolescents (who most likely sleep in their own rooms and maybe awake worrying or checking their social media for extended periods, unbeknown to parents). In addition, adolescents are less likely to reveal their feelings of anxiety or depression to their parents (though they may disclose these feelings to close friends), so parents may have been less aware of their adolescent children's increased feelings of anxiety during quarantine. Adolescents might feel more comfortable telling their parents that they are bored (vs. anxious), which might help explain the findings for boredom across the age groups. This reticence to discuss their feelings may have major implications for the results and their interpretation, representing a limitation of this study.
We relied on parents' perceptions, which aligns with others on COVID-19 (Di Giorgio, Di Riso, Mioni, & Cellini, 2020; Jiao et al., 2020; Orgilés, Morales, et al., 2020), to compare the current situation to a baseline before the outbreak. Although some risks and biases associated with this method may be present, evidence suggests that data collected via retrospective questions are consistent (Hipp, Bünning, Munnes, & Sauermann, 2020). However, we are aware that the parents' distress levels may have affected their ability and capacity to deal with their children's needs and challenges and may have interfered with their capacity to perceive their children's abilities to function accurately. Furthermore, in line with the inclusion criteria for participation, parents could complete the survey for more than one child. Although previous studies used the same study design (Crouch, Waters, McNair, Power, & Davis, 2014; Liang, Mazzeschi, & Delvecchio, 2021; Orgilés, Morales, et al., 2021), we acknowledge it as a limitation in this study.
Furthermore, the reliability of the domains of the Child Coping Strategies-COVID-19 was not as high as was desirable. From our perspective, such values were not surprising due to the different types of strategies included in the same factor. In other words, if a child uses a specific coping strategy does not imply that he/she uses all from the same factor (i.e., that a child asks a lot about the coronavirus does not imply that the child accepts what is happening or that he/she highlights the pros of being at home; see task-oriented strategies). From our perspective, such variability in types of coping strategies may contribute to explain why they do not converge with a consistent high reliability. However, it has to be listed as a study limitation.
It is also essential to identify and study other variables that may explain the levels of the children's and adolescents' psychological reactions and coping strategies. As example, the role of country and the related different levels of restrictions put in place should be explored. Preliminary findings which did not take age into account suggested that Portuguese and Spanish children showed higher psychological and behavioral symptoms than Italian ones during the first weeks of lockdown (Francisco et al., 2020), whereas Portuguese children were the best adapted to the situation over time (Orgilés et al., 2021; Orgilés et al., 2021). Moreover, factors related to the development of coping strategies, facilitators and barriers to the use of coping strategies, amount and quality of information about COVID-19, access to homeschooling during quarantine, availability of safe outdoor space, and family members diagnosed with COVID-19 or hospitalized due to it, look as meaningful variables to include in further research. Future studies should consider children's cognitive developments, as these develop rapidly over the preschool period and into school-age, and may provide a more accurate picture to explain the variation in psychosocial reactions. Furthermore, according to Skinner and Zimmer-Gembeck (2016), more detailed age-group splitting should be carried out (e.g., considering early adolescence) to deepen our knowledge on significant shifts in the nature and frequency of the use of coping responses. Additionally, research is needed into how various degrees of specific coping strategy use are associated with different degrees of adjustment in children and adolescents. The decision to dichotomize variables prevented us from doing so.
Finally, the cross-sectional design of this study precluded examination of the cause-effect relationships between the variables. Longitudinal studies are needed to understand the adjustment trajectories during and after the lockdown and possibly inform the development of interventions to foster positive outcomes in preschoolers, schoolchildren, adolescents, and their parents.
Despite these limitations, this study provides data on the symptoms and coping strategies related to COVID-19 in preschoolers, schoolchildren, and adolescents. Results based on parental perspectives indicated that responses to the stress brought about by the pandemic and its consequences were related to age. Our data emphasized that measures such as a lockdown can affect children of all ages, at least in the immediate aftermath. Children and adolescents are not strangers to stressful events, but these stressful events may become traumatic, posing a threat to their mental, emotional, and physical well-being (Garmezy & Masten, 1986). Age is a primary factor in a wide range of external and internal contributions to these threats.
Implications of the findings
The complex picture reported in our study emphasizes the importance of taking children's ages into account when assessing their psychological reactions to COVID-19 and the related coping strategies. As an index of developmental skills, age is related to children's abilities to understand the risks associated with the situation. Therefore, as Eth and Pynoos (1985) suggested, symptoms and coping strategies may vary according to age. Children's age can either increase or decrease their current, and future psychological adaptations to the changes brought about by COVID-19; conversely, the pandemic situation can impact age-appropriate relevant developmental milestones by either causing them to be delayed or advanced. Recent research showed that psychological symptoms in children and adolescents increased from the second (T1) to the fifth (T2) week of home confinement, and the majority remained stable over time (i.e., two months after the beginning of the home confinement) (Liang et al., 2021; Orgilés, Francisco, et al., 2021).
On the one hand, the current study may contribute to the early detection of long-term psychological maladjustment in children. It may help design more focused, age-related, and practical sessions that target the needs and core areas of maladjustment while informing parents about what common psychological reactions to look out for. At the same time, our data provides information for professionals and parents about children's most common and adaptive coping methods. Promoting programs on coping with distress and modeling positive psychological attitudes to reduce children's stress and divert their attention towards being more resilient might also be relevant for caregivers (Jiao et al., 2020). Resilience is one of the most crucial protective factors during disasters that can help children and adolescents manage their difficulties (Jiao et al., 2020). Programs aimed at enhancing children's self-confidence and emotional resilience while improving their social skills and coping strategies to handle stressful situations and maladjustments, both current and over the long-term, should be implemented on a large scale and in multiple contexts, according to age. For example, the Super-Skills for Life Program (SSL; Essau & Ollendick, 2013) which builds emotional resilience and provides young people (aged 6–10 and 11–18 years) with skills to deal with stressful and challenging situations and to cope with internalizing and externalizing difficulties, has been proven to be effective in helping children to face the COVID-19 situation. Children who participated in the SSL program showed fewer anxiety symptoms, cognitive changes, low mood, and sleep difficulties than the control group. Moreover, they were less likely to refer to emotion-oriented coping strategies, which were linked to higher maladjustment (Orgilés, Espada and Morales, 2020). On the other hand, Zhang and Lee (2020) emphasized the crucial role of supporting the development of preschoolers' emotional resilience at home by practicing the 3 R's: Reassurance, Routine, and Regulation. Healthcare professionals, communities, and schools should refer to the current pandemic as a learning opportunity to prepare them for future situations that may require home confinement and changes in a child's daily routine. Stakeholders should be more aware of the psychological impact of the measures implemented to ensure they are prepared to meet the diverse needs of children and families before, during, and after health crises.
Financial support
This research received support from the Ministry of Science and Innovation of Spain and the European Regional Development Fund. Award Number: PSI2017-85493-P. Recipient: Mireia Orgilés.
Ethical standards disclosure
This study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
CRediT authorship contribution statement
Elisa Delvecchio: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Mireia Orgilés: Conceptualization, Funding acquisition, Writing – review & editing. Alexandra Morales: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. José Pedro Espada: Conceptualization, Project administration. Rita Francisco: Conceptualization, Writing – original draft. Marta Pedro: Data curation. Claudia Mazzeschi: Data curation, Writing – original draft.
Declaration of Competing Interest
The authors declare no conflict of interest.
References
- Achenbach T.M., McConaughy S.H., Howell C.T. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. doi: 10.1037/0033-2909.101.2.213. [DOI] [PubMed] [Google Scholar]
- Akoglu H. User's guide to correlation coefficients. Turkish Journal of Emergency Medicine. 2018;18:91–93. doi: 10.1016/j.tjem.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong R.A. When to use the Bonferroni correction. Ophthalmic and Physiological Optics. 2014;34:502–508. doi: 10.1111/opo.12131. [DOI] [PubMed] [Google Scholar]
- Baggerly J., Exum H.A. Counseling children after natural disasters: Guidance for family therapists. The American Journal of Family Therapy. 2007;36:79–93. doi: 10.1080/01926180601057598. [DOI] [Google Scholar]
- Beasley T.M., Schumacker R.E. Multiple regression approach to analyzing contingency tables: Post hoc and planned comparison procedures. The Journal of Experimental Education. 1995;64:79–93. doi: 10.1080/00220973.1995.9943797. [DOI] [Google Scholar]
- Bernzweig J., Eisenberg N., Fabes R.A. Children’s coping in self-and other-relevant contexts. Journal of Experimental Child Psychology. 1993;55:208–226. doi: 10.1006/jecp.1993.1012. [DOI] [PubMed] [Google Scholar]
- Biddle S.J., Ciaccioni S., Thomas G., Vergeer I. Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychology of Sport and Exercise. 2019;42:146–155. doi: 10.1016/j.psychsport.2018.08.011. [DOI] [Google Scholar]
- Carlo G., Crockett L.J., Wolff J.M., Beal S.J. The role of emotional reactivity, self-regulation, and puberty in adolescents’ prosocial behaviors. Social Development. 2012;21:667–685. doi: 10.1111/j.1467-9507.2012.00660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain, Behavior, and Immunity. 2020;88:36–38. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Compas B.E., Connor-Smith J.K., Saltzman H., Thomsen A.H., Wadsworth M.E. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. doi: 10.1037/0033-2909.127.1.87. [DOI] [PubMed] [Google Scholar]
- Compas B.E., Malcarne V.L., Fondacaro K.M. Coping with stressful events in older children and young adolescents. Journal of Consulting and Clinical Psychology. 1988;56:405–411. doi: 10.1037/0022-006X.56.3.405. [DOI] [PubMed] [Google Scholar]
- Corrarino J.E. Disaster-related mental health needs of women and children. The American Journal of Maternal Child Nursing. 2008;33:242–248. doi: 10.1097/01.NMC.0000326079.26870.e3. [DOI] [PubMed] [Google Scholar]
- Crouch S.R., Waters E., McNair R., Power J., Davis E. Parent-reported measures of child health and wellbeing in same-sex parent families: A cross-sectional survey. BMC Public Health. 2014;14 doi: 10.1186/1471-2458-14-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis J., Vizard T.N., Pearce N., Nafilyan V., Merad S., Goodman A. Mental health of children and young people in England: Predictors of mental disorders. 2018. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017#
- Deering C.G. A cognitive developmental approach to understanding how children cope with disasters. Journal of Child and Adolescent Psychiatric Nursing. 2000;13:7–16. doi: 10.1111/j.1744-6171.2000.tb00070.x. [DOI] [PubMed] [Google Scholar]
- Delvecchio E., Salcuni S., Lis A., Germani A., Di Riso D. Hospitalized children: Anxiety, coping strategies, and pretend play. Frontiers in Public Health. 2019;7 doi: 10.3389/fpubh.2019.00250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giorgio E., Di Riso D., Mioni G., Cellini N. 2020. The interplay between mothers’ and children’s behavioral and psychological factors during COVID-19: An Italian study. Doi:10.31234/osf.io/dqk7h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogan-Ates A. Developmental differences in children’s and adolescents’ post-disaster reactions. Issues in Mental Health Nursing. 2010;31(7):470–476. doi: 10.3109/01612840903582528. [DOI] [PubMed] [Google Scholar]
- Donaldson D., Prinstein M.J., Danovsky M., Spirito A. Patterns of children’s coping with life stress: Implications for clinicians. American Journal of Orthopsychiatry. 2000;70:351–359. doi: 10.1037/h0087689. [DOI] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of the mental health status of children and adolescents in China during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugas M.J., Marchand A., Ladouceur R. Further validation of a cognitive-behavioral model of generalized anxiety disorder: Diagnostic and symptom specificity. Journal of Anxiety Disorders. 2005;19(3):329–343. doi: 10.1016/j.jad.2020.06.029. [DOI] [PubMed] [Google Scholar]
- Dyregrov A., Yule W. A review of PTSD in children. Child and Adolescent Mental Health. 2006;11:176–184. doi: 10.1111/j.1475-3588.2005.00384.x. [DOI] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement. 2020;52:177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- Eschenbeck H., Kohlmann C.W., Lohaus A. Gender differences in coping strategies in children and adolescents. Journal of Individual Differences. 2007;28:18–26. doi: 10.1027/1614-0001.28.1.18. [DOI] [Google Scholar]
- Essau C.A., Ollendick T.H. University of Roehampton; London: 2013. The super skills for life programme. [Google Scholar]
- Eth S., Pynoos R.S., editors. Post-traumatic stress disorder in children. American Psychiatric Press; 1985. [Google Scholar]
- European Centre for Disease Prevention and Control Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK – ninth update. 2020, April 23. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-ninth-update-23-april-2020.pdf
- Fialko L., Bolton D., Perrin S. Applicability of a cognitive model of worry to children and adolescents. Behaviour Research and Therapy. 2012;50:341–349. doi: 10.1016/j.brat.2012.02.003. [DOI] [PubMed] [Google Scholar]
- Fields L., Prinz R.J. Coping and adjustment during childhood and adolescence. Clinical Psychology Review. 1997;17:937–976. doi: 10.1016/S0272-7358(97)00033-0. [DOI] [PubMed] [Google Scholar]
- Fluharty M., Bu F., Steptoe A., Fancourt D. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Social Science & Medicine. 2021;279 doi: 10.1016/j.socscimed.2021.113958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes E.E., Bertocci M.A., Gregory A.M., Ryan N.D., Axelson D.A., Birmaher B., Dahl R.E. Objective sleep in pediatric anxiety disorders and major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:148–155. doi: 10.1097/chi.0b013e31815cd9bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford T., John A., Gunnell D. Mental health of children and young people during the pandemic. BMJ (Clinical research ed.) 2021;37 doi: 10.1136/bmj.n614. [DOI] [PubMed] [Google Scholar]
- Francisco R., Pedro M., Delvecchio E., Espada J.P., Morales A., Mazzeschi C., Orgilés M. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Frontiers in Psychiatry. 2020;11:1329. doi: 10.3389/fpsyt.2020.570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N., Masten A.S. Stress, competence, and resilience: Common frontiers for therapist and psychopathologist. Behavior Therapy. 1986;17:500–521. doi: 10.1016/S0005-7894(86)80091-0. [DOI] [Google Scholar]
- Griffiths J., Ravindran A.V., Merali Z., Anisman H. Dysthymia: A review of pharmacological and behavioral factors. Molecular Psychiatry. 2000;5:242–261. doi: 10.1038/sj.mp.4000697. https://www.nature.com/articles/4000697 [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel P., Petermann F. Age and gender effects on coping in children and adolescents. Journal of Youth and Adolescence. 2005;34:73–83. doi: 10.1007/s10964-005-3207. [DOI] [Google Scholar]
- Hilton J.M., Devall E.L. Comparison of parenting and children’s behavior in single-mother, single-father, and intact families. Journal of Divorce and Remarriage. 1998;29:23–54. doi: 10.1300/J087v29n03_02. [DOI] [Google Scholar]
- Hipp L., Bünning M., Munnes S., Sauermann A. Problems and pitfalls of retrospective survey questions in COVID-19 studies. In Survey Research Methods. 2020;14:109–114. doi: 10.18148/srm/2020.v14i2.7741. [DOI] [Google Scholar]
- Idoiaga N., Berasategi N., Eiguren A., Picaza M. Exploring children’s social and emotional representations of the Covid-19 pandemic. Frontiers in Psychology. 2020 doi: 10.3389/fpsyg.2020.01952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkinson S., Matsuo H., Matthys K. In: Divorce in Europe, new insights in trends, causes and consequences of relation break-ups. Mortelmans D., editor. Springer Open; 2020. Multi-dimensional subjective wellbeing and lone parenthood following divorce in Flanders (Northern Belgium) pp. 211–236. [DOI] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. The Journal of Pediatrics. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korol M., Green B.L., Gleser G.C. Children’s responses to a nuclear waste disaster: PTSD symptoms and outcome prediction. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:368–375. doi: 10.1097/00004583-199904000-00008. [DOI] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer Publishing Company; 1984. Stress, appraisal, and coping. [Google Scholar]
- Li J.-B., Delvecchio E., Di Riso D., Lis A., Salcuni S. Early evidence of the Italian parent-report strengths and difficulties questionnaire (SDQ-P) Child Psychiatry and Human Development. 2017;48:335–345. doi: 10.1007/s10578-016-0646-3. [DOI] [PubMed] [Google Scholar]
- Liang Z., Mazzeschi C., Delvecchio E. The impact of parental stress on Italian adolescents’ internalizing symptoms during the COVID-19 pandemic: A longitudinal study. International Journal of Environmental Research and Public Health. 2021;18:8074. doi: 10.3390/ijerph18158074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin R.M., Xie S.S., Yan Y.W., Yan W.J. Intolerance of uncertainty and adolescent sleep quality: The mediating role of worry. Personality and Individual Differences. 2017;108:168–173. doi: 10.1016/j.paid.2016.12.025. [DOI] [Google Scholar]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Research. 2020;289 doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntosh H.B., Whiffen V.E. Twenty years of progress in the study of trauma. Journal of Interpersonal Violence. 2005;20:488–492. doi: 10.1177/0886260504267836. doi:10.1177%2F088626050426783. [DOI] [PubMed] [Google Scholar]
- McNamara S. London and New York; 2000. Stress in young people: What's new and what to do. [Google Scholar]
- Meherali S., Punjani N., Louie-Poon S., Abdul Rahim K., Das J.K., Salam R.A., Lassi Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: A rapid systematic review. International Journal of Environmental Research and Public Health. 2021;18:3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales A., Melero S., Espada J.P., Orgilés M. 6th international conference on childhood and adolescence and 9th annual meeting of the social paediatric subcommittee (SPS-SPP) of the Portuguese Society of Paediatrics, Oporto, Portugal and online. 2022. “Mom, dad, I can handle this!”: Development of the coping inventory to COVID-19 and home confinement on children and adolescents [poster presentation]https://icca.eventqualia.net/en/2022/home/ [Google Scholar]
- Nearchou F., Flinn C., Niland R., Subramaniam S.S., Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: A systematic review. International Journal of Environmental Research and Public Health. 2020;17:8479. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen G., Pfister G., Bo Andersen L. Gender differences in the daily physical activities of Danish school children. European Physical Education Review. 2011;17:69–90. doi: 10.1177/1356336X11402267. [DOI] [Google Scholar]
- Novins D.K., Althoff R.R., Billingsley M.K., Cortese S., Drury S.S., Frazier J.A., White T.J. JAACAP’s role in advancing the science of pediatric mental health and promoting the care of youth and families during the COVID-19 pandemic. Journal of the American Academy of Child and Adolescent Psychiatry. 2020;59:686–688. doi: 10.1016/j.jaac.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A., Tomova L., Blakemore S.J. The effects of social deprivation on adolescent social development and mental health. Lancet Child Adolescent Health. 2020;4:634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Espada J.P., Delvecchio E., Francisco R., Mazzeschi C., Pedro M., Morales A. Anxiety and depressive symptoms in children and adolescents during COVID-19 pandemic: A transcultural approach. Psicothema. 2021;33:125–130. doi: 10.7334/psicothema2020.287. [DOI] [PubMed] [Google Scholar]
- Orgilés M., Espada J.P., Morales A. How super skills for life may help children to cope with the covid-19: Psychological impact and coping styles after the program. Revista de Psicología Clínica con Niños y Adolescentes. 2020;7:88–93. doi: 10.21134/rpcna.2020.mon.2048. [DOI] [Google Scholar]
- Orgilés M., Francisco R., Delvecchio E., Espada J.P., Mazzeschi C., Pedro M., Morales A. Psychological symptoms in Italian, Spanish and Portuguese youth during the COVID-19 health crisis: A longitudinal study. Child Psychiatry and Human Development. 2021 doi: 10.1007/s10578-021-01211-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Francisco R., Mazzeschi C., Pedro M., Espada J.P. Coping behaviors and psychological disturbances in youth affected by the COVID-19 health crisis. Frontiers in Psychology. 2021;12 doi: 10.3389/fpsyg.2021.565657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.579038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker J.D., Endler N.S. Coping with coping assessment: A critical review. European Journal of Personality. 1992;6:321–344. doi: 10.1002/per.2410060502. [DOI] [Google Scholar]
- Peterson L. Coping by children undergoing stressful medical procedures: Some conceptual, methodological, and therapeutic issues. Journal of Consulting and Clinical Psychology. 1989;57:380–387. doi: 10.1037/0022-006X.57.3.380. [DOI] [PubMed] [Google Scholar]
- Peterson L., Harbeck C., Chaney J., Farmer J. Children's coping with medical procedures: A conceptual overview and integration. Behavioral Assessment. 1990;12:197–212. https://psycnet.apa.org/record/1991-02342-001 [Google Scholar]
- Pfefferbaum B., Noffsinger M.A., Wind L.H., Allen J.R. Children’s coping in the context of disasters and terrorism. Journal of Loss and Trauma. 2014;19:78–97. doi: 10.1080/15325024.2013.791797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus D.B., Friedman A.G. Improving children’s coping with everyday stress: Transporting treatment interventions to the school setting. Clinical Child and Family Psychology Review. 2004;7:223–240. doi: 10.1007/s10567-004-6087-8. [DOI] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. European Child & Adolescent Psychiatry. 2021:1–11. doi: 10.1007/s00787-021-01726-5?s=09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero E., Lopez-Romero L., Dominguez-alvarez B., Villar P., Gomez-Fraguela J., A. Testing the effects of covid-19 confinement in Spanish children: The role of parents’ distress, emotional problems and specific parenting. International Journal of Environmental Research and Public Health. 2020;17:1–23. doi: 10.3390/ijerph17196975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon K., Bryant R.A. Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review. 2002;22:163–188. doi: 10.1016/S0272-7358(01)00086-1. [DOI] [PubMed] [Google Scholar]
- Silverman W.K., La Greca A.M. In: Helping children cope with disasters and terrorism. La Greca A.M., Silverman W.K., Vernberg E.M., Roberts M.C., editors. American Psychological Association; 2002. Children experiencing disasters: Definitions, reactions, and predictors of outcomes; pp. 11–33. [DOI] [Google Scholar]
- Skinner E.A., Zimmer-Gembeck M.J. The development of coping. Annual Review of Psychology. 2007;58:119–144. doi: 10.1146/annurev.psych.58.110405.085705. [DOI] [PubMed] [Google Scholar]
- Skinner E.A., Zimmer-Gembeck M.J. Springer; Cham: 2016. The development of coping. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Szabo T.G., Richling S., Embry D.D., Biglan A., Wilson K.G. From helpless to hero: Promoting values-based behavior and positive family interaction in the midst of Covid-19. Behavior Analysis in Practice. 2020 doi: 10.1007/s40617-020-00431-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y., T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parentchild discussion. Journal of Affective Disorders. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telford R.M., Telford R.D., Olive L.S., Cochrane T., Davey R. Why are girls less physically active than boys? Findings from the LOOK longitudinal study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terranova A.M., Boxer P., Morris A.S. Factors influencing the course of posttraumatic stress following a natural disaster: Children’s reactions to hurricane Katrina. Journal of Applied Developmental Psychology. 2009;30:344–355. doi: 10.1016/j.appdev.2008.12.017. [DOI] [Google Scholar]
- VanMeter F., Handley E.D., Cicchetti D. The role of coping strategies in the pathway between child maltreatment and internalizing and externalizing behaviors. Child Abuse and Neglect. 2020;101 doi: 10.1016/j.chiabu.2019.104323. [DOI] [PubMed] [Google Scholar]
- Verhulst F.C., van der Ende J. Agreement between parents’ reports and adolescents’ self-reports of problem behavior. Journal of Child Psychology and Psychiatry. 1992;33:1011–1023. doi: 10.1111/j.1469-7610.1992.tb00922.x. [DOI] [PubMed] [Google Scholar]
- Waite P., Pearcey S., Shum A., Raw J., A., Patalay P., Creswell C. How did the mental health symptoms of children and adolescents change over early lockdown during the COVID‐19 pandemic in the UK? JCPP Advances. 2021;1 doi: 10.1111/jcv2.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whalen D.J., Gilbert K.E., Barch D.M., Luby J.L., Belden A.C. Variation in common preschool sleep problems as an early predictor for depression and anxiety symptom severity across time. Journal of Child Psychology and Psychiatry. 2017;58:151–159. doi: 10.1111/jcpp.12639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Lee M.K. How to help children develop emotional resilience during coronavirus. North Carolina Medical Journal. 2020;81:137–140. https://lernercenter.syr.edu/wp-content/uploads/2020/05/Zhang_Lee.pdf [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C.…Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. https://link.springer.com/article/10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer-Gembeck M.J., Skinner E.A. The development of coping across childhood and adolescence: An integrative review and critique of research. International Journal of Behavioral Development. 2011;35:1–17. doi: 10.1177/0165025410384923. [DOI] [Google Scholar]