Version Changes
Revised. Amendments from Version 2
We have removed unnecessary information to shorten the introduction to hemophilia and added additional information regarding the importance, burden, and theoretical importance of extended half-life rFVIII in the introduction section. We have revised the numbering of the references to the correct order. We have added more contents for the discussion and we have added Egger's test in the result section.
Abstract
Background: Patients with severe hemophilia often present with painful joint and soft tissue bleeding which may restrict them from their daily activities. The current standard of care still relies on a regular prophylactic factor VIII (FVIII), which has a high daily treatment burden. Recently, rurioctocog alfa pegol, a third-generation recombinant FVIII with a modification in its polyethylene glycol (PEG) component, has been developed. Several trials have studied this synthetic drug as bleeding prophylaxis in severe hemophilia A. This study aims to evaluate the efficacy, safety, and immunogenicity of rurioctocog alfa pegol for previously treated patients with severe hemophilia A.
Methods: This study was conducted in conformity with the PRISMA guidelines. Data were retrieved from PubMed, Scopus, Cochrane Library, Wiley Online Library, and CINAHL (via EBSCOhost). Study qualities were assessed using the Methodological Index for Non-Randomized Studies (MINORS) and Modified Jadad scales.
Results: Four studies involving 517 previously treated severe hemophilia A patients were included in this study. The pooled mean of total annualized bleeding rate (ABR) and hemostatic efficacy was 2.59 (95% CI = 2.04–3.14) and 92% (95% CI = 85%–97%), respectively. Only 30 (2.3%) non-serious and one (1.4%) serious adverse events were considered related to rurioctocog alfa pegol treatment. At the end of the studies, no development of FVIII inhibitory antibodies was observed. None of the developed binding antibodies to FVIII, PEG-FVIII, or PEG was correlated to the treatment efficacy and safety.
Conclusions: Despite the limited availability of direct comparison studies, our analyses indicate that rurioctocog alfa pegol could serve as a safe and effective alternative for bleeding prophylaxis in previously treated hemophilia A patients. Moreover, it appears to have low immunogenicity, which further increases the safety profile of the drug in such clinical conditions.
Keywords: drug safety, efficacy, hemophilia A, human and medicine, immunogenicity, prophylaxis, rurioctocog alfa pegol
Introduction
Hemophilia A is a rare, X-linked recessive, congenital bleeding disorder caused by mutations or defects in the factor VIII (FVIII)-producing genes. 1 Those mutations manifest as a congenitally absence or decrease of the FVIII, an important pro-coagulant cofactor in the bleeding hemostasis. 2 Hemophilia A may be further classified into mild, moderate, and severe based on the FVIII levels. 1 The severe form of hemophilia A is defined as having FVIII levels <1% of normal, while the mild and moderate forms have higher FVIII levels that are approximately 5–50% and 1–5%, respectively. 3 Patients with severe hemophilia often present with internal bleeding, especially in the joints and soft tissues. Joint and soft tissue bleeding, along with painful feelings, may restrict patients from their daily activities due to the restriction on their range of motions. 3 , 4 If this bleeding continues without being treated adequately, hemophilic patients could suffer from more advanced complications, including hemophilic arthropathy. This is important since hemophilic arthropathy could negatively affect their quality of life due to the severe joint immobility. 3
The current management of hemophilia A relies on two options: (1) episodic or on-demand FVIII replacement if the patients present with any bleedings to prevent further bleeding or (2) prophylactic FVIII treatment to maintain the FVIII levels and prevent any future bleedings. 5 However, the first option was no longer recommended as primary long-term management due to no alteration found in its natural disease course. 6 To date, the standard of care for hemophilia A, especially the severe form, still relies on a regular prophylactic intravenous FVIII replacement therapy. 3 The standard prophylactic regimens have shown a positive effect in reducing the future joint disease in hemophilia A. However, their half-lives are considered short, approximately 8–12 h, which will eventually increase the administration frequency. 4 Additionally, more than 30% of patients with hemophilia A may develop ‘inhibitors’ or refer to as neutralizing anti-drug antibodies to the standard prophylactic treatment which has high immunogenicity in inducing its formation. 3 Thus, extended half-life and safer prophylactic agents may be beneficial in reducing the daily treatment burden, and at the same time, those agents could maintain better clinical presentations and improve the treatment efficacy. 7
Recently, rurioctocog alfa pegol (i.e., BAX 855), a third-generation recombinant FVIII (rFVIII) with a modification in its polyethylene glycol (PEG) component, has been developed. The addition of PEG in rFVIII or referred to as PEGylation is addressed to decrease its plasma clearance and to alter its biodistribution in the human body. 8 This modification also prolongs the half-life of rFVIII by 1.4–1.5 folds the original rFVIII, thereby reducing the administration frequency and maintaining better bleeding hemostasis of the hemophilic patients. 8 , 9 The administration of rurioctocog alfa pegol increases the prevalence of zero-bleeding events in hemophilia A patients due to its lower future coagulation factor consumption after injection compared to the standard regimens. Hence, the use of this drug could offer potential advantages and might improve treatment adherence. 8 Yet, to the best of our knowledge, there are no pooled studies assessing the efficacy, safety, and immunogenicity of rurioctocog alfa pegol as a prophylactic treatment. Therefore, here, we aim to evaluate the efficacy, safety, and immunogenicity of rurioctocog alfa pegol, a newly-developed prophylactic agent, in previously treated patients with severe hemophilia A.
Methods
Data search strategy
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 guidelines. 10 A computerized and systematic data searching of relevant studies was conducted in PubMed, Scopus, Cochrane Library, Wiley Online Library, and CINAHL (via EBSCOhost) from inception to 16 February 2021. Keywords were constructed based on Medical Subject Headings (MeSH) terms and other additional terms listed as follows: (“rurioctocog alfa pegol” OR “bax 855” OR “TAK-660” OR “SHP660” OR “adynovate” OR “adynovi”) AND (“hemophilia A” OR “haemophilia A” OR “factor VIII deficiency” OR “factor 8 deficiency” OR “classic hemophilia” OR “classic haemophilia”). Two reviewers searched the literatures independently. Any disagreements were resolved in a consensus involving a third investigator.
Eligibility criteria
Studies were included if the following criteria were met: (1) study design of clinical trial; (2) study population consists of previously treated severe hemophilia A patients with or without healthy subjects as control; (3) rurioctocog alfa pegol as a prophylactic treatment intervention; and (4) the reported outcomes related to the efficacy, safety, and immunogenicity of rurioctocog alfa pegol (annualized bleeding rate [ABR], patients with zero-bleeding during treatment, hemostatic efficacy, adverse events [AEs], number of deaths, development of FVIII ‘inhibitors’, and/or binding antibodies). The exclusion criteria were as follows: (1) irrelevant titles and abstracts; (2) review articles, systematic reviews, meta-analyses, case reports, case series, letter to editors, and conference abstracts; (3) non-English studies; or (4) irretrievable full-text articles.
Data extraction and quality assessment
The following relevant data were extracted from the included studies: (1) author and year of publication; (2) study location; (3) clinical trial number; (4) study design; (5) total patients included for prophylactic treatment, gender, and age; (6) definition of target joint (TJ); (7) regimen type; (8) patient characteristics (with or without target joints); (9) total patients in per-protocol analysis set (PPAS) or analyzed for ABR based on regimen type and target joints; (10) outcomes related to efficacy (types of ABR, number of patients with zero-bleeding during treatment, and/or hemostatic efficacy); (11) outcomes related to safety (number of patients with AEs, total AEs, AEs considered related to treatment, and/or number of deaths); and/or (12) outcomes related to immunogenicity (development of FVIII ‘inhibitors’ and/or binding antibodies). The quality assessment of the included studies was performed using the Methodological Index for Non-Randomized Studies (MINORS) scale 11 for non-randomized studies and Modified Jadad scale 12 for randomized studies. Studies with a MINORS score of ≥ 12 or a Jadad score of ≥ 4 were considered high-quality studies, and the rest were considered low-quality studies. The data extraction and quality assessment were conducted by three reviewers collaboratively through a group discussion and a final decision was taken based on the agreement of all reviewers.
Statistical analysis
Statistical analyses were performed using the latest version of OpenMeta [Analyst] from the Brown University Evidence-Based Practice Center, 13 MetaXL ver. 5.3 (EpiGear International, Sunrise Beach, Australia), and STATA ver. 16.0 (Stata Corporation, College Station, TX, USA). Single-arm meta-analysis of mean and standard deviation values was performed for four different efficacy outcomes: (1) total ABR; (2) spontaneous ABR; (3) injury ABR; and (4) joint ABR. Whilst, a meta-analysis of proportions was performed for two different efficacy outcomes: (1) zero-bleeding prevalence and (2) hemostatic efficacy with the rating of excellent or good. Subgroup analysis based on target joints (TJs) for total ABR was also performed. For the purpose of meta-analyses, 95% confidence intervals were transformed into standard deviation values based on a method suggested by the Cochrane Handbook Chapter 6. 14
Heterogeneity between studies was assessed with a chi-square test (Cochran’s Q statistic) and quantified with the Higgins’ I 2 statistics. P-value < 0.1 from the chi-square test indicated statistical heterogeneity, whereas the level of heterogeneity was determined using I 2 values. I 2 < 25% was considered a low heterogeneity, 25–75% a moderate heterogeneity, and I 2 > 75% a high heterogeneity. If the I 2 value was greater than 50%, a random-effects model was used for the meta-analysis. Otherwise, a fixed-effects model was applied. Publication bias was explored qualitatively using a funnel plot if the number of studies was adequate (n ≥ 10). We additionally performed the Egger’s test to quantitatively search for the potential publication bias. P-value < 0.05 indicated statistical significance in all analyses, unless otherwise stated.
Results
Overview of literature search
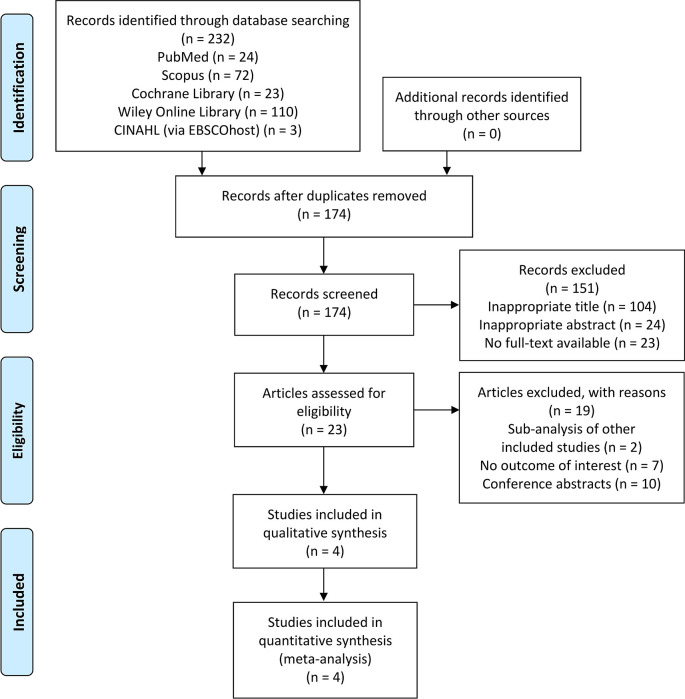
The initial search of this study yielded a total of 232 articles identified from PubMed, Scopus, Cochrane Library, Wiley Online Library, and CINAHL (via EBSCOhost). Of those, 174 studies were screened by titles and abstracts after duplicates removal. Twenty-three were fully reviewed based on the eligibility criteria and 19 of these were excluded due to: (1) studies with a sub-analysis of other included studies (n = 2); (2) not reporting the outcome of interest (n = 7); or (3) conference abstracts (n = 10). Finally, four clinical trials 5 , 7 , 9 , 15 were included in the qualitative and quantitative synthesis. The overall study selection process is illustrated in Figure 1.
Figure 1. PRISMA flow diagram of the study selection process.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of the included studies
Table 1 provides a summary of the studies included in the systematic review. The four uncontrolled clinical trials 5 , 7 , 9 , 15 included a total of 517 previously treated severe hemophilia A patients for prophylactic treatment, with the overall mean ± SD age of 23.9 ± 14.8. Only two studies by Mullins et al. 9 and Chowdary et al. 7 included a female patient. The trials were published between 2015 and 2021 and were all multicentered with a range number of 11 to 23 countries. Three 7 , 9 , 15 out of four studies were in phase 3 clinical trial, whereas the study by Konkle et al. 5 was in a phase 2/3 trial. All studies were non-randomized with the exception of Klamroth et al. 15 Definition of target joint was the same across all studies, except for Klamroth et al. 15 There were two different prophylactic regiment types used between studies: twice-weekly and pharmacokinetic (PK)-guided. The “excellent” hemostatic efficacy rating was defined as a complete resolution of pain and sign of bleedings after a single infusion without the requirement of additional infusion to control the bleeding, while the “good” rating was defined when there was a definite improvement in pain and/or signs of bleeding after a single infusion with a possible requirement of more than one infusion to complete the resolution. The “fair” rating was defined as a slight improvement in pain and/or signs of bleeding after a single infusion with definite requirement of more than one infusion to complete the resolution. If there was no improvement or the condition worsen, the hemostatic efficacy was rated “none”. 5
Table 1.
Characteristics of the included studies.
| Author, year | Study location | Clinical trial number | Study design | Total patients included for prophylactic treatment (F) | Age * | Definition of target joint |
|---|---|---|---|---|---|---|
| Mullins et al., 2017 9 | Multicenter (11 countries) | NCT02210091 | Phase 3, open-label, non-randomized, uncontrolled clinical trial | 66 (1) | 6.0 ± 2.7 | A joint (ankles, knees, hips or elbows) with ≥ 3 spontaneous bleeding episodes in any consecutive 6-month period |
| Chowdary et al., 2020 7 | Multicenter (23 countries) | NCT01945593 (CONTINUATION study) | Phase 3b, open-label, non-randomized, uncontrolled clinical trial | 216 (1) | 22.8 ± 15.7 | A joint with ≥ 3 spontaneous bleeding episodes in any consecutive 6-month period |
| Konkle et al., 2015 5 | Multicenter (20 countries) | NCT01736475 (PROLONG-ATE study) | Phase 2/3, open-label, non-randomized, uncontrolled clinical trial | 120 (0) | 28.7 ± 9.0 | A joint with ≥ 3 spontaneous bleeding episodes in any consecutive 6-month period |
| Klamroth et al., 2020 15 | Multicenter (22 countries) | NCT02585960 (PROPEL study) | Phase 3, open-label, randomized, uncontrolled clinical trial | 57 (0) | 31.0 ± 13.6 | A joint with ≥ 4 spontaneous bleeding episodes in any consecutive 6-month period |
| 58 (0) | 31.6 ± 12.9 |
| Author, year | Regimen type | Patient characteristics | Total patients in PPAS or analyzed for ABR based on regimen Type & TJ | Total ABR | Spontaneous ABR | Injury ABR | Joint ABR | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | SD | Mean (95% CI) | SD | Mean (95% CI) | SD | Mean (95% CI) | SD | ||||
| Mullins et al., 2017 9 | Twice-weekly prophylaxis | With TJs | 14 | 3.54 (1.89–6.64) | 4.11 | 1.20 (0.92–1.56) | 2.22 | 2.09 (1.49–2.93) | 2.93 | 1.10 (0.64–1.91) | 2.58 |
| Without TJs | 52 | 2.92 (2.02–4.24) | 3.99 | ||||||||
| Chowdary et al., 2020 7 | Twice-weekly prophylaxis | With and without TJs | 186 | 2.23 (1.85–2.69) | 3.06 | 1.20 (0.92–1.56) | 2.33 | N/A | N/A | 1.23 (0.96–1.58) | 2.26 |
| PK-guided prophylaxis | With and without TJs | 25 | 2.64 (1.70–4.08) | 1.87 | 0.96 (0.54–1.71) | 0.92 | 1.40 (0.91–2.17) | 0.99 | |||
| Konkle et al., 2015 5 | Twice-weekly prophylaxis | With TJs | 32 | 3 | 4.9 | 2.2 | 3.7 | N/A | N/A | 2.2 | 3.2 |
| Without TJs | 69 | 3.7 | 4.4 | 1.9 | 2.9 | 1.2 | 2.4 | ||||
| Klamroth et al., 2020 15 | PK-guided prophylaxis (1–3%) | With and without TJs | 52 | 2.8 | 3 | 1.7 | 2.5 | 1.1 | 1.9 | 1.8 | 2.2 |
| PK-guided prophylaxis (8–12%) | With and without TJs | 43 | 1.2 | 2.4 | 0.6 | 1.5 | 0.7 | 1.7 | 0.8 | 2.3 | |
| Author, year | Patients with zero-bleeding during treatment | Hemostatic efficacy | Adverse events | Number of deaths | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rating | Events | Total number of bleedings | Number of patients with any AEs (non-SAEs and SAEs) | Total non-SAEs | Non-SAEs considered related to treatment | Number of patients with SAEs | Total SAEs | SAEs considered related to treatment | |||
| Mullins et al., 2017 9 | 25 | Excellent
Good Fair None Not reported |
34
29 4 0 3 |
70 | 43 | 152 | 0 | 3 | 4 | 0 | 0 |
| Chowdary et al., 2020 7 | 51 |
Excellent
Good Fair None Not reported |
438
368 48 4 52 |
910 | 174 | 786 | 20 | 33 | 52 | 0 | 1 (considered unrelated to treatment) |
| Konkle et al., 2015 5 | 40 | Excellent/Good
Fair/ None/Not reported |
498
20 |
518 | 73 | 166 | 7 | 5 | 5 | 0 | 0 |
| Klamroth et al., 2020 15 | 24 | N/A | N/A | N/A | 34 | 97 | 2 | 3 | 4 | 0 | 0 |
| 36 | 36 | 98 | 1 | 4 | 5 | 1 | 0 | ||||
| Author, year | Development of FVIII inhibitory antibodies | Development of binding antibodies to FVIII / PEG-FVIII/PEG during study |
|---|---|---|
| Mullins et al., 2017 9 | No subjects developed inhibitory antibodies |
|
| Chowdary et al., 2020 7 | No subjects developed inhibitory antibodies |
|
| Konkle et al., 2015 5 | No subjects developed inhibitory antibodies |
|
| Klamroth et al., 2020 15 | No subjects developed inhibitory antibodies |
|
| 1 subject (resolved at the study end) |
|
Data are presented in mean ± SD.
ABR, annualized bleeding rate; CI, confidence interval; F, female; FVIII, factor VIII; N/A, not available or not applicable; Non-SAEs, non-serious adverse events; PEG, pegylated; PK, pharmacokinetic; PPAS, per-protocol analysis set; SAEs, serious adverse events; SD, standard deviation; TJ(s), target joint(s).
Efficacy outcomes
Total ABR
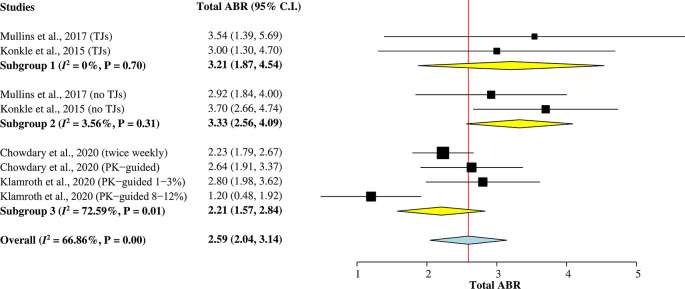
A total of 473 hemophilia A patients from the four studies 5 , 7 , 9 , 15 were included in this subgroup single-arm meta-analysis ( Figure 2) to calculate the pooled mean of total ABR after rurioctocog alfa pegol treatment. A random-effects model was used for the analysis since heterogeneity among studies was greater than 50% ( I 2 = 67%). The overall pooled mean of total ABR was 2.59 (95% CI = 2.04–3.14).
Figure 2. Forest plot of subgroup single-arm meta-analysis for mean of total ABR.
ABR, annualized bleeding rate; CI, confidence interval; PK, pharmacokinetic; TJ, target joint.
Two studies 5 , 9 reporting mean of total ABR individually for patients with target joints (TJs) and without target joints were included in Subgroup 1 and Subgroup 2, respectively. The pooled mean of total ABR in patients with TJs was 3.21 (95% CI = 1.87–4.54), whilst the pooled mean of total ABR in patients without TJs was 3.33 (95% CI = 2.56–4.09). Subgroup 3 included other two studies 7 , 15 with a combined mean of total ABR for patients with and without TJs. The pooled value was 2.21 (95% CI = 1.57–2.84).
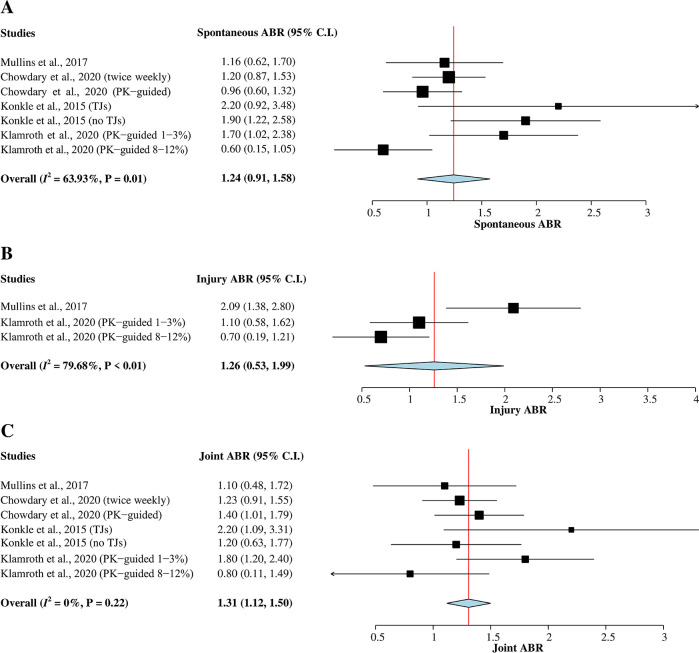
Spontaneous ABR
The four studies 5 , 7 , 9 , 15 with a total of 473 hemophilia A patients were included in this meta-analysis ( Figure 3A). Heterogeneity between studies was greater than 50% ( I 2 = 64%); therefore, a random-effects model was used for the analysis. The result of the pooled mean of spontaneous ABR was 1.24 (95% CI = 0.91–1.58).
Figure 3. Forest plots of single-arm meta-analysis for (A) mean of spontaneous ABR, (B) mean of injury ABR, and (C) mean of joint ABR.
ABR, annualized bleeding rate; CI, confidence interval; PK, pharmacokinetic; TJ, target joint.
Injury ABR
A total of 161 hemophilia A patients from two studies 9 , 15 that reported mean of injury ABR were included in this meta-analysis ( Figure 3B). A random-effects model was used for the analysis since heterogeneity was greater than 50% ( I 2 = 80%). The pooled mean of injury ABR was 1.26 (95% CI = 0.53–1.99).
Joint ABR
A total of 473 hemophilia A patients from the four studies 5 , 7 , 9 , 15 were evaluated in this subgroup analysis of joint ABR ( Figure 3C). The heterogeneity across studies was low ( I 2 = 0%); therefore, a fixed-effects model was used for the analysis. The pooled mean of joint ABR was 1.31 (95% CI = 1.12–1.50).
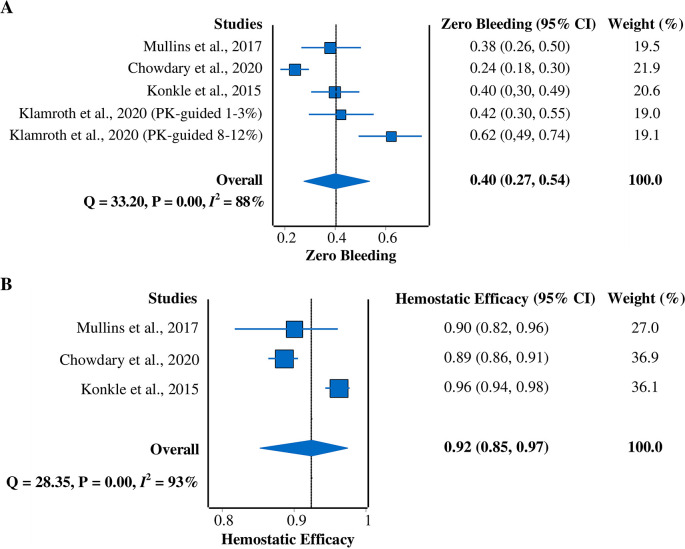
Zero-bleeding prevalence
All four studies 5 , 7 , 9 , 15 were included in this meta-analysis of zero-bleeding prevalence ( Figure 4A). A random-effects model was used due to the heterogeneity of the data ( I 2 = 88%). The pooled prevalence result was 40% (95% CI = 27%–54%).
Figure 4. Forest plots of meta-analysis of proportions for (A) zero-bleeding prevalence and (B) hemostatic efficacy (excellent or good rating).
CI, confidence interval; PK, pharmacokinetic.
Hemostatic efficacy
Three studies 5 , 7 , 9 that reported hemostatic efficacy with the rating of excellent or good were included in this meta-analysis ( Figure 4B). A random-effects model was used due to the heterogeneity across studies ( I 2 = 93%). The pooled hemostatic efficacy was 92% (95% CI = 85%–97%).
Safety outcomes
A total of 1,299 non-serious adverse events (non-SAEs) occurred during the four studies. 5 , 7 , 9 , 15 However, only 30 (2.3%) of them were considered related to rurioctocog alfa pegol treatment. Whilst, a total of 70 serious adverse events (SAEs) were observed in the four studies and only one (1.4%; a transient development of FVIII inhibitory antibodies) of them – as reported by Klamroth et al. 15 – were considered related to treatment. Among all studies, only one death case was reported by Chowdary et al. 7 and was not considered to be related to rurioctocog alfa pegol treatment.
Immunogenicity outcomes
Three studies 5 , 7 , 9 reported no development of FVIII inhibitory antibodies among all patients. Klamroth et al. 15 reported one patient with development of FVIII inhibitory antibodies and was resolved at the end of the study. Development of binding antibodies to either FVIII, PEG-FVIII, or PEG among patients was detected in 52 patients from the four studies. However, none of them was correlated to impaired rurioctocog alfa pegol treatment efficacy and AEs.
Publication bias and quality assessment
Publication bias assessment using funnel plot was not performed due to the low number of the included studies. The results of the Egger’s tests showed no potential publication bias for total ABR ( Z = 1.55; p = 0.12), joint ABR ( Z = 0.77; p = 0.44), and hemostatic efficacy ( Z = −0.4; p = 0.69). However, we found significant Egger’s test results for spontaneous ABR ( Z = 2.32; p = 0.02), injury ABR ( Z = 2.99; p = 0.003), and zero-bleeding prevalence ( Z = 2.59; p = 0.01). Details of the quality assessment using MINORS and Modified Jadad scale are provided in Table 2. All non-randomized studies 5 , 7 , 9 were considered high in quality, whereas the randomized study by Klamroth et al. 15 was considered low in quality.
Table 2. Summary of quality assessment using MINORS and Modified Jadad Scale.
| MINORS Scale | Modified Jadad Scale | ||||
|---|---|---|---|---|---|
| Items | Mullins et al., 2017 9 | Chowdary et al., 2020 7 | Konkle et al., 2015 5 | Items | Klamroth et al., 2020 15 |
| A clearly stated aim | 2 | 2 | 2 | Randomization | 1 |
| Inclusion of consecutive patients | 2 | 2 | 2 | ||
| Prospective collection of data | 2 | 2 | 2 | Concealment | 0 |
| Endpoints appropriate to the aim of the study | 2 | 2 | 2 | ||
| Unbiased assessment of the study endpoint | 0 | 0 | 0 | Blinding | 0 |
| Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | ||
| Loss to follow up less than 5% | 2 | 2 | 2 | Withdrawal or drop-out | 1 |
| Prospective calculation of the study size | 1 | 1 | 1 | ||
| Results | Results | ||||
| Total score | 13 | 13 | 13 | Total score | 2 |
| Study quality | High | High | High | Study quality | Low |
MINORS, Methodological Index for Non-Randomized Studies.
Discussion
This study was the first far-reaching, single-arm meta-analysis that evaluates the efficacy, safety, and immunogenicity of rurioctocog alfa pegol, a newly developed rFVIII product with a prolonged half-life, as a prophylactic treatment for previously treated patients with severe hemophilia A. Rurioctocog alfa pegol (BAX 855) is a pegylated full-length rFVIII product designed to reduce the frequency of prophylactic infusions while maintaining hemostatic efficacy in patients with hemophilia. 16 , 17 This study indicated the long-term safety and efficacy of the pharmacological agent, which were consistent with the study of rurioctocog alfa pegol for perioperative hemostasis in hemophilia A patients, 18 , 19 also with the previous parent studies. 20 – 22
The overall pooled mean of total ABR of rurioctocog alfa pegol is lower compared to the several conventional rFVIIIs ( Advate ®, Xyntha ®, Novoeight ®, REFACTO ®) with their total ABR ranged from 3.3 to 6.5. 23 The ABR of rurioctocog alfa was also lower compared to simoctocog alfa ( Nuwiq ®), a B-domain deleted rFVIII (2.59 vs. 2.91), administered every two days. 24 This could indicate that rurioctocog alfa pegol offers both the higher and long-term efficacy over conventional and other type of rFVIIIs. Compared to other extended half-life rFVIIIs from another study, we found a lower ABR for rurioctocog alfa pegol than efmoroctocog alfa ( Eloctate ®; 2.59 vs. 4.90). 25 Interestingly, a study by Reding et al. 26 showed a lower ABR (1.49) for another novel extended half-life rFVIII, damoctocog alfa pegol ( Jivi ®), than our study finding. This product is potential to be used as other alternative long-term treatments for hemophilia A, but it is still necessary to confirm its efficacy with more clinical trials.
The spontaneous- and injury-related bleeding are important evaluations for hemophilia, especially in prophylactic treatment use. 27 Without an appropriate prophylactic treatment, patients have a tendency to experience monthly spontaneous bleeding episodes (including spontaneous joint bleeds) and prolonged and excessive bleeding after minor trauma. 28 , 29 Our results showed that the ABRs of rurioctocog alfa pegol were similar for spontaneous- and injury-related bleeding. This indicates that rucioctocog alfa pegol can be used to prevent both of conditions. It is also important to evaluate the efficacy of hemophilia treatment for patients with target joints. Untreated bleeding creates a persistent inflammatory response that leads to irreversible changes in the joints, resulting in hemophilic arthropathy and permanent disability. 30 Any reduction in joint bleeds is considered an improvement in quality of life for hemophilia patients. 31 Decreased bleeding in joints thereby shows better joint health, activity, and satisfaction for the patients. 32 The pooled mean ABR for patients with target joints was similar to those without target joints, indicating that rurioctocog alfa pegol had an equal efficacy for both groups of patients. Moreover, all studies reported that rurioctocog alfa pegol had higher good and excellent hemostatic efficacy events. This data was comparable with results reported for other rFVIII preparations. 33 – 36 The efficacy of rurioctocog alfa pegol was also supported by the finding on the pooled zero-bleeding prevalence.
Our study also demonstrated the safety of rurioctocog alfa pegol in patients by assessing the non-SAEs and SAEs. Rurioctocog alfa pegol was proven acceptable and safe for perioperative hemostasis, with minor findings in both non-SAEs and SAEs. 18 Our data showed that most of the adverse reactions were mild, and the prevalence seems rarer than damoctocog alfa pegol (79%–95% patients with AEs). 26 , 37 Additionally, all rFVIIIs usage decreased the risk of blood-borne infections and restored longer life expectancies. 38 As extended half-life rFVIIIs, they can also improve adherence to prophylactic regimens and reduce the burden of treatment. 39 , 40 However, there are some concerns regarding the safety of PEG component, particularly when it is used for lifelong prophylaxis. Nevertheless, the PEG levels found in rurioctocogalfa pegol were minimal (less than 1 mg/dose) and evidence has showed no specific side effects to central nervous system, liver, or kidney. 41
The development of FVIII ‘inhibitors’ is a major issue in patients treated with blood coagulation factor products. The development of neutralizing alloantibodies against FVIII can reduce the treatment benefits. 42 , 43 Currently available studies revealed some predictors of ‘inhibitor’ development, but the predictive power remained low. 44 , 45 Several studies reported either transient or persistent ‘inhibitor’ development in patients treated with plasma-derived FVIII. 46 , 47 Interestingly, the Survey of Inhibitors in Plasma-Product Exposed Toddlers (SIPPET) study revealed lower incidence of ‘inhibitor’ development in previously untreated patients whom treated with plasma-derived FVIII products compared to rFVIII products. 48 This finding attracted a lot of debate among experts, but we yet have to take notice of it to further improve the quality of future rFVIII products. However, our findings showed no development of persistent FVIII inhibitory antibodies, and this was consistent with the US Food and Drug Administration's approval of rurioctocog alfa pegol for the treatment of hemophilia A patients. 49 There was some development of binding antibodies observed. However, this development did not interfere with rurioctocog alfa pegol treatment safety and efficacy until the end of the study. Although this finding may look favorable, all the patients included in our study were previously treated patients. The development of ‘inhibitors’ tends to be rarer in these patients than previously untreated patients. 50 Furthermore, all the included studies excluded patients with the history of and detectable FVIII ‘inhibitors’ at screening before recruitment. 5 , 7 , 9 , 15 Hence, we could assume that positive individual factors of ‘inhibitor’ development, such as underlying gene defects and family history, 43 , 51 might not be present in these patients, since they had been screened previously. Nevertheless, there is still no strong evidence of association between switching types of treatment with the development of ‘inhibitors’ in previously treated patients. Therefore, shifting to other types of treatment might be considered if it is more beneficial for the patients. 52
Overall, our study successfully demonstrated the pooled efficacy, safety, and immunogenicity of rurioctocog alfa pegol as a treatment for hemophilia A. These results can be used to plan an alternative treatment for hemophilia A patients. Nevertheless, high heterogeneity existed between the included studies. We used the random-effects model to minimize this issue. Substantial efforts were made to explore the possible source for heterogeneity, revealing that different dose regimens and prior prophylactic drugs for treatment could be responsible for the high heterogeneity. Regarding the zero-bleeding prevalence ( Figure 4A), a difference in the administered dose regimens was observed among studies. Different dose regimens were considered because pharmacokinetic profiles, targets of FVIII level, and age group varied among patients. The PK-guided dosing was applied to provide more individualized prophylaxis according to each patient’s PK profiles (e.g., plasma half-life), targets of FVIII level, and body weight. Age is also a determining factor since it influences the PK profiles. 6
Several other limitations exist in this meta-analysis. First, our study only included single-arm clinical trials. The highest possible quality cannot be ensured due to the lack of control arms. However, since hemophilia is a rare genetic disease, comparison with a control arm receiving prophylaxis with other conventional FVIII products was not recommended, as stated by the regulatory guide. 53 Second, diverse prior prophylactic strategies in the patients before switching to rurioctocog alfa pegol may affect the treatment outcomes. Third, publication was observed for several outcomes, and thus the results should be interpreted carefully. Finally, only a few published studies were evaluated in this meta-analysis since rurioctocog alfa pegol is a newly-developed drug. However, these limitations were partly compensated by the multicentered settings of the included studies.
Conclusions
Our study suggests that rurioctocog alfa pegol is effective, safe, and has low immunogenicity for previously treated patients with severe hemophilia A. Despite the lack of direct comparison studies, rurioctocog alfa pegol could serve as an alternative bleeding prophylaxis in hemophilia A. A network meta-analysis with a multi-arm approach on hemophilia A treatment is warranted to corroborate the current evidence.
Data availability
All data underlying the results are available as part of the article and no additional source data are required.
Reporting guidelines
Open Science Framework: PRISMA Checklist for “Efficacy, Safety, and Immunogenicity of Rurioctocog Alfa Pegol for Prophylactic Treatment in Previously Treated Patients with Severe Hemophilia A: A Systematic Review and Meta-Analysis of Clinical Trials”. https://doi.org/10.17605/OSF.IO/4EZAG. 54
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC0 1.0 Public domain dedication).
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 3; peer review: 2 approved]
References
- 1. Castaman G, Matino D: Hemophilia A and B: Molecular and clinical similarities and differences. Haematologica. 2019;104(9):1702–9. 10.3324/haematol.2019.221093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schep SJ, Boes M, Schutgens REG, et al. : An update on the ‘danger theory’ in inhibitor development in hemophilia A. Expert. Rev. Hematol. 2019;12(5):335–44. 10.1080/17474086.2019.1604213 [DOI] [PubMed] [Google Scholar]
- 3. Peters R, Harris T: Advances and innovations in haemophilia treatment. Nat. Rev. Drug Discov. 2018;17(7):493–508. 10.1038/nrd.2018.70 [DOI] [PubMed] [Google Scholar]
- 4. Peyvandi F, Garagiola I, Young G: The past and future of haemophilia: diagnosis, treatments, and its complications. Lancet. 2016;388(10040):187–97. 10.1016/S0140-6736(15)01123-X [DOI] [PubMed] [Google Scholar]
- 5. Konkle BA, Stasyshyn O, Chowdary P, et al. : Pegylated, full-length, recombinant factor VIII for prophylactic and on-demand treatment of severe hemophilia A. Blood. 2015;126(9):1078–85. 10.1182/blood-2015-03-630897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Srivastava A, Santagostino E, Dougall A, et al. : WFH Guidelines for the Management of Hemophilia, 3rd edition. Haemophilia. 2020;26(Suppl 6):1–158. 10.1111/hae.14046 [DOI] [PubMed] [Google Scholar]
- 7. Chowdary P, Mullins ES, Konkle BA, et al. : Long-term safety and efficacy results from the phase 3b, open-label, multicentre Continuation study of rurioctocog alfa pegol for prophylaxis in previously treated patients with severe haemophilia A. Haemophilia. 2020;26(4):e168–78. 10.1111/hae.14052 [DOI] [PubMed] [Google Scholar]
- 8. You CW, Baek HJ, Park SK, Park YS, et al. : Subgroup analysis of a phase 2/3 study of rurioctocog alfa pegol in patients with severe hemophilia A: Efficacy and safety in previously treated Korean patients. Blood Res. 2019;54(3):198–203. 10.5045/br.2019.54.3.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mullins ES, Stasyshyn O, Alvarez-Román MT, et al. : Extended half-life pegylated, full-length recombinant factor VIII for prophylaxis in children with severe haemophilia A. Haemophilia. 2017;23(2):238–46. 10.1111/hae.13119 [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, et al. : Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Slim K, Nini E, Forestier D, et al. : Methodological index for non-randomized studies (Minors): Development and validation of a new instrument. ANZ J. Surg. 2003;73(9):712–6. 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 12. Chen W, Jiang H, Zhou ZY, et al. : Is omega-3 fatty acids enriched nutrition support safe for critical Ill patients? A systematic review and meta-analysis. Nutrients. 2014;6(6):2148–64. 10.3390/nu6062148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wallace BC, Schmid CH, Lau J, et al. : Meta-Analyst: Software for meta-analysis of binary, continuous and diagnostic data. BMC Med. Res. Methodol. 2009;9(1):1–12. 10.1186/1471-2288-9-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins JP, Li T, Deeks JJ, editors. Chapter 6: Choosing effect measures and computing estimates of effect. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane;2021. Reference Source [Google Scholar]
- 15. Klamroth R, Windyga J, Radulescu V, et al. : Rurioctocog alfa pegol PK-guided prophylaxis in hemophilia A: results from the phase 3 PROPEL study. Blood. 2021;137(13):1818–27. 10.1182/blood.2020005673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mahlangu J, Young G, Hermans C, et al. : Defining extended half-life rFVIII—A critical review of the evidence. Haemophilia. 2018;24(3):348–58. 10.1111/hae.13438 [DOI] [PubMed] [Google Scholar]
- 17. Tiede A: Half-life extended factor VIII for the treatment of hemophilia A. J. Thromb. Haemost. 2015;13(S1):S176–9. 10.1111/jth.12929 [DOI] [PubMed] [Google Scholar]
- 18. Brand B, Gruppo R, Wynn TT, et al. : Efficacy and safety of pegylated full-length recombinant factor VIII with extended half-life for perioperative haemostasis in haemophilia A patients. Haemophilia. 2016;22(4):e251–8. 10.1111/hae.12963 [DOI] [PubMed] [Google Scholar]
- 19. Gruppo R, López-Fernández MF, Wynn TT, et al. : Perioperative haemostasis with full-length, PEGylated, recombinant factor VIII with extended half-life (rurioctocog alfa pegol) in patients with haemophilia A: Final results of a multicentre, single-arm phase III trial. Haemophilia. 2019;25(5):773–81. 10.1111/hae.13807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Auerswald G, Thompson AA, Recht M, et al. : Experience of advate rahf-pfm in previously untreated patients and minimally treated patients with haemophilia a. Thromb. Haemost. 2012;107(6):1072–82. 10.1160/TH11-09-0642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khair K, Mazzucconi MG, Parra R, et al. : Pattern of bleeding in a large prospective cohort of haemophilia A patients: A three-year follow-up of the AHEAD (Advate in HaEmophilia A outcome Database) study. Haemophilia. 2018;24(1):85–96. 10.1111/hae.13361 [DOI] [PubMed] [Google Scholar]
- 22. Shapiro AD, Schoenig-Diesing C, Silvati-Fidell L, et al. : Integrated analysis of safety data from 12 clinical interventional studies of plasma- and albumin-free recombinant factor VIII (rAHF-PFM) in haemophilia A. Haemophilia. 2015;21(6):791–8. 10.1111/hae.12724 [DOI] [PubMed] [Google Scholar]
- 23. Iorio A, Krishnan S, Myrén KJ, et al. : Indirect comparisons of efficacy and weekly factor consumption during continuous prophylaxis with recombinant factor VIII Fc fusion protein and conventional recombinant factor VIII products. Haemophilia. 2017;23(3):408–16. 10.1111/hae.13160 [DOI] [PubMed] [Google Scholar]
- 24. Klukowska A, Szczepański T, Vdovin V, et al. : Long-term tolerability, immunogenicity and efficacy of Nuwiq® (human-cl rhFVIII) in children with severe haemophilia A. Haemophilia. 2018;24(4):595–603. 10.1111/hae.13460 [DOI] [PubMed] [Google Scholar]
- 25. Hakimi Z, Santagostino E, Postma MJ, et al. : Recombinant FVIIIFc Versus BAY 94-9027 for Treatment of Patients with Haemophilia A: Comparative Efficacy Using a Matching Adjusted Indirect Comparison. Adv. Ther. 2021;38(2):1263–74. 10.1007/s12325-020-01599-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reding MT, Pabinger I, Holme PA, et al. : Confirmed long-term safety and efficacy of prophylactic treatment with BAY 94-9027 in severe haemophilia A: final results of the PROTECT VIII extension study. Haemophilia. 2021;27(3):e347–56. 10.1111/hae.14297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Akdeniz N, Karakuş A, Yıldız İ, et al. : Evaluation of bleeding symptoms and laboratory parameters related to bleeding in sisters of patients with hemophilia A and B. Transfus. Apher. Sci. 2021;60(2):103044. 10.1016/j.transci.2020.103044 [DOI] [PubMed] [Google Scholar]
- 28. Berntorp E, Shapiro AD: Modern haemophilia care. Lancet. 2012;379(9824):1447–56. 10.1016/s0140-6736(11)61139-2 [DOI] [PubMed] [Google Scholar]
- 29. Konkle BA, Huston H, Nakaya Fletcher S, et al. : Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews ®. Seattle (WA): University of Washington, Seattle;2000 Sep 21 [Updated 2017 Jun 22];1993–2021. Reference Source [Google Scholar]
- 30. Roosendaal G, Lafeber FP: Blood-induced joint damage in hemophilia. Semin. Thromb. Hemost. 2003;29(1):37–42. 10.1055/s-2003-37938 [DOI] [PubMed] [Google Scholar]
- 31. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. : Guidelines for the management of hemophilia. Haemophilia. 2013;19(1):e1–e47. 10.1111/j.1365-2516.2012.02909.x [DOI] [PubMed] [Google Scholar]
- 32. Manco-Johnson MJ, Lundin B, Funk S, et al. : Effect of late prophylaxis in hemophilia on joint status: a randomized trial. J. Thromb. Haemost. 2017;15(11):2115–24. 10.1111/jth.13811 [DOI] [PubMed] [Google Scholar]
- 33. Kulkarni R, Karim FA, Glamocanin S, et al. : Results from a large multinational clinical trial (guardian TM3) using prophylactic treatment with turoctocog alfa in paediatric patients with severe haemophilia A: Safety, efficacy and pharmacokinetics. Haemophilia. 2013;19(5):698–705. 10.1111/hae.12165 [DOI] [PubMed] [Google Scholar]
- 34. Young G, Mahlangu J, Kulkarni R, et al. : Recombinant factor VIII Fc fusion protein for the prevention and treatment of bleeding in children with severe hemophilia A. J. Thromb. Haemost. 2015;13(6):967–77. 10.1111/jth.12911 [DOI] [PubMed] [Google Scholar]
- 35. Mahlangu J, Powell JS, Ragni MV, et al. : Phase 3 study of recombinant factor VIII Fc fusion protein in severe hemophilia A. Blood. 2014;123(3):317–25. 10.1182/blood-2013-10-529974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lentz SR, Misgav M, Ozelo M, et al. : Results from a large multinational clinical trial (guardian TM1) using prophylactic treatment with turoctocog alfa in adolescent and adult patients with severe haemophilia A: Safety and efficacy. Haemophilia. 2013;19(5):691–7. 10.1111/hae.12159 [DOI] [PubMed] [Google Scholar]
- 37. Mancuso ME, Biss T, Fischer K, et al. : PROTECT VIII kids extension study: Long-term safety and efficacy of BAY 94-9027 (damoctocog alfa pegol) in children with severe haemophilia A. Haemophilia. 2021;27(3):434–44. 10.1111/hae.14294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Castro HE, Briceño MF, Casas CP, et al. : The history and evolution of the clinical effectiveness of haemophilia type A treatment: A systematic review. Indian J Hematol Blood Transfus. 2014;30(1):1–11. 10.1007/s12288-012-0209-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pipe SW: New therapies for hemophilia. Hematol (United States). 2016;2016(1):650–6. 10.1182/asheducation-2016.1.650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schrijvers LH, Uitslager N, Schuurmans MJ, et al. : Barriers and motivators of adherence to prophylactic treatment in haemophilia: A systematic review. Haemophilia. 2013;19(3):355–61. 10.1111/hae.12079 [DOI] [PubMed] [Google Scholar]
- 41. Stidl R, Denne M, Goldstine J, et al. : Polyethylene glycol exposure with antihemophilic factor (Recombinant), PEGylated (rurioctocog alfa pegol) and other therapies indicated for the pediatric population: History and safety. Pharmaceuticals. 2018;11(3):75. 10.3390/ph11030075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Santagostino E, Young G, Carcao M, et al. : A contemporary look at FVIII inhibitor development: still a great influence on the evolution of hemophilia therapies. Expert. Rev. Hematol. 2018;11(2):87–97. 10.1080/17474086.2018.1419862 [DOI] [PubMed] [Google Scholar]
- 43. Garagiola I, Palla R, Peyvandi F: Risk factors for inhibitor development in severe hemophilia a. Thromb. Res. 2018;168(March):20–7. 10.1016/j.thromres.2018.05.027 [DOI] [PubMed] [Google Scholar]
- 44. Spena S, Garagiola I, Cannavò A, et al. : Prediction of factor VIII inhibitor development in the SIPPET cohort by mutational analysis and factor VIII antigen measurement. J. Thromb. Haemost. 2018;16(4):778–90. 10.1111/jth.13961 [DOI] [PubMed] [Google Scholar]
- 45. Xi M, Makris M, Marcucci M, et al. : Inhibitor development in previously treated hemophilia A patients: A systematic review, meta-analysis, and meta-regression. J. Thromb. Haemost. 2013;11(9):1655–62. 10.1111/jth.12335 [DOI] [PubMed] [Google Scholar]
- 46. Elalfy MS, Elbarbary NS, Eldebeiky MS, et al. : Risk of bleeding and inhibitor development after circumcision of previously untreated or minimally treated severe hemophilia A children. Pediatr. Hematol. Oncol. 2012;29(5):485–93. 10.3109/08880018.2012.704624 [DOI] [PubMed] [Google Scholar]
- 47. Cannavò A, Valsecchi C, Garagiola I, et al. : Nonneutralizing antibodies against factor VIII and risk of inhibitor development in severe hemophilia A. Blood. 2017;129(10):1245–50. 10.1182/blood-2016-06-720086 [DOI] [PubMed] [Google Scholar]
- 48. Peyvandi F, Mannucci PM, Garagiola I, et al. : A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N. Engl. J. Med. 2016;374(21):2054–64. 10.1056/NEJMoa1516437 [DOI] [PubMed] [Google Scholar]
- 49. U.S. Food and Drug Administration (FDA): Adynovate [Bula]. 2016;1–27.
- 50. Franchini M, Tagliaferri A, Mengoli C, et al. : Cumulative inhibitor incidence in previously untreated patients with severe hemophilia A treated with plasma-derived versus recombinant factor VIII concentrates: a critical systematic review. Crit. Rev. Oncol. Hematol. 2012;81(1):82–93. 10.1016/j.critrevonc.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 51. Sherief LM, Gaber OA, Youssef HM, et al. : Factor VIII inhibitor development in Egyptian hemophilia patients: does intron 22 inversion mutation play a role? Ital. J. Pediatr. 2020;46(1):129. 10.1186/s13052-020-00878-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Iorio A, Puccetti P, Makris M: Clotting factor concentrate switching and inhibitor development in hemophilia A. Blood. 2012;120(4):720–7. 10.1182/blood-2012-03-378927 [DOI] [PubMed] [Google Scholar]
- 53. European Medicines Agency: Guideline on the clinical investigation of recombinant and human plasma-derived factor VIII products Guideline on the clinical investigation of recombinant and human plasma-derived factor VIII products Table of contents. 2012. Reference Source
- 54. Witarto BS, Visuddho V, Witarto AP: PRISMA Checklist for “Efficacy, Safety, and Immunogenicity of Rurioctocog Alfa Pegol for Prophylactic Treatment in Previously Treated Patients with Severe Hemophilia A: A Systematic Review and Meta Analysis of Clinical Trials.” 2021. 10.17605/OSF.IO/4EZAG [DOI] [PMC free article] [PubMed]