Abstract
Objectives
This study aimed to explore return to work after COVID-19 and how disease severity affects this.
Study design
This is a Nationwide Danish registry–based cohort study using a retrospective follow-up design.
Methods
Patients with a first-time positive SARS-CoV-2 polymerase chain reaction test between 1 January 2020 and 30 May 2020, including 18–64 years old, 30-day survivors, and available to the workforce at the time of the first positive test were included. Admission types (i.e. no admission, admission to non–intensive care unit [ICU] department and admission to ICU) and return to work was investigated using Cox regression standardised to the age, sex, comorbidity and education-level distribution of all included subjects with estimates at 3 months from positive test displayed.
Results
Among the 7466 patients included in the study, 81.9% (6119/7466) and 98.4% (7344/7466) returned to work within 4 weeks and 6 months, respectively, with 1.5% (109/7466) not returning. Of the patients admitted, 72.1% (627/870) and 92.6% (805/870) returned 1 month and 6 months after admission to the hospital, with 6.6% (58/870) not returning within 6 months. Of patients admitted to the ICU, 36% (9/25) did not return within 6 months. Patients with an admission had a lower chance of return to work 3 months from positive test (relative risk [RR] 0.95, 95% confidence interval [CI] 0.94–0.96), with the lowest chance in patients admitted to an ICU department (RR 0.54, 95% CI 0.35–0.72). Female sex, older age, and comorbidity were associated with a lower chance of returning to work.
Conclusion
Hospitalised patients with COVID-19 infection have a lower chance of returning to work with potential implications for postinfection follow-up and rehabilitation.
Keywords: Covid-19, Return to work, Sick leave, Long-term COVID, Severity, Workforce connection
Introduction
COVID-19 is a global challenge for both public health and the societal economy, which may influence daily living in years to come. Studies are emerging on the long-term effects of COVID-19 where development of neurological disorders, fatigue, respiratory symptoms, muscle weakness, sleep difficulties and anxiety or depression symptoms have been identified as long-term effects of COVID-19.1, 2, 3
COVID-19 has, on an individual level, both direct costs associated with the treatment of the disease and indirect costs with sick leave. The indirect costs have been estimated to be about 10 times higher than the direct costs of influenza.4 With COVID-19 outmatching influenza in transmission and disease severity, it is highly likely that the indirect consequences related to sick leave are much higher for COVID-19.5
Sick leave and long-term sick leave in patients who were part of the workforce before COVID-19 infection may likely reflect the long-term adverse effects of COVID-19 infection. As such, long-term sick leave after COVID-19 infection represents the proportion of patients who are likely to suffer from disabling sequelae after the infection. In contrast, return to work represents the ability to return to a societal function as before the infection. Few studies have explored return to work and sick leave after COVID-19 infection. Older age, hospitalisation, and female sex have been identified as risk factors of longer sick leave after COVID-19 infection.6 , 7 More studies are needed to confirm these previous findings and identify new risk factors of sick leave and delayed return to work.
The primary aim of this study was to explore sick leave and return to work using nationwide register-based data on weekly updated employment status in COVID-19 patients aged between 18 and 64 years. Return to work serves as a proxy for functional recovery, whereas prolonged sick leave indicates long-term impairment. Patients with a positive COVID-19 test not admitted to the hospital are compared with patients admitted to the hospital and patients admitted to an intensive care unit (ICU) as an indicator of disease severity.
The secondary aim was to compare COVID-19 patients admitted to hospital to patients admitted with influenza to explore employment status post-COVID-19 relative to a well-known infectious disease.
The first case of COVID-19 in Denmark was detected in February 2020, with the first lockdown measures starting 13 March, with measures such as social distancing including working from home for non-critical employees, during the first wave. A gradual reopening started on 15 April.
Methods
Study design
This is a Nationwide Danish registry–based cohort study using a retrospective follow-up design.
Data sources and setting
All 5.8 million Danish citizens have a unique civil personal registration (CPR) number. In this study, the CPR number was used to identify individuals across the different national Danish registries.8 Using these nationwide registries, we accessed all positive SARS-CoV-2 polymerase chain reaction (PCR) tests in Denmark. During the study period (1 January 2020 to 30 May 2020), PCR test has been the primary diagnostic tool in Denmark for diagnosing COVID-19. The following registries were used to gather information: (1) the Danish National Patient Registry on admission and comorbidities; (2) The Danish Prescription Registry for prescription medication and to define certain comorbid conditions;9 , 10 (3) the Danish Cause of Death Registry11 for date of death; (4) The Statistics of Denmark for age, sex and educational level;8 , 12 and (5) the Danish Labour Market Registry (the DREAM database) for workforce connection.13 As part of the Danish taxpaying system, all Danish citizens have access to free health care, education, and financial support if citizens are unable to support themselves. Financial support includes, among others, sick leave benefit (available after 4 weeks of sick leave to citizens who are working or available to the workforce), unemployment benefit (for persons who are available to the workforce) and early retirement benefit.
Approval to conduct the study and process the data was granted by The Capital Region of Denmark (approval nr. P-2019-191). Retrospective registry research does not require ethical approval by Danish law.
Population
For the primary analysis, all COVID-19 PCR-positive patients between 1 January 2020 and 30 May 2020 were included at the time of the first positive COVID-19 PCR test. Patients aged <18 or >64 years were excluded from the study together with patients not available to the workforce (e.g. patients receiving early retirement [see table S1]). Patients dying or emigrating within 30 days of inclusion time were excluded.
Influenza patients admitted between 1 February 2019 and 30 May 2020 were included for the purpose of a comparative analysis. The period here differed from the COVID-19 population to ensure enough patients included.
Exposure
Study variables
Admission to the hospital with COVID-19 was defined by a discharge diagnosis of COVID-19 (International Classification of Disease, 10th revision [ICD-10]: DB342 or DB972) after their positive PCR test and an admission less than 30 days from the positive test. Influenza admission was defined as a discharge diagnosis of influenza (ICD-10: DJ09 or DJ10).
Admission to the ICU was defined as admission with a procedure code of either intensive care observation or intensive care treatment (NABE or NABB), which previously has been validated with a positive predictive value of 87.2%.14
Adjustment for age, sex, comorbidities (using Charlson comorbidity index) and education level was performed in all analyses as relevant confounders of return to work. Age was treated as a categorical variable using 18–25, 26–35, 36–45, 46–55, and 56–64 age intervals. Charlson comorbidity index was treated as a categorical variable with a score above or equal to 4 gathered into one group.15 Education was according to the International Standard of Education (ISCED) level divided into short (0–2), medium (3), short higher (5–6), and long higher education (7–8).16 ISCED level 4 is not a part of the Danish education system.
Outcomes
The primary outcome was return to work. The secondary outcome was sick leave. Public sick leave benefits start after 1 month of sick leave and are recorded in the DREAM registry from this timepoint. Because of this delay in recording, follow-up started after 1 month. In the study, we will refer to time from positive test, not start of follow-up. The risk of sick leave is defined as sick leave (yes/no) 1 month after positive test.
Patients who returned to work or who were available to the work force within 1 month of inclusion were classified as ‘early returners’, patients returning to work after 1 month up to a maximum follow-up of 6 months were classified as ‘late returners’, and patients not returning within the 6 months, as ‘non-returners’.
Statistical analysis
Continuous variables are presented using mean and standard deviation when normally distributed and otherwise using median and 25–75 percentiles. Categorical data are presented using counts and percentages. Cumulative incidence plots of return to work are presented for both the primary and the subgroup analyses.
Incidence with confidence intervals at 1, 3, and 6 months of patients not returning to work are shown according to admission, sex, and age.
Multivariable Cox regression analysis was used to explore differences in return to work in patient not admitted, admitted, or admitted to ICU as the primary analysis and between patients admitted with COVID-19 or influenza as part of the subgroup analysis. Cox regression was standardised to the age, sex, comorbidity and educational level status of all included subjects with relative risks and absolute risk at 3 months reported.
Logistic regression analysis was used to explore differences in sick leave 1 month after positive test at the start of follow-up between patient not admitted, admitted, or admitted to ICU as the primary analysis and between patients admitted with COVID-19 or influenza as part of the subgroup analysis. Logistic regression was standardised to the age, sex, comorbidity and educational level status of all included subjects with relative risks and absolute risks reported.
Results
Patients
During the study period, 7640 patients between aged 18 and 64 years who were available to the workforce had a positive COVID-19 test and after exclusion of patients emigrating (N = 32) or dying within 1 month (N = 13) or had missing data (N = 139), 7466 patients were included in the study.
Baseline characteristics are shown in Table 1 .
Table 1.
Baseline characteristics at positive COVID-19 test in Denmark 2020 between 1 January 2020 to 30 May 2020.
| Variable | Level | Not admitted (n = 6590) | Admitted (n = 876) |
|---|---|---|---|
| Admitted to ICU | 24 (2.7) | ||
| Sex | Female | 4128 (62.6) | 389 (44.4) |
| Male | 2462 (37.4) | 487 (55.6) | |
| Age, mean (SD) | 41.6 (12.7) | 46.2 (11.9) | |
| Age group (years) | 18–25 | 844 (12.8) | 65 (7.4) |
| 26–35 | 1503 (22.8) | 180 (20.5) | |
| 36–45 | 1515 (23.0) | 121 (13.8) | |
| 46–55 | 1583 (24.0) | 286 (32.6) | |
| 56–64 | 1145 (17.4) | 224 (25.6) | |
| Education level | Short | 903 (13.7) | 128 (14.6) |
| Medium | 2573 (39.0) | 352 (40.2) | |
| Long | 2204 (33.4) | 252 (28.8) | |
| Very long | 910 (13.8) | 144 (16.4) | |
| Workforce connection | Working | 5658 (85.9) | 756 (86.3) |
| Benefits classified as work | 693 (10.5) | 68 (7.8) | |
| Available to work | 239 (3.6) | 52 (5.9) | |
| Charlson comorbidity score | 0 | 6135 (93.1) | 768 (87.7) |
| 1 | 307 (4.7) | 61 (7.0) | |
| 2 | 120 (1.8) | 29 (3.3) | |
| 3 | 8 (0.1) | 11 (1.3) | |
| 4+ | 20 (0.3) | 7 (0.8) | |
| Return to work | Did not return to work | 51 (0.8) | 58 (6.6) |
| Returned | 6535 (99.2) | 809 (92.4) | |
| Died, emigrated or early retirement | 4 (0.1) | 9 (1.0) | |
| Admission days, median (IQR) | 3 (1, 7) | ||
| Peripheral vascular disease | 18 (0.3) | 7 (0.8) | |
| Coronary artery disease | 14 (0.2) | 4 (0.5) | |
| Chronic heart failure | 13 (0.2) | 4 (0.5) | |
| Cerebrovascular disease | 26 (0.4) | 7 (0.8) | |
| Dementia | ≤3 | ≤3 | |
| Chronic pulmonary disease | 133 (2.0) | 32 (3.7) | |
| Rheumatic disease | 51 (0.8) | 10 (1.1) | |
| Peptic ulcus | 14 (0.2) | ≤3 | |
| Mild liver disease | 27 (0.4) | 8 (0.9) | |
| Diabetes | 62 (0.9) | 14 (1.6) | |
| Diabetes with complications | 24 (0.4) | 11 (1.3) | |
| Hemiplegia | ≤3 | ≤3 | |
| Chronic renal failure | 8 (0.1) | 6 (0.7) | |
| Cancer | 78 (1.2) | 15 (1.7) | |
| Severe liver disease | ≤3 | 4 (0.5) | |
| Cancer with metastases | ≤3 | ≤3 | |
| HIV/AIDS | 14 (0.2) | ≤3 | |
ICU, intensive care unit; IQR, interquartile range; SD, standard deviation.
Return to work
Of the 7466 patients, 82.0% (6119/7466) had returned to work within 4 weeks of their first positive COVID-19 test, an additional of 16.4% (1225/7466) returned within 6 months and 1.5% (109/7466) did not return to work and were receiving sick leave benefit after 6 months. During follow-up, eight patients died without returning to work, and five patients either emigrated or left the workforce permanently without returning to work.
Among 30-day survivors of COVID-19 who were admitted to the hospital and discharged with a primary diagnosis of COVID-19, 72.1% (627/870) had returned to work within 4 weeks, an additional 20.5% (178/870) returned within 6 months, and 6.6% (58/870) did not return within 6 months. Of these 870 patients, 25 were admitted to the ICU, of whom 36% (9/25) did not return within 6 months.
In patients admitted with influenza, 91.6% (377/466) had returned to work within the first 4 weeks from their admission to the hospital, 96.6% (402/416) returned within the 6-months follow-up, and 2.6% (11/416) did not return to work.
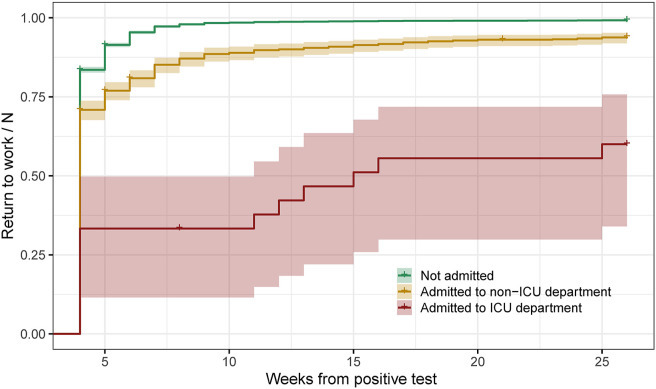
The cumulative incidence plot for return to work between different admission types is shown in Fig. 1 . Patients not admitted are seen with the highest rate of return, patients admitted with a lower rate, and patients admitted to an ICU department with the lowest return rates during follow-up.
Fig. 1.
Cumulative incidence plot of all PCR-positive COVID-19 patients with follow-up starting 4 weeks after positive test.
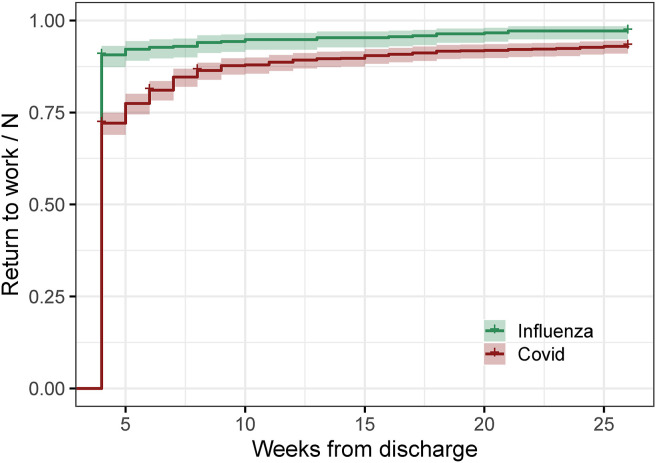
The cumulative incidence plot of return to work between patients admitted with COVID-19 and patients admitted with influenza is shown in Fig. 2 . This figure show patients with COVID-19 have a reduced chance of return to work compared with patients admitted with influenza.
Fig. 2.
Cumulative incidence plot of return to the workforce in patients admitted to the hospital with either COVID-19 or influenza. Follow-up starts 4 weeks after admission.
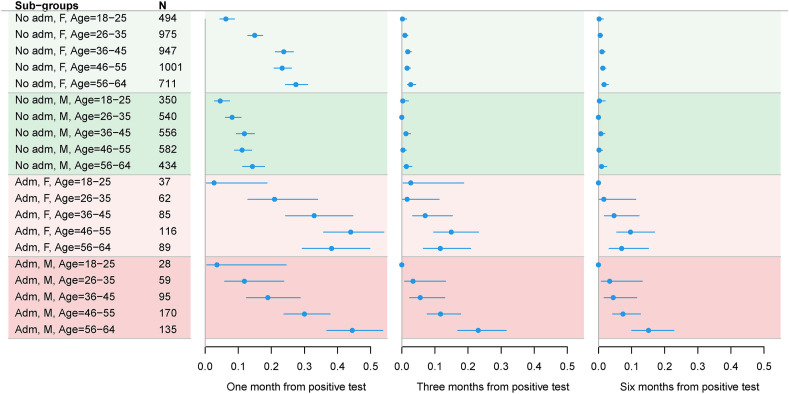
The cumulative incidences of no return to work within 1-, 3-, and 6-month follow-up from positive COVID-19 test in subgroups of admission status, sex, and age are shown in Fig. 3 . Very few patients in all subgroups of no admission did not return to work after 3 months. More female than male patients did not return to work after 1 month in patients not admitted to the hospital. In admitted patients, longer sick leave was overserved at all timepoints compared with patients not admitted, especially men aged 56–64 years experienced long sick leaves.
Fig. 3.
Patients not returning to work in % after first admission to the hospital in subgroups. Estimates and confidence intervals extracted from cumulative incidence. Abreviations: Adm = Admission, M = Male, F = Female.
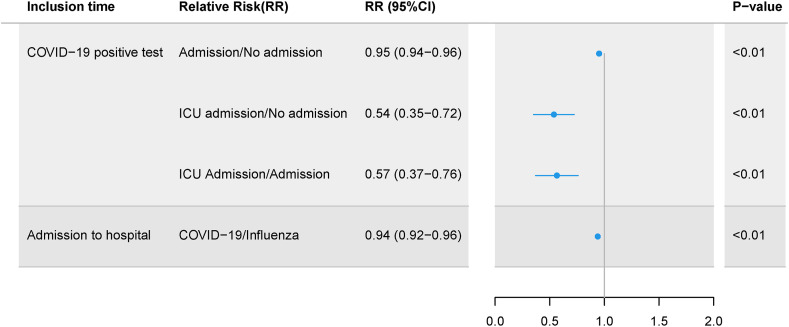
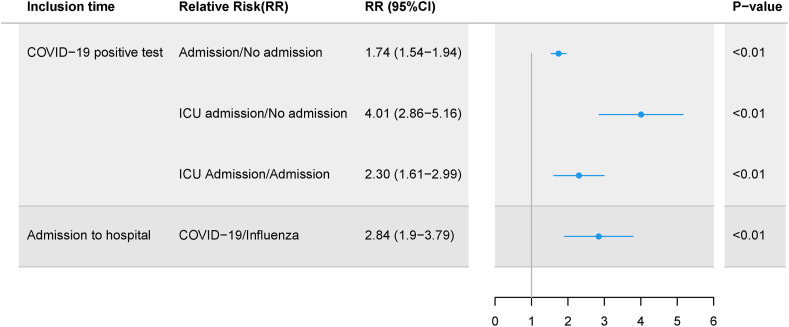
The relative chance of return to work 12 weeks after the first positive test between admission types and between influenza and COVID-19 is shown in Fig. 4 , and the average standardised chance in Table 2 , with the Cox regression used for g-modelling, is shown in figure S1 and S2. These figures show that patients admitted to the ICU are least likely to return to work, followed by patients admitted to a non-ICU department. Furthermore, the Cox model revealed increasing age, female sex, and comorbidity as risk factors for reduced chance of return to work (figure S1).
Fig. 4.
Relative chance of return to work within 3 months calculated from cox regression model. CI, confidence interval.
Table 2.
Mean chance of return to work.
| Inclusion time | Mean risk | Mean risk (95% CI) |
|---|---|---|
| COVID-19 positive test | No admission | 0.99 (0.98–0.99) |
| Admission | 0.94 (0.93–0.95) | |
| ICU admission | 0.53 (0.35–0.71) | |
| Admission to hospital | Influenza | 0.96 (0.94–0.97) |
| COVID-19 | 0.90 (0.88–0.92) |
CI, confidence interval.
Sick leave
The relative risk of sick leave above 4 weeks between patients not admitted vs admitted to non-ICU department vs admitted to ICU department and between influenza and COVID-19 is shown in Fig. 5 , and average standardised risk in Table 3 with the logistic regression model shown in figure S3 and S4. Admission to non-ICU, admission to ICU, and COVID-19 admissions compared with influenza admissions reveal a higher risk of sick leave above 4 weeks, with the highest relative risk in patients not admitted compared with patients admitted to the ICU. Furthermore, the logistic regression model revealed an increased likelihood of sick leave with increasing age, female sex, and in patients with comorbidity.
Fig. 5.
Relative risk of sick leave above 4 weeks calculated from logistic regression model. CI, confidence interval.
Table 3.
Mean chance of sick leave above 4 weeks.
| Inclusion time | Mean risk | Mean risk (95% CI) |
|---|---|---|
| COVID-19 positive test | No admission | 0.16 (0.16–0.17) |
| Admission | 0.29 (0.26–0.32) | |
| ICU admission | 0.66 (0.47–0.84) | |
| Admission to hospital | Influenza | 0.09 (0.06–0.12) |
| COVID-19 | 0.26 (0.23–0.29) |
CI, confidence interval.
Discussion
The study finds that most patients return to work after positive COVID-19 test within 4 weeks and that only very few patients had not returned to work within 6 months of follow-up. Tardive return to work was seen in patients admitted to the hospital and especially patients admitted to the ICU. The chance of returning to work is significantly lower for hospitalised patients compared with patients who were not hospitalised. Return to work after admission to the hospital is less often seen in COVID-19 patients compared with patients admitted with influenza.
Overall, in our study, less than 2% of patients did not return to work within 6 months. With COVID-19 affecting millions of people worldwide, the relatively few patients not returning may still amount to many patients affected as well as a considerable cost for society. Large surges in sick leave have been observed previously in relation to the first wave of COVID-19.17 In our study, we find that 6.6% of patients admitted to the hospital did not return to work. Huang et al. previously explored 6-month consequences of COVID-19 and found that 7% of hospital admitted experienced problems walking around and 2% problems preforming usual activity.1 Disabilities as these may impair patients' ability to work and the result in our study may therefore reflect the lack of recovery seen in some patients. Not surprisingly, the patients admitted to ICU experience a tardive return to work with almost half the relative chance of returning to work compared with patients not admitted to the hospital. Nonetheless, the absolute chance of returning to work within 3 months from positive test was 94% for patients admitted to a non-ICU department and 53% in patients admitted to an ICU department versus 99% in patients not admitted to hospital. Return to work has been explored in a COVID-19 ICU cohort, which found that 73% returned after 6 months.18 In our study, 60% returned to work, which is comparable taking the relatively few ICU admissions into account. In continuation, the difference in return to work seen between non-admitted and admitted patients indicates that the initial disease severity is a good indicator of patients' risk of prolonged return to work.
Poor health has previously been linked with a higher likelihood of unemployment.19 It is likely, with 1.5% still receiving sick leave benefit after 6 months, that some patients may have long-lasting health issues following COVID-19 infection that may make them more vulnerable to unemployment and maybe early retirement. These endpoints were however not explored due to the bias of lockdown measures on unemployment and the relatively limited follow-up time regarding the access to early retirement.
In this study, we found that women and older males had prolonged return to work. In the literature, it is described that males have more severe disease manifestations of COVID-19,20 which support our findings in the male group; however, it is contradictive that females should have longer sick leaves. Nonetheless, it is consistent with the findings in the preliminary results by Skyrud et al.7 Westerlind et al. found that admitted females had shorter sick leaves compared with admitted males, whereas non-admitted females had longer sick leaves compared with males.6 Similar tendencies are seen in this study with the overall effect indicating a reduced chance of return to work in women, which is somewhat surprising; however, nonetheless supported by the other studies.6 , 7
For hospitalised patients, we were able to compare return to work and sick leave in patients hospitalised due to COVID-19 with patients hospitalised due to influenza. We found that 2.6% of patients hospitalised with influenza did not return to work versus 6.6% in patients with COVID-19. The differences seen between influenza and COVID-19 are in line with what other studies have shown in that COVID-19 patients have worse outcomes compared with influenza patients.5 , 21
Long-term physical impairment is a likely underlying cause of the delayed or lack of return to work seen in our study. Others have found that COVID-19 patients admitted to hospital have low physical performance and impaired activities of daily living after hospitalisation.22 Non-admitted patients at a working age have also been found to have symptoms and impairment after the acute phase of COVID-19 infection.23 It is furthermore expected that COVID-19 may come with a risk of continuing to work while unwell, which may create delayed recovery and increased risk of future sick leave.24
Our study indicates that patients admitted to the hospital and patients of higher age are more vulnerable to having longer return to work similar to the findings in Westerlind et al. study.6 These and our other findings may have implications for post-COVID-19 infection control and rehabilitation. Rehabilitation has been shown to improve lung function and quality of life after COVID-19 infection.25 Future studies should explore rehabilitation after COVID-19 infection in patients' part of the workforce, considering the cost-effectiveness. If rehabilitation can improve patients' return to work and recovery, then it is likely that the decreased expenses in sickness benefit and the increased tax revenue is able to finance an increased focus of rehabilitation for this group of patients.
It is expected that the external validity of our results is good with similar findings regarding the effect of age, disease severity, and being female as discussed, with however relatively few studies on return to work after COVID-19 infection available.
Most COVID-19 patients return to the workforce quickly making universal interventions towards COVID-19 patients redundant. Efforts towards improving patients experiencing prolonged recovery from COVID-19 infections are already implemented in many countries with post-COVID-19 clinics. With a public financial incentive for patients to return to work as quickly as possible, efforts such as rehabilitation should be implemented as quickly as possible. These efforts should be aimed at the patients' part of the workforce who do not return to work following the contagious phase. This is not only in the patient's interest but is also likely a cost-effective strategy on a societal level. In the Danish setting, this could be that when public sick leave compensation starts, patients must be seen in a post-COVID-19 clinic to evaluate rehabilitation needs.
Strengths and limitations
Our study uses nationwide data on patients with a positive SARS-COV-2 PCR test, which in the period explored was the primary diagnostic tool for COVID-19 in Denmark. This means that our study includes most patients in the first wave of COVID-19 patients with a confirmed diagnosis, from patients who have mild disease to patients in need of hospital care hereby indicating how COVID-19 impacts longer sick leave periods in Denmark.
Due to the epidemiologic design, there are, however, limitations. The comparison of COVID-19 and influenza patients may be affected by restrictions implemented during the COVID-19 lockdown. Patients dying, emigrating or leaving the workforce due to early retirement were censored in the analyses. However, this was only the case for 13 patients. Patients' work capability at the time of return to work was unfortunately not available. Patients may be returning to part-time work instead of full-time work hereby impacting the workforce further.
Conclusions
The vast majority of patients returned to work after COVID-19 infection, with patients experiencing severe COVID-19 having prolonged time to return to work. Furthermore, COVID-19 patients experience longer time to return to work than what was observed in influenza patients. Future studies should explore if increasing rehabilitation treatment of severe COVID-19 patients can improve return to work and the cost-efficiency of the intervention.
Author statements
Ethical approval
Danish registry studies using encrypted data do not require ethical approval.
Funding
No funding was obtained for this study.
Competing interests
CTP has received grants for studies from Bayer and Novo Nordisk. KK has received research grants from The Laerdal Foundation and speaker's honoraria from Novartis. JB reports advisory board honorary from Bayer. No grants were obtained for the present study. The remaining authors do not have any conflict of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.12.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236379survivors of COVID -19:a retrospective cohort study using electronic health records. Lancet Psychiatr. 2021;8(5):416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiong Q., Xu M., Li J., Liu Y., Zhang J., Xu Y., et al. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect – Off Publ European Soc Clin Microbiol Infect Dis. 2021;27(1):89–95. doi: 10.1016/j.cmi.2020.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xue Y., Kristiansen I.S., de Blasio B.F. Modeling the cost of influenza: the impact of missing costs of unreported complications and sick leave. BMC Publ Health. 2010;10:724. doi: 10.1186/1471-2458-10-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludwig M., Jacob J., Basedow F., Andersohn F., Walker J. Clinical outcomes and characteristics of patients hospitalized for Influenza or COVID-19 in Germany. Int J Infect Dis. 2021;103:316–322. doi: 10.1016/j.ijid.2020.11.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westerlind E., Palstam A., Sunnerhagen K.S., Persson H.C. Patterns and predictors of sick leave after Covid-19 and long Covid in a national Swedish cohort. BMC Publ Health. 2021;21(1):1023. doi: 10.1186/s12889-021-11013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skyrud K., Telle K., Hernæs K., Magnusson K. 2021. Impacts of COVID-19 on sick leave.https://www.medrxiv.org Pre Print available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt M., Pedersen L., Sorensen H.T. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt M., Schmidt S.A., Sandegaard J.L., Ehrenstein V., Pedersen L., Sorensen H.T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kildemoes H.W., Sorensen H.T., Hallas J. The Danish national prescription registry. Scand J Publ Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 11.Helweg-Larsen K. The Danish register of causes of death. Scand J Publ Health. 2011;39(7 Suppl):26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 12.Jensen V.M., Rasmussen A.W. Danish education registers. Scand J Publ Health. 2011;39(7 Suppl):91–94. doi: 10.1177/1403494810394715. [DOI] [PubMed] [Google Scholar]
- 13.Hjollund N.H., Larsen F.B., Andersen J.H. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Publ Health. 2007;35(5):497–502. doi: 10.1080/14034940701271882. [DOI] [PubMed] [Google Scholar]
- 14.Blichert-Hansen L., Nielsson M.S., Nielsen R.B., Christiansen C.F., Norgaard M. Validity of the coding for intensive care admission, mechanical ventilation, and acute dialysis in the Danish National Patient Registry: a short report. Clin Epidemiol. 2013;5:9–12. doi: 10.2147/CLEP.S37763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlson M.E., Pompei P., Ales K.L., Mackenzie C.R. A new method of classifying prognostic Co-morbidity in longitudinal-studies - development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.UNESCO Institute for Statistics . Montréal; 2012. International standard classification of education ISCED 2011. [Google Scholar]
- 17.Calvo-Bonacho E., Catalina-Romero C., Fernandez-Labandera C., Fernandez-Meseguer A., Gonzalez-Quintela A., Martinez-Munoz P., et al. COVID-19 and sick leave: an analysis of the ibermutua cohort of over 1,651,305 Spanish workers in the first trimester of 2020. Front Public Health. 2020;8:580546. doi: 10.3389/fpubh.2020.580546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carenzo L., Dalla Corte F., Haines R.W., Palandri C., Milani A., Aghemo A., et al. Return to work after coronavirus disease 2019 acute respiratory distress syndrome and intensive care admission: prospective, case series at 6 Months from hospital discharge. Crit Care Med. 2021;49(11):e1157–e1162. doi: 10.1097/CCM.0000000000005096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bockerman P., Ilmakunnas P. Unemployment and self-assessed health: evidence from panel data. Health Econ. 2009;18(2):161–179. doi: 10.1002/hec.1361. [DOI] [PubMed] [Google Scholar]
- 20.Kragholm K., Andersen M.P., Gerds T.A., Butt J.H., Ostergaard L., Polcwiartek C., et al. Association between male sex and outcomes of Coronavirus Disease 2019 (Covid-19) - a Danish nationwide, register-based study. Clin Infect Dis. 2021;73(11):e4025–e4030. doi: 10.1093/cid/ciaa924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piroth L., Cottenet J., Mariet A.-S., Bonniaud P., Blot M., Tubert-Bitter P., et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2021;9(3):251–259. doi: 10.1016/S2213-2600(20)30527-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Belli S., Balbi B., Prince I., Cattaneo D., Masocco F., Zaccaria S., et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived hospitalisation. Eur Respir J. 2020;56(4) doi: 10.1183/13993003.02096-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meys R., Delbressine J.M., Goertz Y.M.J., Vaes A.W., Machado F.V.C., Van Herck M., et al. Generic and respiratory-specific quality of life in non-hospitalized patients with COVID-19. J Clin Med. 2020;9(12) doi: 10.3390/jcm9123993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kinman G., Grant C. Presenteeism during the COVID-19 pandemic: risks and solutions. Occup Med (Lond) 2021;71(6-7):243–244. doi: 10.1093/occmed/kqaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu K., Zhang W., Yang Y., Zhang J., Li Y., Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Compl Ther Clin Pract. 2020;39:101166. doi: 10.1016/j.ctcp.2020.101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.