Key Points
Question
Is an initial treatment of physical therapy cost-effective compared with an initial treatment of glucocorticoid injection for patients with knee osteoarthritis?
Findings
In this economic evaluation that included 156 adults participating in a randomized clinical trial, participants receiving physical therapy gained more quality-adjusted life-years compared with those receiving glucocorticoid injection. Costs related to knee care were similar between groups, although total medical costs for any reason were higher in the physical therapy group.
Meaning
The results of this study suggest that although the mean cost of providing an initial course of physical therapy may be higher than an initial course of glucocorticoid injections, the greater improvement in quality-adjusted life-years may be worth the additional cost.
Abstract
Importance
Physical therapy and glucocorticoid injections are initial treatment options for knee osteoarthritis, but available data indicate that most patients receive one or the other, suggesting they may be competing interventions. The initial cost difference for treatment can be substantial, with physical therapy often being more expensive at the outset, and cost-effectiveness analysis can aid patients and clinicians in making decisions.
Objective
To investigate the incremental cost-effectiveness between physical therapy and intra-articular glucocorticoid injection as initial treatment strategies for knee osteoarthritis.
Design, Setting, and Participants
This economic evaluation is a secondary analysis of a randomized clinical trial performed from October 1, 2012, to May 4, 2017. Health economists were blinded to study outcomes and treatment allocation. A randomized sample of patients seen in primary care and physical therapy clinics with a radiographically confirmed diagnosis of knee osteoarthritis were evaluated from the clinical trial with 96.2% follow-up at 1 year.
Interventions
Physical therapy or glucocorticoid injection
Main Outcomes and Measures
The main outcome was incremental cost-effectiveness between 2 alternative treatments. Acceptability curves of bootstrapped incremental cost-effectiveness ratios (ICERs) were used to identify the proportion of ICERs under the specific willingness-to-pay level ($50 000-$100 000). Health care system costs (total and knee related) and health-related quality-of-life based on quality-adjusted life-years (QALYs) were obtained.
Results
A total of 156 participants (mean [SD] age, 56.1 [8.7] years; 81 [51.9%] male) were randomized 1:1 and followed up for 1 year. Mean (SD) 1-year knee-related medical costs were $2113 ($4224) in the glucocorticoid injection group and $2131 ($1015) in the physical therapy group. The mean difference in QALY significantly favored physical therapy at 1 year (0.076; 95% CI, 0.02-0.126; P = .003). Physical therapy was the more cost-effective intervention, with an ICER of $8103 for knee-related medical costs, with a 99.2% probability that results fall below the willingness-to-pay threshold of $100 000.
Conclusions and Relevance
A course of physical therapy was cost-effective compared with a course of glucocorticoid injections for patients with knee osteoarthritis. These results suggest that, although the initial cost of delivering physical therapy may be higher than an initial course of glucocorticoid injections, 1-year total knee-related costs are equivalent, and greater improvement in QALYs may justify the initial higher costs.
Trial Registration
ClinicalTrials.gov Identifier: NCT01427153
This economic evaluation compares the cost-effectiveness of physical therapy vs intra-articular glucocorticoid injection as initial treatment strategies for knee osteoarthritis.
Introduction
Osteoarthritis is the most common type of arthritis, accounting for a disproportionate level of disability and health care expenditures worldwide. It is the eighth most expensive of 154 health conditions to manage in the US, costing more than $80 billion in 2016.1 The knee is one of the more common joints affected by osteoarthritis, with its prevalence doubling during the last 70 years.2 Knee osteoarthritis may begin early in life and progresses slowly, providing opportunities for nonsurgical treatment options.3
Effective nonsurgical treatment options are available for knee OA that should be considered before surgery. The American College of Rheumatology provides guidelines that include 6 strongly and 8 conditionally recommended nonpharmacological interventions, as well as 3 strongly and 4 conditionally recommended pharmacological treatments.4 With so many choices, patients and clinicians often find it challenging to establish optimal treatment plans. One critical component for decision-making is the cost and accessibility of the intervention.
Physical therapy and intra-articular glucocorticoid injections are common treatments for knee osteoarthritis. Data from large health care systems suggest that they are infrequently delivered together,5,6 indicating that patients or their practitioners are more likely to choose one or the other. Exercise therapy, a core nonpharmacological intervention for knee osteoarthritis, is a staple of physical therapy programs. Manual therapy also has proven to be an effective treatment in several clinical trials.7,8,9 A single glucocorticoid injection typically delivered during the same consultation with the diagnosing clinician may be initially less expensive and less time intensive than a course of physical therapy. However, there is concern that glucocorticoid injections may accelerate degenerative changes in the longer term and may not add to the benefit of physical therapy in the short term.10,11,12,13 Consideration for both short- and longer-term outcomes, treatment risks and adverse effects, and the downstream effect of each treatment choice should influence and inform these decisions instead of initial cost alone. Value is defined by the cost incurred to generate a change in outcome.14 Some interventions with lower initial costs may not carry that cost-effectiveness into the long term. Although physical therapy was clinically more effective than glucocorticoid injection in a recent trial,15 a typical course is usually more costly than a single injection ($99-$172 for a primary care office visit and injection procedure and $557-$919 for a low-complexity physical therapy evaluation and 7 additional physical therapy sessions consisting of manual therapy and 30 minutes of exercise per the 2020 Medicare Physician Fee Schedule).16 Given the high prevalence of knee osteoarthritis and the frequency of practical decisions made about best treatment options, we aimed to assess the cost-effectiveness of physical therapy compared with glucocorticoid injection from the health care perspective.
Methods
Overview
We conducted an economic evaluation using patient-level data from a randomized clinical trial15 that captured health care system costs, including knee-specific care costs, and quality-adjusted life-years (QALYs), which is a 2-dimensional metric that incorporates both health-related quality of life and survival. We used the Panel on Cost-Effectiveness in Health and Medicine guidelines for conducting the cost-effectiveness studies17,18 as well as the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) reporting guideline19 to guide reporting of these results. Although we noted a priori that we would capture health care use and compare it between groups in our published protocol,20 we did not formally establish a statistical plan for the cost-effectiveness analysis at that time. Therefore, this evaluation should be considered an unplanned secondary analysis. The health economist and team of statisticians were blinded to the results of the primary study, and the original publication was not published before they planned and performed these analyses. The statistical analysis plan was developed and finalized before receipt of any data. This case analysis comes from the health care perspective rather than payer or societal perspective. The health care perspective includes both current and future costs of care, both related and unrelated to the condition.21 The exception is that out-of-pocket costs were not assessed; however, there is no copayment for care in military treatment facilities, making this potentially less relevant. All participants provided written informed consent. All data were deidentified. Ethics approval was granted for the trial by the Army Pacific Health Command Institutional Review Board.
Data
The full results of the 1-year randomized clinical trial were previously reported.15 Briefly, we recruited patients who met clinical and radiographic criteria for the presence of knee osteoarthritis established by the American College of Rheumatology21 from October 1, 2012, to May 4, 2017, at 2 large military hospitals in the US. Patients were followed up until May 5, 2018. Subsequently, we randomly assigned participants to receive a management strategy that consisted of intra-articular glucocorticoid injections (n = 78) or physical therapy (n = 78), and the primary outcome was the difference in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total score at 1 year. We also collected WOMAC scores at 4, 6, and 26 weeks. Specific details of the treatment in each arm are reported in the published protocol and trial manuscript.15,20 Baseline characteristics of the cohort are described in Table 1.
Table 1. Descriptive and Demographic Variables of the 2 Groups at Baseline.
| Variable | All (n = 156) | Physical therapy (n = 78) | Glucocorticoid injection (n = 78) |
|---|---|---|---|
| Continuous variables, mean (SD) | |||
| Age, y | 56.1 (8.7) | 56.3 (9.2) | 56.0 (8.2) |
| BMI | 31.5 (5.6) | 31.4 (5.1) | 31.6 (6.1) |
| Baseline WOMAC score (total score) | 108.0 (44.7) | 108.8 (47.1) | 107.1 (42.4) |
| Duration of symptoms, mo | 92.5 (107.2) | 100.0 (122.7) | 85.0 (89.2) |
| Categorical variables, No. (%) | |||
| Sex | |||
| Male | 81 (51.9) | 41 (52.6) | 40 (51.3) |
| Female | 75 (48.1) | 37 (47.4) | 38 (48.7) |
| Smoker | 8 (5.1) | 5 (6.4) | 3 (3.8) |
| Beneficiary category | |||
| Active dutya | 41 (26.2) | 20 (25.6) | 21 (26.9) |
| Retired service member | 54 (34.6) | 28 (35.9) | 26 (33.3) |
| Family member or dependent | 61 (39.1) | 29 (37.2) | 32 (41.0) |
| Kellgren-Lawrence gradeb | |||
| 1 | 6 (3.8) | 5 (6.4) | 1 (1.3) |
| 2 | 68 (43.6) | 26 (33.3) | 42 (53.8) |
| 3 | 59 (37.8) | 34 (43.6) | 25 (32.1) |
| 4 | 23 (14.7) | 13 (16.7) | 10 (12.8) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Includes reserve or national guard on active duty.
Radiographic measures of severity are as follows: grade 1, doubtful joint space narrowing and possible osteophytic lipping; grade 2, definite osteophytes and possible joint space narrowing; grade 3, moderate multiple osteophytes, definite narrowing of joint space, and some sclerosis and possible deformity of bone ends; and grade 4, large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone ends.
Costs
We used the Military Health System Data Repository (MDR) to source all costs of care. The MDR captures care for all outpatient and inpatient encounters, ancillary services (radiology and laboratory tests), and pharmacy transactions from military and civilian clinics where TRICARE (the health care system of the US Department of Defense) is the payer. The Military Health System is a closed, single-payer government health system, where typically less than 3% of patients younger than 65 years carry other health insurance.22 Patients in this study had no copayments, which allowed capture of all medical care that was sought by each participant. Exceptions could include care not covered and paid fully out-of-pocket, such as massage therapy or chiropractic services. Although there is no actual exchange of money for care in military facilities, each element of care is assigned a predetermined value and price by the US Defense Health Agency, which is reported in the MDR, to facilitate budgeting and business case analyses. We used these cost values for care in military facilities and costs actually paid by TRICARE for all care in-network facilities. We identified knee-related care through the use of the International Classification of Diseases, Ninth Revision (ICD-9) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) diagnosis codes, as well as relevant procedures based on Current Procedural Terminology (CPT) codes. Both diagnoses and procedure codes used are listed in the eAppendix in the Supplement. Although care spanned a 6-year period, because participants were evenly randomized during this period, we did not make annual adjustments for costs. We created 2 cost outcomes: (1) total costs specifically for knee-related medical care and (2) total medical costs for any reason.
The adjusted generalized linear model with γ distribution and log link was used, controlling for age, sex, body mass index, smoking status, and Kellgren-Lawrence radiographic severity score.23 Estimated marginal means with 95% CIs were reported.
Effectiveness
Effectiveness was measured using QALYs. We used an established mapping algorithm to generate EuroQol 5-Dimension (EQ-5D) health utilities from the WOMAC scores at all time points used in the trial (baseline, 4 weeks, 8 weeks, 26 weeks, and 1 year).24 The EQ-5D is used to assess the perceived limitations of an individual related to mobility, self-care, regular daily activities, discomfort or pain, and anxiety or depression.25 The utility score was calculated for each individual anchored from 0 (death) to 1 (perfect health). The QALY was calculated from estimated EQ-5D at the 1-year interval as follows: QALY = baseline EQ-5D + [(1-year EQ-5D − baseline EQ-5D)/2]. The effectiveness analysis was conducted using an adjusted generalized linear model, reporting estimated marginal means with 95% CIs.
Cost-effectiveness
By comparing between treatment arms, the costs and QALYs were assessed at 1-year follow-up, using conventional decision rules and estimating incremental cost-effectiveness ratios (ICERs) as appropriate. The ICERs were calculated by dividing the difference in costs between both interventions by differences in effectiveness between both interventions. Although the effectiveness of physical therapy was superior in the original trial,15 a typical course of physical therapy may initially be more expensive and usually requires more resources (eg, additional visits). Therefore, we assessed whether an initial treatment choice of physical therapy could be cost-effective compared with an initial choice of glucocorticoid injection. The goal was to determine the incremental cost per effectiveness obtained. This goal was accomplished by calculating the incremental cost divided by the incremental effectiveness to derive the ICER.
The willingness-to-pay (WTP) estimates usually vary by country, with more developed countries often willing to pay more for improvements in QALYs. Although there is no universal consensus for what ICER threshold should be used in the US, we used the threshold of $100 000 per QALY because it is commonly used in the US, particularly with osteoarthritis populations,26,27,28 with compelling arguments to justify it as the minimum threshold.29,30 To express the most cost-effective strategy of the base case in US dollars, we used the net monetary benefit framework to demonstrate the net benefit of each strategy (net monetary benefit = [incremental effectiveness × WTP] – incremental cost). A positive value indicates the intervention is cost-effective at the given WTP level.
Missing Data
Because this is a closed, single-payer government system, we assumed that lack of medical encounters within MDR indicated that the care did not happen, and therefore there were no missing health care utilization data. The MDR has a robust data validation system in which data are imported daily from more than 260 sources worldwide and missing elements are continuously validated across other data sources for 90 days before the validated variable is turned from raw to final+. We pulled all data 90 days after the last participant reached the 1-year mark to ensure final validated data for every individual. We assumed that missing data for the outcomes (WOMAC and subsequent EQ-5D estimation) were missing completely at random (MCAR) and tested this assumption using the Little MCAR test.
Uncertainty
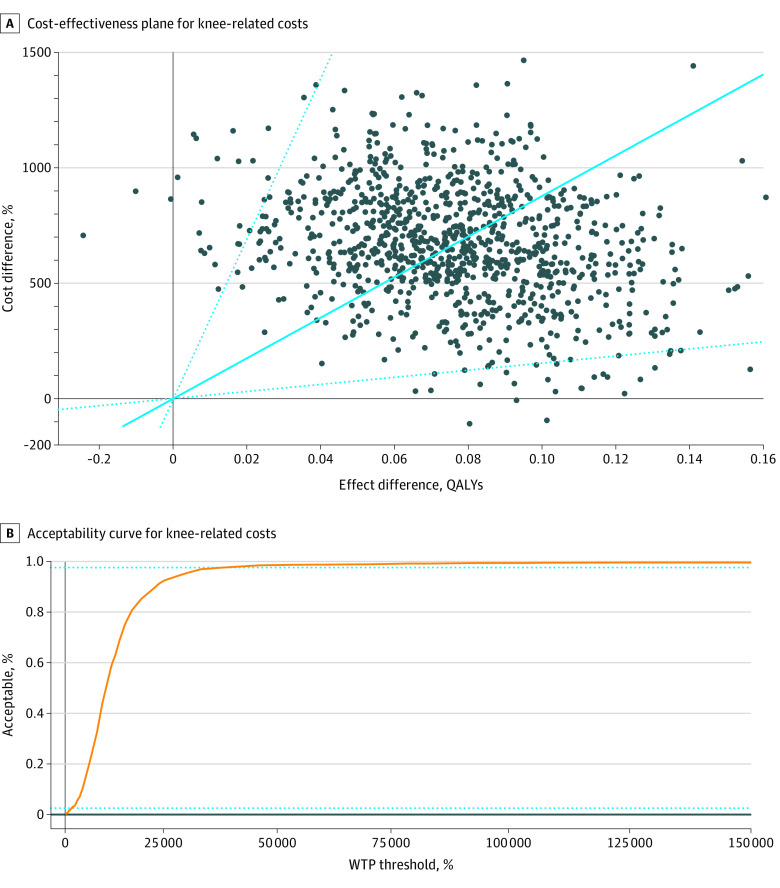
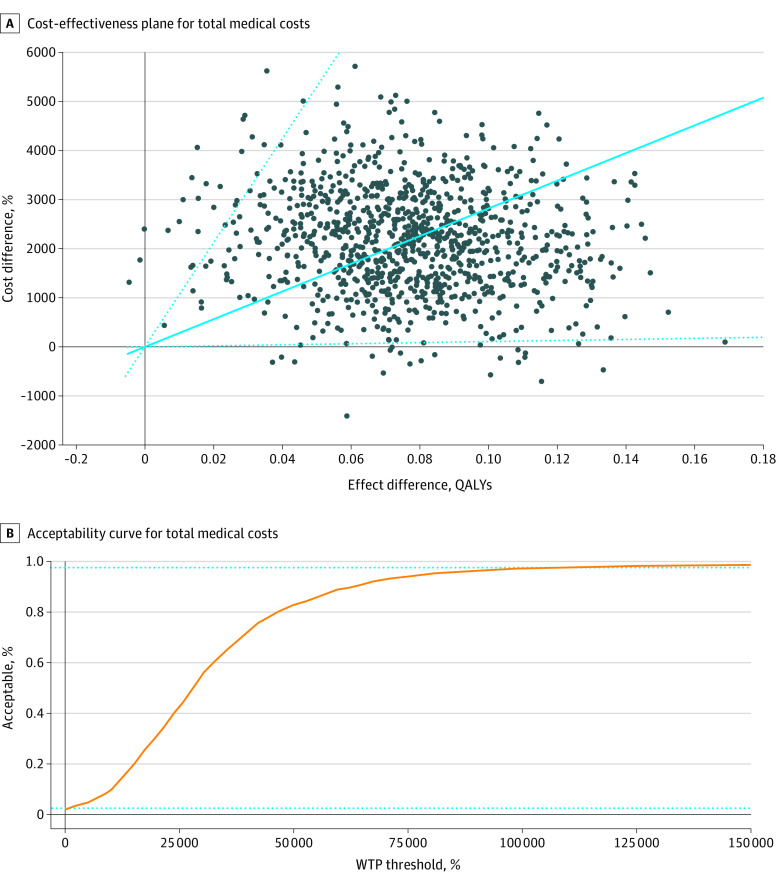
To manage the uncertainty associated with this calculation, we used a bootstrapping method composed of 1000 replications to obtain a 95% CI of the ICER. The resulting acceptability curve of these bootstrapped ICERs show the proportions of ICERs under the WTP level.
Sensitivity Analysis
We planned a priori a series of sensitivity analyses. First, we considered 2 alternate mapping algorithms to establish health utilities from the WOMAC.31,32 For the third analysis, we considered only individuals for whom there were complete follow-up data at 1 year (complete case analysis; N = 150). The fourth and fifth analyses excluded patients who received treatment from the other arm (7 from the physical therapy arm received an injection; 14 from the injection arm received physical therapy).
Statistical Analysis
The statistical significance level was set at 2-sided P < .05. The statistical analyses were conducted using Stata software, version 12 (StataCorp LLC).
Results
A total of 156 participants (mean [SD] age, 56.1 [8.7] years; 81 [51.9%] male) were randomized 1:1 and followed up for 1 year. Six participants did not provide outcomes data at 1 year (5 in the injection group; 1 in the physical therapy group). For those individuals, we used multiple imputation (Markov chain Monte Carlo method, 20 iterations),33 using other follow-up time points as predictors in the imputation model. Every participant had at least 3 of the 5 total data time points. The Little MCAR test suggested that data were indeed missing at random (169.9, P = .51). Baseline variables and demographic characteristics of each group are given in Table 1. The impact inventory recommended for report with cost-effectiveness analysis 11 is found in eTable 1 in the Supplement. Four participants (all in the glucocorticoid injection group) had knee surgery during the 1-year follow-up. Most participants in the glucocorticoid injection group received more than 1 injection (mean, 2.6).
The difference in QALYs between groups was statistically significant, with participants in the physical therapy group gaining 0.08 more QALYs than those in the corticosteroid injection group (95% CI, 0.02-0.13; P = .03) (Table 2). Unadjusted model results are present in eTable 2 in the Supplement.
Table 2. Cost-effectiveness Analysis.
| Variable | Physical therapy (n = 78) | Corticosteroid injection (n = 78) | Difference | P value | Base case ICER, $ | Bootstrapped ICER,a $ | Acceptability, % | INMB (WTP threshold of $100 000), $ | ||
|---|---|---|---|---|---|---|---|---|---|---|
| WTP threshold of $0 | WTP threshold of $50 000 | WTP threshold of $100 000 | ||||||||
| QALYs (95% CI)b | 0.76 (0.73 to 0.80) | 0.69 (0.65 to 0.72) | 0.08 (0.02 to 0.13) | .003 | NA | NA | NA | NA | NA | NA |
| Knee-related cost (95% CI)c, $ | 2449 (1893 to 3004) | 1834 (1454 to 2213) | 615 (–34 to 1263) | .06 | 8103 | 8782 (1540 to 34 975) | 0.3 | 98.5 | 99.2 | 6955 |
| Total medical cost (95% CI)c, $ | 8921 (7208 to 10 634) | 6776 (5476 to 8074) | 2145 (12 to 4279) | .049 | 28 271 | 35 527 (1318 to 206 319) | 2.0 | 82.7 | 97.2 | 5535 |
Abbreviations: ICER, incremental cost-effectiveness ratio; NA, not applicable; INMB, incremental net monetary benefit; QALYs, quality-adjusted life-years; WTP, willingness to pay.
The bootstrapping method with 1000 replications.
Generalized linear model controlling for age, body mass index, female sex, smoking status, and Kellgren-Lawrence radiographic severity score.
Generalized linear model with log link and γ distribution controlling for age, body mass index, female sex, smoking status, and Kellgren-Lawrence radiographic severity score.
Mean (SD) knee-related medical costs for the 1-year follow-up were similar between groups ($2113 [$4224] for glucocorticoid group; $2131 [$1015) for physical therapy) when unadjusted for any covariates (eTable 2 in the Supplement).15 These values included the trial intervention costs. When the costs were adjusted for age, body mass index, female sex, smoking status, and radiographic severity, however, participants in the physical therapy group spent an adjusted mean of $615 more than those in the glucocorticoid injection group, but the mean difference was not significant (95% CI, –$34 to $1263; P = .06) (Table 2). When it came to total medical costs for any reason, participants in the physical therapy group spent an adjusted mean of $2145 more than participants in the glucocorticoid injection group (95% CI, $12-$4279; P = .049) (Table 2).
Cost-effectiveness
Patients in the physical therapy group had a mean QALY of 0.076 more at a mean cost of $615 higher for knee-related medical costs than patients in the injection group, resulting in an ICER of $8103 per QALY. The ICER was $28 271 per QALY when it came to total medical costs for any reason. Both of these are much less than the common WTP thresholds of $50 000 and $100 000, suggesting that physical therapy is a cost-effective intervention despite higher initial costs than glucocorticoid injection. To address uncertainty, we obtained 1000 ICERs with bootstrapping that provided an ICER of $8782 per QALY in respect to knee-related medical costs and an ICER of $28 172 per QALY in respect to total medical costs for any reason (Figure 1). Our cost-effectiveness acceptability curve indicated that 99.2% of 1000 bootstrapped ICERs for knee-related costs and 97.2% for total medical costs for any reason were acceptable at the WTP threshold of $100 000 (Figure 2). The zero net monetary benefit threshold was at the WTP threshold $8103 for knee-related costs and $28 271 for total medical costs, indicating that physical therapy was cost-effective compared with glucocorticoid injection at any higher WTP level (Figure 3). The incremental net monetary benefit at the WTP threshold of $100 000 was $6955 for knee-related costs and $5535 for total medical costs (Figure 3).
Figure 1. Cost-effectiveness Planes and Acceptability Curves for Knee-Related Costs.
Filled circles indicate the incremental cost-effectiveness ratios, with the solid blue line showing the mean incremental cost-effectiveness ratio. Dotted lines indicate 95% CIs. WTP indicates willingness to pay; QALY, quality-adjusted life-year.
Figure 2. Cost-effectiveness Planes and Acceptability Curves for Total Medical Costs (Medical Care for Any Reason).
Filled circles indicate the incremental cost-effectiveness ratios, with the solid blue line showing the mean incremental cost-effectiveness ratio. Dotted lines indicate 95% CIs. WTP indicates willingness to pay; QALY, quality-adjusted life-year.
Figure 3. Monetary Net Benefit (MNB) Threshold.
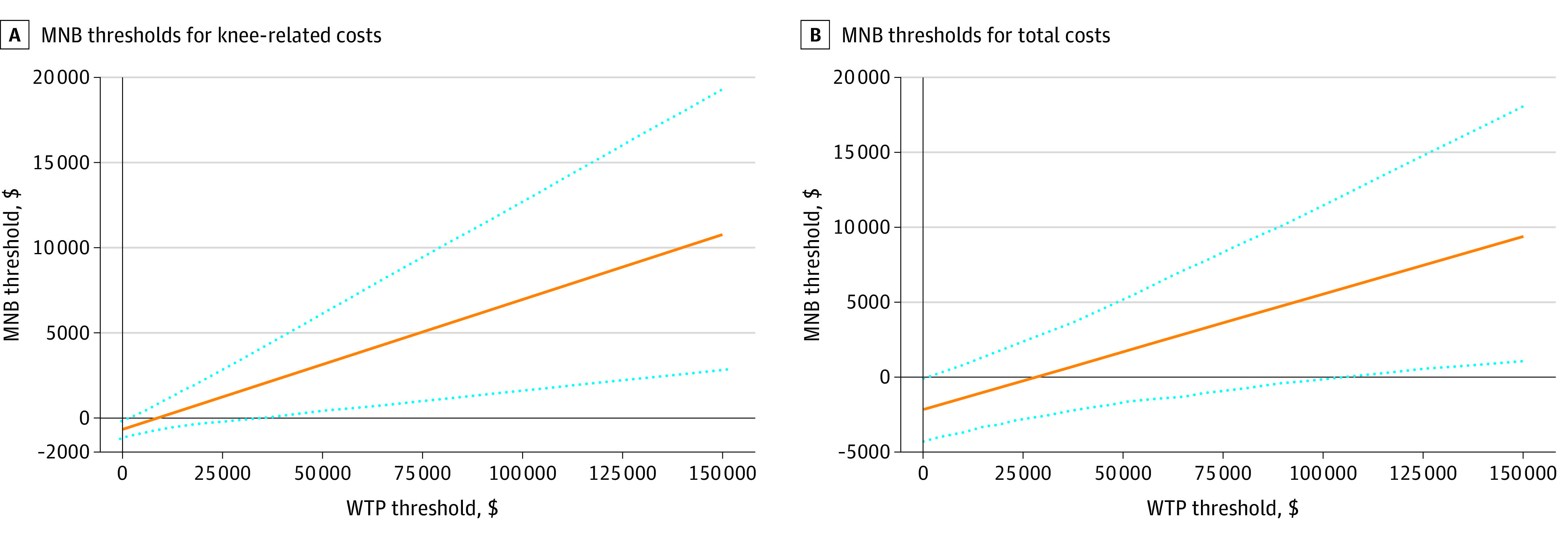
Dotted lines indicate 95% CIs. WTP indicates willingness to pay.
Sensitivity Analysis
After performing all 5 sensitivity analyses, the overall conclusions were unchanged (eTable 3 in the Supplement) The mean difference in QALYs significantly favored physical therapy in all models. The ICER for knee-related medical costs in these models ranged from $6079 to $31 665, all well below the WTP threshold of $100 000 (eTable 3 and eFigures 1-5 in the Supplement). The ICER for total medical costs was below the WTP threshold of $100 00 for all models (range, $24 241-$51 414) except for when using the EQ-5D mapping algorithm by Xie et al25 ($107 796; 95% CI, –$4446 to $412 770) (eTable 3 and eFigures 4 in the Supplement).32
Discussion
This economic evaluation is the first study, to our knowledge, to assess the cost-effectiveness of physical therapy when considered as an alternative to glucocorticoid injection. The primary aim was to estimate the economic benefit of one common treatment for knee osteoarthritis over another, given the quality-of-life improvement and cost associated with each. This analysis suggests that an initial strategy of physical therapy is cost-effective at 1 year compared with an initial strategy of glucocorticoid injection, despite being more expensive than a glucocorticoid injection. Considering all the knee-related care costs during the entire 1-year follow-up, physical therapy resulted in an ICER of $8103 per QALY, which is well below the minimum WTP threshold of $100 000.
Costs, in both time and dollars, are likely relevant decision factors driving the use of each treatment. Physical therapy in this trial involved a typical course of 8 visits during 4 weeks, whereas the injection can be delivered during the initial consultation with guidance for 72 hours of reduced patient activity. For individuals who work or have other responsibilities, the idea of 1 injection could appear more favorable than 8 physical therapy sessions. Missing work to attend sessions can initially appear as a greater burden. However, the notion that 1 or more glucocorticoid injections will fix the problem is also not realistic. In this trial, most patients needed multiple injections (mean, 2.6). In our trial, 14 individuals in the injection group eventually went to physical therapy, and 4 individuals underwent surgery. None in the physical therapy group had surgery. This finding could explain some of the higher-than-expected costs in the injection group. Patients should be made aware of these outcomes when considering the 2 treatment options, as well as the short-term efficacy of a single glucocorticoid injection, typically 1 to 6 weeks,34,35,36 in addition to the associated risks.10,11 Patients may be told an injection can reduce acute pain to ensure that physical therapy is tolerable. The short-term improvement in pain was equal for both interventions in our trial. Prior studies12,13 have found that adding corticosteroid injections to physical therapy or exercise therapy does not improve outcomes beyond the use of these interventions alone.
Other studies26,27,37,38 have assessed the cost-effectiveness of physical therapy for knee osteoarthritis. Bove and colleagues26 compared 4 physical therapy regimens: exercise and manual therapy or exercise alone, each with and without booster treatment sessions. Booster sessions typically consist of 1 to 3 visits that occur several months after the initial physical therapy episode of care to provide additional treatment, check exercises, and provide further reassurance and encouragement. Either treatment group was more cost-effective if it included the booster sessions, despite the additional cost incurred with the extra visits. In similar fashion, our trial also included an option for a booster session for all patients in both the physical therapy and corticosteroid injection arms. Silva et al27 found a 3-year physical activity program for nonactive patients with knee osteoarthritis to be cost-effective when considering long-term improvements in QALYs and reductions in diabetes and cardiovascular disease severity. The ICER in the study by Bove et al26 was $12 900 per QALY gained and was $16 100 per QALY gained for Silva et al.27 In a study in New Zealand,37 exercise therapy and manual physical therapy were both cost-effective compared with usual care, but the combination of both was not. For the group that received a combination of both, investigators noted time restraints that likely reduced the dosing and potentially the effect size. Those findings are noteworthy, although that study had a different comparator than was used in our study, given that the physical therapy program in our study integrated manual techniques with exercise therapy, and patients received an adequate dose of both. Another study38 in the UK found 12 sessions of physical therapy to be cost-effective during a 30-month period when compared with usual care.
After a series of robust sensitivity analyses based on various assumptions, our results remained unchanged. Physical therapy remained cost-effective compared with glucocorticoid injection in every sensitivity model associated with knee-related medical costs. When considering total medical costs for any reason, all models except for one found physical therapy to be cost-effective. Although this was only 1 of 6 models, total medical costs for any reason is likely not ideal for measuring cost-effectiveness because there is the potential for many additional confounders when considering total health costs for any reason (compared with only knee-related costs). Many of these factors are outside the ability of the research team to control in the analysis (eg, comorbidities or unrelated operations and procedures).
Limitations
We used a single-payer government health system, which can limit the generalizability of these findings to other US health systems. For example, individuals seeking care in military hospitals and clinics do not usually have copayments, and direct cost would not be a barrier to seeking care. Costs of physical therapy can vary widely; therefore, different health plans could affect the cost-effectiveness of this intervention. Our focus was on the health care perspective, and as such, we did not capture data from the societal perspective; however, it is likely that the generalizability of results that focus on the societal perspective would also have been limited to this particular setting. Although we had outcomes from the WOMAC available at 5 time points, the costs represented a single value of costs expensed during the entire year and therefore could not be attributed to each of the time points individually. Finally, we used a mapping algorithm to generate EQ-5D values from the WOMAC, and although we conducted multiple sensitivity analyses using several other prominent mapping algorithms, it is possible that results would be different if QALYs were available directly from the EQ-5D. These results need validation in other settings.
Conclusions
A course of physical therapy was a cost-effective intervention compared with a course of glucocorticoid injections for patients enrolled in this trial. Clinicians should consider that although the initial cost of delivering physical therapy may be slightly higher than an initial glucocorticoid injection, the mean improvement in QALYs at 1 year may also be greater with physical therapy. The combination of superior long-term outcomes, cost-effectiveness, and low risk with physical therapy as provided in this clinical trial provides an additional perspective to inform shared decision-making about value-based case between health care practitioners and patients.
eAppendix. International Classification of Diseases (ICD) Codes–9th and 10th Edition and Current Procedural Terminology (CPT) Codes Associated With Knee Osteoarthritis and Knee-Related Care
eReferences
eTable 1. Impact Inventory
eTable 2. Models Without Accounting for Any Covariates (Unadjusted Models)
eTable 3. Sensitivity Analyses for Primary Cost-Effectiveness Analysis
eFigure 1. Histogram of QALY Scores in Each Intervention Group
eFigure 2. Histogram of Knee-Related Costs Scores in Each Intervention Group
eFigure 3. Histogram of Total Costs Scores in Each Intervention Group
eFigure 4. Cost-effectiveness Planes and Acceptability Curves for the Sensitivity Analyses
References
- 1.Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323(9):863-884. doi: 10.1001/jama.2020.0734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallace IJ, Worthington S, Felson DT, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A. 2017;114(35):9332-9336. doi: 10.1073/pnas.1703856114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61(1):7-16. doi: 10.1177/0036933015619588 [DOI] [PubMed] [Google Scholar]
- 4.Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020;72(2):220-233. doi: 10.1002/art.41142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dhawan A, Mather RC III, Karas V, et al. An epidemiologic analysis of clinical practice guidelines for non-arthroplasty treatment of osteoarthritis of the knee. Arthroscopy. 2014;30(1):65-71. doi: 10.1016/j.arthro.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 6.Rhon D, Hando B, Deyle G. Use of physical therapy and corticosteroid injections in the management of knee osteoarthritis in the U.S. military health system. Osteoarthritis Cartilage. 2016;24:S233-S234. doi: 10.1016/j.joca.2016.01.452 [DOI] [Google Scholar]
- 7.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2000;132(3):173-181. doi: 10.7326/0003-4819-132-3-200002010-00002 [DOI] [PubMed] [Google Scholar]
- 8.Deyle GD, Allison SC, Matekel RL, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85(12):1301-1317. doi: 10.1093/ptj/85.12.1301 [DOI] [PubMed] [Google Scholar]
- 9.Abbott JH, Robertson MC, Chapple C, et al. ; MOA Trial team . Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial, 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525-534. doi: 10.1016/j.joca.2012.12.014 [DOI] [PubMed] [Google Scholar]
- 10.Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A. Intra-articular corticosteroid injections in the hip and knee: perhaps not as safe as we thought? Radiology. 2019;293(3):656-663. doi: 10.1148/radiol.2019190341 [DOI] [PubMed] [Google Scholar]
- 11.Wijn SRW, Rovers MM, van Tienen TG, Hannink G. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. Bone Joint J. 2020;102-B(5):586-592. doi: 10.1302/0301-620X.102B5.BJJ-2019-1376.R1 [DOI] [PubMed] [Google Scholar]
- 12.Soriano-Maldonado A, Klokker L, Bartholdy C, et al. Intra-articular corticosteroids in addition to exercise for reducing pain sensitivity in knee osteoarthritis: exploratory outcome from a randomized controlled trial. PLoS One. 2016;11(2):e0149168. doi: 10.1371/journal.pone.0149168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henriksen M, Christensen R, Klokker L, et al. Evaluation of the benefit of corticosteroid injection before exercise therapy in patients with osteoarthritis of the knee: a randomized clinical trial. JAMA Intern Med. 2015;175(6):923-930. doi: 10.1001/jamainternmed.2015.0461 [DOI] [PubMed] [Google Scholar]
- 14.What is value-based healthcare? NEJM Catalyst. January 1, 2017. Accessed September 10, 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
- 15.Deyle GD, Allen CS, Allison SC, et al. Physical therapy versus glucocorticoid injection for osteoarthritis of the knee. N Engl J Med. 2020;382(15):1420-1429. doi: 10.1056/NEJMoa1905877 [DOI] [PubMed] [Google Scholar]
- 16.Medicare Physician Fee Schedule 2020 CMS-1715-F. Published November 15, 2019. Accessed August 14, 2020. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1715-F
- 17.Sanders GD, Maciejewski ML, Basu A. Overview of cost-effectiveness analysis. JAMA. 2019;321(14):1400-1401. doi: 10.1001/jama.2019.1265 [DOI] [PubMed] [Google Scholar]
- 18.Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316(10):1093-1103. doi: 10.1001/jama.2016.12195 [DOI] [PubMed] [Google Scholar]
- 19.Husereau D, Drummond M, Petrou S, et al. ; ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force . Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231-250. doi: 10.1016/j.jval.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 20.Deyle GD, Gill NW, Rhon DI, et al. A multicenter randomised, 1-year comparative effectiveness, parallel-group trial protocol of a physical therapy approach compared to corticosteroid injection on pain and function related to knee osteoarthritis (PTA Trial). BMJ Open. 2016;6(3):e010528. doi: 10.1136/bmjopen-2015-010528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altman RD. Criteria for the classification of osteoarthritis of the knee and hip. Scand J Rheumatol 1987;16(sup65):31-39. doi: 10.3109/03009748709102175 [DOI] [PubMed] [Google Scholar]
- 22.Rhon DI, Clewley D, Young JL, Sissel CD, Cook CE. Leveraging healthcare utilization to explore outcomes from musculoskeletal disorders: methodology for defining relevant variables from a health services data repository. BMC Med Inform Decis Mak. 2018;18(1):10. doi: 10.1186/s12911-018-0588-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. doi: 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wailoo A, Hernandez Alava M, Escobar Martinez A. Modelling the relationship between the WOMAC Osteoarthritis Index and EQ-5D. Health Qual Life Outcomes. 2014;12:37. doi: 10.1186/1477-7525-12-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43(3):203-220. doi: 10.1097/00005650-200503000-00003 [DOI] [PubMed] [Google Scholar]
- 26.Bove AM, Smith KJ, Bise CG, et al. Exercise, manual therapy, and booster sessions in knee osteoarthritis: cost-effectiveness analysis from a multicenter randomized controlled trial. Phys Ther. 2018;98(1):16-27. doi: 10.1093/ptj/pzx104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silva GS, Sullivan JK, Katz JN, Messier SP, Hunter DJ, Losina E. Long-term clinical and economic outcomes of a short-term physical activity program in knee osteoarthritis patients. Osteoarthritis Cartilage. 2020;28(6):735-743. doi: 10.1016/j.joca.2020.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith KC, Paltiel AD, Yang HY, Collins JE, Katz JN, Losina E. Cost-effectiveness of health coaching and financial incentives to promote physical activity after total knee replacement. Osteoarthritis Cartilage. 2018;26(11):1495-1505. doi: 10.1016/j.joca.2018.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796-797. doi: 10.1056/NEJMp1405158 [DOI] [PubMed] [Google Scholar]
- 30.Cameron D, Ubels J, Norström F. On what basis are medical cost-effectiveness thresholds set? clashing opinions and an absence of data: a systematic review. Glob Health Action. 2018;11(1):1447828. doi: 10.1080/16549716.2018.1447828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barton GR, Sach TH, Jenkinson C, Avery AJ, Doherty M, Muir KR. Do estimates of cost-utility based on the EQ-5D differ from those based on the mapping of utility scores? Health Qual Life Outcomes. 2008;6:51. doi: 10.1186/1477-7525-6-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie F, Pullenayegum EM, Li S-C, Hopkins R, Thumboo J, Lo N-N. Use of a disease-specific instrument in economic evaluations: mapping WOMAC onto the EQ-5D utility index. Value Health. 2010;13(8):873-878. doi: 10.1111/j.1524-4733.2010.00770.x [DOI] [PubMed] [Google Scholar]
- 33.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? some practical clarifications of multiple imputation theory. Prev Sci. 2007;8(3):206-213. doi: 10.1007/s11121-007-0070-9 [DOI] [PubMed] [Google Scholar]
- 34.Hepper CT, Halvorson JJ, Duncan ST, Gregory AJM, Dunn WR, Spindler KP. The efficacy and duration of intra-articular corticosteroid injection for knee osteoarthritis: a systematic review of level I studies. J Am Acad Orthop Surg. 2009;17(10):638-646. doi: 10.5435/00124635-200910000-00006 [DOI] [PubMed] [Google Scholar]
- 35.Jüni P, Hari R, Rutjes AWS, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015;10(10):CD005328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. PLoS One. 2017;12(6):e0178621. doi: 10.1371/journal.pone.0178621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pinto D, Robertson MC, Abbott JH, Hansen P, Campbell AJ; MOA Trial Team . Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee. 2: economic evaluation alongside a randomized controlled trial. Osteoarthritis Cartilage. 2013;21(10):1504-1513. doi: 10.1016/j.joca.2013.06.014 [DOI] [PubMed] [Google Scholar]
- 38.Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res (Hoboken). 2012;64(2):238-247. doi: 10.1002/acr.20642 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. International Classification of Diseases (ICD) Codes–9th and 10th Edition and Current Procedural Terminology (CPT) Codes Associated With Knee Osteoarthritis and Knee-Related Care
eReferences
eTable 1. Impact Inventory
eTable 2. Models Without Accounting for Any Covariates (Unadjusted Models)
eTable 3. Sensitivity Analyses for Primary Cost-Effectiveness Analysis
eFigure 1. Histogram of QALY Scores in Each Intervention Group
eFigure 2. Histogram of Knee-Related Costs Scores in Each Intervention Group
eFigure 3. Histogram of Total Costs Scores in Each Intervention Group
eFigure 4. Cost-effectiveness Planes and Acceptability Curves for the Sensitivity Analyses