To date, the COVID-19 pandemic remains widespread globally, placing a heavy burden on healthcare systems around the world. High-flow nasal cannula (HFNC) improves oxygenation and reduces the need for endotracheal intubation in comparison with standard oxygen therapy in patients with severe COVID-19 [1]. During HFNC treatment, the prone position is associated with a significant benefit on oxygenation, but the low compliance of awake patients limits the clinical application of the prone position [2]. The lateral position may also be associated with beneficial effects of gas exchange, especially in unilateral lesions [3]. Although there are studies evaluating the efficacy of both prone and lateral positioning [4, 5], comparative studies on the efficacy of prone and lateral positions in HFNC patients with severe COVID-19 are rarely reported.
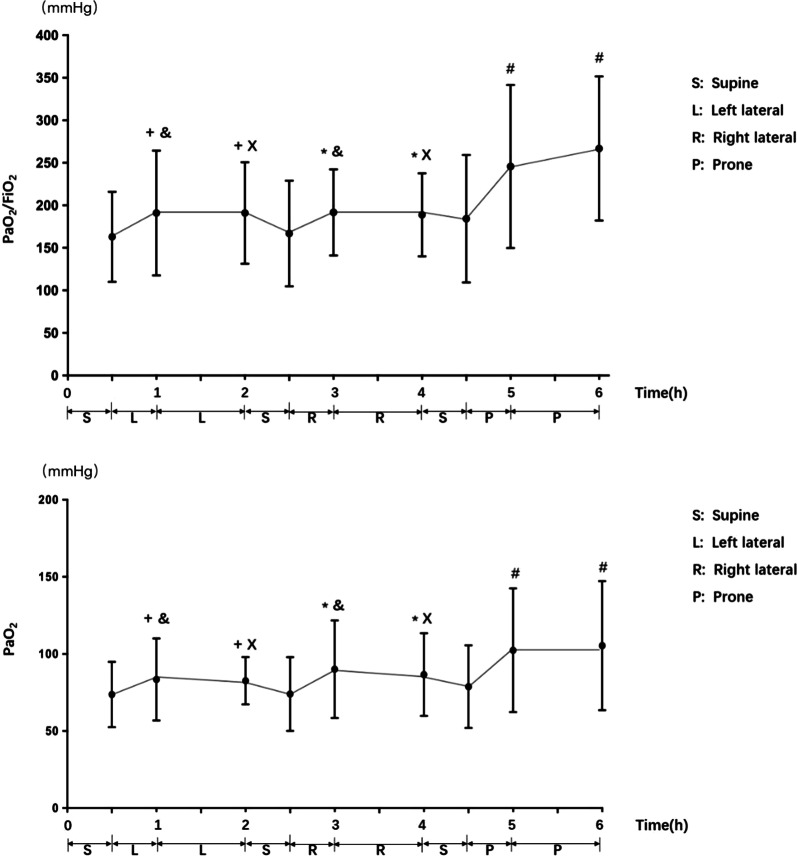
In this single-center prospective study, a total of 10 severe COVID-19 patients were included in the treatment center for severe COVID-19 patients in Heilongjiang Province of China. The severe COVID-19 patients in our study were those admitted to the ICU with PaO2/FiO2 ≤ 300 mmHg. Patients in supine position (0.5 h), left lateral position (1.5 h), supine position (0.5 h), right lateral position (1.5 h), supine position (0.5 h) , and prone position (1.5 h) treatment sequence. Blood oxygen saturation and respiratory rate were observed at each time point, and blood gas analysis was performed. (Fig. 1).
Fig. 1.
PaO2/FiO2 and PaO2 improved in left lateral, right lateral, and prone position compared with supine position (+P < 0.05 vs supine 0.5 h, *P < 0.05 vs supine 2.5 h, #P < 0.05 vs supine 4.5), and the improvement degree of PaO2/FiO2 and PaO2 in left and right lateral position was less than that of prone position (&P < 0.05 vs supine prone 5 h, xP < 0.05 vs supine prone 6h)
SAS v9.4 software was used for statistical analysis. Normally distributed quantitative data are described by the mean ± standard deviation (x ± s). The P values of pairwise comparisons were corrected by the Bonferroni method. The results showed that PaO2/FiO2 and PaO2 improved in the left lateral, right lateral and prone positions compared with the supine position. There was no significant difference between the left and right lateral positions, and it was independent of dominant side decubitus, but the improvement degree of PaO2/FiO2 and PaO2 was less than that of the prone position. There was no significant difference in oxygen saturation or respiration rate among different decubitus positions.
In conclusion, in HFNC patients with severe COVID-19, alternating left and right lateral positions improved oxygenation function. When the prone position is not tolerated for long periods of time, prone and lateral position alternating can be used to improve oxygenation.
Acknowledgements
Not applicable.
Authors' contributions
YC, CN, MZ, KY, and CW conceived and designed the study. YC and CW collected and analyzed the data. CN and CW wrote the manuscript. WM polished the manuscript. MZ, KY, and CW reviewed and revised the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Novel Coronavirus Pneumonia Emergency Treatment and Diagnosis Technology Research Project of the Heilongjiang Provincial Science and Technology Department and Provincial Natural Science Foundation Outstanding Youth Project (NO. JQ2021H003).
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding authors on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the First Affiliated Hospital of Harbin Medical University, code number kyk2020003.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yang Chong and Chuanchuan Nan contributed equally to this work.
Contributor Information
Changsong Wang, Email: changsongwangicu@163.com.
Mingyan Zhao, Email: mingyan1970@126.com.
Kaijiang Yu, Email: drkaijiang@163.com.
References
- 1.Tu GW, Liao YX, Li QY, Dong H, Yang LY, Zhang XY, Fu SZ, Wang RL. Prone positioning in high-flow nasal cannula for COVID-19 patients with severe hypoxemia: a pilot study. Ann Transl Med 2020;8(9):598. 10.21037/atm-20-3005. [DOI] [PMC free article] [PubMed]
- 2.Le MQ, Rosales R, Shapiro LT, Huang LY. The down side of prone positioning: the case of a coronavirus 2019 survivor. Am J Phys Med Rehabil. 2020;99(10):870–872. doi: 10.1097/PHM.0000000000001530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hewitt N, Bucknall T, Faraone NM (2016) Lateral positioning for critically ill adult patients. Cochrane Database Syst Rev 5:CD007205. 10.1002/14651858.CD007205.pub2. [DOI] [PMC free article] [PubMed]
- 4.Schifino G, de Grauw AJ, Daniele F, Comellini V, Fasano L, Pisani L. Effects of prone and lateral position in non-intubated patients with 2019 Novel Coronavirus (COVID-19) pneumonia. Pulmonology. 2021;27(2):167–171. doi: 10.1016/j.pulmoe.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Retucci M, Aliberti S, Ceruti C, Santambrogio M, Tammaro S, Cuccarini F, Carai C, Grasselli G, Oneta AM, Saderi L, Sotgiu G, Privitera E, Blasi F. Prone and lateral positioning in spontaneously breathing patients With COVID-19 pneumonia undergoing noninvasive helmet CPAP treatment. Chest. 2020;158(6):2431–2435. doi: 10.1016/j.chest.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding authors on reasonable request.