Abstract
The exact incidence of Mullerian agenesis is unknown because women with this condition might be asymptomatic and diagnosis is mostly incidental. We report an incidental finding of left Mullerian agenesis involving the left fallopian tube, left ovary, and the left kidney following evaluation and treatment for a right tubal ectopic pregnancy.
Keywords: absent fallopian tube and ovary, absent kidney, Mullerian anomaly
Congenital unilateral or bilateral Mullerian agenesis with renal involvement is a rare event. Diagnosis is mostly incidental. Where desired and possible, fertility should be preserved. If not possible, the patient should be counseled on alternative reproductive options.

1. INTRODUCTION
Congenital absence of an adnexa impacts a patient's fertility potential and could be associated with renal anomalies. Preservation of the existing healthy organ(s) should be the rule and when this is not possible, adequate patient counseling, informed consent, and psychological support should be provided. Congenital absence of the fallopian tube and ovary is a rare finding. The exact incidence is unknown; a rate of 1 in 11,000–12,000 has been quoted in the literatures. 1 , 2 , 3 , 4 , 5 The exact mechanism of occurrence is difficult to determine but many researchers attribute this to one of two possibilities; a congenital absence of the paramesonephric ducts or unilateral torsion and/or vascular accident with necrosis and auto‐amputation of the adnexa during intrauterine life, childhood, or in adult life. 2 , 3 , 4 , 5 We here report an incidental laparoscopic finding of unilateral absence of the left fallopian tube and ovary in a patient undergoing surgical treatment of ectopic pregnancy. A literature review 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 and possible aetiopathogenesis are discussed.
2. CASE REPORT
Ms SM was 36 years old in her second pregnancy who presented to our early pregnancy assessment unit with complaint of irregular vaginal bleeding of 1‐week duration and 8 weeks amenorrhoea. In her first pregnancy, she was delivered via an emergency cesarean section ten months earlier. Following her presentation, she had a transvaginal ultrasound scan which showed an empty uterine cavity with an endometrial thickness measuring 23.0 mm. The right adnexa showed an inhomogeneous mass measuring 49 mm × 24 mm × 24 mm with a visible gestational sac which contained an embryo with a crown‐lump length of 22.2 mm, equivalent to 8 weeks and 6 days gestational age. There was no visible fetal heartbeat. The right ovary was normal. The left ovary was not visualized. There was no haemoperitoneum. A diagnosis of right tubal ectopic pregnancy was made. She gave no history of recent or past pelvic infection, no previous tubal or adnexal surgery, no previous history of acute abdomen, no use of contraceptive, and she was not a smoker. Her blood tests were normal, serum beta human chorionic gonadotrophin level was 22,329 IU/L. She was counseled and consented for a diagnostic laparoscopy and surgical treatment of ectopic pregnancy. Intraoperatively, we noted a complete absence of the left fallopian tube and ovary (blue arrow in Figure 1). The right ovary appeared healthy; the right fallopian tube harboring the ectopic pregnancy was removed (yellow arrow in Figure 2). Postoperatively she was debriefed and discharged the next day. Four weeks later, she had a renal ultrasound scan which showed an absent left kidney (red arrow in Figure 3) with a normal right kidney (white arrow in Figure 4) and bladder. She continued to menstruate, indicating normal ovarian function. She was counseled regarding reproductive options and discharged.
FIGURE 1.
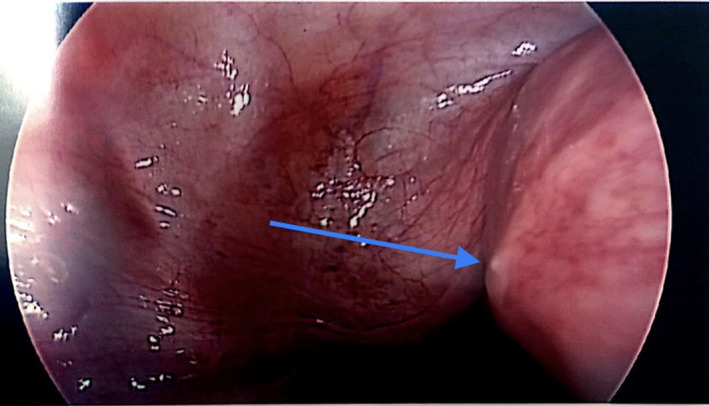
The blue arrow indicates the left uterine Cornu with no tube, round ligament and ovary
FIGURE 2.

The yellow arrow shows the right Fallopian tube stump following right salpinhectomy
FIGURE 3.

Ultrasound image of the left renal bed (red arrow) with no kidney visualised on ultrasound scan
FIGURE 4.

Ultrasound image of the right renal bed showing a well developed right kidney (white arrow)
3. DISCUSSION
Unexplained unilateral or less commonly bilateral absence of the ovary and/or tube in the presence of a normal uterus is a rare finding. 2 , 3 Sometimes, it is difficult to determine the exact cause in any individual patient but three possible mechanism of etiology has been reported in the literatures. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 In no particular order, first is the mechanical hypothesis; this assumes an asymptomatic torsion of one or both adnexa (or either of tube or ovary) during intrauterine development of the fetus, childhood, or adult life. This is believed to result in ischemic necrosis and auto‐amputation of the affected organ. 6 , 7 , 8 The second possible etiology is during organogenesis. Embryologically, the uterus and fallopian tubes develop from the paramesonephric ducts while the ovaries develop from the urogenital ridge with the germ cells arising from the yolk sac. 2 , 6 A defective development or resorption of either of the aforementioned embryological tissues would result in unilateral or bilateral absence of the tube(s) and ovary(ies). This is also more likely to lead to concomitant renal anomalies. 6 Finally, an unexplained asymptomatic vascular accident with ischemic necrosis and resorption of the affected organ during intrauterine or extra‐uterine life has been suggested. 7
This patient had no recollection of an acute abdominal event as a child or adult; an acute pain is one of the typical presenting features of organ torsion associated with ischemia and necrosis. 5 , 6 , 7 Intraoperatively, we did not find any vestigial tissue or fibrous bands suggestive of a previously existing organ that may have undergone infarction. This leaves us with congenital non‐development of the paramesonephric duct and urogenital ridge structures as possible explanation for this finding. This is because she had an absent left ovary, with absent fallopian tube and renal system on the same side. 3 These organs were present, appeared healthy, and functioning normally on the right side safe for the ectopic pregnancy. This possibility is reinforced by findings from similar case reports. 10 , 11
We observe that majority of the patients reported in the literature as detailed in Table 1 had their diagnosis while being investigated for infertility, 1 , 2 , 3 , 5 , 7 , 8 , 9 , 11 , 13 Ms SM never had difficulty with conception but ectopic pregnancy has been reported as a complication of mullerian anomalies. 13 She had salpingectomy which effectively means she would be incapable of a normal natural conception. 9 She was debriefed and counseled on the alternative ways of getting pregnant including the use of in vitro fertilization using own gametes since had a normal right ovary and child adoption. From our literature search (Table 1), 14 of the 22 patients reported, just like our patient had their abnormality on the left side. 1 , 2 , 3 , 4 , 5 , 6 , 8 , 9 , 10 , 11 , 12 The reason for this preponderance is not immediately clear but calls for further research.
TABLE 1.
Literature reports
| Author (Reference) | Indication | Absent adnexal organ | Uterine anomalies | Renal system anomalies |
|---|---|---|---|---|
| Uckuyu et al. 1 | ||||
| Case 1 | Infertility | Left ovary and tube | Normal | Normal |
| Case 2 | Infertility | Right tube | Normal | Not reported |
| Case 3 | Infertility | Left ovary | Normal | Normal |
| Case 4 | Acute abdomen | Left ovary | Normal | Normal |
| Yerebasmaz et al. 2 | ||||
| Case 1 | Acute abdomen | Right fallopian tube and ovary | Not reported | Normal |
| Case 2 | Chronic pelvic pain | Right ovary and tube | Not reported | Normal |
| Case 3 | Adnexal mass | Left fallopian tube and ovary | Not reported | Normal |
| Case 4 | Infertility | Left ovary | Not reported | Normal |
| Sivanesaratnam 3 | ||||
| Case 1 | Sterilization | Left fallopian tube and ovary | Normal | Normal |
| Case 2 | Infertility | Right ovary and tube | Not reported | Normal |
| Tzitzimikas et al. 4 | Acute pelvic pain | Left ovary | Normal | Normal |
| Rastogi et al. 5 | Infertility |
Left ovary and tube |
Normal | Normal |
| Sirisena 6 | Acute abdomen | Left fallopian tube and left ovary | Normal | Normal |
| Eustace 7 | ||||
| Case 1 | Infertility | Right ovary and tube | Normal | Normal |
| Case 2 | Sterilization | Right ovary and tube | Not reported | Not reported |
| Chen et al. 8 | Infertility | Left ovary and tube | Normal | Not reported |
| Pabuccu et al. 9 | Infertility | Left ovary and tube | Normal | Normal |
| Haydardedeoglu et al. 10 | Hysterectomy for fibroid uterus | Left ovary | Unicornuate uterus | Ipsilateral renal agenesis |
| Mulayim et al. 11 | Infertility | Left tube and ovary | Unicornuate uterus | Pelvic kidney |
| Barsky et al. 13 | ||||
| Case 1 | Adnexal torsion | Left ovary and tube | Normal | Normal |
| Case 2 | Adnexal tumor | Right ovary and tube | Normal | Normal |
| Vaiarelli et al. 12 | Infertility | Right ovary and tube | Normal | Normal |
In conclusion, congenital absence of the left kidney, ovary, and fallopian tube are rare events. An incidental finding such as ours should prompt further evaluation to detect co‐existing anomalies. These are important considerations in patient counseling especially with regard to lifestyle modification and/or choices to ensure healthy preservation of existing organ(s).
CONFLICT OF INTEREST
We report no conflict of interest.
AUTHOR CONTRIBUTION
JM and OO conceptualized the case. JM, AO, OO, and NE reviewed the literature. JM and AO with contributions from CO and ZA wrote the initial draft. All authors read and approved the final manuscript.
CONSENT
Informed consent was obtained from the patient to publish this case reports/images in accordance with the journal's patient consent policy and for the sole purpose of advancing scientific knowledge.
ACKNOWLEDGEMENT
We acknowledge every member of the multidisciplinary team that co‐managed the patient and supported in her care.
Mamah JE, Ofodile OO, Onyebuchi AK, Otu CR, Aliyu‐Abubakar Z, Egbuonu N. Unexplained left Mullerian agenesis with agenesis of left kidney: A case report. Clin Case Rep. 2022;10:e05273. doi: 10.1002/ccr3.5273
Funding information
The authors received no external funding for this case report
REFERENCES
- 1. Uckuyu A, Ozcimen EE, Ciftci CS. Unilateral congenital ovarian and partial tubal absence: report of four cases with review of the literature. Fert Steril. 2009;91:936.e5‐936.e8. [DOI] [PubMed] [Google Scholar]
- 2. Yerebasmaz N, Dilbaz B, Sengul O, Cakir L. Four cases with congenital unilateral absence of ovary and fallopian tube: review of the literature. J Clin Anal Med. 2016;7(Suppl 3):275‐278. [Google Scholar]
- 3. Sivanesaratnam V. Unexplained unilateral absence of ovary and fallopian tube. Eur J Obstet Gynecol Reprod Biol. 1986;22:103‐105. [DOI] [PubMed] [Google Scholar]
- 4. Tzitzimikas S, Fragkos M, Karavida A, Mettler L. Unilateral ovarian absence. Gynecol Surg. 2013;10:93‐95. [Google Scholar]
- 5. Rastogi R, Gupta Y, Gupta B, et al. Unilateral Agenesis of Adnexa – A Rare Clinico‐Radiological Condition. Journal of Medical Diagnostic Methods. 2016;5(4):228. doi: 10.4172/2168-9784.1000228 [DOI] [Google Scholar]
- 6. Sirisena LA. Unexplained absence of an ovary and uterine tube. Postgrad Med J. 1978;54:423‐424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eustace DL. Congenital absence of fallopian tube and ovary. Eur J Obstet Gynecol Reprod Biol. 1992;46:157‐159. [DOI] [PubMed] [Google Scholar]
- 8. Chen B, Yang C, Sahebally Z, Jin H. Unilateral ovarian and fallopian tube agenesis in an infertile patient with a normal uterus. Exp Therapeut Med. 2014;8:831‐835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pabuccu E, Kahraman K, Taskin S, Atabekoglu C. Unilateral absence of fallopian tube and ovary in an infertile patient. Fert Steril. 2011;96(1):e55‐e57. [DOI] [PubMed] [Google Scholar]
- 10. Haydardedeoglu B, Simsek E, Kilicdag E, Tarim E, Aslan E, Bagis T. A case of unicornuate uterus with ipsilateral ovarian and renal agenesis. Fert Steril. 2006;85:750.e1‐750.e4. [DOI] [PubMed] [Google Scholar]
- 11. Mulayim B, Demirbasoglu S, Oral O. Unicornuate uterus and unilateral ovarian agenesis associated with pelvic kidney. Surg Endosc. 2003;17:161‐163. [DOI] [PubMed] [Google Scholar]
- 12. Barsky M, Beaulieu AM, Sites CK. Congenital ovarian‐fallopian tube agenesis predisposes to premature surgical menopause: a report of two cases. J Androl Gynaecol. 2015;3(1):3‐6. [Google Scholar]
- 13. Vaiarelli A, Luk J, Patrizio P. Ectopic pregnancy after IVF in a patient with unilateral agenesis of the fallopian tube and ovary and with endometriosis: search of the literature for these associations. J Assist Reprod Genet. 2012;29:901‐904. [DOI] [PMC free article] [PubMed] [Google Scholar]


