Abstract
Introduction
The first presentation of ulcerative colitis may be an acute flare in about 15% of patients, requiring hospital admission. In acute severe steroid-refractory ulcerative colitis, cytomegalovirus (CMV) should be sought because it is a frequent cause of refractory disease. Herpes simplex colitis constitutes a rarer event in ulcerative colitis patients and it is usually associated with immunosuppression.
Case Presentation
We report a case of a first presentation of ulcerative colitis complicated by CMV and herpes simplex type 2 coinfection. After a long period of systemic corticosteroids, the diagnosis of both CMV and herpes colitis was made. Despite antiviral treatment, colectomy was required due to a contained perforation.
Discussion/Conclusion
This report highlights the importance of a high degree of suspicion for opportunistic infections in steroid/immunomodulator refractory ulcerative colitis, even in the first flare.
Keywords: Inflammatory bowel disease, Cytomegalovirus, Herpes simplex virus, Opportunistic infection, Colectomy
Resumo
Introdução
A Colite Ulcerosa pode apresentar-se de forma aguda em até 15% dos casos, com necessidade de internamento hospitalar. Na agudização severa de Colite Ulcerosa refractária a corticoterapia deve ser excluída a infeção por Citomegalovirus (CMV), dado tratar-se de uma causa frequente de doença refractária. A colite por Herpes simplex é mais rara nos doentes com Colite Ulcerosa e associa-se frequentemente a imunossupressão.
Descrição do caso
Relata-se a apresentação inaugural de Colite Ulcerosa complicada por co-infeção por CMV e herpes simplex tipo 2. Após terapêutica prolongada com corticoids sistémicos, foi diagnosticada colite tanto por CMV como Herpes simplex. Apesar de tratamento anti-vírico, foi necessária colectomia por perfuração cólica.
Discussão/Conclusão
Este caso sublinha a importância de um alto grau de suspeição para infeções oportunistas em doentes com doença refractária a corticóide/imunomoduladores, mesmo na primeira agudização.
Palavras Chave: Doença inflamatória intestinal, Citomegalovirus, Vírus herpes simplex, Infeções oportunistas, Colectomia
Introduction
The first presentation of ulcerative colitis may be an acute flare in about 15% of patients [1]. These cases often require hospital admission so that a workup can be performed and adequate treatment can be provided.
Cytomegalovirus (CMV) belongs to the Herpesviridae family, and primary infections in immunocompetent individuals are usually unremarkable [2]. However, virus reactivation in immunosuppressed patients poses a serious threat, capable of multiple organ damage [2, 3]. Currently, CMV disease should be sought in active severe ulcerative colitis, because it is a frequent cause of steroid refractory disease [1]. In order to improve the diagnosis of actual CMV disease, rather than infection, detection of CMV DNA by PCR or histopathology combined with immunohistochemistry is preferred over serology [4].
Herpes simplex (HSV) types 1 and 2, on the other hand, have a less clear role in the exacerbation of ulcerative colitis. Herpes simplex colitis constitutes a rarer event in ulcerative colitis patients [4, 5, 6, 7] and it is usually associated with immunosuppression [8]. Nonetheless, it warrants a swift diagnosis and treatment to prevent poor outcomes [5, 6, 7].
We report a case of a first presentation of ulcerative colitis complicated by CMV and herpes simplex type 2 coinfection.
Case Report/Case Presentation
A 63-year-old female patient with no previous medical history besides an anxiety disorder, usually medicated with cloxazolam, presented to her local hospital with a 1-month history of bloody diarrhea (5 bowel movements per day), colicky abdominal pain, urgency, and fever. She denied weight loss, recent use of antibiotics, or recent travel. In the emergency department, the physical examination was unremarkable apart from mucosal pallor. The patient presented a hemoglobin level of 9.6 g/dL, a C-reactive protein level of 14 g/dL, and albumin level of 2.0 g/dL. Stool testing for Clostridium difficile, as well as parasitical and bacterial cultures, were negative. In the left-sided colonoscopy, continuous mucosal erythema and friability were seen from the distal rectum up to the descending colon, with deep ulcers in all segments, the biopsies of which showed an active colitis pattern without identification of pathogenic microorganisms. Immunohistochemistry for CMV was negative.
She was then admitted and started on mesalazine and intravenous steroids, after a failed cycle of ciprofloxacin, with an assumed diagnosis of ulcerative colitis. During the next 2 months the patient was maintained on systemic corticosteroids, without clinical remission, and developed numerous complications such as respiratory infections, anemia requiring blood transfusion, and diabetes due to corticotherapy.
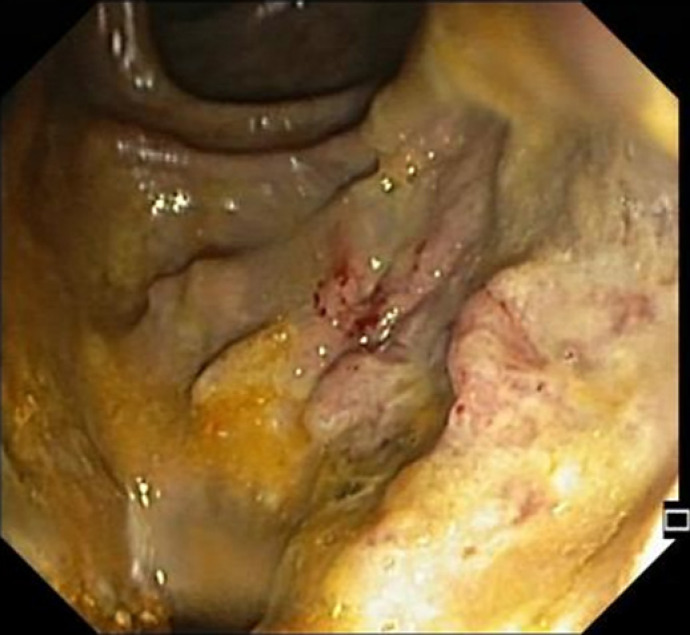
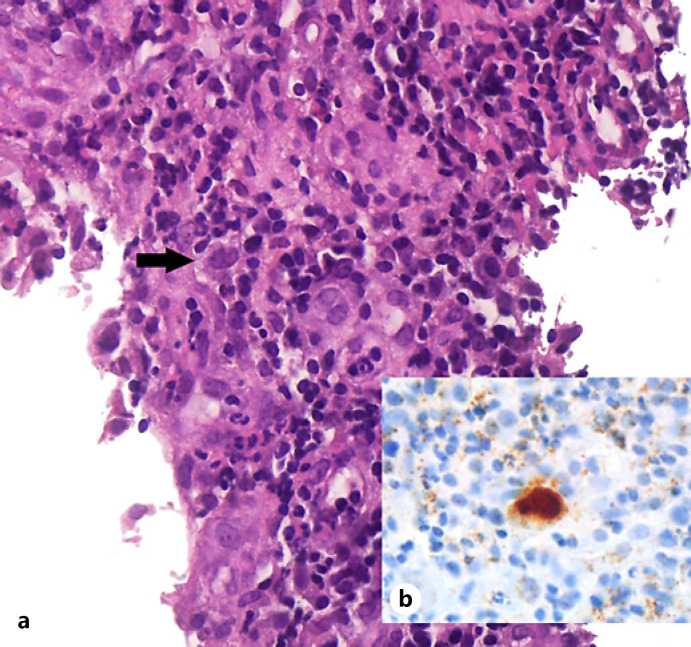
At that point she was diagnosed with severe sepsis due to nosocomial pneumonia and she was transferred to our hospital, where she arrived tachycardic, requiring supplementary oxygen (FiO2 40%), confused, tachypneic, and with muscle wasting. The patient presented ulceration of the perianal region, with multiple, linear, exudating ulcers deriving from the anal verge. The left-sided colonoscopy revealed loss of the vascular pattern, diffuse congestion and erythema and focal areas of superficial ulceration combined with other areas of inflammatory polyps (Fig. 1). Considering the clinical course, the perianal ulceration, and the endoscopic findings, biopsies were made and a tissue analysis by polymerase chain reaction (PCR) was positive for CMV DNA and herpes simplex type 2 DNA. Concerning serology, IgG and IgM for CMV were both positive and for HSV type 2 there was positive IgG but negative IgM. The histopathologic examination confirmed the diagnosis of CMV infection (Fig. 2). Both intravenous ganciclovir and aciclovir were started in order to cover CMV and HSV type 2, and steroid tapering was initiated.
Fig. 1.
Colonoscopy showing deep ulcers in the sigmoid colon.
Fig. 2.
Histological findings of the colon biopsy specimen. a Cells with enlarged nuclei containing basophilic intranuclear inclusions. H&E. ×400. b Immunohistochemical staining for CMV. ×400.
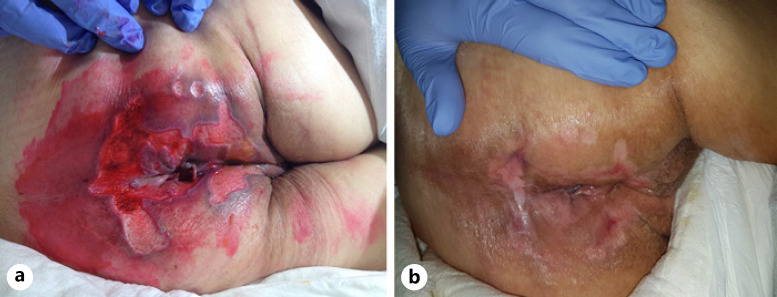
The sepsis responded well to antibiotic treatment and after 2 weeks of treatment the diarrhea had significantly improved, so acyclovir was stopped and ganciclovir was switched to oral valganciclovir. However, the perianal ulcers were not taking a favorable course. The PCR from the skin biopsy was negative for CMV and HSV DNA and the histopathologic analysis was coincident with a nonspecific ulcer. In addition, a rectovaginal fistula 5 cm from the anal verge was found in the follow-up colonoscopy. In consideration of the above, after discussion with the surgical department, a protective ileostomy was performed on the 30th day of admission.
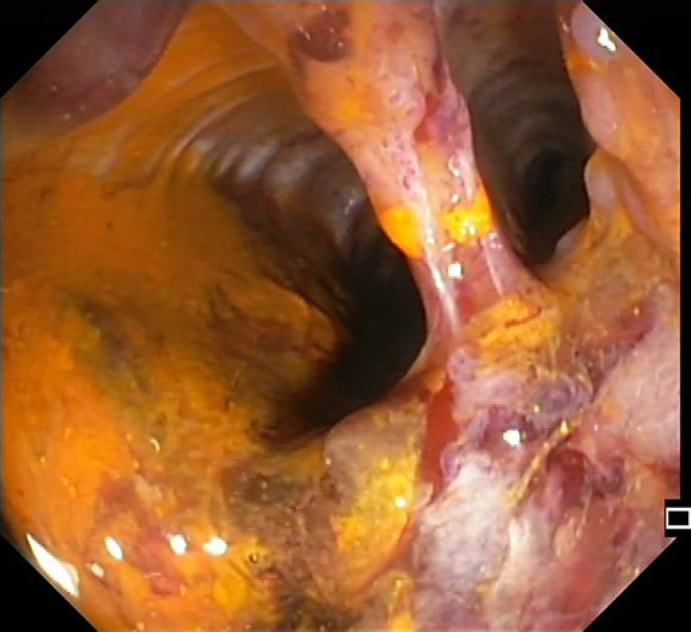
The patient then underwent a physical rehabilitation program while waiting to be transferred to a rehabilitation healthcare unit. With respect to the perianal ulceration, it progressively improved after the ileostomy (Fig. 3). In order to access endoscopic activity and decide on the course of treatment before discharge, a colonoscopy was performed, revealing a contained colonic perforation 30 cm from the anal verge, giving access to the retroperitoneum (Fig. 4). An abdominal CT confirmed the perforation and the patient was submitted to total proctocolectomy and terminal ileostomy on the 53th day of admission, which was considered a more definitive and safer treatment. Histopathologic examination of the surgical specimen revealed, from the distal rectum to 5 cm distal to the ileocecal valve, extensive areas of mucosal ulceration covered by fibrinoleucocyte exudate and the formation of granulation tissue up to the muscularis propria. In the colon, multiple filiform pseudopolyps were seen. In the distal 5 cm of the rectum, polymorphic inflammatory infiltrate in the lamina propria and cryptic abscesses were both observed (Fig. 5).
Fig. 3.
Perianal ulcers. a Poor healing despite topical treatment. b A few weeks after ileostomy.
Fig. 4.
Wide colonic rupture with access to the retroperitoneum.
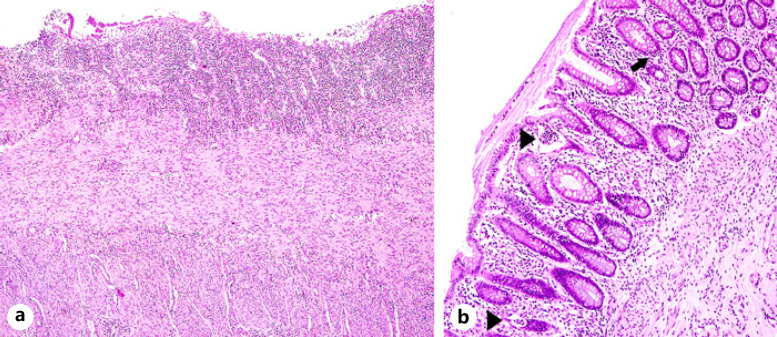
Fig. 5.
Histological findings in the surgical specimen. a Area of ulceration. H&E. ×40. b Mucosa with mild glandular architectural disarray, cryptitis (arrow), and crypt abscesses (arrowheads). H&E. ×100.
Once the postsurgical period had been overcome, the rehabilitation program was resumed and the patient was discharged to another healthcare facility to continue her recovery. Two months later, she returned for observation as an outpatient, with remarkable improvement; she was able to walk with some help, and she was asymptomatic and presented complete healing of the perianal ulcers.
Discussion/Conclusion
To the best of the authors' knowledge, this is the first case of CMV and HSV type 2 coinfection in an ulcerative colitis patient.
Despite the fact that some features, such as the recto-vaginal fistula and the perianal ulcers, suggested Crohn's disease, the endoscopic and histopathologic characteristics pointed toward ulcerative colitis.
A conclusive etiologic diagnosis for the perianal ulcers could not be made. On the one hand, the possibility of cutaneous HSV or CMV infection must be considered. Genital and perianal ulcers are the typical lesions of HSV type 2 [9] and the most frequent manifestation of cutaneous CMV [10]. Conversely, no viral DNA was found by PCR of the skin biopsy tissue. On the other hand, cutaneous involvement by Crohn's disease is part of the differential diagnosis. Perianal ulceration is the most common pattern of skin ulceration in Crohn's disease [11, 12]. Yet, as previously mentioned, ulcerative colitis seemed a stronger possibility and this kind of perianal disease is rare in that condition. In addition, the histopathology of the skin lesion did not reveal any features suggestive of Crohn's disease. Finally, the diagnosis of pressure ulcers should not be overlooked in a debilitated, bedridden patient who was dependent for hygiene care. In consideration of the above, this last hypothesis presents as the most likely, since the ulceration improved after stool transit diversion.
A retrospective study of acute severe UC found that recent therapy with high-dose steroids and colonoscopy with deep ulcers/higher Mayo scores were associated with CMV disease [13], both of which were present in this patient. The same applies to other predictive factors previously identified, i.e., increasing age, duration of disease of <5 years [14], and immunosuppressive therapy [14, 15, 16]. CMV colitis is associated with worse outcomes in severe ulcerative colitis [13, 17, 18]. In fact, there are some reports of colonic perforation in CMV colitis [19, 20, 21, 22]. However, in this case the patient seemed to be improving and had already undergone several weeks of antiviral treatment, which hazes the role of CMV in this outcome.
Regarding the HSV infection, one could argue that it was only found by PCR, which has a high sensitivity, and it could be only an accidental finding. However, PCR for viral DNA from tissue biopsies is a valid method of diagnosis [4] and, considering the severity of this case, specific treatment was mandatory. Although it is an exceptional diagnosis compared to CMV disease in acute severe ulcerative colitis, it should be borne in mind as otherwise a treatable cause of exacerbation will be missed.
Ganciclovir and aciclovir are the first-line treatment for CMV and HSV disease, respectively [4, 23]. Neither is considered adequate for the treatment of both disorders. Consequently, both were rapidly started once the diagnosis had been made. Concerning the duration of treatment, a 2- to 3-week course is usually recommended, with the possibility of switching from ganciclovir to valganciclovir for oral treatment, depending on the clinical course [4, 24]. Similarly, acyclovir is prescribed between 2 and 3 weeks in HSV colitis [5, 7].
In conclusion, this report highlights the importance of a high degree of suspicion for opportunistic infections in steroid/immunomodulator refractory ulcerative colitis, even in the first flare.
Statement of Ethics
This case report was approved by the hospital's health ethics committee and was done in accordance with the Declaration of Helsinki. The patient gave written informed consent for this publication.
Conflict of Interest Statement
The authors have no conflict of interests to declare.
Funding Sources
No funding was received for this work.
Author Contributions
T.L. was responsible for the design of this study, acquisition and analysis of the data, and drafting of this paper. D.C. and C.F. contributed to data acquisition and analysis and critical revision of this work for important intellectual content. B.A., J.B.S., and R.G. interpreted the data for this work and the critically revised this paper for important intellectual content. All of the authors approved the final version to be published and agreed to be accountable for all aspects of the work.
References
- 1.Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. European Crohn's and Colitis Organisation [ECCO] Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohn's Colitis. 2017 Jun;11((6)):649–70. doi: 10.1093/ecco-jcc/jjx008. [DOI] [PubMed] [Google Scholar]
- 2.Sinclair J, Sissons P. Latency and reactivation of human cytomegalovirus. J Gen Virol. 2006 Jul;87((Pt 7)):1763–79. doi: 10.1099/vir.0.81891-0. [DOI] [PubMed] [Google Scholar]
- 3.Hamlin PJ, Shah MN, Scott N, Wyatt JI, Howdle PD. Systemic cytomegalovirus infection complicating ulcerative colitis: a case report and review of the literature. Postgrad Med J. 2004 Apr;80((942)):233–5. doi: 10.1136/pgmj.2003.007385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahier JF, Magro F, Abreu C, Armuzzi A, Ben-Horin S, Chowers Y, et al. European Crohn's and Colitis Organisation (ECCO) Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohn's Colitis. 2014 Jun;8((6)):443–68. doi: 10.1016/j.crohns.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 5.Schunter MO, Walles T, Fritz P, Meyding-Lamadé U, Thon KP, Fellermann K, et al. Herpes simplex virus colitis complicating ulcerative colitis: A case report and brief review on superinfections. J Crohn's Colitis. 2007 Sep;1((1)):41–6. doi: 10.1016/j.crohns.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Blaszyk H, Hyman NH, Cooper K. Herpes simplex virus colitis in ulcerative colitis, simulating malignancy. Histopathology. 2006 Sep;49((3)):316–8. doi: 10.1111/j.1365-2559.2006.02460.x. [DOI] [PubMed] [Google Scholar]
- 7.Phadke VK, Friedman-Moraco RJ, Quigley BC, Farris AB, Norvell JP. Concomitant herpes simplex virus colitis and hepatitis in a man with ulcerative colitis: Case report and review of the literature. In: M Lu., editor. Medicine. (42) Vol. 95. 2016. p. e5082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toruner M, Loftus EV, Jr, Harmsen WS, Zinsmeister AR, Orenstein R, Sandborn WJ, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008 Apr;134((4)):929–36. doi: 10.1053/j.gastro.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Gupta R, Warren T, Wald A. Genital herpes. Lancet. 2007 Dec;370((9605)):2127–37. doi: 10.1016/S0140-6736(07)61908-4. [DOI] [PubMed] [Google Scholar]
- 10.Choi YL, Kim JA, Jang KT, Kim DS, Kim WS, Lee JH, et al. Characteristics of cutaneous cytomegalovirus infection in non-acquired immune deficiency syndrome, immunocompromised patients. Br J Dermatol. 2006 Nov;155((5)):977–82. doi: 10.1111/j.1365-2133.2006.07456.x. [DOI] [PubMed] [Google Scholar]
- 11.Mountain JC. Cutaneous ulceration in Crohn's disease. Gut. 1970 Jan;11((1)):18–26. doi: 10.1136/gut.11.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panackel C, John J, Krishnadas D, Vinayakumar KR. Metastatic Crohn's disease of external genitalia. Indian J Dermatol. 2008;53((3)):146–8. doi: 10.4103/0019-5154.43207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee HS, Park SH, Kim SH, Kim J, Choi J, Lee HJ, et al. Risk factors and clinical outcomes associated with cytomegalovirus colitis in patients with acute severe ulcerative colitis. Inflamm Bowel Dis. 2016 Apr;22((4)):912–8. doi: 10.1097/MIB.0000000000000675. [DOI] [PubMed] [Google Scholar]
- 14.Lévêque N, Brixi-Benmansour H, Reig T, Renois F, Talmud D, Brodard V, et al. Low frequency of cytomegalovirus infection during exacerbations of inflammatory bowel diseases. J Med Virol. 2010 Oct;82((10)):1694–700. doi: 10.1002/jmv.21877. [DOI] [PubMed] [Google Scholar]
- 15.Gauss A, Rosenstiel S, Schnitzler P, Hinz U, Rehlen T, Kadmon M, et al. Intestinal cytomegalovirus infection in patients hospitalized for exacerbation of inflammatory bowel disease: a 10-year tertiary referral center experience. Eur J Gastroenterol Hepatol. 2015 Jun;27((6)):712–20. doi: 10.1097/MEG.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 16.Al-Zafiri R, Gologan A, Galiatsatos P, Szilagyi A. Cytomegalovirus complicating inflammatory bowel disease: a 10-year experience in a community-based, university-affiliated hospital. Gastroenterol Hepatol (N Y) 2012 Apr;8((4)):230–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Papadakis KA, Tung JK, Binder SW, Kam LY, Abreu MT, Targan SR, et al. Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol. 2001 Jul;96((7)):2137–42. doi: 10.1111/j.1572-0241.2001.03949.x. [DOI] [PubMed] [Google Scholar]
- 18.Sager K, Alam S, Bond A, Chinnappan L, Probert CS. Review article: cytomegalovirus and inflammatory bowel disease. Aliment Pharmacol Ther. 2015 Apr;41((8)):725–33. doi: 10.1111/apt.13124. [DOI] [PubMed] [Google Scholar]
- 19.Kishore J, Ghoshal U, Ghoshal UC, Krishnani N, Kumar S, Singh M, et al. Infection with cytomegalovirus in patients with inflammatory bowel disease: prevalence, clinical significance and outcome. J Med Microbiol. 2004 Nov;53((Pt 11)):1155–60. doi: 10.1099/jmm.0.45629-0. [DOI] [PubMed] [Google Scholar]
- 20.Eyre-Brook IA, Dundas S. Incidence and clinical significance of colonic cytomegalovirus infection in idiopathic inflammatory bowel disease requiring colectomy. Gut. 1986 Dec;27((12)):1419–25. doi: 10.1136/gut.27.12.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waters RE, Agarwal A, Tan D. A case report of cytomegalovirus-induced colitis with colonic perforation. Am J Dig Dis. 2015;2((2)):106–10. [Google Scholar]
- 22.Goodman ZD, Boitnott JK, Yardley JH. Perforation of the colon associated with cytomegalovirus infection. Dig Dis Sci. 1979 May;24((5)):376–80. doi: 10.1007/BF01297124. [DOI] [PubMed] [Google Scholar]
- 23.Benson CA, Kaplan JE, Masur H, Pau A, Holmes KK, CDC. National Institutes of Health. Infectious Diseases Society of America Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Recomm Rep. 2004 Dec;53(RR-15):1–112. [PubMed] [Google Scholar]
- 24.Park SC, Jeen YM, Jeen YT. Approach to cytomegalovirus infections in patients with ulcerative colitis. Korean J Intern Med (Korean Assoc Intern Med) 2017 May;32((3)):383–92. doi: 10.3904/kjim.2017.087. [DOI] [PMC free article] [PubMed] [Google Scholar]