Abstract
Aims
A disproportionate number of people with mental ill-health experience social exclusion. Appropriate measurement tools are required to progress opportunities to improve social inclusion. We have developed a novel measure, the Filia Social Inclusion Measure (F-SIM). Here we aimed to present a more concise, easy-to-use form, while retaining its measurement integrity by (i) refining the F-SIM using traditional and contemporary item-reduction techniques; and (ii) testing the psychometric properties of the reduced measure.
Methods
Five hundred and six participants completed the F-SIM, younger and older groups of people with serious mental illness (including psychosis, mood, anxiety disorders) and same-aged community counterparts. The F-SIM was completed at baseline and 2-week follow-up, alongside other measures (including social inclusion, loneliness). The F-SIM was refined using multidimensional scaling network analysis, confirmatory factor analysis and item response theory. The psychometric evaluation included assessment of dimensionality, internal consistency, test–retest reliability, discriminant ability and construct validity.
Results
The F-SIM was reduced from 135-items to 16; with 4-items in each domain of housing and neighbourhood, finances, employment and education and social participation and relationships. Psychometric properties were sound, including strong internal consistency within domains (all α > 0.85) and excellent overall (α = 0.92). Test–retest reliability was also high (γ = 0.90). Differences between groups were observed; clinical subgroups consistently reported lower levels of social inclusion compared to community counterparts.
Conclusions
The F-SIM16 is a sound, reliable, brief self-report measure of social inclusion suitable for use in clinical and research settings. It has the potential to evaluate the effectiveness of interventions, and aid in fostering targeted and personalised needs-based care.
Key words: Social inclusion, social exclusion, psychometrics, self report, surveys and questionnaires
Introduction
While traditionally mental health care focused on the reduction and/or elimination of distressing symptomatology (Slade et al., 2014; van Os et al., 2019), more recently the recovery movement has shifted focus to person-centred holistic care, acknowledging the importance of participation in society (Davidson, 2016). As such, in conjunction with the treatment of symptoms (Le Boutillier et al., 2011; Slade et al., 2014), there has been more consideration of education and employment, finances, housing, physical health, community participation and quality of life (van Os et al., 2019); areas highly valued by people with mental ill-health and their families (Connell et al., 2014; Robotham et al., 2016). Many of these domains are characteristic of social inclusion (Filia et al., 2018), a relatively new concept in the mental health field, with a focus on the degree to which a person participates in their communities (Productivity Commission, 2019). Due to the inter-connected nature of these domains, difficulties in one domain can impact other domains and reduce overall social inclusion. In addition, a negative cycle can ensue between social exclusion and poor mental health that, once started, can be difficult to break (Filia et al., 2021). However, relationships between these domains, and the impact and direction of the relationship with mental health remain underexplored.
Research on social inclusion in those impacted by mental ill-health has been hampered by a lack of definitional consensus, understanding of its components, and how to best measure the construct (Morgan et al., 2007; Huxley et al., 2012; Filia et al., 2018). While a number of measures of social inclusion are available (Stickley and Shaw, 2006; Lloyd et al., 2008; Dorer et al., 2009; Secker et al., 2009; Marino-Francis and Worrall-Davies, 2010; Huxley et al., 2012; Mezey et al., 2013), they have yet to undergo either a complete psychometric evaluation, and/or have restricted use for people with mental ill-health (Coombs et al., 2013; Cordier et al., 2017; O'Donnell et al., 2018). Our team has been working to address these issues, developing the Filia Social Inclusion Measure (F-SIM), with items based on a thematic analysis of the literature (Filia et al., 2018) and a consensus study of those impacted by mental ill-health (Filia et al., 2019a). In its original long-form, the F-SIM has demonstrated validity in discriminating the impacts of mental ill-health on social inclusion of consumers and caregivers (Filia et al., 2019b), and the preliminary characteristics of the measure have been tested in clinical and community-based youth samples (Gardner et al., 2019; Gardner et al., 2020). Refinement of this measure was required to ensure brevity and practicality of use in clinical and research settings. Thus, the aims of this work were to (i) use item reduction techniques to produce a more concise version of the measure; and (ii) test the psychometric properties of the reduced measure, including dimensionality, internal consistency, test–retest reliability, the ability to discriminate between groups, and construct validity.
Methods
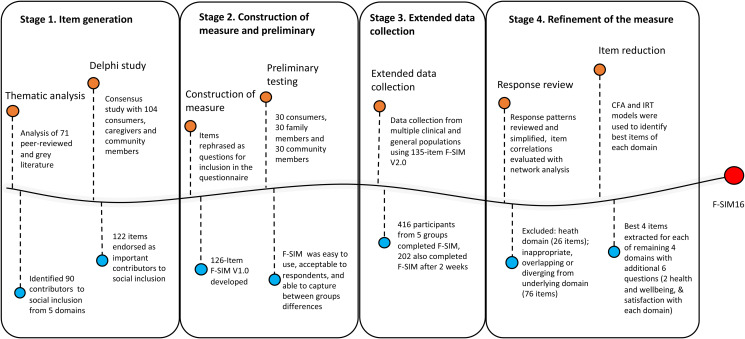
The F-SIM was developed iteratively over several stages briefly outlined here (see Fig. 1 and for more details, Filia et al., 2019b; Gardner et al., 2019).
Fig. 1.
Process of Development of F-SIM16 from Stage 1 (Item Generation) to Stage 4 (Refinement and Validation).
Note: The first iteration of the measure developed (F-SIM V1.0) in Stage 2 comprised 126 items, with a reference period of the past month. Most items were measured on a dichotomous scale (Yes/No), or Likert scales. Nine additional items were included in (F-SIM V2.0) at Stage 3 for clarity. Data collected from Stage 2 and 3 were harmonised and pooled together in Stage 4 for further psychometric evaluation.
Preliminary work
Stage 1. Item generation
An evidence-based definition of social inclusion was established over two studies. First, a thematic analysis of academic peer-reviewed and grey literature to identify conceptualisations of contributors of social inclusion (Filia et al., 2018). Second, a consensus study regarding the relative importance of contributors to social inclusion to those with a lived experience of mental ill-health, and the general community (Filia et al., 2019a).
Stage 2. Construction of measure and preliminary testing
Contributors identified in the thematic analysis, and agreed upon as important in the consensus study, were rephrased into question form to allow self-report administration. We grouped contributors according to the similarity of features into five overarching domains: (i) Housing and neighbourhood (HN); (ii) Social relationships, Participation and limitations (SOC); (iii) Employment and education (EE); (iv) Finances (FIN) and; (v) Health and wellbeing (HW). Preliminary psychometric evaluation of the face and discriminant validity of the 126-item version (F-SIM V1.0) in 90 participants suggested it was easy to use, highly acceptable to respondents, and able to discriminate between groups in terms of social inclusion (Filia et al., 2019b).
Stage 3. Extended data collection
To conduct further validation, we collected data from participants in five groups (N = 416): (i) young people (18–25 years) with a serious mental illness (SMI; psychosis); (ii) same-aged young people with an SMI (not psychosis); (iii) same-aged young people from the general community; (iv) older people (26 years+) with an SMI; and (v) same-aged older people from the general community. The methodology has been detailed previously (Gardner et al., 2019). In brief, participants completed the F-SIM Version 2.0 (a 135-item version, additional questions included for clarity), alongside other measures including an existing, albeit brief social inclusion measure (the Social Inclusion Scale, SIS; Secker et al., 2009), and the UCLA Loneliness Scale (UCLA-LS; Russell, 1996). A subset of participants (n = 202) completed the F-SIM again at a 2-week follow-up.
Current study
Stage 4. Refinement of the measure
Participants and data
Data from Stages 2 (N = 90) and 3 (N = 416) were pooled and analysed in Stage 4 (N = 506). Relevant measures analysed here included the F-SIM, the UCLA-LS and the SIS. Higher scores on the UCLA-LS and SIS indicate greater subjective loneliness and isolation, and degrees of social inclusion respectively.
Item evaluation and reduction
All analyses were conducted using R version 4.0.2 (2020-06-22). Items were refined and recoded according to their distributions (e.g. item response categories with low prevalence were combined). Items were excluded if they had a high degree of overlap (almost identical response patterns), were superseded by other broad or essential questions, or were age-specific.
In the second step, network psychometric analyses were used to understand the interplay between items, and their underlying domains (Borsboom and Cramer, 2013). We used multidimensional scaling (MDS) network analysis (Jones et al., 2018) of the pairwise tetrachoric correlation coefficients, γtc, with the benefit that the distance between any pair of nodes (variables) is directly interpretable as the strength of association. MDS network analysis is additionally helpful for understanding complex associations in high-dimensional data, where other techniques such as factor analysis, can be difficult to interpret (Borsboom and Cramer, 2013; Jones et al., 2018). Using MDS networks we identified: (i) whether items reflected their latent domain (distance of the location from other items in the same domain); and (ii) items with a higher level of overlap.
Third, single factor confirmatory factor analysis (CFA) and Item response theory (IRT) 2PL models were used to identify the best items within each domain for inclusion in the final measure. Items selected included those more reflective of the latent domain(s) of interest (according to CFA and IRT results), and of more relevance to the theoretical framework.
Psychometric evaluation of the revised measure
Pairwise associations between items within each domain were evaluated using tetrachoric correlation coefficients, rtc. Item-to-total correlations within each domain were estimated using biserial correlation coefficients, rbs. Correlations were estimated using pairwise complete observations. Internal reliability was evaluated using Cronbach's alpha, α, based on rtc. MDS network modelling using γtcwas then carried out to obtain an overview of all items. Three CFA models were used to evaluate whether the measure was unidimensional, multidimensional, or best represented by a second-order latent factor. Overall model fit was examined using chi-square (χ2) goodness-of-fit statistics, root mean square error of approximation (RMSEA: <0.08 acceptable; 0.05 excellent), Tucker–Lewis index (TLI: >0.90 acceptable; >0.95 excellent) and comparative fit index (CFI: >0.90 acceptable; >0.95 excellent) (Hooper et al., 2008).
We then examined the capacity of the revised measure to distinguish between groups. First, we visually examined the distributions of domain scores (0–100) across the five groups. Second, we conducted a range of comparisons both across and within clinical and community groups using independent samples t-tests.
Test-retest reliability was evaluated using the 2-week follow-up data. Pearson product-moment correlations (r) were (i) evaluated between baseline and follow-up total scores; and (ii) used to compare the reduced version of the F-SIM with the UCLA-LS and the SIS.
Results
Sample characteristics
The cohort comprised 506 participants from the five different groups : (i) young people (18–25 years) with a SMI (psychosis; n = 149), (ii) young people (18–25 years) with a SMI (not psychosis; n = 26), (iii) young people (aged 18–25 years) from the general community (n = 163), (iv) older people (26 years+) with a SMI (n = 64); and (v) older people (26 years+) from the general community (n = 104; see Table 1).
Table 1.
Demographic characteristics of the total cohort and five population groups
| Overall (N = 506) | Young | Older | ||||||
|---|---|---|---|---|---|---|---|---|
| Psychosis (N = 149) | Clinical not psychosis (N = 26) | General community (N = 163) | p-Valuea | Clinical (N = 64) | General community (N = 104) | p-Valuea | ||
| Gender | 0.9 | 0.4 | ||||||
| Female | 272 (54%) | 70 (47%) | 11 (42%) | 86 (53%) | 37 (58%) | 68 (65%) | ||
| Male | 216 (43%) | 67 (45%) | 12 (46%) | 76 (47%) | 26 (41%) | 35 (34%) | ||
| Non-binary | 18 (4%) | 12 (8%) | 3 (12%) | 1 (0.6%) | 1 (2%) | 1 (1%) | ||
| Age, mean (s.d.) | 27 (11) | 21 (2) | 22 (2) | 21 (2) | 0.11 | 41 (9) | 39 (10) | 0.2 |
| Participation in the follow-up survey | 202 (40%) | 36 (24%) | 10 (38%) | 123 (75%) | <0.001 | 22 (34%) | 11 (11%) | <0.001 |
Pearson's Chi-squared for a categorical variable (excluding the non-binary group due to small cell count); Independent sample t-test or ANOVA test for continuous variable.
Item evaluation and reduction
Item refinement
Distributions of Likert-scaled items (excluding satisfaction items) were either very skewed or bimodal, suggesting the underlying latent factor underpinning these questions was more likely categorical than continuous, or that participants were likely to respond to questions with a binary mindset. Hence, responses were converted to a binary system (Yes/No) allowing ease of comparison with other items, and simplifying response selection for respondents. Examples of binary conversions include Likert responses such as ‘1-Not at all’, ‘2-A little bit’, ‘3-Very much so’ being converted to 1 = No, 2&3 = Yes; or ‘1-Definitely limited’, ‘2-Limited a bit’, ‘3-Not at all’ being converted to 1&2 = Yes, 3 = No.
Forty-five items were excluded after item responses were evaluated for all questions, leaving 90-items remaining.
Item domain mapping
Fifty-seven items were excluded in this stage. Items were considered within the five domains they were initially grouped. Associations between items were mapped using MDS network analysis and data-supported four of the five domains. The remaining domain (Health and Wellbeing), was excluded from the revised measure in its entirety (26 items). MDS analysis indicated that these items did not correlate closely with one another as a cluster. Further, it was determined that health items should be measured independently of social inclusion to account for different health conditions, and allow for a clearer assessment of the relationship between both.
Twenty-five items diverging from their associated latent domain were excluded. For example, the item ‘Of the household members over the age of 18, are all currently employed or attending formal education?’ was found unrelated to the underlying HN domain. Finally, six items had a high degree of overlap with core items of the individual domain and were thus excluded. Thirty-three items remained at this point.
Further item reduction
CFA and IRT models of individual domains supported within-domain unidimensionality for the remaining 33 items. Four items from each domain were selected on the basis of higher factor loadings and lower residuals in the CFA model, and higher discriminant ability and ability to maximise item information in the IRT model. Where items had similar psychometric properties, those that better reflected the theoretical framework of social inclusion were chosen.
F-SIM16 measure
The final version of the measure comprised 16 core items, herein referred to as the F-SIM16. Table 2 contains an overview of items and associated short labels, with the full measure available upon request. An additional six items (not included in final scoring) were included as supplementary questions: two questions related to health and wellbeing (Do you feel your emotional/physical health interferes in your ability to achieve all you would like each day?), and four items related to satisfaction (not collected in the current study) with each of the domains. The supplementary questions provide an overview of the impact of health issues on functioning and satisfaction with domains of social inclusion, and will be validated in future studies.
Table 2.
Questions from the 16 item version of the F-SIM
| Short title | ID | Question content |
|---|---|---|
| Housing and neighbourhood (HN) | ||
| Stable housing | Q1 | Stability of housing |
| House lacking | Q2 | Housing lacking, making it difficult to live in |
| Location not liked | Q3 | Living in a less than ideal location |
| Neighbourhood lacking | Q4 | Neighbourhood lacking in some way |
| Social relationships, participation and limitations (SOC) | ||
| Good friends | Q5 | Good friends to share time, experiences, thoughts and feelings with |
| Don't enjoy | Q6 | Limited in participating socially due to a lack of enjoyment of social activities |
| Not participated long | Q7 | Limited in participating socially due to recent lack of participation in any social or community activities |
| Stigma | Q8 | Limited in participating socially due to regularly experiencing stigma and/or discrimination |
| Employment and education (EE) | ||
| Work/study | Q9 | Employment or education status |
| Good conditions | Q10 | Work/study under good conditions |
| Discrimination | Q11 | Limited ability to obtain or keep a job due to health-related discrimination |
| Impaired ability | Q12 | Impaired ability to perform your occupational role or disrupt employment |
| Finances (FIN) | ||
| Cover basic costs | Q13 | Enough income to cover basic everyday costs |
| Unable to participate | Q14 | Inability to participate in social activities due to income |
| Unable to attend events | Q15 | Inability to attend important events such as weddings, funerals, birthday celebrations due to income |
| Lack savings | Q16 | Lack of savings for use in an emergency |
| Supplementary health and wellbeing (HW) | ||
| Limited by physical health | Q1+ | Ongoing physical ailments that prevent you from achieving all you would like in your life |
| Limited by emotional health | Q2+ | Ongoing emotional health concerns that interfere in your ability to achieve all you would like in your life |
Psychometric evaluation of the F-SIM16
Inter-item correlations
Pairwise rtc between individual items within domains, item-to-total biserial correlations (rbs) and Cronbach's alpha within each domain are provided in Table 3. Inter-item correlations within each domain ranged from medium to strong. Item-to-total biserial correlations (rbs) ranged between 0.75 (HN and Stable housing) and 0.89 (FIN and Unable participate). Each domain showed strong internal consistency (α > 0.85) and the internal consistency for the 16 items was excellent (α = 0.92). Individual item correlations (provided in online Fig. S1 in Supplementary Material) were visualised using network analysis (see online Supplementary Fig. S2). Most items were closely related to items within their overarching domains. The Discrimination and Impaired ability items in the EE domain had moderate correlations with items in the SOC domain.
Table 3.
Inter-item tetrachoric correlations (rtc), item-to-total polyserial correlations (rbs) and Cronbach's alphas (α) for each social inclusion domain
| α | ||||||
|---|---|---|---|---|---|---|
| Housing and neighbourhood (HN) | rtc | rtc | rtc | rtc | rps | 0.929 |
| (1) | (2) | (3) | (4) | HN total score | ||
| Stable housing (1) | 1.000 | 0.747 | ||||
| House lackinga (2) | 0.896 | 1.000 | 0.795 | |||
| Location not likea (3) | 0.833 | 0.693 | 1.000 | 0.883 | ||
| Neighborhood lackinga (4) | 0.877 | 0.570 | 0.722 | 1.000 | 0.821 | |
| Social participation, relationships and limitations (SOC) | 0.854 | |||||
| (5) | (6) | (7) | (8) | SOC total score | ||
| Good friends (5) | 1.000 | 0.814 | ||||
| Don't enjoya (6) | 0.598 | 1.000 | 0.854 | |||
| Not participated longa (7) | 0.671 | 0.705 | 1.000 | 0.877 | ||
| Stigmaa (8) | 0.399 | 0.572 | 0.615 | 1.000 | 0.788 | |
| Employment and education (EE) | 0.877 | |||||
| (9) | (10) | (11) | (12) | EE total score | ||
| Work/study (9) | 1.000 | 0.810 | ||||
| Good conditions (10) | 0.999b | 1.000 | 0.861 | |||
| Discriminationa (11) | 0.449 | 0.589 | 1.000 | 0.835 | ||
| Impaired abilitya (12) | 0.427 | 0.530 | 0.853 | 1.000 | 0.854 | |
| Finances (FIN) | 0.918 | |||||
| (13) | (14) | (15) | (16) | FIN total score | ||
| Cover basic costs (13) | 1.000 | 0.797 | ||||
| Unable participatea (14) | 0.660 | 1.000 | 0.888 | |||
| Unable attend eventsa (15) | 0.620 | 0.857 | 1.000 | 0.871 | ||
| Lack savingsa (16) | 0.709 | 0.813 | 0.767 | 1.000 | 0.883 | |
rpc, tetrachoric correlation coefficient; rps, polyserial correlation coefficient; α, Cronbach's alpha.
Reverse scored.
High correlation here is related to these being nested questions, a high proportion of participants working suggested that they were working in a good condition.
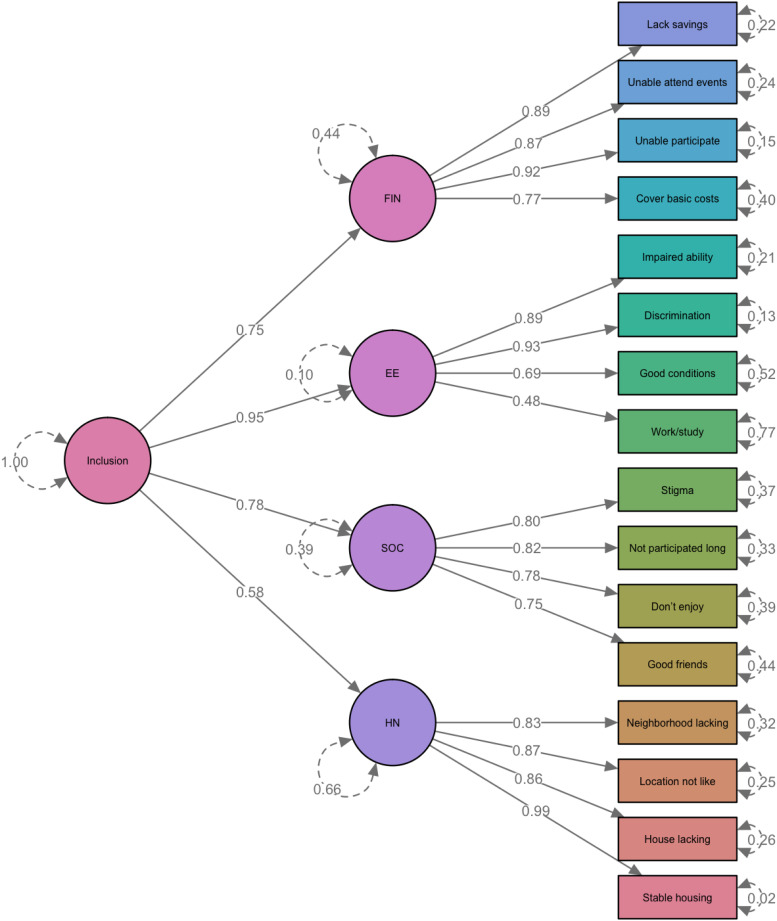
Overall instrument evaluation
Model fit indicators for the three CFA models are provided in online Supplementary Table S1. Both the four-factor and second-order models had an excellent fit with the data (RMSEA < 0.05; CFI/TLI > 0.95). With fewer parameters, the second-order model was preferred. Factor loadings and residual variances estimated for the second-order CFA are displayed in Fig. 2. The second-order model supports the calculation of domain scores, in addition to the total score.
Fig. 2.
Factor Loading and Residual Variance Estimated from the Second-order CFA Model. *Reverse scored items. CFA model was based on 488 records with complete data.
Group differences
Distributions of the F-SIM16 domain and total scores, as well as individual item responses by groups, are provided in online Supplementary Table S2 and Fig. S3. Young people with psychosis or other mental ill-health reported the lowest level of social inclusion in all domains, particularly in the SOC and FIN domains. Although a proportion of older participants from the clinical population reported a lower level of social inclusion, the subgroup experienced a similar level of inclusiveness compared with the general community (reflected by the bimodal distribution in SOC and FIN domain). Pairwise comparisons of the domain and total scores, as shown in online Supplementary Table S3, suggested that clinical subgroups consistently reported lower levels of social inclusion compared to community counterparts across all domains. Participants from the general community groups were more comparable in all domains irrespective of age, except for lower scores in the SOC domain among young people.
Test-retest reliability
The correlation coefficient (r) between baseline and follow-up scores of individual domains varied between 0.68 (HN) and 0.83 (EE and FIN; SOC 0.73). The F-SIM16 total score had a correlation (γ) of 0.90 between baseline and follow-up, indicative of high test-retest reliability.
Correlation with similar constructs
Both the SIS and UCLA Loneliness Scale had strong correlations with the F-SIM16 total score (r > 0.60) (online Supplementary Table S4). As expected, the SIS and UCLA-LS had low correlations with some of the F-SIM16 domains including FIN, EE and HN.
Discussion
Social inclusion is an important concept in mental health, particularly with an increasing focus on consumer-driven outcomes and recovery. To facilitate continued and meaningful progress, novel outcome measures are required. Here we reported on a novel measure of social inclusion, the F-SIM, detailing refinement to a 16-item form (the F-SIM16), using traditional and contemporary psychometric techniques.
The F-SIM16
The F-SIM16 is a brief, easy to use, self-report measure with sound psychometric properties validated in populations of younger and older people with mental ill-health and same-aged community peers. Items were selected using a combination of data and theory-driven approaches. As intentionally designed, items remain a combination of subjective and objective characteristics of social inclusion within each domain.
Psychometric analyses supported the four core domains of social inclusion, as identified in our earlier work (Filia et al., 2018) and endorsed by considerable stakeholder engagement (Filia et al., 2019a, 2019b). We observed high-level internal consistency within domains and an excellent second-order factor model fit, which supported the theoretical underpinnings of this multifarious concept. The cohesive network association also demonstrated multidimensionality, and highlighted interconnected elements.
The measure was found to have good discriminant ability, demonstrating differences in the domain and total scores across different populations, potentially reflective of the particular challenges these groups face as a result of age and/or experience of mental ill-health. This was particularly evident in findings that clinical groups (irrespective of age) reported poorer social inclusion than same-aged general community peers. Young clinical groups also reported lower levels of social inclusion overall compared with the older clinical group. This could indicate that over time older people with mental ill-health find ways of adapting to their circumstances, perhaps having secured stable accommodation, receiving and finding ways to manage finances, and connecting socially in ways that are meaningful to them.
The F-SIM16 demonstrated temporal robustness, making it an excellent tool for evaluating the impact of interventions.
Other measures of social inclusion
As the F-SIM16 was developed in response to an identified need for appropriate measures of social inclusion, so too were other measures, including the SIS (Stickley and Shaw, 2006; Lloyd et al., 2008; Dorer et al., 2009; Secker et al., 2009; Marino-Francis and Worrall-Davies, 2010; Huxley et al., 2012; Mezey et al., 2013). As per the F-SIM16, the development and evaluation of some of these measures have progressed (Huxley et al., 2015; Wilson and Secker, 2015; Mezey et al., 2020), yet none have reported a complete psychometric evaluation to date. Additional limitations include poor generalisability as a result of having been developed for use in specific settings (Stickley and Shaw, 2006; Dorer et al., 2009; Secker et al., 2009; Marino-Francis and Worrall-Davies, 2010) and imbalances in the inclusion of objective/subjective elements (either a greater focus on subjective measures [Stickley and Shaw, 2006; Lloyd et al., 2008; Secker et al., 2009; Marino-Francis and Worrall-Davies, 2010), or an entire focus on objective measures (Dorer et al., 2009)]. Stakeholder engagement also varied considerably, from comprehensive consultation on all stages of measure development (Stickley and Shaw, 2006), to engagement post-measure construction (Marino-Francis and Worrall-Davies, 2010; Mezey et al., 2013). Comparatively, the F-SIM16 possesses a solid theoretical foundation, significant stakeholder engagement during development and testing, generalisability across different groups, and a balance of subjective and objective components of social inclusion across multiple domains. Comparing the F-SIM to other measures indicated that it was the superior tool for measuring social inclusion as a multidimensional construct, with the UCLA-LS and SIS both appearing to measure one domain more generally (SOC).
Limitations
The main limitation of the current research relates to the psychometric evaluation utilising data collected from the original version of the F-SIM. Future studies are needed to further evaluate the psychometric properties of the F-SIM16, and assess the utility of the additional variables (health and wellbeing, and satisfaction with domains). A further limitation is that test-retest validity included a small sample of participants, in part due to low retention of participants. As a result, longitudinal patterns and responses to change are largely unknown. Additional research to address the above is needed.
Strengths and implications
Refining the F-SIM to the F-SIM16, provides a very useful tool with broad clinical and research utility. The F-SIM16 has the potential to contribute significantly to the broader understanding of social inclusion in mental ill-health, and to increase understanding of the dynamics between mental health and social inclusion. The brief, self-report nature enables the collection of wide-scale data via online approaches, ensuring accessibility and completion of the survey by those potentially most excluded, thus reducing bias in assessments, and at a low-cost.
The properties of the F-SIM16 enable the collection of sound empirical data, including data for at-risk, consumer groups and normative data. This implication is by far the most valuable, providing information on the distribution of scores across population groups, and identifying strengths and areas impacted in specific domains. Further, the inclusion of the additional questions related to individual's satisfaction with each domain will ensure we maintain an understanding of how personally satisfied individuals are with their unique circumstances.
The F-SIM16 will aid in determining the effectiveness of programs and interventions designed to improve social inclusion. It will allow for pre- and post-measurement, and the identification of those aspects of social inclusion most receptive to change. This will foster the development of more informed and relevant interventions. The ability to provide data about the extent of social inclusion in various populations (geographical, diagnostic, with respect to age, gender etc.) can inform policy development and service reform to improve both social inclusion, and the health and wellbeing of people with mental illness.
From a clinical perspective, this tool will assist in tailoring treatment plans, and determining the need for collaborative approaches to treatment. Completing a measure of social inclusion at the outset of treatment allows for the charting of progress across time and facilitates more holistic outcome measurement. Completion at routine time points, as well as at times of illness exacerbation, may assist in determining individual risk factors and the relationship between symptomatology and social inclusion, to aid in treatment and maintaining wellbeing.
Together these strengths demonstrate the significant contribution of the F-SIM16 to the field of mental health, with the potential for considerable impact by providing a more rigorously developed, comprehensive measure of social inclusion than previously available. Implementation of the F-SIM16 in research or clinical evaluations to determine treatment, service gaps and needs, and to target facilitators of social inclusion, has significant potential to improve the lives of people with SMI.
Financial support
This work was supported by The University of Melbourne internal grants scheme - ECR Project Grant and Melbourne Research Fellowship (KF).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures were approved by Melbourne Health Human Research and Ethics Committee HREC (2010.105; 2016.311, HREC/16/MH/325).
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796021000755.
click here to view supplementary material
Data
The data that support the findings of this study are available upon reasonable request from the corresponding author (KF) and subject to ethical approval/restrictions.
References
- Borsboom D and Cramer AO (2013) Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Connell J, O'Cathain A and Brazier J (2014) Measuring quality of life in mental health: are we asking the right questions? Social Science & Medicine 120, 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombs T, Nicholas A and Pirkis J (2013) A review of social inclusion measures. Australian and New Zealand Journal of Psychiatry 47, 906–919. [DOI] [PubMed] [Google Scholar]
- Cordier R, Milbourn B, Martin R, Buchanan A, Chung D and Speyer R (2017) A systematic review evaluating the psychometric properties of measures of social inclusion. PLoS One 12, e0179109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L (2016) The recovery movement: implications for mental health care and enabling people to participate fully in life. Health Affairs 35, 1091–1097. [DOI] [PubMed] [Google Scholar]
- Dorer G, Harries P and Marston L (2009) Measuring social inclusion: a staff survey of mental health service users’ participation in community occupations. British Journal of Occupational Therapy 72, 520–530. [Google Scholar]
- Filia K, Jackson HJ, Cotton SM, Gardner A and Killackey EJ (2018) What is social inclusion? A thematic analysis of professional opinion. Psychiatric Rehabilitation Journal 41, 183–195. [DOI] [PubMed] [Google Scholar]
- Filia K, Jackson H, Cotton S and Killackey E (2019a) Understanding what it means to be socially included for people with a lived experience of mental illness. International Journal of Social Psychiatry 65, 413–424. [DOI] [PubMed] [Google Scholar]
- Filia K, Jackson HJ, Cotton SM and Killackey EJ (2019b) Developing and testing the F-SIM, a measure of social inclusion for people with mental illness. Psychiatry Research 279, 1–8. [DOI] [PubMed] [Google Scholar]
- Filia K, Menssink J, Gao CX, Rickwood D, Hamilton M, Hetrick SE, Parker AG, Herrman H, Hickie I, Sharmin S, McGorry PD and Cotton SM (2021) Social inclusion, intersectionality, and profiles of vulnerable groups of young people seeking mental health support. Social Psychiatry and Psychiatric Epidemiology. doi: 10.1007/s00127-021-02123-8 [DOI] [PubMed] [Google Scholar]
- Gardner A, Cotton S, O'Donoghue B, Killackey E, Norton P and Filia K (2019) Group differences in social inclusion between young adults aged 18 to 25 with serious mental illness and same-aged peers from the general community. International Journal of Social Psychiatry 65, 631–642. [DOI] [PubMed] [Google Scholar]
- Gardner A, Cotton S, O'Donoghue B, Killackey E, Norton PJ and Filia K (2020) Preliminary psychometric properties of a measure of social inclusion for young adults aged 18 to 25 with serious mental illness. Psychiatric Rehabilitation Journal 43, 156–169. [DOI] [PubMed] [Google Scholar]
- Hooper D, Coughlan J and Mullen MR (2008) Structural equation modelling: guidelines for determining model fit. Electronic Journal of Business Research Methods 6, 53–59. [Google Scholar]
- Huxley P, Evans S, Madge S, Webber M, Burchardt T, McDaid D and Knapp M (2012) Development of a social inclusion index to capture subjective and objective domains (Phase II): psychometric development study. Health Technology Assessment 16, iii–vii, ix–xii, 1–241. [DOI] [PubMed] [Google Scholar]
- Huxley PJ, Chan K, Chiu M, Ma Y, Gaze S and Evans S (2015) The social and community opportunities profile social inclusion measure: structural equivalence and differential item functioning in community mental health residents in Hong Kong and the United Kingdom. International Journal of Social Psychiatry 62, 133–140. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Mair P and McNally RJ (2018) Visualizing psychological networks: a tutorial in R. Frontiers in Psychology 9, 1742. doi: 10.3389/fpsyg.2018.01742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Boutillier C, Leamy M, Bird VJ, Davidson L, Williams J and Slade M (2011) What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiatric Services 62, 1470–1476. [DOI] [PubMed] [Google Scholar]
- Lloyd C, Waghorn G, Best M and Gemmell S (2008) Reliability of a composite measure of social inclusion for people with psychiatric disabilities. Australian Occupational Therapy Journal 55, 47–56. [DOI] [PubMed] [Google Scholar]
- Marino-Francis F and Worrall-Davies A (2010) Development and validation of a social inclusion questionnaire to evaluate the impact of attending a modernised mental health day service. Mental Health Review Journal 15, 37–48. [Google Scholar]
- Mezey G, White S, Thachil A, Berg R, Kallumparam S, Nasiruddin O, Wright C and Killaspy H (2013) Development and preliminary validation of a measure of social inclusion for use in people with mental health problems: the SInQUE. International Journal of Social Psychiatry 59, 501–507. [DOI] [PubMed] [Google Scholar]
- Mezey G, White S, Harrison I, Bousfield J, Lloyd-Evans B, Payne S and Killaspy H (2020) Validity, reliability, acceptability, and utility of the Social Inclusion Questionnaire User Experience (SInQUE): a clinical tool to facilitate social inclusion amongst people with severe mental health problems. Social Psychiatry and Psychiatric Epidemiology 55, 953–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan C, Burns T, Fitzpatrick R, Pinfold V and Priebe S (2007) Social exclusion and mental health. British Journal of Psychiatry 191, 477–483. [DOI] [PubMed] [Google Scholar]
- O'Donnell P, O'Donovan D and Elmusharaf K (2018) Measuring social exclusion in healthcare settings: a scoping review. International Journal for Equity in Health 17, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Productivity Commission (2019) The Social and Economic Benefits of Improving Mental Health. Canberra, ACT, Australia: Australian Government. [Google Scholar]
- Robotham D, Wykes T, Rose D, Doughty L, Strange S, Neale J and Hotopf M (2016) Service user and carer priorities in a biomedical research centre for mental health. Journal of Mental Health 25, 185–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (1996) UCLA loneliness scale (version 3): reliability, validity, and factor structure. Journal of Personality Assessment 66, 20–40. [DOI] [PubMed] [Google Scholar]
- Secker J, Hacking S, Kent L, Shenton J and Spandler H (2009) Development of a measure of social inclusion for arts and mental health project participants. Journal of Mental Health 18, 65–72. [Google Scholar]
- Slade M, Amering M, Farkas M, Hamilton B, O'Hagan M, Panther G, Perkins R, Shepherd G, Tse S and Whitley R (2014) Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry 13, 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stickley T and Shaw R (2006) Evaluating social inclusion. Mental Health Practice 9, 14–20. [Google Scholar]
- van Os J, Guloksuz S, Vijn TW, Hafkenscheid A and Delespaul P (2019) The evidence-based group-level symptom-reduction model as the organizing principle for mental health care: time for change? World Psychiatry 18, 88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson C and Secker J (2015) Validation of the social inclusion scale with students. Social Inclusion 3, 52–62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796021000755.
click here to view supplementary material
Data Availability Statement
The data that support the findings of this study are available upon reasonable request from the corresponding author (KF) and subject to ethical approval/restrictions.