Abstract
Successful cross-cultural communication is critical for adequate exchange of ideas with our patients. Our communities have become more diverse, and thus, the necessity has increased. The murder of George Floyd and other atrocities have sparked recognition of the need to address social injustice and racism and as we fight the ongoing coronavirus disease 2019 (COVID-19) pandemic. Allergist-immunologists are uniquely trained to explain the complex immunology of COVID-19 to patients, but they have less experience discussing issues of health equity. Here, we explore critical components of patient-provider communication: communicating with those for whom English is a second language, advising patients with limited health literacy, and understanding nonbiomedical views of health and wellness. Two barriers to communication are discussed: implicit bias and structural racism. Finally, we consider how the recent innovations in technology, the electronic health record including its patient portal and the use of telemedicine, have both impeded and improved communication. We offer suggestions as to what we could do to address these in our own local communities that would ensure better understanding and exchange of health information. This perspective grew out of an effort by the American Academy of Allergy, Asthma, and Immunology (AAAAI) Committee on the Underserved to provide training in cross-cultural communication.
Key words: Allergy, Health disparities, Social determinants of health, Health literacy, Structural racism, Illness representation
INFORMATION FOR CATEGORY 1 CME CREDIT.
Credit can now be obtained, free for a limited time, by reading the review articles in this issue. Please note the following instructions.
Method of Physician Participation in Learning Process: The core material for these activities can be read in this issue of the Journal or online at the JACI: In Practice Web site: www.jaci-inpractice.org/. The accompanying tests may only be submitted online at www.jaci-inpractice.org/. Fax or other copies will not be accepted.
Date of Original Release: April 1, 2022. Credit may be obtained for these courses until March 31, 2023.
Copyright Statement: Copyright © 2022-2024. All rights reserved.
Overall Purpose/Goal: To provide excellent reviews on key aspects of allergic disease to those who research, treat, or manage allergic disease.
Target Audience: Physicians and researchers within the field of allergic disease.
Accreditation/Provider Statements and Credit Designation: The American Academy of Allergy, Asthma & Immunology (AAAAI) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The AAAAI designates this journal-based CME activity for 1.00 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
List of Design Committee Members: Lenora Mendoza Noroski, MD, MPH, Kimberly Arcoleo, PhD, MPH, Benjamin D. Reese, Jr., PsyD, and Andrea J. Apter, MD, MA, MS (authors); David A. Khan, MD (editor)
Learning objectives:
-
1.
To understand the significance of low literacy and what we as allergist/immunologists can do about it for our patients.
-
2.
To identify specific “activist” actions that should be taken by healthcare professionals to contribute to eliminating structural racism and healthcare disparities.
-
3.
To identify four of the areas that support and reinforce structural racism in the United States.
-
4.
To discuss how an individual's illness representation influences symptom interpretation, healthcare seeking behavior, and adherence with the treatment regimen.
Recognition of Commercial Support: This CME has not received external commercial support.
Disclosure of Relevant Financial Relationships with Commercial Interests: All authors and reviewers reported no relevant financial relationships.
Introduction
The patient-provider relationship has long revolved around communication, with effective communication enhancing health outcomes, and ineffective communication stymying efforts. Communication within patient encounters encompasses written, spoken, and body language; literacy and technology. It can be impacted by the views that each party holds both explicitly and implicitly. Recent events, including social justice movements and the ongoing coronavirus disease 2019 (COVID-19) pandemic have re-ignited discussions regarding the need to effectively communicate across cultures in health care encounters. Allergists-immunologists are uniquely trained to communicate complex immunology to patients, which is particularly helpful for explaining coronavirus biology. The pandemic has also made it clear that enhancing communication skills are vital to the success of health care visits. Effective communication between patients and providers of different backgrounds is nuanced and requires deep understanding of the barriers and a multilayered approach for success. In this review, we build upon efforts initially undertaken by the American Academy of Allergy, Asthma, and Immunology (AAAAI) Committee on the Underserved to provide training on cross-cultural communication, and we explore critical components of the patient-provider relationship including English as a second language (ESL), health literacy, nonbiomedical views of health and wellness, implicit bias, structural racism, and communication considerations with respect to technology.
Health Literacy and ESL
Inadequate health literacy is considered the silent, hidden epidemic, intertwining the lack of language understanding by the patient with the lack of awareness by health care providers.1 Adequate health literacy “occurs when a society provides accurate health information and services that people can easily find, understand, and use to inform their decisions and actions.”2 Health literacy depends not only on reading and writing skills but also numeracy, listening, and speaking. It relies on cultural interpretations, conceptual knowledge, and integration of complex concepts.1 , 3 , 4 Among those with limited health literacy, quality of life and lifespan are shortened.5 , 6 Persons with low literacy are more likely to live in poverty, have poorer health outcomes, have increased Medicaid charges, and have greater health expenditures.4 , 7
According to the National Adult Literacy Survey (NALS) and International Adult Literacy Surveys (IALS), half of all American adults are below high-school learning levels, have difficulty locating and acting upon health information, and are incapable of accurately integrating written text. Up to 50% of people in developed countries are unable to sufficiently read, write, find, and comprehend the correct health information.1 In the United States, up to 1 in 5 persons speaks a non-English language at home with Spanish as the most common; of these, 40% have limited English proficiency and nearly 10% are considered linguistically isolated.1 , 7 This public health literacy problem is grossly underestimated and far more extreme across poor-resource populations globally, especially among the elderly, poor, racial, and ethnic minority patients, refugee, and non-English speakers.5
In addition to education, preconceived perceptions and learned behaviors are also a function of health literacy. Although health literacy issues are more severe among the poor and racial and ethnic minority communities, impaired health literacy can also be seen among educated populations resulting in distorted interpretations or denial of medical and public health messages.1 , 3 , 4 Individual, community, and cultural attitudes and beliefs play a critical role on how people decide to accept information, where value may be placed on the source and the sender of the information rather than the content of the information itself. The COVID19 pandemic is a potent example of how misinterpretation of evidence-based medical information can be related to the sources of delivery of the information and individual and population attitudes and beliefs.8, 9, 10
As clinicians, educators, and scientists, we all face challenges in getting our medical messages across effectively to our patients, especially to those with low health literacy skills and non-English speakers. Both non-English and English speakers struggle with understanding prescribed plans, interpreting meanings to medical terms and treatments of diseases, navigating health care systems, and identifying how to safely voice their concerns to be able reach and apply their health care effectively. Health care delivery systems are not well designed to serve all people of different languages and cultures. This has left behind poor and non-English speakers, resulting in exclusion or a disconnectedness from their own medical care.1 , 3 , 4 , 11
What Can We Do? Converting Awareness into Actions for Clinicians
A Health Literacy Model—An Awareness of the Problem and Determinant of Healthcare Outcomes is proposed (Figure 1 ). The health literacy constructs are (1) education, (2) cultural beliefs, (3) society attitudes, and (4) health care and government systems.1 Deficits to any of the variables affect health literacy and diminish health outcomes.1 , 3 , 4 Thus, this model of health literacy offers the following opportunities for providers to convert daily communication challenges into meaningful exchanges critical for effective patient care (Table I ).
-
1.
Education: Regardless of the language spoken or understood, present yourself with a welcoming body language to allow your patients to share with you their true concerns. Simplify all plans and language, using the fewest words for descriptions or explanations. Written materials should be provided in officially translated versions. Listen for the needs of your patient and family to be able to direct them to the services needed, such as for shelter, food, and safety in the home. Have your organization provide translators, social workers, and educators to assess and guide families in understanding needs. Utilizing trained translators is recommended instead of using friends and family as translators because they may also have health literacy challenges or could introduce personal beliefs/biases during translation. Electronic devices, from handheld to desktops, are a source for translation apps that are effective for brief phrases, whereas medical translators are necessary to achieve proper communication between health care providers and different-language speakers. Consider development of community-centered workshops to help patients become empowered and learn about their own health care. Develop focus groups for non–English-speaking patients to help providers learn more about patient needs.
-
2.
Cultural beliefs: Respectfully listen to your patients. Allow trust to develop so that patients feel safe in disclosing information that can indicate health literacy needs. Be aware and receptive of the way different cultural backgrounds can impact the interpretations of medical recommendations. Acknowledge and appreciate these differences and guide families to evidence-based resources with explanations for your rationale, in a supportive manner.
-
3.
Health care and government systems: For any discussions with patients and public announcements, avoid medical jargon and complex medical terms. Institute institution-wide health literacy education requirements for medical students, providers, and administrators and incentivize health literacy quality improvement projects. For office practices, implement similar programs or consider programs in the community hospital/clinic.
-
4.
Society attitudes and actions: Understand who your patient follows for advice. Align with patients in identifying a common thread between you and their community to derive empowering ways for having patients engaged. Through connecting patients with the community, society, and health professionals, they may come to rely and value your opinion enough to be able to accept evidence-based recommendations rather than the nonscientific or false information from nontruth sources.
Figure 1.
The Health Literacy Model as the determinant of health outcomes. A proposed model of health literacy constructs, (1) Education (blue); (2) Cultural Beliefs (orange); (3) Health Care and Government Systems (green); (4) Society Attitude and Actions (gray), with associated interacting variables as portals into awareness for needs assessment and opportunities for intervention toward inclusive and competent health literacy and healthy outcomes for all individuals, especially those of low literacy, minority, and non–English-speaking populations.
Table I.
The health literacy model constructs as portals of insight for actions in health equity and inclusion
| Health literacy constructs | Problem awareness and needs assessment | Actions for health equity and inclusions |
|---|---|---|
| Education | Poor literacy Non-English speaker Poor education Poor reading/writing Poor conceptual abilities Poor understanding No computer; no car Insecure or absent job Poor mobility means Household/living instability |
Welcoming body language Translator, native language (in-person, electronic video, voice, phone app) Simplify written action plans and oral explanations in both native language and English Listen for needs; connect patients with support Identify and provide language-specific health care professional advocate as integral to visits (educator, medical assistant, nurse, social worker) |
| Cultural beliefs | Traditions over prescribed medical plans not understood as harmful | Listen and respect traditions Provide rationale for prescribed plans in supportive way to avoid blame or humiliation |
| Health care/government systems | Misconstrued interpretations of complex medical terms and recommendations risk poor outcomes Poor understanding of computer use for digital appointments and care |
Avoid jargon, acronyms, and complex terms Replace complex terms with simple language for clinic visits and in explanations of public health diseases, such as COVID-19 Clarify misinterpretations with understanding Make health literacy an educational requirement for health care providers Identify clinic navigator for on-site/digital access in real time (educator, medical assistant, nurse, social worker) |
| Society attitudes | Impoverished Immigrant Non-English/poor English Learned attitudes; racism Popular but incorrect social media messages as strong influencers in medical decision making |
Listen to fears with without judgment Avoid assumptions in ethnicity and language Provide inclusive health care for all humans For patients: provide safety in the medical home and hospital/department resources/crisis hotline For health and community organizations: provide awareness on health literacy, tolerance, and inclusion Provide resources for health care team members and organizations to benefit all patients, especially those of poor health literacy and non-English speakers |
Nonbiomedical Views of Health and Wellness/Illness Representation
One often overlooked, but critical, content area during the clinical encounter is the individual’s beliefs about health and illness, known as illness representations. Evidence demonstrates that an individual’s illness representation may not be congruent with the health care provider’s, which can lead to treatment nonadherence (intentional and unintentional) and subsequently poor health outcomes.12 , 13 For example, many individuals view asthma as an acute, episodic condition that is unpredictable and not readily controlled. Many of these individuals prefer to be medication-free even if some symptoms remain.14 Conversely, evidence demonstrates that asthma is chronic and present even when an individual is asymptomatic but can be successfully controlled with consistent medication use.15
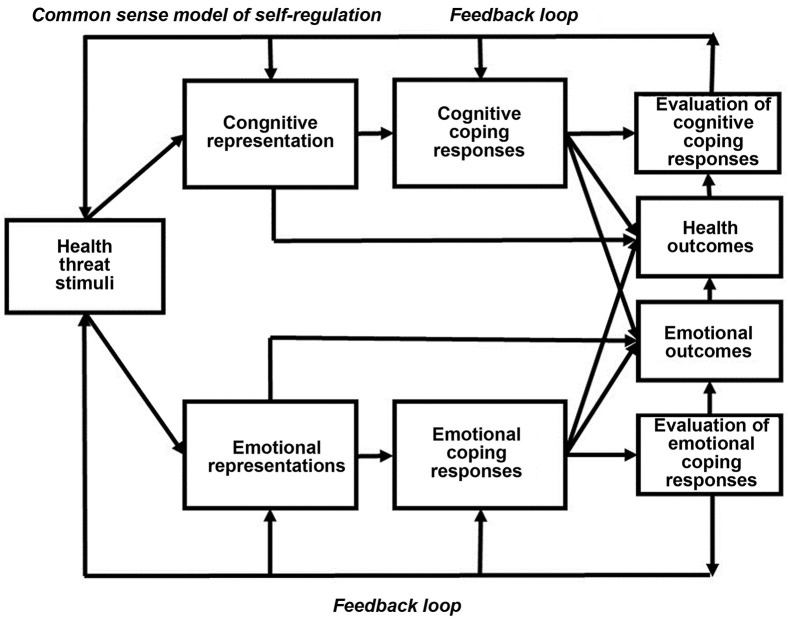
The Common Sense Model of Self-Regulation (CSM) is an extensively used framework for understanding illness representations. The CSM integrates environmental, social, and cultural factors with the individual’s beliefs about health and illness and has parallel arms representing cognitive processing of and emotional responses to the perceived health threat (Figure 2 ).16 , 17 How an individual perceives and interprets somatic sensations leads to recall of the individual’s normal function and prior experience with similar somatic sensations. The individual then constructs a mental representation of the illness threat that includes their beliefs about illness identity, what caused the illness, whether or not it can be controlled, potential consequences of the illness, illness duration, potential treatment/action plans, and finally, appraisal of outcomes.16 The CSM has also been used to understand a phenomenon known as “intentional non-adherence.”18 Intentional nonadherence is defined as when an individual consciously decides to discontinue, omit, or alter the prescribed treatment regimen.19 , 20 It has been estimated that only about half of individuals with a chronic condition take their medications as prescribed, which may be related to the desire to be medication-free.21
Figure 2.
The CSM integrates environmental, social, and cultural factors with the individual’s beliefs about health and illness and has parallel arms representing cognitive processing of and emotional responses to the perceived health threat.
Cultural beliefs and practices (eg, use of ethnomedical therapies) play a role in illness representations and adherence to treatment regimens.22 , 23 In a study by Arcoleo et al,22 among Mexican mothers of children with asthma, it was revealed that mothers had a limited understanding of the disease and had a preference for alternative treatment strategies owing to concerns with daily medication use (eg, fear of addiction, loss of effectiveness), particularly when their child was asymptomatic. One mother stated, “If we can find alternative ways to treat it that would be great… something that’s maybe a little more natural or holistic so that he doesn’t have to rely on so many chemicals.”22 A recent meta-analysis focused on studies using the CSM and reported that cultural beliefs and practices were significantly associated with medication adherence across a range of chronic conditions and that these factors may not always be congruent with Western medical beliefs and practices. Individuals reported that ethnomedical therapies (eg, Traditional Chinese Medicine, herbal preparations) were safer than prescribed medications and this belief may also lead to intentional nonadherence.
In the Latinx culture, familismo is a cultural practice grounded in prioritizing the family in health care decision making and emotional, instrumental, and social support.24 Familismo has demonstrated a protective effect in adolescent substance use, depression, and conduct problems.25, 26, 27 Similar to the Latinx culture, the Native American culture values family as the centerpiece of society and their traditions and practices place a strong emphasis on group involvement and decision making.28, 29, 30 In Native American culture, health is conceptualized as harmony with oneself, others, and the environment and emphasis is placed on spiritual aspects of healing versus a focus on physical aspects in Western medicine. Traditional medicine practitioners utilize a combination of traditional medicines, special foods, and healing and purification activities to restore an individual to health.28 Pasma, 1 of 7 common Filipino cultural beliefs, is the belief that homeostasis in one’s body is achieved by a balance of hot and cold elements and illness is caused by an imbalance in these elements, similar to yin and yang in Chinese culture.31 Health is restored when a condition considered as hot is treated with a cold remedy. These are just a few examples of cultural beliefs systems that health care providers should familiarize themselves with so that respectful, meaningful communication with their patients can occur.
What Can We Do?
Eliciting information about illness representations from patients should be viewed as an ongoing process that occurs over multiple visits. The conversation can begin with a simple question such as “What do you call your illness/condition?” This would provide a nice starting point for understanding the individual’s illness representation of that condition. The following are sample follow-up questions adapted from Kleinman et al, 1978,32 and Arcoleo et al, 201522:
-
1.
What do you think caused (name of illness/condition)?
-
2.
What problems do you think (name of illness/condition) causes?
-
3.
How severe is (name of illness/condition)?
-
4.
Will it have a long or short course?
-
5.
What kind of treatment do you think is necessary?
-
6.
What are the most important results you hope to receive from this treatment?
-
7.
Are there any other treatments or strategies you use to manage (name of illness/condition)?
-
8.
What do you fear most about (name of illness/condition)?
-
9.
What things make it difficult for you to manage (name of illness/condition)?
To fully engage in patient-centered care and achieve optimal health outcomes, it is critical that the individual and health care provider arrive at a shared management plan that acknowledges, respects, and when feasible, integrates these cultural beliefs and practices. Doing so will increase acceptance by patients of these management plans and potentially significantly improve adherence to the treatment plan.
Structural Racism: We Must All Be Activists for Racial Equity
The last decade has seen increased focus on social determinants of health (SDOH), as complementary to the traditional biological model of disease and illness development and progression. Many providers now recognize that individual, family, and community social conditions influence the probability of negative health exposure as well as impact the course and treatment of illnesses. Several seminal events have contributed to this shift.
In the early 2000s, the World Health Organization (WHO) began to increase its examination of nonbiological factors as contributors to health outcomes, particularly health inequities. A significant development was their 2005 Commission on Social Determinants of Health.33 The Commission, composed of international representatives from academia, health care, and politics, highlighted resource distribution and issues of power and powerlessness as impacting global health inequities. Aligning with the work of this global commission, the U.S. Center for Disease Control’s (CDC’s) 2011 Health Inequalities Report included in its determinants of health inequities, air quality, education, health care access, insurance, and housing.34 Although many providers, academics, and policymakers in the United States now acknowledge the role of these social and environmental factors in health inequities, it was not until the murder of George Floyd in May 2020 that these factors were more directly connected to structural racism in the Unites States.
Structural racism can be understood not only in its historical context, related to the enslavement of Africans and the practices and institutional structures of the 1880s, but also in the engrained and current manifestations of those structures. Four areas are prominent in examining the historical and current state of structural racism (not mutually exclusive) in America: (1) formal policies and laws within local and national governments, as well as policies within virtually every organization and institution; (2) norms and historical practices; (3) leadership by those with formal and informal power or influence; and (4) explicit and implicit bias and discriminatory behavior (Figure 3 ). These factors operate in an overlapping and self-reinforcing cycle.
Figure 3.
Structural racism is carved into the supports of our society. To address structural racism, the pillars must be addressed: policies and laws, institutional structures and systems, leadership, norms and practices, explicit and implicit bias.
For example, restrictive racial covenants in the housing contracts of homes in many U.S. cities laid the groundwork, for redlining in the 1930s. This was the practice by which the U.S. Home Owners’ Loan Corporation (HOLC) supported the creation of color-coded maps in 239 cities indicating residential security.35 Areas coded green on these maps were in locations with good housing stock, abundant services, frequently having tree-lined streets and parks. These communities, made up of primarily White residents, were considered highly suitable for mortgage lending support from the government. At the other end of the color-coded scale were primarily Black communities, areas designated in red on these maps. These were areas with poorer housing stock, few high-quality services (eg, stores, schools, health care services), fewer trees and parks and were deemed as risky investments, less suitable for mortgage support.
Although the Fair Housing Act of 1968 formally ended redlining, the engrained practices and biases continue to this day.36 Today, in major cities across the United States, formerly green-coded communities are mostly White, with high-quality housing and community services, and notably, many trees and parks contributing to low average temperatures during hot weather. A New York Times report in 2020 described green-coded communities in Richmond, Virginia, as currently having 42% of their land covered by trees and parks, whereas on average, red-coded communities had only 12% green space.37 Given the tendency for concrete and asphalt absorbing heat, red-coded areas can have a temperature 5° or more higher than neighboring green coded areas. Given the impact of heat-related health conditions, along with poor housing, underfunded schools contributing to poorer educational outcomes, under- and unemployment, few high-quality supermarkets, and health care options, the report documents that in Gilpin, a community in Richmond (formerly red-lined), the average life expectancy is 63 years, whereas in Westover Hills (formerly green-lined), a short drive away, the average life expectancy is 83 years. One cannot truly understand this stark disparity without a full understanding and appreciation of the engrained and overlapping elements of structural racism and implicit bias with its roots in the 1800s, but with present-day implications.
What Can We Do?
What is the role of health care providers and researchers and how is this role related to cross-cultural communication? At first glance, it might appear that most aspects of structural racism are outside of the responsibilities of medical providers and researchers and have little to do with communication with patients. That may be true in a traditional view of our role, in which the focus is primarily on researching and engaging the biological determinants of disease and illness and, in recent years, gaining an understanding of the range of social and cultural influences on illness. The recognition of these nonbiological factors has been a welcome and important development in health care. Communication involves understanding the experiences and heritage of our patients as well as our own unconscious biases. Given the deeply engrained nature of structural racism in America, a greater degree of activism for equitable treatment and racial justice must be part of the responsibilities of health care researchers and providers across our nation. These responsibilities should not be optional. The provider responsibility for effective communication in the clinical encounter is not optional. In research, pursuing knowledge, truth, without error isn’t viewed as optional. Actively engaging in work for racial and social justice must be a required element of the responsibilities of all health care professionals. The precise form of activism certainly depends on the specific context of a given professional role, along with a clear delineation of activities and outcomes, but all of us must share the responsibility for creating a more equitable health care environment and society. A more detailed discussion of this recommendation is beyond the scope of this brief manuscript, but activist responsibilities might include:
-
1.
Required education about the historical determinants and present implications of structural racism and implicit bias in health care, as well as in other sectors of American society
-
2.
Actively working to identify racial inequities, as well as other inequities related to underrepresented groups, in one’s area of practice or responsibility, and actively engaging in efforts to eradicate those inequities
-
3.
Identifying and implementing approaches to mitigate explicit and implicit bias in one’s area of practice or responsibility
-
4.
Identifying inequities in funding for health care, schools, and other public services, eliminating those inequities
-
5.
Examining and modifying professional education models to include not only an understanding of racial inequities but also the required activist role of health care professionals
-
6.
Make this learning part of premedical, medical, and maintenance of certification education
These must be integrated into position descriptions, measured, and individuals and departments must be held accountable. As long as we leave the work of ensuring racial justice and social justice more broadly, to those who specialize in that practice or have a certain title, then the rest of us run the risk of simply reflecting on social determinants of health, passively endorsing the efforts of the few with titles, and in an unintended way, being complicit in reinforcing systems and structures of racial inequities in health care.
Activism for racial and social justice must be the responsibility of all of us in health care.
The Role of Technology in Communication
There is little research on the best methods to communicate across cultures and even less on communication across race and ethnicity. However, technology for communication has increased dramatically as a result of the necessary social isolation caused by the COVID-19 pandemic. In health care, technology is used for virtual appointments, communication through patient electronic medical records portals, and mobile health care apps and monitoring devices. Patients have access to social media platforms that may post carefully vetted information from government agencies or unverified opinions or advertisements. However, not all patients have equal access to this information. This digital divide refers to “the growing gap between the underprivileged members of society, especially the poor, rural, elderly, and handicapped portion of the population who do not have adequate access to computers or the internet; and the wealthy, middle-class, and young Americans living in urban and suburban areas who have access.”38 Similarly, the digital divide affects communication between clinicians and less-privileged patients. In a 2019 American Community Survey, it was found that of 105,312,959 households, 32% were without a desktop or laptop, 21% were without a smartphone with data plan for internet access, and 14% were without any digital access. Furthermore, having no digital access was more frequent in nonmetropolitan households and in non-Latinx Black, Latinx, and Native American patients.39 There is also a digital divide based on age, which could further exacerbate health disparities. In a study of patients ages 65 to 79, it was found that adults ages 70 years and older were significantly less likely to be registered to use patient portals than those ages 65 to 69 years, and across the entire study population, Latinx, Black, and Filipino patients were less likely to use patient portals, own a digital device (in those > 75 years of age), use the internet or email, compared with non-Latinx White and Chinese patients.40 Even further illustrating the need for technology equity is a study showing that, among adults studied in a National Cancer Institute Survey on the use of eHealth, although there was no digital-use divide found by race or ethnicity, patients with lower socioeconomic status and lower education levels were less likely to communicate with providers online, track personal health information online, or download health information.41
Technology has advantages and disadvantages with respect to patient-clinician communication. For example, it has been used to advantage in virtual appointments. Virtual appointments allow patients who cannot travel to an appointment to have an evaluation. During the pandemic or during very bad weather, patients could still be evaluated. However, the resolution of the video for the encounters might not be adequate to diagnose some problems, for example, a skin eruption. It does not easily allow a physical examination, obtaining vital signs, or for procedures such as skin testing or food/drug challenges. Although there are devices on the market that allow for remote assessment of physical examination, these are not readily available to most providers. Another obvious disadvantage manifests when patients are unable to use or have limited access to the technology available to others. There are also many unanswered questions with respect to telemedicine such as how effective translation services are with telemedicine and how comfortable patients are with showing their home environments to providers on video visits.
What can we do?
Technology can be used to bridge health disparities if the equity issues are taken into consideration. Technology can be used to provide patients with essential information---explanations of how to take a medication or use an inhaler or to remind a patient of an appointment. Presented as a video, the information may be an invaluable device for overcoming low literacy or limited English proficiency. The challenge remains how to overcome barriers such as poor access to devices, poor access to internet connection whether wireless or data plan, and lack of knowledge and comfort level on how to use the technology. Methods to overcome these challenges include having accessible education on use of computers, internet, and mobile devices, with particular focus on funding for such education for rural and urban low-income areas. Health care institutions, agencies, practices, and hospitals could devote efforts to offer free health technology education for patients as well as education for providers on how to better reach and communicate with patients who do not have such access. At a broader level, efforts must be taken to address barriers that increase the social and digital divide. The social divide correlates with income: Latinx households are less likely to own computers than White households and less likely to use the internet. Schools with more minority students have fewer computers. Low-income communities, in general, lack the infrastructure available in more affluent communities. Over 100 years ago, electricity became available first only to the well-to-do. Similarly, consistent access to the internet is now potentially available to all, but must be made widely available. Universal internet access is as necessary as access to electricity, clean water, and basic phone service. Community-based internet access centers such as libraries and community centers must be supported. Also necessary are well-trained staff to support these centers; the use of computers and internet must be taught in the schools, with funding made available for rural and urban low-income areas. These resources should be accessible in public housing and become a requirement for all housing. Now more than ever, technology plays a crucial role in supporting and enhancing provider and patient communication. Evening the playing field and supporting efforts to improve technology issues will help address this critical aspect of health communication.
Discussion
Effective cross-cultural communication cannot be accomplished by addressing only solitary aspects such as ESL or literacy challenges. Rather, optimal communication requires acknowledgment of the full breadth of challenges and incorporating multiple strategies in a personalized fashion to achieve the necessary outcomes. Generally patient-provider encounters are short and must be focused, making addressing challenges and creating opportunities difficult. On the surface, it may seem that the major obstacle in a difficult- to-control asthma or eczema visit is compliance and language barriers but, when examined more deeply, also may include health literacy issues; cultural nonbiomedical views of illness and wellness, may be impacted by issues that are created by structural racism such as inadequate housing and poor access to services; and lastly exacerbated by lack of technology education to access resources suggested by the provider. How can one overcome this all in one visit? The answer is that it is not possible to tackle all of these complex issues in a typical 15- to 30-minute visit, but with preparation, providers can be well informed and anticipate and address these very real challenges. Preparing offices and staff to provide multilingual patient educational resources, having access to interpreters, screening for health literacy, and understanding both the economic and the societal challenges that an individual patient and community deal with provide a starting point for preparation for such visits. Identifying local resources to help with technology education, transportation, and addressing barriers to compliance may include not only social work but, in practices that do not have institutional resources, social workers, or interpreters, also might involve partnering with institutions and community organizations to best leverage available resources and to advocate for those needed, but not readily accessible, resources. Understanding the community that one serves is a critical starting point to understanding cultural nonbiomedical views of health and wellness, and to begin critical conversations to better understand, communicate, and utilize shared decision making. At a broader level, addressing structural racism and implicit bias at the practice level, institutional level, and as a citizen locally and nationally helps to pave the way to more equitable patient-provider encounters and better outcomes for all.
Footnotes
No funding has been received for this study.
Conflicts of interest: P. U. Ogbogu is on the advisory boards of AstraZeneca and GSK; and receives research funding from AstraZeneca. A. J. Apter is a consultant for UptoDate; associate editor of Journal of Allergy and Clinical Immunology; and receives support from the National Institutes of Health (R01HL143364, U01 HL138687). B. D. Reese, Jr., is CEO of BenReese, LLC. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Kindig D.A., Panzer A.M., Nielsen-Bohlman L., editors. Health Literacy: A Prescription to End Confusion. The National Academies of Sciences Engineering Medicine. National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Office of Disease Prevention and Health Promotion History of health literacy definitions https://health.gov/our-work/national-health-initiatives/healthy-people/healthy-people-2030/health-literacy-healthy-people-2030/history-health-literacy-definitions . Accessed September 23, 2021.
- 3.The National Academies of Sciences, Engineering, and Medicine . National Academies Press; Washington, DC: 2020. Health Literacy in Clinical Research: Practice and Impact. [PubMed] [Google Scholar]
- 4.Institute of Medicine of the National Academies . The National Academies Press; Washington, DC: 2013. Organizational Change to Improve Health Literacy: Workshop Summary. [DOI] [PubMed] [Google Scholar]
- 5.Fleary S.A., Ettienne R. Social disparities in health literacy in the United States. Health Lit Res Pract. 2019;3:e47–e52. doi: 10.3928/24748307-20190131-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nutbeam D., Lloyd J.E. Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Health. 2021;42:159–173. doi: 10.1146/annurev-publhealth-090419-102529. [DOI] [PubMed] [Google Scholar]
- 7.Glick J.E., Walker L., Luz L. Linguistic isolation in the home and community: protection or risk for young children? Soc Sci Res. 2013;42:140–154. doi: 10.1016/j.ssresearch.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sentell T., Vamos S., Okan O. Interdisciplinary perspectives on health literacy research around the world: more important than ever in a time of COVID-19. Int J Environ Res Public Health. 2020;17:3010. doi: 10.3390/ijerph17093010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gates B. Responding to COVID-19—a once-in-a-century pandemic? N Engl J Med. 2020;382:1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 10.Abel T., McQueen D. Critical health literacy in pandemics: the special case of COVID-19. Health Promot Int. 2021;36:1473–1481. doi: 10.1093/heapro/daaa141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Academies of Sciences, Engineering, and Medicine . The National Academies Press; Washington, DC: 2021. Exploring the Role of Critical Health Literacy in Addressing the Social Determinants of Health: Proceedings of a Workshop in Brief. [PubMed] [Google Scholar]
- 12.Kaptein A.A., Klok T., Moss-Morris R., Brand P.L. Illness perceptions: impact on self-management and control in asthma. Curr Opin Allergy Clin Immunol. 2010;10:194–199. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- 13.Arcoleo K., Marsiglia F., Serebrisky D., Rodriguez J., Mcgovern C., Feldman J. Explanatory Model for Asthma Disparities in Latino Children: Results from the Latino Childhood Asthma Project. Ann Behav Med. 2020;54:223–236. doi: 10.1093/abm/kaz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGovern C., Feldman J. Explanatory model for asthma disparities in Latino children: results from the Latino Childhood Asthma Project. Ann Behav Med. 2020;54:223–236. doi: 10.1093/abm/kaz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI) administered and coordinated National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC) Cloutier M.M., Baptist A.P., Blake K.V., Brooks E.G., Bryant-Stephens T., et al. 2020 Focused Updates to the Asthma Management Guidelines: a Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group [published correction appears in J Allergy Clin Immunol 2021;147:1528-30] J Allergy Clin Immunol. 2020;146:1217–1270. doi: 10.1016/j.jaci.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leventhal H., Phillips L.A., Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. 2016;39:935–946. doi: 10.1007/s10865-016-9782-2. [DOI] [PubMed] [Google Scholar]
- 17.Hagger M.S., Koch S., Chatzisarantis N.L.D., Orbell S. The common sense model of self-regulation: meta-analysis and test of a process model. Psychol Bull. 2017;143:1117–1154. doi: 10.1037/bul0000118. [DOI] [PubMed] [Google Scholar]
- 18.Mukhtar O., Weinman J., Jackson S.H.D. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31:149–157. doi: 10.1007/s40266-014-0153-9. [DOI] [PubMed] [Google Scholar]
- 19.Lehane E., McCarthy G. Intentional and unintentional medication non-adherence: a comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007;44:1468–1477. doi: 10.1016/j.ijnurstu.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Wroe A. Intentional and unintentional nonadherence: a study of decision making. J Behav Med. 2002;25:355–372. doi: 10.1023/a:1015866415552. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization . WHO; Geneva: 2003. Adherence to Long-Term Therapies: Evidence for Action. [Google Scholar]
- 22.Arcoleo K., Zayas L.E., Hawthorne A., Begay R. Illness representations and cultural practices play a role in patient centered care in childhood asthma: experiences of Mexican mothers. J Asthma. 2015;52:699–706. doi: 10.3109/02770903.2014.1001905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shahin W., Kennedy G.A., Stupans L. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Pref Adher. 2019;13:1019–1035. doi: 10.2147/PPA.S212046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabogal F., Marín G., Otero-Sabogal R., et al. Hispanic, familism and acculturation: what changes and what doesn't? Hisp J Behav Sci. 1987;9:397–412. [Google Scholar]
- 25.Stein G.L., Gonzalez L.M., Cupito A.M., Kiang L., Supple A.J. The protective role of familism in the lives of Latino adolescents. J Family Issues. 2015;36:1255–1273. [Google Scholar]
- 26.Lopez-Tamayo R., Seda A., Jason L.A. The role of familismo and acculturation as moderators of the association between family conflict and substance abuse on Latino adult males. Public Health (Fairfax) 2016;1:48–56. doi: 10.17140/PHOJ-1-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Germá M., Gonzalez N.A., Dumka L. Familism Values as a protective factor for Mexican-origin adolescents exposed to deviant peers. J Early Adolescence. 2009;29:16–42. doi: 10.1177/0272431608324475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duran B.E.S. American Indian belief systems and traditional practices. http://www.wellnesscourts.org/files/Duran%20-%20American%20Indian%20Belief%20Systems.pdf Accessed September 30, 2021.
- 29.Edwards E.D., Edwards M.E. American Indians: working with individuals and groups. Social Casework. 1980;61:498–506. [Google Scholar]
- 30.Tarrell A., Portman A., Garrett M.T. Native American healing traditions. Int J Disabil Dev Educ. 2006;53:453–469. [Google Scholar]
- 31.Abad P.J.B., Tan M.L., Baluyot M.M.P., Villa A.Q., Talapian G.L., Reyes M.E., et al. Cultural beliefs on disease causation in the Philippines: challenge and implications in genetic counseling. J Community Genet. 2014;5:399–407. doi: 10.1007/s12687-014-0193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleinman A., Eisenberg L., Good B. Culture, illness and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. 2008. https://www.who.int/publications/i/item/9789241563703 Accessed August 29, 2021. [DOI] [PubMed]
- 34.Centers for Disease Control and Prevention CDC Health Disparities and Inequalities Report. 2011. https://www.cdc.gov/mmwr/pdf/other/SU6001.pdf Accessed August 29, 2021.
- 35.U.S. Congress. U.S. Code: Home Owners' Loan Act, 12 U.S.C. §§1461-1468. 1934. Retrieved from the Library of Congress. https://www.loc.gov/item/uscode1934-001012012/ Accessed August 29, 2021.
- 36.Civil Rights Act of 1968. Section 800.
- 37.Plummer B. How Decades of racist housing policy left neighborhoods sweltering. The New York Times. August 24, 2020. https://www.nytimes.com/interactive/2020/08/24/climate/racism-redlining-cities-global-warming.html?searchResultPosition=
- 38.Stanford Computer Science. Digital Divide. Accessed August 6, 2021. https://cs.stanford.edu/people/eroberts/cs181/projects/digital-divide/start.html
- 39.Curtis ME, Clingan SE, Guo H, Zhu Y, Mooney LJ, Hser YI. Disparities in digital access among American rural and urban households and implications for telemedicine-based services. J Rural Health. Published online August 6, 2021. https://doi.org/10.1111/jrh.12614 [DOI] [PMC free article] [PubMed]
- 40.Gordon N.P., Hornbrook M.C. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res. 2016;18:e50. doi: 10.2196/jmir.5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kontos E., Blake K.D., Chou W.Y., Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;16:e172. doi: 10.2196/jmir.3117. [DOI] [PMC free article] [PubMed] [Google Scholar]