Abstract
Rationale
Pneumonia is the leading cause of death in children worldwide. Identifying and appropriately managing severe pneumonia in a timely manner improves outcomes. Little is known about the readiness of healthcare facilities to manage severe pediatric pneumonia in low-resource settings.
Objectives
As part of the HAPIN (Household Air Pollution Intervention Network) trial, we sought to identify healthcare facilities that were adequately resourced to manage severe pediatric pneumonia in Jalapa, Guatemala (J-GUA); Puno, Peru (P-PER); Kayonza, Rwanda (K-RWA); and Tamil Nadu, India (T-IND). We conducted a facility-based survey of available infrastructure, staff, equipment, and medical consumables. Facilities were georeferenced, and a road network analysis was performed.
Measurements and Main Results
Of the 350 healthcare facilities surveyed, 13% had adequate resources to manage severe pneumonia, 37% had pulse oximeters, and 44% had supplemental oxygen. Mean (±SD) travel time to an adequately resourced facility was 41 ± 19 minutes in J-GUA, 99 ± 64 minutes in P-PER, 40 ± 19 minutes in K-RWA, and 31 ± 19 minutes in T-IND. Expanding pulse oximetry coverage to all facilities reduced travel time by 44% in J-GUA, 29% in P-PER, 29% in K-RWA, and 11% in T-IND (all P < 0.001).
Conclusions
Most healthcare facilities in low-resource settings of the HAPIN study area were inadequately resourced to care for severe pediatric pneumonia. Early identification of cases and timely referral is paramount. The provision of pulse oximeters to all health facilities may be an effective approach to identify cases earlier and refer them for care and in a timely manner.
Keywords: pneumonia, health service accessibility, pneumonia, pulse oximetry, low- and middle-income country
At a Glance Commentary
Scientific Knowledge on the Subject
Severe cases of pneumonia, such as those marked with clinical features of hypoxemia, carry the highest risk of morbidity and mortality. Early diagnosis and treatment of severe pneumonia are associated with reduced mortality. There are limited data on the geographic accessibility of facilities that are adequately resourced to care for severe pediatric pneumonia in low- and middle-income countries.
What This Study Adds to the Field
To our knowledge, this is the first study to characterize the geographic accessibility of adequately resourced healthcare facilities to manage severe pediatric pneumonia in low- and middle-income country settings. We found inconsistent levels of resources across facilities and significant heterogeneity in the availability of healthcare personnel, equipment, and medications in nonhospital facilities. Although most of the population at each site had access to a facility within 30 minutes of travel time, few healthcare facilities were adequately resourced to manage severe pneumonia. Expanding the availability of pulse oximetry devices to all facilities may be an effective approach to identify cases earlier and refer them for care in a timely manner.
Pneumonia is the leading cause of death in children less than 5 years of age worldwide (1). Once hospitalized, mortality from pediatric pneumonia in high-income settings is 7–14% and 30–62% if complicated by hypoxemia or sepsis (2–4). Severe cases of pneumonia, such as those marked with clinical features of hypoxemia, carry the highest risk of morbidity and mortality (5). Timely diagnosis of severe pneumonia and early treatment is associated with reduced mortality. This includes recognizing clinical features of severity, such as hypoxemia and sepsis, and treating with supplemental oxygen (reduces mortality by 35%) and antibiotics (reduces mortality by 23%) (6, 7). However, for children to receive an appropriate diagnosis and be appropriately treated, a healthcare facility must have adequate resources: namely, a physician who is available for either management or consultation and can recognize severe presentations and progression to acute respiratory failure, pulse oximeters and supplemental oxygen to identify and treat hypoxemia, chest imaging to identify complications, and antibiotics (8–17).
Geographic inaccessibility is another barrier to appropriate care. Previous studies have shown that longer travel times to healthcare services are associated with a lower likelihood of seeking care and higher mortality (18). This disparity is greater in rural areas, where roads cannot always be traversed by car and many people rely on walking, bicycles, or public transportation (18). Expert groups have recommended that emergency services should be available within a 2-hour travel time, but there is limited assessment of this standard (19). Facilities that are adequately resourced to diagnose and treat severe pneumonia need to be identified so that patients can be directed to the appropriate facility. Healthcare facilities that implement effective triage to identify the most severely ill children were able to lower inpatient mortality (20, 21). To that end, infrastructure to facilitate transfers must exist. For example, equipment such as pulse oximeters can assist in early diagnosis and expedite appropriate triage. In the United States and other high-income countries, triage is done by centralized emergency dispatch systems. Triage teams use pulse oximetry as one tool to assess the severity of illness (22, 23). These systems remain underdeveloped in low-resource settings (24, 25).
There are limited data on the geographic accessibility of facilities that are adequately resourced to care for severe pediatric pneumonia in low- and middle-income countries (LMICs). We sought to understand the resource availability and geographic accessibility of facilities in four resource-poor settings in Guatemala, Peru, Rwanda, and India. We conducted a survey to identify the location, assets, and supplies that make a facility adequately resourced to care for severe pneumonia within the boundaries of the four LMIC sites. These resources were identified as necessary by a review of the literature and consensus among experts in pneumonia. Such resources include infrastructure, human resources, equipment, and medications in healthcare facilities. This evaluation allowed us to conduct a road network analysis and study the relationship between geography and facility-level resources.
Methods
Study Setting
This study was conducted as formative research for the HAPIN (Household Air Pollution Intervention Network) randomized controlled trial (see the online supplement). The HAPIN trial (https://clinicaltrials.gov/ct2/show/NCT02944682) is testing a complex clean energy intervention that consists of a liquefied petroleum gas stove, continuous fuel distribution, and behavioral messaging in 3,200 households at four international sites: Jalapa, Guatemala (J-GUA); Puno, Peru (P-PER); Kayonza, Rwanda (K-RWA); and Nagapattinam and Villupuram in Tamil Nadu, India (T-IND). Although all settings are rural, each site varies in size, population density, altitude, and indicators of wealth status (Table 1) (26–29). One of four primary outcomes for the HAPIN trial is the incidence of severe pneumonia. Therefore, understanding the healthcare system resources at each site was a necessary step in the design of a pneumonia surveillance strategy (26, 27).
Table 1.
Summary of Key Characteristics of Sites by Country Based on Sampling, Government Information, or Published Studies
| Jalapa, Guatemala | Puno, Peru | Kayonza, Rwanda | Tamil Nadu, India | |
|---|---|---|---|---|
| Regions | Santa Maria Xalapam, Ladinos Pardos | Puno, San Roman, Azangaro, Huancane, El Collao, Chicuito | Kabere, Kabarondo, Murama | Villupuram, Nagapattinam |
| Department or state | Jalapa | Puno | Kayonza | Tamil Nadu |
| Setting | Rural | Rural | Rural | Rural |
| Altitude range, mean, m (28) | 1,036–2,107 (1,362) | 3,827–4,348 (4,088) | 1,449–1,644 (1,547) | 1–919 (464) |
| Population density, people/km2 (38) | 482.1 | 32.5 | 93.2 | 737.5 |
| Study area, km2 (33) | 790 | 32,834 | 1,076 | 4,112 |
| 2019 GDP, USD, millions (29) | 1,340 | 226,848 | 10,122 | 2,875,142 |
| 2019 GDP per capita, USD (29) | 2,104 | 6,978 | 802 | 4,620 |
Definition of abbreviations: GDP = gross domestic product; USD = U.S. dollars.
Study Design
Investigators at each site were asked to identify public and private health facilities in the study area that treat children. Each site identified facilities to approach on the basis of recommendations of the regional ministries of health offices and previous experience. Facilities that care for specialized populations (e.g., veterans, military, or police) were excluded. A survey was developed by HAPIN investigators with local input to evaluate the type of facility, hours of operation, inpatient bed availability, healthcare personnel, equipment, and medications, together with availability of vaccines and implementation of cold-chain protocols (see the online supplement). The section on vaccines and cold-chain availability was only completed by J-GUA and P-PER. The survey was translated into each site’s local language and back-translated for quality control. Once developed, this survey was piloted in a selection of facilities and iteratively revised on the basis of feedback. HAPIN personnel approached each facility to administer the survey in person and collect geographic coordinates. Usually, the administrative leader of the facility was interviewed. All responses were entered into Research Electronic Data Capture software (Vanderbilt University) (30, 31). The study took place between February 17, 2018, and November 29, 2019.
Definitions
We trained research staff on how to complete the survey (online supplement). Facilities were categorized as hospitals, health centers, health posts, or other facilities (e.g., community centers or private clinics) on the basis of the self-report of facility type. We defined a facility as being open every day if it accepted patients for evaluation and treatment 7 d/wk, having overnight beds if it had beds that could be occupied overnight by a child, and having access to physicians who can recognize severe presentations of pneumonia or progression to acute respiratory failure that requires immediate intervention.
For the purposes of this paper, we defined equipment as long-term assets such as pulse oximeters and imaging equipment, and we defined medical consumables as short-term supplies that require consistent restocking such as antibiotics and oxygen. Supplemental oxygen was defined as oxygen therapy administered via a cylinder, compressor, or concentrator via nasal cannula, and a respiratory support device was defined as continuous positive airway pressure (CPAP), noninvasive positive pressure ventilation, or a mechanical ventilator. Finally, chest imaging was defined as having X-ray or ultrasound capacity, and antibiotics were antibacterial medications that could be administered orally, intravenously, or intramuscularly. We classified facilities as adequately resourced to manage severe pneumonia if they were open every day, had overnight beds, and had an available physician, a pulse oximeter, supplemental oxygen, respiratory support devices, X-ray or ultrasound capacity, and antibiotics. Our definition to classify a facility as adequately resourced is derived from a review of the literature and consensus among the experts engaged in the formative work for the pneumonia outcome of the HAPIN trial (27, 32).
Geospatial Database
For each study site, we built a geospatial database of health facilities, population density, road networks, and other topographic features such as mountains, rivers, and lakes relevant to travel by using ArcGIS Pro version 2.6.2 (ESRI). First, we mapped health facility locations by using longitude and latitude measurements obtained by study staff with a Global Positioning System receiver. We then mapped study boundaries by drawing a buffer around each surveyed health facility. The buffer distance was equal to the average distance between each health facility and the nearest health facility at that site. We constructed road networks by using OpenStreetMap (33) shapefiles and assigned half the maximum travel speeds on the basis of OpenStreetMap road classifications and publicly available speed limits for each country (34–37). We created population density layers by using raster surfaces from the 2018 WorldPop database (University of Southampton) (38). The WorldPop raster surfaces were based on census population counts that were disaggregated across 10,000-m2 grids weighted by land use, the degree of urbanization, and other demographic factors, as previously described elsewhere (39).
Geospatial Analysis
To assess the geographic accessibility of health facilities in each study area, we conducted a series of road network analyses by using the origin–destination cost matrix solver in the ArcGIS Pro Network Analyst extension (40). We divided every study area into a gridded matrix of 0.1 × 0.1-km cells and used the origin–destination cost matrix tool to estimate travel times on the basis of the least-cost pathway from every cell to different types of facilities. Travel time estimates incorporated multiple modes of travel, including walking to the road at 5 km/h and driving thereafter. Travel times also accounted for important network attributes such as speed limits or one-way roads; however, we did not account for traffic patterns or seasonal flooding. We then identified geographic regions that were within 30-, 60-, 90-, or 120-minute travel times to facilities with the following characteristics: any health facility, health facilities with all the necessary resources to manage severe pneumonia, health facilities with pulse oximeters, and health facilities with supplemental oxygen. To assess population accessibility, we overlayed the origin–destination cost matrix results on population density layers to determine the percentage of the study area population that was within each category of travel time.
Timely access to care in a healthcare network requires adequately resourced facilities that can manage severe pneumonia and lower-level facilities that can help diagnose severe pneumonia and refer cases promptly for treatment. We estimated the distribution of travel times for the population between two care-access scenarios: one with facilities that currently have pulse oximeters for the diagnosis of severe pneumonia and another hypothetical scenario in which all facilities had pulse oximeters.
Statistical Analyses
To compare the proportions of human resources, equipment, or medical consumables among sites, we used chi-square tests or Fisher exact tests (for variables with cell counts under five). To compare the distributions of travel times between the two care scenarios mentioned above, we used t tests. Statistical analyses and visualizations were conducted in R version 4.0.3 (“Bunny-Wunnies Freak Out,” R Foundation for Statistical Computing) by using the packages tidyverse, dplyr, formattable, reshape, and tibble (41).
Ethics Approval and Dissemination
The study protocol was reviewed and approved by institutional review boards or ethics committees at Emory University (00089799), Johns Hopkins University (00007403), the Sri Ramachandra Institute of Higher Education and Research (IEC-N1/16/JUL/54/49), the Health Ministry Screening Committee of the Indian Council of Medical Research [5/8/4-30/(Env)/Indo-US/2016-NCD-I], the Universidad del Valle de Guatemala (146-08-2016/11-2016), the Guatemalan Ministry of Health National Ethics Committee (11-2016), the Asociación Benéfica PRISMA, the London School of Hygiene and Tropical Medicine (11664-5), the Rwandan National Ethics Committee (No. 357/RNEC/2018), and Washington University in St. Louis (201611159). The study results will be disseminated to the appropriate stakeholders through presentations, conferences, and peer-reviewed journals.
Role of the Study Sponsors
The study sponsors participated in regular conference calls, made recommendations about study design, and participated in final decision-making on the study protocol; however, they did not have a role in the writing of this report or influence the decision to submit it for publication. The corresponding author had final responsibility for the decision to submit for publication.
Results
Description of Surveyed Facilities
We surveyed 350 facilities across all four settings, and completion rates at each site were as follows: J-GUA, 86%; P-PER, 99.5%; K-RWA, 100%; and T-IND, 96.2%. K-RWA had the highest number of facilities by population density, whereas T-IND had the highest number of facilities by area. Most facilities surveyed in T-IND and less than half of facilities surveyed in K-RWA were privately run, whereas all of those in J-GUA and P-PER were public. The geographic distribution of health facilities varied by country (Figure 1). For example, P-PER and J-GUA had one hospital per province with a spoke-and-wheel distribution of health centers and other facilities. Meanwhile, facilities were most evenly distributed in K-RWA and were most strongly clustered in a small geographic area in T-IND.
Figure 1.
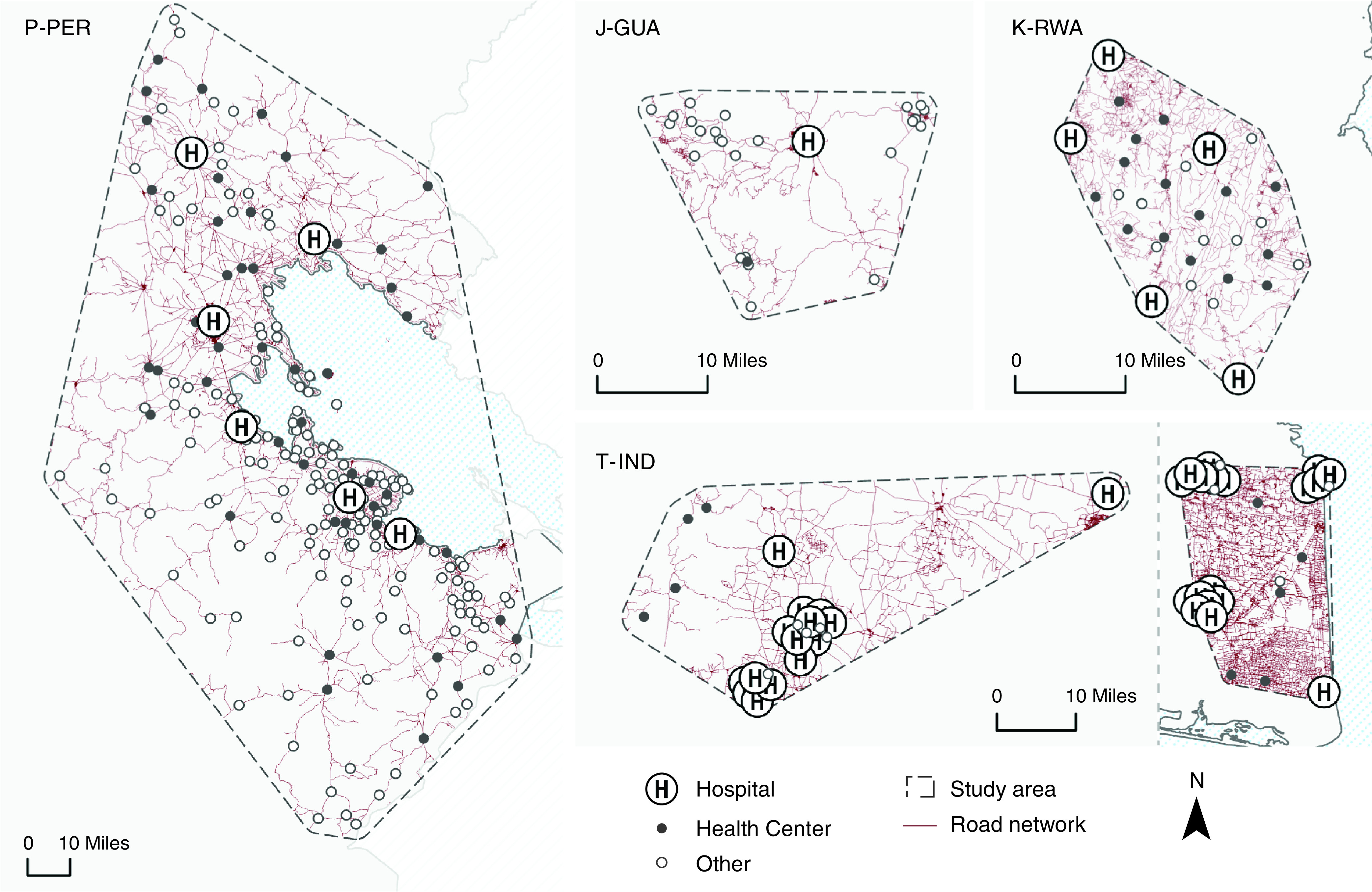
Healthcare facility locations and road networks in the study boundaries in J-GUA, P-PER, K-RWA, and T-IND. Each map displays the healthcare facilities by type and road network within the boundaries of each study site. Maps are not drawn to scale; they are sized to optimize the display of facility distribution at each site. Facility locations in India were offset with a minimum separation of 2.5 km so that facilities in very close proximity could be distinguished. Facility type (i.e., hospital, health center, and other) is based on country-specific designations. The “other” category includes health posts, community health centers, and private clinics. The T-IND study site comprises two separate sites in Villupuram (left) and Nagapattinam (right). J-GUA = Jalapa, Guatemala; K-RWA = Kayonza, Rwanda; P-PER = Puno, Peru; T-IND = Tamil Nadu, India.
Facility Characteristics
We summarized facility characteristics in Table 2. There was at least one hospital in each study catchment area by setting. Almost all hospitals were open every day and had overnight beds. K-RWA had the highest density of hospitals by population, whereas T-IND had the highest density of hospitals by area. In contrast, J-GUA had the lowest density of hospitals by population, and P-PER had the lowest density by area. K-RWA had the highest density of facilities with overnight beds by population and area, whereas J-GUA had the lowest. K-RWA also had the highest density of facilities that were open every day, whereas J-GUA had the lowest. P-PER had a large proportion of health posts that were open every day and had the highest density of health posts open every day by population and area.
Table 2.
Characteristics of Healthcare Facilities in the Four Resource-limited Settings of J-GUA, P-PER, K-RWA, and T-IND
| Number (%) of Facilities (n = 345) |
Facilities per Population of 100,000 |
Facilities per 100 km2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| J-GUA (n = 30) | P-PER (n = 221) | K-RWA (n = 41) | T-IND (n = 53) | J-GUA | P-PER | K-RWA | T-IND | J-GUA | P-PER | K-RWA | T-IND | |
| Type | ||||||||||||
| Hospital | 1 (3) | 6 (3) | 6 (15) | 35 (66) | 0.3 | 1 | 6 | 1 | 3 | 0.4 | 14 | 22 |
| Health center | 1 (3) | 60 (27) | 18 (44) | 9 (17) | 0.3 | 6 | 18 | 0.3 | 3 | 4 | 43 | 6 |
| Health post/other | 28 (93) | 155 (71) | 17 (41) | 9 (17) | 7 | 14 | 17 | 0.3 | 92 | 11 | 41 | 6 |
| Ownership | ||||||||||||
| Public | 30 (100) | 221 (100) | 25 (61) | 13 (25) | 7.9 | 20.7 | 24.9 | 0.4 | 98.4 | 16.0 | 60.2 | 8.2 |
| Private | 0 (0) | 0 (0) | 16 (39) | 40 (75) | 0 | 0 | 16.0 | 1.3 | 0 | 0 | 38.5 | 25.2 |
| Open every day | ||||||||||||
| All facilities | 2 (6) | 200 (90) | 31 (76) | 47 (89) | 0.5 | 18.7 | 30.9 | 1.5 | 2 | 18.0 | 343.0 | 20.0 |
| Hospitals | 1 (100) | 6 (100) | 6 (100) | 33 (94) | 0.3 | 0.6 | 6.0 | 1.1 | 1.0 | 6.0 | 6.0 | 33.0 |
| Health centers | 0 (0) | 60 (100) | 18 (100) | 9 (100) | 0 | 5.6 | 17.9 | 0.3 | 0 | 60.0 | 18.0 | 9.0 |
| Health posts/other | 1 (4) | 134 (86) | 7 (41) | 5 (56) | <0.1 | 12.4 | 7.0 | <0.1 | <0.1 | 133.0 | 7.0 | <0.1 |
| Overnight beds | ||||||||||||
| All facilities | 3 (10) | 28 (13) | 23 (56) | 35 (71) | 0.8 | 2.6 | 22.9 | 1.2 | 4.0 | 3.0 | 255.0 | 15.0 |
| Hospital | 1 (100) | 6 (100) | 6 (100) | 26 (74) | 0.3 | 0.6 | 6.0 | 0.9 | 1.0 | 6.0 | 6.0 | 26.0 |
| Health centers | 1 (100) | 20 (33) | 17 (94) | 8 (89) | 0.3 | 1.9 | 16.9 | 0.3 | 1.0 | 20.0 | 17.0 | 8.0 |
| Health posts/other | 1 (4) | 2 (1) | 0 (0) | 1 (11) | 0.3 | 0.2 | 0 | <0.1 | 1.0 | 2.0 | 0 | 1.0 |
Definition of abbreviations: J-GUA = Jalapa, Guatemala; K-RWA = Kayonza, Rwanda; P-PER = Puno, Peru; T-IND = Tamil Nadu, India.
More than 75% of facilities reported data.
Geographic and Population Accessibility to Health Facilities
Mean travel time from any location within the study area to the nearest facility ranged from 15 minutes in K-RWA up to 48 minutes in P-PER (Table 3). After accounting for population density, we found that at least 69% of people across all study areas live within 30 minutes of travel time to the nearest health facility (Figure 2). We observed greater variability in population accessibility with shorter travel times. Only a portion of health facilities were adequately resourced to manage severe pneumonia: 3% in J-GUA (1 hospital), 7% in P-PER (6 hospitals and 10 health centers), 15% in K-RWA (6 hospitals), and 42% in T-IND (15 hospitals and 6 health centers). Accordingly, the mean travel time to a facility ready to care for severe pneumonia ranged from 31 minutes in T-IND to 99 minutes in P-PER (Table 3). This represents an increase in travel time of 80% in J-GUA, 108% in P-PER, 161% in K-RWA, and 15% in T-IND when compared with travel times to the closest facility. Similarly, geographic accessibility to facilities with the necessary resources to manage severe pneumonia was lower than that of any facility across all settings (Figure 3). We found that only 43–63% of our populations lived within 30 minutes of travel time to a facility that was adequately resourced to care for severe pneumonia, with 5% of the population in P-PER being outside of a 2-hour travel time.
Table 3.
Mean Travel Times ± SD in Minutes for the Population at Each Site to Reach a Healthcare Facility by Resource Availability
| Any Facility in the Boundaries | Facilities with Pulse Oximetry | Facilities with Supplemental Oxygen | Facilities Ready to Diagnose and Treat Cases of Severe Pneumonia | |
|---|---|---|---|---|
| J-GUA | 23 ± 15 | 41 ± 19 | 32 ± 17 | 41 ± 19 |
| P-PER | 48 ± 36 | 67 ± 43 | 56 ± 9 | 99 ± 64 |
| K-RWA | 15 ± 8 | 22 ± 11 | 36 ± 19 | 40 ± 19 |
| T-IND | 27 ± 17 | 30 ± 19 | 30 ± 19 | 31 ± 19 |
For definition of abbreviations, see Table 2.
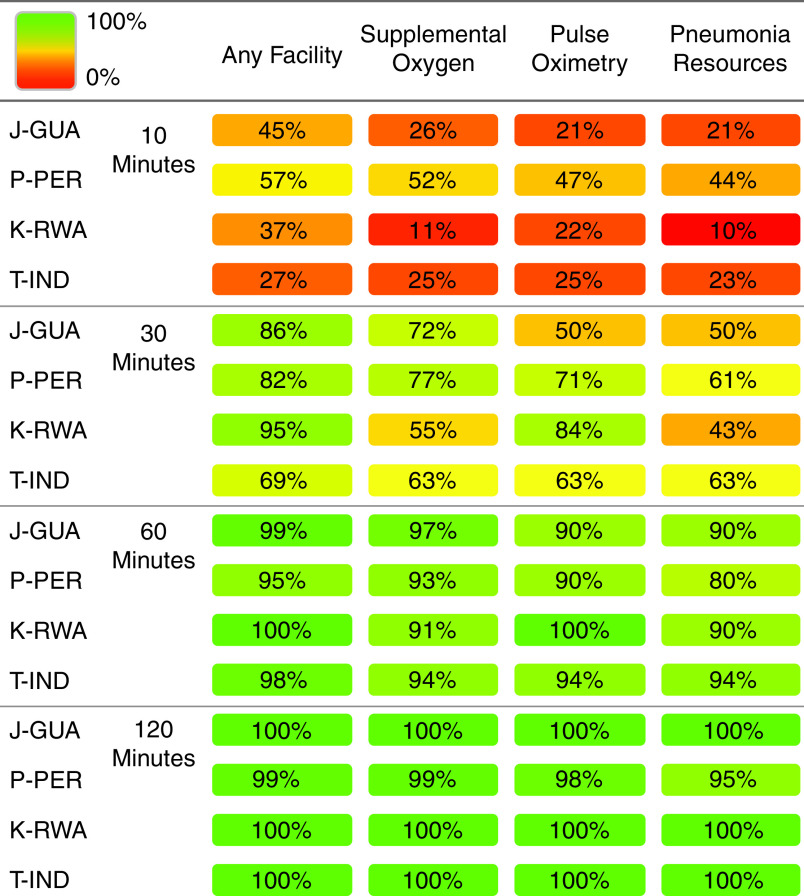
Figure 2.
Percentage of the modeled population living within a 10-, 30-, 60-, or 120-minute travel time to any health facility and to any health facility with available resources to administer supplemental oxygen, conduct pulse oximetry assessments, and diagnose and treat severe pneumonia. Study locations are J-GUA, P-PER, K-RWA, and T-IND. For definition of abbreviations, see Figure 1.
Figure 3.
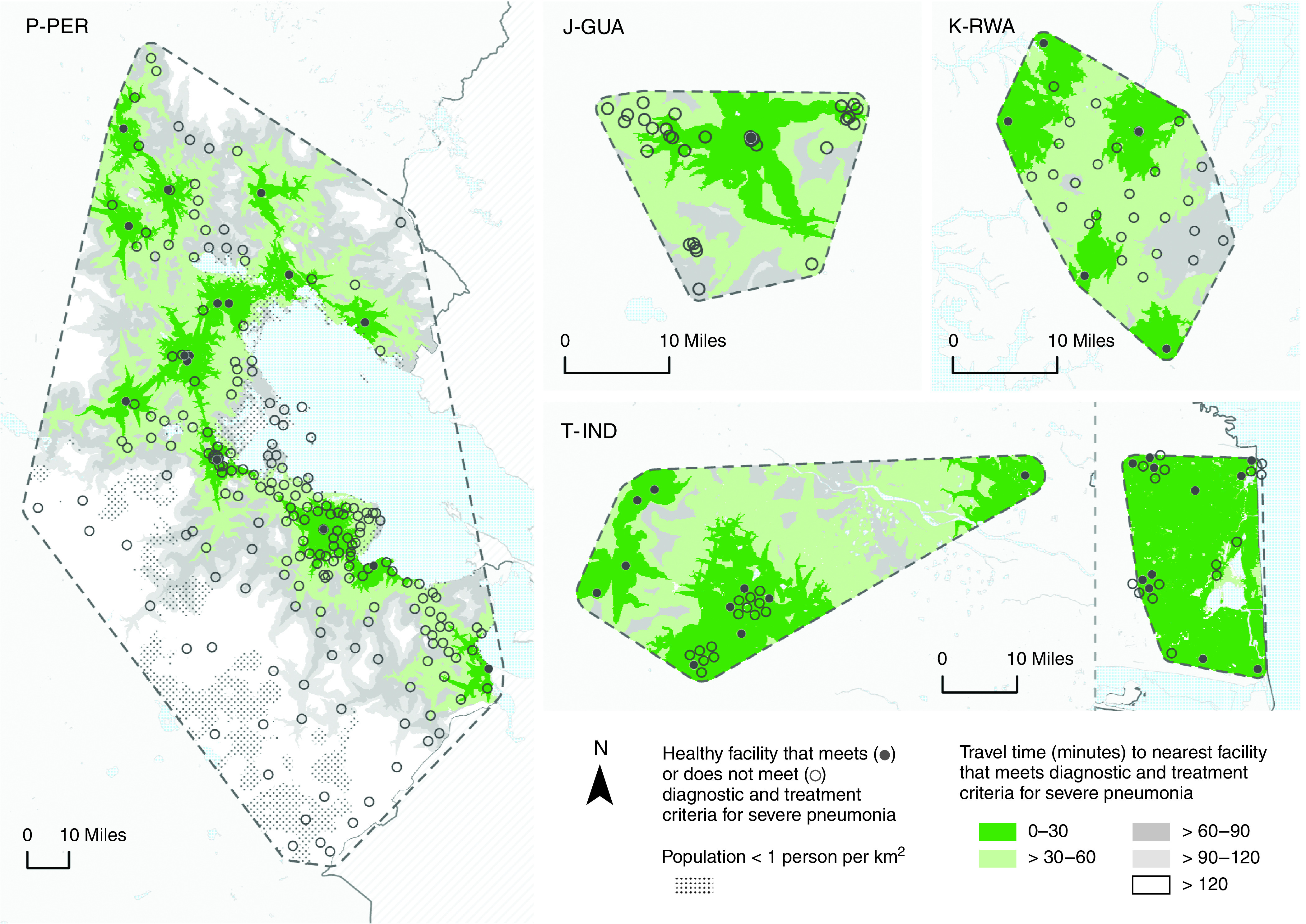
Geographic accessibility to health facilities adequately resourced to diagnose and treat severe pneumonia in J-GUA, P-PER, K-RWA, and T-IND. Solid and open circles represent health facilities that do or do not meet criteria to manage severe pneumonia (i.e., open every day with overnight beds, a physician onsite, pulse oximeters, supplemental oxygen, chest radiography or ultrasound capacity, and antibiotics available), respectively. Shading identifies regions that are within 30, 60, 90, and 120 minutes of facilities meeting these criteria. All maps were constructed in ArcGIS Pro version 2.6.2. Health facility locations were based on Global Positioning System (GPS) coordinates measured by study staff, and the availability of resources was derived from a comprehensive survey administered to facility leaders. Mapping and analysis were limited to facilities that provided information about pneumonia treatment criteria in the survey. Study area boundaries were estimated by using buffers equaling the average distance between each health facility and its closest neighboring health facility. Road networks were constructed by using OpenStreetMap roads where motorized travel was possible. Each study area was divided into a gridded matrix of 0.1 × 0.1-km cells, and the origin–destination cost matrix solver from ArcGIS Pro Network Analyst was used to estimate the least-cost pathway in minutes from every cell to the nearest facility meeting pneumonia management criteria. Travel time accounted for road attributes, such as speed limits and directional limitations, and incorporated multiple modes of travel (i.e., walking to the road at 5 km/h and driving at half of the speed limit thereafter). Maps were not drawn to scale. The T-IND study site comprises two separate sites in Villupuram (left) and Nagapattinam (right). For definition of abbreviations, see Figure 1.
Human Resources
We summarized available human resources in Table 4. K-RWA had the highest proportion of physicians available in all facilities, and it also had the highest density of physicians by population and area. In contrast, J-GUA had the lowest density of physicians in facilities by population, and P-PER had the lowest density by area. Nurses were more readily available than physicians across all facilities. Over 90% of facilities in T-IND and K-RWA had a nurse available during the day, whereas less than 35% of facilities in J-GUA and P-PER did. K-RWA had the highest density of nurses across all facilities, but T-IND had the highest density of nurses in hospitals.
Table 4.
Human Resource Availability of Healthcare Facilities in the Four Resource-limited Settings of J-GUA, P-PER, K-RWA, and T-IND
| Number (%) of Facilities (n = 345) |
Facilities per Population of 100,000 |
Facilities per 100 km2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| J-GUA (n = 30) | P-PER (n = 221) | K-RWA (n = 41) | T-IND (n = 53) | J-GUA | P-PER | K-RWA | T-IND | J-GUA | P-PER | K-RWA | T-IND | |
| Physician | ||||||||||||
| All Facilities | ||||||||||||
| ⩾1 during the day | 3 (25)* | 26 (21)† | 5 (100)* | 26 (67)† | 0.8* | 2.4† | 5.0* | 0.9† | 4.0* | 2.0† | 55.0* | 11.0† |
| ⩾1 each night of the week | 3 (23)* | 11 (9)† | 5 (100)* | 19 (53)† | 0.8* | 1.1† | 5.0* | 0.6† | 4.0* | 1.0† | 55.0* | 8.0† |
| Hospitals | ||||||||||||
| ⩾1 during the day | 1 (100)* | 6 (100)† | 5 (83)* | 18 (51)† | 0.3* | 0.6† | 5.0* | 0.6† | 1.0* | 6.0† | 5.0* | 18.0† |
| ⩾1 each night of the week | 1 (100)* | 6 (100)† | 5 (83)* | 11 (31)† | 0.3* | 0.6† | 5.0* | 0.4† | 1.0* | 6.0† | 5.0* | 11.0† |
| Nurses | ||||||||||||
| All Facilities | ||||||||||||
| ⩾1 during the day | 3 (16)† | 69 (32)‡ | 25 (96)† | 27 (90)† | 0.8† | 6.5‡ | 24.9† | 0.9† | 4.0† | 6.0‡ | 277† | 12.0† |
| ⩾1 each night of the week | 3 (10)† | 18 (8)‡ | 23 (74)† | 22 (81)† | 0.8† | 1.8‡ | 23.9† | 0.8† | 4.0† | 2.0‡ | 266† | 10.0† |
| Hospitals | ||||||||||||
| ⩾1 during the day | 1 (100)† | 6 (100)‡ | 6 (100)† | 18 (51)† | 0.3† | 0.6‡ | 6.0† | 0.6† | 1.0† | 6.0‡ | 6.0† | 18.0† |
| ⩾1 night of the week | 1 (100)† | 6 (100)‡ | 5 (83)† | 17 (49)† | 0.3† | 0.6‡ | 5.0† | 0.6† | 1.0† | 6.0‡ | 5.0† | 17.0† |
For definition of abbreviations, see Table 2.
Less than 50% of facilities reported data.
Between 50 and 75% of facilities reported data.
More than 75% facilities reported data.
Equipment and Medical Consumables
We summarized the availability of equipment and medical consumables across health facilities in each study area in Table 5. Equipment and consumables were widely available in T-IND. In contrast, J-GUA had the lowest proportion of facilities with available equipment and consumables. Specifically, a higher percentage of facilities in T-IND had available pulse oximeters (P < 0.001), respiratory rate counters (P < 0.001), oxygen supplementation (P < 0.001), and X-ray (P < 0.001) or ultrasound capacity (P < 0.001) available when compared with facilities in the other three settings. We mapped the geographic accessibility to supplemental oxygen across our settings in Figure 4. Supplemental oxygen was widely available in T-IND but was only available anywhere at 1 in 10 facilities in J-GUA, less than 2 in 10 facilities in K-RWA, and less than half of facilities in P-PER. Despite the limited availability of oxygen in J-GUA and K-RWA, 93% and 87% of the population were within 1 hour of a facility with oxygen, respectively. Only a small proportion of the population (6%) and the study area (8%) in T-IND were 1 hour away or more from a facility with oxygen. In contrast, 7% of the population and 38% of the study area in P-PER were 1 hour away or more from a facility with oxygen.
Table 5.
Equipment, Antibiotic, and Supplemental Oxygen Availability within Study Boundaries of Healthcare Facilities in the Four Resource-limited Settings of J-GUA, P-PER, K-RWA, and T-IND
| Number (%) of Facilities (n = 345) |
Facilities per Population of 100,000 |
Facilities per 100 km2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| J-GUA (n = 30) | P-PER (n = 221) | K-RWA (n = 41) | T-IND (n = 53) | J-GUA | P-PER | K-RWA | T-IND | J-GUA | P-PER | K-RWA | T-IND | |
| Pulse oximeter | 1 (3) | 69 (32) | 15 (37) | 45 (92) | 0.3 | 6.5 | 15 | 1.5 | 1.0 | 6.0 | 166 | 19 |
| Respiratory rate timer | 1 (3) | 99 (45) | 26 (63) | 41 (93) | 0.3 | 9.3 | 25.9 | 1.4 | 1.0 | 9.0 | 288 | 18 |
| Supplemental oxygen | 3 (10) | 104 (47) | 7 (17) | 42 (86) | 0.8 | 9.7 | 7.0 | 1.4 | 4.0 | 9.0 | 77 | 18 |
| Tank* | 3 (9) | 102 (46) | 6 (15) | 39 (74) | 0.8 | 9.5 | 6.0 | 1.3 | 4.0 | 9.0 | 66 | 17 |
| Compressor* | 1 (3) | 18 (8) | 1 (2) | 3 (6) | 0.3 | 1.7 | 1.0 | 0.1 | 1.0 | 2.0 | 11 | 1.0 |
| Ultrasound | 2 (7) | 31 (14) | 7 (17) | 33 (62) | 0.5 | 2.9 | 7.0 | 1.1 | 2.0 | 3.0 | 77 | 14 |
| X-ray machine | 1 (3) | 6 (3) | 6 (15) | 31 (60) | 0.3 | 0.6 | 6.0 | 1.0 | 1.0 | 1.0 | 66 | 13 |
| Infant scale | 28 (93) | 210 (95) | 29 (71) | 36 (78) | 7.4 | 19.7 | 28.9 | 1.2 | 35 | 19 | 321 | 15 |
| Child Scale | 29 (97) | 211 (96) | 35 (85) | 35 (78) | 7.6 | 19.8 | 34.9 | 1.2 | 36 | 19 | 387 | 15 |
| Antibiotics | ||||||||||||
| Always | 29 (97) | 132 (61) | 41 (100) | 40 (82) | 7.6 | 12.4 | 40.9 | 1.3 | 95.1 | 10.4 | 98.7 | 25.2 |
| Sometimes | 1 (3) | 64 (29) | 0 (0) | 0 (0) | 0.3 | 6.0 | 0 | 0 | 3.3 | 5.1 | 0 | 0 |
| Never | 0 (0) | 22 (10) | 0 (0) | 9 (18) | 0 | 2.1 | 0 | 0.3 | 0 | 1.5 | 0 | 5.7 |
| Antibiotic delivery | ||||||||||||
| i.v./i.m.* | 3 (9) | 197 (89) | 28 (68) | 29 (55) | 0.8 | 18.4 | 27.9 | 1.0 | 4 | 18 | 310 | 12 |
| p.o.* | 30 (86) | 99 (45) | 0 (0) | 35 (66) | 0.8 | 9.3 | 0 | 1.2 | 37 | 9.0 | 0 | 15 |
Definition of abbreviations: i.m. = intramuscular; i.v. = intravenous; J-GUA = Jalapa, Guatemala; K-RWA = Kayonza, Rwanda; p.o. = by mouth; P-PER = Puno, Peru; T-IND = Tamil Nadu, India.
Values represent the number and proportion of reporting facilities with indicated resources available. More than 75% of facilities reported data for each category.
Subcategories are not mutually exclusive, and proportions may add to more than 100%.
Figure 4.
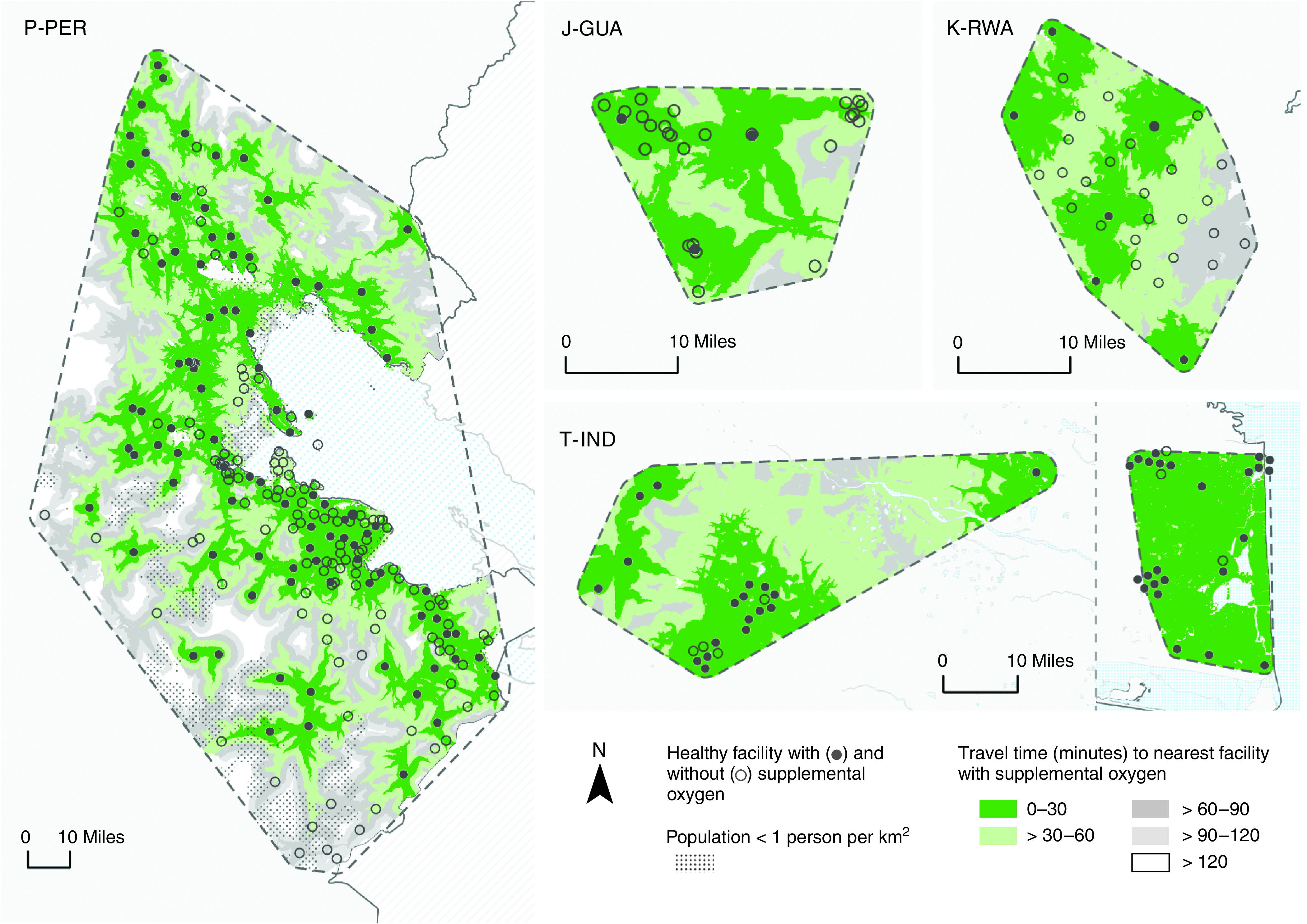
Geographic accessibility to health facilities with supplemental oxygen in J-GUA, P-PER, K-RWA, and T-IND. Solid and open circles represent health facilities with and without supplemental oxygen, respectively. Shading identifies regions that are within 30-, 60-, 90-, or 120-minute travel times to facilities with supplemental oxygen within study area boundaries. All maps were constructed in ArcGIS Pro version 2.6.2. Health facility locations were based on Global Positioning System (GPS) coordinates measured by study staff, and the availability of oxygen was derived from a comprehensive survey administered to facility leaders. Mapping and analysis were limited to facilities that provided survey responses for oxygen supplementation. Study area boundaries were estimated by using buffers equaling the average distance between each health facility and its closest neighboring health facility. Road networks were constructed by using OpenStreetMap roads where motorized travel was possible. Each study area was divided into a gridded matrix of 0.1 × 0.1-km cells, and the origin–destination cost matrix solver from ArcGIS Pro Network Analyst was used to estimate the least-cost pathway in minutes from every cell to the nearest facility with supplemental oxygen. Travel time accounted for road attributes, such as speed limits and directional limitations, and incorporated multiple modes of travel (i.e., walking to the road at 5 km/h and driving at half of the speed limit thereafter). Maps are not drawn to scale. The T-IND study site comprises two separate sites in Villupuram (left) and Nagapattinam (right). For definition of abbreviations, see Figure 1.
Expanding Coverage with Universal Pulse Oximetry
We mapped travel times for the two care-access scenarios in Figure 5: one with facilities that currently have pulse oximeters for the diagnosis of severe pneumonia and another hypothetical scenario in which all facilities had pulse oximeters. In the first scenario, mean travel time to the nearest facility with pulse oximeters ranged from 22 minutes in K-RWA to 67 minutes in P-PER. Expanding pulse oximetry coverage to all facilities reduced mean travel times by 18 minutes in J-GUA (44% reduction in mean travel time when compared with the first care-access scenario; P < 0.001), 19 minutes in P-PER (29% reduction; P < 0.001), 6 minutes in K-RWA (29% reduction; P < 0.001), and 3 minutes in T-IND (11% reduction; P < 0.001).
Figure 5.
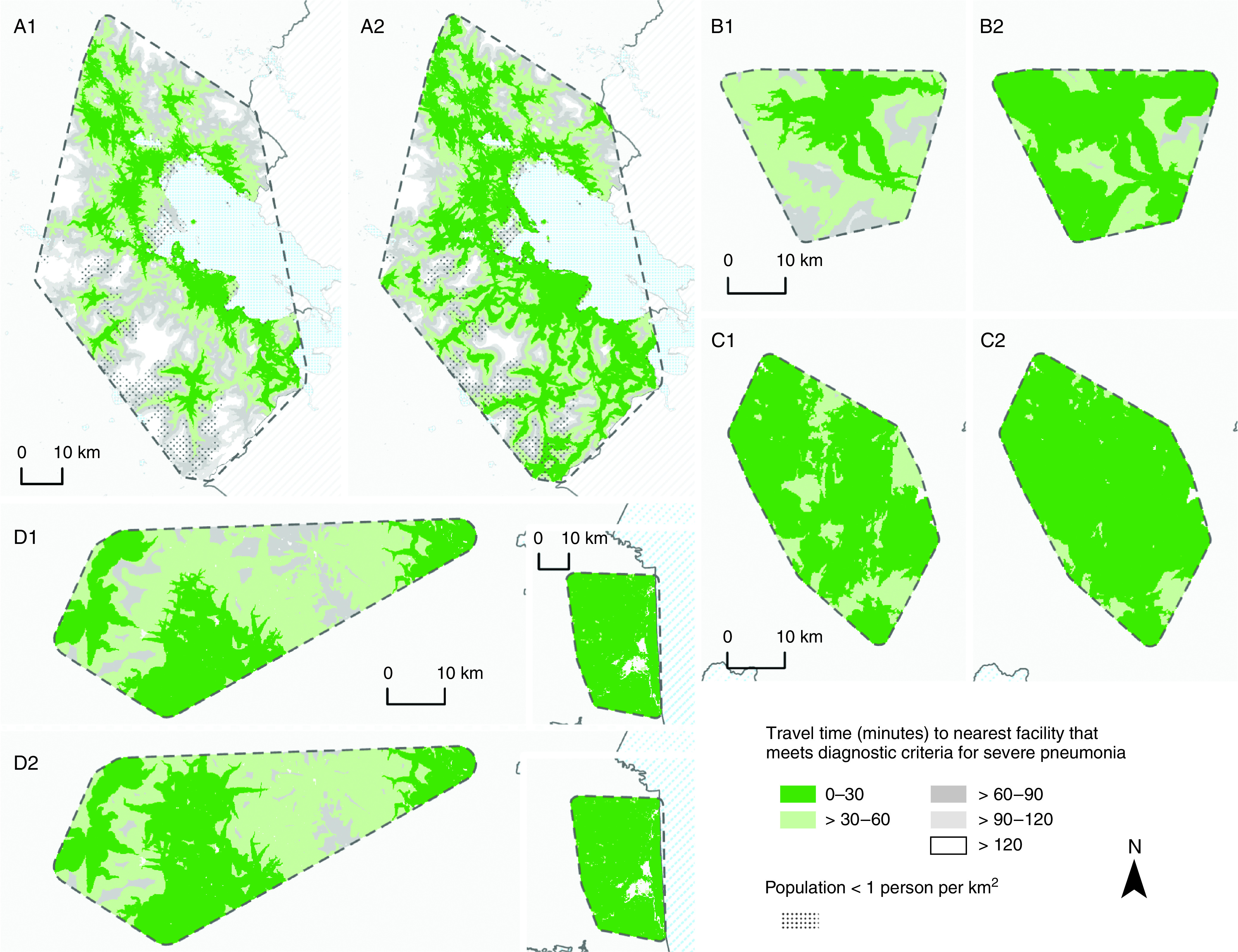
Geographic access to health facilities adequately resourced to diagnose and refer cases of severe pneumonia before and after the implementation of universal pulse oximetry coverage. (A1, B1, C1, and D1) Shading indicates the study areas in Puno, Peru; Kayonza, Rwanda; Jalapa, Guatemala; and Tamil Nadu, India (T-IND), respectively, that were within 10, 30, 60, 90, or 120 minutes of a facility with pulse oximetry (at the time of survey administration) for the diagnosis and referral of severe pneumonia; by default, this included facilities that were adequately resourced to treat severe pneumonia. (A2, B2, C2, and D2) Shading indicates regions in Puno, Peru; Kayonza, Rwanda; Jalapa, Guatemala; and T-IND, respectively, that would be within 30, 60, 90, or 120 minutes of a facility meeting the same diagnostic criteria if pulse oximetry were universally available in all facilities. Study area boundaries were estimated by using buffers equaling the average distance between each health facility and its closest neighboring health facility. Road networks were constructed by using OpenStreetMap roads where motorized travel was possible. Each study area was divided into a gridded matrix of 0.1 × 0.1-km cells, and the origin–destination cost matrix solver from ArcGIS Pro Network Analyst was used to estimate the least-cost pathway in minutes from every cell to the nearest facility with pulse oximetry before and after the hypothetical pulse oximetry intervention. Travel time accounted for road attributes, such as speed limits and directional limitations, and incorporated multiple modes of travel (i.e., walking to the road at 5 km/h and driving at half of the speed limit thereafter). Maps were not drawn to scale. The T-IND study site comprises two separate sites in Villupuram (left) and Nagapattinam (right).
Vaccine and Cold-Chain Availability
Streptococcus pneumoniae, rotavirus, and influenza vaccines were widely available in J-GUA and P-PER (Table 6). Although Haemophilus influenzae b vaccine was available widely in P-PER, it was less available in J-GUA. Not all parts of a cold-chain protocol were available in facilities that administered vaccines, but 73% of facilities in J-GUA and 99% of facilities in P-PER had parts of a comprehensive protocol in place.
Table 6.
Vaccine and Supporting Supply Availability in the Healthcare Facilities of J-GUA and P-PER
| Number (%) of Facilities (n = 251) |
||
|---|---|---|
| J-GUA (n = 30) | P-PER (n = 221) | |
| S. pneumoniae | ||
| Pneumococcal 13-valent conjugate vaccine | 28 (80) | 180 (81) |
| Pneumococcal polysaccharide vaccine (23-valent) | 0 (0) | 24 (11) |
| 10 or fewer serotypes/none | 1 (3) | 16 (7) |
| H. influenzae | ||
| ActHIB | 0 (0) | 1 (0.5) |
| Hiberix | 1 (3) | 22 (10) |
| Pentacel | 0 (0) | 6 (3) |
| Hib only available as part of pentavalent vaccine | 0 (0) | 176 (80) |
| None | 9 (26) | 13 (6) |
| Other | 7 (20) | 2 (1) |
| Rotavirus | 29 (97) | 200 (91) |
| Influenza | 28 (93) | 189 (86) |
| Pentavalent (DPT, HBV, Hib) | 7 (20) | 2 (1) |
| Supplies for storage and administration | ||
| Syringes and needles | 29 (97) | 209 (97) |
| Refrigerator | 17 (49) | 196 (89) |
| Freezer | 8 (23) | 217 (98) |
| Cold boxes | 3 (9) | 215 (97) |
| Vaccine carrier | 28 (80) | 218 (99) |
| Gel packs | 0 (0) | 31 (14) |
| Ice packs | 25 (71) | 218 (99) |
| Foam packs | 1 (3) | 213 (96) |
| Temperature monitoring device/data logger | 2 (6) | 211 (95) |
| Thermometer | 24 (69) | 213 (96) |
| Cold-chain protocol | 22 (73) | 214 (99) |
Definition of abbreviations: DPT = diphtheria, pertussis, and tetanus; H. influenzae = Haemophilus influenzae; HBV = hepatitis B virus; Hib = H. influenzae type b; J-GUA = Jalapa, Guatemala; P-PER = Puno, Peru; S. pneumoniae = Streptococcus pneumoniae.
Discussion
To our knowledge, this is the first study to characterize the geographic accessibility of healthcare facilities and their adequacy of resources to manage severe pediatric pneumonia in four LMIC settings. We found inconsistent levels of resources across facilities and significant heterogeneity in the availability of healthcare personnel, equipment, and medications in nonhospital facilities. Healthcare facilities in T-IND were better resourced than those at other study sites. K-RWA had the highest density of facilities, overnight beds, healthcare staff, equipment, and medications by population. Although most of the population at each site had access to a facility within 30 minutes of travel time, few healthcare facilities were adequately resourced to manage severe pneumonia. Consequently, the average population travel time to access severe pneumonia care was much greater than that for general services at all sites. As time is critical in the management of severe pediatric pneumonia, we found that the implementation of universal pulse oximetry across facilities reduced travel time and is a potentially cost-effective intervention. With reduced travel time, patients are more likely to seek care, receive an earlier diagnosis, and be triaged to a facility with adequate resources.
Resource availability in health facilities is largely driven by a country’s gross domestic product (42). T-IND, for example, had a higher percentage of adequately resourced facilities for the management of severe pneumonia; however, facilities were clustered, leading to longer travel times for remote-area populations. Despite having the lowest gross domestic product per capita, facilities in K-RWA had the highest availability of resources by population. This may be due in part to the national prioritization of universal health care after the genocide in 1994, in which over 1 million Rwandans were killed and many more were more displaced, which was followed by a collapse of the healthcare system (43, 44). Few facilities in P-PER had pulse oximeters and supplemental oxygen resources available, but remotely located facilities provide an opportunity to improve triage for severe pneumonia by adding universal pulse oximetry coverage. Overall, J-GUA had the fewest resources. Our evaluation also found that facilities in J-GUA and P-PER were adequately resourced with vaccines for pneumonia and cold-chain technology. As vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are becoming more available worldwide, knowledge of cold-chain availability is critical for vaccine distribution (45–47).
Our results align with those of previous studies demonstrating inconsistent availability of resources and geographic accessibility across healthcare facilities in LMICs (8, 12, 48, 49). For example, Ouma and colleagues (8) assembled the first Pan-African geocoded database of emergency care facilities and found that only a third of the countries surveyed met recommended population accessibility goals. A previous study conducted a detailed analysis of healthcare facility resources to manage severe acute respiratory disease in Vietnam and cited significant variation between district-and provincial-level hospitals but did not assess geographic accessibility (50). Expanding on these approaches, we combined geographic and population accessibility analyses with a refined assessment of resources to manage severe pneumonia. We propose a definition to recognize a facility as adequately resourced to manage severe pneumonia if certain components are met. Currently, the literature does not have a comprehensive definition to define a facility as adequately resourced to appropriately manage severe pneumonia. These findings support the need to develop publicly available facility lists that identify the available resources. Indeed, the World Health Organization has called on countries to develop such lists, which can be used to identify gaps in coverage and resource planning (48, 51–53). For example, supplemental oxygen should be universally available; however, this is not realistic in most low-resource settings. For supplemental oxygen to be available, facilities need to have consistent electricity for compressors and concentrators (54). Furthermore, facilities need to maintain a stock of nasal cannulas and train medical staff on how to provide appropriate oxygen therapy (54). Nonetheless, more cost-effective solutions may be available to overcome limitations in oxygen availability. Here, we demonstrated that expanding coverage of pulse oximeters in local facilities can assist in the triage of severe pneumonia to adequately resourced facilities. A recent study in Nigeria found that implementing an improved oxygen system had no effect on outcomes in children when compared against the introduction of pulse oximetry, which may have reduced death from pneumonia by 50% (55).
Despite the strengths of this study, we acknowledge some potential shortcomings. First, we assumed that all roads were traversable; however, roads in low-resource LMIC settings may be unreliable and in poor condition for travel (18, 56). Moreover, many patients in LMIC populations must walk, bike, or use public transportation to reach facilities because of lack of access to a private vehicle or limited access to taxis (56). Second, our analysis is based on most but not all healthcare facilities in each study area, potentially introducing selection bias (12). Specifically, excluded health facilities may have shorter travel times, whereas not all health facilities in the survey may be financially accessible. Third, we relied on the self-report of resources by a facility representative. We did not visually confirm the availability of infrastructure, staff, equipment, and medical consumables or assess equipment functionality. For example, supplemental oxygen tanks may be present but not filled with oxygen (14). Furthermore, there may be a limited supply of oxygen because of production or transportation. We also did not evaluate clinical knowledge of staff or their ability to use the equipment. For example, oxyhemoglobin saturation should be measured in each patient with suspected pneumonia to evaluate for hypoxemia as a decision tool to provide supplemental oxygen (10). A recent study in Nigeria evaluated 12 secondary hospitals and found that only 19.4% of children who were hypoxemic during admission received supplemental oxygen. Furthermore, this study found that the determination that children were hypoxemic was often based on clinical judgment rather than pulse oximeter data, even if a pulse oximeter was available (57). Hospital staff are often not properly trained to operate other lifesaving equipment such as invasive and noninvasive ventilators, which could be lifesaving in a critically ill patient (14, 58). Along the same lines, we had a low response rate to survey questions evaluating whether staff were trained to conduct and interpret an X-ray or perform and interpret a lung ultrasound, thus limiting our ability to assess whether staff were adequately trained to use these modalities. Fourth, we did not account for resources at nontraditional facilities (e.g., holistic care) or within local community health worker networks. Fifth, we required facilities to have a physician available as a criterion to assess readiness to manage severe pneumonia cases, given that licensed physicians usually receive more advanced training in the management of severe respiratory illnesses and complications. This survey was designed by a multidisciplinary team of experts in pneumonia, and we agreed by consensus that a physician is the ideal healthcare provider to be present in a facility to guide the management of severe pneumonia. Although we agree that other healthcare personnel may be equally as capable as physicians of managing most cases and presentations of pneumonia, severe pediatric pneumonia is a serious, life-threatening, and complicated condition that requires higher-level management, and physicians should be available as a resource for management or consultation. Because the front-line provider may not be a physician in many LMIC settings, further assessment of the scope and quality of other healthcare professional training for severe cases of pneumonia may be warranted; however, this was outside the scope of this study. Sixth, we had a low response rate regarding the availability of respiratory support devices. Although high-flow systems that include nasal cannulas, CPAP, and mechanical ventilators are critical tools for the management of severe pneumonia, they are uncommon in most resource-poor facilities of LMICs. Moreover, use of devices like the bubble CPAP for severe pneumonia management in LMICs is controversial (59). If a child is failing supplemental oxygen, then we would recommend referral to a facility with a higher level of clinical expertise and knowledge of these advanced respiratory support devices. Finally, we assumed that patients would travel to the closest facility and did not account for other factors, such as trust and familiarity, which often influence or drive healthcare facility choices (24).
In summary, we found that most healthcare facilities in our low-resource study settings in Guatemala, Peru, Rwanda, and India were inadequately equipped to provide care for severe pneumonia. Early identification of cases and timely referral is therefore paramount. However, given the lack of centralized emergency dispatch systems for patient triage, universal coverage of health facilities with pulse oximeters may be an effective approach to identify cases of severe pneumonia closer to a patient’s home and appropriately refer them for care.
Acknowledgments
Acknowledgment
The authors thank the pneumonia experts who participated in their workshops: Prof. Heather Zar of the University of Cape Town (Cape Town, South Africa), Prof. Harry Campbell of the University of Edinburgh (Edinburgh, United Kingdom), Prof. Claudio Lanata of the Instituto De Investigacion Nutricional (Lima, Peru), Dr. Carina King (Karolinska Institute, Sweden), and Dr. Laura Hammitt (Johns Hopkins University, Baltimore, Maryland). In addition, they thank Katerina Lescouflair, M.S.P.H., and Delaney Connolly from Johns Hopkins University (Baltimore, Maryland) for assistance with preparation of the protocols and development of materials, as well as Michael Peters, M.S.P.H., from the Johns Hopkins School of Public Health and Juan Eugenio Hernandez Avila from the Medical Sciences at the Instituto Nacional de Salud Pública for their expert input on the geospatial component. A multidisciplinary, independent data and safety monitoring board appointed by the NHLBI monitors the quality of the data and protects the safety of patients enrolled in the HAPIN trial.
NHLBI Data and Safety Monitoring Board: Nancy R. Cook, Stephen Hecht, Catherine Karr, Katie H. Kavounis, Dong-Yun Kim, Joseph Millum, Lora A. Reineck, Nalini Sathiakumar, Paul K. Whelton, and Gail G. Weinmann.
Program Coordination: Gail Rodgers, Bill and Melinda Gates Foundation; Claudia L. Thompson, National Institute of Environmental Health Science; Mark J. Parascandola, National Cancer Institute; Danuta M. Krotoski, Eunice Kennedy Shriver National Institute of Child Health and Human Development; Joshua P. Rosenthal, Fogarty International Center; Conception R. Nierras, NIH Office of Strategic Coordination Common Fund; Antonello Punturieri; and Barry S. Schmetter, NHLBI.
HAPIN Investigators: Vigneswari Aravindalochanan, Kalpana Balakrishnan, Dana B. Barr, Vanessa Burrowes, Devan Campbell, Eduardo Canuz, Adly Castañaza-Gonzalez, Howard Chang, William Checkley, Yunyun Chen, Marilú Chiang, Maggie L. Clark, Thomas F. Clasen, Rachel Craik, Mary E. Crocker, Victor Dávila-Román, Lisa de las Fuentes, Oscar De Léon, Anaité Diaz-Artiga, Ephrem Dusabimana, Lisa Elon, Juan Gabriel Espinoza, Irma S. Pineda Fuentes, Sarada S. Garg, Dina Goodman, Savannah Gupton, Meghan Hardison, Stella Hartinger, Steven A. Harvey, Mayari Hengstermann, Phabiola Herrera, Shakir Hossen, Penelope Howards, Lindsay Jaacks, Shirin Jabbarzadeh, Michael A. Johnson, Abigail Jones, Katherine Kearns, Miles A. Kirby, Jacob Kremer, Margaret Laws, Patricia M. Lenzen, Jiawen Liao, Amy Lovvorn, Fiona Majorin, Eric D. McCollum, John P. McCracken, Julia McPeek, Rachel M. Meyers, J. Jaime Miranda, Erick Mollinedo, Lawrence Moulton, Krishnendu Mukhopadhyay, Luke Naeher, Abidan Nambajimana, Florien Ndagijimana, Azhar Nizam, Jean de Dieu Ntivuguruzwa, Aris Papageorghiou, Jennifer L. Peel, Ricardo Piedrahita, Ajay Pillarisetti, Naveen Puttaswamy, Elisa Puzzolo, Ashlinn Quinn, Sarah Rajkumar, Usha Ramakrishnan, Davis Reardon, Ghislaine Rosa, Joshua Rosenthal, P. Barry Ryan, Zoe Sakas, Sankar Sambandam, Jeremy Sarnat, Suzanne M. Simkovich, Sheela Sinharoy, Kirk R. Smith, Kyle Steenland, Damien Swearing, Gurusamy Thangavel, Lisa M. Thompson, Ashley K. Toenjes, Lindsay J. Underhill, Jean Damascene Uwizeyimana, Viviane Valdes, Amit Verma, Lance Waller, Megan Warnock, Kendra Williams, Wenlu Ye, and Bonnie Young.
Footnotes
A complete list of HAPIN Investigators may be found before the beginning of the References.
Supported by the U.S. NIH (cooperative agreement 1UM1HL134590; multiple principal investigators: W.C., T.F.C., J.L.P.) in collaboration with the Bill and Melinda Gates Foundation (OPP1131279). Participating NIH organizations include the NHLBI, National Institute of Environmental Health Sciences, National Cancer Institute, National Institute of Child Health and Human Development, Fogarty International Center, and the NIH Common Fund. S.M.S. was supported by funding from the NHLBI (1F32HL143909-01, K12HL137942). L.J.U. was supported by the Fogarty International Center (University of North Carolina at Chapel Hill–Johns Hopkins University–Morehouse School of Medicine–Tulane University Fogarty Global Health Fellowship training grant D43TW009340; multiple principal investigators: P. Buekens, W.C., B. Chi, and K. Kondwani) funded by the U.S. NIH through the following Institutes and Centers: the Fogarty International Center, National Institute of Neurological Disorders and Stroke, National Institute of Mental Health, NHLBI, and National Institute of Environmental Health Sciences. D.G. was supported by the Harvard Cardiovascular Epidemiology Research Training Program (T32HL098048). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. NIH or Department of Health and Human Services.
Author Contributions: S.M.S., L.J.U., and W.C. validated the underlying data, verified the reproducibility of the analyses, designed the data analysis plan, and wrote the original manuscript draft. M.E.C., D.G., and W.C. conceptualized the survey and supervised data collection in the field. L.J.U. conducted the data analysis and geospatial analysis with input from W.C., and S.M.S. T.F.C., J.L.P., and W.C. supervised the study activities and were responsible for the acquisition of funding. L.M.T., J.P.M., A.D.-A., and A.C.-G. were responsible for administration and data collection in Guatemala. S.S.G., K.B., and G.T. were responsible for administration and data collection in India. M.E.C., D.G., S.M.S., L.J.U., and W.C. were responsible for administration and data collection in Peru. M.A.K. and G.R. were responsible for administration and data collection in Rwanda. E.D.M. and W.C. supervised child pneumonia–related activities during the trial, and E.D.M. provided scientific input to data analysis and interpretation. All co-authors reviewed the manuscript and contributed to reviews and drafting.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202104-1013OC on October 18, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
Contributor Information
the HAPIN Investigators:
Vigneswari Aravindalochanan, Dana B. Barr, Vanessa Burrowes, Devan Campbell, Eduardo Canuz, Howard Chang, Yunyun Chen, Marilú Chiang, Maggie L. Clark, Rachel Craik, Victor Dávila-Román, Lisa de las Fuentes, Oscar De Léon, Ephrem Dusabimana, Lisa Elon, Juan Gabriel Espinoza, Irma S. Pineda Fuentes, Savannah Gupton, Meghan Hardison, Stella Hartinger, Steven A. Harvey, Mayari Hengstermann, Phabiola Herrera, Shakir Hossen, Penelope Howards, Lindsay Jaacks, Shirin Jabbarzadeh, Michael A. Johnson, Abigail Jones, Katherine Kearns, Jacob Kremer, Margaret Laws, Patricia M. Lenzen, Jiawen Liao, Amy Lovvorn, Fiona Majorin, Julia McPeek, Rachel M. Meyers, J. Jaime Miranda, Erick Mollinedo, Lawrence Moulton, Krishnendu Mukhopadhyay, Luke Naeher, Abidan Nambajimana, Florien Ndagijimana, Azhar Nizam, Jean de Dieu Ntivuguruzwa, Aris Papageorghiou, Ricardo Piedrahita, Ajay Pillarisetti, Naveen Puttaswamy, Elisa Puzzolo, Ashlinn Quinn, Sarah Rajkumar, Usha Ramakrishnan, Davis Reardon, Joshua Rosenthal, P. Barry Ryan, Zoe Sakas, Sankar Sambandam, Jeremy Sarnat, Sheela Sinharoy, Kirk R. Smith, Kyle Steenland, Damien Swearing, Ashley K. Toenjes, Jean Damascene Uwizeyimana, Viviane Valdes, Amit Verma, Lance Waller, Megan Warnock, Kendra Williams, Wenlu Ye, and Bonnie Young
References
- 1. McAllister DA, Liu L, Shi T, Chu Y, Reed C, Burrows J, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health . 2019;7:e47–e57. doi: 10.1016/S2214-109X(18)30408-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Williams DJ, Zhu Y, Grijalva CG, Self WH, Harrell FE, Jr, Reed C, et al. Predicting severe pneumonia outcomes in children. Pediatrics . 2016;138:20161019. doi: 10.1542/peds.2016-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Koh JWJC, Wong JJ, Sultana R, Wong PPC, Mok YH, Lee JH. Risk factors for mortality in children with pneumonia admitted to the pediatric intensive care unit. Pediatr Pulmonol . 2017;52:1076–1084. doi: 10.1002/ppul.23702. [DOI] [PubMed] [Google Scholar]
- 4. Zhu YF, Xu F, Lu XL, Wang Y, Chen JL, Chao JX, et al. Chinese Collaborative Study Group for Pediatric Hypoxemic Respiratory Failure Mortality and morbidity of acute hypoxemic respiratory failure and acute respiratory distress syndrome in infants and young children. Chin Med J (Engl) . 2012;125:2265–2271. [PubMed] [Google Scholar]
- 5. Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T, Hypoxaemia in Developing Countries Study Group The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect Dis . 2009;9:219–227. doi: 10.1016/S1473-3099(09)70071-4. [DOI] [PubMed] [Google Scholar]
- 6. Duke T, Wandi F, Jonathan M, Matai S, Kaupa M, Saavu M, et al. Improved oxygen systems for childhood pneumonia: a multihospital effectiveness study in Papua New Guinea. Lancet . 2008;372:1328–1333. doi: 10.1016/S0140-6736(08)61164-2. [DOI] [PubMed] [Google Scholar]
- 7. Theodoratou E, Al-Jilaihawi S, Woodward F, Ferguson J, Jhass A, Balliet M, et al. The effect of case management on childhood pneumonia mortality in developing countries. Int J Epidemiol . 2010;39:i155–i171. doi: 10.1093/ije/dyq032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ouma PO, Maina J, Thuranira PN, Macharia PM, Alegana VA, English M, et al. Access to emergency hospital care provided by the public sector in Sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health . 2018;6:e342–e350. doi: 10.1016/S2214-109X(17)30488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sivanandan S, Agarwal R, Sethi A. Respiratory distress in term neonates in low-resource settings. Semin Fetal Neonatal Med . 2017;22:260–266. doi: 10.1016/j.siny.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 10. Graham H, Tosif S, Gray A, Qazi S, Campbell H, Peel D, et al. Providing oxygen to children in hospitals: a realist review. Bull World Health Organ . 2017;95:288–302. doi: 10.2471/BLT.16.186676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Floyd J, Wu L, Hay Burgess D, Izadnegahdar R, Mukanga D, Ghani AC. Evaluating the impact of pulse oximetry on childhood pneumonia mortality in resource-poor settings. Nature . 2015;528:S53–S59. doi: 10.1038/nature16043. [DOI] [PubMed] [Google Scholar]
- 12. Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci . 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 13. McCollum ED, Smith AG, Eckerle M, Mvalo T, O’Brien KL, Baqui AH. CPAP treatment for children with pneumonia in low-resource settings. Lancet Respir Med . 2017;5:924–925. doi: 10.1016/S2213-2600(17)30347-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Inglis R, Ayebale E, Schultz MJ. Optimizing respiratory management in resource-limited settings. Curr Opin Crit Care . 2019;25:45–53. doi: 10.1097/MCC.0000000000000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gallagher KE, Knoll MD, Prosperi C, Baggett HC, Brooks WA, Feikin DR, et al. The predictive performance of a pneumonia severity score in human immunodeficiency virus-negative children presenting to hospital in 7 low- and middle-income countries. Clin Infect Dis . 2020;70:1050–1057. doi: 10.1093/cid/ciz350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lazzerini M, Sonego M, Pellegrin MC. Hypoxaemia as a mortality risk factor in acute lower respiratory infections in children in low and middle-income countries: systematic review and meta-analysis. PLoS One . 2015;10:e0136166. doi: 10.1371/journal.pone.0136166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang L, Mendoza-Sassi R, Santos JC, Lau J. Accuracy of symptoms and signs in predicting hypoxaemia among young children with acute respiratory infection: a meta-analysis. Int J Tuberc Lung Dis . 2011;15:317–325. [PubMed] [Google Scholar]
- 18. Kironji AG, Hodkinson P, de Ramirez SS, Anest T, Wallis L, Razzak J, et al. Identifying barriers for out of hospital emergency care in low and low-middle income countries: a systematic review. BMC Health Serv Res . 2018;18:291. doi: 10.1186/s12913-018-3091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet . 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 20. Gondwe MJ, Henrion MYR, O’Byrne T, Masesa C, Lufesi N, Dube Q, et al. Clinical diagnosis in paediatric patients at urban primary health care facilities in southern Malawi: a longitudinal observational study. BMC Health Serv Res . 2021;21:150. doi: 10.1186/s12913-021-06151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ . 2006;84:314–319. doi: 10.2471/blt.04.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kievlan DR, Martin-Gill C, Kahn JM, Callaway CW, Yealy DM, Angus DC, et al. External validation of a prehospital risk score for critical illness. Crit Care . 2016;20:255. doi: 10.1186/s13054-016-1408-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cydulka RK, Shade B, Emerman CL, Gershman H, Kubincanek J.Prehospital pulse oximetry: useful or misused? Ann Emerg Med 199221675–679.. [Published erratum appears in Ann Emerg Med 21:1162.] [DOI] [PubMed] [Google Scholar]
- 24. Suryanto PV, Plummer V, Boyle M. EMS systems in lower-middle income countries: a literature review. Prehosp Disaster Med . 2017;32:64–70. doi: 10.1017/S1049023X1600114X. [DOI] [PubMed] [Google Scholar]
- 25. Chowdhury AI, Haider R, Abdullah AYM, Christou A, Ali NA, Rahman AE, et al. Using geospatial techniques to develop an emergency referral transport system for suspected sepsis patients in Bangladesh. PLoS One . 2018;13:e0191054. doi: 10.1371/journal.pone.0191054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Clasen T, Checkley W, Peel JL, Balakrishnan K, McCracken JP, Rosa G, et al. HAPIN Investigators Design and rationale of the HAPIN study: a multicountry randomized controlled trial to assess the effect of liquefied petroleum gas stove and continuous fuel distribution. Environ Health Perspect . 2020;128:47008. doi: 10.1289/EHP6407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Simkovich SM, Underhill LJ, Kirby MA, Goodman D, Crocker ME, Hossen S, et al. Design and conduct of facility-based surveillance for severe childhood pneumonia in the Household Air Pollution Intervention Network (HAPIN) trial. ERJ Open Res . 2020;6:00308-2019. doi: 10.1183/23120541.00308-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Crocker ME, Hossen S, Goodman D, Simkovich SM, Kirby M, Thompson LM, et al. HAPIN Investigators Effects of high altitude on respiratory rate and oxygen saturation reference values in healthy infants and children younger than 2 years in four countries: a cross-sectional study. Lancet Glob Health . 2020;8:e362–e373. doi: 10.1016/S2214-109X(19)30543-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.GDP (current US$): India. Washington, DC: The World Bank; 2020. [updated 2021; accessed 2020 Aug 21]. Available from: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD?locations=IN [Google Scholar]
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG.Research Electronic Data Capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support J Biomed Inform 200942377–381.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium The REDCap Consortium: building an international community of software platform partners. J Biomed Inform . 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization. Integrated management of childhood illness: chart booklet. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 33.OpenStreetMap Data Extracts. Karlsruhe, Germany: Geofabrik; 2018. [updated 2021; accessed 2019 Jul 10]. Available from: https://download.geofabrik.de/. [Google Scholar]
- 34.General information. Kigali, Rwanda: Rwanda Directorate General of Immigration and Emigration; 2020. [accessed 2020 Oct 1]. Available from: https://www.migration.gov.rw/useful-links/information-for-migrants/general/ [Google Scholar]
- 35.Congreso de la Republica de Guatemala. Ley de tránsito y su reglamento con sus reformas: decreto 132-96 Guatemala City: Departamento de Tránsito de la Dirección General de la Policía Nacional Civil, Gobierno de Guatemala; 2015 [accessed 2020 Oct 1]. Available from: https://transito.gob.gt/wp-content/uploads/2015/06/Ley-y-Reglamento-Transito.pdf [Google Scholar]
- 36.S.O. 1522(E) regarding Revised Speed Limits. New Delhi, India: Ministry of Road Transport and Highways, Government of India; 2018. [accessed 2020 Oct 1]. Available from: https://morth.nic.in/sites/default/files/notifications_document/Draft_Notification_no_S_O_1522E_dated_6_4_2018_regarding_Revised_Speed_Limits_0.pdf. [Google Scholar]
- 37.Texto único ordenado del Reglamento Nacional de Tránsito: código de tránsito. Decreto supremo nº 016-2009-MTC. Lima, Peru: Superintendencia de Transporte Terrestre de Personas, Carga, y Mercancias, Republica del Peru; 2014. [accessed 2020 Oct 1]. Available from: http://www.sutran.gob.pe/wp-content/uploads/2015/08/D_-NRO_016-2009-MTC_AL_05.05.14.pdf. [Google Scholar]
- 38.WorldPop open population repository. Southampton, United Kingdom: University of Southampton; 2018. [accessed 2020 Sep 10]. Available from: https://www.worldpop.org/. [Google Scholar]
- 39.Stevens FR, Gaughan AE, Linard C, Tatem AJ.Disaggregating census data for population mapping using random forests with remotely-sensed and ancillary data PLoS One 201510e0107042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Make OD cost matrix layer (Network Analyst) Middleton, MA: ESRI; 2012 [accessed 2021 Jul 10]. Available from: https://pro.arcgis.com/en/pro-app/latest/tool-reference/network-analyst/make-od-cost-matrix-layer.htm [Google Scholar]
- 41.R Core Team. R: a language and environment for statistical computing Vienna, Austria: R Foundation for Statistical Computing; [accessed 2021 Jul 10]. Available from: https://www.r-project.org. [Google Scholar]
- 42.Organisation for Economic Co-operation and Development. Paris, France: OECD Publishers; 2019. Health expenditure in relation to GDP. In: Health at a glance 2019: OECD indicators. [DOI] [Google Scholar]
- 43.Word Health Organization. Primary Health Care Systems (PRIMASYS): case study from Rwanda. Abridged version Geneva, Switzerland: World Health Organization; 2017. [accessed 2021 Aug 10]. Available from: https://www.who.int/alliance-hpsr/projects/AHPSR-PRIMASYS-Rwanda-Abridged.pdf?ua=1 [Google Scholar]
- 44. Logie DE, Rowson M, Ndagije F. Innovations in Rwanda’s health system: looking to the future. Lancet . 2008;372:256–261. doi: 10.1016/S0140-6736(08)60962-9. [DOI] [PubMed] [Google Scholar]
- 45. Portnoy A, Ozawa S, Grewal S, Norman BA, Rajgopal J, Gorham KM, et al. Costs of vaccine programs across 94 low- and middle-income countries. Vaccine . 2015;33:A99–A108. doi: 10.1016/j.vaccine.2014.12.037. [DOI] [PubMed] [Google Scholar]
- 46. Kristensen DD, Bartholomew K, Villadiego S, Lorenson K. What vaccine product attributes do immunization program stakeholders value? Results from interviews in six low- and middle-income countries. Vaccine . 2016;34:6236–6242. doi: 10.1016/j.vaccine.2016.10.057. [DOI] [PubMed] [Google Scholar]
- 47. Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines. Results of a survey conducted by Imprint: the Immunising Pregnant Women and Infants Network. Vaccines (Basel) . 2020;8:556. doi: 10.3390/vaccines8030556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. Master facility list resource package: guidance for countries wanting to strengthen their master facility list. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 49. Ortiz JR, Jacob ST, West TE. Clinical care for severe influenza and other severe illness in resource-limited settings: the need for evidence and guidelines. Influenza Other Respir Viruses . 2013;7:87–92. doi: 10.1111/irv.12086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dat VQ, Long NT, Giang KB, Diep PB, Giang TH, Diaz JV. Healthcare infrastructure capacity to respond to severe acute respiratory infection (SARI) and sepsis in Vietnam: a low-middle income country. J Crit Care . 2017;42:109–115. doi: 10.1016/j.jcrc.2017.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Spiegel DA, Abdullah F, Price RR, Gosselin RA, Bickler SW. World Health Organization Global Initiative for Emergency and Essential Surgical Care: 2011 and beyond. World J Surg . 2013;37:1462–1469. doi: 10.1007/s00268-012-1831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van der Walt A, South A., Exploring open African health facility data Geneva, Switzerland: Zenodo; 2020. [accessed 2021 Jul 10]. Available from: 10.5281/zenodo.3871224 [DOI] [Google Scholar]
- 53. Mpango J, Nabukenya J. A qualitative study to examine approaches used to manage data about health facilities and their challenges: a case of Uganda. AMIA Annu Symp Proc . 2020;2019:1157–1166. [PMC free article] [PubMed] [Google Scholar]
- 54. Otiangala D, Agai NO, Olayo B, Adudans S, Ng CH, Calderon R, et al. Oxygen insecurity and mortality in resource-constrained healthcare facilities in rural Kenya. Pediatr Pulmonol . 2020;55:1043–1049. doi: 10.1002/ppul.24679. [DOI] [PubMed] [Google Scholar]
- 55. Graham HR, Bakare AA, Ayede AI, Gray AZ, McPake B, Peel D, et al. Oxygen systems to improve clinical care and outcomes for children and neonates: a stepped-wedge cluster-randomised trial in Nigeria. PLoS Med . 2019;16:e1002951. doi: 10.1371/journal.pmed.1002951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nielsen K, Mock C, Joshipura M, Rubiano AM, Zakariah A, Rivara F. Assessment of the status of prehospital care in 13 low- and middle-income countries. Prehosp Emerg Care . 2012;16:381–389. doi: 10.3109/10903127.2012.664245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bakare AA, Graham H, Ayede AI, Peel D, Olatinwo O, Oyewole OB, et al. Providing oxygen to children and newborns: a multi-faceted technical and clinical assessment of oxygen access and oxygen use in secondary-level hospitals in southwest Nigeria. Int Health . 2020;12:60–68. doi: 10.1093/inthealth/ihz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gopinathan U, Lewin S, Glenton C. Implementing large-scale programmes to optimise the health workforce in low- and middle-income settings: a multicountry case study synthesis. Trop Med Int Health . 2014;19:1437–1456. doi: 10.1111/tmi.12381. [DOI] [PubMed] [Google Scholar]
- 59. McCollum ED, Mvalo T, Eckerle M, Smith AG, Kondowe D, Makonokaya D, et al. Bubble continuous positive airway pressure for children with high-risk conditions and severe pneumonia in Malawi: an open label, randomised, controlled trial. Lancet Respir Med . 2019;7:964–974. doi: 10.1016/S2213-2600(19)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]