Abstract
Aims
The clinical outcomes of individuals at clinical high risk of psychosis (CHR-P) who do not transition to psychosis are heterogeneous and inconsistently reported. We aimed to comprehensively evaluate longitudinally a wide range of outcomes in CHR-P individuals not developing psychosis.
Methods
“Preferred Reporting Items for Systematic reviews and Meta-Analyses” and “Meta-analysis Of Observational Studies in Epidemiology”-compliant meta-analysis (PROSPERO: CRD42021229212) searching original CHR-P longitudinal studies in PubMed and Web of Science databases up to 01/11/2021. As primary analysis, we evaluated the following outcomes within CHR-P non-transitioning individuals: (a) change in the severity of attenuated psychotic symptoms (Hedge's g); (b) change in the severity of negative psychotic symptoms (Hedge's g); (c) change in the severity of depressive symptoms (Hedge's g); (d) change in the level of functioning (Hedge's g); (e) frequency of remission (at follow-up). As a secondary analysis, we compared these outcomes in those CHR-P individuals who did not transition vs. those who did transition to psychosis at follow-up. We conducted random-effects model meta-analyses, sensitivity analyses, heterogeneity analyses, meta-regressions and publication bias assessment. The risk of bias was assessed using a modified version of the Newcastle-Ottawa Scale (NOS).
Results
Twenty-eight studies were included (2756 CHR-P individuals, mean age = 20.4, 45.5% females). The mean duration of follow-up of the included studies was of 30.7 months. Primary analysis: attenuated psychotic symptoms [Hedges’ g = 1.410, 95% confidence interval (CI) 1.002–1.818]; negative psychotic symptoms (Hedges’ g = 0.683, 95% CI 0.371–0.995); depressive symptoms (Hedges’ g = 0.844, 95% CI 0.371–1.317); and functioning (Hedges’ g = 0.776, 95% CI 0.463–1.089) improved in CHR-P non-transitioning individuals; 48.7% remitted at follow-up (95% CI 39.3–58.2%). Secondary analysis: attenuated psychotic symptoms (Hedges’ g = 0.706, 95% CI 0.091–1.322) and functioning (Hedges’ g = 0.623, 95% CI 0.375–0.871) improved in CHR-P individuals not-transitioning compared to those transitioning to psychosis, but there were no differences in negative or depressive symptoms or frequency of remission (p > 0.05). Older age was associated with higher improvements of attenuated psychotic symptoms (β = 0.225, p = 0.012); publication years were associated with a higher improvement of functioning (β = −0.124, p = 0.0026); a lower proportion of Brief Limited Intermittent Psychotic Symptoms was associated with higher frequencies of remission (β = −0.054, p = 0.0085). There was no metaregression impact for study continent, the psychometric instrument used, the quality of the study or proportion of females. The NOS scores were 4.4 ± 0.9, ranging from 3 to 6, revealing the moderate quality of the included studies.
Conclusions
Clinical outcomes improve in CHR-P individuals not transitioning to psychosis but only less than half remit over time. Sustained clinical attention should be provided in the longer term to monitor these outcomes.
Keywords: Psychosis, clinical high risk, clinical outcomes, progression, transition, meta-analysis
Introduction
Indicated prevention in individuals at clinical high risk for psychosis (CHR-P) is one of the most promising primary preventive approaches in psychiatry (Fusar-Poli et al., 2017b). CHR-P individuals are young and they accumulate risk factors such as living alone or being unemployed (Fusar-Poli et al., 2017e; Radua et al., 2018; Oliver et al., 2019) that enrich their level of risk for psychosis (Fusar-Poli et al., 2016c). In turn, this can lead to functional impairments (Fusar-Poli et al., 2015c) and the onset of attenuated psychotic symptoms (Fusar-Poli et al., 2017c). The distress associated with these experiences can prompt CHR-P individuals to seek help (Falkenberg et al., 2015) at specialised mental health clinics (Kotlicka-Antczak et al., 2020; Salazar de Pablo et al., 2021a). In these clinics, the prognosis is formulated reaching very good accuracy using psychometric instruments (Fusar-Poli et al., 2015a).
The majority of CHR-P individuals do not transition to psychosis within the first 2 years of presentation. After 2 years, 16% of CHR-P individuals transition to psychosis, and the transition risk continues to rise until about 4 years of follow-up, reaching 36% at 10–11 years (Salazar de Pablo et al., 2021c). Clinical outcomes in CHR-P individuals who do not transition to psychosis remain scattered, heterogeneous and inconsistent (Simon et al., 2011). It remains unclear how many will improve, permanently or only temporarily (Schultze-Lutter, 2009; Fusar-Poli et al., 2013), or whether the poor mental health outcomes observed are mostly driven by the presence of transitioning CHR-P individuals. Longitudinal research comparing individuals who develop psychosis with those who do not is overall inconsistent (Fusar-Poli et al., 2013).
Following an earlier meta-analysis, published 10 years ago, evaluating the proportion of individuals who do not transition to psychosis and the frequency of remission (Simon et al., 2011), a more recent update found that 28–71% of CHR-P individuals who do not transition to psychosis, do not remit from their CHR-P either and 22–82% still have one or more clinical diagnosis in the long-term (Beck et al., 2019a). Additional meta-analyses have focused on other clinical outcomes in all CHR-P individuals (transitioning and non-transitioning individuals), including the level of functioning (Fusar-Poli et al., 2015c, 2017e), quality of life (Fusar-Poli et al., 2015c), comorbid disorders (Albert et al., 2018) and remission (Simon et al., 2013). However, no comprehensive meta-analysis has addressed these outcomes together in individuals at CHR-P not developing psychosis. Also, no meta-analysis has evaluated outcomes in CHR-P individuals not transitioning to psychosis, comparing to those developing it. We aimed to comprehensively assess the broad longitudinal clinical outcomes of attenuated psychotic symptoms, negative symptoms, depressive symptoms, functioning and remission in CHR-P individuals who did not transition to psychosis. Furthermore, we aimed to compare these outcomes between those CHR-P transitioning or not to psychosis, while controlling for some potential moderators.
Methods
The protocol for this study was registered on PROSPERO (CRD42021229212). This study was conducted in accordance with the ‘Preferred Reporting Items for Systematic reviews and Meta-Analyses’ (PRISMA) (Moher et al., 2009) (online Supplementary eTable 1), ‘Meta-analysis Of Observational Studies in Epidemiology’ (MOOSE) (Stroup et al., 2000) (online Supplementary eTable 2) and ‘Reporting Tool for Practice Guidelines in Health Care’ (RIGHT) (Chen et al., 2017) statements.
Literature search
A multi-step literature search from inception until 1 November 2020 was performed by independent researchers on PubMed and on the Web of Science database (Clarivate Analytics), which incorporates the Web of Science Core Collection, MEDLINE, BIOSIS Citation Index, KCI-Korean Journal Database, Russian Science Citation Index and SciELO Citation Index.
The following search terms were applied: ‘risk’ OR ‘prodrom*’ OR ‘prediction’ OR ‘onset’ OR ‘ultra-high risk’ OR ‘clinical high risk’ OR ‘attenuat*’ OR ‘APS’ OR ‘high risk’ OR ‘BLIPS’ OR ‘brief limited’ OR ‘brief intermitent’ OR ‘genetic high risk’ OR ‘GRD’ OR ‘at risk mental state’ OR ‘risk of progression’ OR ‘progression to first-episode’ OR ‘basic symptoms’ AND ‘psychosis’ OR ‘schizophrenia’ OR ‘schizoaffective’. We manually reviewed the references of previously published meta-analyses and extracted additional relevant titles. Articles identified were reviewed as abstracts. The full texts of the relevant manuscripts were assessed for eligibility. After the exclusion of those that did not meet our inclusion criteria, final decisions were made regarding their inclusion in the meta-analysis. Disagreements in selection criteria were resolved through discussion and consensus.
Condition and individuals being studied
Studies included were (a) original articles; (b) conducted on CHR-P individuals according to established psychometric instruments (online Supplementary eMethods 1); (c) conducted on CHR-P individuals who did not transition to psychosis (compared or not with those transitioning to psychosis, online Supplementary eMethods 1); (d) cohort studies that provided longitudinal (baseline and follow-up data) (see online Supplementary eMethods 2); (e) published in English.
Studies excluded were (a) review papers, clinical case studies, conference proceedings, study protocols or grey literature; (b) studies conducted on individuals not formally assessed for CHR-P criteria, including those with a schizotypal personality disorder or those with a genetic risk for psychosis (twins, first- or second-degree relatives) without impaired functioning; (c) studies in which transition status at follow-up was not reported; (d) cross-sectional studies; (e) studies in another language other than English; (f) overlapping studies. When a study included data on both individuals who transitioned to psychosis and those who did not, the study was only included if it provided independent stratified outcome results for the two groups of participants. Randomised controlled trials were included using only the placebo/needs-based intervention arm, if available. When there were two or more studies from the same centre, we contacted the authors to clarify whether there was an overlap in the respective samples and the largest and most recent sample was retained.
Outcomes
Outcomes measured were: (a) change (baseline to follow-up) in the severity of attenuated psychotic symptoms; (b) change (baseline to follow-up) in the severity of negative symptoms; (c) change (baseline to follow-up) in the severity of depressive symptoms; (d) change (baseline to follow-up) in the level of functioning; (e) frequency of remission (at follow-up). These outcomes were operationalised as indicated in online Supplementary eTable 3.
Data extraction and descriptive variables
Independent researchers extracted data from all the included studies into a database. The data were then cross-checked by a third researcher to ensure high quality of data extraction. Descriptive variables included the following information (more details can be found in online Supplementary eMethods 2): first author and year of publication; country; design; CHR-P sample size; CHR-P subgroups; age; sex; CHR-P assessment tools (see online Supplementary eMethods 1); follow up period; outcome data (at baseline and at follow-up); duration of untreated attenuated psychotic symptoms; transition status; International Classification of Diseases (ICD)-defined (World Health Organization, 2018) or Diagnostic and Statistical Manual of Mental Disorders (DSM)-defined (American Psychiatric Association, 2013) comorbidity; exposure to baseline interventions. For each outcome, data (severity or levels for outcomes a-d and raw counts for outcome e) were extracted at baseline and at 12 months (6–17.9 months); 24 months (18–35.9 months); ⩾36 months follow-up. These outcome data were extracted for both individuals who did not transition and those who did transition to psychosis.
Risk of bias (quality) assessment
The risk of bias was assessed using a modified version of the Newcastle-Ottawa Scale (NOS) for cohort studies. Studies were awarded 0–8 points according to their representativeness, exposure, outcomes, follow-up period and losses to follow-up (online Supplementary eTable 4).
Strategy for data synthesis
The primary analysis focused on outcomes within CHR-P individuals who did not transition to psychosis: (a) change (baseline to follow-up) in the severity of attenuated psychotic symptoms; (b) change (baseline to follow-up) in the severity of negative symptoms; (c) change (baseline to follow-up) in the severity of depressive symptoms; (d) change (baseline to follow-up) in the level of functioning, (e) frequency of remission (at follow-up). Outcomes a-d were estimated using the Hedges’ g (Hedges, 2007), with positive values indexing improvements from baseline to 12, 24 or ⩾36 months follow-up. These time points were initially pooled using the last follow-up time; however, we also presented sensitivity analyses stratified by follow-up time (when at least three studies per follow-up were available). Hedges’ g values were interpreted as small (g = 0.2), medium (g = 0.5) or large (g = 0.8) effect sizes (Cohen, 1988; Hedges, 2007). Outcome e was estimated through the meta-analytical proportion [95% confidence interval (CI)] of remission in our primary outcome and OR (95% CI) in our secondary outcome.
The secondary analysis compared outcomes a–e across CHR-P individuals who developed psychosis and those who did not. Outcomes a-d were again measured with Hedge's g, with positive values indicating improvements in those non-transitioning compared to those transitioning. Outcome e was analysed with OR, with values greater than 1 indexing higher frequencies in those transitioning compared to those non-transitioning. Secondary analyses were conducted only when there were at least two studies per outcome comparing transitioning and non-transitioning individuals.
Because the studies were expected to be heterogeneous, meta-analytical random-effects models were used. Heterogeneity among study point estimates was assessed with the Q statistic. The magnitude of heterogeneity was evaluated with the I2 index. For the primary and secondary analyses, outcomes (a) to (d), publication bias was examined by visually inspecting funnel plots and applying the regression intercept of Egger for outcomes (Higgins et al., 2011). Publication bias is not typically assessed for proportions -outcome (e)-, as there are no undesirable or negative results that may have biased publications (Maulik et al., 2011); however, we tested this by conducting a meta-regression of the effect size on study's sample size. Meta-regressions were performed, when at least seven studies per outcome were available. We investigated the influence of the following factors: continent (Europe vs. North America vs. Other); type of psychometric instrument (CAARMS vs. SIPS vs. Other); quality of the study (NOS total score); CHR-P subgroups: (a) proportion of Attenuated Psychosis Symptoms (APS), (b) proportion of Brief and Limited Intermittent Psychotic Symptoms (BLIPS), (c) proportion of Genetic Risk and Deterioration syndrome (GRD), (d) proportion of Basic Symptoms (BS); mean age; sex (% female); year of publication; duration of untreated attenuated psychotic symptoms; ICD or DSM-defined comorbidity; exposure to baseline interventions. The significance level was set at α = 0.05, and all tests were two-tailed. Heterogeneity was considered significant when p < 0.10 (Fletcher, 2007). Comprehensive Meta-Analysis Software, version 3 (Biostat, Inc) was used for the analyses (Borenstein et al., 2013).
Results
Characteristics of the database
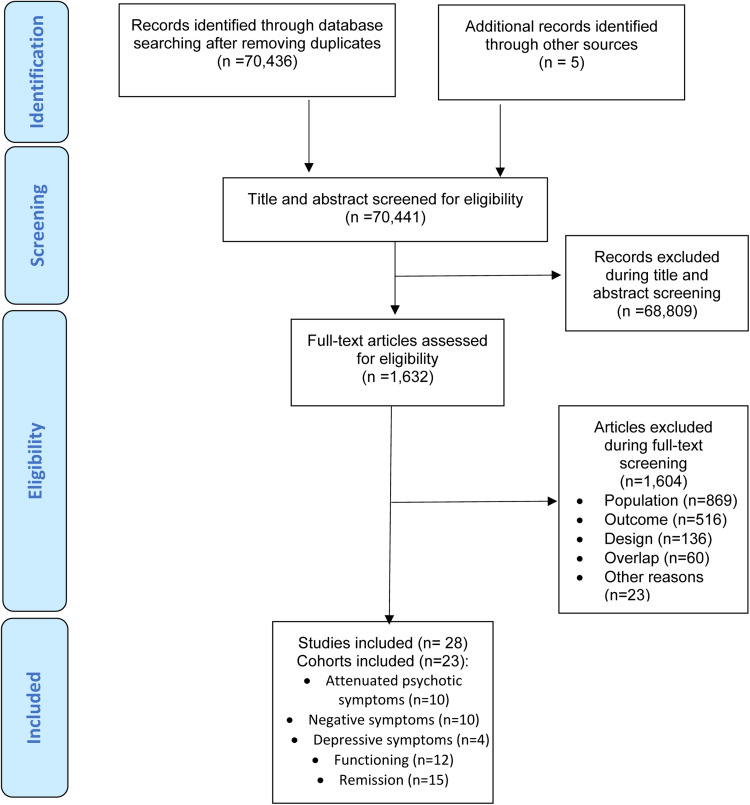
The literature search yielded 70 441 citations after removing duplicates, which were screened for eligibility. Of those, 1632 were assessed for eligibility at full text. After excluding 1604 studies, 28 studies – 27 (96.4%) longitudinal cohorts and 1 (3.6%) randomised clinical trial- fulfilling our inclusion criteria from 23 cohorts were included in at least one of the meta-analysis (in descending order of frequency): 10 cohorts provided attenuated psychotic symptoms data, 10 cohorts provided negative psychotic symptoms data, four cohorts provided depressive symptoms, 12 cohorts provided functioning data, data and 15 cohorts provided remission data (Fig. 1). Of the 23 cohorts, 11 (47.8%) were conducted in Europe, six (26.1%) in North America, four (17.5%) in Asia, one (4.3%) in Australia and one (4.3%) in more than one continent. The mean duration of the follow-up of the included studies was 30.7 months (range 6–192 months). The overall database comprised 2756 CHR-P individuals (mean age = 20.4 years, 45.5% females) (Table 1, online Supplementary eTable 5).
Fig. 1.
PRISMA Flowchart Outlining Study Selection Process.
Table 1.
Characteristics of the included studiesa
| First author, year | Country, Continent | Design | CHR-P sample size | CHR-P subgroups | Age: mean (s.d.), range [years] | Sex: % female | CHR-P assessment tools | Total duration of follow-up [months] | NOS |
|---|---|---|---|---|---|---|---|---|---|
| Addington et al. (2011) | USA | Longitudinal cohort | 303 | N.a. | 18 (4.9), 12–36 | 44.0 | SIPS/SOPS | 30 | 4 |
| Addington et al. (2019) | Multi | Longitudinal cohort | 278 | N.a. | 18,8 (4.4) | 44.4 | SIPS/SOPS | 24 | 4 |
| Armando et al. (2015) | Italy | Longitudinal cohort | 35 | 82.9% APS, 14.3% BLIPS, 11.4% GRD | 13.8 (2.1), 9–17 | 48.6 | SIPS/SOPS | 12 | 5 |
| Beck et al. (2019b) | Switzerland | Longitudinal cohort | 255 | N.a. | 24.1 (8.2), 14–57 | 59.0 | SIPS/SOPS | 192 | 3 |
| Cannon et al. (2015) | Multi | Longitudinal cohort | 274 | N.a. | 19.6 (4.2) | 37.6 | SIPS/SOPS | 12 | 5 |
| Chen et al. (2016) | China | Longitudinal cohort | 63 | 100% APS | 21.9 (4.5), 14–30 | 47.6 | SIPS/SOPS | 6 | 4 |
| Cotter et al. (2017) | Australia | Longitudinal cohort | 268 | 70.5% APS, 11.2% BLIPS, 24.6% GRD | 18.6 (2.3), 15–30 | 48.9 | CAARMS | 178.4 | 5 |
| de Wit et al. (2014) | Netherlands | Longitudinal cohort | 44 | N.a. | 14.9; 2.2, 12–18 | 47.1 | SIPS/SOPS | 72 | 4 |
| Falkenberg et al. (2017) | UK | Longitudinal cohort | 34 | N.a. | 22.0, 14–35 | 29.4 | CAARMS | 24 | 4 |
| Guo et al. (2019) | USA | Longitudinal cohort | 117 | N.a. | 16.6 (3.5), 12–25 | 42.7 | SIPS/SOPS | 12 | 4 |
| Kline et al. (2016) | USA | Longitudinal cohort | 21 | N.a. | 16.2 (3.1), 12–22 | 65.0 | SIPS/SOPS | 6 | 3 |
| Landa et al. (2016) | USA | Longitudinal cohort | 6 | 66.7% APS, 16.7% BLIPS, 16.7% GRD | 19.5 (1.5), 16–21 | 66.7 | CAARMS | 6.7 | 3 |
| Lemos-Giráldez et al. (2009) | Spain | Longitudinal cohort | 61 | 85.2% APS, 4.9% BLIPS, 9.8% GRD | 21.7 (3.8), 15–31 | 34.4 | SIPS/SOPS | 36 | 5 |
| Lin et al. (2013) | Australia | Longitudinal cohort | 325 | 79.7% APS, 13.5% BLIPS, 28.6% GRD | 19.1 (3.3), 15–30 | 52.9 | CAARMS | 178.3b | 5 |
| Michel et al. (2018) | Germany | Longitudinal cohort | 194 | 95.9% APS, 12.9% BLIPS, 1.0% GRD, 34.5% BS | 25.3 (5.9), 16.6–39.7 | 37.0 | SIPS/SOPS | 55.9b | 4 |
| Mittal et al. (2010) | USA | Longitudinal cohort | 90 | N.a. | 15.6 (3.0), 11–29 | 32.2 | SIPS/SOPS | 24 | 5 |
| Mongan et al. (2020) | Multi | Longitudinal cohort | 133 | N.a. | 22.6 (4.5) | 49.0 | CAARMS | 24 | 6 |
| Pelizza et al. (2019) | Italy | Longitudinal cohort | 55 | 90.9% APS, 5.5% BLIPS. 30.9% GRD | 18.4 (4.9), 13–35 | 49.2 | CAARMS, PANSS | 12 | 6 |
| Phillips et al. (2007) | Australia | Randomised clinical trial | 17 | N.a. | N.a., 14–30 | N.a. | BPRS, SANS | 48 | 5 |
| Rüsch et al. (2015) | Switzerland | Longitudinal cohort | 172 | N.a. | 21.4 (5.8), 13–35 | 41.0 | SIPS/SOPS | 12 | 3 |
| Rutigliano et al. (2016) | UK | Longitudinal cohort | 154 | 83.8% APS, 16.2% BLIPS | 23.4 (4.6), 14–35 | 39.6 | CAARMS | 120 | 4 |
| Ryan et al. (2017) | Australia | Longitudinal cohort | 180 | 83.3% APS, 2.8% BLIPS, 23.3% GRD | 18.2 (2.7), 15–24 | 62.8 | CAARMS | 12 | 5 |
| Sawada et al. (2017) | Japan | Longitudinal cohort | 47 | N.a. | 19.9, 3.5, 12–30 | 52.9 | SIPS/SOPS | 54 | 5 |
| Shi et al. (2016) | China | Longitudinal cohort | 32 | N.a. | 18.8 (1.1) | 59.4 | SIPS/SOPS | 6 | 5 |
| Velthorst et al. (2011) | Netherlands | Longitudinal cohort | 77 | N.a. | 19.2 (3.8), 12–35 | 33.8 | SIPS/SOPS | 36 | 5 |
| Yee et al. (2018) | Singapore | Longitudinal cohort | 211 | N.a. | 21.8 (3.6), 14–29 | 32.4 | CAARMS | 24 | 3 |
| Zhang et al. (2017) | China | Longitudinal cohort | 117 | 78.6% APS, 3.4% BLIPS, 23.1% GRD | 24.7 (7.6), 15–45 | 52.1 | SIPS/SOPS | 28.3b | 4 |
| Ziermans et al. (2011) | Netherlands | Longitudinal cohort | 72 | N.a. | 15.3 (1.9), 12–18 | 38.9 | SIPS/SOPS | 24 | 4 |
APS, Attenuated Psychosis Symptoms; BLIPS, Brief Limited Intermittent Psychotic Symptoms; BS, Basic symptoms; CAARMS, Comprehensive Assessment of At-Risk Mental States; CHR-P, Clinical high risk of psychosis; GRD, Genetic risk and deterioration syndrome; NOS, Newcastle-Ottawa Scale; PANSS, Positive and Negative Syndrome Scale; SIPS, Structured Interview for Prodromal Syndromes.
Overlapping samples can contribute with different outcomes.
Mean duration of follow-up.
Clinical outcomes within CHR-P individuals non-transitioning to psychosis
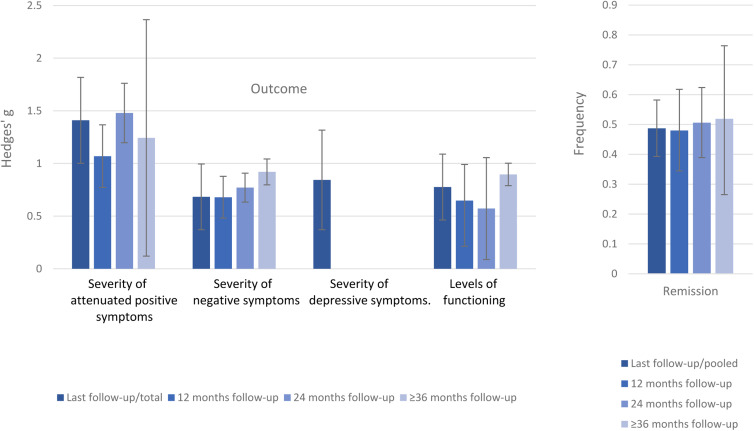
Within CHR-P individuals not transitioning to psychosis, there was a baseline to follow-up improvement in attenuated psychotic symptoms (k = 10, n = 872, Hedges’ g = 1.410, 95% CI 1.002–1.818), negative psychotic symptoms (k = 10, n = 872, Hedges’ g = 0.683, 95% CI 0.371–0.995); depressive symptoms (k = 4, n = 301, Hedges’ g = 0.844, 95% CI 0.371–1.317) (online Supplementary eTable 6, Fig. 2) and functioning (k = 12, n = 1095, Hedges’ g = 0.776, 95% CI 0.463–1.089). The frequency of remission was 48.7% (95% CI 39.3–58.2%) (k = 15, n = 1219).
Fig. 2.
Clinical outcomes CHR-P individuals who do not transition to psychosis. Positive values of Hedge's g indicate improvements at follow-up compared to baseline.
In the sensitivity analyses stratified by follow-up time, attenuated psychotic symptoms improved at 12- (Hedges' g = 1.069, 95% CI 0.772–1.367), 24- (Hedges’ g = 1.479, 95% CI 1.197–1.761) and ⩾36 months follow-up (Hedges’ g = 1.243 95% CI 0.120–2.366). Negative psychotic symptoms improved at 12- (Hedges’ g = 0.679, 95% CI 0.481–0.878), 24- (Hedges’ g = 0.771, 95% CI 0.633–0.908) and ⩾36 months follow-up (Hedges’ g = 0.920, 95% CI 0.797–1.043). Functioning improved at 12- (Hedges’ g = 0.647, 95% CI 0.393–0.991), 24- (Hedges’ g = 0.572, 95% CI 0.086–1.058) and ⩾36 months follow-up (Hedges’ g = 0.896, 95% CI 0.779–1.012). The frequency of remission was 48.0% (95% CI 34.5–61.8%) after 12 months, 50.6% (95% CI 38.9–62.4%) after 24 months and 51.9% (95% CI 26.5–76.4%) after ⩾36 months. For depressive symptoms, there were not enough data to conduct sensitivity analyses (online Supplementary eTable 6, Fig. 2).
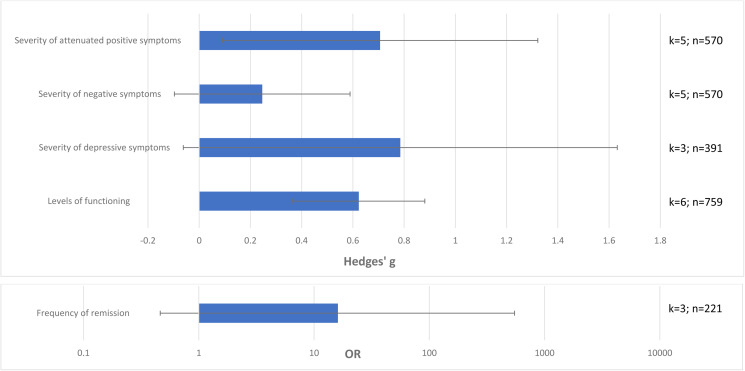
Clinical outcomes in CHR-P non-transitioning v. those transitioning to psychosis
Attenuated psychotic symptoms (k = 5, n = 570, Hedges’ g = 0.706, 95% CI 0.091–1.322) and functioning (k = 6, n = 759, Hedges’ g = 0.623, 95% CI 0.375–0.871) improved in CHR-P individuals who did not transition to psychosis compared to those who transitioned to psychosis. There were no statistically significant differences in negative symptoms (k = 5, n = 570, Hedges’ g = 0.246, 95% CI −0.097 to 0.589), depressive symptoms (k = 3, n = 391, Hedges’ g = 0.785, 95% CI −0.062 to 1.632) or frequency of remission (k = 3, n = 221, OR = 16.110, 95% CI 0.473–549.02) between CHR-P individuals who did not transition to psychosis and those transitioning to psychosis (online Supplementary eTable 7, Fig. 3).
Fig. 3.
Clinical outcomes in CHR-P individuals not-transitioning to psychosis vs. those transitioning to psychosis at follow-up, with 95% CIs. Positive values of Hedge's g or OR indicate higher improvements in CHR-P individuals not transitioning to psychosis v. those transitioning to psychosis.
Heterogeneity and publication bias
Heterogeneity was statistically significant for all of the primary analyses (p < 0.10), ranging from 79.488 (depressive symptoms) to 94.681% (functioning). Heterogeneity was also significant for all the secondary analyses, ranging from 15.823 (functioning) to 92.142% (attenuated psychotic symptoms). Egger's test was not significant for the primary analysis and secondary analyses (p > 0.05) (online Supplementary eTables 6 and 7).
Quality assessment and meta-regressions
The NOS scores were 4.4 ± 0.9, ranging from 3 to 6, revealing the moderate quality of the included studies. Older age was associated with higher improvements of attenuated psychotic symptoms (β = 0.225, p = 0.012). Publication year was associated with a higher improvement of functioning (β = −0.124, p = 0.0026). Finally, a lower proportion of Brief Limited Intermittent Psychotic Symptoms was associated with higher frequencies of remission (β = −0.054, p = 0.0085). The meta-regressions did not reveal any significant association between the study continent, the psychometric instrument used, the quality of the study or the proportion of females (all p > 0.05) (online Supplementary eTable 8). There were not enough data to perform meta-regressions for the duration of untreated attenuated psychotic symptoms, ICD or DSM-defined comorbidity or exposure to baseline interventions.
Discussion
To our knowledge, this is the first meta-analysis to comprehensively evaluate numerous clinical outcomes (attenuated psychotic symptoms, negative symptoms, depressive symptoms, functioning and remission) in CHR-P individuals who do not transition to psychosis. Evaluating 2756 CHR-P individuals from 23 prospective cohorts, we showed that, although CHR-P individuals improved on several outcomes, more than half of them did not reach remission.
The main finding of this meta-analysis is to have demonstrated a variable improvement of clinical outcomes over follow-up. The effect size for the improvement in the evaluated outcomes was large for attenuated psychotic symptoms (Hedges’ g = 1.410) and depressive symptoms (Hedges’ g = 0.844), and medium for negative psychotic symptoms (Hedges’ g = 0.683). Furthermore, there was a medium effect size for functional improvements (Hedges’ g = 0.776). The large effect size improvements in attenuated psychotic symptoms compared to other outcomes may be explained by a better therapeutic response for positive symptoms, which tends to respond better to antipsychotic medication or cognitive-behavioural therapy, compared to other outcomes such as negative symptoms (Woodward et al., 2014). However, there is no convincing evidence suggesting that specific preventive interventions can specifically improve attenuated (as opposed to established) psychotic symptoms better than others, including needs-based interventions (Davies et al., 2018; Fusar-Poli et al., 2019a, 2020c). A specific concern relates to the impact of antipsychotics in CHR-P individuals, which appears to be largely secondary to the high comorbidities accumulated and their transdiagnostic impact on the clinical presentation (Salazar de Pablo et al., 2020b; Fusar-Poli and Salazar de Pablo, 2021). Similarly, depressive symptoms seem to improve over time, which is relevant clinically given that depression and anxiety are common reasons for seeking help in CHR-P individuals (Falkenberg et al., 2015). Furthermore, previous meta-analytical evidence suggests that 40.7% of CHR-P individuals (Fusar-Poli et al., 2014) and 49% of individuals with DSM-5 Attenuated Psychosis Syndrome (Salazar de Pablo et al., 2019) present with comorbid depressive disorders. Previous studies have indicated that persistence of depression in CHR-P individuals is associated with decreased remission from a CHR-P status (Rutigliano et al., 2016; Kline et al., 2018; Fusar-Poli et al., 2019c). Depression is also associated with more pronounced negative psychotic symptoms and general symptoms, and it may contribute beyond the impact of positive and negative symptoms to impairments in social functioning (Fusar-Poli et al., 2014). Despite these findings, depressive symptoms do not lead to an increased risk of developing psychosis in CHR-P individuals (Fusar-Poli et al., 2014). Improvements on negative findings were less marked but still significant. We also showed that negative symptom improvements in CHR-P individuals who do not transition are of similar magnitude to those observed in individuals with schizophrenia (ES = 0.66) (Savill et al., 2015). Negative symptoms are often the first symptoms that CHR-P individuals develop (Metzak et al., 2020). There is a strong negative relationship between negative symptoms and functioning in CHR-P individuals (Devoe et al., 2020; Metzak et al., 2020), a finding also confirmed in individuals with schizophrenia (Ventura et al., 2009). Therefore, the observed clinical improvements in the severity of core CHR-P symptoms were paralleled by functional improvements at follow-up. It is well established that, similar to other psychiatric disorders, functional impairments are common in CHR-P individuals (Fusar-Poli et al., 2015c). However, the functional improvement may not be sufficient to reach the full functional remission (see below). Previous evidence on CHR-P individuals not transitioning to psychosis indicated that 45.3% of them still remain functionally impaired after 6 years (Rutigliano et al., 2016). This is not surprising given the lack of robust interventions to improve functional outcomes in this population.
Another core finding of this meta-analysis is to have complemented the analysis of continuous outcomes such as the severity of symptoms or levels of functioning with other real-world categorical outcomes that are directly informative of clinical care. In fact, statistically significant improvements of attenuated psychotic symptoms, depressive or negative symptoms and functioning do not automatically translate into tangible benefits for the lives of CHR-P individuals. This phenomenon has already been observed in psychopharmacological interventions for negative symptoms in schizophrenia, where statistically significant improvements were associated with negligible patient-level perceived improvements (Fusar-Poli et al., 2015b). Indeed, despite the symptomatic and functional improvements observed above, our meta-analytic frequency of remission indicates that only less than half (48.7%) of CHR-P not developing psychosis eventually remitted at follow-up. Our results align with a systematic review which found that 28–71% of CHR-P individuals who do not transition to psychosis, do not achieve remission (Beck et al., 2019a). Our increased frequencies of remission are due to the exclusion of CHR-P individuals who transitioned to psychosis. Interestingly, our frequency of remitters appeared lower than that observed during a first episode of psychosis (58% at 66 months) (Lally et al., 2017). This conflicts with one of the core foundations of the clinical staging model, which assumes that early stages are associated with a more favourable outcome and the likelihood of remission (Fusar-Poli et al., 2017b). Future research is required to address this issue.
According to our sensitivity analyses, frequencies of remission do not substantially increase throughout the follow-up. Improvements in functioning, attenuated psychotic symptoms and negative symptoms are also variable, without a significant pattern towards a prolonged improvement. This suggests that preventive interventions and monitoring may be needed in the long-term to support CHR-P individuals who do not remit, and individuals with negative symptoms and poor functioning. Currently, only 27.6% of clinical services to prevent psychosis provide care for more than 24 months (Salazar de Pablo et al., 2021a). Unfortunately, 2 years of care is not sufficient to capture the very real long-term clinical outcomes of this vulnerable population (Fusar-Poli et al., 2020b). A need for specialised services to detect CHR-P individuals and to offer needs-based and psychological interventions has been identified (Fusar-Poli et al., 2020d). This meta-analysis advances knowledge by clarifying that those CHR-P individuals who do not transition require extended support for their mental health, as non-transition does not automatically imply restoring a healthy status.
Our secondary analyses compared CHR-P individuals developing psychosis and not on the same outcomes. We found that functioning (Hedges’ g = 0.623) and attenuated psychotic symptoms (Hedges’ g = 0.706) improved in CHR-P individuals who did not transition to psychosis compared to those who did. Functioning is closely related to both the duration and severity of attenuated psychotic symptoms (Salazar de Pablo et al., 2020a). These findings indicate that the level of functioning of CHR-P individuals is strictly closed to transition to psychosis (Fusar-Poli et al., 2015c), confirming that transition to psychosis from a CHR-P state is associated with severe real-world clinical outcomes. A recent study confirmed that CHR-P individuals transitioning to psychosis (n = 130) were more likely to receive antipsychotic medication, to be admitted informally and on a compulsory basis, and to have spent more time in hospital than first-episode patients who presented to early intervention services (n = 1121), with a comparable likelihood of receiving clozapine (Fusar-Poli et al., 2020a). Surprisingly, we found no statistically significant differences in remission, negative and depressive symptoms between CHR-P individuals who transition or not to psychosis. It is important to highlight that statistical potency for these analyses was low, due to the limited number of prospective cohorts included. The lack of differences on negative or depressive features may be explained by the fact that no effective interventions are available for these domains in CHR-P individuals, beyond the presence of subthreshold or frank positive psychotic symptoms. The lack of difference in frequency of remission may be explained by the rapid and intensive package of early intervention care typically received by CHR-P individuals who develop over threshold psychosis, which has been demonstrated to be highly effective in improving clinical outcomes (Correll et al., 2018).
According to the meta-regressor factors tested, higher age was associated with a higher longitudinal improvement in attenuated psychotic symptoms. We previously found that age does not appear to modulate transition risk (Catalan et al., 2020). However, positive psychotic symptoms, such as hallucinations, are common in children and adolescents (Stevens et al., 2014). This may be related to the high prevalence of previous traumatic events in adolescents at CHR-P (63.2–85.0%) (Catalan et al., 2020), which are associated with the severity of positive symptoms, such as hallucinations and delusions (Bailey et al., 2018). There is also converging evidence indicating that early onset of psychosis is associated with poorer longer-term outcomes (Salazar de Pablo et al., 2021b). We also found that publication year was associated with better functioning. While declining transition risks over the years have been observed in the early days (Fusar-Poli et al., 2012), these have been disconfirmed in the most recent literature (Salazar de Pablo et al., 2021c). These discrepancies may be due to heterogeneous risk enrichment during the recruitment of young adults undergoing a CHR-P assessment (Fusar-Poli et al., 2016c, 2016d; Rice et al., 2019), with the associated variable impact of comorbid conditions (Salazar de Pablo et al., 2020a). Overall, the association between publication year and functioning may be secondary to sampling biases (Fusar-Poli et al., 2016d, 2018). We also found lower frequencies of remission in BLIPS individuals. This is an established finding, because BLIPS have poor mental health outcomes (Fusar-Poli et al., 2017b, 2017d) such as the higher risk of developing psychosis, being admitted compulsorily into hospital, receiving antipsychotics and benzodiazepines and lower probability of receiving psychotherapy (Fusar-Poli et al., 2016a, 2016b, 2017a, 2017d, 2019b, 2020b).
This study has several limitations. First, the available studies to meta-analyse some of the clinical outcomes (e.g., depressive and negative symptoms) evaluated was limited. As noted above, lack of power for some may have led to non-statistically significant differences in frequency of remission between CHR-P individuals who transitioned to psychosis or not. However, the database was sufficiently powered to run our primary analyses. Second, additional outcomes, such as quality of life, were not assessed as these were hardly ever reported in a meta-analysable manner. Third, there was high heterogeneity across the included studies, which we partially addressed in meta-regression analyses. Fourth, it was not possible to test some meta-regressors, including duration of untreated attenuated psychotic symptoms, ICD or DSM-defined comorbidity and exposure to baseline interventions, due to a limited amount of studies. Fifth, as noted above, the clinical meaning of changes in clinical and functional outcomes are not always directly interpretable. For instance, a decrease from 6 to 3 in one of the CHR-P symptoms may be more clinically relevant than a decrease from 3 to 0. Nevertheless, these findings confirm that transition to psychosis is not a trivial event of little clinical meaning, as argued by some authors, but related to real-world morbidity and mortality (Fusar-Poli et al., 2020b). Sixth, as transition to psychosis is defined by the worsening of attenuated psychotic symptoms, differences in secondary outcome were somewhat tautologically expected. Finally, we could not stratify our results according to the CHR-P subgroups, and we could only test their association with one of our outcomes (remission).
Conclusion
Clinical outcomes improve in CHR-P individuals not transitioning to psychosis but only less than half remit over time. Sustained clinical attention should be provided in the longer term to monitor these outcomes.
Financial support
This study is funded by the PSYSCAN project to Professor McGuire and Professor Fusar-Poli through the European Commission. Dr Salazar de Pablo is supported by the Alicia Koplowitz Foundation.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796021000639.
click here to view supplementary material
Data
The studies included in this review were publicly available. The lead author and corresponding author can be contacted.
Conflict of interest
Dr Salazar de Pablo has received honoraria from Janssen Cilag. Professor Fusar-Poli has received research fees from Lundbeck and honoraria from Lundbeck, Angelini, Menarini and Boehringer Ingelheim outside the current study.
References
- Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW and Heinssen R (2011) At clinical high risk for psychosis: outcome for nonconverters. The American Journal of Psychiatry 168, 800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Bearden CE, Mathalon DH, Santesteban-Echarri O and Woods SW (2019) Clinical and functional characteristics of youth at clinical high-risk for psychosis who do not transition to psychosis. Psychological Medicine 49, 1670–1677. [DOI] [PubMed] [Google Scholar]
- Albert U, Tomassi S, Maina G and Tosato S (2018) Prevalence of non-psychotic disorders in ultra-high risk individuals and transition to psychosis: a systematic review. Psychiatry Research 270, 1–12. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association. [Google Scholar]
- Armando M, Pontillo M, De Crescenzo F, Mazzone L, Monducci E, Lo Cascio N, Santonastaso O, Pucciarini ML, Vicari S, Schimmelmann BG and Schultze-Lutter F (2015) Twelve-month psychosis-predictive value of the ultra-high risk criteria in children and adolescents. Schizophrenia Research 169, 186–192. [DOI] [PubMed] [Google Scholar]
- Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E and Bendall S (2018) Childhood trauma Is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophrenia Bulletin 44, 1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck K, Andreou C, Studerus E, Heitz U, Ittig S, Leanza L and Riecher-Rössler A (2019a) Clinical and functional long-term outcome of patients at clinical high risk (CHR) for psychosis without transition to psychosis: a systematic review. Schizophrenia Research 210, 39–47. [DOI] [PubMed] [Google Scholar]
- Beck K, Studerus E, Andreou C, Egloff L, Leanza L, Simon AE, Borgwardt S and Riecher-Rössler A (2019b) Clinical and functional ultra-long-term outcome of patients with a clinical high risk (CHR) for psychosis. European Psychiatry 62, 30–37. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J and Rothstein H (2013) Comprehensive Meta-Analysis Version 3. Englewood, NJ: Biostat. [Google Scholar]
- Cannon TD, Chung Y, He G, Sun D, Jacobson A, van Erp TG, McEwen S, Addington J, Bearden CE, Cadenhead K, Cornblatt B, Mathalon DH, McGlashan T, Perkins D, Jeffries C, Seidman LJ, Tsuang M, Walker E, Woods SW, Heinssen R and Consortium NAPLS (2015) Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biological Psychiatry 77, 147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalan A, Salazar de Pablo G, Vaquerizo Serrano J, Mosillo P, Baldwin H, Fernández-Rivas A, Moreno C, Arango C, Correll CU, Bonoldi I and Fusar-Poli P (2020) Annual research review: prevention of psychosis in adolescents – systematic review and meta-analysis of advances in detection, prognosis and intervention. Journal of Child Psychology and Psychiatry 62, 657–673. [DOI] [PubMed] [Google Scholar]
- Chen FZ, Wang Y, Sun XR, Yao YH, Zhang N, Qiao HF, Zhang L, Li ZJ, Lin H, Lu Z, Li J, Chan RCK and Zhao XD (2016) Emotional experiences predict the conversion of individuals with attenuated psychosis syndrome to psychosis: a 6-month follow up study. Frontiers in Psychology 7, 818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Yang K, Marušic A, Qaseem A, Meerpohl JJ, Flottorp S, Akl EA, Schünemann HJ, Chan ES, Falck-Ytter Y, Ahmed F, Barber S, Chen C, Zhang M, Xu B, Tian J, Song F, Shang H, Tang K, Wang Q, Norris SL and Group RRIfPGiHW (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Annals of Internal Medicine 166, 128–132. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic. [Google Scholar]
- Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, Craig TJ, Nordentoft M, Srihari VH, Guloksuz S, Hui CLM, Chen EYH, Valencia M, Juarez F, Robinson DG, Schooler NR, Brunette MF, Mueser KT, Rosenheck RA, Marcy P, Addington J, Estroff SE, Robinson J, Penn D, Severe JB and Kane JM (2018) Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 75, 555–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter J, Lin A, Drake RJ, Thompson A, Nelson B, McGorry P, Wood SJ and Yung AR (2017) Long-term employment among people at ultra-high risk for psychosis. Schizophrenia Research 184, 26–31. [DOI] [PubMed] [Google Scholar]
- Davies C, Cipriani A, Ioannidis JPA, Radua J, Stahl D, Provenzani U, McGuire P and Fusar-Poli P (2018) Lack of evidence to favor specific preventive interventions in psychosis: a network meta-analysis. World Psychiatry 17, 196–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devoe DJ, Braun A, Seredynski T and Addington J (2020) Negative symptoms and functioning in youth at risk of psychosis: a systematic review and meta-analysis. Harvard Review of Psychiatry 28, 341–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit S, Schothorst PF, Oranje B, Ziermans TB, Durston S and Kahn RS (2014) Adolescents at ultra-high risk for psychosis: long-term outcome of individuals who recover from their at-risk state. European Neuropsychopharmacology 24, 865–873. [DOI] [PubMed] [Google Scholar]
- Falkenberg I, Valmaggia L, Byrnes M, Frascarelli M, Jones C, Rocchetti M, Straube B, Badger S, McGuire P and Fusar-Poli P (2015) Why are help-seeking subjects at ultra-high risk for psychosis help-seeking? Psychiatry Research 228, 808–815. [DOI] [PubMed] [Google Scholar]
- Falkenberg I, Valli I, Raffin M, Broome MR, Fusar-Poli P, Matthiasson P, Picchioni M and McGuire P (2017) Pattern of activation during delayed matching to sample task predicts functional outcome in people at ultra-high risk for psychosis. Schizophrenia Research 181, 86–93. [DOI] [PubMed] [Google Scholar]
- Fletcher J (2007) What is heterogeneity and is it important? BMJ 334, 94–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P and Salazar de Pablo G (2021) Antipsychotics and attenuated psychosis syndrome: transdiagnostic assessment and discontinuation strategies. Schizophrenia Research. doi: 10.1016/j.schres.2021.06.030. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E and McGuire P (2012) Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives Of General Psychiatry 69, 220–229. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rossler A, Schultze-Lutter F, Keshavan M, Wood S, Ruhrmann S, Seidman LJ, Valmaggia L, Cannon T, Velthorst E, De Haan L, Cornblatt B, Bonoldi I, Birchwood M, McGlashan T, Carpenter W, McGorry P, Klosterkotter J, McGuire P and Yung A (2013) The psychosis high-risk state a comprehensive state-of-the-art review. JAMA Psychiatry 70, 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Nelson B, Valmaggia L, Yung A and McGuire P (2014) Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophrenia Bulletin 40, 120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Rutigliano G, Schultze-Lutter F, Bonoldi I, Borgwardt S, Riecher-Rössler A, Addington J, Perkins D, Woods SW, McGlashan TH, Lee J, Klosterkötter J, Yung AR and McGuire P (2015a) At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry 14, 322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Papanastasiou E, Stahl D, Rocchetti M, Carpenter W, Shergill S and McGuire P (2015b) Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophrenia Bulletin 41, 892–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rocchetti M, Sardella A, Avila A, Brandizzi M, Caverzasi E, Politi P, Ruhrmann S and McGuire P (2015c) Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. British Journal of Psychiatry 207, 198–206. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Bonoldi I, Hui LM, Rutigliano G, Stahl DR, Borgwardt S, Politi P, Mishara AL, Lawrie SM, Carpenter WT and McGuire PK (2016a) Prognosis of brief psychotic episodes: a meta-analysis. JAMA Psychiatry 73, 211–220. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Borgwardt S, Woods SW, Addington J, Nelson B, Nieman DH, Stahl DR, Rutigliano G, Riecher-Rössler A, Simon AE, Mizuno M, Lee TY, Kwon JS, Lam MM, Perez J, Keri S, Amminger P, Metzler S, Kawohl W, Rössler W, Lee J, Labad J, Ziermans T, An SK, Liu CC, Woodberry KA, Braham A, Corcoran C, McGorry P, Yung AR and McGuire PK (2016b) Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry 73, 113–120. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Rutigliano G, Stahl D, Schmidt A, Ramella-Cravaro V, Hitesh S and McGuire P (2016c) Deconstructing pretest risk enrichment to optimize prediction of psychosis in individuals at clinical high risk. JAMA Psychiatry 73, 1260–1267. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Schultze-Lutter F, Cappucciati M, Rutigliano G, Bonoldi I, Stahl D, Borgwardt S, Riecher-Rössler A, Addington J, Perkins DO, Woods SW, McGlashan T, Lee J, Klosterkötter J, Yung AR and McGuire P (2016d) The dark side of the moon: meta-analytical impact of recruitment strategies on risk enrichment in the clinical high risk state for psychosis. Schizophrenia Bulletin 42, 732–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, De Micheli A, Rutigliano G, Bonoldi I, Tognin S, Ramella-Cravaro V, Castagnini A and McGuire P (2017a) Diagnostic and prognostic significance of brief limited intermittent psychotic symptoms (BLIPS) in individuals at ultra-high risk. Schizophrenia Bulletin 43, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, McGorry PD and Kane JM (2017b) Improving outcomes of first-episode psychosis: an overview. World Psychiatry 16, 251–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Raballo A and Parnas J (2017c) What is an attenuated psychotic symptom? On the importance of the context. Schizophrenia Bulletin 43, 687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rutigliano G, Stahl D, Davies C, De Micheli A, Ramella-Cravaro V, Bonoldi I and McGuire P (2017d) Long-term validity of the at-risk mental state (ARMS) for predicting psychotic and non-psychotic mental disorders. European Psychiatry 42, 49–54. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Tantardini M, De Simone S, Ramella-Cravaro V, Oliver D, Kingdon J, Kotlicka-Antczak M, Valmaggia L, Lee J, Milian MJ, Galderisi S, Balottin U, Ricca V and McGuire P (2017e) Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra-high-risk. European Psychiatry 40, 65–75. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Palombini E, Davies C, Oliver D, Bonoldi I, Ramella-Cravaro V and McGuire P (2018) Why transition risk to psychosis is not declining at the OASIS ultra-high-risk service: the hidden role of stable pretest risk enrichment. Schizophrenia Research 192, 385–390. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Davies C, Solmi M, Brondino N, De Micheli A, Kotlicka-Antczak M, Shin JI and Radua J (2019a) Preventive treatments for psychosis: umbrella review (just the evidence). Frontiers in Psychiatry 10, 764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, De Micheli A, Chalambrides M, Singh A, Augusto C and McGuire P (2019b) Unmet needs for treatment in 102 individuals with brief and limited intermittent psychotic symptoms (BLIPS): implications for current clinical recommendations. Epidemiology and Psychiatric Sciences 29, e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, Borgwardt S, Lawrie SM, Parnas J and McGuire P (2019c) Transdiagnostic psychiatry: a systematic review. World Psychiatry 18, 192–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, De Micheli A, Patel R, Signorini L, Miah S, Spencer T and McGuire P (2020a) Real-world clinical outcomes two years after transition to psychosis in individuals at clinical high risk: electronic health record cohort study. Schizophrenia Bulletin 46, 1114–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, De Micheli A, Signorini L, Baldwin H, de Pablo GS and McGuire P (2020b) Real-world long-term outcomes in individuals at clinical risk for psychosis: the case for extending duration of care. EClinicalMedicine 28, 100578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Radua J, McKenna PJ, Laws K, Davies C and Jauhar S (2020c) Methodological biases in CBT trial-commentary: modular cognitive-behavioral therapy for affective symptoms in young individuals at ultra-high risk of first episode of psychosis: randomized controlled trial. Frontiers in Psychiatry 11, 394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Salazar de Pablo G, Correll CU, Meyer-Lindenberg A, Millan MJ, Borgwardt S, Galderisi S, Bechdolf A, Pfennig A, Kessing LV, van Amelsvoort T, Nieman DH, Domschke K, Krebs MO, Koutsouleris N, McGuire P, Do KQ and Arango C (2020d) Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiatry 77, 755–765. [DOI] [PubMed] [Google Scholar]
- Guo JY, Niendam TA, Auther AM, Carrion RE, Cornblatt BA, Ragland JD, Adelsheim S, Calkins R, Sale TG, Taylor SF, McFarlane WR and Carter CS (2019) Predicting psychosis risk using a specific measure of cognitive control: a 12-month longitudinal study. Psychological Medicine 50, 2230–2239. [DOI] [PubMed] [Google Scholar]
- Hedges LV (2007) Effect sizes in cluster-randomized designs. Journal of Educational and Behavioral Statistics 32, 341–370. [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Group CBM and Group CSM (2011) The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline E, Thompson E, Demro C, Bussell K, Reeves G and Schiffman J (2016) Self-report instruments for clinical monitoring of psychosis risk states. Psychiatric Services 67, 456–459. [DOI] [PubMed] [Google Scholar]
- Kline ER, Seidman LJ, Cornblatt BA, Woodberry KA, Bryant C, Bearden CE, Cadenhead KS, Cannon TD, Mathalon DH, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW and Addington J (2018) Depression and clinical high-risk states: baseline presentation of depressed vs. non-depressed participants in the NAPLS-2 cohort. Schizophrenia Research 192, 357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotlicka-Antczak M, Podgórski M, Oliver D, Maric NP, Valmaggia L and Fusar-Poli P (2020) Worldwide implementation of clinical services for the prevention of psychosis: the IEPA early intervention in mental health survey. Early Intervention in Psychiatry 14, 741–750. [DOI] [PubMed] [Google Scholar]
- Lally J, Ajnakina O, Stubbs B, Cullinane M, Murphy KC, Gaughran F and Murray RM (2017) Remission and recovery from first-episode psychosis in adults: systematic review and meta-analysis of long-term outcome studies. British Journal of Psychiatry 211, 350–358. [DOI] [PubMed] [Google Scholar]
- Landa Y, Mueser KT, Wyka KE, Shreck E, Jespersen R, Jacobs MA, Griffin KW, van der Gaag M, Reyna VF, Beck AT, Silbersweig DA and Walkup JT (2016) Development of a group and family-based cognitive behavioural therapy program for youth at risk for psychosis. Early Intervention in Psychiatry 10, 511–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemos-Giráldez S, Vallina-Fernández O, Fernández-Iglesias P, Vallejo-Seco G, Fonseca-Pedrero E, Paíno-Piñeiro M, Sierra-Baigrie S, García-Pelayo P, Pedrejón-Molino C, Alonso-Bada S, Gutiérrez-Pérez A and Ortega-Ferrández JA (2009) Symptomatic and functional outcome in youth at ultra-high risk for psychosis: a longitudinal study. Schizophrenia Research 115, 121–129. [DOI] [PubMed] [Google Scholar]
- Lin A, Yung AR, Nelson B, Brewer WJ, Riley R, Simmons M, Pantelis C and Wood SJ (2013) Neurocognitive predictors of transition to psychosis: medium- to long-term findings from a sample at ultra-high risk for psychosis. Psychological Medicine 43, 2349–2360. [DOI] [PubMed] [Google Scholar]
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T and Saxena S (2011) Prevalence of intellectual disability: a meta-analysis of population-based studies. Research in Developmental Disabilities 32, 419–436. [DOI] [PubMed] [Google Scholar]
- Metzak PD, Devoe DJ, Iwaschuk A, Braun A and Addington J (2020) Brain changes associated with negative symptoms in clinical high risk for psychosis: a systematic review. Neuroscience & Biobehavioral Reviews 118, 367–383. [DOI] [PubMed] [Google Scholar]
- Michel C, Ruhrmann S, Schimmelmann BG, Klosterkötter J and Schultze-Lutter F (2018) Course of clinical high-risk states for psychosis beyond conversion. European Archives of Psychiatry and Clinical Neuroscience 268, 39–48. [DOI] [PubMed] [Google Scholar]
- Mittal VA, Walker EF, Bearden CE, Walder D, Trottman H, Daley M, Simone A and Cannon TD (2010) Markers of basal ganglia dysfunction and conversion to psychosis: neurocognitive deficits and dyskinesias in the prodromal period. Biological Psychiatry 68, 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG and Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongan D, Föcking M, Healy C, Susai SR, Heurich M, Wynne K, Nelson B, McGorry PD, Amminger GP, Nordentoft M, Krebs MO, Riecher-Rössler A, Bressan RA, Barrantes-Vidal N, Borgwardt S, Ruhrmann S, Sachs G, Pantelis C, van der Gaag M, de Haan L, Valmaggia L, Pollak TA, Kempton MJ, Rutten BPF, Whelan R, Cannon M, Zammit S, Cagney G, Cotter DR, McGuire P and Group ENoNSNSG-EIE-GHRS (2020) Development of proteomic prediction models for transition to psychotic disorder in the clinical high-risk state and psychotic experiences in adolescence. JAMA Psychiatry 78, 77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver D, Reilly TJ, Baccaredda Boy O, Petros N, Davies C, Borgwardt S, McGuire P and Fusar-Poli P (2019) What causes the onset of psychosis in individuals at clinical high risk? A meta-analysis of risk and protective factors. Schizophrenia Bulletin 46, 110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelizza L, Paterlini F, Azzali S, Garlassi S, Scazza I, Pupo S, Simmons M, Nelson B and Raballo A (2019) The approved Italian version of the comprehensive assessment of at-risk mental states (CAARMS-ITA): field test and psychometric features. Early Intervention in Psychiatry 13, 810–817. [DOI] [PubMed] [Google Scholar]
- Phillips LJ, McGorry PD, Yuen HP, Ward J, Donovan K, Kelly D, Francey SM and Yung AR (2007) Medium term follow-up of a randomized controlled trial of interventions for young people at ultra-high risk of psychosis. Schizophrenia Research 96, 25–33. [DOI] [PubMed] [Google Scholar]
- Radua J, Ramella-Cravaro V, Ioannidis JPA, Reichenberg A, Phiphopthatsanee N, Amir T, Thoo HY, Oliver D, Davies C, Morgan C, McGuire P, Murray RM and Fusar-Poli P (2018) What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 17, 49–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice S, Polari A, Thompson A, Hartmann J, McGorry P and Nelson B (2019) Does reason for referral to an ultra-high risk clinic predict transition to psychosis? Early Intervention in Psychiatry 13, 318–321. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Heekeren K, Theodoridou A, Müller M, Corrigan PW, Mayer B, Metzler S, Dvorsky D, Walitza S and Rössler W (2015) Stigma as a stressor and transition to schizophrenia after one year among young people at risk of psychosis. Schizophrenia Research 166, 43–48. [DOI] [PubMed] [Google Scholar]
- Rutigliano G, Valmaggia L, Landi P, Frascarelli M, Cappucciati M, Sear V, Rocchetti M, De Micheli A, Jones C, Palombini E, McGuire P and Fusar-Poli P (2016) Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra-high risk for psychosis. Journal of Affective Disorders 203, 101–110. [DOI] [PubMed] [Google Scholar]
- Ryan J, Graham A, Nelson B and Yung A (2017) Borderline personality pathology in young people at ultra-high risk of developing a psychotic disorder. Early Intervention in Psychiatry 11, 208–214. [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G, Catalan A and Fusar-Poli P (2019) Clinical validity of DSM-5 attenuated psychosis syndrome: advances in diagnosis, prognosis, and treatment. JAMA Psychiatry 77, 311–320. [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G, Guinart D, Cornblatt BA, Auther AM, Carrión RE, Carbon M, Jiménez-Fernández S, Vernal DL, Walitza S, Gerstenberg M, Saba R, Lo Cascio N, Brandizzi M, Arango C, Moreno C, Van Meter A, Fusar-Poli P and Correll CU (2020a) DSM-5 Attenuated psychosis syndrome in adolescents hospitalized with non-psychotic psychiatric disorders. Frontiers in Psychiatry 11, 568982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G, Jauhar S and Fusar-Poli P (2020b) Psychosocial intervention without antipsychotic medication for brief psychotic episodes? Schizophrenia Bulletin Open 1, sgaa037. [Google Scholar]
- Salazar de Pablo G, Estradé A, Cutroni M, Andlauer O and Fusar-Poli P (2021a) Establishing a clinical service to prevent psychosis: what, how and when? Systematic review. Translational Psychiatry 11, 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G, Moreno D, Gonzalez-Pinto A, Payá B, Castro-Fornieles J, Baeza I, Graell M, Arango C, Rapado-Castro M and Moreno C (2021b) Affective symptom dimensions in early-onset psychosis over time: a principal component factor analysis of the Young Mania Rating Scale and the Hamilton Depression Rating Scale. European Child & Adolescent Psychiatry. doi: 10.1007/s00787-021-01815-5. [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G, Radua J, Pereira J, Bonoldi I, Arienti V, Besana F, Soardo L, Cabras A, Fortea L, Catalan A, Vaquerizo-Serrano J, Coronelli F, Kaur S, Da Silva J, Il Shin J, Solmi M, Brondino N, Politi P, McGuire P and Fusar-Poli P (2021c) Probability of transition to psychosis in individuals at clinical high risk: an updated meta-analysis. JAMA Psychiatry 78, 970–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savill M, Banks C, Khanom H and Priebe S (2015) Do negative symptoms of schizophrenia change over time? A meta-analysis of longitudinal data. Psychological Medicine 45, 1613–1627. [DOI] [PubMed] [Google Scholar]
- Sawada K, Kanehara A, Sakakibara E, Eguchi S, Tada M, Satomura Y, Suga M, Koike S and Kasai K (2017) Identifying neurocognitive markers for outcome prediction of global functioning in individuals with first-episode and ultra-high-risk for psychosis. Psychiatry and Clinical Neurosciences 71, 318–327. [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F (2009) Subjective symptoms of schizophrenia in research and the clinic: the basic symptom concept. Schizophrenia Buletinl 35, 5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi J, Wang L, Yao Y, Chen F, Su N, Zhao X and Zhan C (2016) Protective factors in Chinese university students at clinical high risk for psychosis. Psychiatry Research 239, 239–244. [DOI] [PubMed] [Google Scholar]
- Simon AE, Velthorst E, Nieman DH, Linszen D, Umbricht D and de Haan L (2011) Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophrenia Research 132, 8–17. [DOI] [PubMed] [Google Scholar]
- Simon AE, Borgwardt S, Riecher-Rössler A, Velthorst E, de Haan L and Fusar-Poli P (2013) Moving beyond transition outcomes: meta-analysis of remission rates in individuals at high clinical risk for psychosis. Psychiatry Research 209, 266–272. [DOI] [PubMed] [Google Scholar]
- Stevens JR, Prince JB, Prager LM and Stern TA (2014) Psychotic disorders in children and adolescents: a primer on contemporary evaluation and management. Primary Care Companion CNS Disorders 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- Velthorst E, Nieman DH, Klaassen RM, Becker HE, Dingemans PM, Linszen DH and De Haan L (2011) Three-year course of clinical symptomatology in young people at ultra-high risk for transition to psychosis. Acta Psychiatrica Scandinavida 123, 36–42. [DOI] [PubMed] [Google Scholar]
- Ventura J, Hellemann GS, Thames AD, Koellner V and Nuechterlein KH (2009) Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophrenia Research 113, 189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward TS, Jung K, Smith GN, Hwang H, Barr AM, Procyshyn RM, Flynn SW, van der Gaag M and Honer WG (2014) Symptom changes in five dimensions of the Positive and Negative Syndrome Scale in refractory psychosis. European Archives of Psychiatry and Clinical Neuroscience 264, 673–682. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2018) International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). World Health Organization. Retrieved from https://icd.who.int/browse11/l-m/en. [Google Scholar]
- Yee JY, Lee T-S and Lee J (2018) Levels of serum brain-derived neurotropic factor in individuals at ultra-high risk for psychosis-findings from the longitudinal youth at risk study (LYRIKS). International Journal of Neuropsychopharmacology 21, 734–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang TH, Li HJ, Woodberry KA, Xu LH, Tang YY, Guo Q, Cui HR, Liu XH, Chow A, Li CB, Jiang KD, Xiao ZP, Seidman LJ and Wang JJ (2017) Two-year follow-up of a Chinese sample at clinical high risk for psychosis: timeline of symptoms, help-seeking and conversion. Epidemiology and Psychiatric Sciences 26, 287–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziermans TB, Schothorst PF, Sprong M and van Engeland H (2011) Transition and remission in adolescents at ultra-high risk for psychosis. Schizophrenia Research 126, 58–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796021000639.
click here to view supplementary material
Data Availability Statement
The studies included in this review were publicly available. The lead author and corresponding author can be contacted.